Introduction:
Patients with cirrhosis have high admission and readmission rates, resulting in a substantial burden to both patients and the healthcare system. 1 In this context, insurance companies are shifting toward value-based care and incentivizing hospitals to develop innovative care management strategies to prevent unnecessary hospitalizations.
As with other clinical populations, there may be an opportunity to avoid inpatient admission through observation in the emergency department or close outpatient follow-up for patients with cirrhosis. Emergency department observation units (EDOU) have been successfully used to rule out myocardial infarction or manage a heart failure exacerbation.2-5 Similarly, protocols that identify low acuity populations for expedited short term interventions and directed observation through the emergency department can improve patient care.6
We sought to find opportunities to reduce a subset of admissions related to cirrhosis. Our process, which was IRB-approved, included 1) medical record review, 2) provider surveys, and 3) patient interviews to identify a targetable low acuity condition. First, chart review conducted for hospitalizations with a length of stay of less than 3 days from July 2015-September 2016 (n=210) identified two low acuity conditions in patients with cirrhosis: ascites requiring large volume paracenteses (LVPs) (10.3% of unplanned admissions) and mild hepatic encephalopathy (9.6% of unplanned admissions). Next, in order to determine whether there was provider consensus on safely triaging patients with these two conditions, a multicenter survey was conducted. 7 At our institution, there was a response rate of 85.6% (24 hepatology and 45 ED providers). Notably, the majority (86.2%) of providers believed an EDOU protocol to expedite LVPs for patients with ascites would safely prevent admission. There was less consensus on management of mild hepatic encephalopathy (16.9% recommended admission; 29% recommended care in the EDOU; 53% recommended isolated ED care). Therefore, we targeted our intervention to uncontrolled ascites. Finally, 10 semi-structured patient interviews were conducted in which two themes emerged: first, patients sought a system for the fastest possible LVP. Based on prior experiences, they were frustrated that the ED did not have the capability to perform the procedure, and that inpatient services by interventional radiology and housestaff were often delayed. Second, they valued providers reviewing their fluid results and laboratory values in a timely fashion to ensure that there was no additional problem beyond the presence of ascites. These preliminary studies supported the development of an EDOU protocol to reduce admissions for LVPs.
Development of QI protocol to reduce admissions for paracenteses:
Multidisciplinary stakeholder collaboration:
To develop our intervention, we convened key stakeholders in gastroenterology, emergency medicine, interventional radiology, and critical care to discuss aforementioned findings, available resources, and potential solutions.
A total of three in-person meetings took place. The initial meeting included eight participants, all of whom were providers (physicians or APPs) along with the hospital Chief Medical Officer (CMO). The hospital CMO emphasized the executive leadership’s investment in identifying targetable opportunities to prevent admissions safely. During this meeting, the data from preliminary studies were presented in order to define the scope and context of admissions for ascites. Afterward, each stakeholder outlined resources available and limitations. Specifically, the interventional radiology team did not have the bandwidth to expedite LVPs, as more urgent cases were taking priority. The critical care team proposed that we utilize the “Procedure Team” to expedite paracenteses, and for the remaining two meetings, members of the Procedure Team were engaged in drafting the protocol with leaders in the EDOU and gastroenterology division.
Procedure Team:
At our institution, there is an advanced practitioner (APP)-run “Procedure Team” with physician oversight. This team is comprised of one APP working in conjunction with a collaborating faculty member and a resident on a weeklong elective. There are 22 participating pulmonary and critical care attending physicians and 19 APPs who rotate on the staff of the Procedure Team. Procedures can be completed independently by a certified APP or by an APP or resident trainee with direct supervision by faculty. Any team throughout the hospital can place a request through our electronic consult system for a procedure to be performed all days of the week. Once the team receives the request, they coordinate peri-procedural transfusions and anticoagulation management, provision of sedation when necessary, and coordination of timing based on urgency with the primary team. Procedures include bedside cases such as central and arterial line insertion, paracentesis, thoracentesis, and lumbar puncture. For paracenteses, APPs commonly conduct the entirety of the procedure without attending participation. Faculty participation usually occurs only when further training is needed (i.e. resident physician or new APP).
Emergency Department Observation Unit (EDOU):
The EDOU is staffed by both APPs and attending physicians in the emergency department who are assigned to care for EDOU patients only. The primary goal is to safely expedite triage for patients who can be discharged quickly or require further evaluation through inpatient admission. The goal in the EDOU is to designate further triage within 24-36 hours. Therefore, stakeholders in the EDOU were primarily focused on expediting paracenteses for our patients. The Procedure Team agreed to prioritize these cases as much as possible, allowing for buy-in from EDOU leadership.
Protocol development:
Through collaboration with medical leadership of the Procedure Team, the EDOU, and gastroenterology, a protocol was created to expedite paracenteses for patients who present to the emergency department.
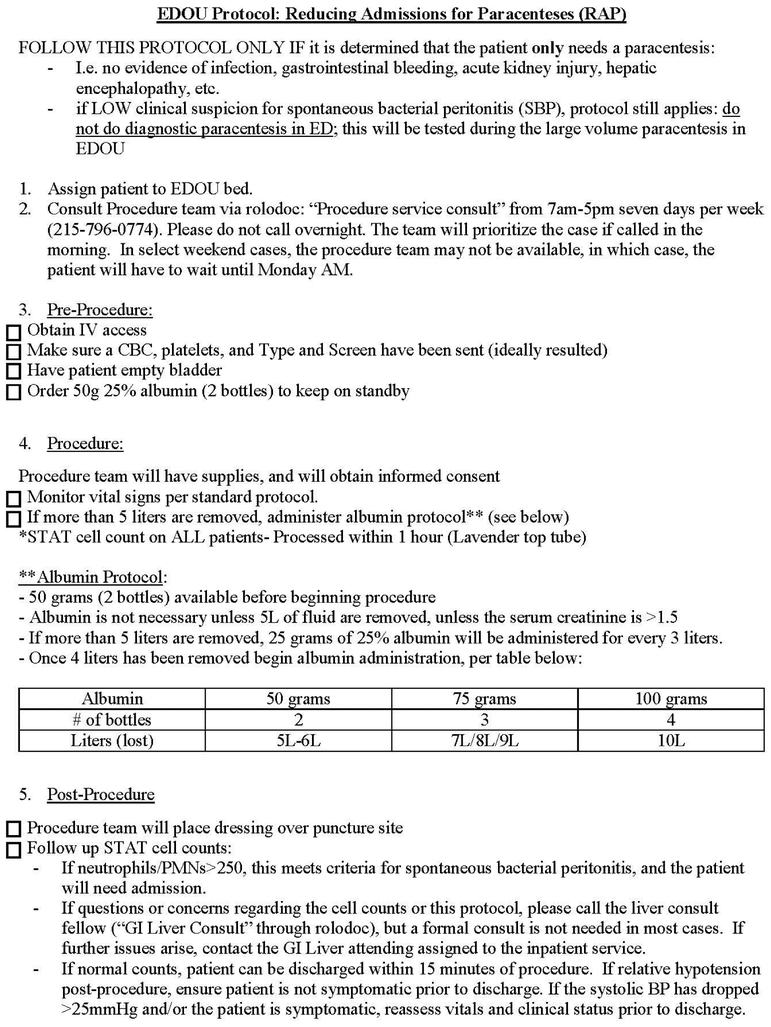
This protocol specified limited inclusion criteria: patients with ascites qualified if they required LVP and have no evidence of infection, gastrointestinal bleeding, acute kidney injury, hepatic encephalopathy, or other acute decompensation. Patients were included if the ED providers had a low suspicion for spontaneous bacterial peritonitis (SBP), but were excluded if there was a high suspicion. The protocol entailed the following components:
Pre-procedure: expedited triage of patient from ED to EDOU, Procedure Team consultation, lab orders for complete blood count, coagulation labs, and blood type and screen, instructions for patient to empty their bladder, and orders for albumin to keep on standby.
Procedure: Vital signs monitoring, diagnostic and therapeutic LVP for all patients, and albumin protocol if more than 5 liters of ascitic fluid are removed. A STAT cell count is ordered for all patients, which is processed within one hour. A reflex culture is sent if positive.
Post-procedure: EDOU team follows up on diagnostic paracentesis results, and the GI Liver consult team is available 24/7 to aid the ED and EDOU providers if there is any clinical uncertainty regarding patient management during the protocol.
For patients outside the ED, a fast track option was also provided. For example, if a hepatology provider identified a patient in clinic or on the phone who required an expedited diagnostic and therapeutic LVP, they could call the ED triage nurse to fast track patients through the ED to the EDOU.
Metrics were also selected prior to protocol implementation. Our primary outcome was admissions for LVPs in patients with cirrhosis. Secondary outcomes included admission for any reason, 30-day readmission to our institution, total “institutional” length of stay (encompassing length of stay in the emergency department and the EDOU), and provider follow-up within 2 weeks after discharge from the EDOU (phone call or outpatient visit). As our ED is often busy and full, we did not want to increase length of stay within the ED, which could have a downstream effect of increased waiting times for other patients. As such, we created a balancing metric of ED length of stay (LOS).
Pre-protocol data (based on 15 months of chart review) was compared with post-protocol data (March 2017 to March 2019), and were analyzed using descriptive statistics (Wilcoxon ranked sum). Additionally, the x-chart, a type of statistical process control chart, was used to assess changes in LOS.10 All analyses were conducted using Stata, Version 14.
Protocol Results:
The protocol was implemented in March 2017. The initial plan was for a 3-month pilot period, but given success of the protocol, it has been maintained in an ongoing fashion. The data presented are over a two year span until March 2019.
Primary outcome: Admission for LVP in patients with cirrhosis:
Prior to the protocol, 15 patients presented to the ED, and all patients were admitted given no system in place to care for them outside of an inpatient admission. Since initiation of the protocol, over two years, 30 patients presented to the ED with uncontrolled or new ascites. None were admitted exclusively for paracentesis (Appendix Table 1).
Secondary outcomes:
Admission for any reason:
Two patients who went through the protocol were admitted after receiving the LVP in the EDOU; one patient was found to have SBP; the GI Liver team was consulted and recommended an inpatient admission. The second patient was recognized to have elevated liver tests; again, the GI Liver team was consulted, and admitted the patient for a flare of autoimmune hepatitis. In both cases, the patient required additional care beyond the scope of the protocol, and management was escalated for inpatient admission.
Admissions within 30 days of discharge:
The time for assessing 30-day readmission started with the date of discharge from the inpatient stay in the pre-protocol period and from the EDOU during the post-protocol period. We observed no significant difference in admissions within 30-days of discharge between the groups (15.4% vs. 17.2%, p=0.84).
Further proof of the benefit of the protocol was measured when studying its use in patients with recent admissions. 12 out of the 30 patients undergoing the drainage protocol were admitted within the prior 30 days. If the protocol were not in place, their presentation to the ED would have resulted in an admission for a LVP (i.e. a 30-day readmission).
Length of stay:
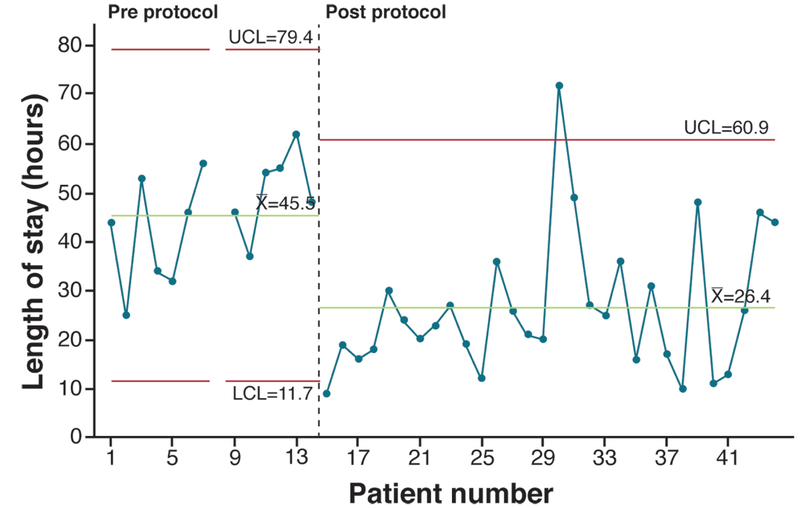
The mean total length of stay prior to the protocol implementation was 45.5 hours; it decreased to 26.4 hours after protocol implementation (p=0.001) (Figure 1). This reduction persisted despite including one outlier patient who had a 72-hour length of stay post-protocol implementation, which was due to the need for an upper endoscopy recommended by the GI liver consult team during the EDOU stay.
Figure 1: Statistical Process Control chart for Length of Stay.
LOS = Length of Stay in hours. UCL=Upper Control Limit, X=Mean, LCL=Lower Control Limit
Length of stay was also examined by type (occurring in ED vs. EDOU vs. inpatient). The mean length of stay in the emergency department was 9.8 hours pre-protocol and 7.3 hours post-protocol implementation (p=0.04).
Outpatient follow-up:
Arranging outpatient follow-up on discharge from an inpatient admission or ED visit is standard of care at our institution. There was no significant difference in outpatient follow-up (76.9% vs. 82.8%, p=0.96), which included a phone call or outpatient visit from a liver provider or primary care physician (Appendix Table 1).
Impact in a value-based marketplace:
This practice innovation has successfully prevented admissions for paracenteses, utilizing a safe and efficient route in the EDOU. Identifying low acuity conditions to utilize fast tracks in the emergency department or observation unit has been very successful for various clinical conditions, including ruling out myocardial infarction, heart failure exacerbation, and post-procedural visits 2-5. Such interventions have been shown to expedite patient care, reduce length of stay in the emergency department, and reduce costs. At other institutions, patients with cirrhotic ascites are often admitted for inpatient management with significant cost burden; in other scenarios, they have been shown to be successfully safely managed in a day hospital.11-13 By avoiding inpatient admission, we have reduced a subset of 30-day readmissions.
The recent national focus on readmissions has resulted in efforts to find methods to care for patients more effectively outside of a hospitalization. Often, this entails complex management strategies in an outpatient setting. However, identifying patients in the emergency department who could safely avoid inpatient admission is an important targetable opportunity. At our institution, the hospital is held accountable for all-cause 30-day readmissions for patients covered by our largest insurer. Similarly, national measures through Medicare inpatient quality reporting result in hospital penalties for 30-day readmissions. Such financial arrangements now incentivize health systems to develop novel methods to safely reduce admissions. Through patient and provider engagement, we were able to determine a safe care pathway based on the comfort of providers at our institution to carefully triage and provide resources for our patients.
Acknowledgments
Disclosures:
All authors have no disclosures relevant to this study.
Grant funding: T32-DK007740
Appendix Online-Only Material
Appendix Table 1:
Protocol outcomes for patients presenting with ascites requiring paracenteses
| Metric | Pre-protocol | Post-protocol | P-value |
|---|---|---|---|
| Admissions | Frequency (%) | Frequency (%) | |
| For LVPs | 15/15 (100%) | 0/30 (0%) | N/A |
| Any cause | 15/15 (100%) | 2/30 (6.7%) | <0.05 |
| Admissions within 30 days of discharge | Frequency (%) | Frequency (%) | |
| Admissions after hospital or ED visit | 2/13* (15.4%) | 5/29* (17.2%) | 0.84 |
| Length of Stay (hours) | Mean (S.D) | Mean (S.D) | |
| Total LOS (ED, EDOU, and Inpatient) | 45.5 (10.4) | 26.4 (13.9) | 0.001 |
| ED LOS | 9.8 (2.5) | 7.3 (3.6) | 0.04 |
| Outpatient follow-up | Frequency (%) | Frequency (%) | |
| Follow-up with PCP or liver provider within 2 weeks | 10/13* (76.9%) | 24/29 (82.8%) | 0.96 |
| - Phone call | 5/13* (38.5%) | 14/29* (48.3%) | |
| - Outpatient visit | 5/13* (38.5%) | 10/29* (34.5%) |
Lower denominator due to patients deceased or sent to hospice within 30 days of discharge Abbreviations: LVP = large volume paracenteses, LOS = length of stay, ED = emergency department, EDOU = emergency department observation unit, PCP = primary care physician
Appendix Figure 1: EDOU Protocol: Reducing Admissions for Paracenteses (RAP).
Protocol document.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Bajaj JS, Reddy KR, Tandon P et al. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016. 64(1), 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Damiani G, Pinnarelli L, Sommella L,Vena V, Magrini P, Ricciardi W. The short stay unit as a new options for hospitals: a review of the scientific literature. Med Sci Monit. 2011;17(6):SR15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Downing H, Scott C, Kelly C. Evaluation of a dedicated short-stay unit for acute medical admissions. Clinical Medicine. 2008;8(1):18–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mace SE, Graff L, Mikhail M, et al. A national survey of observation units in the United States. Am J Emerg Med. 2003;21:529–533. [DOI] [PubMed] [Google Scholar]
- 5.Marcantuono R, Gutsche J, Burke-Julien M et al. Rationale, development, implementation, and initial results of a fast track protocol for transfemoral transcatheter aortic valve replacement (TAVR). Cathet. Cardiovasc. Intervent, 85: 648–654. [DOI] [PubMed] [Google Scholar]
- 6.Mercer MP, Singh MK, Kanzaria HK. Reducing Emergency Department Length of Stay. JAMA. Published online March 19, 2019. Doi: 10.1001/jama.2018.21812 [DOI] [PubMed] [Google Scholar]
- 7.Siddique SM, Lane-Fall M, McConnell MJ et al. Exploring opportunities to prevent cirrhosis admissions in the emergency department: A multicenter multidisciplinary survey. Hepatol Commun 2018. January 26;2(3):237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 2015;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagan KJ, Zhao EY, Horsfall LU, Ruffin BJ, Kruger MS, McPhail SM, et al. Burden of decompensated cirrhosis and ascites on hospital services in a tertiary care facility: time for change? Intern Med J. 2014. September;44(9):865–72. [DOI] [PubMed] [Google Scholar]
- 12.Morando F, Maresio G, Piano S, Fasolato S, Cavallin M, Romano A et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013. August;59(2):257–64. [DOI] [PubMed] [Google Scholar]
- 13.Hudson B, Round J, Georgeson B, Pring A, Forbes K, McCune CA et al. Cirrhosis with ascites in the last year of life: a nationwide analysis of factors shaping costs, health-care use, and place of death in England. Lancet Gastroenterol Hepatol. 2018. February;3(2):95–103. [DOI] [PubMed] [Google Scholar]