Among Latino day laborers at risk for unhealthy alcohol use, those who received a culturally adapted brief intervention did not reduce their alcohol use more than those not receiving the brief intervention.
Keywords: Screening and brief intervention, Latino, Cultural adaptation, Alcohol use
Abstract
Latino immigrant men are at increased risk for unhealthy alcohol use. Vida PURA is a culturally adapted evidence-based intervention that consists of promotores providing screening and brief intervention to reduce unhealthy alcohol use among Latino immigrant men. The purpose was to assess the efficacy of Vida PURA in a pilot randomized control trial. Participants were screened for eligibility at a day labor worker center using the Alcohol Use Disorders Identification Test (AUDIT). Those with an AUDIT score ≥ 6 (N = 121) were randomized into an intervention (N = 77) or control group (N = 44). Participants in the intervention group received a brief intervention from a promotor including personalized feedback, motivational interviewing to assess their readiness to change, and referral to services. Participants in the control group received information about local substance use treatment services. We assessed changes in AUDIT scores, drinks per drinking day, drinking days, and frequency of heavy episodic drinking at 2 and 8 weeks following the baseline survey using a mixed-effects regression model. Many men had high AUDIT scores, indicating dependence. Both the intervention and control groups reduced their alcohol-related behaviors over time, but there were no significant differences between the groups. A culturally adapted brief intervention may not be enough to significantly reduce alcohol use among Latino day laborers, especially among those that are dependent. We discuss lessons learned from this trial, including the value of community-based approaches to reaching high-risk and underserved populations.
Implications.
Practice: Screening and brief intervention to reduce unhealthy alcohol use can reach high-risk underserved populations when implemented in community settings.
Policy: Latino immigrant men seeking day labor employment are at increased risk for unhealthy alcohol use, yet lack access to effective low-cost alcohol treatment options.
Research: Future studies should identify effective culturally appropriate community-based strategies to reducing unhealthy alcohol use among high-risk Latino immigrant men.
INTRODUCTION
After arriving in the USA, Latino immigrants face many stressors associated with immigration, such as poverty, undocumented immigration status, language barriers, and social isolation [1,2]. Exposure to these stressors can result in the adoption of avoidant coping strategies, such as unhealthy drinking [3–6]. Latino men are, in fact, more likely to engage in unhealthy drinking than Latina women and men in other racial/ethnic groups [7–9]. Unhealthy drinking among Latino men also increases with acculturation and length of residence in the USA [10].
Some Latino immigrant men living in the USA turn to day labor as a source of income. Day labor is a form of contingent nonpermanent employment offering limited job security, where workers are hired and paid 1 day at a time for physically strenuous labor. Workers seek employment on street corners and through worker centers that match workers with jobs [11]. They often have low socio-economic status and undocumented immigration [11]. This economic and social context compounds Latino day laborers’ risk for unhealthy drinking [1,12–14].
The U.S. Preventive Services Task Force recommends screening and brief intervention (SBI) in primary care for reducing unhealthy drinking among adults [15,16]. Studies evaluating the effectiveness of brief interventions have found that they can be effective among Latinos [17–20]. However, their reach is limited when offered only in clinical settings. Latino day laborers are often hesitant to seek health care in the USA because of the perception that seeking health care may make them vulnerable to deportation and the potential loss of earnings [21,22]. Furthermore, most day laborers lack health insurance and cannot afford the high cost of health care due to their low wages [23–25]. Latino day laborers therefore rarely seek health services, making them unlikely to access alcohol abuse prevention interventions that are offered only in clinical settings [21,26].
Researchers and practitioners have increasingly called for studies to evaluate the efficacy of offering SBI in community settings where high-risk populations are more likely to access them [24,27,28]. SBI may be most effective if the intervention delivery, setting, and content have been culturally adapted for Latino immigrant men [29–31]. Our study assessed the efficacy of culturally adapted screening and brief intervention to reduce unhealthy alcohol use among Latino day laborers in a pilot randomized trial.
MATERIALS AND METHODS
Study design
The Vida PURA (Puede Usted Reducir su consumo de Alcohol), which translates to “Pure Life (You can reduce your alcohol use),” intervention was culturally adapted using an established framework [32]. Cultural adaptations of SBI included: screening in a day labor worker center, using promotores to deliver the brief intervention, and offering referral to low-cost Spanish speaking services [27]. Promotores are trained community health workers with an appreciation of the social and cultural context of the communities they serve, in part, due to their shared demographic characteristics. Previous studies have shown that community health workers can be trained to provide SBI in various settings [33,34].
The current pilot study used a randomized control trial design. Men waiting for work opportunities at a day labor worker center in Seattle, Washington were approached and screened for eligibility by promotores. Those who identified as Latino, spoke Spanish, were foreign-born, over the age of 18 and had a score of 6 or more on the Alcohol Use Disorder Identification Test (AUDIT) were invited to participate in the study. The cutoff was slightly lower than recommended levels for screening in clinical settings, in an effort to reach as many men as possible. Each participant completed a baseline survey and was randomized to an intervention or control group, using a 2:1 ratio so that two-thirds of the participants were offered the intervention. The recruitment goal of 120 was based on an 80% completion rate, and an effect size (0.69) similar to changes in AUDIT scores observed in our previous studies. Participants in the intervention group received a brief intervention immediately following the baseline survey while those in the control group received information on local substance use treatment services. Participants were then contacted 2 and 8 weeks after baseline to complete follow-up surveys. All study procedures were approved by the University of Washington’s Institutional Review Board.
Brief intervention content and delivery
Promotores were Spanish-speaking Latino immigrants selected based on their previous experience with health education, research, and working with Latino communities. Training included an overview of alcohol-related disorders and disease, as well as basic information about alcohol use, including what is considered a “standard drink,” AUDIT risk levels, and National Institute for Alcohol Abuse and Alcoholism (NIAAA) guidelines for unhealthy alcohol use [35]. They also received specialized training in motivational interviewing (several days in person in Spanish), in addition to ongoing supervision and evaluation of intervention fidelity using the Motivational Interviewing Treatment Integrity Tool [36].
The 30 min brief intervention included core elements of effective brief interventions, starting with personalized feedback about alcohol use in comparison to NIAAA guidelines [35]. This was followed by a discussion of motivations and consequences of drinking, an assessment of their readiness to change, the negotiation of a plan/goal, and information on local substance use treatment services [16]. Promotores utilized simple graphics on a tablet to guide their conversation during the session. They were also trained to recognize immigration-related stressors that might contribute to unhealthy drinking and offer relevant strategies for reducing drinking.
Control condition
Participants randomized to the control condition were offered information about two local agencies providing substance use education, counseling, medical care, and referrals to in-patient treatment. Both agencies offered services in Spanish for low-income and uninsured patients.
Recruitment and data collection procedures
Promotores were present at the day labor center to screen and recruit participants at least 2 days a week for 14 months. Recruitment strategies included: announcements made to the men waiting for work opportunities; informational posters; and outreach to street corners and home improvement stores. Promotores approached interested men to be screened and those that met the criteria were invited to participate in the study. All surveys were administered by a promotor who recorded the participant responses on a tablet, in private rooms within the day labor center. They took on average 40 min to complete and participants completing the baseline survey received US$30 for each survey they completed, for a potential total of US$90.
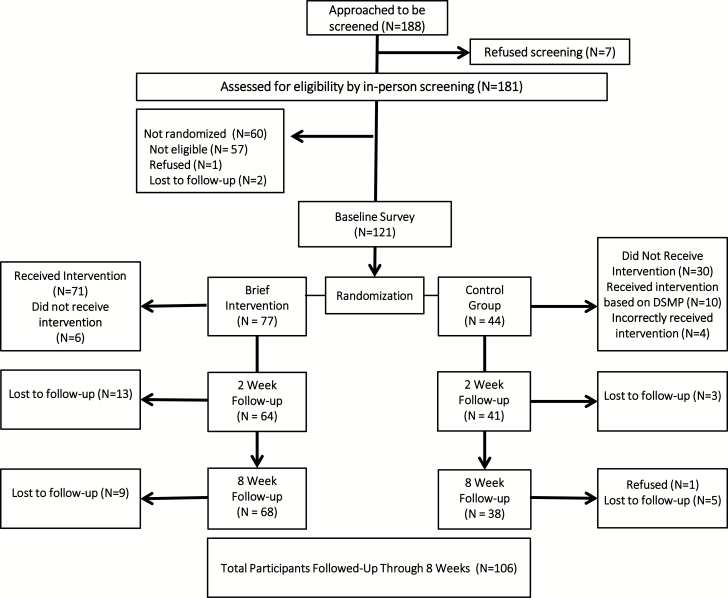
The tablets were programmed to randomize participants after completion of the baseline survey (Fig. 1). Those in the intervention group were invited to receive a brief intervention with a different promotor from the one with whom they had completed the baseline survey. Due to high AUDIT scores reported early in the study, we modified our protocol so that participants with a score of 27 or higher received a brief intervention regardless of their randomization group.
Fig. 1.
CEASE implementation comic (artwork done by Nathan Yuen).
The same promotor that completed the original baseline survey contacted participants to complete follow-up surveys 2 and 8 weeks after completing the baseline survey.
Measures
We used the Alcohol Use Disorders Identification Test (AUDIT) to screen participants and assess levels of unhealthy alcohol use [15]. The AUDIT consists of 10 questions that assess: recent hazardous alcohol consumption (questions 1–3), alcohol dependence (questions 4–6), and harmful alcohol use over the past year (questions 7–10). Item responses are summed to create a total score which can range from 0 to 40, including different zones of risk (6–15, risky or hazardous; 15–19, harmful; and 20 or higher, severe, and likely dependent) [37]. Total AUDIT scores and the single AUDIT question 3 were used as outcomes in this study. The AUDIT question 3 asks how often the subject had six or more drinks on one occasion in the past year and was considered a measure of heavy episodic drinking, with the following response options: never (0), less than monthly (1), monthly (2), weekly (3), and daily or almost daily (4) (Tuunanen, Aalto, and Seppa, 2007). The time frame for questions 3–10 was not changed for follow-up assessments. The AUDIT has been previously translated into Spanish and used with Latino populations in both the USA and Spanish-speaking countries, including day [38–40].
The number of drinks per day of self-reported alcohol use was computed based on a timeline follow-back procedure, collected at baseline, and follow-up assessments [41]. Participants were asked to indicate the number of drinks per day for the previous 2 weeks, from which we calculated the number of drinks per drinking day and the number of drinking days in that time period.
We also collected the following demographic information from participants at baseline: age, country of origin, language use, marital status, days per week laborer comes to work center, education level, current employment status, paid hours per week, weekly income, number of people income supports, living situation, and years living in the both the USA and in the Seattle area.
Data analysis
We calculated means, ranges, and percentages to describe participant characteristics. We also calculated means, standard deviations, and 95% confidence intervals for AUDIT score, drinks per drinking day, drinking days in past 14 days, and heavy episodic drinking. Statistical analyses included both (1) intent-to-treat (ITT) based on the initial treatment assignment and (2) the actual intervention-received. The ITT analyses included participants randomized to intervention (N = 77, although six of these participants did not receive a brief intervention) and those randomized to control (N = 44, 14 of which received a brief intervention due to their high AUDIT scores, resulting in 30 who did not). The intervention-received analyses consisted of N = 71 + 14 = 85 who actually received a brief intervention and N = 30 + 6 = 36 that did not receive a brief intervention irrespective of randomization. We conducted both types of analyses due to the fact 16% (N = 20, including 6 in intervention group who did not receive intervention and 14 from control group who did) of the total sample (N = 121) failed to be included in their original randomization assignment, and 32% (N = 14) of those initially randomized to control actually received the intervention (Fig. 1). Because of the large percentage of participants who had an AUDIT score over 27 (indicating risk for alcohol dependence), we also conducted a sensitivity analysis restricting the sample those with AUDIT scores under 27.
Repeated measures analysis considered baseline, 2 and 8 week follow-up assessments between the ITT intervention versus control or the actual treatment-received. Each outcome measure (AUDIT, number of drinks per drinking day and number of drinking days, heavy episodic drinking) was each assessed with a mixed-effects regression model. Analyses allowed for maximum-likelihood estimation of missing values in order to retain the entire sample for maximum statistical power in this study, and to obtain least squares means estimated from the model. Each regression analysis considered the intervention, time, and intervention-by-time effects. Post hoc evaluations consisted of pairwise contrasts for the time effect (baseline vs. 2 week follow-up, baseline vs. 8 week follow-up, and 2 vs. 8 week follow-up).
RESULTS
Screening, recruitment, and retention
We approached 188 day laborers, of which 181 were screened for unhealthy alcohol use and 124 (69%) were eligible to participate in the study based on all eligibility criteria. (Fig. 1). Of the 181 participants screened, 55 (30%) were not drinking at unhealthy levels. Of those eligible, 121 (97%) completed baseline surveys and 71 of 77 randomized participants received an intervention (92% completion rate). Additionally, 14 control participants had an AUDIT score of 27 or greater indicating a high risk of unhealthy alcohol use. Based on our data safety and monitoring plan, promotores offered these participants a brief intervention, of which 10 received one. Furthermore, four control participants were provided a brief intervention that had an AUDIT score less than 27 due to errors in implementing the protocol. Participant retention rates were 87% for the 2 week survey and 88% for the 8 week follow-up. Loss to follow-up was generally due to participant scheduling, participants moving away from the area or losing cell phone access.
Sample characteristics
Table 1 presents characteristics of the study sample. Participants ranged in age from 18 to 75 years, with a mean of 47.8 years (SD = 11.6). The majority were either single (54.5%) or divorced/widowed (17.4%). Day laborers came to the center for work on an average of 3.8 days per week (SD = 2.0), and 58.3% were paid for 20 hr or less of work time in a typical week. Most (65.3%) indicated Mexico as their country of origin, with an additional 26.5% from Central America (includes Guatemala, Honduras, El Salvador, and Nicaragua) and 8.3% from other countries (Bolivia, Brazil, Colombia, Cuba, Puerto Rico, and Venezuela). Over half (55.4%) had less than a high school education or equivalence and a majority (78.6%) made less than US$400 in weekly salary. Men indicated they had been in the USA on an average of 20.2 years (SD = 11.4) and living in the Seattle area for an average of 10.2 years (SD = 7.2).
Table 1.
Sample characteristics (N = 121)
| Demographic Characteristics | N | % |
|---|---|---|
| Age in years | ||
| 18–34 | 19 | 15.7 |
| 35–49 | 36 | 29.8 |
| 50+ | 66 | 54.6 |
| Marital status | ||
| Single | 66 | 54.5 |
| Divorced/widowed | 34 | 17.4 |
| Married/cohabitating | 21 | 28.1 |
| Days per week laborer comes to center for work | ||
| 0–1 | 17 | 14.2 |
| 2–3 | 39 | 32.5 |
| 4–5 | 16 | 23.3 |
| 6–7 | 48 | 30.0 |
| Hours of paid work in a typical week | ||
| 0 | 15 | 12.5 |
| 1–10 | 32 | 26.7 |
| 11–20 | 23 | 19.2 |
| 21–30 | 33 | 27.5 |
| 31–50 | 17 | 14.2 |
| Number of people income supports | ||
| 0–2 | 67 | 56.3 |
| 3–4 | 37 | 31.1 |
| 5–6 | 15 | 12.6 |
| Years living in the USA | ||
| 0–5 | 12 | 9.9 |
| 6–10 | 14 | 11.6 |
| 11–15 | 18 | 14.9 |
| 16–20 | 22 | 18.2 |
| 21–25 | 12 | 9.9 |
| 26–30 | 17 | 14.1 |
| 30+ | 26 | 21.5 |
| Country of origin | ||
| Mexico | 79 | 65.3 |
| Central America | 32 | 26.5 |
| Other | 10 | 8.3 |
| Language used for reading and speaking | ||
| Only Spanish | 35 | 28.9 |
| More Spanish than English | 63 | 52.1 |
| Both Spanish and English | 23 | 19.0 |
| Education level | ||
| Primary or less | 67 | 55.4 |
| High school graduate or GED | 35 | 28.9 |
| Some college or more | 19 | 15.7 |
| Current employment status | ||
| Employed year round | 4 | 3.3 |
| Day labor, seasonal, or temporary | 99 | 82.5 |
| Currently not working | 14 | 14.2 |
| Weekly salary | ||
| US$200 or less | 36 | 30.8 |
| US$200–US$300 | 30 | 25.6 |
| US$300–US$400 | 26 | 22.2 |
| US$400 or more | 25 | 21.4 |
| Living situation | ||
| Rent own apartment/house | 26 | 21.5 |
| Rent a room in apartment/house | 43 | 35.5 |
| Shelter/car/camper/streets | 33 | 27.3 |
| Staying with friends/family | 19 | 15.7 |
| Years living in Seattle area | ||
| 0–5 | 37 | 30.8 |
| 6–10 | 31 | 25.8 |
| 11–15 | 29 | 24.2 |
| 16–20 | 11 | 9.2 |
| 21+ | 12 | 10.0 |
| Outcome measures at baseline | M | (SD) |
| Total AUDIT | 20.0 | (9.7) |
| Drinks per drinking day | 3.5 | (4.5) |
| Drinking days in 14 days | 6.2 | (4.4) |
| Heavy episodic drinking | 2.5 | (1.1) |
In terms of their alcohol use, 37.2% of participants had an AUDIT score of 6–15 indicating risky drinking, 13.2% had a score of 16–19 indicating alcohol abuse, and 49.6% had a score of 20–40 indicating alcohol dependence. The mean total AUDIT score was 20.0 (SD = 9.7), with an average of 3.5 (SD = 4.5) drinks per drinking days and 6.2 (SD = 4.4) drinking days in the past 2 weeks. Participants also reported a mean score of 2.5 (SD = 1.1) on the third question of the AUDIT, indicating at least monthly heavy episodic drinking.
Since randomization is intended to reduce bias in trials by establishing groups with similar characteristics, it was important to evaluate whether baseline characteristics were similar across groups. Statistical tests between the intervention and control groups as defined by both ITT and actual treatment received approaches were conducted on the variables presented in Table 1. Results indicated statistically significant differences for only two variables: Living situation (χ(3)2 = 6.7, p = .08 for ITT; χ(3)2 = 9.2, p = .03 for actual treatment-received) and years living in Seattle (t(118) = 2.11, p = .03 for ITT; t(118) = 0.25, p = .81 for actual treatment-received). We also tested for differences between the groups on the four outcomes at baseline, the treatment group, and actual treatment-received group had lower scores on all outcomes than the control group or group not receiving the intervention. However, these differences were not statistically significant.
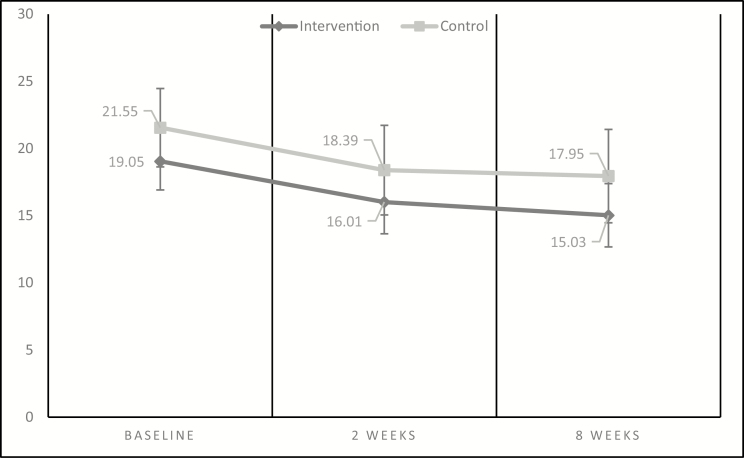
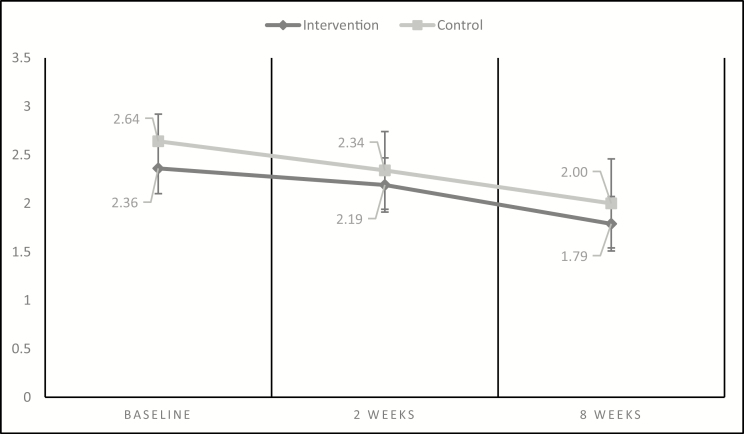
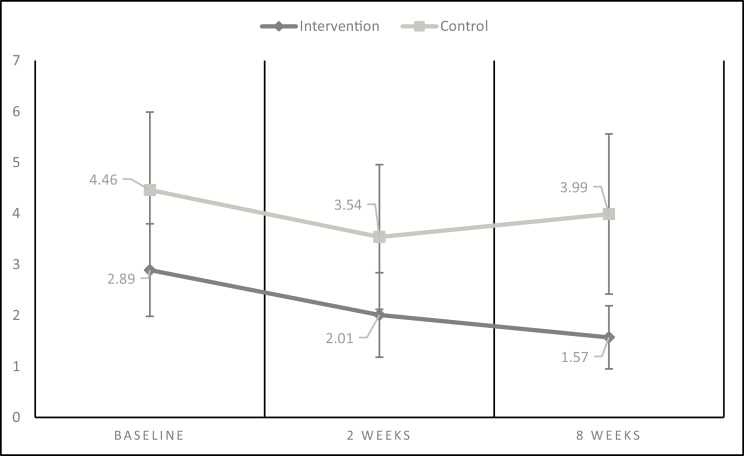
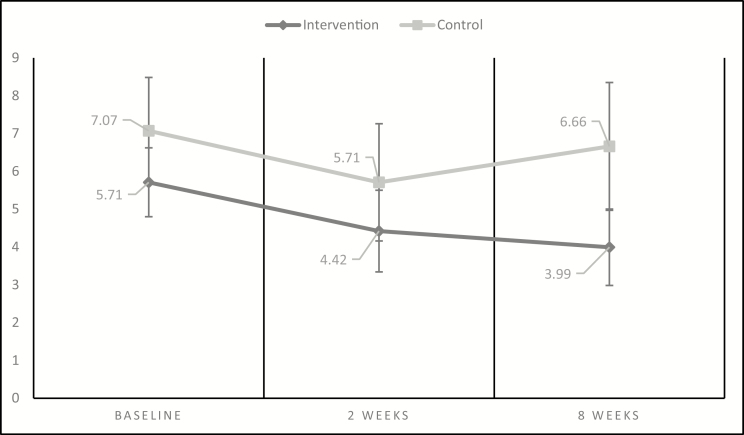
ITT analyses
In Figs. 2–5, we present means and 95% confidence intervals for all four outcomes across intervention and control groups at baseline and each of the two follow-up assessments. The figures show that for the AUDIT (Fig. 2) and heavy episodic drinking (Fig. 5), the declines in scores were consistent across intervention and control but with tighter confidence intervals for the intervention group. For the number of drinks (Fig. 3) and drinking days (Fig. 4), declines were steeper and more consistent across time for the intervention group compared with the control group.
Fig. 2.
Changes in AUDIT score.
Fig. 5.
Changes in heavy episodic drinking.
Fig. 3.
Changes in drinks per drinking day in the past 14 days.
Fig. 4.
Changes in drinking days in the past 14 days.
In the ITT mixed effects regressions analyses, there were main effect differences for drinks per drinking day and number of drinking days in 14 days (Table A1). However, it should be noted that the difference in these observed outcomes reflects larger values for control participants compared with intervention participants at all time points, especially at the 8 week follow-up assessment. There were main effects for time alone for all four outcomes and pairwise contrasts demonstrated that these differences occurred between baseline and each of the two follow-up assessments. However, there were no statistically significant effects of the intervention-by-time interactions.
The effect size (ES) differences between the control and intervention groups for baseline, 2, and 8 week follow-up, respectively, were ES = .35 (p = .067), ES = .39 (p = .055), and ES = .67 (p = .001) for the number of drinks per drinking day, and ES = .31 (p = .101), ES = .27 (p = .173), and ES = .58 (p = .005) for the number of drinking days in 14 days.
Actual treatment received and restricted sample analyses
The results for the actual intervention received analyses did not demonstrate any statistically significant intervention main effects, but showed similar results to the ITT analyses with the time effect (Table A2). However, similar to ITT, there were no statistically significant treatment-by-time interaction effects in the intervention-received sample.
Similar analyses were also conducted for a restricted sample that did not include those with AUDIT scores equal to or over 27 (indicating very high levels of alcohol risk and likely dependence. The results were similar with only main effects for time, but not intervention or intervention-by-time interactions (Table A3).
DISCUSSION
In our study, 69% of Latino day laborers screened at a day labor worker center met the criteria for unhealthy alcohol use. This is higher than what has been reported in previous studies evaluating screening and brief intervention among Latinos in other clinical settings [19,42]. Among those who screened positive for unhealthy alcohol use, many met criteria for frequent heavy episodic drinking and dependence. Similar patterns have been reported in previous studies of alcohol use in Latino day laborer or other similar samples of Latino male working populations [39,43–45]. Together, these studies confirm that Latino day laborers are a high risk group among Latino immigrant men.
Although both the intervention and control groups reduced their unhealthy alcohol use over time, there were larger and more consistent changes in drinking quantity and frequency in the intervention group. We also observed narrower confidence intervals for the mean changes in the intervention compared with control group. Our results suggest that it may be feasible to achieve small changes in drinking behaviors, even among men high levels of alcohol use. These changes could also have reduced the negative social and economic consequences of their drinking, such as having problems at work. Increasing the intensity or duration of the intervention and strengthening our referral to treatment could help achieve larger reductions.
We may have observed reductions in both the intervention and control groups due to an assessment effect. In our study, promotores spent 30–45 min with participants completing the survey, including several minutes spent explaining and completing the timeline follow-back procedure in order to assess the frequency and quantity of their drinking. Completing the timeline follow-back may have served as a form of personalized feedback, resulting in men either changing their drinking behavior following the survey or reporting less drinking regardless of their behavior [46,47]. Participants may have also been motivated to reduce their drinking (regardless of condition) because they knew they would be assessed again or out of desire to meet the expectations of the promotores.
Another potential explanation for our findings is that the regular presence of promotores at the worker center or interactions with men in the intervention group caused men in the control group to evaluate and reduce their drinking. Men randomized to both conditions remarked on the value of having the promotores on-site. Although intervention participants were asked by promotores to keep information about the brief intervention to themselves, men in the control group may have still been affected by a change in social norms at the worker center.
Only two other studies have tested the use of promotores to conduct screening and brief intervention with Latino populations. In a pilot two-group randomized trial, Latino day laborers in Los Angeles, California were offered three brief interventions using motivational enhancement therapy [33]. Although not significant, results at 6 weeks post-intervention showed reductions in both AUDIT scores and drinks per week that were consistent with the effect sizes in our study. Another study conducted a randomized controlled trial of promotor-delivered brief intervention for young adult Latino patients in the emergency department in El Paso, Texas [34]. They observed reductions in number of drinking days per week for the intervention group, at levels that were comparable to our study [19]. Results from our current study were also similar to our previous pilot work which assessed pre- and post-test differences among men receiving a brief intervention with no comparison group [48].
CONCLUSIONS
We found that a culturally adapted brief intervention was not effective in reducing Latino day laborers unhealthy drinking over time. Although offering screening and brief intervention in community settings can help reach high-risk populations that may not otherwise have access to evidence-based interventions to reduce alcohol use, interventions with more intensity or longer duration may be needed to reduce unhealthy drinking. Future studies should consider whether multiple brief interventions, as well as a stronger focus on connecting dependent men with treatment can be effective in reducing risk in this group. In addition, larger trials may be more able to detect differences between intervention and control groups. It is critical to identify opportunities to reduce unhealthy alcohol use and its consequences among this population.
Acknowledgments
We acknowledge the efforts of the entire research team as well as the support of our community partners Casa Latina. We further acknowledge the contributions of all the participants. We also want to thank the anonymous reviewers for their suggestions and Francisco Rios Casas for his assistance with revisions.
Table A1.
Intent-to-treat (ITT) analysis (N = 121)
| Repeated measures model effects | Total AUDIT | Drinks per drinking day | Drinking days in 14 days | Heavy episodic drinking |
|---|---|---|---|---|
| ITT Intervention main effect | F = 1.93 (p = .1676) | F = 6.07 (p = .0152) | F = 4.22 (p = .0421) | F = 1.16 (p = .2828) |
| Time main effect | F = 11.81 (p < .0001) | F = 8.44 (p = .0004) | F = 10.00 (p < .0001) | F = 16.18 (p < .0001) |
| ITT Intervention x Time interaction | F = 0.05 (p = .9473) | F = 0.67 (p = .5119) | F = 1.57 (p = .2117) | F = 0.12 (p = .8846) |
| Model-based least squares means | Baseline | 2 Weeks FU | 8 Weeks FU | Average Row |
| Total AUDIT | ||||
| Intervention | 19.05 | 16.70 | 15.58 | 17.11 |
| Control | 21.55 | 18.92 | 18.15 | 19.54 |
| Average column | 20.30 | 17.81 | 16.86 | |
| Drinks per drinking day | ||||
| Intervention | 2.89 | 1.96 | 1.75 | 2.20 |
| Control | 4.46 | 3.59 | 3.81 | 3.95 |
| Average column | 3.67 | 2.77 | 2.78 | |
| Drinking days in 14 days | ||||
| Intervention | 5.71 | 4.54 | 4.17 | 4.81 |
| Control | 7.07 | 5.75 | 6.45 | 6.42 |
| Average column | 6.39 | 5.14 | 5.31 | |
| Heavy episodic drinking | ||||
| Intervention | 2.36 | 2.17 | 1.82 | 2.12 |
| Control | 2.64 | 2.36 | 2.01 | 2.33 |
| Average column | 2.50 | 2.26 | 1.92 | |
| Pairwise contrasts for time effect | Total AUDIT | Drinks per drinking day | Drinking days in 14 days | Heavy episodic drinking |
| Baseline vs. 2 Weeks FU | t = 3.64 (p = .0004) | t = 3.98 (p = .0001) | t = 4.38 (p < .0001) | t = 2.55 (p = .0120) |
| Baseline vs. 8 Weeks FU | t = 4.84 (p < .0001) | t = 3.42 (p = .0009) | t = 3.10 (p = .0024) | t = 5.65 (p < .0001) |
| 2 Weeks FU vs. 8 Weeks FU | t = 1.71 (p = .0900) | t = −0.02 (p = .9807) | t = −0.55 (p = .5826) | t = 3.70 (p = .0003) |
Degrees of freedom for F-tests are df = 1,119 for the ITT intervention main effect, and df = 2,119 for both the time main and ITT intervention x time interaction effects. Degrees of freedom for all pairwise contrast t-tests are df = 119. N = 77 for the ITT intervention group and N = 44 for the ITT control group.
Table A2.
Actual intervention received analysis (N = 121)
| Repeated measures model effects | Total AUDIT | Drinks per drinking day | Drinking days in 14 days | Heavy episodic drinking |
|---|---|---|---|---|
| Intervention Received main effect | F = 1.09 (p = .2980) | F = 0.01 (p = .9542) | F = 0.01 (p = .9168) | F = 4.15 (p = .0439) |
| Time main effect | F = 10.66 (p = .0001) | F = 8.89 (p = .0003) | F = 8.03 (p = .0005) | F = 15.37 (p < .0001) |
| Intervention Received x Time interaction | F = 0.06 (p = .9441) | F = 0.85 (p = .4286) | F = 1.20 (p = .3040) | F = 0.55 (p = .5810) |
| Model-based Least Squares Means | Baseline | 2 Weeks FU | 8 Weeks FU | Average Row |
| Total AUDIT | ||||
| Intervention | 20.51 | 18.15 | 17.05 | 18.57 |
| Control | 18.67 | 15.98 | 15.26 | 16.64 |
| Average column | 19.59 | 17.06 | 16.16 | |
| Drinks per drinking day | ||||
| Intervention | 3.42 | 2.52 | 2.62 | 2.85 |
| Control | 3.55 | 2.65 | 2.22 | 2.81 |
| Average column | 3.48 | 2.58 | 2.42 | |
| Drinking days in 14 days | ||||
| Intervention | 6.37 | 5.06 | 4.84 | 5.42 |
| Control | 5.83 | 4.77 | 5.39 | 5.33 |
| Average column | 6.10 | 4.91 | 5.12 | |
| Heavy episodic drinking | ||||
| Intervention | 2.55 | 2.34 | 2.03 | 2.32 |
| Control | 2.25 | 1.88 | 1.57 | 1.90 |
| Average column | 2.40 | 2.14 | 1.80 | |
| Pairwise contrasts for time effect | Total AUDIT | Drinks per Drinking Day | Drinking Days in 14 days | Heavy Episodic Drinking |
| Baseline vs. 2 Weeks FU | t = 3.49 (p = .0007) | t = 3.79 (p = .0002) | t = 3.94 (p = .0001) | t = 2.70 (p = .0079) |
| Baseline vs. 8 Weeks FU | t = 4.59 (p < .0001) | t = 3.90 (p = .0002) | t = 2.70 (p = .0080) | t = 5.53 (p < .0001) |
| 2 Weeks FU vs. 8 Weeks FU | t = 1.53 (p = .1276) | t = 0.80 (p = .4279) | t = -0.62 (p = .5361) | t = 3.39 (p = .0010) |
Degrees of freedom for F-tests are df = 1,119 for the intervention-received main effect, and df = 2,119 for both the time main and intervention-received x time interaction effects. Degrees of freedom for all pairwise contrast t-tests are df = 119. N = 85 for the intervention-received group and N = 36 for the control-received group.
Table A3.
Intent-to-treat (ITT) analysis-restricted sample (N = 88)
| Repeated measures model effects | Total AUDIT | Drinks per drinking day | Drinking days in 14 days | Heavy episodic drinking |
|---|---|---|---|---|
| Intervention main effect | F = 0.70 (p = .4060) | F = 2.21 (p = .1412) | F = 0.98 (p = .3258) | F = 0.12 (p = .7259) |
| Time main effect | F = 4.72 (p = .0113) | F = 7.35 (p = .0011) | F = 4.75 (p = .0110) | F = 13.58 (p < .0001) |
| Intervention x Time interaction | F = 0.58 (p = .5622) | F = 0.53 (p = .5890) | F = 0.90 (p = .4116) | F = 0.47 (p = .6270) |
| Model-based least squares means | Baseline | 2 Weeks FU | 8 Weeks FU | Average Row |
| Total AUDIT | ||||
| Intervention | 16.33 | 14.45 | 14.18 | 14.99 |
| Control | 14.79 | 13.88 | 12.44 | 13.71 |
| Average column | 15.56 | 14.16 | 13.31 | |
| Drinks per drinking day | ||||
| Intervention | 2.06 | 1.42 | 1.38 | 1.62 |
| Control | 2.86 | 2.51 | 2.12 | 2.50 |
| Average column | 2.46 | 1.97 | 1.75 | |
| Drinking days in 14 days | ||||
| Intervention | 5.05 | 4.24 | 3.82 | 4.37 |
| Control | 5.73 | 4.70 | 5.24 | 5.23 |
| Average column | 5.39 | 4.47 | 4.53 | |
| Heavy episodic drinking | ||||
| Intervention | 2.04 | 1.91 | 1.53 | 1.82 |
| Control | 2.23 | 1.97 | 1.49 | 1.90 |
| Average column | 2.13 | 1.94 | 1.51 | |
| Pairwise contrasts for time effect | Total AUDIT | Drinks per drinking day | Drinking days in 14 days | Heavy episodic drinking |
| Baseline vs. 2 Weeks FU | t = 1.95 (p = .0545) | t = 2.38 (p = .0197) | t = 3.00 (p = .0035) | t = 1.74 (p = .0859) |
| Baseline vs. 8 Weeks FU | t = 3.06 (p = .0029) | t = 3.83 (p = .0002) | t = 2.16 (p = .0335) | t = 5.04 (p < .0001) |
| 2 Weeks FU vs. 8 Weeks FU | t = 1.50 (p = .1377) | t = 1.23 (p = .2205) | t = −0.17 (p = .8649) | t = 3.89 (p = .0002) |
Degrees of freedom for F-tests are df = 1,86 for the intervention-received main effect, and df = 2,86 for both the time main and intervention-received x time interaction effects. Degrees of freedom for all pairwise contrast t-tests are df = 86.
Funding
This study was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) 1R34AA022696-01A1 and the Center for Studies in Demography and Ecology (CSDE) at the University of Washington.
Compliance with Ethical Standards
Conflict of Interest: All authors declare that they have no conflicts of interest.
Authors’ Contributions: IO conceived of the study, assisted with analyses and drafted the manuscript. SD conducted the analyses. VT assisted with study development, data collection, data analysis and manuscript revisions. SS assisted with study development, implementation, data analysis, and drafting the manuscript. BD and DD assisted with study development, implementation, interpretation of findings and manuscript revisions.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national researchcommittee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.” The study was reviewed and approved by the University of Washington Office of Human Subjects Research. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Negi NJ. Battling discrimination and social isolation: psychological distress among latino day laborers. Am J Community Psychol. 2012; 51(1–2):164–174. [DOI] [PubMed] [Google Scholar]
- 2. Negi NJ. Identifying psychosocial stressors of well-being and factors related to substance use among Latino day laborers. J Immigr Minor Health. 2011;13(4):748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ornelas IJ, Eng E, Perreira KM. Perceived barriers to opportunity and their relation to substance use among Latino immigrant men. J Behav Med. 2011;34(3):182–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rhodes SD, Hergenrather KC, Griffith DM, et al. Sexual and alcohol risk behaviours of immigrant Latino men in the South-eastern USA. Cult Health Sex. 2009;11(1):17–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rhodes SD, McCoy TP, Hergenrather KC, et al. Prevalence estimates of health risk behaviors of immigrant latino men who have sex with men. J Rural Health. 2012;28(1):73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Welland C, Ribner N. Culturally specific treatment for partner-abusive Latino men: a qualitative study to identify and implement program components. Violence Vict. 2010;25(6):799–813. [DOI] [PubMed] [Google Scholar]
- 7. Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): rates and predictors of alcohol abuse and dependence across Hispanic national groups. J Stud Alcohol Drugs. 2008;69(3):441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans baseline alcohol survey (HABLAS): DUI rates, birthplace, and acculturation across Hispanic national groups. J Stud Alcohol Drugs. 2008;69(2):259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): the association between birthplace, acculturation and alcohol abuse and dependence across Hispanic national groups. Drug Alcohol Depend. 2009;99(1-3):215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Blanco C, Morcillo C, Alegría M, et al. Acculturation and drug use disorders among Hispanics in the U.S. J Psychiatr Res. 2013;47(2): 226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Valenzuela Jr. A, Theodore N, Melendez E, Gonzalez A. . On the Corder: Day Labor in the United States. 2006. pp. 1–39. UCLA Center for the Study of Urban Poverty. [Google Scholar]
- 12. Cepeda A, Valdez A, Kaplan C, Hill LE. Patterns of substance use among hurricane Katrina evacuees in Houston, Texas. Disasters. 2010;34(2):426–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. del Pino HE, Méndez-Luck C, Bostean G, Ramírez K, Portillo M, Moore AA. Leveraging family values to decrease unhealthy alcohol use in aging Latino day laborers. J Immigr Minor Health. 2013;15(5):1001–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Worby PA, Organista KC. Contextual influences on the drinking of male Latino immigrant day laborers. Subst Use Misuse. 2013;48(5):391–403. [DOI] [PubMed] [Google Scholar]
- 15. Babor T, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test, 2nd ed. World Health Organization; 2001. [Google Scholar]
- 16. Whitlock EP, Polen MR, Green CA, Orleans T, Klein J; U.S. Preventive Services Task Force Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557–568. [DOI] [PubMed] [Google Scholar]
- 17. Arroyo JA, Miller WR, Tonigan JS. The influence of Hispanic ethnicity on long-term outcome in three alcohol-treatment modalities. J Stud Alcohol. 2003;64(1):98–104. [DOI] [PubMed] [Google Scholar]
- 18. Arroyo JA, Westerberg VS, Tonigan JS. Comparison of treatment utilization and outcome for Hispanics and non-Hispanic whites. J Stud Alcohol. 1998;59(3):286–291. [DOI] [PubMed] [Google Scholar]
- 19. Cherpitel CJ, Ye Y, Bond J, et al. Brief intervention in the emergency department among Mexican-origin young adults at the US-Mexico border: outcomes of a randomized controlled clinical trial using promotores. Alcohol Alcohol. 2016;51(2):154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tonigan JS. Project match treatment participation and outcome by self-reported ethnicity. Alcohol Clin Exp Res. 2003;27(8):1340–1344. [DOI] [PubMed] [Google Scholar]
- 21. Leclere OA, López RA. The jornalero: perceptions of health care resources of immigrant day laborers. J Immigr Minor Health. 2012;14(4):691–697. [DOI] [PubMed] [Google Scholar]
- 22. Walter N, Bourgois P, Margarita Loinaz H, Schillinger D. Social context of work injury among undocumented day laborers in San Francisco. J Gen Intern Med. 2002;17(3):221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38(3):809–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mulia N, Ye Y, Greenfield TK, Zemore SE. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcohol Clin Exp Res. 2009;33(4):654–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatry. 2001;158(12):2027–2032. [DOI] [PubMed] [Google Scholar]
- 26. Manuel JK, Satre DD, Tsoh J, et al. Adapting screening, brief intervention, and referral to treatment for alcohol and drugs to culturally diverse clinical populations. J Addict Med. 2015;9(5):343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ornelas IJ, Allen C, Vaughan C, Williams EC, Negi N. Vida PURA: a cultural adaptation of screening and brief intervention to reduce unhealthy drinking among Latino day laborers. Subst Abus. 2015;36(3):264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Platt L, Melendez-Torres GJ, O’Donnell A, et al. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? Findings from a systematic review and metaregression analysis. BMJ Open. 2016;6(8):e011473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;2:CD004148. [DOI] [PubMed] [Google Scholar]
- 30. Lee CS, López SR, Colby SM, et al. Culturally adapted motivational interviewing for Latino heavy drinkers: results from a randomized clinical trial. J Ethn Subst Abuse. 2013;12(4):356–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nilsen P. Brief alcohol intervention–where to from here? Challenges remain for research and practice. Addiction. 2010;105(6):954–959. [DOI] [PubMed] [Google Scholar]
- 32. Barrera M Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. 2013;81(2):196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Moore AA, Karno MP, Ray L, et al. Development and preliminary testing of a promotora-delivered, Spanish language, counseling intervention for heavy drinking among male, Latino day laborers. J Subst Abuse Treat. 2016;62:96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ramos R, Cherpitel CJ, Alvarez J, et al. Preparing Mexican-origin community health advocates (promotores) to conduct SBIRT for problem drinking in the emergency room. Pedagog Health Promot. 0(0):2373379918756425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. National Institute for Alcoholism and Alcohol Abuse. “Drinking Levels Defined”. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed May 16, 2019. [Google Scholar]
- 36. Serrano SE, Serafini K, Eller N, Torres VN, Donovan D, Ornelas IJ. Vida PURA: an assessment of the fidelity of promotor-delivered screening and brief intervention to reduce unhealthy alcohol use among Latino day laborers. J Ethn Subst Abuse. 2018;17(4):519–531 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Saitz R. Alcohol: no ordinary health risk. Addiction. 2015;110(8): 1228–1229. [DOI] [PubMed] [Google Scholar]
- 38. Babor T, Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT Cuestionario de Identificacion de los Transtornos debidos al Consumo de Alcohol. Organizacion Mundial de la Salud Generalitat Valenciana, 2001. [Google Scholar]
- 39. Ornelas IJ, Toress V, Serrano S. Patterns of alcohol use among Latino day laborers. Health Behav Policy Rev. 2016;3(4):361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Alvarado ME, Garmendia ML, Acuña G, Santis R, Arteaga O. [Assessment of the alcohol use disorders identification test (AUDIT) to detect problem drinkers]. Rev Med Chil. 2009;137(11):1463–1468. [PubMed] [Google Scholar]
- 41. Agrawal S, Sobell MB, Sobell LC.. Calendar and Time Diary. Thousand Oaks, CA:SAGE Publications, Inc., 2009. [Google Scholar]
- 42. Field CA, Caetano R, Harris TR, Frankowski R, Roudsari B. Ethnic differences in drinking outcomes following a brief alcohol intervention in the trauma care setting. Addiction. 2010;105(1):62–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arcury TA, Talton JW, Summers P, Chen H, Laurienti PJ, Quandt SA. Alcohol consumption and risk for dependence among male Latino migrant farmworkers compared to Latino nonfarmworkers in North Carolina. Alcohol Clin Exp Res. 2016;40(2):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Daniel-Ulloa J, Reboussin BA, Gilbert PA, Mann L, Alonzo J, Downs M, Rhodes SC. Predictors of heavy episodic drinking and weekly drunkenness among immigrant Latinos in North Carolina. Am J Mens Health. 2014;8(4):339–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sánchez J. Alcohol use among Latino migrant workers in South Florida. Drug Alcohol Depend. 2015;151:241–249. [DOI] [PubMed] [Google Scholar]
- 46. McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. Plos One. 2011;6(10):e23748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: a randomized controlled trial. J Consult Clin Psychol. 2006;74(5):943–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ornelas IJ, Allen C, Vaughan C, Negi N, Williams E.. “Cuando Tomo Mas, Siento Que Es Un Refugio”: using mixed methods to understand the context of alcohol use among Latino immigrant men. Alcohol.: Clin Exp Res. 2014;38(1):39a–39a. [Google Scholar]