Abstract
Purpose.
Among diverse, low-income urban adolescents with persistent asthma, we examined whether ADHD comorbidity, compared to asthma alone, was associated with clinical outcomes, healthcare utilization, and responsibility for self-management.
Methods.
We conducted a secondary analysis of data from a large school-based study of adolescents with asthma in Rochester, NY. Adolescents reported asthma symptoms over 2 weeks, and primary care and hospital admissions over one year. We assessed shared responsibility for asthma management between caregivers and adolescents.
Results.
ADHD comorbidity was common (28%) in this sample of 370 adolescents. Adolescents with ADHD had more primary care utilization and hospitalizations than those without, despite having similar asthma symptoms. Caregivers and adolescents with ADHD reported that adolescents had less shared responsibility for 9 asthma management tasks.
Conclusions.
Adolescents with ADHD share less responsibility for asthma self-management. These teens’ increased healthcare use might provide opportunities for clinicians to provide extra self-management support.
Introduction:
Asthma and attention deficit-hyperactivity disorder (ADHD) are common chronic diseases of childhood, affecting 13.2% and 9.6% of American children, respectively.[1] Youth with asthma are more likely than those without to be diagnosed with ADHD; one report estimates the national comorbidity rate to be 12%.[2] Adolescents with asthma struggle with self-management, and often their asthma symptoms worsen during adolescence.[3] Effective self-management skills improve asthma control, but ADHD may limit an adolescent’s ability to use these skills.[4, 5]
To explore associations between asthma self-management and ADHD comorbidity, we conducted a secondary analysis of data from a sample of diverse urban adolescents. We hypothesized that a dual diagnosis of ADHD and asthma increases asthma risk. Specifically, we predicted that adolescents with asthma and ADHD, compared to those with asthma alone, would have more asthma symptoms and health care utilization, and take less responsibility for asthma self-management.
Methods:
The School-based Asthma Care for Teens study was an IRB-approved randomized controlled trial to promote asthma self-management in adolescents. Our cross-sectional study was a secondary analysis of baseline data from surveys of enrolled adolescents and caregivers collected at the start of 3 consecutive school years (September through January; 2015-2017). Caregivers and adolescents (12-16 years old) were eligible if the caregiver reported that the adolescent had physician-diagnosed asthma with either persistent severity or poor control, as defined by National Heart, Lung, and Blood Institute guidelines.[6] We defined ADHD as answering “yes” to the question “Has a doctor ever diagnosed you with ADD/ADHD?” Data on specific ADHD symptoms and treatment were not collected.
Survey questions addressed demographics, health status, health care utilization, and shared responsibility for asthma self-management. Adolescents reported asthma symptoms over the past 2 weeks, including number of: 1) symptom-free days, 2) days/nights with symptoms, and 3) days with activity limitations (including in sports). They also reported number of PCP visits and hospital admissions in the prior year.
Caregivers and adolescents rated shared responsibility for asthma management, using an adaptation of two validated scales: the Asthma Responsibility Interview provided appropriate content, and our response format was based on the Diabetes Family Responsibility Questionnaire.[7, 8] They independently reported shared responsibility for 9 asthma management tasks (e.g., remembering and taking medications, avoiding triggers). Scaled responses for each task were: 1= managed by the parent only, 2= managed by parent and adolescent equally, and 3= managed by the adolescent. Total scores ranged from 9 to 27, with 18 representing equally shared responsibilities. We used independent samples, two-sided T-tests to compare groups (SPSS).
Results:
The analysis included 370 pairs of adolescents and caregivers (response rate, 79%), who were racially and ethnically diverse and economically disadvantaged (Table 1). The prevalence of asthma and ADHD comorbidity was 28% (104/370). The ADHD and non-ADHD cohorts were different in gender (80% vs 46% male), but similar in age, race, ethnicity and insurance type (Table 1).
Table 1.
Adolescents with persistent or poorly controlled asthma: Comparison of those with and without ADHD
| Teens with ADHD (n=104) |
ADHD (n=266) |
p-Value | |
|---|---|---|---|
| Demographics-n(%) | |||
| Teen Gender : Male | 84 (80%) | 123 (46%) | <0.001* |
| Teen Age: (mean, SD) | 13.4 (1.3) | 13.5 (1.2) | 0.59 |
| Teen Ethnicity: Hispanic | 40 (38%) | 80 (30%) | 0.14 |
| Teen Race: African American | 54 (50%) | 149 (56%) | 0.22 |
| Teen Insurance: Public | 90 (87%) | 222 (83%) | 0.42 |
| Teen-Reported symptom severity in last 14 Days- mean (SD) | |||
| Symptom free days | 7.2 (4.7) | 8.0 (5.0) | 0.18 |
| Nighttime symptoms | 4.7 (3.9) | 4.6 (4.6) | 0.95 |
| Daytime symptoms | 2.4 (3.2) | 2.4 (3.6) | 0.9 |
| Days needing to slow down | 3.3 (3.9) | 2.4 (3.6) | 0.04* |
| Days needing to take rescue medication | 3.5 (3.9) | 3.1 (4.1) | 0.35 |
| Teen-Reported health care utilization over previous year- mean (SD) | |||
| Primary care visits for any reason | 7.4 (11.7) | 4.4 (5.7) | <0.01* |
| Hospital visits for asthma | 0.17 (0.8) | 0.04 (0.2) | 0.02* |
| Teen-Reported asthma medication- n(%) | |||
| Has controller med at home | 73 (70%) | 152 (58%) | 0.03* |
| Took controller everyday for last 2 weeks | 20 (26%) | 45 (28%) | 0.75 |
The two cohorts had similar asthma symptoms, except that adolescents with ADHD comorbidity more often reported “needing to slow down.” Despite this similarity, adolescents with ADHD reported significantly more primary care visits in the prior year than participants without ADHD (x̄=7.4 vs 4.4, p<0.01). Adolescents with ADHD also had significantly more hospital admissions, although admissions per year were low in both groups (x̄=0.17vs0.04, p=0.02). They were also more likely to have an asthma controller medication at home (x̄=70% vs 58%, p=0.03), although they were no more likely to report consistent adherence (x̄=26% vs 28%, p=.75) (Table 1).
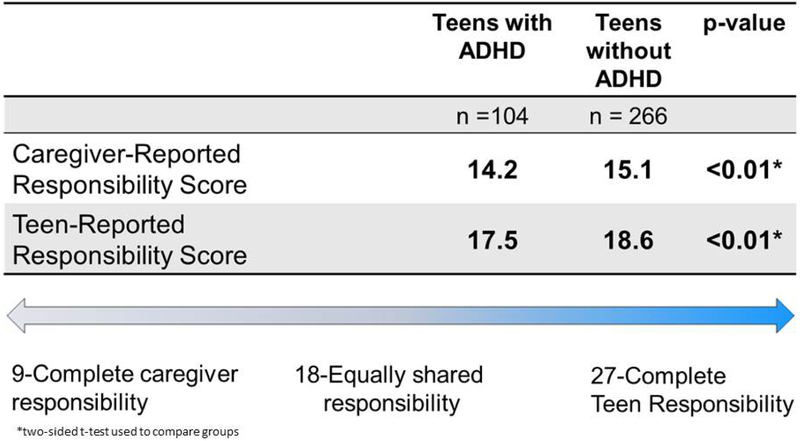
Caregivers of adolescents with ADHD perceived their teens to be less responsible for asthma self-management than caregivers of adolescents without ADHD, with a mean responsibility score of 14.2 vs 15.1 (p<0.01). Teens with ADHD agreed that their caregivers were more responsible for asthma treatment than they were (mean score <18). In both cohorts, adolescents rated their levels of responsibility higher than their caregivers did (Figure 1).
Figure 1: Teen responsibility for asthma management.
Teens and caregivers both provided data on shared responsibility for asthma care, using a validated scale. A score of 18 would indicate that the adolescent and caregiver share responsibility equally. Teens with ADHD had significantly lower scores for self-management than those without ADHD. Follow-up analysis showed that this difference was significant regardless of the age of the adolescent.
Discussion:
This study is innovative in assessing the clinical and healthcare implications of asthma and ADHD comorbidity, and the potential role of ADHD in asthma self-management. We report a high rate of comorbidity in this sample, 28% compared to 12% nationally. This may reflect our low-income sample of urban adolescents, a group known to have high risk for both asthma and ADHD.[9, 10] Our data were also collected in the fall and winter, when symptoms of both conditions might be elevated.
Contrary to our hypothesis, we found that asthma symptoms were similar between cohorts. However, adolescents with ADHD were more likely to seek primary care and be hospitalized. More frequent use of primary care could reflect their need for treatment for both conditions; more frequent follow-up might also have improved their asthma control. However, while more teens with ADHD reported having a controller medication, in both groups only around ¼ reported consistent adherence, reflecting a need for enhanced preventive care in both groups.
As we predicted, both adolescents with ADHD and their caregivers reported that caregivers carry more responsibility for asthma management, compared to caregivers of teens with asthma only. Asthma self-management may be a particular challenge for low-income youth, because they are likely to be given responsibility for asthma management at an early age.[5] Caregivers may need to provide additional support to adolescents with ADHD, who have impaired concentration and attention. Clinicians should recognize the challenges of transition to self-management for adolescents with ADHD by supporting their development of knowledge, skills, and autonomy. They should also consider linking them to available community resources.
Study limitations include our cross-sectional design, which cannot show causal associations, e.g., between ADHD and responsibility for asthma management. We did not collect data about ADHD symptoms or treatment. Data from this diverse, low-income sample with persistent or poorly controlled asthma may not generalize to all populations. Recall and reporting bias are also possible.
Conclusion and Implications:
Adolescents with both ADHD and asthma and their caregivers may benefit from focused anticipatory guidance about asthma self-management, especially since these adolescents may have inattention or organizational difficulties. This support is particularly important at a time when adolescents are developing autonomy in asthma self-management.
Acknowledgements:
We would like to acknowledge the Rochester City School District, and their nurses for their ongoing partnership and support of our work. We thank the School-Based Telemedicine Enhanced Asthma Management study team for their energy to help children with asthma. We thank the children, families, and primary care clinicians who participated in this study. I would also like to acknowledge the University of Rochester Academic Pediatric Fellowship for the time and support to complete this project.
Funding sources:
The School-Based Telemedicine Enhanced Asthma Management Study is sponsored by the National Heart, Lung, and Blood Institute R18 HL116244
Dr. Milne Wenderlich is supported by the Empire Clinical Research Investigator Program (ECRIP) at the University of Rochester Medical Center, sponsored by the New York State Department of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC. NHIS 2017 Sample Child File Frequency Report. 2017. May 22, 2018; Available from: https://www.cdc.gov/nchs/nhis/nhis_2017_data_release.htm.
- 2.Blackman JA and Gurka MJ, Developmental and Behavioral Comorbidities of Asthma in Children. Journal of Developmental & Behavioral Pediatrics, 2007. 28(2): p. 92–99. [DOI] [PubMed] [Google Scholar]
- 3.McQuaid EL, et al. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol, 2003. 28(5): p. 323–33. [DOI] [PubMed] [Google Scholar]
- 4.Schaefer MR, et al. Adherence to Attention-Deficit/Hyperactivity Disorder Medication During the Transition to College. J Adolesc Health, 2017. 60(6): p. 706–713. [DOI] [PubMed] [Google Scholar]
- 5.Jones MR, et al. Transition Readiness for Talking With Providers in Urban Youth With Asthma: Associations With Medication Management*. Journal of Adolescent Health, 2019. 64(2): p. 265–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma–Summary Report 2007. Journal of Allergy and Clinical Immunology, 2007. 120(5, Supplement): p. S94–S138. [DOI] [PubMed] [Google Scholar]
- 7.Wade SL, et al. Division of responsibility for asthma management tasks between caregivers and children in the inner city. Journal of developmental and behavioral pediatrics : JDBP, 1999. 20(2): p. 93–98. [DOI] [PubMed] [Google Scholar]
- 8.Vesco AT, et al. Responsibility Sharing between Adolescents with Type 1 Diabetes and Their Caregivers: Importance of Adolescent Perceptions on Diabetes Management and Control. Journal of Pediatric Psychology, 2010. 35(10): p. 1168–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pulcini CD, et al. Examining Trends and Coexisting Conditions Among Children Qualifying for SSI Under ADHD, ASD, and ID. Acad Pediatr, 2015. 15(4): p. 439–43. [DOI] [PubMed] [Google Scholar]
- 10.Akinbami LJ, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. 2012. [PubMed] [Google Scholar]