Abstract
Recently there has been considerable concern related to the presence of bacteria, in particular Enterobacter sakazakii, in powdered infant formula milk. This paper considers the bacteria in these products at point of sale, with reference to current microbiological testing and the need for good hygienic practice in their subsequent preparation before feeding. The ingestion of raised numbers of E. sakazakii resulting from temperature abuse after reconstitution is highlighted as well as the uncertain routes of E. sakazakii product contamination.
Keywords: Enterobacter sakazakii, powdered infant milk formula
The microbial flora of powdered infant formula milk
The newborn infant has a sterile gastrointestinal tract that is quickly colonized through oral ingestion (Mackie et al. 1999). Where appropriate, powdered infant formula milk (PIF) is offered in place of breast milk and therefore influences the development of the gut flora. PIF is not a sterile product and various microbiological tests are applied to samples from each production batch which are compared with microbiological criteria. These values are set by the Codex Alimentarius Commission (i.e. CAC 1979), company–company agreements as well as ‘in‐house’ levels regarded as workable based upon prior experience.
Specific microbes commonly tested for in PIF are Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, Enterobacteriaceae (or coliforms) and Salmonella. In addition, the general microbial flora is counted and is referred to as the ‘aerobic plate count’ (APC). The APC determines the general microbial load as a measure of quality and does not reflect the presence of pathogenic organisms. In contrast, S. aureus, B. cereus, C. perfringens and Salmonella serovars are specified pathogens and their presence in PIF could be serious for the infant. A number of S. aureus strains are capable of producing enterotoxins which are resistant to most cooking time‐temperature regimes. The toxin is only produced in sufficient quantities when the bacterial number exceeds 104 cells per gram. Therefore, it is reasonable for a certain level of S. aureus to be tolerable. B. cereus can also produce toxins and survives mild heat treatment such as boiling because of spore formation. Again as this organism is in the environment (in particular soil and plant material), there is a regular exposure to the organism and hence a certain level is deemed tolerable in many foods. The Enterobacteriaceae direct count (or the slightly more specific test ‘coliform’ test) direct count is used to measure the number of enteric‐like organisms that are present in the sample. These organisms commonly inhabit the large intestines of animals and humans as well as soil and are not necessarily harmful. Therefore, their presence is used only as an indication of the presence of serious intestinal pathogens. In simple terms, the Enterobacteriaceae direct count test determines whether heat‐treatment has been adequate, or if post‐treatment contamination has occurred. However, this group of microbes has been hard to specifically define over the years, and the test does not allow for the recovery of bacterial cells which may be injured during processing (i.e. dehydration) and need resuscitation before they can grow on selective agars. The current ‘Enterobacteriaceae’ direct count test therefore does not guarantee the absence of enteric pathogens. Hence currently there is an additional specific requirement for PIF to be tested for Salmonella, which are members of the Enterobactericaeae family. Salmonella has been extensively studied over the years and numerous test methods have been developed. It is possible for industry to manufacture foods without this organism and so a ‘zero tolerance’ has been applied worldwide. Although Enterobacter sakazakii is a member of the Enterobacteriaceae, the ‘Enterobacteriacae’ and ‘coliform’ direct count test does not always detect the organism in PIF samples (Iversen & Forsythe 2004). This probably results from the low cell number and injury to the organism during desiccation. Therefore, specific test methods are being developed (cf. Fig. 1) and microbiological criteria for PIF revised by international authorities, which are expected to be published in 2005.
Figure 1.
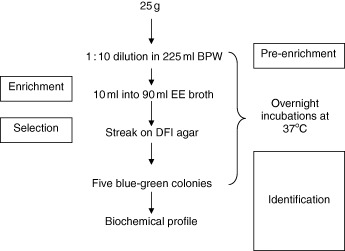
Presence–absence test method for Enterobacter sakazakii (Iversen et al. 2004a). BPW, buffered peptone water; EE, enterobacteriaceae enrichment broth; DFI agar, Druggan‐Forsythe‐Iversen chromogenic agar.
Muytjens et al. (1988) and Iversen & Forsythe (2004) reported the isolation of the Enterobacteriaceae from PIF samples after pre‐enrichment (resuscitation) procedures. The Enterobacteriacae isolated included Enterobacter agglomerans (now called Pantoea and Escherichia vulneris), E. cloacae, E. sakazakii, Citrobacter koseri (formerly C. diversus), C. freundii and Klebsiella oxytoca. Iversen & Forsythe (2004) also reported the absence of Salmonella.
The 2004 Food and Agriculture Organization of the United Nations and World Health Organization (FAO‐WHO) meeting in Geneva to consider ‘E. sakazakii and other microorganisms in powdered infant formula’ reviewed the published refereed literature concerning bacterial infections attributed to PIF (FAO‐WHO 2004). It also reviewed what is known about possible infectious organisms and categorized them into three groups:
Category A, Clear evidence of causality; Salmonella and E. sakazakii.
Category B, Causality plausible, but not yet demonstrated; E. vulneris, C. koseri, E. cloacae, Hafnia alvei, Pantoea agglomerans, Klebsiella pneumoniae, K. oxytoca.
Category C, Causality less plausible or not yet demonstrated; Clostridium botulinum, S. aureus, Listeria monocytogenes and B. cereus.
Therefore, currently only Salmonella and E. sakazakii are attributed to causing neonatal infection through contaminated PIF.
Enterobacter sakazakii
Enterobacter sakazakii is a motile, nonsporeforming, Gram‐negative facultative anaerobe. It was known as ‘yellow pigmented Enterobacter cloacae’ until 1980 when it was designated by Farmer et al. as a new species and named in honour of the Japanese bacteriologist Riichi Sakazaki.
Enterobacter sakazakii is an occasional contaminant of PIF that can cause a rare, but life‐threatening form of neonatal meningitis, bacteraemia, necrotizing enterocolitis (NEC) and necrotizing meningoencephalitis after ingestion (Muytjens et al. 1983; Iversen & Forsythe 2003). The organism was first associated with neonatal deaths in 1958 by Urmenyi & Franklin (1961). Recently, the International Commission on Microbiological Specification for Foods (2002) ranked the organism as ‘Severe hazard for restricted populations, life threatening or substantial chronic sequelae of long duration’. Subsequently it has the same ranking as more familiar food and waterborne pathogens such as L. monocytogenes, C. botulinum types A and B and Cryptosporidium parvum.
A risk profile of E. sakazakii has already been published by Iversen & Forsythe (2003) and a detailed risk analysis by the FAO‐WHO (2004). A review of reported cases and sources of E. sakazakii can be found in the author's previous risk profile and so will not be reproduced in detail here. Nevertheless, it is pertinent to state that although the neonatal meningitis cases resulting from E. sakazakii are rare, the number of attributable NEC cases are less certain. NEC is the most common important gastrointestinal illness in the premature newborn and can be caused by a variety of bacterial pathogens. The pathogenesis is associated with neonatal intestinal ischaemia, microbial colonization of the gut and excess protein substrate in the intestinal lumen. The latter is associated with oral formula feeding. It has an incidence of 2–5% in premature infants and 13% in those weighing less than 1.5 kg at birth. Lucas & Cole (1990) reported that NEC is 10 times as common in babies fed with formula milk compared with those fed with breast milk. Both meningitis and NEC caused by E. sakazakii have high mortality rate of 40–80% and 10–55%, respectively. In a study of 125 neonates with NEC, Enterobacter spp. were the most common organisms, being isolated from 29% of patients (Chan et al. 1994). Van Acker et al. (2001) described 12 cases of NEC in neonates that occurred in 1998. In the outbreak, a total of 11 E. sakazakii strains were isolated from a cohort of 50 neonates from stomach aspirate anal swabs and blood samples.
The first reported cases of meningitis caused by ‘yellow‐pigmented E. cloacae’ occurred in the UK (Urmenyi & Franklin 1961). Since then cases have been reported worldwide including countries such as Denmark, Iceland, the Netherlands, Greece, Canada and the USA. Most reports are from hospital nurseries and neonatal intensive care units. It is probable that premature infants and those with underlying medical conditions are at highest risk for developing an E. sakazakii infection. However, it has been reported that a healthy, full‐term, newborn infant in Iceland became ill prior to hospital discharge and suffered permanent neurological sequelae as a result of an E. sakazakii infection (Health Canada Food Program 2002). The low incidence is predictable as healthy neonates not requiring intensive care will be less susceptible to E. sakazakii infection. Muytjens et al. (1983) re‐evaluated Enterobacter strains from blood and cerebral spinal fluid (CSF) and uncovered several cases of meningitis and bacteraemia caused by E. sakazakii infection. This suggests that the organism had been under‐reported. In addition to the reported 40–80% case‐fatality rate for E. sakazakii meningitis, it should be recognized that in survivors, severe neurological sequelae such as hydrocephalus, quadriplegia and retarded neural development often occur.
Enterobacter sakazakii infection of the neonate
Figure 2 shows that sources of E. sakazakii in contaminated PIF are the powder itself, the equipment and possibly personnel preparing the feed. To date there is no evidence of infection of the newborn baby through vertical transmission from the mother during birth (Muytjens & Kollée 1990). The first reported association of E. sakazakii with contaminated PIF was by Muytjens et al. (1983). In this outbreak E. sakazakii was isolated from prepared milk formula, a dish brush and a stirring spoon.
Figure 2.

Risk factors concerning the ingestion of Enterobacter sakazakii. a. Source contamination of powdered infant formula milk (PIF). b. Contamination of PIF by people during reconstitution, that is, faecal carriage rate. c. Contamination of PIF during reconstitution resulting from unclean equipment, that is, spoon. d. Contamination of fresh reconstitution PIF resulting from inadequate cleaning of contaminated feeding bottle. e. Death of E. sakazakii resulting from temperature of water used to reconstitute PIF. f. Multiplication of E. sakazakii following reconstitution, prior to ingestion, that is, room temperature storage. g. Survival and possible growth of E. sakazakii in the neonate stomach prior to transit into the small intestines.
Enterobacter sakazakii incidence in powdered infant formula milk
As stated earlier, PIF preparations are not manufactured as sterile products. In fact the paper by Farmer et al. (1980) defining E. sakazakii species includes a strain which was originally isolated from dried milk in 1960. Therefore, E. sakazakii has been present in dried milk products for many decades. Muytjens et al. (1988) found 14% of 141 PIF samples contained E. sakazakii. In total E. sakazakii was cultured from unused infant formula products from 13 countries. The level of contamination ranged from 0.36 to 66.0 cfu per 100 g. This is similar to the value of 8 cells per 100 g estimated by Simmons et al. (1989) for an open can of powdered milk formula used during the time of an outbreak on a neonatal intensive care unit. Nazarowec‐White & Farber (1997a) tested 120 cans of infant formula from five different companies in Canada and found 6.7% contained E. sakazakii. The levels of E. sakazakii in positive samples were frequently 0.36 cfu per 100 g.
More recently, Iversen & Forsythe (2004) reported that 3/102 PIF, 5/49 dried baby foods and 3/72 milk powders contained E. sakazakii. Our group uses a specific chromogenic agar to isolate E. sakazakii from food samples. The medium is called the ‘Druggan‐Forsythe‐Iversen’ agar and its formula is given in two papers (Iversen & Forsythe 2004; Iversen et al. 2004a); alternatively it can be purchased from Oxoid Ltd (UK, CM1055). In general these reports show that when the organism is present in PIF the levels are very low: less than one bacterial cell per gram. Despite the dry nature of PIF, the organism is able to survive in the powder for at least 12 months (Caubilla‐Barron et al. 2004).
Personnel
The faecal carriage of the organism has not been demonstrated and so it is uncertain how often contamination of PIF may occur during preparation. However, it is well accepted that basic aspects of personnel hygiene are frequently ignored and poor hygienic practice has been the probable source of outbreaks (Clark et al. 1990; Smeets et al. 1998; Block et al. 2002).
Environment
Enterobacter sakazakii has been isolated from diverse environments including soil, rats, flies, beer mugs, milk powder factories, a chocolate factory and households (Neelam et al. 1987; Skladal et al. 1993; Kandhai et al. 2004). Because of the ubiquity of the organism, cases of E. sakazakii can only be attributed to PIF if identical strains are isolated from unopened tins of the same batch.
The organism is found in the hospital environment. Nazarowec‐White & Farber (1999) studying three isolates obtained from one hospital over 11 years showed that they were indistinguishable. Smeets et al. (1998) showed that isolates from a contaminated dish brush used for cleaning bottles in a hospital and the isolates from three patients were identical making an epidemiological connection likely. The organism has also been isolated from a doctor's stethoscope (Farmer et al. 1980) and from nursery food preparation equipment such as spoons and a blender (Simmons et al. 1989; Noriega et al. 1990; Bar‐Oz et al. 2001).
Enterobacter sakazakii forms biofilms on plastic surfaces (Iversen et al. 2004b). Levels on silicon and latex from infant feeding bottles were of the order 104 bacteria cm−2 (see Fig. 3). Therefore, inefficient cleaning of the feeding bottle and utensils could result in the accumulation of the organism and act as a source of infection. Kleiman et al. (1981) and Adamson & Rogers (1981) reported separate cases of previously healthy 5‐week‐old infants admitted to hospital with meningitis caused by E. sakazakii, showing that the infection can also be acquired in the home environment.
Figure 3.

Enterobacter sakazakii biofilm on latex during growth in infant formula milk (reproduced from Iversen et al. 2004b).
Enterobacter sakazakii growth in reconstituted powdered infant formula milk
Reconstituted PIF is nutritious and can support bacterial growth when given favourable conditions of water availability, time and temperature. Therefore, once rehydrated the only remaining barriers to increased bacterial growth and risk of infection, are time and temperature.
Measuring the rate of bacterial growth at different temperatures gives graphs similar to that in Fig. 4. There are three cardinal temperatures with respect to bacterial growth: the minimum, optimum and maximum. For E. sakazakii these are 6, 39 and 46°C, respectively (Iversen et al. 2004b). As an increase in microbial numbers equates to an increased risk of infection, it is important to recognize the temperature range over which E. sakazakii (and other bacterial pathogens) can multiply. It takes approximately 14 h for E. sakazakii to double at 10°C, which is slightly above normal refrigeration, whereas at room temperature this only takes 45 min. Clearly room temperature supports rapid bacterial growth. According to FAO‐WHO (2004), after 6 h at 25°C the relative risk of ingesting E. sakazakii will increase by 30‐fold and after 10 h at 25°C the relative risk will increase by 30 000‐fold. Therefore, risk reduction can be achieved by ensuring that reconstituted PIF not for immediate use is rapidly cooled to below 10°C and that the time between reconstitution and consumption is minimized.
Figure 4.

Growth range of Enterobacter sakazakii.
Figure 3 also shows the recommended temperature range for reconstituting PIF. These temperatures are above the growth range, but are not high enough (i.e. >70°C) to rapidly kill the intrinsic bacteria. Although one early paper suggested E. sakazakii was very thermotolerant (Nazarowec‐White & Farber 1997b), subsequent work showed that the organism is less thermotolerant than L. monocytogenes (2004b, 1999), and Edelson‐Mammel & Buchanan (2004) have shown that the sensitivity to raised temperature does vary between E. sakazakii strains. Further work is required to clarify the situation.
Factors affecting the probability of infection (which is different from probability of ingestion) relate to the pathogen, the food and the host. The pathogen may be adapted to survive heat‐treatment and the acidity of the neonatal stomach. The food may have a high buffering capacity and hence protect the bacterium's transit through the stomach, and the host's immune status will affect the likelihood of infection. The infectivity therefore can vary according to the organism's history (i.e. prior adaptation to heat and acidity), the host state (healthy or immunocompromised) and food matrix. In the case of PIF and neonates, the organism will have been stressed during spray drying and storage, the host is immunocompromised and being a liquid the initial portion of the feed may pass quickly through the stomach (mild acidic conditions) into the small intestines.
Conclusion
The newborn infant is so susceptible to infections that PIF requires a high level of microbiological quality control during production, distribution and usage. It is important to ensure that PIF is prepared using good hygienic procedures, along with rapid cooling, and minimization of the time between preparation and consumption to reduce the risk of E. sakazakii infection. Despite the publicized outbreaks and product recalls, infant deaths caused by E. sakazakii infection is fortunately rarely reported.
Acknowledgements
The author is grateful for the financial and technical support of the Nottingham Trent University and Oxoid Ltd (UK).
References
- Adamson D.H. & Rogers J.R. (1981) Enterobacter sakazakii meningitis with sepsis. Clinical Microbiology Newsletter 3, 19–20. [Google Scholar]
- Bar‐Oz B., Preminger A., Peleg O., Block C. & Arad I. (2001) Enterobacter sakazakii infection in the newborn. Acta-Paediatrica 90, 356–358. [PubMed] [Google Scholar]
- Block C., Peleg O., Minster N., Bar‐Oz B., Simhon A., Arad I. et al. (2002) Cluster of neonatal infectious in Jerusalem due to unusual biochemical variant of Enterobacter sakazakii . European Journal of Clinical Microbiology and Infectious Diseases 21, 613–616. [DOI] [PubMed] [Google Scholar]
- Codex Alimentarius Commission (CAC) (1979) Recommended International Code of Hygienic Practice for Foods for Infants and Children. CAC/RCP‐21. Alinorm 79/38, Rome.
- Caubilla‐Barron J., Iversen C. & Forsythe S.J. (2004) The Desiccation Survival of Enterobacter sakazakii and Related Enterobacteriaceae. 104th ASM General Meeting, New Orleans.
- Chan K.L., Saing H., Yung R.W., Yeung Y.P. & Tsoi N.S. (1994) A study of preantibiotic bacteriology in 125 patients with necrotizing enterocolitis. Acta Paediatrica Supplement 396, 45–48. [DOI] [PubMed] [Google Scholar]
- Clark N.C., Hill B.C., O'Hara C.M., Steingrimsson O. & Cooksey R.C. (1990) Epidemiologic typing of Enterobacter sakazakii in two neonatal nosocomial outbreaks. Diagnostic Microbiology and Infectious Disease 13, 467–472. [DOI] [PubMed] [Google Scholar]
- Edelson‐Mammel S.G. & Buchanan R.L. (2004) Thermal inactivation of Enterobacter sakazakii in rehydrated infant formula. Journal of Food Protection 67, 60–63. [DOI] [PubMed] [Google Scholar]
- FAO‐WHO (2004) Joint FAO‐WHO workshop of Enterobacter sakazakii and other microorganisms in powdered infant formula, Geneva, 2–5 February 2004. Online report: http://www.who.int/foodsafety/micro/meetings/feb2004/en/[accessed 25 July 2004].
- Farmer J.J., Asbury M.A., Hickman F.W., Brenner D.J. & Enterobacteriaceae Study Group (USA ) (1980) Enterobacter sakazakii: new species of Enterobacteriaceae isolated from clinical specimens. International Journal of Systematic Bacteriology 30, 569–584. [Google Scholar]
- Health Canada Food Program (2002) Health Professional Advisory: Enterobacter sakazakii infection and powdered infant formulas. Available at: http://www.hc-sc.gc.ca/food-aliment/mh-dm/mhe-dme/e_enterobacter_sak.html[accessed 25 July 2004].
- International Commission on Microbiological Specification for Foods (2002) Selection of cases and attribute plans In: Micro‐Organisms in Foods Vol. 7 Microbiological Testing in Food Safety Management. Chapter 8. Kluwer Academic/Plenum Publishers: New York. [Google Scholar]
- Iversen C., Druggan P. & Forsythe S.J. (2004a) A selective differential medium for Enterobacter sakazakii . International Journal of Food Microbiology 96, 133–139. [DOI] [PubMed] [Google Scholar]
- Iversen C. & Forsythe S.J. (2003) Risk profile of Enterobacter sakazakii, an emergent pathogen associated with infant milk formula. Trends in Food Science and Technology 14, 443–454. [Google Scholar]
- Iversen C. & Forsythe S.J. (2004) Isolation of Enterobacter sakazakii and other Enterobacteriaceae from powdered infant formula milk and related products. Food Microbiology 21, 771–776. [Google Scholar]
- Iversen C., Lane M. & Forsythe S.J. (2004b) The growth profile, thermotolerance and biofilm formation of Enterobacter sakazakii grown in infant formula milk. Letters in Applied Microbiology 38, 378–382. [DOI] [PubMed] [Google Scholar]
- Kandhai M.C., Reij M.W., Gorris L.G.M., Guillaume‐Gentil O. & Van Schothorst M. (2004) Occurrence of Enterobacter sakazakii in food production environments and households. Lancet 363, 39–40. [DOI] [PubMed] [Google Scholar]
- Kleiman M.B., Allen S.D., Neal P. & Reynolds J. (1981) Meningoencephalitis and compartmentalization of the cerebral ventricles caused by Enterobacter sakazakii . Journal of Clinical Microbiology 14, 352–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas A. & Cole T.J. (1990) Breast milk and neonatal necrotizing enterocolitis. Lancet 336, 1519–1523. [DOI] [PubMed] [Google Scholar]
- Mackie R.I., Sghir A. & Gaskins H.R. (1999) Developmental microbial ecology of the neonatal gastrointestinal tract. American Journal of Clinical Nutrition 69, 1035S–1045S. [DOI] [PubMed] [Google Scholar]
- Muytjens H.L. & Kollée L.A. (1990) Enterobacter sakazakii meningitis in neonates: causative role of formula? Pediatric Infectious Disease Journal 9, 372–373. [DOI] [PubMed] [Google Scholar]
- Muytjens H.L., Roelofs W.H. & Jaspar G.H.J. (1988) Quality of powdered substitutes for breast milk with regard to members of the family Enterobacteriaceae . Journal of Clinical Microbiology 26, 743–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muytjens H.L., Zanen H.C., Sonderkamp H.J., Kollée L.A., Wachsmuth I.K. & Farmer J.J. (1983) Analysis of eight cases of neonatal meningitis and sepsis due to Enterobacter sakazakii . Journal of Clinical Microbiology 18, 115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazarowec‐White M. & Farber J.M. (1997a) Incidence, survival, and growth of Enterobacter sakazakii in infant formula. Journal of Food Protection 60, 226–230. [DOI] [PubMed] [Google Scholar]
- Nazarowec‐White M. & Farber J.M. (1997b) Thermal resistance of Enterobacter sakazakii in reconstituted dried‐infant formula. Letters in Applied Microbiology 24, 9–13. [DOI] [PubMed] [Google Scholar]
- Nazarowec‐White M. & Farber J.M. (1999) Phenotypic and genotypic typing of food and clinical isolates of Enterobacter sakazakii . Journal of Medical Microbiology 48, 559–567. [DOI] [PubMed] [Google Scholar]
- Neelam M., Nawaz Z. & Riazuddin S. (1987) Hydrocarbon biodegradation biochemical characterization of bacteria isolated from local soils. Pakistan Journal of Scientific and Industrial Research 30, 382–385. [Google Scholar]
- Noriega F.R., Kotloff K.L., Martin M.A. & Schwalbe R.S. (1990) Nosocomial bacteremia caused by Enterobacter sakazakii and Leuconostoc mesenteroides resulting from extrinsic contamination of infant formula. Pediatric Infectious Disease Journal 9, 447–449. [PubMed] [Google Scholar]
- Simmons B.P., Gelfand M.S., Haas M., Metts L. & Ferguson J. (1989) Enterobacter sakazakii infections in neonates associated with intrinsic contamination of a powdered infant formula. Infection Contrological and Hospital Epidemiology 10, 398–401. [DOI] [PubMed] [Google Scholar]
- Skladal P., Mascini M., Salvadori C. & Zannoni G. (1993) Detection of bacterial contamination in sterile UHT milk using an L‐lactate biosensor. Enzyme and Microbial Technology 15, 508–512. [Google Scholar]
- Smeets L.C., Voss A., Muytjens H.L., Meis J.F.G.M. & Melchers W.J.G. (1998) Genetische karakterisatie van Enterobacter sakazakii‐isolaten van Nederlandse patiënten met neonatale meningitis. Nederlands Tijdschrift voor Medische Microbiologie 6, 113–115. [Google Scholar]
- Urmenyi A.M.C. & Franklin A.W. (1961) Neonatal death from pigmented coliform infection. Lancet 11, 313–315. [DOI] [PubMed] [Google Scholar]
- Van Acker J., De Smet F., Muyldermans G., Bougatef A., Naessens A. & Lauwers S. (2001) Outbreak of necrotizing enterocolitis associated with Enterobacter sakazakii in powdered milk formula. Journal of Clinical Microbiology 39, 293–297. [DOI] [PMC free article] [PubMed] [Google Scholar]


