Successful intervention in rural opioid misuse requires a better understanding of how local social norms and networks, and employment and medical care access, combine to facilitate or hinder individual use.
Keywords: Opioid, Rural, Stigma, Social norms, Social networks
Abstract
Prescription and illicit opioids were involved in over 42,000 deaths in the USA in 2016. Rural counties experience higher rates of opioid prescribing and, although opioid prescribing rates have fallen in recent years, the rate of decline is less in rural areas. The sociocultural context of rural life may impact opioid misuse in important ways; however, little research directly explores this possibility. We performed a systematic review of English-language manuscripts in U.S. context to determine what is known about social networks, norms, and stigma in relation to rural opioid misuse. Of nine articles identified and reviewed, two had only primary findings associated with social networks, norms, or stigma, five had only secondary findings, and two had both primary and secondary findings. The normalization of prescription opioid use along with environmental factors likely impacts the prevalence of opioid misuse in rural communities. Discordant findings exist regarding the extent to which social networks facilitate or protect against nonmedical opioid use. Lastly, isolation, lack of treatment options, social norms, and stigma create barriers to substance use treatment for rural residents. Although we were able to identify important themes across multiple studies, discordant findings exist and, in some cases, findings rely on single studies. The paucity of research examining the role of social networks, norms, and stigma in relation to nonmedical opioid use in rural communities is evident in this review. Scholarship aimed at exploring the relationship and impact of rurality on nonmedical opioid use is warranted.
Implications.
Practice: Addressing the opioid epidemic in rural areas will require discussions and collaborations with drug misusers to ensure that needed services are made available in a fashion that ensures anonymity and does not exacerbate stigma.
Policy: Community leaders and stakeholders should work to change the community narrative regarding drug use to one that is more accommodating to the needs of people seeking help with addiction.
Research: Further work should examine means to both evaluate, describe, and mold community norms and stigmatizing behaviors as well as increasing the resilience of those who are stigmatized.
INTRODUCTION
According to the Centers for Disease Control and Prevention (CDC), prescription and nonprescription opioids were involved in over 42,000 deaths in 2016 [1]. As early as 2008, data from the CDC demonstrated that rural counties (frequently impoverished) experienced higher rates of opioid prescribing, and prescription opioid overdose death, as compared to urban counties [2]. While overall opioid prescribing rates have fallen in recent years due to new guidelines, publicity, and other factors, the rate of decline is less in rural areas [3]. Prescribing patterns are important, as multiple studies find strong associations between initial prescription use and transition to nonmedical use (e.g., taking opioids in a manner or dose other than prescribed or to feel euphoria) and heroin use [4]. Once heroin use begins, research demonstrates quick transitions from ingestion/snorting/smoking to injection as tolerance increases, though the same scenario applies to prescription medication such as Oxycontin [4–7]. This change to injection use is associated with increased likelihood of disease transmission as individuals share needles and equipment and contributes to a heightened risk of hepatitis C virus (HCV) and human immunodeficiency virus (HIV) infection [3,8,9].
The risk of injection-associated disease transmission may be greater in rural communities. Such areas have fewer screening and treatment resources in general, and more recent years have seen reductions in funding for sexually transmitted infection intervention and HIV screening [10–12]. The CDC and others have reported increased rates of HIV/HCV contraction and transmission in multiple rural areas attributed to injection risk behaviors associated with opioid use [13–18]. For example, acute HCV infection among those aged 30 years and younger in Kentucky, Tennessee, Virginia, and West Virginia increased by 364% from 2006 to 2012, with the rate of infection in rural areas nearly double that of urban communities, the authors linking this increase to injection opioid use [19]. Still, outright screening and resource increases may not adequately address the problem.
Rurality and social networks
There are multiple ways to conceptualize social networks and their relationship to drug use. Bohnert et al. explored social influence and social selection in relation to the use of cocaine and heroin [20]. Social influence suggests that observed substance use by network members leads to changes in use among network members [21]. Thus, one’s actions become more similar to that of their peers [22]. Social selection suggests that one actively seeks out individuals exhibiting their own behavior [21]. The Bohnert study found that, while more drug use change was associated with network changes (i.e., social selection), there was also some influence observed among existing network members (i.e., social influence) [20].
Thus, the structure of social networks, influenced by larger cultural norms, transportation patterns, and geography, likely impact substance use patterns in rural communities [9,17,23–26]. In the case of opioid initiation, specifically, Keyes et al. assert that a main source of nonmedical prescription opioids is through kinship and friendship networks [25]. As such, strong social bonds within these networks may make the proliferation of illicit opioid use possible via influence. Moreover, because social ties in rural communities are often large and dense, due to large family structures and role multiplexity, the diffusion process of illicit prescription opioids may happen more quickly than in urban areas [25]. This circumstance may not be uniform, however, as other work suggests that such strong and large social ties and networks in rural areas may actually guard against substance use, as there is greater capacity to communally shoulder the stress of financial struggles or other stressors [27]. Overall, social networks may be disproportionately influential in nonmedical opioid use in rural communities, but the nature of that influence and how it in turn might be influenced requires further examination.
Rurality, stigma, and social norms
While networks are important diffusers of information and influence, and provide intracommunity social ties, they also exist within the context of local stigma and norms. Stigma was first conceptualized by Erving Goffman and further expanded by Link and Phelan [28,29]. Link and Phelan define stigma as having four interconnected and often co-occurring modalities: labeling, stereotyping, separation, status loss, and discrimination [29]. Labeling differences among people and attaching various negative stereotypes to these differences makes it possible to assert and justify the notion that the negatively labeled individuals are decidedly different from others who are not labeled as such. In this way, labels and negative stereotyping necessitates the differentiation of “us” from “them,” which lends itself to separation, status loss, and discrimination against the labeled group [29].
As loss of status reduces the power of the stigmatized group, relative to broader society, social stigma extends beyond patterns of labeling to have real consequences in terms of how individuals can lead their lives [28,29]. People who misuse opioids likely face direct and structural discrimination as a result of their stigmatized status, which can impact access to housing, health care, treatment, and other domains of life [29]. Importantly, cultural stereotypes are learned early in life, meaning those who use opioids nonmedically are likely aware of dominant beliefs and assumptions surrounding those who struggle with substance use disorder [29]. As such, stigma, or the fear of being stereotyped, may be internalized as those who misuse opioids expect to be treated poorly or rejected by society [29]. According to Link and Phelan, the effects of such internalized stigma or fear of being stereotyped may manifest in diminished self-esteem, unemployment and income loss, further isolation, and a generally lower quality of life [28].
In the context of nonmedical opioid use, rurality and stigma are leading barriers to prevention and treatment of HIV among people who inject opioids [14]. Stigma associated with nonmedical opioid use, particularly injection delivery, may be exacerbated in rural contexts where anonymity may be more difficult to ensure. An “us versus them” context could perpetuate nonmedical opioid use as these peer groups bond over their mutual dislocation from society, creating durable and intense social ties. In these ways, perceived and enacted stigma may be a significant barrier to treatment and recovery for those who use opioids nonmedically [30,31]. Stigma against nonmedical opioid use may be operationalized at the community level by limited availability and use of disease prevention resources (e.g., syringe exchange programs), overdose antidotes (e.g., Naloxone), and treatment services (e.g., behavioral counseling) [30].
Given the concept of social networks, and the thought that such networks in rural communities might be both fewer in number and include greater proportions of residents “where everyone knows everyone,” social norms and stigma may have strong impacts regarding addressing nonmedical opioid use. A substantial body of research suggests that rural social norms may significantly differ from urban cultural norms [23,32–35].
The case of Scott County, Indiana
The oft-referenced outbreak of HIV in Scott County, IN, highlights many of these concepts. In 2014–2015, large networks of individuals sharing needles and injecting Opana resulted in 181+ cases of HIV [34]. Scott County is a rural community, and reports find that social networks of injection drug users were particularly large and dense, often characterized by sharing of needles and injection equipment [34]. Resources, stigma, and norms all come into play here, as modeling suggests that a more robust response—including disease screening and treatment, syringe exchange, and partner outreach—could have lessened the scale of the outbreak [36]. This, of course, would have necessitated availability of screening and treatment and social support for such (reduced stigma) so that those in need can access these services. Risky injection behaviors were significantly reduced upon implementation of a syringe exchange program, and program success and utilization is greatly facilitated by the social influence of the first few who accessed it [37]. A review of HIV outbreaks among those who inject drugs (including Scott County) concludes that many methods of preventing/limiting future outbreaks will have limited effectiveness unless drug use-associated stigma is reduced to facilitate individuals accessing syringe exchange and disease screening and treatment programs [38].
While HIV, and to some extent HCV, are already stigmatized infections, individuals located at the intersection of injection drug use, HIV, and HCV diagnosis may experience compounding social stigma that further deters prevention and treatment. As rural communities continue to be significantly impacted by nonmedical opioid use, research aimed at disentangling the effects of social norms, networks, and stigma on opioid use in the rural context must be identified and extended [3]. Our objective in the present analysis is to systematically review the peer-reviewed literature regarding the dynamics of nonmedical opioid use, social networks and norms, and stigma in rural locales to identify places where further scholarship is warranted.
METHODS
Articles were considered for review if they met the following criteria: provided new, primary data; written in English language; peer-reviewed; U.S. context; and explored rural opioid use with attention to social networks, cultural norms and acceptance, or stigma. Primary data for this review could be reported as primary (e.g., main outcomes) or secondary findings (i.e., other, nonmain outcomes) for included studies. Editorials and articles discussing summary or other nonprimary data were not included.
We searched EbscoHost (Academic Search Premier, CINAHL, MEDLINE, PsychINFO, and SocINDEX) and PubMed using the following strategies:
- Strategy 1:
- term 1a = TITLE/ABSTRACT “opioid” OR “heroin”;
- term 1b = TITLE/ABSTRACT “rural”; and
- term 1c = ANY TEXT “social networks” OR “social norms” OR “norms” OR “stigma.”
- Strategy 2 (using selected medical subject heading terms):
- term 2a = TITLE/ABSTRACT “opioid” OR “addiction/opiate” OR “heroin abuse”;
- term 2b = TITLE/ABSTRACT “rural population”; and
- term 2c = TITLE/ABSTRACT “social networks.”
Retrieved articles’ bibliographies were examined for additional manuscripts not otherwise identified. Study abstracts retrieved by the search were reviewed (R.B., K.E., W.Z., and W.D.J.) and eligibility was determined by consensus.
We extracted the following data from each article, as available: years performed; study location and design; number and type of participants; study objective; study results; and limitations. Further, the 10-item risk of bias tool was utilized to assess and rate each study [39]. Values range from highest risk of bias (1) to lowest (10). The authors examined all primary and secondary findings to identify any themes, that is, similar results or findings across at least three studies.
RESULTS
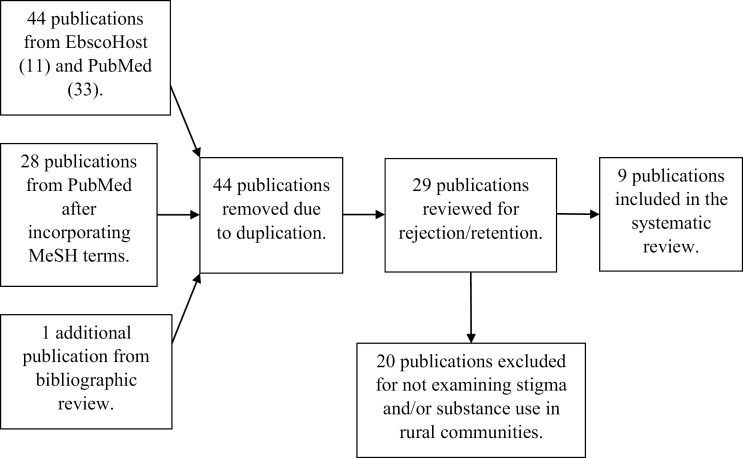
The literature search returned 73 manuscripts (11 from EbscoHost, 33 from PubMed, 28 from PubMed using medical subject heading terms, and 1 additional publication from bibliographic review; Fig. 1). We removed 44 publications due to duplication. The remaining 29 manuscripts were reviewed by the authors (R.B., K.E., W.Z., and W.D.J.) for inclusion based on study criterion and rejection/retention determined by consensus. Nine studies were identified as analyzing opioid use, social networks, norms, and stigma in rural communities. Studies included in this review varied in years conducted but were spatially quite close. For example, seven manuscripts were from Kentucky (five from a single large study) and another from Ohio. While the objectives and results of each study differed, similar themes emerged (Table 1).
Figure 1 .
Article identification, review, and retention flowchart.
Table 1.
Manuscripts identified from the systematic reviewa
| Authors | Year(s), conducted location |
Number and type of participants |
Study design | Study outcome measure | Primary findings | Secondary findings | Risk of bias score |
|---|---|---|---|---|---|---|---|
| Draus and Carlson (2006)[42] | 2002–2004, rural Ohio |
25 people who recently injected heroin | Qualitative interviews and focus groups | Describe situational factors that contribute to initiation of heroin injection | • Most initiations facilitated by predominantly male friends or family • Sometimes traumatic events precipitated initiation • Often curiosity outweighed fear of negative outcomes • Transition from snorting to injecting heroin facilitated by economic constraints and growing dependency |
5 | |
| Havens et al. (2011)[43] | 2010, Appalachian Kentucky |
400 people who use drugs | Respondent-driven sampling survey | Prevalence of nonfatal and witnessed overdose | • Almost one-third of participants had experienced a nonfatal overdose • Almost 60% had witnessed an overdose |
• Larger support network significantly associated with more nonfatal overdoses • Larger support networks and outdegree centrality strongly associated with witnessed overdose |
6 |
| Havens et al. (2013)[44] | 2008–2010, Appalachian Kentucky |
392 people who inject drugs | Respondent-driven sampling survey | HCV Prevalence among rural people who inject drugs | • Over half of rural people who inject drugs tested positive for HCV • Greater network connectivity was associated with increased HCV infection risk |
• Longer duration of injection and syringe sharing correlated with HCV infection • Diagnostic and statistical manual of mental disorders-IV criteria for post-traumatic stress disorder decreased risk • Cocaine injectors more central to drug networks than opioid injectors |
5 |
| Jonas et al. (2012)[41] | 2008–2010, Appalachian Kentucky |
503 people who use drugs | Respondent-driven sampling survey | Substance use and social/drug use networks | • Daily OxyContin use was found to be significantly associated with greater social capital and daily marijuana use was associated with less social capital. | 5 | |
| Leukefeld et al. (2007)[40] | 2004–2005, two counties in Appalachian Kentucky |
70 community leaders, educators, health care providers, law enforcement, or justice personnel | Snowball sampling and qualitative interviews | Perceptions and opinions about drug abuse, sources of drugs, rationale for misuse, and solutions | • Medicaid and elderly patients often sell prescriptions to supplement income • Selling prescription drugs replacing growing marijuana • All groups identified misuse/nonprescription use as a long standing and cultural problem |
• Most informants learned about or experienced prescription drugs through family or friends who misused them • Two most common cited pathways to misuse are physical pain and recreational misuse • Lack of employment opportunities and need to escape as reasons for drug misuse |
4 |
| Monnat and Rigg (2016)[46] | 2011–2012, USA |
32,036 adolescents aged 12–17 | Secondary data analysis using a nationally representative survey | Past-year prescription opioid misuse (POM) | • Rural adolescents have 35% greater odds of past-year POM than large urban adolescents | • Criminal behavior, lower perceived substance use risk, and past-year emergency department treatment positive mediators of POM and more likely among rural adolescents • Past-year major depressive episode, peer substance use, lower importance of religious beliefs, and drug access are positive mediators of POM and less likely among rural adolescents |
10 |
| Oser and Harp (2015)[48] | 2010–2012, Kentucky |
187 drug treatment clients who misused prescription drugs | Survey and qualitative interviews | Geographical discordance between treatment county and home county | • Rural participants more likely to receive treatment outside home county • Geographical discordance significantly predicted relapse of POM |
• Rural clients more likely than urban clients to report past-year incarceration at baseline • Geographic discordance linked to anxiety and increased odds of incarceration • Clients who experienced geographic discordance less likely to report self-help group attendance at follow up |
5 |
| Smith et al. (2017)[47] | Appalachian Kentucky | 503 people who use drugs | Respondent-driven sampling survey | Lifetime antisocial personality disorder (ASPD) in active drug users | • One-third of participants met Diagnostic and statistical manual of mental disorders-IV ASPD criteria | • Participants reporting higher average trust in social support network had reduced odds of meeting ASPD criteria • Every additional network member reported as “not on good terms with” increased odds of meeting ASPD criteria by 33% • Daily communication or living close to more people was associated with higher odds of meeting ASPD criteria |
5 |
| Young et al. (2013) [45] | 2008–2010, Appalachian Kentucky |
436 people who use opioids nonmedically | Respondent-driven sampling survey | RNA homophily within drug network | • Significant homophily value for drug networks • Individuals who are HCV RNA positive are more likely to be tied to each other in the network of drug relationships than would be expected at random |
• HCV RNA positive individuals had higher egocentric drug network density and less turnover into networks | 6 |
aRisk of bias 10-item tool was utilized to rate articles. Values range from highest risk of bias (1) to lowest risk (10).
Of the nine studies retained, two had only primary finding associated with social networks, norms, or stigma (ref #21 and 42), five had only secondary findings (ref #40, 43, 45–47), and two had both primary and secondary findings (ref #44 and 48). Primary findings were determined as associated with each study’s main outcomes and secondary those also reported. The risk of bias scores ranged from 4 to 6 for eight studies, but one study scored a 10 (ref #46). We identified three thematic areas addressed through multiple studies and other singular findings that warrant further investigation.
Findings suggest that rural environmental factors facilitate nonmedical opioid use as dominant industry in rural spaces is labor intensive, often resulting in increased cases of chronic pain among workers. Moreover, a review of the literature indicates that rural social norms impact opioid use in various ways, including that social capital, in the form of resources and popularity among network members, may be gained from daily OxyContin use. Additionally, rural networks (social and drug use) are associated with increased opioid use and adverse outcomes such as overdose and infection. Lastly, findings illustrate that the geographical reality and social context of rural opioid use limit access to effective treatment.
Environmental impact on opioid use
Rural residents in one of the studies described a widespread, longstanding acceptance of opioid use as contributing to the nonmedical use of prescription opioids [40]. One reason prescription opioid use, particularly OxyContin, is widely accepted in rural spaces could be the due to the context of rural life, where coal miners and other laborers rely on pain medication to continue production [41]. As such, the normalization of prescription opioid use may impact the proliferation of nonmedical opioid use across rural residents.
Social networks in rural localities
Lack of entertainment and excitement, and higher proportions of jobs resulting in personal injury and pain, in rural areas may be a “driving factor” for rural use; however, a complementary “drawing factor” may be social capital, defined as access to various resources and the ability to span structural holes within a social network, gained through daily OxyContin use [41,42]. Indeed, Jonas et al. found that social norms regarding drug use, coupled with the lack of local economic opportunities, provided individuals an opportunity to gain social capital through OxyContin use [41]. Those who reported daily OxyContin use tended to be popular among their peers and often occupied central locations within social networks.
Social networks proved to be important for making sense of initiation into injection use in Draus and Carlson’s study as they found that 80% of the participants were initiated into injection use by a friend or family member [42]. Furthermore, the participants reported that fear associated with injection risk was mitigated by peer testimony regarding pain and physiological effects [42]. As such, the participants reported that they trusted their friends and/or family members who were injecting heroin to initiate them into injecting and they reported a general sense that “everyone was doing it,” thus normalizing injecting behaviors [42]. Although these findings may not be specific to rural spaces, scholarship exploring social networks of rural people who use drugs is sparse; therefore, further research is needed to offer a comprehensive understanding of rural social networks as the social context of rurality likely results in important variations from conceptualizations of urban social networks.
Network size, position, and density are associated with injection risk factors. Havens et al. found that larger networks (support, sexual, and drug use) and network eigenvector centrality (the extent to which one network member is connected to other members who are connected to additional people who use illicit substances) were significantly associated with higher numbers of nonfatal overdoses and greater likelihood of witnessing an overdose [43]. In addition, Havens et al. found that rural participants with greater network centrality were more likely to be HCV positive [44]. Social network importance is reflected in the testimony that “the major source of syringes are family members or friends” [44]. Similarly, Young et al. found that those who were HCV positive had significantly higher egocentric drug network density [45].
The data do not uniformly describe negative findings or outcomes regarding rural populations and pathways to drug use; in fact, there are areas where protective factors exert greater influence. For example, data indicate that some rural adolescents enjoy some, at least partial, barriers to initiation into nonmedical opioid use such as less peer use, less access to illicit drugs, and stronger religious beliefs [46]. Social networks were also shown to be important in terms of lifetime antisocial personality disorder (ASPD) among rural individuals experiencing substance use disorder, and that greater trust of network members was associated with lower odds of ASPD, though directionality is unclear [47]. Network influence for infection risk is not definitive, as the data indicate that turnover into one’s social network was negatively associated with HCV infection, indicating purposeful serosorting (where individuals seek out others of similar infection status) [45].
Barriers to substance use treatment
Although there are multiple rural-specific factors contributing to use, there are similar factors hindering effective treatment and recovery. For example, rural residents more frequently travel to a county with a different sociocultural context, that is, a more metropolitan locale, for treatment [48]. This geographic discordance is important as those needing such travel (vs. those traveling between concordant areas) are more likely to experience a relapse, more likely to become incarcerated, and less likely to attend self-help groups in the past month [48]. Social norms relating to community strength and resilience in rural contexts, along with social stigma, create barriers to accessing treatment [48]. Furthermore, people in rural communities are more likely to meet the criteria for comorbid substance use disorders and mental illness, which may lead to compounding stigma, making treatment more difficult to access [47]. Finally, rural residents may view substance use as less risky than their urban peers, perhaps lessening motivation to seek treatment [46].
DISCUSSION
In this systematic review of rural opioid use, we found little research and data explicitly examining the role of social norms and stigma relating to nonmedical opioid use in rural communities. Furthermore, almost all of these studies focused on nonmedical opioid use in Kentucky, and a majority were from the same study of the mountain areas of East Kentucky. Thus, a primary finding of this review is that there has been very little attention paid to these issues outside of Kentucky, and more variation is needed. An initial exploration of community stigma associated with nonmedical opioid use found no reported work and, by expanding our search to include aspects of social networks and risk factors, we were able to identify nine articles. From these, we were able to identify three themes across multiple studies, indicating that: rural environmental factors facilitate nonmedical opioid use; there are multiple aspects of social norms and social capital that support nonmedical opioid use and networks (social and drug use) in rural areas have increased association with opioid use and adverse outcomes such as overdose and infection; and the geographical and social context of rural opioid use is a barrier to effective treatment.
Dominant industry requiring intense manual labor in rural spaces likely impacts social norms surrounding opioid use as workers seek medication for pain management in order to continue production [40]. The widespread acceptance of opioid use for pain management may lend itself to the facilitation of nonmedical use as individuals begin to take opioids outside of prescribed parameters. Additionally, prescribed opioids may be diverted and subsequently used nonmedically as rural residents look for ways to supplement their income through the sale of culturally valuable pills [40,41]. Indeed, findings suggest that OxyContin use is related to increased social capital and greater network centrality among social network members [41]. Further, network centrality and social capital may well differ by specific drug type used [42,44]. This may have implications given high prevalence of polysubstance use, which could complicate network-based interventions and analyses.
Furthermore, rural social networks are important for understanding the proliferation of injection drug use as findings indicate that initiation into injection use took place primarily through friends and family [42]. This finding may not be specific to rural spaces; however, existing scholarship illustrates that rural life and culture is markedly different from the metropolitan case. Therefore, future research should examine rural social networks of people who use drugs to identify the ways in which these relations operate in particular ways to promote and/or protect against nonmedical opioid use. Additionally, making sense of rural networks (social and drug use) may lend itself to best practices related to implementation of harm reduction and treatment services, particularly as the Scott County case illustrated the importance of social influence in accessing such services [34]. In fact, our review demonstrates discordant findings related to the role of rural social networks in nonmedical opioid use as some indicate that rural networks may in some circumstances be protective of opioid use initiation and lead to reduction of some outcomes (e.g., reduce the risk of infection and mental illness) [46,47].
Moreover, rural social norms that highly value community strength and resilience, coupled with social stigma and lack of access to treatment facilities in rural spaces, impede opportunities for effective recovery [48]. Future research that explores the role of rural social norms on nonmedical opioid use has the potential to uncover intervention strategies that are culturally appropriate and work to decrease social stigma and increase education and community buy-in for important prevention and treatment services. Indeed, important work related to accessibility of and referral to PrEP through Telehealth illustrates that such services are effective in the prevention of HIV and treatment of STIs among geographically dispersed rural populations [49]. Given the paucity of data overall, and the reliance of single studies for some results, much work is needed to achieve a level of consistency of rural influences and the local nuances impacting the direction and magnitude of specific factors.
There are limitations to this work. First, the selected manuscripts uniformly did not explicitly examine stigma per se and, while stigma is strongly associated with avoidance of care and adverse personal health, we cannot evaluate how this might be experienced in rural communities. Second is the lack of consistent outcome measures across studies. While we were able to identify common themes (e.g., network characteristics and infection risk), it is difficult to draw firm conclusions on most points due to a single data source. Additionally, drawing comparisons across studies was difficult given the diversity of articles. Further, the data were occasionally contradictory, highlighting the very localized aspects of social networks and norms and that they may substantially vary. Finally, the majority of the data were drawn from Kentucky and Appalachia. It is unknown how such findings may/may not be reflective of other distinct rural areas such as the Deep South, Delta Regional Authority, or the Northwest.
Rural communities represent a minority of the U.S. population but, in many respects, bear a disproportionate burden of the opioid epidemic. The decline of economic opportunity and permissive prescribing patterns have contributed to greater risk for nonmedical opioid use at a system level, and these are perhaps compounded by local level social and cultural influences that condone/encourage drug use and limit opportunities for effective treatment. The lack of data indicates the need for further work to understand the contextual factors influencing nonmedical opioid use in rural communities, how they may/may not be distinct from urban areas, and what factors may be relatively consistent across communities and which are much more locally variable.
Funding: This work was supported by the National Institutes of Health/National Institute on Drug Abuse (1UG3DA044829-01).
Compliance with Ethical Standards
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Authors’ Contributions: RB collected, extracted, and analyzed the data, and developed and revised the manuscript; KE collected, extracted, and analyzed the data, and assisted with manuscript revision; WEZ collected, extracted, and analyzed the data, and assisted with manuscript revision; SW assisted with manuscript development and revision; SM assisted with data analysis and organization, and assisted with manuscript revision; JS guided the bias scoring, and assisted with manuscript development and revision; CR assisted with data organization, and manuscript revision; JE assisted with manuscript development and revision; LO assisted with manuscript development and revision; SF assisted with manuscript development and revision; MP assisted with manuscript development and revision; WDJ contributed to data analysis and organization, and manuscript development.
Ethical Approval: This article does not contain any studies with human participants performed by any of the authors. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: This article does not involve human participants and informed consent was, therefore, not required.
References
- 1. Centers for Disease Control and Prevention (CDC). Opioid overdose Available at https://www.cdc.gov/drugoverdose/index.html. Accessibility verified January 25, 2019.
- 2. CDC. Vital signs: overdoses of prescription opioid pain relievers–-United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 3. CDC. Annual surveillance report of drug-related risks and outcomes, United States 2017. Available at https://www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf. Accessibility verified January 25, 2019.
- 4. Compton WM, Jones CM, Baldwin GT. Nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(13):1296. [DOI] [PubMed] [Google Scholar]
- 5. Grau LE, Dasgupta N, Harvey AP, et al. Illicit use of opioids: is OxyContin a “gateway drug”? Am J Addict. 2007;16(3):166–173. [DOI] [PubMed] [Google Scholar]
- 6. Muhuri PK, Groerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. Available at https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm. Accessibility verified January 25, 2019. [Google Scholar]
- 7. Siegal HA, Carlson RG, Kenne DR, Swora MG. Probable relationship between opioid abuse and heroin use. Am Fam Physician. 2003;67(5):942, 945. [PubMed] [Google Scholar]
- 8. Burnett JC, Broz D, Spiller MW, Wejnert C, Paz-Bailey G. HIV infection and HIV-associated behaviors among persons who inject drugs—20 cities, United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(1):23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Young AM, Havens JR. Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: a cross-sectional comparison and retrospective survival analysis. Addiction. 2012;107(3):587–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Henderson ER, Subramaniam DS, Chen J. Rural-urban differences in human immunodeficiency virus testing among US adults: findings from the behavioral risk factor surveillance system. Sex Transm Dis. 2018;45(12):808–812. [DOI] [PubMed] [Google Scholar]
- 11. National Public Radio. “A Failure Of Public Health.” Sexually transmitted diseases rise as health budgets fall Available at http://www.wkyufm.org/post/failure-public-health-sexually-transmitted-diseases-rise-health-budgets-fall#stream/0. Accessibility verified December 14, 2018.
- 12. Benjamin G, Kizer KW, Pane G, Gimson W, Sofaer S.. The Impact of Sexually Transmitted Diseases on the United States: Still Hidden, Getting Worse, can be Controlled. A Report by a Panel of the National Academy of Public Administration. 2018. Available online at: http://www.ncsddc.org/resource/the-impact-of-sexually-transmitted-diseases-on-the-united-states-still-hidden-getting-worse-can-be-controlled/ [Google Scholar]
- 13. CDC. HIV and injection drug use Available at https://www.cdc.gov/vitalsigns/hiv-drug-use/infographic.html. Accessibility verified January 25, 2019.
- 14. Draus P, Carlson RG. Down on main street: drugs and the small-town vortex. Health Place. 2009;15(1):247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Des Jarlais DC, Nugent A, Solberg A, Feelemyer J, Mermin J, Holtzman D. Syringe service programs for persons who inject drugs in urban, Suburban, and rural areas - united states, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(48):1337–1341. [DOI] [PubMed] [Google Scholar]
- 16. Midgard H, Hajarizadeh B, Cunningham EB, et al. ; ACTIVATE Study Group. Changes in risk behaviours during and following treatment for hepatitis C virus infection among people who inject drugs: the ACTIVATE study. Int J Drug Policy. 2017;47:230–238. [DOI] [PubMed] [Google Scholar]
- 17. Staton M, Ciciurkaite G, Havens J, et al. Correlates of injection drug use among rural Appalachian women. J Rural Health. 2018;34(1):31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stephens DB, Young AM, Havens JR. Healthcare contact and treatment uptake following hepatitis C virus screening and counseling among rural Appalachian people who use drugs. Int J Drug Policy. 2017;47:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zibbell JE, Iqbal K, Patel RC, et al. ; CDC. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- 20. Bohnert AS, Bradshaw CP, Latkin CA. A social network perspective on heroin and cocaine use among adults: evidence of bidirectional influences. Addiction. 2009;104(7):1210–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dohrenwend BP, Levav I, Shrout PE, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255(5047):946–952. [DOI] [PubMed] [Google Scholar]
- 22. Reifman A, Watson WK, McCourt A. Social networks and college drinking: probing processes of social influence and selection. Pers Soc Psychol Bull. 2006;32(6):820–832. [DOI] [PubMed] [Google Scholar]
- 23. Miller MK, Crader KW. Rural-urban differences in two dimension of community satisfaction. Rural Sociol. 1979;44(3):489–504. [Google Scholar]
- 24. Beggs JJ, Haines VA, Hurlbert JS. Revisiting the rural-urban contrast: personal networks in nonmetropolitan and metropolitan settings. Rural Sociol. 1996;61(2):306. [Google Scholar]
- 25. Keyes KM, Cerdá M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Young AM, Havens JR, Leukefeld CG. A comparison of rural and urban nonmedical prescription opioid users’ lifetime and recent drug use. Am J Drug Alcohol Abuse. 2012;38(3):220–227. [DOI] [PubMed] [Google Scholar]
- 27. Dew B, Elifson K, Dozier M. Social and environmental factors and their influence on drug use vulnerability and resiliency in rural populations. J Rural Health. 2007;23 (Suppl):16–21. [DOI] [PubMed] [Google Scholar]
- 28. Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, NY: J. Aronson; 1974. [Google Scholar]
- 29. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363. [Google Scholar]
- 30. Appalachian Regional Commission. Communicating about opioids in Appalachia: challenges, opportunities, and best practices Available at https://www.orau.org/impact/health-communication/opioid-abuse-crisis-in-appalachia.html. Accessibility verified January 25, 2019.
- 31. Corrigan PW, Nieweglowski K. Stigma and the public health agenda for the opioid crisis in America. Int J Drug Policy. 2018;59:44–49. [DOI] [PubMed] [Google Scholar]
- 32. Buttel FH, Flinn WL. Sources and consequences of agrarian values in american society. Rural Sociol. 1975;40(2):134–151. [Google Scholar]
- 33. Miller MK, Luloff AE. Who is rural? A typological approach to the examination of rurality. Rural Sociol. 1981;46(4):608–625. [Google Scholar]
- 34. Peters PJ, Pontones P, Hoover KW, et al. ; Indiana HIV outbreak investigation team. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375(3):229–239. [DOI] [PubMed] [Google Scholar]
- 35. Willits FK, Bealer RC, Crider DM. Leveling of attitudes in mass society: rurality and traditional morality in America. Rural Sociol. 1973;38(1):36–45. [Google Scholar]
- 36. Gonsalves GS, Crawford FW. Dynamics of the HIV outbreak and response in Scott County, IN, USA, 2011-15: a modelling study. Lancet HIV. 2018;5(10):e569–e577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patel MR, Foote C, Duwve J, et al. Reduction of injection-related risk behaviors after emergency implementation of a syringe services program during an HIV outbreak. J Acquir Immune Defic Syndr. 2018;77(4):373–382. [DOI] [PubMed] [Google Scholar]
- 38. Des Jarlais DC, Kerr T, Carrieri P, Feelemyer J, Arasteh K. HIV infection among persons who inject drugs: ending old epidemics and addressing new outbreaks. AIDS. 2016;30(6):815–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. [DOI] [PubMed] [Google Scholar]
- 40. Leukefeld C, Walker R, Havens J, Tolbert V. What does the community say: key informant perceptions of rural prescription drug use. United States. J Drug Is. 2007;37(3):503–524. [Google Scholar]
- 41. Jonas AB, Young AM, Oser CB, Leukefeld CG, Havens JR. OxyContin as currency: oxyContin use and increased social capital among rural Appalachian drug users. Soc Sci Med. 2012;74(10):1602–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Draus PJ, Carlson RG. Needles in the haystacks: the social context of initiation to heroin injection in rural Ohio. Subst Use Misuse. 2006;41(8):1111–1124. [DOI] [PubMed] [Google Scholar]
- 43. Havens JR, Oser CB, Knudsen HK, et al. Individual and network factors associated with non-fatal overdose among rural Appalachian drug users. Drug Alcohol Depend. 2011;115(1–2):107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Havens JR, Lofwall MR, Frost SD, Oser CB, Leukefeld CG, Crosby RA. Individual and network factors associated with prevalent hepatitis C infection among rural Appalachian injection drug users. Am J Public Health. 2013;103(1):e44–e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Young AM, Jonas AB, Havens JR. Social networks and HCV viraemia in anti-HCV-positive rural drug users. Epidemiol Infect. 2013;141(2):402–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health. 2016;32(2):204–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Smith RV, Young AM, Mullins UL, Havens JR. Individual and network correlates of antisocial personality disorder among rural nonmedical prescription opioid users. J Rural Health. 2017;33(2):198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Oser CB, Harp KL. Treatment outcomes for prescription drug misusers: the negative effect of geographic discordance. J Subst Abuse Treat. 2015;48(1):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hoth AB, Shafer C, Dillon DB, Mayer R, Walton G, Ohl ME. Iowa TelePrEP: a public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state. Sex Transm Dis. 2019;46(8):507–512. [DOI] [PubMed] [Google Scholar]