Abstract
Background:
Increasing smartphone use has led to the introduction of smartphone addiction as a behavioral addiction with detrimental effects on health. This phenomenon has not been widely studied in the Indian context. This study assessed the rate of smartphone addiction in a sample of medical students, with a focus on its correlation with sleep quality and stress levels.
Methods:
A cross-sectional study was conducted between November 2016 and January 2017 in 195 medical students. Their smartphone use, level of smartphone addiction, sleep quality, and perceived stress levels were measured using the Smartphone Addiction Scale-Short Version (SAS-SV), the Pittsburgh Sleep Quality Index (PSQI), and the Perceived Stress Scale (PSS-10), respectively.
Results:
Of the 195 students, 90 (46.15%) had smartphone addiction as per the scale. A self-reported feeling of having smartphone addiction, use of the smartphone right before sleeping, PSS scores, and PSQI scores were found to be significantly associated with the SAS-SV scores. Significant positive correlations were observed between the SAS-SV and PSS-10 scores, and the SAS-SV and PSQI scores.
Conclusions:
There is a high magnitude of smartphone addiction in medical students of a college in Western Maharashtra. The significant association of this addiction with poorer sleep quality and higher perceived stress is a cause for concern. The high self-awareness among students about having smartphone addiction is promising. However, further studies are required to determine whether this self-awareness leads to treatment seeking. Further studies are required to explore our finding of the association of smartphone addiction with using the smartphone before sleeping.
Keywords: Addiction, India, medical, smartphone, students
Key messages: •A high proportion of the medical students of a college in Western Maharashtra have smartphone addiction., •Smartphone addiction has significant associations with impaired sleep and high stress., •Smartphone addiction is significantly associated with a self-reported feeling of having the addiction.
The 21st century has witnessed a rapid growth in technology and, with the introduction of the Internet, a revolutionization of information access. The legacy of these noteworthy milestones is captured by the innovation and popularization of the “smartphone”.[1]
Addiction is a process whereby a behavior that can function both to produce pleasure and to provide an escape from internal discomfort is employed in a pattern characterized by (1) recurrent failure to control the behavior (powerlessness) and (2) continuation of the behavior despite significant negative consequences (unmanageability).[2] The increasing use of and dependence on the Internet brought to the surface a new public health concern near the start of the century “Internet Addiction Disorder,” which was eventually included in the Diagnostic and Statistical Manual of diseases (DSM-5) under conditions for further study.[3] On the heels of this, the close association between the internet and the smartphone led to the introduction of “Smartphone Addiction,” a behavioral addiction characterized by the presence of symptoms of tolerance, salience, mood changes, and dependence on smartphones.[4] Consequently, the “Smartphone Addiction Scale” was developed for its quantification.[5] This addiction has been associated with depression, anxiety, accidents, poor sleep, poor academic performance, fatigue, and high stress.[6,7,8] There is some debate among academicians on whether it can be called an “addiction” which is why alternate terms like “Problematic Smartphone Use” and “Smartphone Use Disorder” have been proposed.[9,10]
A 2017 study revealed that over 300 million people in India use a smartphone.[11] A large proportion of the Indian population is thus at potential risk of addiction. However, there is a paucity of studies related to it in the Indian population. Students having birth years between 1990 and 2000 (i.e., the age group of 17--27 years) have been introduced to smartphones in their formative adolescent years. Exploring smartphone addiction in this cohort is, thus, especially crucial.
Recent studies have revealed a high prevalence of smartphone addiction in university students and not only urban but also rural school students.[12,13,14,15] Studies in medical students in Jammu and Kashmir, Delhi, and Maharashtra have found a high prevalence of smartphone addiction, ranging from 34% to 40%.[13,14,16,17] However, the studies in Maharashtra have been limited to private medical institutions. The socioeconomic background of students in government-run medical institutions being different from that of private medical institutions makes it important to study the addiction in the former group. This study aims to assess the prevalence of smartphone addiction in medical students in a government-run medical college in Western Maharashtra. It further aims to explore the sociodemographic and smartphone use related correlates of smartphone addiction, and the association of this addiction with stress levels and quality of sleep. To the best of our knowledge, this is one of the first studies on this topic in a government-run medical college in Western Maharashtra.
MATERIALS AND METHODS
A cross-sectional study was conducted between November 2016 and January 2017 in a Government Medical College in Western Maharashtra. Ethical approval was obtained from the Institutional Ethics Committee.
A questionnaire was prepared using validated scales (described below) and administered as a Google form. Adequate permission was obtained from the authors for the use of the scales. The questionnaire comprised of:
Part 1: A semi-structured questionnaire to assess the correlates of smartphone addiction. It recorded the demographic profile (age, sex, residence, and year of MBBS), history of psychiatric/neurological illness, and the pattern of smartphone use (age of commencement of use, most frequent purpose of use, use right before sleeping at night, and the subjective feeling of having smartphone addiction).
-
Part 2: Validated Scales
A. Cohen's Perceived Stress Scale (PSS-10):[18,19] It is a self-administered psychological instrument for assessing the perception of stress. It consists of 10 questions on the subjective stress levels of the participant during the previous month. The responses are scored according to a five-point Likert scale. The scale has a minimum score of zero and a maximum score of 40. There is no predetermined cut-off for gauging stress; higher scores indicate a higher stress level. The scale shows good convergent validity and reliability (Cronbach's alpha 0.89).[20] It has been used in the Indian population but has not been validated in the Indian student population.[17,21,22]
B. Smartphone Addiction Scale-Short Version (SAS-SV):[23] It is a self-administered scale to screen smartphone addiction in the community. It consists of 10 questions scored on a six-point scale that can be self-administered by the participant. It has a minimum score of 10 and a maximum score of 60. The SAS-SV provides a cut-off value for addiction, which is 31 for boys and 33 for girls. It has been previously used for an age group similar to the one chosen for this study.[24] It shows good concurrent validity with the SAS and reliability (Cronbach's alpha 0.91). It has been widely used in Indian students but has not been validated for this population.[16,17]
C. Pittsburgh Sleep Quality Index (PSQI):[25] The PSQI is a self-administered scale which contains 19 questions related to the previous month's sleep patterns. This questionnaire has seven components that measure the different aspects of sleep (C1-Subjective sleep quality, C2-Sleep latency, C3-Sleep duration, C4-Habitual efficacy, C5-Sleep disturbances, C6-Use of sleep medication, C7-Daytime dysfunction). It has a minimum score of “zero” and a maximum score of “21” with “five” as a cut-off value for impaired sleep. It has acceptable measures of reliability (Cronbach's alpha 0.83) and validity. It has been widely used in the Indian population and has shown good validity in Indian university students.[26,27]
The questionnaire was piloted in 10 students, and clarifications were made based on their recommendations. Based on prior studies that have shown a prevalence of 44% in the Indian population, a minimum required sample size of 112 was calculated to estimate the prevalence of addiction at 95% confidence and 10% precision.[28] The contact numbers of students from each batch were obtained from the class representatives. All the contact numbers that the class representative had saved in his/her phone were included. The researchers then contacted the students via a text message or a phone call and explained the study in detail. Oral informed consent was obtained from those who were willing to participate. For students who had not completed 18 years of age, consent was obtained from their parents over a telephonic conversation. Additionally, there was a consent page at the beginning of the questionnaire, which explained the details of the study and the purpose for which the information provided by the participants would be used. The questionnaire was then sent as a Google form link via text message to the students that were willing to participate. All queries were resolved by the researcher, and a confirmation via text message was requested after the participant had filled the questionnaire. The data collected were transferred from Google Docs to a Microsoft Excel sheet. Incomplete entries were deleted. No identifying information was retained. Students who, in the questionnaire, reported having a history of psychiatric/neurological disorders were excluded. The data was initially split into two groups, “Smartphone Addiction Positive” and “Smartphone Addiction Negative,” using predetermined cut-offs of the SAS-SV. The differences in sociodemographic and smartphone use related factors in the two groups were analyzed using the Chi-square, Fisher's exact, and independent samples t-test as applicable. This was followed by a multiple regression model with SAS-SV as the dependent variable and the sociodemographic and smartphone use related factors, PSS-10, and PSQI as the independent variables. The correlation of SAS-SV scores with PSS-10 and PSQI scores was assessed by a Pearson's correlation test. A value of P < 0.05 was taken to be significant.
RESULTS
Demographics of the study population
We contacted 250 students whose contact numbers were obtained. Two hundred forty students consented to the study. Of these, 215 filled the questionnaire. The response rate was thus 89.6%. Seven students with a self-reported history of psychiatric disorders and 13 whose forms were inadequate were excluded, leaving behind an effective sample size of 195.
The sample consisted of 99 (50.77%) females and 96 (49.23%) males. There were 51 (26.15%) students from the 1st year, 54 (27.70%) from the 2nd year, 47 (24.10%) from the 3rd year (Part 1), and 43 (22.05%) from the 3rd year (Part 2). The age ranged from 17 to 27 years, with a mean (±SD) of 20.23 (±1.63). All students identified themselves as being from the lower middle to upper-middle socioeconomic class.
Smartphone use
The mean age of beginning to use a smartphone was 17.15 (±1.58) years. 66 (33.85%) of 195 students listed Whatsapp as their favorite application, making it the most popular application, followed by Instagram (12.31%) and Facebook (5.13%). Text messaging was the most common purpose of using the smartphone, as stated by 100 (57.14%) of 175 students who responded adequately to this item on the questionnaire. This was followed by internet browsing (10.86%).
Smartphone addiction
Of the195 students, 90 (46.15%) screened positive for smartphone addiction as per the SAS-SV scores. These included 45 (45.45%) of the 99 females and 45 (47.87%) of the 94 males. The SAS-SV scores ranged from 10 to 57, with an average score of 31.59 (±9.89). Of the 90 students who screened positive for addiction, 69 (76.67%) had a self-reported feeling of having smartphone addiction, while of the 105 students who screened negative, 27 (25.71%) felt that they had it. Tables 1 and 2 show the sociodemographic and smartphone use related differences in those with and without smartphone addiction by the Chi-square test, Fisher's exact test, and t-test as applicable. A statistically significant proportion of those with a self-reported feeling of having smartphone addiction, and those using the smartphone right before sleeping were screened positive for smartphone addiction [Table 1]. A multiple regression model was run, which brought forth four significant factors associated with smartphone addiction: (1) a self-reported feeling of having smartphone addiction, (2) use of the smartphone right before sleeping, (3) PSS scores, and (4) PSQI scores [Table 3]. No other sociodemographic or smartphone use related variables were seen to have a significant association with smartphone addiction.
Table 1.
Sociodemographic and smartphone use related differences in groups with and without smartphone addiction (Chi-Square, Fischer’s Exact Test)
| Socio-Demographic and Smartphone Use Variables | Addiction Present* |
Addiction Absent* |
Chi-Square Value (df‡) | P§ (two tailed) | ||
|---|---|---|---|---|---|---|
| Chi-Square Test | Fisher’s Exact Test† | |||||
| Gender | Male | 45 (50.00%) | 51 (48.57%) | 0.04 (1) | 0.84 | |
| Female | 45 (50.00%) | 54 (51.43%) | ||||
| Year of MBBS | 1st year 2nd year 3rd year 4th year |
17 (18.89%) 24 (26.67%) 26 (28.89%) 23 (25.56%) |
34 (32.38%) 30 (28.57%) 21 (20.00%) 20 (19.05%) |
5.96 (3) | 0.11 | |
| What do you use your smartphone the most for? | Reading Songs Messaging Internet Browsing Phone calls Social Media Watching videos Gaming |
5 (6.25%) 3 (3.75%) 47 (58.75%) 10 (12.50%) 1 (1.25%) 4 (5.00%) 3 (3.75%) 7 (8.75%) |
4 (4.26%) 9 (9.57%) 53 (56.38%) 9 (9.57%) 6 (6.38%) 5 (5.32%) 3 (3.19%) 5 (5.32%) |
0.50 | ||
| Do you use your smartphone right before sleeping? | Yes No |
87 (98.86%) 1 (1.14%) |
96 (91.43%) 9 (8.57%) |
0.02 | ||
| Do you think you have smartphone addiction? | Yes No |
69 (78.41%) 19 (21.59%) |
27 (25.71%) 78 (74.29%) |
53.18 (1) | <0.001 | |
*Observed counts of students followed by the column percentage in parenthesis have been reported in each cell. †The Fisher’s Exact Test has been used instead of the Chi-Square test when more than 20% of the cells have an expected count of less than five. §The significant p values are in bold letters. ‡df – Degrees of freedom
Table 2.
Sociodemographic and smartphone use related differences in groups with and without smartphone addiction (independent samples t-test)
| Socio-Demographic and Smartphone Use Variables | Addiction Present* (n†) | Addiction Absent* (n†) | t (df‡) | P§ (two-tailed) |
|---|---|---|---|---|
| Age (in years) | 20.43±1.63, (n=86) | 20.06±1.61, (n=98) | 1.54 (182) | 0.13 |
| Age of commencing smartphone use (in years) | 17.09±1.64, (n=89) | 17.20±1.54, (n=102) | 0.46 (189) | 0.65 |
| PSS-10 scores | 19.73±6.14, (n=84) | 16.04±5.64, (n=102) | 4.36 (184) | <0.001 |
| PSQI scores | 7.60±4.43, (n=90) | 5.31±4.24, (n=105) | 3.68 (193) | <0.001 |
*Smartphone Addiction Scale-Short Version (SAS-SV) scores have been reported in the cells as (Mean±Standard Deviation). §The significant p values are in bold letters. †n – Total count of participants under each cell; df – Degrees of freedom, PSS-10 – Perceived stress scale, PSQI – Pittsburgh sleep quality index
Table 3.
Sociodemographic and smartphone use related correlates of SAS-SV scores (a multiple regression model)
| Socio-Demographic and Smartphone Use Variables*,† | β | P‡ (two tailed) | 95% Confidence Interval | Model Summary | |
|---|---|---|---|---|---|
| Gender | Male (1) Female (2) |
-0.03 | 0.68 | (-2.83, 1.86) | R=0.67; |
| Age | 0.11 | 0.11 | (-0.16, 1.55) | R2=0.45; | |
| Age of onset of smartphone use | 0.04 | 0.62 | (-0.66, 1.11) | F=19.16; | |
| Do you use your smartphone right before sleeping? | Yes (1) No (2) |
-0.16 | 0.01 | (-11.49, -1.65) | P<0.001 |
| Do you think you have smartphone addiction? | Yes (1) No (2) |
-0.48 | <0.001 | (-11.74, -6.93) | |
| PSQI Scores | 0.14 | 0.04 | (0.02,0.58) | ||
| PSS Scores | 0.18 | 0.01 | (0.07,0.51) | ||
*The variables ‘age’ and ‘year of MBBS’ are logically related to each other, causing potential bias in a regression model. Thus, only the ‘age’ variable has been considered in this model. †The nominal variables have been assigned dummy numbers as enumerated in the cells in parenthesis (E.g., male=1 and female=2). ‡The significant p values are in bold letters. SAS-SV – Smartphone Addiction scale-short version, PSQI – Pittsburgh sleep quality index, PSS-10 – Perceived stress scale
Smartphone addiction, stress, and sleep
The PSQI scores in the sample ranged from zero to 20, with an average score of 6.37 (±4.47). Of the 195 students, 91 (46.67%) had impaired sleep. The PSS scores ranged from zero to 37, with an average score of 17.70 (±6.14). Significantly higher PSS scores and PSQI scores were found in students who screened positive for smartphone addiction than those who did not [Table 2]. A weak positive linear correlation between the SAS-SV and PSQI scores (r = 0.31, P < 0.001) and a moderate positive linear correlation between the SAS-SV and PSS-10 scores (r = 0.40, P < 0.001) were found by the Pearson's correlation test [Figures 1 and 2].
Figure 1.
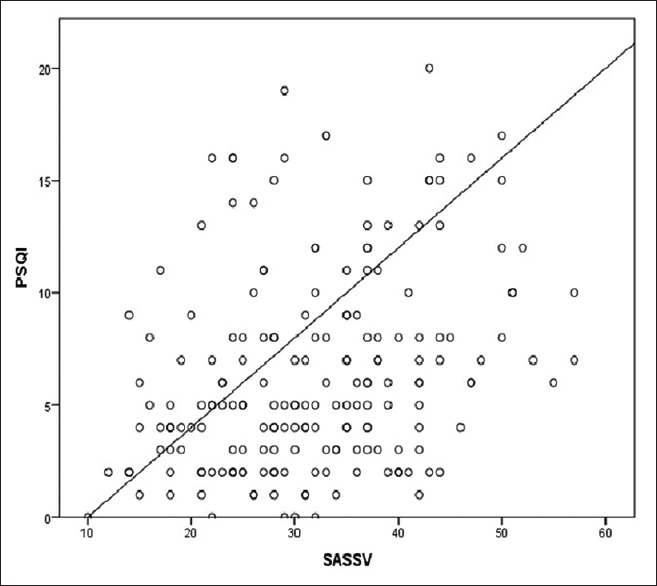
Correlation between SAS-SV and PSQI scores. SAS-SV - Smartphone addiction scale-short version, PSQI - Pittsburgh sleep quality index
Figure 2.
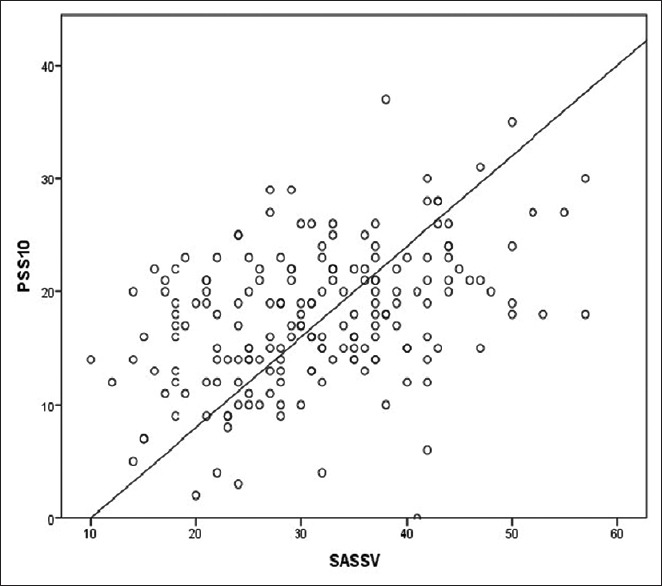
Correlation between SAS-SV and PSS-10 score. SAS-SV - Smartphone addiction scale-short version, PSS-10 - Perceived stress scale
DISCUSSION
Smartphones are rapidly evolving, and their use is constantly on the rise. Smartphone addiction has been identified as a behavioral addiction in the recent decade but has not yet been established as a real problem, especially in India. Our results show that within a small population of Indian medical students, almost half (46.15%) screened positive for smartphone addiction. This frequency of smartphone addiction is higher than the range (39% to 44%) found in the Indian population by a meta-analysis of six Indian studies in 2014 and recent studies in medical students.[6,12,13]
This study found no significant gender differences in addiction as opposed to the higher smartphone addiction in female students observed by authors in Korea and the Middle-East.[29,30,31] Similar to our study, no significant gender difference was observed by Basu et al. in medical students in India.[12] Using the smartphone right before sleeping was found to have a significant association with SAS-SV scores in our study. Similar to these results, the night-time usage of smartphones was found to be significantly higher in those having smartphone addiction in a study done in Korea, which used an application to track smartphone usage.[32] We also found a significant association between the PSQI and SAS-SV scores, similar to studies in medical students in Saudi Arabia and China.[24,33] While the former study used the Problematic Mobile Phone Use Questionnaire for gauging addiction, the SAS-SV was used in the latter. It could be hypothesized that higher levels of smartphone addiction cause students to spend more time on their smartphones at night, thus impairing sleep quality. The positive correlation between PSS and SAS-SV scores in our study was higher than the correlation of r = 0.30 reported in another study in medical students in Maharashtra.[13] Samaha et al. used similar scales and scoring systems and found an association between smartphone addiction and perceived stress, while another Romanian study reiterated these findings, albeit with different scales of measurement.[34,35] Smartphone addiction provides an escape from reality and could be hypothesized to be a mechanism adopted by students to alleviate stress, but further studies are required in this regard.
A positive Pearson's correlation between the smartphone addiction scores with the stress and sleep quality scores depict simultaneous greater values of each than their respective means, which indicates a perfect positive relationship between the two variables and adds weightage to the study. The association of smartphone addiction with higher stress and impaired sleep is concerning, as it has the potential to adversely affect the quality of life.[25]
This study found an association of self-reported feelings of addiction with having smartphone addiction as per the SAS-SV. No other studies reporting this parameter were found. This finding implies that most of those having smartphone addiction are self-aware of their addiction and is important as it suggests an insight into the problem---an important motivator for seeking preventive measures and treatment.
This study is cross-sectional in nature and is limited to a small population of medical students in a college in Western Maharashtra. It is thus limited in terms of generalizability. A sample of convenience was used, leading to a potential bias. The history of psychiatric/neurological illness was obtained by self-reports, which may have led to a limitation in adequately excluding all such cases. The fact that only one self-reported scale was used to assess smartphone addiction is certainly a limitation to the accuracy of the results. However, the study was one of the first of its kind in a government-run medical college in Western Maharashtra. Also, it must be noted that the entrance criteria and curricula of government medical colleges in India are homogeneous, and the findings of this sample may thus be relevant to other medical students.
Smartphone use is not limited to medical students and is ever on the rise. This addiction thus needs to be recognized and made known to the lay public. Further studies of a larger scale across different age groups, professions, and socioeconomic backgrounds are required to adequately define this problem in India. Preventive measures need to be introduced and made popular. Telemetric approaches have been found effective to track smartphone usage and detect excessive smartphone use.[17] High self-awareness of having an addiction was seen in this study, but further studies are required to assess if such self-awareness leads to treatment seeking. Psychosocial treatments like cognitive behavioral therapy, motivational therapy, and mindfulness behavioral cognitive treatment have been recommended to combat excessive smartphone use. However, the efficacy of such interventions remains unsubstantiated due to lack of data, and further studies are required.[36]
Data sharing statement
De-identified individual participant data that underlies the results reported in this article (including data dictionaries) will be made available in addition to the study protocol and statistical analysis plans. The data will be made available upon publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal.
Financial support and sponsorship
No sources of funding.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Smartphone. 2019. [online] [Last accessed on 2019 Feb 04]. Available from: https://en.oxforddictionaries.com/definition/smartphone .
- 2.Goodman A. Addiction: Definition and implications. Br J Addict. 1990;85:1403–8. doi: 10.1111/j.1360-0443.1990.tb01620.x. [DOI] [PubMed] [Google Scholar]
- 3.Young KS. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol Behav. 1998;1:237–44. [Google Scholar]
- 4.Griffiths M. A 'components' model of addiction within a biopsychosocial framework. J Subst Use. 2005;10:191–7. [Google Scholar]
- 5.Kwon M, Lee JY, Won WY, Park JW, Min JA, Hahn C, et al. Development and validation of a smartphone addiction scale (SAS) PLoS One. 2013;8:e56936. doi: 10.1371/journal.pone.0056936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davey S, Davey A. Assessment of smartphone addiction in Indian adolescents: A mixed method study by systematic-review and meta-analysis approach. Int J Prev Med. 2014;5:1500–11. [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HJ, Min JY, Kim HJ, Min KB. Accident risk associated with smartphone addiction: A study on university students in Korea. J Behav Addict. 2017;6:699–707. doi: 10.1556/2006.6.2017.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. 2015;4:85–92. doi: 10.1556/2006.4.2015.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panova T, Carbonell X. Is smartphone really an addiction.? J Behav Addict. 2018;2:252–9. doi: 10.1556/2006.7.2018.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterka-Bonetta J, Sindermann C, Elhai JD, Montag C. Personality associations with smartphone and internet use disorder: A comparison study including links to impulsivity and social anxiety. Front Public Health. 2019;7:127. doi: 10.3389/fpubh.2019.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iyengar R. India Poised for smartphone revolution. [Last retrieved on 2017 Sep 28]. Available from: https://money.cnn.com/2017/09/26/technology/india-mobile-congress-market-numbers/index.html .
- 12.Basu S, Garg S, Singh MM, Kohli C. Addiction-like behavior associated with mobile phone usage among medical students in Delhi. Indian J Psychol Med. 2018;40:446–51. doi: 10.4103/IJPSYM.IJPSYM_59_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mangot AG, Murthy VS, Kshirsagar SV, Deshmukh AH, Tembe DV. Prevalence and pattern of phantom ringing and phantom vibration among medical interns and their relationship with smartphone use and perceived stress. Indian J Psychol Med. 2018;40:440–5. doi: 10.4103/IJPSYM.IJPSYM_141_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikhita CS, Jadhav PR, Ajinkya SA. Prevalence of mobile phone dependence in secondary school adolescents. J Clin Diagn Res. 2015;9:VC06. doi: 10.7860/JCDR/2015/14396.6803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jamir L, Duggal M, Nehra R, Singh P, Grover S. Epidemiology of technology addiction among school students in rural India. Asian J Psychiatr. 2019;40:30–8. doi: 10.1016/j.ajp.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Nowreen N, Ahad F. Effect of smartphone usage on quality of sleep in medical students. Natl J Physiol Pharm Pharmacol. 2018;8:1366–70. [Google Scholar]
- 17.Prasad S, Harshe D, Kaur N, Jangannavar S, Srivastava A, Achanta U, et al. A study of magnitude and psychological correlates of smartphone use in medical students: A pilot study with a novel telemetric approach. Indian J Psychol Med. 2018;40:468–75. doi: 10.4103/IJPSYM.IJPSYM_133_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Thousand Oaks, CA: Sage Publications; 1988. pp. 31–67. [Google Scholar]
- 19.Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. 2012;6:121–7. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 20.Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Couns. 2006;9:135–47. [Google Scholar]
- 21.Chilukuri H, Bachali S, Naidu JN, Basha AS, Selvam VS. Perceived stress amongst medical and dental students. AP J Psychol Med. 2012;13:104–7. [Google Scholar]
- 22.Muthukrishnan S, Jain R, Kohli S, Batra S. Effect of mindfulness meditation on perceived stress scores and autonomic function tests of pregnant Indian women. J Clin Diagn Res. 2016;10:CC05. doi: 10.7860/JCDR/2016/16463.7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwon M, Kim DJ, Cho H, Yang S. The smartphone addiction scale: Development and validation of a short version for adolescents. PLoS One. 2013;8:e83558. doi: 10.1371/journal.pone.0083558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen B, Liu F, Ding S, Ying X, Wang L, Wen Y. Gender differences in factors associated with smartphone addiction: A cross-sectional study among medical college students. BMC Psychiatry. 2017;17:341. doi: 10.1186/s12888-017-1503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 26.Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara institute of medical sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. 2013;3:51–4. doi: 10.4103/2141-9248.109488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manzar MD, Moiz JA, Zannat W, Spence DW, Pandi-Perumal SR, BaHammam AS, et al. Validity of the Pittsburgh sleep quality index in Indian university students. Oman Med J. 2015;30:193. doi: 10.5001/omj.2015.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Albursan IS, Al Qudah MF, Dutton E, Hassan EM, Bakhiet SF, Alfnan AA, et al. National, sex and academic discipline difference in smartphone addiction: A study of students in Jordan, Saudi Arabia, Yemen and Sudan. Community Ment Health J. 2019;19:1–6. doi: 10.1007/s10597-019-00368-x. [DOI] [PubMed] [Google Scholar]
- 30.Mok JY, Choi SW, Kim DJ, Choi JS, Lee J, Ahn H, et al. Latent class analysis on internet and smartphone addiction in college students. Neuropsych Dis Treat. 2014;10:817. doi: 10.2147/NDT.S59293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi SW, Kim DJ, Choi JS, Ahn H, Choi EJ, Song WY, et al. Comparison of risk and protective factors associated with smartphone addiction and Internet addiction. J Behav Addict. 2015;4:308–14. doi: 10.1556/2006.4.2015.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahn H, Wijaya ME, Esmero BC. A systemic smartphone usage pattern analysis: Focusing on smartphone addiction issue. Int J Multimedia Ubiquitous Engineering. 2014;9:9–14. [Google Scholar]
- 33.Ibrahim NK, Baharoon BS, Banjar WF, Jar AA, Ashor RM, Aman AA, et al. Mobile phone addiction and its relationship to sleep quality and academic achievement of medical students at King Abdulaziz University, Jeddah, Saudi Arabia. J Res Health Sci. 2018;18:e00420. [PMC free article] [PubMed] [Google Scholar]
- 34.Samaha M, Hawi NS. Relationships among smartphone addiction, stress, academic performance, and satisfaction with life. Comput Human Behav. 2016;57:321–5. [Google Scholar]
- 35.Gligor Ş, Mozoş I. Indicators of smartphone addiction and stress score in university students. Wien Klin Wochenschr. 2018;6:1–6. doi: 10.1007/s00508-018-1373-5. [DOI] [PubMed] [Google Scholar]
- 36.Kim H. Exercise rehabilitation for smartphone addiction. J Exerc Rehabil. 2013;9:500–5. doi: 10.12965/jer.130080. [DOI] [PMC free article] [PubMed] [Google Scholar]


