Abstract
Objectives:
We aimed to investigate the effects of propolis nanoparticles (prpNPs) on antimicrobial property and shear bond strength (SBS) of orthodontic composite bonded to bovine enamel.
Materials and Methods:
Sixty bovine teeth were randomly divided into five groups (n=12). PrpNPs were prepared at concentrations of 0% (control), 1%, 2%, 5%, and 10% in Transbond XT composite to bond stainless steel brackets to the teeth. SBS between brackets and teeth was measured using a universal testing machine. After debonding, the adhesive remnant index (ARI) on bracket bases was measured. In the microbial test, composites with the aforementioned concentrations of prpNPs were cured in metal discs. The bacteria included Streptococcus mutans (S. mutans), Streptococcus sanguinis (S. sanguinis), and Lactobacillus acidophilus (L. acidophilus), and antimicrobial effects of prpNPs were investigated by anti-biofilm, disc agar diffusion and eluted component tests.
Results:
The 10% prpNPs group showed the lowest SBS. Colony growths of S. mutans and S. sanguinis at all concentrations (except for 1%) was significantly lower than the control group. L. acidophilus colony growth was significantly reduced at 5% and 10% concentrations. Growth inhibition zone developed at 2%, 5%, and 10% concentrations for S. mutans and S. sanguinis. The lowest numbers of S. mutans and S. sanguinis colonies at all concentrations were observed on day 15. L. acidophilus colonies decreased significantly at all concentrations (except for 1%) until day 30.
Conclusion:
Nano propolis has a significant antimicrobial effect at 2% and 5% concentrations, and the SBS is maintained within the acceptable clinical range.
Keywords: Propolis Nanoparticles, Orthodontic Composite, Dental Bonding, Microbial Sensitivity Tests, Transbond XT
INTRODUCTION
Orthodontic banding has been replaced by bonding brackets due to more acceptable appearance, ease of use, and better oral hygiene control since the 1980s. Nevertheless, there are still problems like debonding and demineralization around the brackets as a consequence of microbial plaque accumulation [1–3].
In an ideal bonding, bond strength should prevent brackets from being dislodged during treatment, while it should not be so high as to cause tooth damage during debonding [4]. Effective factors on the bond strength of brackets to enamel have been extensively discussed in several studies. They include enamel surface preparation techniques, various adhesive systems, and bracket-related factors such as area and design of the bracket base [5,6]. Recent studies have shown that 50% to 75% of patients, experience demineralization of dental surfaces during fixed orthodontic treatment [7,8]. An increase in Streptococcus mutans (S. mutans) and Lactobacillus count has been reported in the oral cavity after the placement of fixed orthodontic appliances [9]. Fixed orthodontic treatment makes oral hygiene maintenance difficult and increases plaque accumulation around brackets and bands, leading to an increased risk of dental caries and formation of white spot lesions (WSLs) [10–12]. In addition, enamel etching weakens the structure of the enamel by decalcification and increases the risk of decays [13]. WSLs result from bacterial activity. S. mutans has been associated with decay and plays a major role in the onset of decays [14].
Lactobacillus acidophilus (L. acidophilus) is a secondary invasive bacterium associated with advanced carious lesions. Humans with a high level of L. acidophilus count usually experience more advanced carious lesions compared to those with lower levels of this bacterium [15]. Since demineralization is a major concern during orthodontic treatment, precise maintenance of oral hygiene and regular application of fluoride-containing toothpastes and mouthwashes are recommended to prevent carious lesions [16]. The patients’ cooperation is very important in the mentioned methods. Therefore, other less patient-dependent methods of reducing dental caries should be considered. Using an anti-decay composite for bonding could be an effective alternative.
Nano-scale structures, such as nanoparticles, have a high surface-to-volume ratio which extremely increases the reactivity of these materials because the number of atoms or molecules in the sample mass would be very high [17].
Adding nanoparticles to composite resins not only could have specific biological and chemical effects, such as the accumulation of microorganisms, but also might change their physical and mechanical properties [18].
Considering the fact that the main etiologic factor of tooth decay and periodontal disease is the dental plaque, finding natural products with antiplaque and antimicrobial activities can be very beneficial. Propolis (bee glue) is a viscous organic substance obtained from beeswax. The bees use propolis to block their hives’ pores against other insects, to disinfect hives, and to combat climate change. Apart from the geographical origin, all propolises contain flavonoids and phenolic acid and have been shown to have antibacterial, antiviral, and antifungal effects [19–22].
Propolis has broad proven biological effects. Dicaffeoylquinic acid and flavonoids are essential components of propolis and have protective effects in the liver (hepato-protective). Caffeic acid phenethyl ester (CAPE) in propolis is a potent anticancer component. Other effects of propolis include antimicrobial and antioxidant activities [23].
According to an investigation by Koo et al [24], propolis inhibits the growth and adherence of S. mutans and Streptococcus sobrinus (S. sobrinus). The purpose of the present study was to evaluate the effect of propolis nanoparticles (prpNPs) incorporated in an orthodontic adhesive on its antimicrobial properties and shear bond stress (SBS) when bonded to bovine enamel.
MATERIALS AND METHODS
Nano propolis preparation:
Twenty grams of pure propolis bulk was dissolved in 100 ml of ethanol. The solution was stirred at room temperature for seven days, and the product was filtered using filter papers (Whatman, 40 Ashless, Germany) to remove impurities. The filtered solution was added at 1:10 ratio to distilled water to isolate pure propolis particles. The suspension was placed in an ultrasonic bath for 20–30 minutes to obtain prpNPs. Afterwards, nano propolis was acquired in the colloid state. In this colloid, nanoparticles of propolis were observed using a scanning electron microscope (SEM; Zeiss, Oberkochen, Germany) at a magnification of 65,000 (Fig. 1).
Fig. 1.
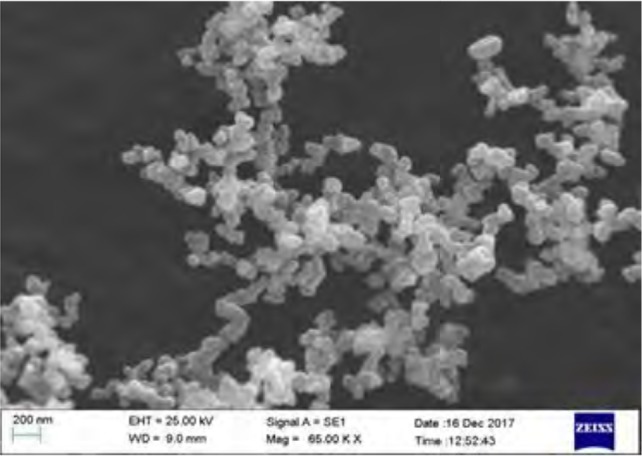
Nano propolis at ×65,000 magnification under scanning electron microscopy
Colloid nano propolis was centrifuged (Unicem M, Herolab GmbH, Stuttgart, Germany) for 20 minutes at 9000 rpm (revolutions per minute). Next, it was filtered using filter paper followed by subjection to freeze-drying (Freeze dryer, Martin Christ GmbH, Osterode am Harz, Germany) for 24 hours at −70°C. After this time, prpNPs were obtained in powder form [25–27].
Bonding the brackets:
Five groups of samples including one control group and four composite groups containing 1%, 2%, 5%, and 10% prpNPs were evaluated in this study. A laboratory scale (U.S. Solid, ND, USA) with a precision of 0.0001 g was used for weighing the composite and nanoparticles. The nanocomposites were stored in a dark environment at room temperature before bonding. Sixty sound bovine incisors without any enamel cracks, decay, erosions or fractures were collected. They were kept at 4°C in a solution of 0.5% Chloramine for four weeks. Afterwards, the samples were randomly divided into five groups (n=12): four groups for bonding with nanocomposites and one group for composite without prpNPs. The teeth were cleaned using a prophylaxis brush, then rinsed and finally dried. The buccal surfaces of the teeth were etched with 37% phosphoric acid gel (Ultra etch; Ultradent Products Inc., South Jordan, UT, USA) for 30 seconds, then washed with water for 30 seconds and dried with air without moisture or oil. A thin layer of bonding primer (3M Unitek, Monrovia, CA, USA) was placed uniformly on the etched surfaces of all teeth and exposed to a light-curing device (Demetron, Kerr, Orange, CA, USA) for 10 seconds.
The same amount of composite was added to the base of standard edgewise 0.18-inch slot stainless steel brackets (American Orthodontics, Sheboygan, WI, USA) with a base area of 12.62 mm2. In the control group, we used Transbond XT composite (3M Unitek, Monrovia, CA, USA) without prpNPs, and in the experimental groups, we used composites containing 1%, 2%, 5%, and 10% prpNPs. The brackets were placed in the middle part of the crown of the teeth in both mesiodistal and incisogingival directions. After aligning the longitudinal axis of the brackets with the longitudinal axis of the dental crowns, the remaining adhesives were removed with a scaler, and finally, each tooth was exposed to 40 seconds of light-curing (10 seconds from each side) for polymerization. All stages were performed by a single operator.
The samples were thermocycled (Vafaei Industrial, Tehran, Iran) to simulate the stresses and physical conditions of the mouth. The teeth were subjected to 24 hours of thermocycling for 1500 cycles. In each cycle, the blocks were placed in 5°C water for 15 seconds, out of water for 10 seconds, and in 55°C water for 15 seconds. After completion of thermocycling, the samples were mounted in metal molds with dimensions of 2.5×2.5×3 cm3. The teeth were fixed to a 16-inch×22-inch rectangular stainless steel wire using elastomeric rings. Each tooth was placed in the middle of the mold. Finally, an auto-polymerizing acrylic resin (Acropars, Tehran, Iran) was prepared as paste and was poured in the molds up to the level of the cementoenamel junction of the teeth (Fig. 2).
Fig. 2.

Acrylic blocks containing teeth prepared for shear bond strength testing
SBS test:
After polymerization, acrylic blocks containing the teeth were removed from the metal molds. The bond strengths were measured using a universal testing machine (Zwick/Roell, Ulm, Germany).
The samples were placed inside the machine so that each bracket base was completely parallel to the vector of the applied force. The metal blade of the machine (with a tip thickness of about 0.6 mm) applied the load in an incisogingival direction at a crosshead speed of 0.5 mm/minute until bracket debonding.
The forces recorded in Newton (N) were determined as the bond force for each sample. Next, they were divided by the base area of the brackets in square millimeters (mm2), and the SBS was determined in Megapascal (MPa). In order to determine the amount of remaining adhesive, debonded bracket bases were examined under a stereomicroscope (SMZ800, Nikon, Japan) at ×10 magnification. Adhesive remnant index (ARI) for each tooth was scored from 0 to 4 based on the following categorization [28]:
0) No adhesive on the bracket base
1) <25% of the adhesive on the bracket base
2) 25–50% of the adhesive on the bracket base
3) 50–75% of the adhesive on the bracket base
4) 75–100% of the adhesive on the bracket base.
Antimicrobial tests:
Two-hundred and twenty-five composite discs were prepared for antimicrobial tests. Each test was repeated three times for each sample.
Composite discs for antimicrobial tests were prepared by placing composites in metal washers with a diameter of 5 mm and a height of 0.65 mm. After that, a thin layer of bonding was applied on the samples, gentle pressure was applied on top of the samples by a thin and flat glass, and the samples were cured with the light-curing device for 40 seconds. The samples were separated from the metal washers by double-sided finger pressure. All samples were fabricated at a temperature of 22–25°C by a single operator. Finally, the samples were sterilized by gamma ray with a minimum dose of 25 kilograys.
Species preparation:
Standard strains of S. mutans (ATCC 35668), S. sanguinis (ATCC 10556) and L. acidophilus (ATCC 314) were purchased from the National Center for Genetic Reserves and were incubated at 37°C for 48 hours.
Determination of biofilm inhibition:
In order to evaluate the biofilm formation of each microorganism on composite discs containing prpNPs, after placing composite discs in wells, a microbial suspension was prepared at a concentration of 1.5×108 colony-forming units (CFU)/ml and added to each well and incubated at 37°C to form a biofilm. After 72 hours, composite discs were rinsed with sterile saline to dislodge the planktonic and loosely attached bacteria. Afterwards, the discs were placed in tubes containing 1 ml of sterile saline under sonication at 50 Hz and 150 W (Bandelin-sonicator, SONOPULS, Germany) for one minute and were vortexed. Microbial CFU/ml in the suspension that was obtained from successive dilution in microtiter plates and subsequent spread-culturing in Trypticase soy agar (TSA) medium was counted by the drop-plate method; thus, CFUs/mm2 of the discs were determined.
Disc agar diffusion (DAD) test:
The antimicrobial activity in composite discs containing prpNPs was measured based on the release of prpNPs from composite discs through the DAD test. In this test, a suspension of 1.5×108 CFU/ml from each bacterium was prepared in Mueller Hinton Broth and was cultured in Mueller Hinton Agar (HiMedia, Mumbai, India). After cultivation, the discs were placed at a distance of 2 cm from each other in the culture medium inoculated with microorganisms, and the plates were incubated at 37°C for 24 hours. The diameters of inhibitory zones were measured by a ruler.
Eluted component test:
The antimicrobial effects of the liquid mediums containing possibly released nanoparticles from composite discs were also studied. Composite discs were placed in microtubes containing one ml of brain heart infusion (BHI) broth. On days 3, 15, and 30, 50 μl from BHI broths were removed from the microtubes and were placed in another tube; 50 μl of bacterial culture was added into each tube (final concentration of 105 CFU/ml in one ml of the medium).
The microtubes were shaken for 24 hours at 37°C at 300 rpm. Next, microbial CFUs/ml in the suspension were serially diluted in microtiter plates and spread-cultured in TSA. The bacterial colonies (CFU/ml) were counted using the drop-plate method.
Statistical analysis:
The data were analyzed by SPSS version 20 (SPSS Inc., Chicago, IL, USA). One-way analysis of variance (ANOVA) was used to compare the five groups. Tamhane test and Tukey’s post-hoc test were used for pairwise comparisons. ARI and DAD test results were analyzed by Kruskal-Wallis test. P<0.05 was considered statistically significant.
RESULTS
Table 1 shows the results of the SBS test. The highest mean SBS belonged to the control group (29.90±7.12 MPa) and the lowest was for the group with 10% concentration (0.79±0.78 MPa). According to the results of one-way ANOVA, a significant difference was found between the SBS of the studied groups (P<0.001). Pairwise comparisons of the groups with Tamhane test showed that SBS in the control group was significantly higher compared to the groups containing prpNPs. In addition, a significant difference was found between all groups (P<0.05), except between 2% and 5% concentrations (P=0.705; Table 2).
Table 1.
Descriptive data of shear bond strength (MPa) in the four studied groups (N=12)
| NP % | Min | Max | Mean | SD |
|---|---|---|---|---|
| 0 | 16.72 | 40.67 | 29.90 | 7.12 |
| 1 | 10.33 | 26.68 | 19.64 | 5.38 |
| 2 | 6.85 | 16.12 | 11.37 | 3.22 |
| 5 | 1.42 | 16.82 | 8.04 | 5.17 |
| 10 | 0.74 | 2.71 | 1.80 | 0.79 |
NP: Nanoparticle; SD: Standard Deviation
Table 2.
Pairwise comparisons of shear bond strength (SBS) of the five groups
| Pairwise comparison | P-value |
|---|---|
| Control-1% | 0.007 |
| Control-2% | <0.001 |
| Control-5% | <0.001 |
| Control-10% | <0.001 |
| 1%–2% | 0.010 |
| 1%–5% | <0.001 |
| 1%–10% | <0.001 |
| 2%–5% | 0.705 |
| 2%–10% | 0.006 |
| 5%–10% | 0.015 |
The amounts of ARI of the studied groups are given in Tables 3 and 4; Kruskal-Wallis test did not show any significant differences between the groups (P=0.166).
Table 3.
Amount of remaining adhesive based on the adhesive remnant index (ARI)
| Nanoparticle percentage (n=12) | ARI | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| 0 | 0 | 3 | 2 | 3 | 4 |
| 1 | 1 | 2 | 4 | 2 | 3 |
| 2 | 0 | 4 | 3 | 3 | 2 |
| 5 | 1 | 4 | 2 | 3 | 2 |
| 10 | 2 | 5 | 3 | 2 | 0 |
Table 4.
Descriptive values of colony count (CFU/mm2) for each bacterial strain (N=3) in the four groups (n=12)
| Nanoparticle % | Bacterial Strain | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| 0 | S. mutans | 180000 | 260000 | 230000 | 43588 |
| S. sanguinis | 260000 | 330000 | 290000 | 36055 | |
| L. acidophilus | 330000 | 400000 | 363333 | 35118 | |
| 1 | S. mutans | 100000 | 120000 | 110000 | 10000 |
| S. sanguinis | 100000 | 150000 | 126666 | 25166 | |
| L. acidophilus | 220000 | 280000 | 243333 | 32145 | |
| 2 | S. mutans | 12000 | 17000 | 15000 | 2645 |
| S. sanguinis | 19000 | 24000 | 21000 | 2645 | |
| L. acidophilus | 290000 | 380000 | 346666 | 49328 | |
| 5 | S. mutans | 1200 | 1600 | 1366 | 208 |
| S. sanguinis | 1700 | 2500 | 2166 | 416 | |
| L. acidophilus | 32000 | 37000 | 34666 | 2516 | |
| 10 | S. mutans | 200 | 400 | 266 | 115 |
| S. sanguinis | 500 | 800 | 666 | 152 | |
| L. acidophilus | 9000 | 13000 | 11000 | 2000 |
SD: Standard Deviation
Biofilm inhibition test:
The mean numbers of colony count for different microorganisms are shown in Table 4. The results of the post-hoc test revealed that the number of colonies (CFU/ml) of S. mutans and S. sanguinis at 2%, 5%, and 10% concentrations was significantly lower compared to conventional composites (P<0.05). In addition, for L. acidophilus, the CFU/ml only decreased significantly at 5% and 10% concentrations (P<0.05).
DAD test:
The results showed that the inhibition zone diameter for S. mutans was 6.46 mm, 7.2 mm, and 8 mm at 2%, 5%, and 10% concentrations, respectively. The inhibition zone diameter for S. sanguinis was 2.5 mm, 5.73 mm, and 7. 23 mm in average at 2%, 5%, and 10% concentrations, respectively. No inhibition zone was observed for discs containing 1% prpNPs for S. mutans and S. sanguinis. Furthermore, no inhibition zone was formed against L. acidophilus at any of the concentrations.
Eluted component test:
Results of Tukey’s HSD (honestly significant difference) test showed that at 1% concentration for all microorganisms, the lowest colony count was observed on the 15th day, which was not significant, while there was a significant increase in colony counts on the 30th day (P<0.001).
The numbers of S. mutans and S. sanguinis colonies decreased significantly (about 85%) on the 15th day at 2% concentration of prpNPs (P<0.05). After that, the number of S. mutans and S. sanguinis colonies increased until the 30th day. Evaluation of discs containing 5% and 10% prpNPs showed that the number of S. mutans and S. sanguinis colonies decreased significantly on the third and 15th days (P<0.05; about 80% and 95% lower than the control group, respectively), while these colonies increased on the 30th day. The number of L. acidophilus colonies decreased significantly until the 30th day at 2%, 5%, and 10% concentrations of prpNPs (P<0.001).
DISCUSSION
It has been well-documented that orthodontic treatment with fixed appliances makes patients more susceptible to the accumulation of bacterial plaque and enamel demineralization [26].
This problem is due to the interference of the appliances with mechanical removal of the plaque, making it difficult to maintain proper oral hygiene [26]. One of the effective methods of preventing enamel demineralization without. dependence on the patients’ cooperation is the use of orthodontic adhesives resistant to bacterial adhesion and biofilm formation by adding various elements to composite resins [27].
Using nanoparticles with antibacterial activity is practical only if the physical and mechanical properties of the composite remain unchanged or in the clinically acceptable range [28]. In this regard, nanoparticles have been suggested to be incorporated in adhesives. The antibacterial activity of several nanoparticles such as Zinc (Zn) [29–31], gold [32], and silver [33–34] has been proven. One of the reasons for choosing propolis in this study is that, despite its antibacterial activity, propolis is a non-toxic and safe substance. Grenho et al [34] studied the non-cytotoxicity of propolis in addition to examining its antibacterial activity. They found that propolis inhibited the growth of bacteria and biofilm formation, while cell culture experiments showed the growth of fibroblasts and high metabolic activity without membrane damage. As a result, propolis is a biocompatible biomaterial that can be used in oral hygiene products [34]. The bond strength of an orthodontic bracket should be sufficient to resist the forces applied during the treatment.
Reynolds and von Fraunhofer [35] showed that bond strengths of 5.9–7.8 MPa are sufficient to resist chewing forces, while Sharma et al [36] reported this value to be 9.7 MPa for Transbond XT composite. The results of the present study showed that increasing the percentage of prpNPs leads to a decrease in SBS in a dose-dependent manner. The SBS in the 1% prpNPs group (average of 19.6 MPa) and the 2% prpNPs group (average of 11.3 MPa) was above the acceptable clinical range, whereas in the 5% prpNPs group (8.03 MPa), it was within the clinically acceptable range. However, the SBS of the 10% prpNPs group was significantly lower compared to the conventional composite and much lower than the acceptable range, which is not recommended for clinical use. The results of the present study are in line with the results reported by Mirhashemi et al [37] who revealed that using chitosan and zinc oxide (ZnO) nanoparticles up to 5% concentration retained the SBS of Transbond XT composite in the clinically acceptable range, while adding the concentration of 10% reduced it to an unacceptable level for clinical use.
Unlike our results, Poosti et al [38] showed that the SBS of composites containing 1% titanium oxide (TiO2) nanoparticles was similar to that of the control group. This difference is mainly due to different nanoparticle types and dissimilar thermocycling methods.
Akhavan et al [33] pointed out the increase in SBS as a result of adding silver/hydroxyapatite nanoparticles to the composite at 1% concentration, while the SBS reduced at concentrations of 5% and 10%. These results are similar to that of the present study in a dose-dependent manner but differ from the results of this study in terms of the SBS at 1% concentration. The main difference of that study is the addition of nanoparticles to primers instead of the paste and the type of teeth used in the research. They also noted that the increased strength in the 1% concentration group was due to the ability of silver/hydroxyapatite nano-particles to improve the adhesion at the interface between the restorative materials and the enamel surface by increasing the mechanical strength of the adhesive layer and reinforcing the supportive structures [33].
The present study evaluated the SBS of orthodontic brackets in a controlled in-vitro condition. However, the forces applied to the brackets in the oral environment are somewhat different. A combination of tensile, shear, and rotary forces are exerted to the brackets in vivo. In addition, there are different types of stresses in the oral environment such as temperature changes, humidity, and bacterial plaques that make generalization of laboratory to clinical conditions difficult [39]. Therefore, the results of in vitro studies should be interpreted more carefully. The results of the biofilm inhibition tests showed that adhesives containing 2% concentration of prpNPs significantly inhibited S. mutans and S. sanguinis biofilm formation. Increasing prpNPs concentration up to 5% and 10%, significantly decreased biofilm formation of all 3 bacterial types.
A study conducted by Mirhashemi et al [37] showed that only the 10% concentration of nano-Zn and nano-chitosan particles had a significant effect on all three microorganisms, while the 5% concentration was not effective on L. acidophilus. These findings were in contrast to those obtained in the present study; however, similar to the current investigation, the 1% concentration could not significantly influence any of the three microorganisms.
Sodagar et al [40] concluded that addition of curcumin nanoparticles at concentrations of 1%, 2%, and 10% to composite reduced the number of colonies of all three bacterial species compared to the control group. The antimicrobial activity caused by ion release from the nanoparticles in the composite resin was measured by the DAD test. The importance of this test is due to the fact that WSLs are usually formed around the bracket base. Therefore, the ideal antimicrobial material in the orthodontic adhesive should be able to diffuse through the surrounding medium. The results of this study showed that concentrations of 2%, 5%, and 10% of prpNPs in composite discs produced a growth inhibition zone against S. mutans and S. sanguinis. This indicates the release of prpNPs to the surrounding medium and the expression of a significant non-contact antimicrobial effect. Similar results were reported by Sodagar et al [28] regarding the inhibition zone formed by TiO2 nanoparticles. In addition, in studies conducted on silver [34] and chitosan/Zn [37], an inhibitory growth zone was observed at concentrations of 5% and 10%, respectively.
Unlike prpNPs, in the study conducted by Aydin Sevinç and Hanley [29], Zn nanoparticles showed low diffusion, and no inhibition zone was formed in the DAD test. Curcumin nanoparticles also did not form any inhibition zone at any of the concentrations of 1%, 5%, and 10% in the study by Sodagar et al [40].
In the eluted component test, the antimicrobial effect of the solutions containing the possibly released nanoparticles from nanocomposite discs is monitored over time, indicating the continuation of antimicrobial activity in the liquid medium.
The results of our study showed that the lowest numbers of colonies of S. mutans and S. sanguinis at all four concentrations were counted on day 15, which was significantly reduced at concentrations of 2%, 5%, and 10%. However, the colony counts of these bacteria increased until day 30. The colony counts of L. acidophilus at concentrations of 2%, 5%, and 10% reduced significantly until day 30, indicating the high diffusion and solubility of prpNPs in the liquid medium, increasing the effect of prpNPs on L. acidophilus over time. Due to the fact that WSLs are a long-term problem and require an antibacterial effect of more endurance, it is better to study the antibacterial effect for longer time periods or by adding prpNPs to the O-rings or the chain elastics that are changed monthly in orthodontic practice.
The results of the study by Mirhashemi et al [37] on chitosan/ZnO nanoparticles incorporated into composite resins showed that the colony counts reduced only on day 30 for L. acidophilus. Sodagar et al [40] stated that the total number of colonies reduced with increasing the concentration of nanosilver/nanohydroxyapatite, and the average number of colonies for all microorganisms increased over time. At 10% concentration and on the third day, the lowest number of colonies and the greatest microbial growth inhibition were observed, which indicate the short-term effect of this nanoparticle despite its proper solubility [40]. Given the good 30-day effect of prpNPs, it is recommended to conduct further studies for longer time periods.
CONCLUSION
Incorporation of nano propolis at concentrations of 2% and 5% into orthodontic adhesives is significantly effective against S. mutans, S. sanguinis, and L. acidophilus, and maintains the SBS within the acceptable clinical range.
ACKNOWLEDGMENTS
This study was funded and supported by the Dental Research Center of Tehran University of Medical Sciences (TUMS); Grant No. 96-01-70-35053. This study was part of a DDS thesis registered at Tehran University of Medical Sciences; Grant No. T922.
Footnotes
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Mansour AY, Drummond JL, Evans CA, Bakhsh Z. In vitro evaluation of self-etch bonding in orthodontics using cyclic fatigue. Angle Orthod. 2011. September;81(5):783–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y, Zhang L, Niu LN, Yu T, Xu HHK, Weir MD, et al. Antibacterial and remineralizing orthodontic adhesive containing quaternary ammonium resin monomer and amorphous calcium phosphate nanoparticles. J Dent. 2018. May;72:53–63. [DOI] [PubMed] [Google Scholar]
- 3.Restrepo M, Bussaneli DG, Jeremias F, Cordeiro RCL, Magalhães AC, Palomari Spolidorio DM, et al. Control of White Spot Lesion Adjacent to Orthodontic Bracket with Use of Fluoride Varnish or Chlorhexidine Gel. ScientificWorldJournal. 2015;2015:218452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Waveren Hogervorst WL, Feilzer AJ, Prahl-Andersen B. The air-abrasion technique versus the conventional acid-etching technique: A quantification of surface enamel loss and a comparison of shear bond strength. Am J Orthod Dentofacial Orthop. 2000. January;117(1):20–6. [DOI] [PubMed] [Google Scholar]
- 5.Dalaie K, Mirfasihi A, Eskandarion S, Kabiri S. Effect of bracket base design on shear bond strength to feldspathic porcelain. Eur J Dent. 2016. Jul-Sep;10(3):351–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajesh RN, Girish KS, Sanjay N, Scindhia RD, Kumar SG, Rajesh S. Comparison of Bond Strength of Brackets with Foil Mesh and Laser Structure Base using Light Cure Composite Resin: An in vitro Study. J Contemp Dent Pract. 2015. December 1;16(12):963–70. [DOI] [PubMed] [Google Scholar]
- 7.Ahn SJ, Lim BS, Lee SJ. Surface characteristics of orthodontic adhesives and effects on streptococcal adhesion. Am J Orthod Dentofacial Orthop. 2010. April;137(4):489–95. [DOI] [PubMed] [Google Scholar]
- 8.Cohen WJ, Wiltshire WA, Dawes C, Lavelle CL. Long-term in vitro fluoride release and rerelease from orthodontic bonding materials containing fluoride. Am J Orthod Dentofacial Orthop. 2003. November;124(5):571–6. [DOI] [PubMed] [Google Scholar]
- 9.Anderson AM, Kao E, Gladwin M, Benli O, Ngan P. The effects of argon laser irradiation on enamel decalcification: An in vivo study. Am J Orthod Dentofacial Orthop. 2002. September;122(3):251–9. [DOI] [PubMed] [Google Scholar]
- 10.Knosel M, Klang E, Helms HJ, Wiechmann D. Occurrence and severity of enamel decalcification adjacent to bracket bases and sub-bracket lesions during orthodontic treatment with two different lingual appliances. Eur J Orthod. 2016. October;38(5):485–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988. July;94(1):68–73. [DOI] [PubMed] [Google Scholar]
- 12.Ogaard B, Rolla G, Arends J, ten Cate JM. Orthodontic appliances and enamel demineralization. Part 2. Prevention and treatment of lesions. Am J Orthod Dentofacial Orthop. 1988. August;94(2):123–8. [DOI] [PubMed] [Google Scholar]
- 13.Harazaki M, Hayakawa K, Fukui T, Isshiki Y, Powell LG. The Nd-YAG laser is useful in prevention of dental caries during orthodontic treatment. Bull Tokyo Dent Coll. 2001. May;42(2):79–86. [DOI] [PubMed] [Google Scholar]
- 14.Gaines S, James TC, Folan M, Baird AW, O’Farrelly C. A novel spectrofluorometric microassay for Streptococcus mutans adherence to hydroxylapatite. J Microbiol Methods. 2003. September;54(3):315–23. [DOI] [PubMed] [Google Scholar]
- 15.Ruparelia JP, Chatterjee AK, Duttagupta SP, Mukherji S. Strain specificity in antimicrobial activity of silver and copper nanoparticles. Acta Biomater. 2008. May;4(3):707–16. [DOI] [PubMed] [Google Scholar]
- 16.Kirschneck C, Christl JJ, Reicheneder C, Proff P. Efficacy of fluoride varnish for preventing white spot lesions and gingivitis during orthodontic treatment with fixed appliances-a prospective randomized controlled trial. Clin Oral Investig. 2016. December;20(9):2371–2378. [DOI] [PubMed] [Google Scholar]
- 17.Taylor R, Coulombe S, Otanicar T, Phelan P, Gunawan A, Lv W, et al. Small particles, big impacts: A review of the diverse applications of nanofluids. J Appl Phys. 2013. January;113(1):011301. [Google Scholar]
- 18.Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003. October;134(10):1382–90. [DOI] [PubMed] [Google Scholar]
- 19.Moreno MI, Isla MI, Sampietro AR, Vattuone MA. Comparison of the free radical-scavenging activity of propolis from several regions of Argentina. J Ethnopharmacol. 2000. July;71(1–2):109–14. [DOI] [PubMed] [Google Scholar]
- 20.Kujumgiev A, Tsvetkova I, Serkedjieva Y, Bankova V, Christov R, Popov S. Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J Ethnopharmacol. 1999. March;64(3):235–40. [DOI] [PubMed] [Google Scholar]
- 21.Castaldo S, Capasso F. Propolis, an old remedy used in modern medicine. Fitoterapia. 2002. November;73 Suppl 1:S1–6. [DOI] [PubMed] [Google Scholar]
- 22.Ghisalberti EL. Propolis: A Review. Bee World. 1979;60(2):59–84. [Google Scholar]
- 23.Banskota AH, Tezuka Y, Kadota S. Recent progress in pharmacological research of propolis. Phytother Res. 2001. November;15(7):561–71. [DOI] [PubMed] [Google Scholar]
- 24.Koo H, Gomes BP, Rosalen PL, Ambrosano GM, Park YK, Cury JA. In vitro antimicrobial activity of propolis and Arnica montana against oral pathogens. Arch Oral Biol. 2000. February;45(2):141–8. [DOI] [PubMed] [Google Scholar]
- 25.Sawicka D, Car H, Borawska MH, Niklinski J. The anticancer activity of propolis. Folia Histochem Cytobiol. 2012. April 24;50(1):25–37. [DOI] [PubMed] [Google Scholar]
- 26.Todd MA, Staley RN, Kanellis MJ, Donly KJ, Wefel JS. Effect of a fluoride varnish on demineralization adjacent to orthodontic brackets. Am J Orthod Dentofacial Orthop. 1999. August;116(2):159–67. [DOI] [PubMed] [Google Scholar]
- 27.Ahn SJ, Lee SJ, Kook JK, Lim BS. Experimental antimicrobial orthodontic adhesives using nanofillers and silver nanoparticles. Dent Mater. 2009. February;25(2):206–13. [DOI] [PubMed] [Google Scholar]
- 28.Sodagar A, Akhoundi MSA, Bahador A, Jalali YF, Behzadi Z, Elhaminejad F, et al. Effect of TiO2 nanoparticles incorporation on antibacterial properties and shear bond strength of dental composite used in Orthodontics. Dental Press J Orthod. 2017. Sep-Oct;22(5):67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aydin Sevinç B, Hanley L. Antibacterial activity of dental composites containing zinc oxide nanoparticles. J Biomed Mater Res B Appl Biomater. 2010. July;94(1):22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tavassoli Hojati S, Alaghemand H, Hamze F, Ahmadian Babaki F, Rajab-Nia R, Rezvani MB, et al. Antibacterial, physical and mechanical properties of flowable resin composites containing zinc oxide nanoparticles. Dent Mater. 2013. May;29(5):495–505. [DOI] [PubMed] [Google Scholar]
- 31.Kasraei S, Sami L, Hendi S, AliKhani MY, Rezaei-Soufi L, Khamverdi Z. Antibacterial properties of composite resins incorporating silver and zinc oxide nanoparticles on Streptococcus mutans and Lactobacillus. Restor Dent Endod. 2014. May;39(2):109–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hernández-Sierra JF, Ruiz F, Pena DC, Martínez-Gutiérrez F, Martínez AE, Guillén Ade J, et al. The antimicrobial sensitivity of Streptococcus mutans to nanoparticles of silver, zinc oxide, and gold. Nanomedicine. 2008. September;4(3):237–40. [DOI] [PubMed] [Google Scholar]
- 33.Akhavan A, Sodagar A, Mojtahedzadeh F, Sodagar K. Investigating the effect of incorporating nanosilver/nanohydroxyapatite particles on the shear bond strength of orthodontic adhesives. Acta Odontol Scand. 2013. September;71(5):1038–42. [DOI] [PubMed] [Google Scholar]
- 34.Grenho L, Barros J, Ferreira C, Santos VR, Monteiro FJ, Ferraz MP, et al. In vitro antimicrobial activity and biocompatibility of propolis containing nanohydroxyapatite. Biomed Mater. 2015. March 18;10(2):025004. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds IR, von Fraunhofer JA. Direct bonding of orthodontic brackets--a comparative study of adhesives. Br J Orthod. 1976. July;3(3):143–6. [DOI] [PubMed] [Google Scholar]
- 36.Sharma S, Tandon P, Nagar A, Singh GP, Singh A, Chugh VK. A comparison of shear bond strength of orthodontic brackets bonded with four different orthodontic adhesives. J Orthod Sci. 2014. Apr-Jun;3(2):29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mirhashemi A, Bahador A, Kassaee M, Daryakenari G, Ahmad-Akhoundi M, Sodagar A. Antimicrobial Effect of Nano-Zinc Oxide and Nano-Chitosan Particles in Dental Composite Used in Orthodontics. JMB. 2013;2(3–4):1–10. [Google Scholar]
- 38.Poosti M, Ramazanzadeh B, Zebarjad M, Javadzadeh P, Naderinasab M, Shakeri MT. Shear bond strength and antibacterial effects of orthodontic composite containing TiO2 nanoparticles. Eur J Orthod. 2013. October;35(5):676–9. [DOI] [PubMed] [Google Scholar]
- 39.Fernandez L, Canut JA. In vitro comparison of the retention capacity of new aesthetic brackets. Eur J Orthod. 1999. February;21(1):71–7. [DOI] [PubMed] [Google Scholar]
- 40.Sodagar A, Bahador A, Pourhajibagher M, Ahmadi B, Baghaeian P. Effect of Addition of Curcumin Nanoparticles on Antimicrobial Property and Shear Bond Strength of Orthodontic Composite to Bovine Enamel. J Dent (Tehran). 2016. September;13(5):373–82. [PMC free article] [PubMed] [Google Scholar]


