Abstract
Bisphosphonate use has been associated with atypical pathologic fracture and slowed bone turnover. We present a case of a bisphosphonate-associated peri-implant atypical femur fracture following use of a recon nail for treatment of a prior bisphosphonate-associated atypical femur fracture.
Keywords: denosumab, bisphosphonates, atypical femoral fractures, peri-implant fractures
Introduction
Bisphosphonates are a drug class used to increase bone density in patients with osteoporosis by the reduction of osteoclast driven bone resorption. Their use has been associated with atypical subtrochanteric femur fractures hypothesized to be secondary to a decrease in bone remodeling.1–3 Like bisphosphonates, denosumab has been studied in the long-term treatment of postmenopausal women with osteoporosis. In their study of 4550 women with up to 8 years of denosumab use, Papapoulos, et al, report that markers of bone turnover continued to decrease and bone mineral density continued to significantly increase to 18.4% at the lumbar spine and 8.3% at the hip.4 Unfortunately, although the incidence was low, atypical femoral fracture and osteonecrosis of the jaw was also observed, similar to the complications observed in the long-term use of bisphosphonate. This has been reflected in several case reports.5–7
Recently a new clinical entity involving bisphosphonateassociated pathologic fracture of the femur has been identified: the bisphosphonate-associated periprosthetic fracture. Although the majority of case reports have identified stress fractures distal to the tip of the femoral stem following total hip arthroplasty,8–11 Lee, et al, identified a series of patients with atypical bisphosphonate associated peri-implant fractures with a low energy mechanism occurring at stress risers such as the end of the plate or the penultimate screw hole.12 These underwent revision surgery with a slower radiographic union at an average of 2–4 months. To our knowledge, this is the first report of a denosumab-associated atypical peri-implant femur fracture around a femoral nail.
Case Report
This is a case of a 92-year-old woman with a history of rheumatoid arthritis (RA), hypertension and remote history of bilateral atypical femur fracture status post bilateral fixation who presented to the emergency department in February of 2018 after a ground level presyncopal fall earlier that day. An angiotensin II receptor blocker (valsartan) was added to her low-dose beta blocker therapy a few weeks prior and she had been experiencing intermittent dizziness when rising to stand from sitting since initiation of her therapy. On the day of her presentation, she fell onto her buttocks when she stood up and felt dizzy and had immediate onset of inability to bear weight on her left lower extremity. She had been otherwise asymptomatic and functioning well prior to her fall. Her RA was mild and managed with 2.5mg of prednisone daily.
Most significant in her history was a history of sequential atypical femur fracture with subsequent surgical fixation. In 2008, following a multi-year history of treatment of osteoporosis with alendronate, she presented with an atypical subtrochanteric right femur fracture following a mechanical fall while walking her dog. She underwent uncomplicated fixation with a cephalomedullary device and returned to home following a brief stay in a shortterm rehabilitation facility. There was concern for pathologic fracture and her prednisone was decreased from 5mg daily to 2.5 mg daily. Alendronate was continued.
In 2010, she suffered an atypical left subtrochanteric femur fracture, again following a mechanical fall (Figure 1). She underwent uncomplicated fixation of her fracture with an intramedullary recon nail (Figure 2). As the fracture was distal in the femur, fixation was not placed into the femoral neck and head. Bisphosphonates were initially discontinued following this fracture. However, two years later, she was started on denosumab injection every 6 months starting in mid-2012, which was continued up to her current presentation.
Figure 1.
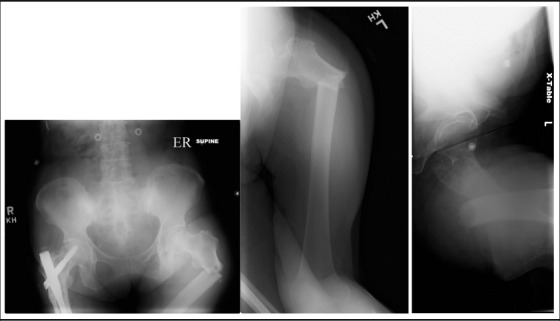
Prior Initial Injury Films Depicting Atypical Subtrochanteric Femur Fracture. Note that the \Contralateral Atypical Subtrochanteric Femur Fracture had been Treated with a Cephalomedullary Device.
Figure 2.
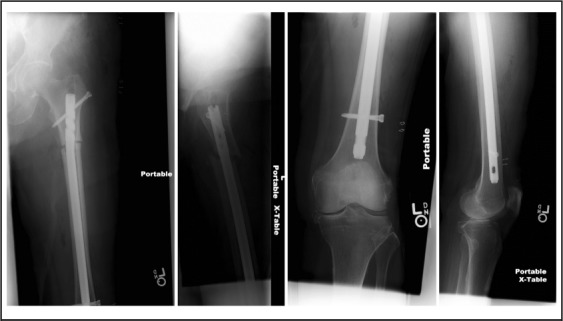
Postoperative Films Following Treatment of Atypical Subtrochanteric Femur Fracture with Reamed Intramedullary Femoral Recon Nail.
Radiographs obtained at the time of her current presentation demonstrated interval healing of her previous subtrochanteric fracture and an acute intertrochanteric fracture through the proximal locking screw with avulsion of the lesser trochanter (Figure 3). She was treated with a transition to a reamed cephalomedullary nail (Figure 4). Of note, she had broken the proximal interlocking screw at the site of the fracture. The medial fragment of the screw was left in situ as it did not block the intramedullary canal and the benefit versus risk analysis did not favor retrieval of the screw fragment. Antiresorptive agents were discontinued following her revision surgery. She recovered in a short-term rehabilitation facility followed by return to independent living at home. Interval healing has been noted on follow up radiographs.
Figure 3.

Injury Films Demonstrating Healing of Previous Atypical Femur Fracture Following Reamed Intramedullary Nail Placement, but New Atypical Peri-implant Femur Fracture Through and Around Previously Placed Locking Screw.
Figure 4.
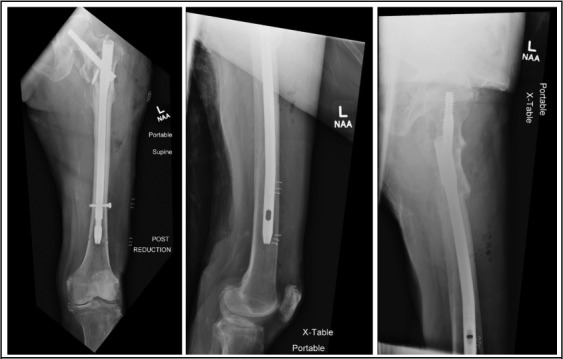
Postoperative Imaging Following Transition to Cephalomedullary Femoral Nail.
Discussion
In 2014, the task force from the American Society of Bone and Mineral Research revised the criteria for the diagnosis of a bisphosphonate associated atypical femoral fracture to a fracture found “just distal to the lesser trochanter to just proximal to the supracondylar flare” with at least four of the five identified major features:3
The fracture is associated with minimal or no trauma, as in a fall from a standing height or less
The fracture line originates at the lateral cortex and is substantially transverse in its orientation, although it may become oblique as it progresses medially across the femur
Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex
The fracture is noncomminuted or minimally comminuted
Localized periosteal or endosteal thickening of the lateral cortex is present at the fracture site (“beaking” or “flaring”)
Nevertheless, numerous studies have identified a number of cases where periprosthetic and peri-implant fractures have been associated with antiresorptive that present in a similar fashion, if not in the location described in the criteria. Sayed- Noor and Sjoden reported on a patient with history of nine years of bisphosphonate use and six years status post cemented total hip arthroplasty (THA) who sustained a thigh injury that progressed to a displaced Vancouver C atypical femur fracture over the course of 4 months.10 This was treated with a long locked plate and went onto eventual healing. Tantavisut, et al, described a 75-year-old woman with a seven year history of bisphosphonate use and two year history status post THA that was consistent with an atypical periprosthetic acetabular fracture by pattern and histology.13 Robinson, et al, studied the differences between patients on long term bisphosphonates with atypical femur fractures and atypical periprosthetic femur fractures.11 Periprosthetic femur fractures were found primarily in patients who had undergone THA and presented as stress fractures just distal to the tip of the stem. There were no cases of femoral stem loosening in this group. Fractures were treated with long locked plate fixation. They found atypical femur fractures occurred much more commonly that atypical periprosthetic femur fractures at a rate of 89% vs 11%, respectively. They also noted that patients who suffered atypical periprosthetic femur fractures had an increased time to union (8 months vs 5 months), increased mortality (10% vs 1%) and increased complications (25% vs 12%), although only increased complications reached statistical significance (P = .013). And as noted previously, Lee, at al, found a series of patients who sustained bisphosphonate associated peri-implant fractures.12
Connecting all these fractures—the atypical femur fracture, the atypical peri-prosthetic fracture and the atypical peri-implant fracture—is the occurrence of these fractures through areas of stress concentration under physiologic or low energy mechanisms. Whereas the native femur tends to fail in the tension sided subtrochanteric region, the presence of a prosthesis or implant changes the stress distribution of the femur and therefore the fracture location. Although a hip prosthesis appears to concentrate this stress just distal to the tip of the femoral stem, a plate or intramedullary implant appears to concentrate this stress at or near the end of the plate or nail, leading to fracture at the end of the plate or through a fixation hole near the end of the construct. This was the case observed in our patient. The presence of a stress riser with impaired resorption and accumulation of microfractures at this side may have led to the metal fatigue observed in the proximal locking screw and the subsequent intertrochanteric fracture.
An interesting finding in this case is that no fatigue failure or hardware complication has been observed on the right femur which was treated with a cephalomedullary nail for a bisphosphonate-associated atypical femur fracture two years prior to the placement of the left femoral nail which subsequently failed. This is similar to the findings of the cases of bisphosphonate-associated periprosthetic femur fractures where no stem loosening was noted and in the three dynamic hip screw cases reported by Lee, et al, where fracture consistently occurred distal to the plate.8–12 This suggests that failure in tension may be a key feature of antiresorptive-associated atypical femur fracture and constructs that protect the femur from tensile stress such as long cephalomedullary devices or long locked implants may be preferable in these patients.
We acknowledge that this is a retrospective review of a single patient with a rare presentation. However, we feel that this adds to knowledge of the variation in presentation of antiresorptiveassociated peri-implant femur fracture and identifies denosumabassociated peri-implant fracture as a clinical entity. Although this patient was previously on bisphosphonate therapy and was on corticosteroid therapy, her steroid therapy was sub-physiologic and nearly a decade had passed since the discontinuation of her bisphosphonate therapy, lessening the possible effect of these medications.
Further studies and identification of patients with similar presentations could help to further elucidate this condition. Consideration of primary placement of a long cephalomedullary device for these fractures may also be considered.
Glossary
- RA
rheumatoid arthritis
- THA
total hip arthroplasty
Conflicts of Interest
None of the authors identify any conflicts of interest.
References
- 1.Odvina C, Zerwekh J, Rao D, Maalouf N, Gottschalk F, Pak C. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90:1294–1301. doi: 10.1210/jc.2004-0952. [DOI] [PubMed] [Google Scholar]
- 2.Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364((18)):1728–37. doi: 10.1056/NEJMoa1010650. [DOI] [PubMed] [Google Scholar]
- 3.Shane E, Burr D, Abrahamsen B, Adler R, Brown T, Cheung A, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Howe TS, van der Meulen MCH, Weinstein RS, Whyte MP. Atypical Subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29((1)):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 4.Papapoulos S, Lippuner K, Roux C, Lin CJF, Kendler DL, Lewiecki EM, Brandi ML, Czerwinski E, Franek E, Lakatos P, Mautalen C, Minisola S, Reginster JY, Jensen S, Daizadeh NS, Wang A, Gavin M, Libanati C, Wagman RB, Bone HG. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM Extension study. Osteoporosis Int. 2015;26:2773–2783. doi: 10.1007/s00198-015-3234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schilcher J, Aspenberg P. Atypical fracture of the femur in a patient using denosumab – a case report. Acta Orthopaedica. 2014;85((1)):6–7. doi: 10.3109/17453674.2014.885355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drampalos E, Skarpas G, Barbounakis N, Michos I. Atypical femoral fractures bilaterally in a patient receiving denosumab. Acta Orthop. 2014;85((1)):3–5. doi: 10.3109/17453674.2013.854668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson RN, Armstrong CL, Heyburn G. Bilateral atypical femoral fractures in a patient prescribed denosumab - a case report. Bone. 2014;61:44–7. doi: 10.1016/j.bone.2013.12.027. [DOI] [PubMed] [Google Scholar]
- 8.Chen F, Bhattacharyya T. Periprosthetic fracture of the femur after long-term bisphosphonate use: a case report. JBJS Case Connect. 2012;2:e21. doi: 10.2106/JBJS.CC.K.00085. [DOI] [PubMed] [Google Scholar]
- 9.Chen F, Li R, Lall A, Kim SJ, Hirsh DM, Schwechter EM. Atypical Vancouver type-C periprosthetic fracture complicated by nonunion: a case report. JBJS Case Connect. 2015;5:e44. doi: 10.2106/JBJS.CC.N.00180. [DOI] [PubMed] [Google Scholar]
- 10.Sayed-Noor AS, Sjoden GO. Two femoral insufficiency fractures after long-term alendronate therapy. Clinical Orthop Relat Res. 2009;467:1921–1926. doi: 10.1007/s11999-009-0725-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson J, Leighton RK, Trask K, Bogdan Y, Tornetta P. Periprosthetic atypical femoral fractures in patients on long-term bisphosphonates: a multicenter retrospective review. J. Orthop Trauma. 2016;30((4)):170–176. doi: 10.1097/BOT.0000000000000508. [DOI] [PubMed] [Google Scholar]
- 12.Lee JYY, Soh T, Howe TS, Koh JSB, Kwek EBK, Chua DTC. Bisphosphonate-associated periimplant fractures: a new clinical entity? Acta Orthopaedica. 2015;86((5)):622–626. doi: 10.3109/17453674.2015.1036339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tantavisut S, Tanavalee A, Thanakit V, Ngarmukos S, Wilairatana V, Wanggroonsub Y. Spontaneous acetabular periprosthetic fracture in a patient continuously having zolendronic acid. Clinics in Orthopedic Surgery. 2014;6:358–360. doi: 10.4055/cios.2014.6.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]


