Abstract
Hip fractures are a common cause of acute pain in elderly patients. However, pain may be undertreated due medical comorbidities. Strong evidence supports the use of regional nerve blocks to reduce preoperative pain after hip fracture. Despite recommendations for their use, regional nerve blocks may not be in widespread practice in the United States. To help promote the addition of regional nerve blocks into hip fracture protocols, this paper will provide an overview of two commonly used regional nerve blocks for hip fracture (fascia iliaca compartment block and femoral nerve block), review the regional nerve block protocols presented in 12 studies, and present the detailed protocol currently in use at The Queen's Medical Center in Honolulu, HI.
Keywords: Hip fracture, Femoral Nerve Block, Fascia Iliaca Compartment Block, Regional Anesthesia, Continuous Block, Opioid Sparing
Introduction
Each year over 300,000 people aged 65 and older are hospitalized for hip fractures in the United States.1 Providing effective analgesia for these patients is complicated by advanced age and concomitant comorbidities. Inadequately treated pain has several repercussions for geriatric patients with hip fractures. Delirium is a common complication of hip fractures, affecting approximately 13%–61% of patients, and undertreated pain significantly increases the risk of perioperative delirium in cognitively intact patients.2 Increased post-operative pain is also associated with significantly longer lengths of stay, delayed ambulation, missed or shortened physical therapy sessions, and impaired locomotion at 6 months following injury.3 According to a national database in 2014, the average length of stay for a femoral neck fracture in Hawai‘i was 7.1 days costing an average of $48,911.1 In this current climate of increasing health care costs, improving perioperative pain control could be an important step toward reducing these numbers.
The American Academy of Orthopaedic Surgeons (AAOS) clinical practice guidelines on management of hip fractures in the elderly provide a strong recommendation for regional analgesia to improve preoperative pain control.4 A Cochrane review demonstrated high-quality evidence that regional blockade reduces pain on movement within 30 minutes of block placement and moderate- quality evidence for decreased time to first mobilization after surgery.5 Despite the potential benefits of these procedures and national guidelines recommending their use, studies in the United Kingdom and Australia have demonstrated regional nerve blocks are not being used on a regular basis.6,7 To help promote implementation of regional nerve blocks for proximal femur fractures, this paper will give an overview of common regional nerve blocks for hip fractures, protocols presented in the literature, as well as present the protocol currently used at The Queen's Medical Center (QMC) in Honolulu, HI.
Type of Block
The primary regional nerve blocks presented in the literature for proximal femur fractures include femoral nerve blocks (FNB) and fascia iliaca compartment blocks (FICB). The main nerves innervating the hip joint are the femoral, obturator, superior gluteal, and nerve to quadratus femoris and inferior gemellus.8 Of note, these described blocks do not anesthetize the posterior hip joint.
Femoral Nerve Block
Key landmarks for the femoral nerve block include the inguinal ligament, inguinal crease, and femoral artery. The needle is inserted at the femoral crease both below the inguinal crease and 1-2 cm lateral to the pulse of the femoral artery (Figure 1). The needle tip must be positioned below the fascia iliaca to obtain a complete femoral nerve block.9,10 In the “3-in-1” technique described by Winnie, et al,9 digital pressure can be applied distal to the injection site to promote spread of the anesthetic cranially and laterally to block the femoral, obturator, and lateral femoral cutaneous nerves. Placement of the femoral nerve block can be assisted by ultrasound, nerve stimulation, or elicited paresthesias, per the proceduralist‘s choice.
Figure 1.

Anatomic landmarks for femoral nerve block. (Source: NYSORA.COM)
Fascia Iliaca Compartment Block
The fascia iliaca compartment is a potential space delineated by the fascia iliaca anteriorly (Figure 2), the outer aspect of the iliacus muscle posteriorly, the vertebral column and upper part of sacrum medially, and the inner lip of the iliac crest laterally and rostrally. This compartment contains the lateral femoral cutaneous nerve, femoral nerve, and obturator nerve.11 The goal insertion point is 1cm caudal to the point dividing the lateral third and middle third of the line connecting the anterior superior iliac spine to the pubic tubercle. The injection site is several centimeters lateral to the femoral artery.12 Proceduralist may use either ultrasound guidance or the loss of resistance technique, where two “pops” are felt as the needle passes through the fascia lata then fascia iliaca.11 One study13 demonstrated increased efficacy of sensory blockade with ultrasound guidance compared to the loss of resistance technique.
Figure 2.
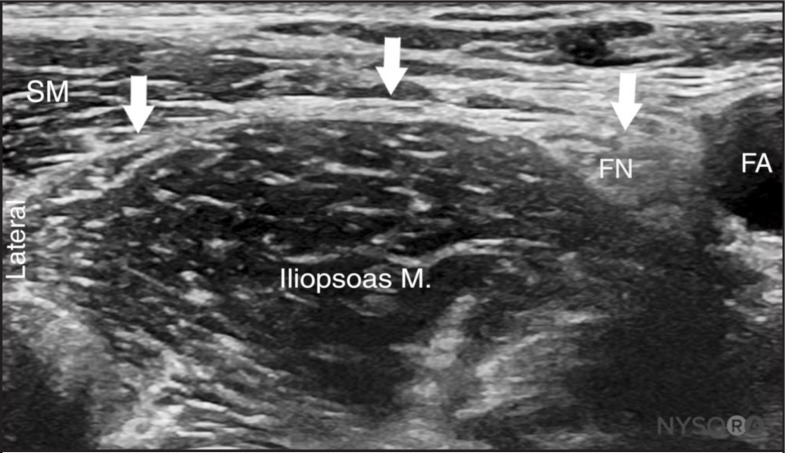
Ultrasound image of the fascia iliaca (white line and arrows) at the level of the inguinal ligament. FN = femoral nerve. FA = femoral artery. SM = sartorious muscle. (Source: NYSORA.COM)
Method of Delivery
These blocks can be delivered as either a single shot or a continuous infusion catheter. The anatomic technique for continuous infusion catheter is like that for a single shot. Once the needle is in the correct position for either block, a catheter can be inserted 2–4 cm beyond the tip of the needle. After a negative aspiration test, a bolus dose of local anesthetic is injected followed by either a continuous infusion and/or intermittent boluses of local anesthetic via an infusion pump. Infusion pumps can either be electronic or nonelectronic. Of nonelectronic mechanisms, only elastomeric pumps have been studied in depth for continuous regional anesthesia.14
Protocols
Several protocols for regional nerve blocks for hip fractures have been presented in the literature. Table 1 summarizes important logistic variables for regional block protocols including the type and duration of block, anesthetic utilized (and pump if applicable for continuous blocks), proceduralist, and location of where block was placed. These protocols highlight how different specialties and different levels of medical experience have all been utilized to perform regional nerve blocks.
Table 1.
Summary of Regional Nerve Block Protocols for Hip Fracture Presented in the Literature
| Study | Country | Type of Block | Duration | Technique | Proceduralist | Anesthetic Pump (if applicable) | Location |
|---|---|---|---|---|---|---|---|
| Foss, et al,12 | Denmark | FICB | Single | Loss of resistance | Junior anesthesiologists with less than two years of training | 1% mepivacaine with 1:200,000 epinephrine 40 mL | Emergency department (ED) |
| Li, et al,15 | US | FNB | Single | Ultrasound guidance | Anesthesiologist | 0.5% ropivacaine 30 mL | Not specified |
| Fletcher, at al,16 | UK | FNB | Single | Elicited paresthesias | ED staff - two consultants, four middle-grade physicians, seven senior house officers | 0.5% bupivacaine 20 mL | ED |
| Monzon, et al,17 | Argentina | FICB | Single Loss of resistance | Four ED attending physicians | Monzon, et al,17 Argentina FICB Single Loss of resistance Four ED attending physicians | 0.25% bupivacaine at 0.3 mL/kg | ED |
| Haddad, et al,18 | UK | FNB | Single | Elicited paresthesias | Senior author–orthopedic surgeon | 0.25% bupivacaine at 0.3 mL/kg | Not specified |
| Mouzopoulos, et al,19 | Greece | FICB | Multiple single – administered preop and daily every 24h until delirium occurrence or discharge | Loss of resistance | Orthopaedic surgeons | 0.25 mg dose of 0.3 mL/kg bupivacaine | Not specified |
| Yun, et al,20 | Korea | FICB | Single | Loss of resistance | Senior author – experienced anesthesiologist | 3.75 mg/mL ropivacaine 30 mL | Anesthesia induction room |
| Høgh, et al,21 | Denmark | FICB | Single | Loss of resistance | Junior registrars | 2.5 mg/mL bupivacaine 30 mL and 2% lidocaine 10 mL (quantity halved if patient weighed >50 kg) | ED |
| Haines, et al,22 | US | FICB | Single | Ultrasound | ED physicians | 0.25% bupivacaine 30mL | ED |
| Nie, et al,23 | China | FICB | Continuous | Loss of resistance | Anesthesiologist | Initial weight-based bolus of 0.5% ropivacaine (20 mL for >50 kg, 25 mL for 50 kg to 70 kg, 30 mL for <70 kg), followed by 0.25% ropivacaine infused at 0.1 mL/kg/h for 48 hours Electronic pump (Apon, Apon Ltd, China) |
Intraop |
| Szucs, et al,24 | Ireland | FNB | Continuous | Nerve stimulation | Senior author – experienced anesthesiologist | Initial bolus of 10 mL of 2% lidocaine and 10 mL of 0.5% bupivacaine over 2–3 minutes followed by 0.25% bupivacaine infused at 4 mL per hour for 72 hours Elastomeric pump (Acemedical, AutoFUser, Seoul, South Korea) | ED |
| Luger, et al,25 | Austria | FNB | Continuous | Ultrasound | Attending anesthesiologists | Initial bolus of 30 mL 0.25% bupivacaine followed by 0.125% bupivacaine infused at 6 mL/h; if sensory block was inadequate, an additional 10 mL bolus of 0.125% bupivacaine administered Pump not specified |
Not specified |
Practicality for goals of hip fracture protocols must be taken into consideration. For example, one study15 set time goals for eligible patients to receive a FNB that took working hours into account – either within 45 minutes of arrival at the hospital during work hours (7:00 – 19:00) or within 4 hours during off hours (19:00 – 7:00). All medically cleared patients then underwent surgery within 24 hours of arrival to the facility. Only one study2424 noted the duration of the block procedure, which was less than 15 minutes for insertion and securing the femoral nerve catheter for a continuous femoral nerve block performed by an attending anesthesiologist.
Two studies16,22 outlined a training program for performing their regional block of interest. Both protocols included a lecture session followed by supervised placement on a patient. Neither study commented on the number of supervised attempts required before competency was achieved. Although another study21 did not outline the training program for junior registrars learning to perform FICB, the authors noted that the learning curve was “relatively easy” as the efficacy of the block did not correlate to the number previously performed by the junior registrar. Two other studies17,18 noted that physicians in training could successfully perform their studied block with minimal instruction. However, resident physicians were not used as the proceduralists in these studies and the method of instruction was not elucidated.
The studies12,15–18,20–22 for single-shot nerve blocks all demonstrated efficacy as pre-operative analgesia for hip fractures. The duration of a single bolus of bupivacaine 0.5% 20 mL for FNB is only 22 hours (range 15–32),26 which limits its application for post-operative analgesia. Either repeated single injections19 or continuous block catheters provide the advantage of both pre- and post-operative analgesia.
QMC Protocol
Once the patient is determined by the orthopaedic consult to have an eligible hip fracture (acetabular fractures excluded), anesthesia is consulted for possible block placement. Both surgical and non-surgical patients are eligible. The goal is to have the patient evaluated and blocked by the anesthesiologist within two hours of consultation. CRNAs may relieve the MD during ongoing cases to facilitate block placement. Patients are deemed eligible for block placement by anesthesia if preoperative risk stratification is completed, conditions present on admission are documented, and if they pass the “4 Nos then Go”:
Does the patient have an active cardiac condition (evolving MI, decompensated CHF, etc.)?
Does the patient have a significant coagulopathy?
Does the patient have an active stroke?
Does the patient have a condition requiring ICU level of care (sepsis, severe metabolic derangement, respiratory failure)?
If the answer is “No” to all four questions, the patient is eligible for a block and optimized for fast track to the OR. The anesthesiologist books the block placement with the OR. The patient is admitted to the hospital by the appropriate service and then transferred to the pre-op area during normal business hours or the post-anesthesia care unit (PACU) after-hours for block placement. These areas were chosen for block placement as all applicable anesthesia equipment including ultrasound machines, infusion pumps, and medications are readily available, and staff have the appropriate training for procedural documentation and toxicity monitoring. Either pre-op nurses assist during normal business hours or operative nurses assist after-hours. For surgical patients, the block placement is covered under the standard surgical consent form at QMC and a separate written consent is not required.
The anesthesiologist confers with the orthopaedic surgeon to ensure any invasive procedure is in alignment with the surgical preparation and plan for the patient. All patients are provided with multimodal analgesia while limiting narcotics and avoiding sedatives when possible. The anesthesiologist may then decide to place a single shot nerve block of 20–30 mL 0.2% ropivacaine based on weight, place a continuous nerve block with local anesthetic delivered via ON-Q pain pump (Kimberly Clark, Roswell, GA), or decline block placement and use only multimodal analgesia. The type of nerve block used (FNB versus FICB) and method of placement is at the discretion of the anesthesiologist, however most place a FICB (either single shot or continuous infusion) under ultrasound guidance. If the catheter tip conflicts with the surgical incision site, a bolus may be given prior to catheter tip removal in the OR. A new catheter may be placed post-op if needed. Post-operatively, the anesthesiologist (or one of their partners) evaluates the patient within 12 hours postoperatively. The patient's first mobilization postop is with the physical therapist, who then provides feedback to the anesthesiologist regarding mobility. The infusion rate can be adjusted by the anesthesiologist if femoral weakness is an issue. If a catheter infusion is used, it is recommended to keep in place between 12–72 hours post placement. Appropriate DVT prophylaxis may be used postoperatively with catheter in place. The catheter is removed the day before discharge either by the anesthesiologist or RN.
Discussion
Further research into continuous regional nerve blocks is warranted. The influence of femoral weakness on postoperative mobility with continuous regional nerve blocks was not assessed in the cited studies.23–25 Furthermore, the risk of infection stemming from the in-dwelling catheter is not fully understood. One study27 FNB 48 hours after insertion and showed 57% had positive bacterial colonization, with Staphylococcus epidermidis as the most common organism. A different study,23 however, cultured all catheter tips from continuous FICB and no positive cultures nor signs of infection were observed. There was no long-term follow-up in either study to see if bacterial colonization of catheters correlated with development of surgical site infections. The economic impact of continuous nerve blocks also merits further evaluation.
Careful consideration of available resources, including available staff and equipment, can help lead to the successful addition of regional nerve blocks in hip fracture protocols. A regional nerve block program may not require investment in expensive equipment depending on the technique used. Two studies explicitly chose to not use peripheral nerve stimulators to confirm block placements as the equipment was expensive,17 we tested the efficacy of using fascia-iliaca blocks (FICB or frequently “misplaced” and “time-consuming to use.”16 Different specialties and levels of experience can be trained to successfully perform these procedures. Regional nerve blocks for hip fractures can be a quick and safe procedure to improve analgesia and patient satisfaction. Hopefully this overview of regional nerve block protocols in the literature and the detailed presentation of the protocol in use at QMC will help spearhead more widespread use of these valuable procedures.
Abbreviations
- FICB
fascia iliaca compartment block
- FNB
femoral nerve block
- QMC
The Queen's Medical Center, Honolulu, HI
Conflicts of Interest
None of the authors identify any conflicts of interest.
References
- 1.Agency for Healthcare Research and Quality; HCUPnet. Healthcare Cost and Utilization Project (HCUP) http://hcupnet.ahrq.gov. Published 2014. Accessed May 27, 2019. [PubMed] [Google Scholar]
- 2.Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58((1)):76–81. doi: 10.1093/gerona/58.1.m76. http://www.ncbi.nlm.nih.gov/pubmed/12560416. [DOI] [PubMed] [Google Scholar]
- 3.Morrison SR, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103((3)):303–311. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Orthopaedic Surgeons Board of Directors Strong evidence supports regional analgesia to improve preoperative pain control in patients with hip fracture. Management of Hip Fractures in the Elderly - Evidence-Based Clinical Practice Guideline. 2014. http://www.orthoguidelines.org/guideline-detail?id=1231.
- 5.Guay J, Mj P, Griffiths R, Kopp S. Peripheral nerve blocks for hip fractures ( Review ) SUMMARY OF FINDINGS FOR THE MAIN COMPARISON. 2017;((5)) doi: 10.1002/14651858.CD001159.pub2. www.cochranelibrary.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holdgate A, Shepherd SA, Huckson S. Patterns of analgesia for fractured neck of femur in Australian emergency departments: Original Research. EMA - Emerg Med Australas. 2010;22((1)):3–8. doi: 10.1111/j.1742-6723.2009.01246.x. [DOI] [PubMed] [Google Scholar]
- 7.Mittal R, Vermani E. Femoral nerve blocks in fractures of femur: Variation in the current UK practice and a review of the literature. Emerg Med J. 2014;31((2)):143–147. doi: 10.1136/emermed-2012-201546. [DOI] [PubMed] [Google Scholar]
- 8.Functional Regional Anesthesia Anatomy - NYSORA. https://www.nysora.com/foundationsof-regional-anesthesia/anatomy/functional-regional-anesthesia-anatomy/. Accessed July 29, 2019.
- 9.Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg. 1973;52((6)):989–996. http://www.ncbi.nlm.nih.gov/pubmed/4796576. [PubMed] [Google Scholar]
- 10.Femoral Nerve Block - Landmarks and Nerve Stimulator Technique - NYSORA. https://www.nysora.com/techniques/lower-extremity/femoral/femoral-nerve-block/. Accessed May 25, 2019.
- 11.Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69((6)):705–713. doi: 10.1213/00000539-199004000-00044. [DOI] [PubMed] [Google Scholar]
- 12.Foss NB, Kristensen BB, Bundgaard M, et al. Fascia Iliaca Compartment Blockade for Acute Pain Control in Hip Fracture Patients. Anesthesiology. 2007;106((4)):773–778. doi: 10.1097/01.anes.0000264764.56544.d2. [DOI] [PubMed] [Google Scholar]
- 13.Dolan J, Williams A, Murney E, Smith M, Kenny GNC. Ultrasound Guided Fascia Iliaca Block: A Comparison With the Loss of Resistance Technique. Reg Anesth Pain Med. 2008;33((6)):526–531. doi: 10.1016/j.rapm.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Continuous Peripheral Nerve Blocks: Local Anesthetic Solutions and Infusion Strategies - NYSORA. https://www.nysora.com/foundations-of-regional-anesthesia/pharmacology/continuous-peripheral-nerve-blocks-local-anesthetic-solutions-infusion-strategies/. Accessed July 11, 2019.
- 15.Li J, Dai F, Chang D, et al. A Practical Analgesia Approach to Fragility Hip Fracture: A Single-Center, Retrospective, Cohort Study on Femoral Nerve Block. J Orthop Trauma. 2019;33((4)):175–179. doi: 10.1097/BOT.0000000000001391. [DOI] [PubMed] [Google Scholar]
- 16.Fletcher AK, Rigby AS, Heyes FLP. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: A randomized, controlled trial. Ann Emerg Med. 2003;41((2)):227–233. doi: 10.1067/mem.2003.51. [DOI] [PubMed] [Google Scholar]
- 17.Monzon DG, Iserson KV, Vazquez JA. Single Fascia Iliaca Compartment Block for Post-Hip Fracture Pain Relief. J Emerg Med. 2007;32((3)):257–262. doi: 10.1016/j.jemermed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Haddad F, Williams R, Williams RL. Femoral nerve block in extracapsular femoral neck fractures. J Bone Joint Surg Br. 1995;77-B((6)):922–923. doi: 10.1302/0301-620X.77B6.7593107. [DOI] [PubMed] [Google Scholar]
- 19.Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: A randomized placebo-controlled study. J Orthop Traumatol. 2009;10((3)):127–133. doi: 10.1007/s10195-009-0062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yun MJ, Kim YH, Han MK, Kim JH, Hwang JW, Do SH. Analgesia before a spinal block for femoral neck fracture: Fascia iliaca compartment block. Acta Anaesthesiol Scand. 2009;53((10)):1282–1287. doi: 10.1111/j.1399-6576.2009.02052.x. [DOI] [PubMed] [Google Scholar]
- 21.Høgh A, Dremstrup ÆL, Skov ÆS. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. 2008:65–70. doi: 10.1007/s11751-008-0037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haines L, Dickman E, Ayvazyan S, et al. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med. 2012;43((4)):692–697. doi: 10.1016/j.jemermed.2012.01.050. [DOI] [PubMed] [Google Scholar]
- 23.Nie H, Yang Y-X, Wang Y, Liu Y, Zhao B, Luan B. Effects of continuous fascia iliaca compartment blocks for postoperative analgesia in patients with hip fracture. Pain Res Manag. 2015;20((4)):210–212. doi: 10.1155/2015/872651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szucs S, Iohom G, O'Donnell B, et al. Analgesic efficacy of continuous femoral nerve block commenced prior to operative fixation of fractured neck of femur. Perioper Med (London, England) 2012;1((1)):4. doi: 10.1186/2047-0525-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luger TJ, Kammerlander C, Benz M, Luger MF, Garoscio I. Peridural Anesthesia or Ultrasound-Guided Continuous 3-in-1 Block : Which Is Indicated for Analgesia in Very Elderly Patients With Hip. Fracture in the Emergency Department? 2013;3((3)):121–128. doi: 10.1177/2151458512470953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cuvillon P, Nouvellon E, Ripart J, et al. A comparison of the pharmacodynamics and pharmacokinetics of bupivacaine, ropivacaine (with epinephrine) and their equal volume mixtures with lidocaine used for femoral and sciatic nerve blocks: a double-blind randomized study. Anesth Analg. 2009;108((2)):641–649. doi: 10.1213/ane.0b013e31819237f8. [DOI] [PubMed] [Google Scholar]
- 27.Cuvillon P, Ripart J, Lalourcey L, et al. The continuous femoral nerve block catheter for postoperative analgesia: Bacterial colonization, infectious rate and adverse effects. Anesth Analg. 2001;93((4)):1045–1049. doi: 10.1097/00000539-200110000-00050. [DOI] [PubMed] [Google Scholar]


