Abstract
Since 2009, the New York City Department of Health and Mental Hygiene (DOHMH) has received FoodCORE funding to hire graduate students to conduct in-depth food exposure interviews of salmonellosis case patients. In 2011, an increase in the number of Salmonella Heidelberg infections with pulsed-field gel electrophoresis XbaI pattern JF6X01.0022 among observant Jewish communities in New York and New Jersey was investigated. As this pattern is common nationwide, some cases identified were not associated with the outbreak. To reduce the number of background cases, DOHMH focused on the community initially identified in the outbreak and defined a case as a person infected with the outbreak strain of Salmonella Heidelberg with illness onset from 1 April to 17 November 2011 and who consumed a kosher diet, spoke Yiddish, or self-identified as Jewish. Nationally, 190 individuals were infected with the outbreak strain of Salmonella Heidelberg; 63 New York City residents met the DOHMH case definition. In October 2011, the graduate students (Team Salmonella) interviewed three case patients who reported eating broiled chicken livers. Laboratory testing of chicken liver samples revealed the outbreak strain of Salmonella Heidelberg. Although they were only partially cooked, the livers appeared fully cooked, and consumers and retail establishment food handlers did not cook them thoroughly before eating or using them in a ready-to-eat spread. This investigation highlighted the need to prevent further illnesses from partially cooked chicken products. Removing background cases helped to focus the investigation. Training graduate students to collect exposure information can be a highly effective model for conducting foodborne disease surveillance and outbreak investigations for local and state departments of public health.
Foodborne diseases have been thrust into the national spotlight as a result of high-profile outbreaks caused by food items such as spinach and peanut butter (1,2). Concern about the burden of foodborne disease and increased public awareness has led public health agencies to enhance efforts to detect more outbreaks and solve them faster. Adequate laboratory and epidemiology resources can increase the timeliness and accuracy of foodborne disease surveillance and investigations (9, 16, 20). One major component of this capacity is having epidemiologists trained to obtain extensive food histories from case patients (10). The signing of the Food Safety Modernization Act, in which reduction of adverse health consequences of foodborne diseases was identified as a key goal by the Centers for Disease Control and Prevention (CDC), has increased recognition of the urgent need for additional resources to improve foodborne disease investigations (4).
In 2009, the New York City Department of Health and Mental Hygiene (DOHMH) was chosen as one of three pilot sites for the OutbreakNet Sentinel Site program. This program expanded to seven centers in 2010 and was renamed the Foodborne Diseases Centers for Outbreak Response Enhancement (FoodCORE). FoodCORE is funded by CDC with support from the U.S. Department of Agriculture Food Safety and Inspection Service (FSIS) and the Association of Public Health Laboratories (APHL). The goal of FoodCORE is to enhance the epidemiology and laboratory capacity of local and state health departments so responses to foodborne disease investigations are quicker and more comprehensive (5). Through FoodCORE, a team of public health graduate students, known as Team Salmonella, was hired by DOHMH to conduct food exposure interviews of all individuals reported with salmonellosis. Student-based surveillance and interview teams have been used to improve the quality and outcome of public health investigations (8, 12), most notably at the Minnesota Department of Health (19).
In 2011, an investigation of cases of Salmonella Heidelberg infection caused by a strain with pulsed-field gel electrophoresis (PFGE) XbaI pattern JF6X01.0022 was initiated among observant or ultraorthodox Jewish populations primarily residing in New York and New Jersey (3). This Salmonella Heidelberg PFGE pattern is common in the United States. According to PulseNet, the CDC subtyping network for foodborne illness, approximately 30 to 40 infections of Salmonella Heidelberg with the same PFGE pattern would be expected in the United States each year (17). The present article documents how efforts were focused to avoid including background cases unrelated to the outbreak and how Team Salmonella was integral to the investigation, quickly interviewing case patients and ultimately determining the source of the infections.
MATERIALS AND METHODS
Salmonella surveillance: epidemiology.
All culture-confirmed cases of salmonellosis in New York City are reportable to DOHMH by law. Before FoodCORE funding began in 2009, DOHMH was able to interview only those salmonellosis case patients who were daycare workers or attendees, food handlers, health care workers, or part of a cluster identified by a neighboring jurisdiction or CDC. Therefore, before 2009 only 7% of the 1,200 salmonellosis case patients reported in New York City each year were interviewed. Since 2009, the DOHMH has annually hired and trained a team of six public health graduate students, based on a model of student interviewers developed by the Minnesota Department of Health (15). The students are trained in foodborne disease epidemiology and patient interview techniques, advised about patient confidentiality issues, and instructed on the management and analysis of large data sets.
Salmonella surveillance: laboratory.
All Salmonella isolates confirmed by clinical laboratories in New York City must be forwarded to the DOHMH Public Health Laboratory for confirmation, serotyping, and subtyping by PFGE. The PFGE results are uploaded to PulseNet for comparison with national data (17).
Salmonella Heidelberg investigation.
On 6 July 2011, a foodborne disease epidemiologist from the New Jersey Department of Health (NJDOH) contacted the New York State Department of Health (NYSDOH) and DOHMH regarding an increase in Salmonella Heidelberg infections among the observant Jewish population in New Jersey. Before laboratory confirmation that the cases were indistinguishable by PFGE, NJDOH, NYSDOH, and DOHMH immediately responded by assessing food histories of case patients with Salmonella Heidelberg infections for possible commonalities. Subsequent laboratory findings confirmed the presence of an outbreak; the Salmonella Heidelberg isolates from the observant Jewish communities all shared an indistinguishable PFGE pattern.
For this investigation, all Salmonella Heidelberg case patients were interviewed first using DOHMH’s standard food exposure questionnaire, which consists of questions about more than 200 food items and potential exposures. As the investigation progressed, a supplemental questionnaire developed by CDC and state and local health departments was used to inquire about additional food items commonly consumed by the observant Jewish community.
Nationally, a case was defined as a person with a culture-confirmed Salmonella Heidelberg infection with PFGE XbaI pattern JF6X01.0022 that was diagnosed from 1 April to 17 November 2011 and reported to PulseNet. In New York City, the case definition also included only people who reported consuming a kosher diet or speaking Yiddish in their home or who self-identified as Jewish. Since JF6X01.0022 was the most common PFGE pattern of Salmonella Heidelberg in the PulseNet database, refining the case definition helped remove unrelated (background) case patients. A contingency table was used to assess the ability of the DOHMH case definition to remove background cases. Differences in food exposures were compared between ill persons who reported a kosher diet or speaking Yiddish or who self-identified as Jewish and those who did not report any of these three criteria. Food exposure questionnaires were administered to all persons diagnosed with Salmonella Heidelberg infection, but DOHMH focused on the food exposures for those who fit the refined case definition.
Students and staff visited grocery stores to assess food items sold at specialty markets identified by case patients. Food samples collected during inspections from implicated food establishments were cultured. Any Salmonella isolates recovered were then subtyped by the New York State Department of Agriculture and Markets (NYSAM).
RESULTS
Seventy-three cases of Salmonella Heidelberg with indistinguishable PFGE patterns obtained with the restriction enzyme XbaI were identified in New York City, with isolation dates of 1 April to 17 November 2011; 63 of those cases met the DOHMH case definition. The majority of case patients resided in one borough or county of New York City; however, in October 2011, a subcluster of seven cases was identified in another borough. During the food exposure interviews, Team Salmonella students noted that three case patients from this subcluster reported eating a kosher broiled chicken liver product before illness onset. Whole chicken livers and chicken liver spreads were not specifically asked about on the standard or supplemental questionnaire; however, one question concerned consuming whole chicken or chicken parts. Three locations of two local chain grocery stores were noted as places where case patients had purchased the whole broiled chicken livers or chicken liver spreads. Two of the case patients reported that they did not heat the chicken livers thoroughly before eating them. Team Salmonella recognized this as an important finding and immediately reported the common chicken liver exposure to a DOHMH foodborne disease epidemiologist.
On 24 October 2011, DOHMH contacted NYSAM regarding kosher broiled chicken liver products at the two specific grocery chains and the possible link to the ongoing outbreak of Salmonella Heidelberg infections. During a site visit, NYSAM collected samples of broiled chicken livers and spreads and initiated a traceback of the products. Laboratory testing conducted by the NYSAM Laboratory Division identified the outbreak strain of Salmonella Heidelberg in samples of kosher broiled chicken livers and chopped liver products obtained from the retail establishments. All the liver products were made by a single producer, Corporation A. The investigation conducted by FSIS determined that Corporation A kosher broiled chicken livers were distributed to New York, New Jersey, Pennsylvania, Maryland, Minnesota, Ohio, Rhode Island, and Florida.
Nationally, 190 cases of infection with the Salmonella Heidelberg outbreak strain were confirmed 1 April to 17 November 2011 in states where these kosher broiled chicken livers were distributed. The majority of case patients were residents of New York City (73), New Jersey (62), and New York State outside of New York City (36); cases also were reported in Pennsylvania (10), Maryland (6), Ohio (2), and Minnesota (1). The median age of the case patients was 14 years (range, <1 to 97 years), and 49% were female. Among the 154 case patients with available information, 30 (19%) were hospitalized. No deaths were reported. Sixty-three case patients met the DOHMH case definition, with a median age of 17 (range, <1 to 90 years), and 49% were female. Among 39 ill persons who were asked about chicken livers, 28 (72%) reported consuming kosher chicken liver products in the week before onset of symptoms.
When comparing food exposures to assess the DOHMH case definition, 10 (59%) of 17 case patients who followed nonkosher diets reported consuming chicken before illness onset compared with 24 (92%) of 26 case patients who followed kosher diets (P = 0.006). Of the 27 case patients who reported eating chicken liver and responded to the dietary restriction question, 100% reported eating a kosher diet.
Traceback of the kosher broiled chicken livers led investigators to Corporation A, which prepared and distributed the product. The chicken livers were shipped in bulk to retail stores, repackaged, and sold in smaller quantities. Grocery stores also used this product to make ready-to-eat chicken liver spreads, which were sold to consumers. The label on the whole chicken livers indicated that the product required “further thermal processing” and recommended cooking to 160°F (71 °C) (Fig. 1). As these products appeared to be fully cooked, consumers and retail establishment food handlers did not recognize the need to cook the product thoroughly before eating or before using in a ready-to-eat product. On 8 November 2011, Corporation A announced a recall of all of their kosher broiled chicken liver products and discontinued production of the partially broiled chicken liver product.
FIGURE 1.
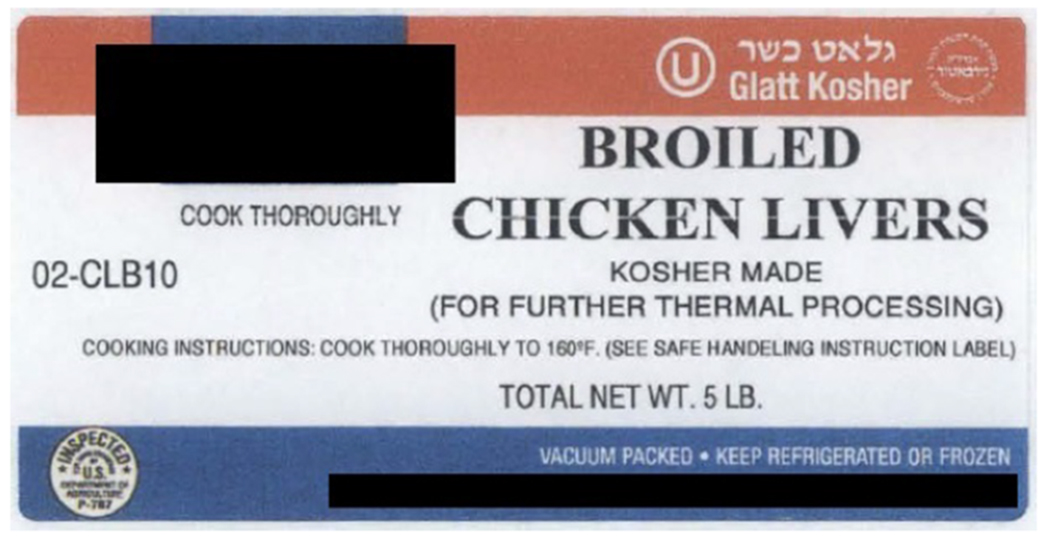
Kosher broiled chicken liver label.
DISCUSSION
Broiled chicken livers that appeared to be ready-to-eat but were not fully cooked were the vehicle in this Salmonella Heidelberg outbreak. Although chicken is a well-documented source of Salmonella (14), in the past decade notable outbreaks of salmonellosis have been associated with partially cooked chicken products, such as frozen strips, nuggets, or stuffed pieces (7, 18). The breading or browned appearance of these products and inadequate labeling mislead consumers into thinking these products are fully cooked and require only reheating (11, 13). In this Salmonella Heidelberg outbreak investigation, the chicken product was sold partially broiled, remaining raw inside. As the chicken livers had a browned appearance and were labeled “broiled,” many consumers and food handlers assumed the product was fully cooked. The label indicated that the product required “further thermal processing,” but this instruction may not have been clearly understood by some consumers and food handlers. The recommended cooking temperature of 160°F on the bulk container labels also is below the required 165°F (74°C) for poultry products in New York State. Improved labeling and consumer education is needed to prevent further illnesses from partially cooked chicken products.
Since the PFGE pattern of the outbreak strain was the most common pattern among the Salmonella Heidelberg isolates uploaded to PulseNet, DOHMH epidemiologists found that refining the case definition to include only those individuals who ate kosher diets, spoke Yiddish at home, or identified as Jewish helped to remove unrelated background cases. Sometimes outliers can shed light on an investigation. However, this outbreak clearly affected a specific religious community, primarily in New York and New Jersey, with specific eating practices. Patients whose infection matched the outbreak strain but who were not part of this community likely did not consume the item of concern; thus, inclusion of their food exposure histories would have diluted the findings. The national guidelines for conducting foodborne disease outbreak investigations established by the Council to Improve Foodborne Outbreak Response (CIFOR) recommends inclusion of more specific classifications or characteristics to help distinguish outbreak cases from background cases (6). When outbreaks occur within distinct populations, utilizing demographic or food preference information can help focus the investigation and facilitate identification of the exposure that caused illness.
This multistate investigation was particularly noteworthy because of DOHMH’s ability to rapidly respond and thus solve this outbreak through the work of the Team Salmonella students. Before FoodCORE funding, DOHMH lacked adequate staffing to interview the 1,200 salmonellosis cases reported each year. Therefore, salmonellosis interviews were conducted only when an outbreak was confirmed by laboratory analysis, which was usually weeks or months after the case patient’s diagnosis. Often by that time, patients were not able to recall their entire food history, reducing the utility of the data for the investigation. Collecting complete and timely exposure information from a case patient is vital to a successful epidemiologic investigation.
Questions about the food item that was the ultimate source of the outbreak were not explicitly included in either the initial or supplemental questionnaire, which highlights the value of well-trained interviewers. The primary task of a Team Salmonella student is to conduct a 21-page interview with all salmonellosis case patients; this interview covers more than 200 food items and potential exposures. Using a standardized questionnaire is a model practice highlighted by CIFOR for conducting foodborne disease outbreak investigations (6). The DOHMH Team Salmonella is taught to probe case patients to identify other foods eaten but not directly asked on the questionnaire and to collect additional information about food preparation when applicable. The graduate students sit close together in the office, which fosters communication and discussion of unusual cases. Hiring students can be cost-effective because they receive a modest hourly wage, work part time, and do not receive benefits. However, students graduate and leave their positions as interns at the health department, necessitating yearly rounds of recruiting, interviewing, hiring, and training that would not occur as often with full-time staff. Despite the limitations, hiring public health graduate students to conduct in-depth food exposure interviews can be a highly effective and efficient model for local and state departments of public health conducting foodborne disease surveillance and outbreak investigations.
ACKNOWLEDGMENTS
This work was supported by funding through the FoodCORE Program. We thank FoodCORE, APHL, and FSIS for their continued support. We also acknowledge all of the Team Salmonella graduate students who have worked since 2009 performing enhanced Salmonella surveillance.
REFERENCES
- 1.Cavallaro E, Date K, Medus C, Meyer S, Miller B, Kim C, Nowicki S, Cosgrove S, Sweat D, Phan Q, Flint J, Daly ER, Adams J, Hyytia-Trees E, Gerner-Smidt P, Hoekstra RM, Schwensohn C, Langer A, Sodha SV, Rogers MC, Angulo FJ, Tauxe RV, Williams IT, and Behravesh CB, for the Salmonella Typhimurium Outbreak Investigation Team. 2011. Salmonella Typhimurium infections associated with peanut products. N. Engl. J. Med 365:601–610. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2006. Ongoing multistate outbreak of Escherichia coli serotype O157:H7 infections associated with consumption of fresh spinach—United States, September 2006. Morb. Mortal. Wkly. Rep 55:1045–1046. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2012. Salmonella Heidelberg—chicken livers. Available at: http://www.cdc.gov/salmonella/heidelberg-chickenlivers/index.html Accessed 5 December 2013.
- 4.Centers for Disease Control and Prevention. 2013. Winnable battles. Available at: http://www.cdc.gov/WinnableBattles/FoodSafety/ Accessed 5 December 2013.
- 5.Centers for Disease Control and Prevention. 2013. FoodCORE. Available at: http://www.cdc.gov/foodcore/ Accessed 5 December 2013.
- 6.Council to Improve Foodborne Disease Outbreak Response. 2009. Guidelines for foodborne disease outbreak response. Available at: http://www.cifor.us/CIFORGuidelinesProjectMore.cfm Accessed 3 March 2014.
- 7.Currie A, MacDougall L, Aramini J, Gaullin C, Ahmed R, and Isaacs S. 2005. Frozen chicken nuggets and strips and eggs are leading risk factors for Salmonella Heidelberg infections in Canada. Epidemiol. Infect 133:809–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gebbie E, Morse S, Hanson H, McCollum M, Reddy V, Gebbie K, Smailes E, and Balter S. 2007. Training for and maintaining public health surge capacity: a program for disease outbreak investigation by student volunteers. Public Health Rep. 122:127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedberg CW, Greenblatt JF, Matyas BT, Lemmings J, Sharp DJ, Skibicki RT, and Liang AP, for the Enteric Disease Investigation Timeline Study Work Group. 2008. Timeliness of enteric disease surveillance in 6 US states. Emerg. Infect. Dis 14: 311–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones T, Imhoff B, Samuel M, Mshar P, McCombs KG, Hawkins M, Deneen V, Cambridge M, and Olsen SJ, for the Emerging Infections Program FoodNet Working Group. 2004. Limitations to successful investigation and reporting of foodborne outbreaks. Clin. Infect. Dis 38(Suppl. 3):S297–S302. [DOI] [PubMed] [Google Scholar]
- 11.Kenny B, Hall R, and Cameron S. 1999. Consumer attitudes and behaviours—key risk factors in an outbreak of Salmonella Typhimurium phage type 12 infection sourced to chicken nuggets. Aust. N. Z. J. Public Health 23:164–167. [DOI] [PubMed] [Google Scholar]
- 12.MacDonald P, Davis M, and Horney J. 2010. Review of the UNC Team Epi-Aid graduate student epidemiology response program six years after implementation. Public Health Rep. 125:70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacDougall L, Fyfe M, McIntyre L, Paccagnella A, Cordner K, Kerr A, and Aramini J. 2004. Frozen chicken nuggets and strips—newly identified risk factor for Salmonella Heidelberg infection in British Columbia, Canada. J. Food Prot 67:1111–1115. [DOI] [PubMed] [Google Scholar]
- 14.Marcus R, Varma J, Medus C, Boothe E, Anderson B, Crume T, Fullerton K, Moore M, White P, Lyszkowicz E, Voetsch A, and Angulo FJ, for the Emerging Infections Program FoodNet Working Group. 2007. Re-assessment of risk factors for sporadic Salmonella serotype Enteritidis infections: a case-control study in five FoodNet sites, 2002–2003. Epidemiol. Infect 135:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minnesota Department of Health. 2009. Foodborne outbreak protocol: procedures for responding to foodborne disease outbreaks in food service establishments in Minnesota. Available at: http://www.health.state.mn.us/divs/eh/food/pwdu Accessed 5 December 2013.
- 16.Murphree R, Garman K, Phan Q, Everstine K, Gould LH, and Jones T. 2012. Characteristics of foodborne disease outbreak investigations conducted by Foodborne Diseases Active Surveillance Network (FoodNet) sites, 2003–2008. Clin. Infect. Dis 54(Suppl. 5):S498–S503. [DOI] [PubMed] [Google Scholar]
- 17.Ribot E, Fair M, Gautom R, Cameron D, Hunter S, Swaminathan B, and Barrett T. 2006. Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathog. Dis 3:59–67. [DOI] [PubMed] [Google Scholar]
- 18.Smith K, Medus C, Meyer S, Boxrud D, Leano F, Hedberg C, Elfering K, Braymen C, Bender J, and Danila R. 2008. Outbreaks of salmonellosis in Minnesota (1998 through 2006) associated with frozen, microwaveable, breaded, stuffed chicken products. J. Food Prot 71:2153–2160. [DOI] [PubMed] [Google Scholar]
- 19.Smith T 2009. “Team Diarrhea” follows a trail of sickness caused by tainted food. Scientific American; Available at: http://www.scientificamerican.com/article/team-diarrhea/ Accessed 19 February 2014. [Google Scholar]
- 20.Waechter H, Reddy V, Hanson H, and Balter S. 2013. Evaluation of enhanced Salmonella surveillance in New York City: the effectiveness of a student-based interview model. J. Food Prot. Trends 33:300–306. [Google Scholar]


