Abstract
Carpal tunnel syndrome costs the United States billions of dollars each year. The majority of patients are industrial workers, females, and the elderly who first present to their primary care physicians. Therefore, it is essential that the primary care physician understand this syndrome in order to diagnose and direct treatment. Here we present a review of the anatomy, pathophysiology, diagnosis, and current treatment of carpal tunnel syndrome that is relevant for the treating primary care physician. In addition, we discuss the role of the primary care physician in the diagnosis, management, and treatment of carpal tunnel syndrome. The aim of this review is to improve the integrated care of those patients suffering from carpal tunnel syndrome.
Keywords: Carpal Tunnel Syndrome, Peripheral Nerve Entrapment Syndrome
Introduction
Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment syndrome. It is defined as a compression of the median nerve at the level of the wrist joint associated with decreased function of the nerve at that level.1,2 It can be either acute or chronic, with chronic being much more common.1,3 Likewise, CTS is the most expensive upper extremity musculoskeletal disorder in the United States, with costs exceeding $2 billion annually.4 According to Dale, et al, CTS in the United States has an incidence of 5.8% and a prevalence of 7 to 19%, with higher numbers seen in industrial workers, females, and the elderly.4,5 As such, many patients with signs and symptoms of CTS will present initially to their primary care physician (PCP) who must in turn understand the syndrome in order to identify it and guide proper treatment.
Anatomy and Pathophysiology
The floor of the carpal tunnel is formed by the carpal bones, while the roof of the carpal tunnel is formed by the flexor retinaculum; which includes the transverse carpal ligament (TCL). There are ten structures running through the carpal tunnel: flexor pollicis longus, four tendons of flexor digitorum superficialis, four tendons of flexor digitorum profundus, and the median nerve (Figure 1).
Figure 1.
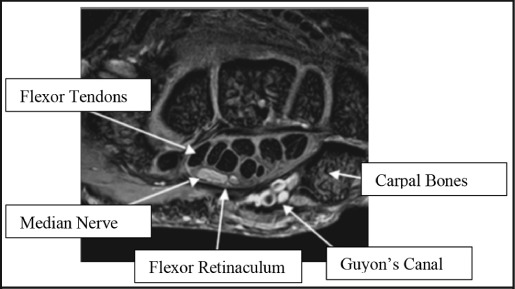
Carpal Tunnel Anatomy. CT wrist, axial view with wrist pronated. The floor of the carpal tunnel is formed by the carpal bones, while the roof of the carpal tunnel is formed by the flexor retinaculum.
The median nerve lies just below the TCL and is the most superficial structure in the tunnel. The recurrent motor branch of the median nerve most commonly divides from the median nerve proximal to the flexor retinaculum and innervates the muscles of the thenar muscles (abductor pollicis, the superficial head of flexor pollicis brevis, and the opponens muscle). Less commonly the recurrent motor branch divides in a subligamentous or transligamentous pattern. The median nerve continues through the carpal tunnel into the palm where it divides into digital nerves that provide sensation to the thumb, index, middle, and radial half of the ring finger.
The carpal tunnel is open both proximally and distally, but despite this it maintains a distinct tissue fluid pressure level due to its fibrous borders. The pressure in the carpal tunnel of a healthy individual ranges from 2.5 to 13 mmHg.6,7 A decrease in the cross-sectional area of the carpal tunnel can lead to an elevation in pressure that becomes critical above 20 to 30 mmHg.6,8 At this point epineural blood flow and axoplasmic flow is impeded, and nerve dysfunction, edema, and scarring can result9.
The most common symptoms of carpal tunnel syndrome are numbness, pain, and/or paresthesia in the thumb, index, middle, and radial half of the ring finger that is worst at night. Wrist flexion and extension increase pressure in the carpal canal, and wrist flexion during sleep may worsen symptoms such that patients awake with burning and numbness to the hand. Patients with moderate to severe disease can present with atrophy of the thenar muscles and, variably, decreased pinch and grip strength. They may also have pain that migrates proximally.
Risk Factors
Chronic Carpal Tunnel Syndrome
The majority of CTS cases are chronic and idiopathic; however, several risk factors have been identified. These include female gender (peak age 45 to 54 years), increasing age, obesity, thyroid disease, diabetes, pregnancy, renal failure, alcoholism, primary amyloidosis, and drug toxicity.5,7 Less commonly, space occupying lesions in the carpal tunnel may lead to compression of the median nerve. These include a persistent median artery, infection, ganglion cyst, tumor, or scar tissue. Rheumatoid arthritis is also a risk factor as it may lead to an increase in carpal tunnel pressure secondary to pannus formation or synovitis.7 Additionally, cervical degenerative disc disease may complicate the clinical picture due to overlapping symptoms or mimicking symptoms of CTS.
Carpal Tunnel Syndrome and Work
CTS is common in working age adults. The literature does show an association between CTS and the use of vibratory tools, increased hand force, repetitive wrist motion, and extreme flexion/extension of the wrist.5,7,10 Work activities that patients often associate with the onset of CTS is excessive keyboarding and mouse use. However, to date there has been no evidence to support this association. Thomsen et al performed a systematic review of the literature and concluded that there is insufficient evidence that computer work (keyboarding and mouse use) causes CTS.11 Additionally, they reviewed several papers looking at positions and forces exerted by computer users and concluded that carpal tunnel pressure increases with keyboarding and mouse use, but the pressure was still below potential harmful levels.11 Patients with CTS can be counseled, therefore, that use of a keyboard and mouse at work is unlikely to be the cause of their symptoms, but it is possible that these activities may aggravate them.
Acute Carpal Tunnel Syndrome
The clinician must be able to differentiate chronic CTS from acute CTS, as release of the carpal tunnel becomes urgent in the latter. The acute forms of CTS can be divided into traumatic and atraumatic. Traumatic CTS often results from wrist and carpal bone trauma resulting from direct compression or indirect compression of the nerve via hematoma and/or soft tissue swelling. Less commonly, the nerve may be directly injured (ie, transected) in a traumatic event. The uncommon atraumatic causes of acute CTS include septic arthritis, pseudogout, topaceous gout, soft tissue infections, calcifying tendinitis, tumoral calcinosis, and pigmented villonodular synovitis.3
Diagnosis
In 2007, the American Academy of Orthopedic Surgery (AAOS) released guidelines for diagnosing CTS.2 The following is a review of those guidelines in addition to our own recommendations.“
History
The diagnosis of CTS should always begin with a history. The clinician should ask about duration of symptoms, severity and character of symptoms, location of symptoms, radiation (eg, Do symptoms radiate from the shoulder?), progression of symptoms (better, worse, stable?), patient's lifestyle/activities, and any comorbidities. Table 1 describes classic features that may be obtained in a patient with CTS and may have clinical significance.
Table 1.
History of Present Illness in Carpal Tunnel Syndrome
| Clinical Question | Classic Presentation of CTS | Clinical Significance |
|---|---|---|
| Duration | Variable | Unclear whether duration of symptoms correlates with amount of nerve injury. This should be correlated with physical exam and diagnostic findings. |
| Location/Radiation | Along the median nerve distribution | Location and/or radiation of symptoms outside of this distribution may prompt the physician to consider diagnosis other than CTS. If there are symptoms within the median nerve distribution in addition to other distributions (eg, The ulnar nerve distribution) the physician may consider other diagnosis (ie, proximal nerve compression syndrome) that mimics CTS. |
| Association Symptoms | Decreased strength with pinching or grip | Due to atrophy of the thenar muscles |
| Timing of Symptoms | Increased symptoms at night when sleeping | It is common for patients to sleep with their elbows and wrist fully flexed, leading to an increase pressure in the carpal canal. Therefore, it is common for patients to report increased symptoms at night or when first waking up. |
| Lifestyle Activities | Activities that fully extend the wrist (driving, holding a telephone) or fully flex the wrist. Also, occupational hazards such as use of vibratory tools. | See Risk Factors in text. |
| Comorbidities | Obesity Diabetes | See Risk Factors in text. |
Physical Exam
The physical exam should note the patient's age, BMI, body habitus, range of motion of the wrist and hand, any deformities, swelling, atrophy, and skin trophic changes. In addition, pinch and grip strength can be measured if the proper equipment is available. A sensory and motor exam should be performed, along with provocative tests (described below). Table 2 describes classic features that may be observed in a patient with CTS.
Table 2.
Physical Exam in Carpal Tunnel Syndrome
| Physical Exam | Classic Presentation in CTS | Clinical Significance |
|---|---|---|
| Patient characteristics | Middle age female Obese | See Risk Factors in text. |
| Visual Findings | Thenar Atrophy | Thenar atrophy is predictive of CTS, but its appearance is rare. |
| Sensory Exam | Decreased Sensation in 1st through 3rd digit and radial side of 4th digit. Patient will report decreased sensation in the palmar aspect of the index finger when compared to palmar aspect of the index finger | Can help localize symptoms to the median nerve distribution. |
| Motor Exam | Weakness with pinch, grip, and thumb abduction | Patients may describe unintentional dropping of objects and clumsiness. |
Electrodiagnostic Studies
Electrodiagnostic studies include electromyography (EMG) and nerve conduction studies. Nerve conduction studies measure the strength and speed of impulses propagated down the length of a peripheral nerve. These studies measure the action potentials of both sensory and motor fibers. From these recordings, the amplitude of the waveform is measured, indicating the strength of the impulse via the number of axons successfully activated (unit is microvolts). Also measured is the latency, which reflects the speed of transmission through the nerve, also known as the nerve conduction velocity (units milliseconds).13 The EMG portion of the electrodiagnostic study involves a needle-recording of electrical activity and can indicate denervation or reinnervation in the setting of nerve injury.14 With regards to CTS, nerve conduction studies with a distal motor latency of greater than 4.5 ms and a sensory latency greater than 3.5 ms is considered abnormal. Further, the EMG may show evidence of nerve injury (increased insertional activity, positive sharp waves, fibrillations at rest, decreased motor recruitment, and complex repetitive discharges).15
The AAOS guidelines state that the physician may obtain electrodiagnostic tests to differentiate among diagnoses. However, they do not suggest using these tests as the primary diagnostic tool as electrodiagnostic studies have well recognized limitations. For instance, nerve conduction studies are limited to the evaluation of large myelinated nerves, and the results reflect the function of the best fibers rather than the worst. Also, electrodiagnostic tests are sensitive, but not specific (90%–94% sensitive, 50%–60% specific);14,16 which may lead to an erroneous diagnosis of “asymptomatic CTS”. Finally, there is limited evidence correlating electrodiagnostic tests findings alone with functional recovery or reemployment after carpal tunnel release (CTR);15 which limits the prognostic use of these studies. Electrodiagnostic testing cannot replace the clinical exam when making a diagnosis; however, in combination with the clinical exam these tests can be confirmatory. The AAOS guidelines recommend that physicians obtain electrodiagnostic tests if clinical and/or provocative tests are positive and surgical management is being considered.2
Ultrasonography
There has been recent interest in the use of ultrasonography in the diagnosis of carpal tunnel syndrome, stemming from a desire to decrease discomfort to the patient (associated with electrodiagnostic studies) and the increased use of ultrasound in general. Proponents of ultrasound argue that an increased cross-sectional area of the median nerve at the distal wrist crease will correlate with a diagnosis of CTS. Recently, Ting et al demonstrated a positive correlation between these ultrasound measurements and electrodiagnostic studies in patients with a diagnosis of CTS.17 Also, Wessel et al demonstrated a correlation between severity of CTS and both a thickening of the TCL and increased cross-sectional area of the median nerve.18 Although these findings are encouraging, there is not enough evidence to date to recommend ultrasound in the formal diagnosis of CTS.
Treatment
Once CTS is suspected or established, the patient should be referred to an orthopedic surgeon, ideally one that specializes in Hand and Upper Extremity. Primary care physicians can counsel their patients that treatment may include conservative management versus surgical management depending on the severity of disease.
Splints
Splinting is often recommended for patients with mild symptoms of CTS. The patient is placed into a wrist splint that maintains the wrist at neutral. The primary care physician can place any patient, regardless of suspected severity of disease, into a wrist splint as preliminary treatment. It may be particularly pertinent to initiate wrist splints if the patient cannot be seen immediately by the orthopedic surgeon.
When counseling the patient, it can be stressed that the wrist splint may alleviate some symptoms but may not cure CTS in every patient. Kaplan et al found five factors to be important in determining the success of nonoperative treatment. These include: (1) age over 50 years, (2) duration greater than 10 years, (3) constant paresthesia, (4) stenosing flexor tenosynovitis, (5) positive Phalen's test in less than 30 seconds. They found that conservative management was successful in up to 83.3% of patients if two or less factors were present. However, if three factors were present then success rates were less than 7%; and if four or five factors were present then the success rate was 0%.9,19
Injections
Corticosteroid injections may be recommended for patients with mild to moderate CTS. These injections have shown to provide effective relief of symptoms, but the effects are usually temporary.20,21 It has also been found that injections are more effective in men and patients older than 40 years.9 Aside from its use in treatment, alleviation of symptoms after a corticosteroid injection can confirm the diagnosis and likely success of carpal tunnel surgery. We recommend these injections be done by an orthopedic surgeon or provider that is performing them on a regular basis as misplaced injections can result in unresolved symptoms, earlier recurrence of symptoms and nerve damage with accidental intra-neural injection.
Surgical
Studies have shown superior outcomes with CTR as compared to splinting or injections.22 Conservative treatment is often exhausted before CTR is recommended, unless symptoms are severe (eg, thenar atrophy) on initial presentation. The surgery involves releasing the TCL longitudinally to relieve pressure within the carpal tunnel and decompress the median nerve. This can be done either with an open approach, a mini-open approach, or endoscopically. There is debate regarding the optimal approach and patient factors. Surgeon's experience will often play a role in choosing the surgical technique. Patients can be counseled that long-term outcomes are similar regardless of approach.
Summary
CTS is the most common compressive neuropathy. Conservative care is warranted in mild cases or in cases with recent onset of symptoms. Surgical treatment is effective for moderate to severe cases of CTS and will involve release of the TCL in order to relieve pressure within the carpal tunnel. Patient communication regarding expectations and outcomes is paramount, and many times will start with the primary care physician.
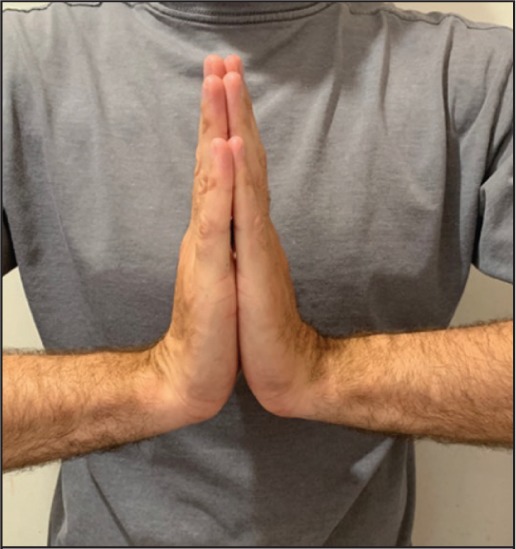
Figure 2.

Phalen Test. Dorsum of hands placed together so that maximum wrist flexion is achieved. This is held for 60 seconds.
Figure 3.
Reverse Phalen Test. Palms of hands placed together so that maximum wrist extension is achieved. This is held for 60 seconds.
Figure 4.

Median Nerve Compression Test. With patient's wrist at neutral, the examiner places moderate pressure over the carpal tunnel for 30 seconds.
Table 3.
Provocative Testing for Carpal Tunnel Syndrome
| Provocative Test | Clinical Presentation in CTS |
|---|---|
| Phalen Test (Figure 2) | Dorsum of hands placed together so that maximum wrist flexion is achieved. This is held for 60 seconds. |
| Reverse Phalen Test (Figure 3) | Palms of hands placed together so that maximum wrist extension is achieved. This is held for 60 seconds. |
| Tinel Sign | Pain or paresthesia in median nerve distribution elicited when examiner percusses from the palmar crease to the distal wrist crease. |
| Median Nerve Compression Test (Figure 4) | With patient's wrist at neutral, the examiner places moderate pressure over the carpal tunnel for 30 seconds. Consider the most sensitive and specific provocative test for diagnosing CTS (Sensitivity 87%, Specificity 90%). |
Abbreviations
- CTS
Carpal Tunnel Syndrome
- PCP
Primary Care Physician
- TCL
Transverse Carpal Ligament
Conflicts of Interest
None of the authors identify any conflicts of interest.
References
- 1.Day CS. Chapter 7: Fractures of the Metacarpals and Phalanges. Green7#x0027;s Operative Hand Surgery, 7th Edition [Google Scholar]
- 2.Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91((10)):2478–2479. doi: 10.2106/JBJS.I.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schnetzler KA. Acute carpal tunnel syndrome. J Am Acad Orthop Surg. 2008;16((5)):276–282. doi: 10.5435/00124635-200805000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Dale AM, Harris-Adamson C, Rempel D, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39((5)):495–505. doi: 10.5271/sjweh.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newington L, Harris EC, Walker-Bone K. Carpal tunnel syndrome and work. Best Pract Res Clin Rheumatol. 2015;29((3)):440–453. doi: 10.1016/j.berh.2015.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luchetti R, Schoenhuber R, De Cicco G, Alfarano M, Deluca S, Landi A. Carpal-tunnel pressure. Acta Orthop Scand. 1989;60((4)):397–399. doi: 10.3109/17453678909149305. [DOI] [PubMed] [Google Scholar]
- 7.Cranford CS, Ho JY, Kalainov DM, Hartigan BJ. Carpal tunnel syndrome. J Am Acad Orthop Surg. 2007;15((9)):537–548. doi: 10.5435/00124635-200709000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Lundborg G, Gelberman RH, Minteer-Convery M, Lee YF, Hargens AR. Median nerve compression in the carpal tunnel--functional response to experimentally induced controlled pressure. J Hand Surg Am. 1982;7((3)):252–259. doi: 10.1016/s0363-5023(82)80175-5. [DOI] [PubMed] [Google Scholar]
- 9.Azar FM, Beaty JH, Canale ST. Campbell7#x0027;s Operative Orthopaedics. Vol Four. Elsevier; 2017. [Google Scholar]
- 10.Barcenilla A, March LM, Chen JS, Sambrook PN. Carpal tunnel syndrome and its relationship to occupation: a meta-analysis. Rheumatology (Oxford) 2012;51((2)):250–261. doi: 10.1093/rheumatology/ker108. [DOI] [PubMed] [Google Scholar]
- 11.Thomsen JF, Gerr F, Atroshi I. Carpal tunnel syndrome and the use of computer mouse and keyboard: a systematic review. BMC Musculoskelet Disord. 2008;9:134. doi: 10.1186/1471-2474-9-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atroshi I, Gummesson C, Ornstein E, Johnsson R, Ranstam J. Carpal tunnel syndrome and keyboard use at work: a population-based study. Arthritis Rheum. 2007;56((11)):3620–3625. doi: 10.1002/art.22956. [DOI] [PubMed] [Google Scholar]
- 13.Gooch CL, Weimer LH. The electrodiagnosis of neuropathy: basic principles and common pitfalls. Neurol Clin. 2007;25((1)):1–28. doi: 10.1016/j.ncl.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 14.David P, Green M. Green's Operative Hand Surgery. 5th ed. Vol One. Elsevier; 2005. [Google Scholar]
- 15.Azar FM. Campbell's: Operative Orthopaedics. 13th Edition ed. Vol One. Philadelphia: Elsevier; 2017. [Google Scholar]
- 16.Wang WL, Buterbaugh K, Kadow TR, Goitz RJ, Fowler JR. A Prospective Comparison of Diagnostic Tools for the Diagnosis of Carpal Tunnel Syndrome. J Hand Surg Am. 2018;43((9)):833–836. e832. doi: 10.1016/j.jhsa.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Ting BL, Blazar PE, Collins JE, et al. Median Nerve Ultrasonography Measurements Correlate With Electrodiagnostic Carpal Tunnel Syndrome Severity. J Am Acad Orthop Surg. 2019;27((1)):e17–e23. doi: 10.5435/JAAOS-D-17-00557. [DOI] [PubMed] [Google Scholar]
- 18.Wessel LE, Marshall DC, Stepan JG, et al. Sonographic Findings Associated With Carpal Tunnel Syndrome. J Hand Surg Am. 2019;44((5)):374–381. doi: 10.1016/j.jhsa.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan SJ, Glickel SZ, Eaton RG. Predictive factors in the non-surgical treatment of carpal tunnel syndrome. J Hand Surg Br. 1990;15((1)):106–108. doi: 10.1016/0266-7681_90_90061-8. [DOI] [PubMed] [Google Scholar]
- 20.Meys V, Thissen S, Rozeman S, Beekman R. Prognostic factors in carpal tunnel syndrome treated with a corticosteroid injection. Muscle Nerve. 2011;44((5)):763–768. doi: 10.1002/mus.22183. [DOI] [PubMed] [Google Scholar]
- 21.Huisstede BM, Hoogvliet P, Randsdorp MS, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments--a systematic review. Arch Phys Med Rehabil. 2010;91((7)):981–1004. doi: 10.1016/j.apmr.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM. Splinting vs surgery in the treatment of carpal tunnel syndrome: a randomized controlled trial. JAMA. 2002;288((10)):1245–1251. doi: 10.1001/jama.288.10.1245. [DOI] [PubMed] [Google Scholar]


