Abstract
Introduction:
Sugar-sweetened beverage (SSB) overconsumption is a major contributor to obesity. To reduce SSB consumption, policymakers have proposed requiring health warnings on SSBs. Randomized trials indicate that SSB warnings reduce SSB purchases, but uncertainty remains about how warnings affect population-level dietary and health outcomes.
Methods:
This study developed a stochastic microsimulation model of dietary behaviors and body weight using the 2005–2014 National Health and Nutrition Examination Surveys, research on SSB health warnings, and a validated model of weight change. In 2019, the model simulated a national SSB health warning policy’s impact on SSB intake, total energy intake, BMI, and obesity among U.S. adults during a 5-year period. Sensitivity analyses varied assumptions about: (1) how warning efficacy changes over time, (2) the magnitude of warnings’ impact on SSB intake, and (3) caloric compensation.
Results:
A national SSB health warning policy would reduce average SSB intake by 25.3 calories/day (95% uncertainty interval [UI]= −27.0, −23.6) and total energy intake by 31.2 calories/day (95% UI= −32.2, −30.1). These dietary changes would reduce average BMI by 0.64 kg/m2 (95% UI= −0.67, −0.62) and obesity prevalence by 3.1 percentage points (95% UI= −3.3%, −2.8%). Obesity reductions persisted when assuming warning efficacy wanes over time and when using conservative estimates of warning impact and caloric compensation. Benefits were larger for black and Hispanic adults than for white adults and for adults with lower SES than for those with higher SES.
Conclusions:
A national SSB health warning policy could reduce adults’ SSB consumption and obesity prevalence. Warnings could also narrow sociodemographic disparities in these outcomes.
INTRODUCTION
Nearly 40% of U.S. adults have obesity.1 A leading cause of death,2,3 obesity increases risk for cardiovascular disease, Type 2 diabetes, and some cancers.4,5 Overconsumption of sugar-sweetened beverages (SSBs) is a key driver of the obesity epidemic.6–9 Average SSB consumption among U.S. adults remains well above recommended levels,10–12 and is even higher among non-Hispanic black and Hispanic individuals10 and those with lower educational attainment and income.13 To reduce obesity, policymakers continue to seek strategies for addressing overconsumption of SSBs.14
Implementing health warnings on harmful products is a key tool that governments use to reduce unhealthy behaviors. For example, warnings on cigarettes are required in more than 150 countries,15 including the U.S., and have been found to reduce smoking.16 Increasingly, governments are also considering health warnings on foods and beverages, including SSBs. As of early 2019, five U.S. states have proposed policies that would require health warnings be displayed on SSB containers, vending machines selling SSBs, and at the point of purchase of unsealed SSBs.14,17–21 Online studies find that health warnings reduce intentions to purchase SSBs22–24 and recent experimental and quasi-experimental research indicates warnings reduce SSB purchases by up to 22%.25,26
Although experimental studies provide insight into how purchases may change under SSB health warning policies, it remains unknown how these individual-level changes affect the population-level health outcomes of most interest to policymakers. These population-level impacts depend not just on warnings’ effects on SSB purchases, but also on pre-policy beverage consumption, the relationship between SSB consumption and other dietary behaviors, and how dietary behaviors affect health outcomes like obesity.27 Simulation models can integrate this information systematically to estimate a policy’s impact on population health.28 Previous studies have used simulation models to examine SSB taxes,29–31 changes to federal nutrition assistance programs,32,33 and city-level SSB warning policies.27 To date, SSB warning policies have been proposed at the state and local levels, but the U.S. Food and Drug Administration has the regulatory authority to require SSB warnings nationwide.34,35 Recent experience with other public health policies (e.g., tobacco control efforts,36 requirements that restaurants post calorie information on menus37) suggests that state and local policies can spur national regulations. Thus, to inform ongoing policy debates, this study aimed to project plausible effects of a national SSB health warning policy on U.S. adults’ dietary behaviors and body weight.
METHODS
This study developed and applied a stochastic microsimulation model, representing events at the individual level.38 Analyses assessed outcomes during a 5-year period. Nearly all weight loss occurs in the first 3 years after a reduction in caloric intake,39,40 making a 5-year time horizon sufficient to capture the weight loss benefits from simulated policy changes. Table 1 describes key input parameters (see also Technical Appendix Tables 1 and 10, available online).
Table 1.
Input Parameters and Sources
| Parameter | Source(s) |
|---|---|
| Baseline characteristics | |
| Height and weight distributions for each | NHANES 2005–2014 cycles75 |
| demographic group | |
| Distribution of usual SSB intake for each | NHANES 2005–2014 cycles75 |
| demographic group | |
| Model representations of changes in diet and weight overtime | |
| Change in SSB intake due to a health warning policy | |
| Primary policy scenario | |
| Smallest reduction (12.7%) | Previous study of effect of health warnings on willingness to pay for SSBs;22 systematic review of price elasticity of demand for SSBs76 |
| Alternative scenarios | |
| Smallest reduction + decreasing efficacy overtime (−10%/year) | Previous study of change in cigarette warnings’ efficacy over time58 |
| Smallest reduction + increasing efficacy over time (+10%/year) | Previous study of change in cigarette warnings’ efficacy over time61 |
| Medium reduction (14.7%) | Previous study of graphic health warnings’ effect on SSB purchases25 |
| Largest reduction (22.4%) | Previous study of effect on SSB health warnings on SSB calories purchased26 |
| Change in total energy intake due to a change in SSB intake (i.e., caloric compensation) | |
| Primary policy scenario | |
| Sample from a distribution of possible values for caloric compensation suggesting a 1.0-calorie change in SSB intake yields a 0.63- to 1.84-calorie change in total energy intake | Range of estimates from previous studies25,48–52 |
| Alternative scenario | |
| More conservative estimate of caloric compensation applied to all individuals (1.0-calorie change in SSB intake yields a 0.63-calorie change in total energy intake) | Previous crossover trial examining caloric compensation after supplementation with SSBs or artificially-sweetened beverages48 |
| Change in body weight due to a change in total energy intake | Validated equations by Hall et al. (2011)39 |
| Population structure | |
| Population demographic distribution | American Community Survey Public Use Microdata Sample (ACS PUMS)55 |
NHANES, National Health and Nutrition Examination Survey; SSB, sugar-sweetened beverage.
Study Population
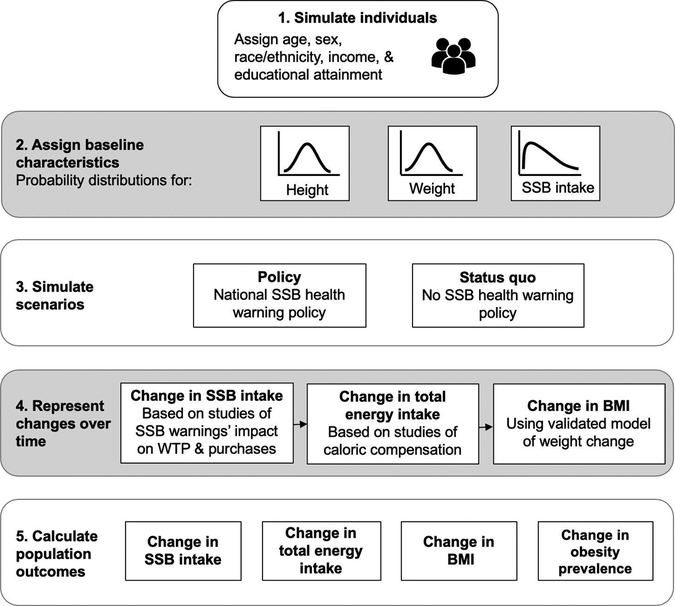
The model simulated an analytic sample of U.S. adults with varying demographic characteristics predictive of SSB intake10,13,41–43 (Figure 1; Technical Appendix Figure 1, available online). Each individual was assigned an age group (18–39 versus 40–65 years), sex (male versus female), race/ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic/Mexican American), education (some college or lower versus college degree or higher), and income (≤ 185% vs. >185% of the federal poverty level, the eligibility cut off for nutrition assistance programs in many states), similar to the approach used in previous studies32 (Technical Appendix, Section 2A).
Figure 1.
Simulation model overview.
SSB, sugar-sweetened beverage; WTP, willingness to pay.
The model used Monte Carlo sampling to assign baseline (pre-policy) height, weight, and SSB intake to simulated individuals, drawing from demographic-specific distributions estimated using dietary recall and anthropometric data from the National Health and Nutrition Examination Survey Cycles 2005–2014 (Technical Appendix, Section 2B and Table 2). Based on previous literature41–45 and existing U.S. policies,46,47 analyses defined SSBs as non-diet, non-alcoholic beverages with added sugars containing ≥5 calories/100 g, including sodas, sports drinks, energy drinks, fruit drinks, and pre-sweetened coffees and teas, but excluding 100% juice, milk-based drinks, and homemade SSBs (e.g., coffee sweetened with sugar by the consumer) that would not be subject to warnings.17–21
Procedures
The model represented two scenarios: a policy scenario assuming simulated individuals experienced a national SSB health warning policy and a status quo scenario assuming they experienced no SSB health warning policy (Technical Appendix, Section 3). The policy scenario assumed that simulated individuals could change their SSB intake in response to the warnings, then represented how change in SSB consumption would affect total energy intake, and finally translated change in total energy intake into change in body weight over time using a validated model of weight change dynamics.39 The status quo scenario assumed no change in SSB intake in response to health warnings. Both scenarios allowed SSB intake to change as individuals aged into the older category10,43 and incorporated secular trends in total energy intake (Technical Appendix, Sections 4A and 4B).
The policy scenario represented how individuals would respond to a SSB health warning policy (Technical Appendix, Section 4A). The primary policy scenario assumed that warnings would yield an average reduction in SSB intake of 12.7%, the most conservative (i.e., smallest) estimate of warning impact from previous experimental22,26 and quasi-experimental25 studies measuring the effect of SSB warnings on willingness to pay or beverage purchases among adults (assumption varied in sensitivity analyses described in the Statistical Analysis section). The model allowed for variation in individual responses to the SSB health warning policy by assigning each simulated individual a proportional change in SSB intake drawn from a triangular distribution of potential responses centered on a 12.7% reduction. The primary policy scenario assumed that change in SSB intake would be constant over time; for example, if an individual reduced their SSB intake by 10%, this one-time reduction would persist throughout the 5-year simulation period (assumption varied in sensitivity analyses). The status quo scenario assumed no change in SSB intake except from aging.
Individuals who reduce their SSB intake may replace SSB calories with calories from other sources. Previous studies suggest that a 1.0-calorie reduction in SSB intake yields a reduction in total energy intake of 0.63–1.84 calories;25,48–52 that is, individuals may partially compensate reductions in SSB intake, or may make additional dietary changes that further reduce total energy intake beyond SSB reductions. The primary policy scenario accounted for potential compensatory eating and drinking by having each simulated individual sample from a uniform distribution of values for caloric compensation (range, 0.63–1.84), following the approach used by Long et al.53 and others30,54 (Technical Appendix, Section 4B and Table 8; assumption varied in sensitivity analyses). The model multiplied individuals’ simulated change in SSB intake by their sampled compensation factor to yield change in total energy intake in calories/day.
To translate change in total energy intake into change in body weight, the model applied NIH’s validated model of weight change dynamics,39 which quantifies how body weight responds to changes in net caloric intake (Technical Appendix, Table 9). The weight change model was run in daily time steps during the 5-year simulation period, updating each individual’s body weight daily based on their net energy intake relative to their energy needs (Technical Appendix, Section 4C). Individuals’ BMI (kg/m2) and obesity status (BMI ≥30 kg/m2) were calculated using baseline height.
Statistical Analysis
The model estimated the effect of implementing a national SSB health warning policy on four outcomes: SSB intake, total energy intake, BMI, and obesity prevalence. Analyses used a difference-in-differences (DD) framework, comparing the change from baseline to the end of the 5-year simulation period when the simulated population experienced the SSB health warning policy scenario to change over time when the simulated population experienced the status quo scenario (Technical Appendix, Section 5). Results show policy impacts for U.S. adults aged 18–65 years at model initiation (hereafter “U.S. adults”), who were aged 23–70 years at the end of the 5-year simulation period. To produce estimates representative of this subset of U.S. adults, all analyses weighted observations based on the American Community Survey Public Use Microdata Sample55 (Technical Appendix, Section 5). Analyses examined outcomes both overall and within demographic subgroups. To explore the potential for warnings to reduce disparities, analyses computed differences in warning impact between demographic subgroups.
The model used Monte Carlo sampling from predetermined distributions of model input parameters (Technical Appendix, Section 6 and Table 10). Analyses calculated average impacts as the mean of the DD estimates from 10,000 repetitions56,57 of the model and reported 95% uncertainty intervals (UIs) bounded by the 2.5th and 97.5th percentiles of the DD estimates. This study used de-identified secondary data and was exempt from review by the University of North Carolina, Chapel Hill, IRB. Analyses occurred in 2019 using Stata, SE version 15.1.
Sensitivity analyses examined alternate assumptions about three key model parameters: (1) the trajectory of warning efficacy over time, (2) the magnitude of warnings’ impact on SSB intake, and (3) caloric compensation (Technical Appendix, Section 7). First, analyses varied assumptions about how SSB health warnings’ effectiveness may change over time. To date, only one study has examined the efficacy of SSB health warnings beyond immediate impacts, finding that graphic SSB health warnings exerted stable effects on SSB purchases during a 2-week period.25 Literature on tobacco warnings provides additional estimates of how warning efficacy may change over time. Some studies have reported that cigarette warnings’ efficacy “wears out” (decreases) by 1.1%–4.8% per year,58 whereas others found the opposite, that behavioral responses to cigarette warnings increase over time by as much as 20% per year.59–61 Sensitivity analyses evaluated two scenarios: first, assuming the impact of warnings on SSB consumption decreases by 10% per year (about twice the maximum rate of decline observed in a prior study58) and second, assuming impact increases by 10% per year (about half the maximum rate of increase observed in a prior study61).
Second, sensitivity analyses evaluated two alternate estimates of the impact of SSB health warnings on SSB consumption. Based on a quasi-experiment of graphic SSB health warnings,25 analyses evaluated policy impact when assuming SSB health warnings would yield a 14.8% reduction in SSB consumption. Analyses also examined outcomes when assuming that warnings produce a 22.4% reduction in SSB consumption, the impact of text health warnings on SSB purchases observed in a recent RCT.26 Finally, analyses evaluated an alternate assumption about caloric compensation, assuming that a 1-calorie reduction in SSB intake would yield only a 0.63-calorie reduction in total energy intake, the most conservative estimate of caloric compensation (i.e., highest degree of compensation) from previous trials of SSB caloric compensation in adults.48,50,51
Simulated baseline average height, weight, and SSB intake accurately reflected actual population averages of these variables (Technical Appendix, Section 8, Tables 3–5). Additionally, the model’s simulated average changes in SSB intake and total energy intake closely matched changes in these variables expected based on input parameters (Technical Appendix, Section 8, Tables 6 and 7). The NIH weight change model has been validated previously against observed weight changes in weight loss trials.39 Model testing analyses62 provided additional evidence supporting the validity of the weight change model by showing that it accurately reproduced secular trends in BMI from 2007 to 2014 (Technical Appendix, Section 8 and Figure 2).
Figure 2.
Estimated impacts of a national sugar-sweetened beverage health warning policy by model assumptions, mean (95% uncertainty interval).
RESULTS
Relative to the status quo, implementing a national SSB health warning policy would reduce SSB intake over baseline consumption levels by 25.3 calories/day (95% UI= −27.0, −23.6) under primary policy scenario assumptions (Figure 2). The reduction in SSB intake would reduce total energy intake by 31.2 calories/day (95% UI= −32.2, −30.1) (Figure 2). These dietary changes would yield gradual reductions in BMI over time (Figure 3). At the end of the 5-year simulation period, average BMI among individuals experiencing the SSB health warning policy would be 0.64 kg/m2 lower than in the status quo model (95% UI= −0.67, −0.62) (Figure 2). In turn, obesity prevalence among U.S. adults (aged 23–70 years at the end of the 5-year simulation period) would be reduced by 3.1 percentage points (95% UI= −3.3%, −2.8%) (Figure 2).
Figure 3.
Impact of a national sugar-sweetened beverage health warning policy on average BMI over 5 years, primary policy scenario vs. status quo scenario (95% uncertainty interval).
Reductions in SSB intake, total energy intake, BMI, and obesity were present for all demographic groups, including white, black, and Hispanic adults; younger and older adults; those with lower and higher education and income; and male and female adults (Appendix Figure 3). Some groups experienced larger reductions than others (Appendix Table 11). For example, black adults experienced larger reductions in obesity prevalence (−3.7 percentage points) than white adults (−2.7 percentage points) (difference in reductions: 0.9 percentage points, 95% UI=0.4%, 1.5%), as did Hispanic adults compared with white adults (difference in reductions: 1.1 percentage points, 95% UI=0.6%, 1.7%). Adults with lower education showed larger reductions in obesity prevalence than adults with higher education (difference in reductions: 1.7 percentage points, 95% UI=1.2%, 2.2%). Likewise, a similar pattern was found for adults with lower versus higher income (difference in reductions: 0.9 percentage points, 95% UI=0.4%, 1.4%).
The dietary and health benefits of the SSB warning policy were robust to different assumptions about the trajectory of warnings’ efficacy over time. Results were similar to the primary policy scenario when assuming warning efficacy would decrease by 10%per year and when assuming that warning efficacy would increase by 10% per year (Figure 2).
When SSB health warnings were assumed to reduce SSB intake by 14.8%, reductions in obesity prevalence increased in magnitude (DD= −3.9 percentage points, 95% UI= −4.2%, −3.7%) (Figure 2). Benefits were even larger when assuming SSB health warnings would reduce SSB consumption by 22.4% (Figure 2).
Using a more conservative assumption about caloric compensation yielded smaller reductions in total energy intake compared with the primary policy scenario (DD= −15.9 calories/day, 95% UI= −16.4, −15.4), but still yielded reductions in obesity prevalence (DD= −1.8 percentage points, 95% UI= −2.0, −1.6%).
DISCUSSION
Average SSB consumption in the U.S. remains well above recommended levels.10–12 Recent research indicates SSB health warnings would reduce SSB purchases,22,25,26 suggesting warnings could be a promising strategy for improving population health. The current study found that implementing a national SSB health warning policy could reduce adults’ SSB consumption by about 25 calories/day. This reduction in SSB intake yielded a 3.1–percentage point reduction in obesity prevalence, consistent with previous simulations showing that modest dietary changes can affect obesity.27,29–32,53 Although this reduction in obesity prevalence may appear modest, on a national scale, it equates to more than 5 million fewer adults with obesity.
Warnings reduced obesity prevalence in all demographic groups. Further, obesity reductions were larger for black and Hispanic adults compared with white adults, and for adults with lower educational attainment and lower income versus adults with higher educational attainment and higher income. These larger obesity reductions reflect the persistently higher levels of SSB intake and obesity among racial/ethnic minorities and those with lower SES.13,63 These results suggest that SSB health warnings could help narrow these disparities.
Results were robust to a range of assumptions tested in sensitivity analyses. Assuming that SSB health warnings will become 10% less effective per year had minimal effect on results compared to assuming constant efficacy over time. This finding reflects the dynamics of weight change and the limited time horizon of the model: Because much of expected weight loss occurs in the first year after reducing caloric intake,39 substantial weight loss is achieved before warning efficacy begins to wane.
Of the parameters varied in sensitivity analyses, changing assumptions about SSB health warnings’ impact on SSB consumption had the largest effect on projected dietary and health outcomes. Compared with the primary policy scenario, which assumed the most conservative reduction, using the largest estimate of warnings’ impact on SSB consumption nearly doubled the obesity reduction benefits of implementing a national SSB health warning policy. These findings highlight the importance of designing SSB warnings to maximize behavioral impact. Previous research suggests this goal may be accomplished by using pictorial warnings,16,24,25,64 making warnings larger and more prominent,65,66 or presenting warnings on black67 or red68 labels.
Two key strengths of this study are that it used detailed, nationally representative dietary and anthropometric data to establish characteristics of the simulated population and that it applied a validated model of weight change. This study also evaluated a range of sensitivity analyses to account for uncertainty about key parameters.
Limitations
This study also had several limitations. First, like all models, this microsimulation was a simplification of reality and did not reflect all possible factors affecting diet and obesity. Second, this study conducted one-way sensitivity analyses, and future studies should explore interactions between different assumptions about key parameters. Third, because no studies to date have estimated SSB health warnings’ impact on SSB consumption, the model used estimates of impact on willingness to pay or purchases as proxies for impact on consumption. Additionally, the model assumed that SSB health warnings would exert the same proportional effect on SSB consumption for all demographic groups. Previous studies of SSB22,23,26,68 and cigarette warnings16 have generally not found differences in warning efficacy by key demographic characteristics, but it is possible that sociodemographics may moderate SSB warnings’ impact on behavior in ways not reflected in the model, causing overestimation or underestimation of warnings’ benefits.
The model’s scope was constrained by lack of data on warnings’ impacts on social norms, reformulation, and interactions with other policies. SSB warnings could strengthen norms about limiting SSB consumption, which might amplify warnings’ impacts,69–71 but the model did not examine this possibility. The model also did not incorporate the possibility that manufacturers will reformulate products in response to warning policies, for example, by lowering SSBs’ calorie content to avoid triggering a warning, thereby providing healthier options for consumers.72–74 These assumptions could cause analyses to underestimate warnings’ benefits. Additionally, the model assumed no other policy changes, though SSB warnings could be implemented in tandem with other policies, such as SSB taxes. As more data on norms, reformulation, and other policies become available, future studies can incorporate this information.
CONCLUSIONS
Average SSB consumption in the U.S. remains high,10–12 increasing the risks for obesity and weight-related chronic diseases. This microsimulation study provides timely evidence that implementing a national SSB health warning policy could yield meaningful reductions in obesity prevalence.
Supplementary Material
ACKNOWLEDGMENTS
We wish to thank Sandeep Sarangi for assistance with research computing.
The research presented in this paper is that of the authors and does not reflect official policy of NIH.
AHG received training support from NIH (T32 HD007168, Principal Investigator: Entwisle) and the University of North Carolina Royster Society of Fellows (no award number). AHG, NRS, and LST received general support from NIH (CPC P2C HD050924, Principal Investigator: Frankenberg). NRS received training support from NIH (T32 HD091058, Principal Investigator: Aiello). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. This study used de-identified secondary data and was exempt from review by the IRB.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Ogden C, Carroll M, Kit B, Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The U.S. Burden of Disease Collaborators. The state of U.S. health, 1990–2016: burden of diseases, injuries, and risk factors among U.S. states. JAMA. 2018;319(14):1444–1472. 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 4.National Institute of Diabetes and Digestive and Kidney Diseases Health risks of being overweight. www.niddk.nih.gov/health-information/weight-management/health-risks-overweight. Published February 2015. Accessed July 29, 2019. [Google Scholar]
- 5.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2224–2260. 10.3410/f.719894684.793533485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malik VS, Popkin BM, Bray GA, Després J-P, Hu FB. Sugar-sweetened beverages, obesity, Type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121(11):1356–1364. 10.1161/circulationaha.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu F Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14(8):606–619. 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brownell KD, Frieden TR. Ounces of prevention: the public policy case for taxes on sugared beverages. N Engl J Med. 2009;360(18):1805–1808. 10.1056/nejmp0902392. [DOI] [PubMed] [Google Scholar]
- 9.Woodward-Lopez G, Kao J, Ritchie L. To what extent have sweetened beverages contributed to the obesity epidemic? Public Health Nutr. 2011;14(3):499–509. 10.1017/s1368980010002375. [DOI] [PubMed] [Google Scholar]
- 10.Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003–2014. Obesity. 2018;26(2):432–441. 10.1002/oby.22056. [DOI] [PubMed] [Google Scholar]
- 11.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–944. 10.1161/cir.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 12.HHS, United States Department of Agriculture. Dietary Guidelines for Americans 2015–2020. 8th ed http://health.gov/dietaryguidelines/2015/guidelines/. Published December 2015. Accessed November 10, 2016. [Google Scholar]
- 13.Rehm C, Peñalvo J, Afshin A, Mozaffarian D. Dietary intake among U.S. adults, 1999–2012. JAMA. 2016;315(23):2542–2553. 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falbe J, Madsen K. Growing momentum for sugar-sweetened beverage campaigns and policies: costs and considerations. Am J Public Health. 2017;107(6):835–838. 10.2105/ajph.2017.303805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Canadian Cancer Society. Cigarette Package Health Warnings: International Status Report. https://tobaccolabels.s3.ca-central-1.amazonaws.com/uploads/2016/11/Cigarette-Package-Health-Warnings-International-Status-Report-English-CCS-Oct-2016.pdf. Published October 2016. Accessed July 3, 2019. [Google Scholar]
- 16.Brewer NT, Hall MG, Noar SM, et al. Effect of pictorial cigarette pack warnings on changes in smoking behavior: a randomized clinical trial. JAMA Intern Med. 2016;176(7):905–912. 10.1001/jamainternmed.2016.2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sugar-Sweetened Beverages: Safety Warnings, SB 347, California Legislature, 2019–2020 Regular Sess. (2019).
- 18.Concerning Mitigation of the Adverse Impacts of Sugar-Sweetened Beverages, HB 2798, Washington State Legislature, 2016 1st Special Sess. (2016).
- 19.Relating to Health, HB 1209, State of Hawaii House of Representatives, 29th Legislature (2017).
- 20.An Act Related to Health and Safety Warnings on Sugar-Sweetened Beverages, H433, Vermont General Assembly, 2017–2018 Sess. (2017).
- 21.Requires Sugar-Sweetened Beverages to Be Labeled with a Safety Warning, S473, New York State Senate, 2019–2020 Legislative Sess. (2019).
- 22.Roberto CA, Wong D, Musicus A, Hammond D. The influence of sugar-sweetened beverage health warning labels on parents’ choices. Pediatrics. 2016;137(2):e20153185 10.1542/peds.2015-3185. [DOI] [PubMed] [Google Scholar]
- 23.VanEpps EM, Roberto CA. The influence of sugar-sweetened beverage warnings: a randomized trial of adolescents’ choices and beliefs. Am J Prev Med. 2016;51(5):664–672. 10.1016/j.amepre.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bollard T, Maubach N, Walker N, Mhurchu CN. Effects of plain packaging, warning labels, and taxes on young people’s predicted sugar-sweetened beverage preferences: an experimental study. Int J Behav Nutr Phys Act. 2016;13(1):95 10.1186/s12966-016-0421-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donnelly G, Zatz L, Svirsky D, John L. The effect of graphic warnings on sugary-drink purchasing. Psych Science. 2018;29(8):1321–1333. 10.1177/0956797618766361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grummon AH, Taillie LS, Golden SD, Hall MG, Ranney LM, Brewer NT. Sugar-sweetened beverage health warnings and purchases: a randomized controlled trial. Am J Prev Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee BY, Ferguson MC, Hertenstein DL, et al. Simulating the impact of sugar-sweetened beverage warning labels in three cities. Am J Prev Med. 2018;54(2):197–204. 10.1016/j.amepre.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rutter CM, Zaslavsky AM, Feuer EJ. Dynamic microsimulation models for health outcomes: a review. Med Decis Making. 2011;31(1):10–18. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basu S, Vellakkal S, Agrawal S, Stuckler D, Popkin B, Ebrahim S. Averting obesity and Type 2 diabetes in India through sugar-sweetened beverage taxation: an economic-epidemiologic modeling study. PLoS Medicine. 2014;11(1):e1001582 10.1371/journal.pmed.1001582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Coxson P, Shen Y-M, Goldman L, Bibbins-Domingo K. A penny-per-ounce tax on sugar-sweetened beverages would cut health and cost burdens of diabetes. Health Aff. 2012;31(1):199–207. 10.1377/hlthaff.2011.0410. [DOI] [PubMed] [Google Scholar]
- 31.Lin B-H, Smith TA, Lee, Hall KD. Measuring weight outcomes for obesity intervention strategies: the case of a sugar-sweetened beverage tax. Econ Hum Biol. 2011;9(4):329–341. 10.1016/j.ehb.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Basu S, Seligman HK, Gardner C, Bhattacharya J. Ending SNAP subsidies for sugar-sweetened beverages could reduce obesity and Type 2 diabetes. Health Aff. 2014;33(6):1032–1039. 10.1377/hlthaff.2013.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basu S, Seligman H, Bhattacharya J. Nutritional policy changes in the Supplemental Nutrition Assistance Program: a microsimulation and cost-effectiveness analysis. Med Decis Making. 2013;33(7):937–948. . [DOI] [PubMed] [Google Scholar]
- 34.Pomeranz JL. Advanced policy options to regulate sugar-sweetened beverages to support public health. J Public Health Policy. 2012;33(1):75–88. 10.1057/jphp.2011.46. [DOI] [PubMed] [Google Scholar]
- 35.Pomeranz JL. Outstanding questions in First Amendment Law related to food labeling disclosure requirements for health. Health Aff. 2015;34(11):1986–1992. 10.1377/hlthaff.2015.0616. [DOI] [PubMed] [Google Scholar]
- 36.Shipan CR, Volden C. Bottom-up federalism: the diffusion of antismoking policies from U.S. cities to states. Am J Pol Sci. 2006;50(4):825–843. 10.1111/j.1540-5907.2006.00218.x. [DOI] [Google Scholar]
- 37.Block JP. The calorie-labeling saga: federal preemption and delayed implementation of public health law. N Engl J Med. 2018;379:103–105. 10.1056/nejmp1802953. [DOI] [PubMed] [Google Scholar]
- 38.Briggs AD, Wolstenholme J, Blakely T, Scarborough P. Choosing an epidemiological model structure for the economic evaluation of non-communicable disease public health interventions. Popul Health Metr. 2016;14(1):17 10.1186/s12963-016-0085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hall KD, Sacks G, Chandramohan D, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378(9793):826–837. 10.1016/s0140-6736(11)60812-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Polglase B NIH research model predicts weight with varying diet, exercise changes: Findings challenge one-size-fits all weight assumptions. NIH. www.nih.gov/news-events/news-releases/nih-research-model-predicts-weight-varying-diet-exercise-changes. Published August 25, 2011. Accessed July 17, 2019. [Google Scholar]
- 41.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet. 2013;113(1):43–53. 10.1016/j.jand.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among U.S. adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2008;89(1):372–381. 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 43.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98(1):180–188. 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Popkin BM, Haines PS, Siega-Riz AM. Dietary patterns and trends in the United States: the UNC-CH approach. Appetite. 1999;32(1):8–14. 10.1006/appe.1998.0190. [DOI] [PubMed] [Google Scholar]
- 45.Wang Y, Bleich S, Gortmaker S. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among U.S. children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–e1614. 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 46.Alameda County Registrar of Voters. Measure D- City of Berkeley. www.acgov.org/rov/current_election/226/index.htm. Published November 12, 2014. Accessed June 16, 2015. [Google Scholar]
- 47.An Ordinance Imposing a Tax on Engaging in the Business of Distributing Sweetened Beverages, Seattle Municipal Code Ordinance No. 125324, § 2, Chapter 5 (2017).
- 48.Tordoff MG, Alleva AM. Effect of drinking soda sweetened with aspartame or high-fructose corn syrup on food intake and body weight. Am J Clin Nutr. 1990;51(6):963–969. 10.1093/ajcn/51.6.963. [DOI] [PubMed] [Google Scholar]
- 49.Finkelstein EA, Zhen C, Bilger M, Nonnemaker J, Farooqui AM, Todd JE. Implications of a sugar-sweetened beverage (SSB) tax when substitutions to non-beverage items are considered. J Health Econ. 2013;32:219–239. 10.1016/j.jhealeco.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 50.Reid M, Hammersley R, Hill AJ, Skidmore P. Long-term dietary compensation for added sugar: effects of supplementary sucrose drinks over a 4-week period. Br J Nutr. 2007;97(1):193–203. 10.1017/s0007114507252705. [DOI] [PubMed] [Google Scholar]
- 51.Van Wymelbeke V, Béridot-Thérond M-E, de La Guéronnière V, Fantino M. Influence of repeated consumption of beverages containing sucrose or intense sweeteners on food intake. Eur J Clin Nutr. 2003;58:154–161. 10.1038/sj.ejcn.1601762. [DOI] [PubMed] [Google Scholar]
- 52.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes. 2000;24(6):794–800. 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 53.Long MW, Gortmaker SL, Ward ZJ, et al. Cost effectiveness of a sugar-sweetened beverage excise tax in the U.S. Am J Prev Med. 2015;49(1):112–123. 10.1016/j.amepre.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sánchez-Romero LM, Penko J, Coxson PG, et al. Projected impact of Mexico’s sugar-sweetened beverage tax policy on diabetes and cardiovascular disease: a modeling study. PLoS Med. 2016;13(11):e1002158 10.1371/journal.pmed.1002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Census Bureau U.S. PUMS Data. American Community Survey (ACS). www.census.gov/programs-surveys/acs/data/pums.html. Published August 23, 2018. Accessed October 2, 2018. [Google Scholar]
- 56.Mundform DJ, Schaffer J, Kim M-J, Shaw D, Thongteeraparp A, Supawan P. Number of replications required in Monte Carlo simulation studies: a synthesis of four studies. J Mod Appl Stat Methods. 2011;10(1):4 10.22237/jmasm/1304222580. [DOI] [Google Scholar]
- 57.Schaffer JR, Kim M-J. Number of replications required in control chart Monte Carlo simulation studies. Commun Stat Simul Comput. 2007;36(5):1075–1087. 10.1080/03610910701539963. [DOI] [Google Scholar]
- 58.Hitchman SC, Driezen P, Logel C, Hammond D, Fong GT. Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002–2011. Nicotine Tob Res. 2014;16(5):536–543. 10.1093/ntr/ntt196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parada H, Hall MG, Boynton MH, Brewer NT. Trajectories of responses to pictorial cigarette pack warnings. Nicotine Tob Res. 2018;20(7):876–881. 10.1093/ntr/ntx182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers. Am J Public Health. 2004;94(8):1442–1445. 10.2105/ajph.94.8.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Swayampakala K, Thrasher JF, Yong H-H, et al. Over-time impacts of pictorial health warning labels and their differences across smoker subgroups: results from adult smokers in Canada and Australia. Nicotine Tob Res. 2018;20(7):888–896. 10.1093/ntr/ntx134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM, Wong JB. Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–7. Med Decis Making. 2012;32(5):733–743. . [DOI] [PubMed] [Google Scholar]
- 63.Ogden CL, Fakhouri TH, Carroll MD, et al. Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2017;66(50):1369–1373. 10.15585/mmwr.mm6650a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2015;25:341–354. 10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. 10.1016/j.socscimed.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Noar SM, Francis DB, Bridges C, Sontag JM, Brewer NT, Ribisl KM. Effects of strengthening cigarette pack warnings on attention and message processing: a systematic review. Journal Mass Commun Q. 2016;94(2):416–442. 10.1177/1077699016674188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cabrera M, Machín L, Arrúa A, et al. Nutrition warnings as front-of-pack labels: influence of design features on healthfulness perception and attentional capture. Public Health Nutr. 2017;20(18):3360–3371. 10.1017/s136898001700249x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grummon AH, Hall MG, Taillie LS, Brewer NT. How should sugar-sweetened beverage health warnings be designed? A randomized experiment. Prev Med. 2019;121:158–166. 10.1016/j.ypmed.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Orbell S, Lidierth P, Henderson CJ, et al. Social–cognitive beliefs, alcohol, and tobacco use: a prospective community study of change following a ban on smoking in public places. Health Psychol. 2009;28(6):753–761. 10.1037/a0016943. [DOI] [PubMed] [Google Scholar]
- 70.Brown A, Moodie C, Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine Tob Res. 2009;11(8):924–932. 10.1093/ntr/ntp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Khademi A, Zhang D, Giabbanelli PJ, Timmons S, Luo C, Shi L. An agent-based model of healthy eating with applications to hypertension In: Giabbanelli PJ, Mago VK, Papageorgiou EI, eds. Advanced Data Analytics in Health. Cham, Switzerland: Springer International Publishing; 2018:43–58. 10.1007/978-3-319-77911-9_3. [DOI] [Google Scholar]
- 72.Cawley J, Frisvold D, Hill A, Jones D. The Impact of the Philadelphia Beverage Tax on Prices and Product Availability. National Bureau of Economic Research. www.nber.org/papers/w24990. Published September 2018. Accessed January 5, 2019. [Google Scholar]
- 73.Batis C, Rivera JA, Popkin BM, Taillie LS. First-year evaluation of Mexico’s tax on nonessential energy-dense foods: an observational study. PLoS Med. 2016;13(7):e1002057 10.1371/journal.pmed.1002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bíró A Did the junk food tax make the Hungarians eat healthier? Food Policy. 2015;54:107–115. 10.1016/j.foodpol.2015.05.003. [DOI] [Google Scholar]
- 75.Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7(1):121–134. 10.3945/an.115.009258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obes Rev. 2013;14(2):110–128. 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.