Abstract
Purpose
The ability to convert scores between cognitive measurements would facilitate the longitudinal assessment of cognition in clinical practice and the comparison and synthesis of cognitive data from international, multicenter, or longitudinal studies. The primary aim of this study was to apply a simple and reliable method for converting scores from the Korean Dementia Screening Questionnaire (KDSQ) to those of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE).
Patients and methods
A total of 627 participants, with and without cognitive dysfunction, received both the KDSQ and the IQCODE at the same visit. The scores of both tools were calculated, and equipercentile equating was used to create a method for converting scores from the KDSQ to the IQCODE.
Results
KDSQ scores were highly correlated with IQCODE scores (Pearson r = 0.905, P < 0.01). We developed scores for converting the KDSQ to the IQCODE using equipercentile equating and log-linear smoothing. We provide an easy-to-use table that enables the conversion of KDSQ scores to IQCODE scores.
Conclusion
We delivered a simple and reliable method for converting scores from the KDSQ to the IQCODE. The conversion score table reported here enables direct and easy comparison of these cognitive measurements in older adults.
Keywords: KDSQ, IQCODE, cognition, equation
Introduction
With the rapid growth of the elderly population, the global prevalence of dementia has rapidly increased.1 In Korea, there are presently about 700,000 people with dementia and 1,590,000 people with mild cognitive impairment (MCI) in 2017, and these number are expected to rise rapidly.2,3 Thus, adequate and effective cognitive screening is essential. Even with the emergence of sophisticated imaging technologies and biomarkers, brief cognitive screening tools remain a core component of dementia diagnosis, as they are quick and useful methods for assessing overall cognition.4,5
Brief cognitive tools can be used in several ways, through patient performance-based measures or informant-based reports. The advantages of informant-based reports are that they can assess cognitive decline as well as current functioning, they are applicable for people with limited education, and they are less of a threat to the self-esteem of the person assessed.6 Among informant-based reports, the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is one of the most well-known and widely used.6,7 It requires relatives or friends to compare a patient’s current cognitive and functional performances in everyday life to past performance.
Cognitive dysfunction has been assessed regarding functional status and everyday performance, which were required for adapting the tests for use in individuals with differing cultural backgrounds. However, the successful application of existing cognitive assessment tools may be limited for different ethnicities or different cultural groups.8,9 New tools have been developed that have been adapted for specific cultures. In Korea, the Korean Dementia Screening Questionnaire (KDSQ) has been widely used because of its ease of use and culturally specific adaptation with high validity and reliability for the screening of dementia in elderly people.3,10,11 Moreover, the Korean Ministry of Health and Welfare began a new National Screening Program for Transitional Age for people who are 66 years old, and all participants in this program completed part of the KDSQ to screen for cognitive dysfunction.12
Although the KDSQ has been widely used in Korea, it has not been used outside of Korea. The clinical trials using the KDSQ or screening results from the KDSQ have been difficult to compare to those from different centers or cultures that have not used the KDSQ. If the KDSQ and other widely used tools can be made interchangeable, it will be useful for interpreting or comparing the results from these different tools.
Therefore, this study provides a method for converting KDSQ scores to IQCODE scores. The results will facilitate the comparison of data from different clinical or research settings.
Materials And Methods
Participants
This is an observational cross-sectional study of performance using two cognitive screening questionnaires in consecutive patients who visited a memory clinic at a university hospital in the Republic of Korea and were referred for neuropsychological testing. A total of 627 participants were recruited: 337 participants with dementia, 213 participants with MCI, and 77 participants who were cognitively normal (control). A consensus diagnosis was determined using standardized clinical criteria for MCI13 and dementia.14 MCI subtypes and dementia subtypes were not analyzed in this study. The controls did not meet the criteria for MCI or dementia but were identically recruited and assessed as the patients with MCI and dementia.
All participants were evaluated on the basis of their medical history, physical and neurological examinations, laboratory tests, brain imaging, and a neuropsychological battery. Consensus diagnoses by a geriatric physician and a neuropsychologist were used to determine each subject’s clinical status on the basis of the clinical evaluations. The exclusion criteria included preexisting conditions that might affect participants’ performance on cognitive measures, such as intellectual disability, drug or substance abuse, and severe psychiatric illness. All participants who were accompanied by an informant were included. The informants were participants’ spouses or relatives who lived in the same household and reported no psychiatric or neurological disease themselves. All informants were administered the IQCODE after the KDSQ during the same day. The results of both KDSQ and IQCODE were not available during consensus diagnosis. This study was approved by the Institutional Review Board of Korea University Ansan Hospital, which waived the requirement to obtain informed consent. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Clinical Assessments
Korean Dementia Screening Questionnaire (KDSQ)
The KDSQ is an informant-based questionnaire that addresses changes in elderly participants’ cognitive performance over the previous year.3,10,11 It has 15 cognitive dysfunction items, each rated on a three-point scale: 0 (no change), 1 (sometimes/occasional change), and 2 (often/frequent change), with a higher score indicating poorer function and a greater frequency. Five KDSQ items assessed global memory function: (i) does not know the date or day; (ii) cannot find things he or she previously put down; (iii) keeps repeating the same questions; (iv) forgets appointments; and (v) comes back without things he or she had intended to pick up. Five items assessed other cognitive functions and behavior. These included the following: (vi) mumbles because names of people or things slip their mind; (vii) keeps asking questions because he/she does not get the point; (viii) gets lost or goes astray; (ix) has difficulty with financial affairs (e.g., paying bills or calculating change); and (x) his/her personality has changed. Another five items assessed instrumental activities of daily living. These included (xi) difficulty operating appliances (e.g., washing machine, electric cooker, or cultivator); (xii) cannot keep rooms or house clean; (xiii) does not wear outfits that fit the time, place, or occasion; (xiv) finds it hard to go somewhere on his/her own using public transportation (except in the case of physical disability, such as arthritis); and (xv) refuses to change dirty underwear or clothes. The KDSQ (cut-off point 8) has a sensitivity of 0.75 and specificity of 0.73 for dementia and it is not influenced by age or educational level.8,11
Informant Questionnaire On Cognitive Decline In The Elderly (IQCODE)
The IQCODE is a reliable, validated informant-based questionnaire with the goal of assessing change in cognitive and functional performance over 10 years and has been widely adopted by clinical researchers across different cultures and languages.6,7 This study was based on the 26-item Korean version of the IQCODE,15 and the cognitive changes were scored on a five-point scale, with 1 indicating “much improved,” 3 indicating “not much change,” and 5 indicating “much worse.” The total score derived from averaging the ratings over the total number of completed items and can range from 1.0 to 5.0, with higher scores indicating worse decline. The Korean version of IQCODE (cut-off point 3.6) has a sensitivity of 0.90 and specificity of 0.79 for dementia.15
Both the KDSQ and the IQCODE were autonomously completed by the informants, after they received the appropriate instructions, while the participants were undergoing neuropsychological assessment. At the end of the participant’s testing session, the KDSQ and IQCODE were scored by an examiner (one psychology trainee) blind to the participant’s assessment after the responses had been checked with the informant to ensure full comprehension and completion of questions.
Other Clinical Assessments
Demographic data (age and sex) and information about years of education were collected from the participants and informants. The screening and cognitive assessments included the Mini-Mental State Examination (MMSE),16 the Clinical Dementia Rating (CDR),17 the Geriatric Depression Scale (GDpS),18 and the neuropsychological battery. The neuropsychological battery was used with the Korean version of the assessment packet developed by the Consortium to Establish a Registry for Alzheimer’s Disease.19
Statistical Analyses
Data are expressed as the means (standard deviation) for continuous variables and as a percentage for the categorical variables. Demographic and clinical characteristics were evaluated with chi-squared tests for the difference between proportions, and Kruskal–Wallis test was used to test differences between continuous variables after performing Levene’s test for equality of variance. Bonferroni correction was used for post hoc comparisons. The overall agreement between the two measurements was assessed using Pearson’s correlation coefficient (r).
To convert scores from the KDSQ to the IQCODE, we generated an equating table to link the two tools using the R “equate” package.20 The single group design method was used in this study, reflecting that the same population was assessed using the two cognitive tools (the KDSQ and the IQCODE). We used the equipercentile equating method.21 This method has been used to equate numerous standardized tests in patients with cognitive dysfunction.22–28, This statistical method allows for the determination of comparable test scores from two different measures on the basis of their corresponding percentile ranks. The advantage of the equipercentile equating method is that the equated scores always fall within the range of possible scores, which is not always true when using traditional mean and linear equating methods. However, this method can lead to an irregular distribution of scores, and thus, a log-linear transformation of each measurement’s raw score is necessary before the equating to smooth the raw scores and to create a normal distribution without irregularities that are attributable to sampling. Log-linear transformation enhances equating accuracy.
Analyses were performed using SPSS for Windows, version 20.0 (IBM Corporation, Armonk, NY, USA) and R 3.2.4 software (The R Foundation for Statistical Computing, Vienna, Austria). Statistical tests were two-tailed, and α was set at <0.05.
Results
The clinical characteristics of the study participants are presented in Table 1. The average KDSQ scores based on cognitive status were 2.81 (2.50) in control, 5.41 (4.26) in MCI, and 18.66 (7.11) in dementia groups. The average IQCODE scores based on cognitive status were 3.24 (0.20) in control, 3.41 (0.31) in MCI, and 4.34 (0.43) in dementia groups. As expected, the KDSQ (H=390.21, P<0.001) and IQCODE (H=402.39, P<0.001) scores significantly differed across each group of participants based on cognitive status in the post hoc analyses.
Table 1.
Demographic Characteristics
| Variables | Total (n=627) | Cognitive Status | P | ||
|---|---|---|---|---|---|
| Dementia (n=337) | MCI (n=213) | Control (n=77) | |||
| Demographics | |||||
| Age, year | 71.26 (10.94) | 71.56 (10.38) | 70.86 (9.84) | 70.75 (7.74) | 0.371a |
| Sex, female | 363 (57.9%) | 201 (59.6%) | 117 (54.9%) | 45 (58.4%) | 0.549b |
| Education, year | 7.53 (4.99) | 7.35 (5.04) | 7.72 (4.33) | 7.82 (4.69) | 0.450a |
| Clinical assessments | |||||
| MMSE | 21.29 (10.21) | 17.18 (12.25) | 25.50 (3.02) | 27.61 (1.96) | <0.001a |
| CDR | 0.77 (0.54) | 1.10 (0.54) | 0.52 (0.10) | 0.00 (0.00) | <0.001a |
| GDpS | 7.25 (4.26) | 7.59 (4.42) | 7.22 (4.14) | 5.92 (3.68) | 0.008a |
| Informant questionnaires | |||||
| KDSQ | 12.21 (9.12) | 18.66 (7.11) | 5.41 (4.26) | 2.81 (2.50) | <0.001a |
| IQCODE | 3.89 (0.61) | 4.34 (0.43) | 3.41 (0.31) | 3.24 (0.20) | <0.001a |
Notes: Values are presented as the means (SD) or numbers (%). aKruskal–Wallis test. bChi-squared test.
Abbreviations: MCI, mild cognitive impairment; control, cognitively normal; MMSE, Mini-Mental Status Examination; CDR, Clinical Dementia Rating; GDpS, Geriatric Depression Scale; KDSQ, Korean Dementia Screening Questionnaire; IQCODE, Informant Questionnaire on Cognitive Decline in the Elderly.
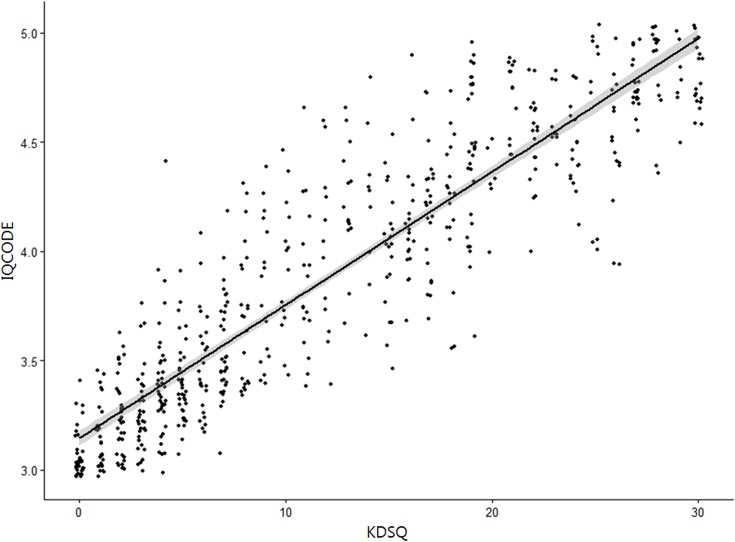
The correlation between the KDSQ and the IQCODE scores was statistically significant. The KDSQ scores were positively correlated with the IQCODE scores (r=0.905, P<0.01). Figure 1 presents the scatterplot for the KDSQ and IQCODE scores in individual participants and the correlation line between the KDSQ and IQCODE scores. The plot of equipercentile equivalent scores on the KDSQ and IQCODE is presented in Figure 2. For example, a score of 10 on the KDSQ is equivalent to a score of 3.77 on the IQCODE, with both of these scores falling at approximately the 50th percentile rank. Table 2 shows scores on the KDSQ and their respective equivalents, averages, medians, and ranges on the IQCODE. A lower KDSQ score was equal to a lower IQCODE score.
Figure 1.
Relationship of the KDSQ scores to the IQCODE scores (Pearson r = 0.905, P<0.01). The line represents linear regression of the data (y=0.061x + 3.147, r2=0.818).
Figure 2.
Equipercentile equating of the KDSQ (black color) and the IQCODE (gray color) corresponding to test scores and percentile ranks allows conversion of the KDSQ scores to the IQCODE scores. For example, a KDSQ score of 10 (50th percentile) is equivalent to an IQCODE score of 3.77 (50th percentile).
Table 2.
KDSQ To IQCODE Conversion Table
| KDSQ Score | IQCODE Score | N | |||
|---|---|---|---|---|---|
| Equivalent | Average | Median | Range | ||
| 0 | 3.01 | 3.07 (0.11) | 3.00 | 3.00–3.38 | 33 |
| 1 | 3.08 | 3.14 (0.15) | 3.07 | 3.00–3.46 | 29 |
| 2 | 3.16 | 3.23 (0.18) | 3.19 | 3.00–3.61 | 37 |
| 3 | 3.25 | 3.27 (0.18) | 3.23 | 3.00–3.76 | 34 |
| 4 | 3.34 | 3.41 (0.26) | 3.34 | 3.00–4.38 | 38 |
| 5 | 3.43 | 3.40 (0.18) | 3.38 | 3.07–3.88 | 35 |
| 6 | 3.48 | 3.47 (0.23) | 3.42 | 3.19–4.07 | 26 |
| 7 | 3.54 | 3.57 (0.23) | 3.51 | 3.07–4.15 | 32 |
| 8 | 3.60 | 3.71 (0.32) | 3.70 | 3.34–4.34 | 22 |
| 9 | 3.69 | 3.82 (0.33) | 3.83 | 3.42–4.42 | 16 |
| 10 | 3.77 | 3.91 (0.31) | 3.94 | 3.46–4.46 | 14 |
| 11 | 3.85 | 3.86 (034) | 3.73 | 3.42–4.65 | 17 |
| 12 | 3.92 | 3.98 (0.38) | 3.96 | 3.38–4.62 | 13 |
| 13 | 3.98 | 4.21 (0.28) | 4.19 | 3.65–4.65 | 14 |
| 14 | 4.08 | 4.23 (0.35) | 4.28 | 3.65–4.80 | 9 |
| 15 | 4.18 | 4.01 (0.28) | 4.07 | 3.47–4.53 | 20 |
| 16 | 4.27 | 4.14 (0.26) | 4.07 | 3.69–4.88 | 19 |
| 17 | 4.30 | 4.18 (0.26) | 4.19 | 3.73–4.69 | 23 |
| 18 | 4.35 | 4.21 (0.31) | 4.26 | 3.57–4.76 | 19 |
| 19 | 4.41 | 4.45 (0.34) | 4.47 | 3.61–4.92 | 30 |
| 20 | 4.47 | 4.33 (0.17) | 4.34 | 4.03–4.50 | 6 |
| 21 | 4.52 | 4.71 (0.18) | 4.76 | 4.42–4.92 | 13 |
| 22 | 4.57 | 4.51 (0.21) | 4.57 | 4.00–4.84 | 18 |
| 23 | 4.61 | 4.60 (0.15) | 4.57 | 4.38–4.84 | 9 |
| 24 | 4.64 | 4.48 (0.17) | 4.46 | 4.15–4.76 | 16 |
| 25 | 4.71 | 4.65 (0.42) | 4.83 | 4.00–5.00 | 10 |
| 26 | 4.74 | 4.49 (0.29) | 4.50 | 3.96–5.00 | 15 |
| 27 | 4.81 | 4.77 (0.11) | 4.75 | 4.57–5.00 | 18 |
| 28 | 4.87 | 4.84 (0.22) | 4.96 | 4.38–5.00 | 15 |
| 29 | 4.92 | 4.79 (0.16) | 4.78 | 4.50–5.00 | 8 |
| 30 | 4.99 | 4.82 (0.14) | 4.76 | 4.61–5.00 | 19 |
Notes: Equivalent IQCODE scores were generated using equipercentile equating methods. The equivalent, average, median, and range of the IQCODE scores are shown for each possible score on the KDSQ. Average is presented as the means (SD).
Abbreviations: KDSQ, Korean Dementia Screening Questionnaire; IQCODE, Informant Questionnaire on Cognitive Decline in the Elderly.
Discussion
This study aimed to develop a method for converting scores from the KDSQ to the IQCODE using equipercentile equating and log-linear smoothing. To our knowledge, this is the first study on the conversion of cognitive screening tools with the KDSQ and the IQCODE.
Early and accurate detection of cognitive dysfunction in older adults who indicate that they may be transitioning into dementia can enhance clinical management and lead to a better understanding of individual differences in disease progression.1–5 As early detection becomes more necessary, well-validated and brief measurements of cognitive performance are needed. However, these measurements should be appropriate for each ethnic or cultural situation. Various brief cognitive screening tools or questionnaires have been recommended: the General Practitioner Assessment of Cognition (GPCOG), the Mini-Cog, the Memory Impairment Screen (MIS), the Short Form of the IQCODE (Short IQCODE), the eight-item informant interview to differentiate aging and dementia (AD8) by the Alzheimer’s Association,29 the Samsung Dementia Questionnaire (SDQ), the KDSQ, and the Korean AD8 by the Clinical Research Center for Dementia of South Korea.30
Because a variety of tools can be used and in some cases over time, one tool should be substitutable for another, and we perceived the need to develop a method for converting the score from one tool to that of another. Equating methodologies can facilitate comparisons between studies using different tools to measure the same construct. Such conversions will facilitate both the continuity of longitudinal cognitive tracking in clinical practice and the comparison and synthesis of cognitive data from international, multicenter, or longitudinal studies.
For cognitive screening, the KDSQ is the most commonly used questionnaire in Korea,3,11,12 and the IQCODE is one of the most widely used in the world.7 A reliable conversion of the two screening tools to ensure continuity in various settings would facilitate a smooth transition from the KDSQ to the IQCODE. This study has derived an equating rule to allow for the accurate conversion of scores between the two tools. Transitioning from the KDSQ to the IQCODE is, however, complicated by the fact that the KDSQ was developed for Korean people with their specific cultural adaptations, and it evaluates changes in an elderly subject’s cognitive performance over the previous year. Since the IQCODE is globally used and it evaluates the subject’s current cognitive performance with his/her level of functioning over the previous 10 years, these scores cannot be regarded as equivalent. However, this study showed that the KDSQ had a significant correlation with the IQCODE and a reliable conversion between the two screening questionnaires using equipercentile equating and log-linear smoothing was established.
This study developed a conversion score between the KDSQ and the IQCODE and provided a table of conversion scores that enables the widely recognized scores of the KDSQ to be reliably compared with scores on the IQCODE. Equating scores as well as the averages, medians, and ranges for these two measures provides a straightforward way of comparing the KDSQ to the IQCODE, thus allowing for continuity in cognitive tracking.
The limitations of this study include that it applied to Korean people and that the participants were not representative of the entire population, as they were only people who visited clinics. Participants with subjective cognitive impairment (SCI) might have been recruited as control. Neither dementia subtypes nor MCI subtypes were specifically examined. In this study, the lowest raw score for the IQCODE was 3.00 points. Originally, the score of IQCODE ranged from 1.00 points to 5.00 points.6,7 Because all the participants in this study were older adults, and the IQCODE compares their present cognitive and functional performances with those of 10 years ago, all the subjects did not answer with “much improved” or “a bit improved” (1–2 points) but instead answered from the choices “not much change” to “much worse” (3–5 points). Therefore, it should be taken into account that the range of IQCODE scores may be different in older adults.
Conclusion
This study reported that the KDSQ and the IQCODE have high agreement when used to assess older adults. This study derived a conversion rule using equipercentile equating and log-linear smoothing. It showed that scores of these commonly used cognitive tools can be converted; this could help standardize the assessment of cognitive function. The results of this study can facilitate the comparison and synthesis of cognitive data from international, multicenter, or longitudinal studies.
Acknowledgments
This study was supported by the Korea University Research Fund. The abstract of the preliminary results was presented at the Alzheimer’s Association International Conference 2018 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Alzheimer’s & Dementia titled “Relationship between the Korean Dementia Screening Questionnaire and the Information Questionnaire on Cognitive Decline in the elderly” Hyperlink with https://doi.org/10.1016/j.jalz.2018.06.336.
Ethics
As stated in the manuscript, this retrospective study was conducted with institutional review board approval of Korea University Ansan Hospital. Our institutional review board provided a waiver of informed consent; as this was a retrospective review, all participant records/information were anonymized and de-identified prior to analysis, the waiver is not inconsistent with national law, the research involves no more than minimal risk to the participants, the research could not practicably be carried out without the waiver or alteration, and the waiver or alteration will not adversely affect the rights and welfare of the participants. No data in this paper reveal the identity of the participants.
Author contributions
All authors contributed toward data analysis and drafting and revision of the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M. World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs Now and in the Future. London, UK: Alzheimer’s Disease International (ADI); 2016. [Google Scholar]
- 2.Nam HJ, Hwang SH, Kim YJ, Kim KW. Korean Dementia Observatory 2018. Seoul, Korea: National Institute of Dementia; 2018. [Google Scholar]
- 3.Lee SJ, Han JH, Hwang JW, Paik JW, Han C, Park MH. Screening for normal cognition, mild cognitive impairment, and dementia with the Korean dementia screening questionnaire. Psychiatry Investig. 2018;15(4):384–389. doi: 10.30773/pi.2017.08.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aisen PS, Cummings J, Jack CR Jr., et al. On the path to 2025: understanding the Alzheimer’s disease continuum. Alzheimers Res Ther. 2017;9(1):60. doi: 10.1186/s13195-017-0283-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frisoni GB, Boccardi M, Barkhof F, et al. Strategic roadmap for an early diagnosis of Alzheimer’s disease based on biomarkers. Lancet Neurol. 2017;16(8):661–676. doi: 10.1016/S1474-4422(17)30159-X [DOI] [PubMed] [Google Scholar]
- 6.Jorm AF, Korten AE. Assessment of cognitive decline in the elderly by informant interview. Br J Psychiatry. 1988;152:209–213. doi: 10.1192/bjp.152.2.209 [DOI] [PubMed] [Google Scholar]
- 7.Jorm AF. The informant questionnaire on cognitive decline in the elderly (IQCODE): a review. Int Psychogeriatr. 2004;16(3):275–293. doi: 10.1017/S1041610204000390 [DOI] [PubMed] [Google Scholar]
- 8.Rosli R, Tan MP, Gray WK, Subramanian P, Chin AV. Cognitive assessment tools in Asia: a systematic review. Int Psychogeriatr. 2016;28(2):189–210. doi: 10.1017/S1041610215001635 [DOI] [PubMed] [Google Scholar]
- 9.Yong TT, Choong TYO, Silva E, Guevarra ACD, Lim L, Kandiah N. Long-term outcomes of a multi-domain cognitive intervention among Asian patients with mild dementia [abstract]. Alzheimers Dement. 2017;13(7):614–615. doi: 10.1016/j.jalz.2017.06.675 [DOI] [Google Scholar]
- 10.Yang DW, Cho B, Chey JY, Kim SY, Kim BS. The development and validation of Korean Dementia Screening Questionnaire (KDSQ). J Korean Neurol Assoc. 2002;20(2):135–141. [Google Scholar]
- 11.Shin MH, Lee YM, Park JM, et al. A combination of the korean version of the mini-mental state examination and korean dementia screening questionnaire is a good screening tool for dementia in the elderly. Psychiatry Investig. 2011;8(4):348–353. doi: 10.4306/pi.2011.8.4.348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HS, Shin DW, Lee WC, Kim YT, Cho B. National screening program for transitional ages in Korea: a new screening for strengthening primary prevention and follow-up care. J Korean Med Sci. 2012;27(Suppl):S70–S75. doi: 10.3346/jkms.2012.27.S.S70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment–beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med. 2004;256(3):240–246. doi: 10.1111/jim.2004.256.issue-3 [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders- Fourth Edition, Text Revision. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- 15.Lee DW, Lee JY, Ryu SG, et al. Validity of the Korean version of Informant Questionnaire on the Cognitive Decline in the Elderly (IQCODE). J Korean Geriatr Soc. 2005;9(3):196–202. [Google Scholar]
- 16.Han C, Jo SA, Jo I, Kim E, Park MH, Kang Y. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008;47(3):302–310. doi: 10.1016/j.archger.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 17.Choi SH, Na DL, Lee BH, et al. Estimating the validity of the Korean version of expanded Clinical Dementia Rating (CDR) scale. J Korean Neurol Assoc. 2001;19(6):585–591. [Google Scholar]
- 18.Jung IK, Kwak DI, Shin DK, Lee MS, Lee HS, Kim JY. A reliability and validity study of geriatric depression Scale. J Korean Neuropsychiatr Assoc. 1997;36(1):103–112. [Google Scholar]
- 19.Lee JH, Lee KU, Lee DY, et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):47–53. doi: 10.1093/geronb/57.1.P47 [DOI] [PubMed] [Google Scholar]
- 20.Albano AD. equate: an R package for observed-score linking and equating. J Stat Softw. 2016;74(8):1–36. doi: 10.18637/jss.v074.i08 [DOI] [Google Scholar]
- 21.Kolen MJ, Brennan RL. Test Equating, Scaling, and Linking: Methods and Practices. Berlin, Germany: Springer Science & Business Media; 2014. [Google Scholar]
- 22.Fong TG, Fearing MA, Jones RN, et al. Telephone interview for cognitive status: creating a crosswalk with the mini-mental state examination. Alzheimers Dement. 2009;5(6):492–497. doi: 10.1016/j.jalz.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lawton M, Kasten M, May MT, et al. Validation of conversion between mini-mental state examination and montreal cognitive assessment. Mov Disord. 2016;31(4):593–596. doi: 10.1002/mds.26498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roalf DR, Moberg PJ, Xie SX, Wolk DA, Moelter ST, Arnold SE. Comparative accuracies of two common screening instruments for classification of Alzheimer’s disease, mild cognitive impairment, and healthy aging. Alzheimers Dement. 2013;9(5):529–537. doi: 10.1016/j.jalz.2012.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roalf DR, Moore TM, Mechanic-Hamilton D, et al. Bridging cognitive screening tests in neurologic disorders: a crosswalk between the short montreal cognitive assessment and mini-mental state examination. Alzheimers Dement. 2017;13(8):947–952. doi: 10.1016/j.jalz.2017.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saczynski JS, Inouye SK, Guess J, et al. The montreal cognitive assessment: creating a crosswalk with the mini-mental state examination. J Am Geriatr Soc. 2015;63(11):2370–2374. doi: 10.1111/jgs.13710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trzepacz PT, Hochstetler H, Wang S, Walker B, Saykin AJ. Alzheimer’s disease neuroimaging initiative. relationship between the montreal cognitive assessment and mini-mental state examination for assessment of mild cognitive impairment in older adults. BMC Geriatr. 2015;15:107. doi: 10.1186/s12877-015-0103-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Steenoven I, Aarsland D, Hurtig H, et al. Conversion between mini-mental state examination, montreal cognitive assessment, and dementia rating scale-2 scores in Parkinson’s disease. Mov Disord. 2014;29(14):1809–1815. doi: 10.1002/mds.v29.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cordell CB, Borson S, Boustani M, et al. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the medicare annual wellness visit in a primary care setting. Alzheimers Dement. 2013;9(2):141–150. doi: 10.1016/j.jalz.2012.09.011 [DOI] [PubMed] [Google Scholar]
- 30.Ku BD, Kim SG, Lee JY, et al. Clinical practice guideline for dementia by clinical research center for dementia of South Korea. J Korean Med Assoc. 2011;54(8):861–875. doi: 10.5124/jkma.2011.54.8.861 [DOI] [Google Scholar]