Abstract
Background
Endophthalmitis, or inflammation of the internal tissues of the eye, may follow trauma and results in loss of vision if not treated promptly. Vitrectomy is used to debride the inflamed vitreous. This retrospective study aimed to compare the outcome from conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV) performed for endophthalmitis within five days and 10 days after open ocular trauma.
Material/Methods
The clinical data from 18 patients (18 eyes) with endophthalmitis caused by open ocular trauma were analyzed at a single center. CV or EAV was performed based on the degree of vision and the involvement of the vitreous cavity.
Results
Of the 18 patients with endophthalmitis, seven patients underwent EAV, and 11 patients underwent CV. The number of cases with preoperative corneal laceration, edema, bleeding, and formation of corneal nebular opacity was higher in the EAV group compared to the CV group. Four patients had retinal detachment, of which three patients were treated with EAV. Seventeen patients had their sight restored by a single vitrectomy procedure. In 10 cases, the culture of the vitreous fluid was positive for infection, and eight patients had Gram-positive Staphylococcus epidermidis infection. Follow-up showed that vitrectomy performed within five days (P=0.001) and 10 days (P=0.047) of open ocular trauma resulted in significant improvement of visual acuity.
Conclusions
Vitrectomy for endophthalmitis due to open ocular trauma performed within five days of injury restored visual acuity. EAV was shown to be an effective alternative to CV.
MeSH Keywords: Endophthalmitis, Endoscopes, Eye Injuries, Vitrectomy
Background
Endophthalmitis, or inflammation of the internal tissues of the eye, may follow trauma and results in loss of vision if not treated promptly. Open ocular trauma is associated with infection of the anterior and posterior segments of the eye when destruction of the ocular tissue destroys the anatomical barrier that prevents infection. Intraocular infection due to pathogenic microorganisms is the cause of 20–30% of cases of endophthalmitis [1] and occurs in 2–7% of all cases of open ocular trauma [2–4]. Delayed or inappropriate treatment of endophthalmitis can result in serious damage to visual function and may result in ocular atrophy. In posttraumatic endophthalmitis following open-globe injury, the risk factors for the development of endophthalmitis include laceration and delayed vitrectomy [5]. However, independent factors that protect against the development of endophthalmitis include early primary repair (healing), self-sealing ocular wounds, and intraocular tissue prolapse [5]. Risk factors for poor outcome in terms of vision for open traumatic endophthalmitis include globe rupture, retinal detachment, injury to zone 2 (<5 mm posterior to the limbus) or zone 3 (>5 mm posterior to the limbus), severe intraocular hemorrhage, and retinal, vitreal, or uveal prolapse [7–9].
Open ocular trauma is the most common cause of endophthalmitis, mainly affects men, and most cases result from work-related injury [7,10]. The development of posttraumatic endophthalmitis is an important turning point in visual prognosis. Previous studies have focused on methods to prevent the occurrence of postoperative endophthalmitis and have explored factors associated with prognosis [7–11]. Vitrectomy, which used to debride the inflamed vitreous, is currently considered to be an effective method to treat endophthalmitis, but the choice of approach remains controversial [12–14].
Therefore, this retrospective study aimed to compare the outcome in terms of improvement in vision from conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV) performed for endophthalmitis within five days and 10 days after open ocular trauma.
Material and Methods
Patients and study inclusion criteria
A retrospective study included 18 patients (18 eyes) who underwent ophthalmic surgery for traumatic endophthalmitis at the Lixiang Eye Hospital of Soochow University from April 2014 to December 2018. This study was conducted in accordance with the principles of the Declaration of Helsinki and followed the guidelines approved by the Ethics Committee of the Hospital Institutional Review Board (IRB). The study inclusion criteria were patients with a diagnosis of endophthalmitis caused by open ocular wounds that included signs of infection on ocular examination, who had bacterial or fungal growth in the vitreous or aqueous humor. The exclusion criteria were preexisting retinal disease, a history of other ocular injuries, severe systemic disease, and other infectious diseases.
The study included 14 men (14 eyes) and four women (four eyes), with an average age of 41.0±17.4 years (range, 3–81 years). Of the 18 eyes evaluated, 13 had penetrating injuries, and five had rupture of the globe. Of the 13 eyes with penetrating injuries, eight had corneal injuries, one had a scleral injury, and four had corneoscleral injuries. All patients were routinely examined using slit-lamp microscopy, orbital computed tomography (CT), or magnetic resonance imaging (MRI), and were assessed for best-corrected visual acuity (BCVA). Fundal examination was performed if the refractive stroma was clear. A-mode or B-mode ultrasound was used to examine some cases of open wounds with no tissue incarceration and good closure following suture and/or visual electrophysiology.
Assessment of visual acuity
On admission, the visual acuity of the affected eye ranged from no light perception (NLP) to counting fingers (CF) perception at 30 cm. Among the 18 cases, two cases (11.1%) had NLP, nine cases (50.0%) had light perception (LP), six cases (38.9%) could perceive hand movements (HM), and one case (5.6%) perceived CF. The intraocular pressure (IOP) ranged from 4–18 mmHg (1 mmHg=0.133 kPa) in the 18 eyes and five eyes had a pressure ≤9 mmHg.
Criteria for the diagnosis of traumatic endophthalmitis
The clinical diagnosis of traumatic endophthalmitis was based on clinical history, the patients’ symptoms, and imaging findings. The study participants had a history of open ocular trauma, including penetrating injury, rupture of the globe, and the presence of intraocular foreign bodies (IOFBs). Typical clinical symptoms and signs included an acute loss of visual acuity, ocular pain, inflammatory cells or exudates in the anterior chamber, or an inflammatory opacity in the vitreous cavity. A-mode and B-mode ultrasound examination showed a continuous low reflection wave, diffuse distribution of a granular bright spot in the vitreous cavity, diffuse thickening of the retina and choroid, and the presence of an exudative or tractional retinal detachment. CT and MRI were used to detect IOFBs, and a visual electrophysiological examination was undertaken using electroretinography (ERG).
Surgical procedures
A licensed physician performed all surgical procedures. All patients were treated with intravenous antibiotics, with the most frequent combination being vancomycin and ceftazidime. Preoperatively, under sterile conditions, 0.2 ml of aqueous humor or vitreous was removed with a disposable syringe, or about 3 ml of vitreous humor was taken before perfusion for vitrectomy. A smear of the extracted sample was used for bacterial and fungal culture and antimicrobial drug susceptibility testing.
Intravitreal injection of antimicrobial agents
Under topical anesthesia, 0.1 ml vancomycin (1 mg/ml), or 0.08 ml of dexamethasone combined with 0.1 ml ceftazidime (2.25 mg/0.1 ml) were administered as an intravitreal injection. In cases of fungal infection, voriconazole (100 μg/0.1ml) was administered as an intravitreal injection.
Conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV)
The patients underwent either CV or EAV. When the cornea was not clear enough to visualize the intraocular structures under the surgical microscope, EAV was performed. In patients who underwent CV, the corneal epithelium was removed, or the cornea was dehydrated when necessary. In most cases, surgery was performed under general anesthesia. However, in select cases, anesthesia was monitored depending on the patients’ condition and the degree of ocular injury. During vitrectomy, vancomycin 5 mg (10 mg/ml) and dexamethasone 10 mg (2 ml) were added to every 500 ml of perfusate. The vitreous was removed as much as possible during the operation.
A standard three-channel surgical incision was used in the EAV group. EAV was performed using an Endo Optiks endoscope (Endo Optiks, Little Silver, NJ, USA) combined with a 25-g trochar and cannula system (Alcon Labs, Fort Worth, TX, USA), using the corneal limbal channel (corneal laceration or corneal limbus), when necessary. The perfusion head was placed under the inferior region, and the surgical method used was similar to that described by De Smetet al. [15]. During EAV surgery, the posterior vitreous detachment was from the edge of the optic disc in each case. The exudate membrane in front and behind the iris, the vitreous at the base, and cyclitic membrane at the back of the eye, were removed as completely as possible, sometimes using endoscopy. Patients with opacity or rupture of the damaged lens underwent lensectomy.
Postoperative antimicrobial treatment
After surgery, all patients were given intravenous antibiotics or antifungal drugs, which were adjusted depending on the culture and drug sensitivity results. Topical antimicrobial eye drops were given, which were stopped once the inflammation resolved.
Patient follow-up
The patients underwent follow-up for 12.52±5.3 months (range, 6–20 months). During the follow-up, the BCVA, cornea, anterior chamber, lens, vitreous body, and retina were all evaluated. The follow-up period after silicone oil removal was 6.3±1.2 months (range, 5–8 months) in cases of silicone oil retinal tamponade. The final BCVA values were recorded following the extraction of silicone oil at final follow-up. Also, some patients underwent B-mode ultrasound and optical coherence tomography (OCT) examination.
Data analysis
Data were analyzed using SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA). Continuous data were presented as the mean±standard deviation (SD), and categorical variables were described as the frequency (%). Data on the classification grades were analyzed using the Mann–Whitney U-test, and the changes in preoperative and postoperative visual acuity were compared using the paired t-test. The relationship between the presence of an IOFB, vitrectomy, and the visual acuity results evaluated using an independent sample t-test. A P-value of <0.05 was considered to be statistically significant. All Snellen or best-corrected visual acuity (BCVA) values were converted to the logarithm of the minimum angle of resolution (LogMAR) for statistical analysis. If the visual acuity was <20/800, the LogMAR value was as follows: counting fingers (CF)=2.3, hand motion (HM)=2.6, light perception (LP)=2.9, and no light perception (NLP)=3.2.
Results
The preoperative condition of the cornea
As shown in Table 1, patients in the endoscope-assisted vitrectomy (EAV) group included an increased number of cases with corneal laceration, edema, blood staining, and corneal nebular opacity compared with the conventional vitrectomy (CV) group.
Table 1.
Causes of preoperative corneal opacity in 18 patients (18 eyes) who underwent conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV) for endophthalmitis due to open ocular trauma.
| Corneal laceration | Corneal edema | Corneal blood staining | Corneal nebular opacity | |
|---|---|---|---|---|
| CV (11 eyes) | 6 (54.5%) | 1 (9.1%) | 0 (0.0%) | 0 (0.0%) |
| EAV (7 eyes) | 5 (71.4%) | 5 (71.4%) | 1 (14.2%) | 1 (14.2%) |
CV – conventional vitrectomy; EAV – endoscope-assisted vitrectomy.
Surgical outcome
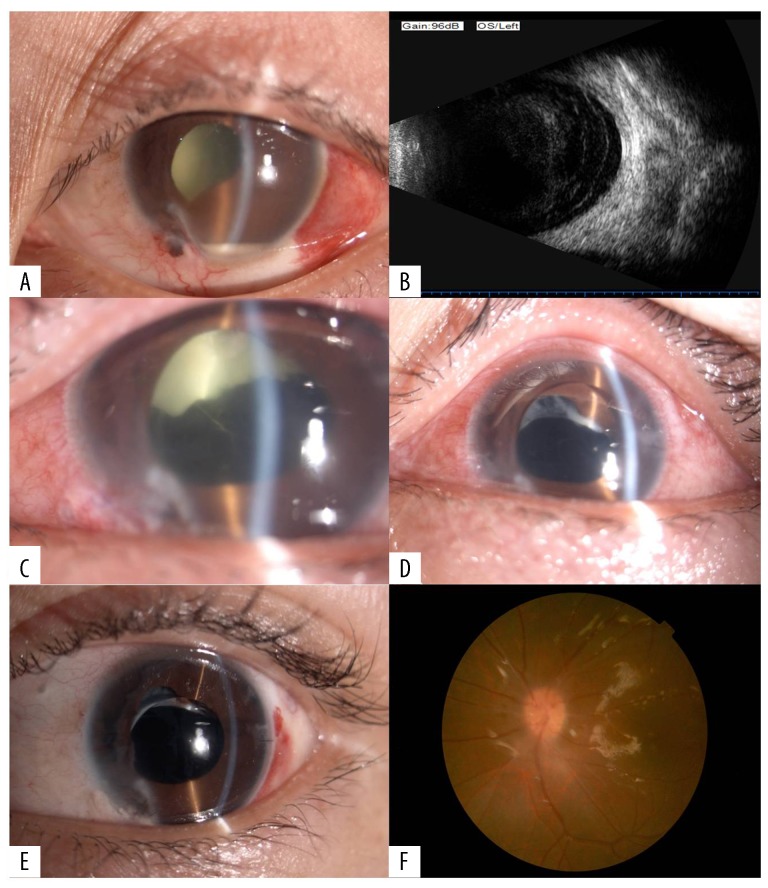
Among the 18 eyes of the 18 patients studied, 12 were treated with vitrectomy after intravitreal injection. However, in one case (Case 14), which had a Gram-negative infection, an intravitreal injection was given four times after vitrectomy. Images of the eye in Case 14 are shown in Figure 1. Seven patients (38.9%) underwent EAV, and the remaining 11 (61.1%) underwent CV. Four patients had retinal detachment, and three of them underwent EAV. Eleven eyes were injected with silicone oil after vitrectomy, and four were injected with a long-acting inert gas. The patient characteristics are summarized in Table 2.
Figure 1.
The left eye of Case 14 who had a penetrating corneal injury and Pseudomonas aeruginosa infection, before and after endoscope-assisted vitrectomy (EAV). (A) The day of admission (10/11/2016). The eye shows an irregular pupil, empyema of the anterior chamber, corneal laceration, iris incarceration, and traumatic cataract. (B) The day of admission (10/11/2016). Flocculent turbidity can be seen in the vitreous cavity. (C) Postoperative day 5 (10/14/2016). Following endoscope-assisted vitrectomy (EAV), there is lens comminution, laser photocoagulation, gas-liquid exchange, oil injection, pupillary formation, the presence of a corneal scleral debridement suture, and intravitreal injection (0.1 ml/2 mg ceftazidime and 0.08 ml dexamethasone). (D) Postoperative day 11 (10/20/2016). A small number of white flakes are visible and associated with the pupil, and the vitreous cavity is filled with silicone oil. (E) Outpatient follow-up (12/09/2016). The eye at the time of outpatient review. The upper capsule appears white, with no sign of inflammation. (F) Outpatient follow-up (12/09/2016). The eye at the time of outpatient review. There is a clear retina, with no sign of inflammation.
Table 2.
Characteristics of 18 patients who underwent conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV) for endophthalmitis due to open ocular trauma.
| No | Gender | Age yrs | Eye | Characteristics of IOFB | Surgical procedure | Culture results | Preoperative BCVA | Final BCVA | Preoperative IOP (mmHg) | Final IOP (mmHg) | Intraocular retinal amponade | Retinaldetachment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 31 | OS | – | CV | Staph. epidermidis | LP | FC/ 30 cm | 17 | 17 | SO | − |
| 2 | M | 55 | OS | – | EAV | – | NLP | FC/ 10 cm | 12 | 12 | SO | + |
| 3 | M | 22 | OS | – | CV | Staph. epidermidis | LP | FC/ 40 cm | 14 | 17 | SO | − |
| 4 | M | 23 | OS | Metal | CV | – | HM/ 10 cm | 20/500 | 16 | 15 | SO | − |
| 5 | M | 47 | OS | Metal | EAV | Staph. epidermidis | LP | 20/333 | 15 | 10 | SO | − |
| 6 | F | 30 | OD | – | EAV | – | HM/ 20 cm | HM/ 50 cm | 5 | 14 | SO | + |
| 7 | F | 39 | OS | Metal | CV | – | HM/30 cm | 20/1000 | 18 | 24 | SO | − |
| 8 | M | 53 | OS | Non-metal | CV | – | NLP | NLP | 4 | 10 | SO | + |
| 9 | M | 41 | OS | Non-metal | CV | Staph. epidermidis | HM/ 30 cm | 20/100 | 12 | 18 | C3F8 | − |
| 10 | M | 58 | OD | Metal | CV | – | LP | FC/ 10 cm | 5 | 10 | SF6 | − |
| 11 | M | 51 | OS | – | CV | – | HM/ 50 cm | FC/ 50 cm | 13 | 13 | SO | |
| 12 | M | 47 | OD | Non-metal | EAV | – | LP | FC/ 30 cm | 12 | 15 | C2F6 | |
| 13 | M | 3 | OD | – | EAV | Alternaria | LP | HM/ 10 cm | 8 | 12 | SO | + |
| 14 | M | 23 | OS | – | EAV | Pseudomonas aeruginosa | LP | 20/333 | 11 | 10 | BSS | − |
| 15 | M | 46 | OS | – | CV | Staph. epidermidis | FC/ 30 cm | 20/160 | 15 | 15 | SO | − |
| 16 | F | 49 | OD | – | CV | Staph. epidermidis | LP | FC/ 10 cm | 14 | 19 | SO | − |
| 17 | M | 39 | OS | – | CV | Staph. epidermidis | LP | FC/ 20 cm | 6 | 14 | SF6 | − |
| 18 | F | 81 | OS | – | EAV | Staph. epidermidis | HM/ 10 cm | FC/ 5 cm | 17 | 14 | BSS | − |
BSS – balanced salt solution; F – female; IOFB – intraocular foreign body; IOP – intraocular pressure; M – male; OD – right eye; OS – left eye; SO – silicon oil; Y – year; LP – light perception; NLP – no light perception; HM – hand motion; CF – counting fingers; BVCA – best-corrected visual acuity.
Successful treatment of endophthalmitis
Endophthalmitis was effectively treated with one vitrectomy in 17/18 cases (94.4%). However, one case of proliferative vitreoretinopathy (Case 4) required a second vitrectomy to control the inflammation. The control of endophthalmitis was determined based on the gradual disappearance of the inflammatory reaction in the eye, the appearance of a clear retina, no reappearance of pus or turbidity in the vitreous body, and the absence of inflammation in the anterior chamber.
Best-corrected visual acuity (BCVA) and intraocular pressure (IOP)
Following vitrectomy, the number of no light perception (NLP) eyes decreased from 2 to 1, including Case 2 who had undergone EAV, and the number of counting fingers (CF) eyes significantly increased. A significant number of eyes showed improved BCVA following vitrectomy (Z=−4.307, P<0.001). There was a significant improvement in visual acuity when vitrectomy was performed within 10 days of ocular trauma (p=0.047), and when performed within five days of ocular trauma (p=0.001). Five cases that had reduced IOP before vitrectomy had a normal IOP after surgery. Table 3 summarizes the BCVA results before and after vitrectomy. The relationships between the time that vitrectomy was performed, and visual acuity at follow-up are shown in Table 4.
Table 3.
The number of eyes and the changes in best-corrected visual acuity (BCVA) before and after surgery.
| VA (LogMAR) | Preoperative | Last follow-up |
|---|---|---|
| NLP (3.2) | 2 | 1 |
| LP (2.9) | 9 | 0 |
| HM (2.6) | 6 | 2 |
| CF (2.3) | 1 | 9 |
| >CF (0.7–1.7) | 0 | 6 |
VA – visual acuity; LP – light perception; NLP – no light perception; HM – hand motion; CF – counting fingers; LogMAR – logarithm of the minimum angle of resolution. Z=−4.307; P=0.000.
Table 4.
Relationship between the time of vitrectomy and visual acuity.
| Time of vitrectomy after trauma | Number of patients | Preoperative BCVA | Final BCVA | P-value |
|---|---|---|---|---|
| Within 5 days | 10 | 2.72±0.21 | 1.87±0.68 | 0.001 |
| Between 5 and 10 days | 5 | 2.78±0.16 | 1.86±0.60 | 0.047 |
| After 10 days | 3 | 3.10±0.17 | 2.70±0.46 | 0.270 |
BCVA – best-corrected visual acuity.
Microbial infection in endophthalmitis
Vitreous culture was positive in 10 patients (55.6%), with most infections caused by Gram-positive cocci. Eight of the 10 cases had Gram-positive Staphylococcus epidermidis infection (80.0%), one patient had a Gram-negative bacterial infection (10.0%), and one patient had a fungal infection (10.0%).
Intraocular foreign bodies (IOFBs)
Of the 18 patients, 7 (38.9%) had IOFBs, which were non-metallic in three cases and metallic in the remaining four cases. There was no significant association between IOFBs, vitrectomy, and visual acuity (Table 5).
Table 5.
Relationship between intraocular foreign bodies (IOFBs), vitrectomy, and visual acuity.
| Number of patients | Preoperative BCVA | BCVA at last follow-up | t-value | P-value | |
|---|---|---|---|---|---|
| IOFB | |||||
| Yes | 7 | 2.81±0.23 | 1.97±0.68 | – | – |
| No | 11 | 2.79±0.24 | 2.12±0.55 | 0.722 | 0.481 |
| CV | 11 | 2.76±0.25 | 1.96±0.74 | – | – |
| EAV | 7 | 2.86±0.21 | 2.07±0.61 | 0.300 | 0.768 |
IOFB – intraocular foreign body; CV – conventional vitrectomy; EAV – endoscope-assisted vitrectomy; BCVA – best-corrected visual acuity.
Discussion
The aim of this retrospective study was to compare the outcome from conventional vitrectomy (CV) and endoscope-assisted vitrectomy (EAV) for endophthalmitis performed after open ocular trauma. Open ocular trauma is defined as a full corneal or scleral thickness injury with or without the presence of an intraocular foreign body (IOFB), including self-sealing defects. The subtypes of ocular trauma were previously classified according to the Ocular Trauma Classification Group (OTCG) categories [16]. Ocular trauma can be classified by zone: zone 1 includes involvement of the cornea, including corneoscleral limbus; zone 2 includes any involvement of corneoscleral limbus to a point 5 mm posterior to the sclera; and zone 3 includes any involvement of the globe posterior to zone 2. In the present study, none cases had a zone 1 injury, six cases had a zone 2 injury, and three cases had a zone 3 injury. Most of the intraocular foreign bodies that were present in five cases were in the posterior segment. Zone 2 or 3 ocular injury has been reported to be a clinical factor associated with poor final visual outcome [7,17]. Also, an acceptable visual effect can be obtained after the removal of a posterior IOFB by vitrectomy [18,19]. These findings indicate the importance of ocular protection and timely vitrectomy.
In cases with open ocular trauma, pathogenic bacteria enter into the eye through the ruptured eyeball. The majority of infections are due to Gram-positive staphylococcal organisms, which is consistent with the findings in the present study [20–22]. Previous studies have shown that isolates of Staphylococcus epidermidis from patients with endophthalmitis were sensitive to vancomycin, but patient outcome in terms of visual acuity did not depend on antibiotic sensitivity [23,24]. The vitreous humor is a natural culture medium for the growth of microbial pathogens, which multiply and rapidly damage the structures in the eye. If infection is not treated in a timely manner, the results can include loss of vision and atrophy of the eye. Worldwide, standard practice is to restore the structural integrity of the eye as early as possible. Vitrectomy can take days or even weeks to be completed because experienced vitreoretinal trauma surgeons may not be available in all hospitals. This preliminary retrospective study included 18 patients and focused on the relationship between vitrectomy and the restoration of visual acuity, to present the real-world experience from a specialized vitreoretinal trauma surgery unit.
In this study, patient follow-up showed a significant improvement in the overall visual acuity with adequate control of infection and inflammation. These findings highlight that early repair of open eye trauma is critical and any significant delay might harm the outcome in terms of vision [25,26]. In cases of severe ocular trauma previously studied by Sabti et al. [27], there was a significant improvement in vision when vitrectomy was performed within three days. However, currently, there are no reported long-term follow-up studies in patients treated with vitrectomy for open ocular trauma.
This study analyzed patient follow-up outcome when vitrectomy was performed within 10 days of ocular injury and showed that surgery performed within five days of injury resulted in significantly greater visual acuity, compared with the preoperative values. This improvement showed no significant change when vitrectomy was performed between 5–10 days of the injury. These findings highlight the significance of the timing of vitrectomy in cases of open ocular traumatic endophthalmitis. However, some patients can suffer from laceration, severe edema, and blood staining of the cornea, which exclude them from vitrectomy under direct vision. These patients have to wait until their corneal opacity clears, or they may require a temporary keratoprosthesis combined with corneal heterografting with a traditional pars plana vitrectomy after identifying the intraocular structures. In these cases, the optimal time or window for surgery is lost, which may lead to serious consequences that include loss of vision or loss of the eye. When EAV is performed promptly, together with intravitreal antimicrobial treatment, improves the chances for the patient of restoring visual acuity following treatment of traumatic endophthalmitis [15,28,29].
In cases of endophthalmitis, the most important aspect of EAV is the early and complete removal of the vitreous humor and the cyclitic membrane that forms on the back of the lens due to inflammation, especially when there is infection of the pars plana near the junction of the sclera and iris [29–31]. Removal of the vitreous humor and the cyclitic membrane helps to reduce the effects of residual bacteria and bacterial toxin residues. In this study, three of the four patients with severe ocular trauma and retinal detachment underwent EAV. One patient who had a preoperative assessment of no light perception (NLP) also underwent EAV, which led to a postoperative visual acuity of counting fingers (CF) at 10 cm. The proportion of patients with corneal damage, including laceration, edema, blood staining, and opacity that affected surgical refraction was greater in the EAV group compared to the CV group. The presence of IOFBs and the choice of two vitrectomy procedures were not directly related to visual acuity, which might have been because IOFBs did not affect the macula in patients in this study. Previously published studies have shown that the size and location of the IOFBs were important predictive factors for visual prognosis [32–34], but there were no significant association between the time before removal of IOFBs and poor visual outcomes [34,35]. Immediate removal of the IOFBs has been reported to reduce the risk of endophthalmitis [36]. In the present study, 61.1% of the patients required silicone oil injection into the vitreous cavity after vitrectomy. We chose to use silicone oil retinal tamponade for cases of retinal detachment, severe proliferative vitreoretinopathy, suspicious vitreous residues without complete resection, and ocular atrophy. Previous studies have shown that filling the vitreous cavity with silicone oil restored the detached retina and also controlled endophthalmitis, as silicone oil has antimicrobial effects as a nutrient-depleted medium that prevents the growth of pathogenic bacteria [37–39].
This study had several limitations, including the small number of patients. Also, the study was conducted at a single center. The patients had different eye conditions following trauma that may have affected the outcome. Some factors that may affect visual acuity were not evaluated in this study, including previous ocular damage, the virulence of the microbial pathogens and their sensitivity to antimicrobial agents. The findings from this preliminary retrospective study support the need for future prospective clinical studies to compare outcome from the timely use of vitrectomy for endophthalmitis resulting from open ocular trauma.
Conclusions
This retrospective study included 18 patients who underwent either conventional vitrectomy (CV) or endoscope-assisted vitrectomy (EAV) for endophthalmitis after the diagnosis of open ocular trauma. The findings showed that vitrectomy performed within five days of ocular injury improved patient prognosis in terms of visual acuity. The findings support the use of intravitreal injection of antibiotics after vitrectomy to prevent infection. EAV was shown to be an effective alternative to CV and also resulted in improved outcome for the prevention of corneal opacity and its associated refraction defects.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Schrader WF. Epidemiology of open globe eye injuries: analysis of 1026 cases in 18 years. Klin Monbl Augenheilkd. 2004;221:629–35. doi: 10.1055/s-2004-813254. [DOI] [PubMed] [Google Scholar]
- 2.Kong GY, Henderson RH, Sandhu SS, et al. Wound-related complications and clinical outcomes following open globe injury repair. Clin Exp Ophthalmol. 2015;43:508–13. doi: 10.1111/ceo.12511. [DOI] [PubMed] [Google Scholar]
- 3.Faghihi H, Hajizadeh F, Esfahani MR, et al. Posttraumatic endophthalmitis: Report No. 2. Retina. 2012;32:146–51. doi: 10.1097/IAE.0b013e3182180087. [DOI] [PubMed] [Google Scholar]
- 4.Dehghani AR, Rezaei L, Salam H, et al. Posttraumatic endophthalmitis: Incidence and risk factors. Glob J Health Sci. 2014;6:68–72. doi: 10.5539/gjhs.v6n6p68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Zhang MN, Jiang CH, et al. Endophthalmitis following open globe injury. Br J Ophthalmol. 2010;94:111–14. doi: 10.1136/bjo.2009.164913. [DOI] [PubMed] [Google Scholar]
- 6.Essex RW, Yi Q, Charles PG, Allen PJ. Post-traumatic endophthalmitis. Ophthalmology. 2004;111:2015–22. doi: 10.1016/j.ophtha.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 7.Kong GY, Henderson RH, Sandhu SS, et al. Wound-related complications and clinical outcomes following open globe injury repair. Clin Exp Ophthalmol. 2015;43:508–13. doi: 10.1111/ceo.12511. [DOI] [PubMed] [Google Scholar]
- 8.Feng K, Hu YT, Ma Z. Prognostic indicators for no light perception after injury: Eye injury vitrectomy study. Am J Ophthalmol. 2011;152:654–62.e2. doi: 10.1016/j.ajo.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Feng K, Wang CG, Hu YT, et al. Clinical features and prognosis of eyeball ruptureEye injury vitrectomy study. Clin Exp Ophthalmol. 2015;43:629–36. doi: 10.1111/ceo.12534. [DOI] [PubMed] [Google Scholar]
- 10.Yang XB, Liu YY, Huang ZX, et al. Clinical analysis of 1593 patients with infectious endophthalmitis: A 12-year study at a tertiary referral center in western China. Chin Med J (Engl) 2018;131:1658–65. doi: 10.4103/0366-6999.235866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang CS, Lu CK, Lee FL, et al. Treatment and outcome of traumatic endophthalmitis in open globe injury with retained intraocular foreign body. Ophthalmologica. 2010;224:79–85. doi: 10.1159/000235725. [DOI] [PubMed] [Google Scholar]
- 12.Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19:227–34. doi: 10.1111/1469-0691.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ye JJ, Guo LB, Wang SR, et al. [Vitreal surgery and etiological diagnosis of bacterial endophthalmitis]. Zhonghua Yan Ke Za Zhi. 2012;48:995–1000. [in Chinese] [PubMed] [Google Scholar]
- 14.Aggarwal P, Garg P, Sidhu HK, et al. Post-traumatic endophthalmitis with retained intraocular foreign body – a case report with review of literature. Nepal J Ophthalmol. 2012;4:187–90. doi: 10.3126/nepjoph.v4i1.5875. [DOI] [PubMed] [Google Scholar]
- 15.De Smet MD, Carlborg EA. Managing severe endophthalmitis with use of an endoscope. Retina. 2005;25:976–80. doi: 10.1097/00006982-200512000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Kuhn F, Morris R, Whitherspoon CD, et al. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234:399–403. doi: 10.1007/BF00190717. [DOI] [PubMed] [Google Scholar]
- 17.Jin W, Xu Y, Wang W, et al. Open-globe injuries with posterior segment IOFBs have a guarded visual prognosis, particularly when associated with RD. Increased awareness of the importance of eye protection can help minimize the occurrence of these injuries. Curr Eye Res. 2017;42:1143–48. [Google Scholar]
- 18.Maneschg OA, Resch M, Papp A, Németh J. Prognostic factors and visual outcome for open globe injuries with intraocular foreign bodies. Klin Monbl Augenheilkd. 2011;228:801–7. doi: 10.1055/s-0029-1245756. [DOI] [PubMed] [Google Scholar]
- 19.Mukkamala LK, Soni N, Zarbin MA, et al. Posterior segment intraocular foreign bodies: A 10-year review. Ophthalmol Retina. 2017;1:272–77. doi: 10.1016/j.oret.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Alfaro DV, Roth D, Liggett PE. Posttraumatic endophthalmitis. Causative organisms, treatment, and prevention. Retina. 1994;14:206–11. [PubMed] [Google Scholar]
- 21.Banker TP, McClellan AJ, Wilson BD, et al. Culture-Positive endophthalmitis after open globe injuries with and without retained intraocular foreign bodies. Ophthalmic Surg Lasers Imaging Retina. 2017;48(8):632–37. doi: 10.3928/23258160-20170802-05. [DOI] [PubMed] [Google Scholar]
- 22.Li X, Zarbin MA, Langer PD, Bhagat N. Posttraumatic endophthalmitis: An18-Year Case Series. Retina. 2018;38:60–71. doi: 10.1097/IAE.0000000000001511. [DOI] [PubMed] [Google Scholar]
- 23.Yannuzzi NA, Patel NA, Relhan N, et al. Clinical features, antibiotic susceptibilities, and treatment outcomes of endophthalmitis caused by Staphylococcus epidermidis. Ophthalmol Retina. 2018;2:396–400. doi: 10.1016/j.oret.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 24.Miller DM, Vedula AS, Flynn HW, Jr, et al. Endophthalmitis caused by Staphylococcus epidermidis: In vitro antibiotic susceptibilities and clinical outcomes. Ophthalmic Surg Lasers Imaging. 2007;38(6):446–51. doi: 10.3928/15428877-20071101-01. [DOI] [PubMed] [Google Scholar]
- 25.Blanch RJ, Bishop J, Javidi H, Murray PI. Effect of time to primary repair on final visual outcome after open globe injury. Br J Ophthalmol. 2019 doi: 10.1136/bjophthalmol-2017-311559. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Agrawal R. Prognostic factors for final vision outcome in patients with open globe injuries. Indian J Ophthalmol. 2011;59:259–60. doi: 10.4103/0301-4738.81030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sabti KA, Raizada S. Endoscope-assisted pars plana vitrectomy in severe ocular trauma. Br J Ophthalmol. 2012;96:1399–403. doi: 10.1136/bjophthalmol-2012-302187. [DOI] [PubMed] [Google Scholar]
- 28.Ren H, Jiang R, Xu G, et al. Endoscopy-assisted vitrectomy for treatment of severe endophthalmitis with retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2013;251(7):1797–800. doi: 10.1007/s00417-013-2297-4. [DOI] [PubMed] [Google Scholar]
- 29.Yang X, Li QY, Pang XQ, et al. [Endoscopically guided thorough vitrectomy for management of exogenous endophthaImitis with cloudy cornea]. Chin J Ocul Fundus Dis. 2008;24:202–5. [article in Chinese] [Google Scholar]
- 30.Sabti KA, Raizada S. Endoscope-assisted pars plana vitrectomy in severe ocular trauma. Br J Ophthalmol. 2012;96:1399–403. doi: 10.1136/bjophthalmol-2012-302187. [DOI] [PubMed] [Google Scholar]
- 31.Marra KV, Yonekawa Y, Papakostas TD, Arroyo JG. Indications and techniques of endoscope assisted vitrectomy. J Ophthalmic Vis Res. 2013;8:282–90. [PMC free article] [PubMed] [Google Scholar]
- 32.Liu CC, Tong JM, Li PS, Li KK. Epidemiology and clinical outcome of intraocular foreign bodies in Hong Kong: A 13-year review. Int Ophthalmol. 2016;37:55–61. doi: 10.1007/s10792-016-0225-4. [DOI] [PubMed] [Google Scholar]
- 33.Maneschg O, Resch M, Papp A, Németh J. [Prognostic factors and visual outcome for open globe injuries with intraocular foreign bodies]. Klin Monbl Augenheilkd. 2010;228:801–7. doi: 10.1055/s-0029-1245756. [article in German] [DOI] [PubMed] [Google Scholar]
- 34.Liu Y, Wang S, Li Y, et al. Intraocular foreign bodies: Clinical characteristics and prognostic factors influencing visual outcome and globe survival in 373 eyes. J Ophthalmol. 2019;2019 doi: 10.1155/2019/5208092. 5208092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falavarjani K, Fazel A, Hashemi M, et al. Vitrectomy for posterior segment intraocular foreign bodies, visual and anatomical outcomes. Middle East Afr J Ophthalmol. 2013;20:244–47. doi: 10.4103/0974-9233.114803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicoară SD, Irimescu I, Călinici T, Cristian C. Outcome and prognostic factors for traumatic endophthalmitis over a 5-year period. J Ophthalmol. 2014;2014:7. doi: 10.1155/2014/747015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ornek N, Apan T, Oğurel R, Ornek K. Comparison of the antimicrobial effect of heavy silicone oil and conventional silicone oil against endophthalmitis-causing agents. Indian J Ophthalmol. 2014;62:388–91. doi: 10.4103/0301-4738.126994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yan H, Li J. An experimental study on antimicrobial activity of silicone oil in vitro. Ophthalmologica. 2008;222:245–48. doi: 10.1159/000131104. [DOI] [PubMed] [Google Scholar]
- 39.Adams F, Romero IL, Silva CB, Manzano RP. Evaluation of silicon oil on bacterial growth. Arq Bras Oftalmol. 2012;75:89–91. doi: 10.1590/s0004-27492012000200003. [DOI] [PubMed] [Google Scholar]