Abstract
Background:
Infertility has deep psychological impacts on the sexual function of women such as a sense of fear, failure, and incompetence. It can also result in reduced sexual desire, unattained orgasm, and other sexual disorders. However, sexual education is assumed to improve the sexual function in these cases. Therefore, we study the effect of sexual education based on Sexual Health Model (SHM) on sexual function disorders in women with infertility.
Materials and Methods:
A singleblind, randomized controlled trial was conducted on 108 women with infertility (54 intervention group and 54 control group) aged between 18 and 40 years at the Milad Infertility Center of Mashhad in 2016. The intervention comprised three 90-min sessions administered during 1 week. At first, a pretest (Female Sexual Function Index [FSFI]) was completed, and 1 month after the end of the intervention, the posttest (FSFI) was completed. To analyze the data, independent t-test, Mann–Whitney test, and Wilcoxon test were run.
Results:
The mean (Standard Deviation [SD]) age of women and their spouses was 30.61 (5.42) and 34.42 (5.73)years, respectively. Results of Mann–Whitney test showed that after 1 month of intervention, there was a significant difference between intervention and control groups (Z = −4.87, p < 0.001). Moreover, results of Wilcoxon test showed a significant difference in the sexual function in the intervention group before and after the intervention (Z = 2.81, p < 0.001).
Conclusions:
Given the positive effects of SHM-based sexual education, this method could be considered as a subset of sexual education materials used for women with infertility suffering from sexual disorders.
Keywords: Infertility, Iran, sex education
Introduction
According to previous studies, infertility, an inability in conceiving after 1 year of continuous unprotected sex, is a major problem for about 50–80 millions of people worldwide.[1] The rate of infertility varies among different communities. The prevalence of infertility among American couples was estimated to be around 10%–15%[2] and for Iranians, the prevalence of infertility is reported to be 10.2%.[3] In general, infertility has deep psychological impacts on the sexual function, in particular in women.[4] In such state, sex is accompanied with a sense of fear, failure, and incompetence, or if it becomes forceful, it will cause reduced sexual desire, unattained orgasm, and other sexual disorders.[5]
Burgeoning body of evidence show that most of the women with infertility have suffered from sexual function disorders.[6,7,8] On the other hand, it is also believed that there is a significant correlation between sexual function disorders and infertility in women.[9,10,11] Despite these difficulties, many couples sense shame and feel guilty to speak about their sexual problems.[12] One solution to this problem is sexual education which helps people acquire information, attitude, and skills on sexual issues to enable couples in satisfying mutual needs and balancing individual, social, and family life.[13] Recently, numerous methods and models for sexual education have been proposed among which Sexual Health Model (SHM) is supposed to have some superiority because of its capacity to be provided for groups and its cost-effectiveness.[14]
The SHM gives people a theoretical framework to improve their sexual health through providing them with correct information, personal awareness, and self-acceptance. In fact, the SHM enables people to intimate and speak about their needs and sexual desires with their spouses in a clear, responsible, and respectful way and without unwanted behaviors or diseases. The SHM includes ten essential aspects of sexual health involving talking about sex; sexual anatomy functioning; challenges, culture, and sexual identity; sexual health care and safer sex; positive sexuality; body image; fantasy; relationships; intimacy; and spirituality.[15,16,17] Despite the major problems experienced by women with infertility and the effectiveness of SHM, no study has yet been conducted to assess the effect of SHM on sexual function of women with infertility. Therefore, we decided to study the effects of sexual education based on the SHM on sexual function disorders of women with infertility presenting at the Milad Infertility Center of Mashhad during June 21 to the end of September 2016.
Materials And Methods
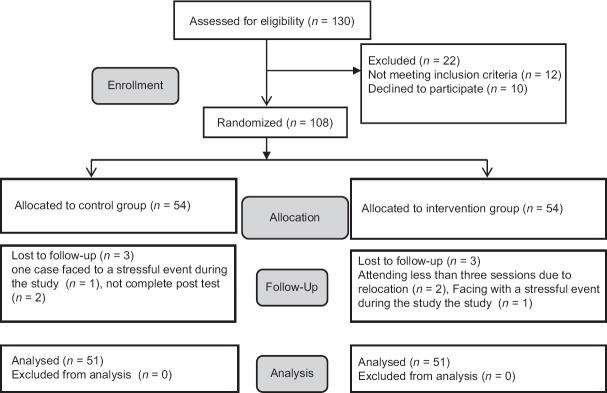
A singleblind, randomized controlled trial (IRCT2016102724469N2) was carried out on 108 women with infertility who were referred to the Milad Infertility Center from June 21 to the end of September 2016. Women with infertility were selected through available sampling from whom informed written consent was obtained. Qualified women were randomly divided into intervention and control groups using shuffled cards ( = 54). Using mean comparison formula with confidence level of 95% and statistical power of 80%, the sample size was determined to be 42 women in each group, accounting for 30% attrition set to the 54 women. Finally, six women withdrew (two attended <3 sessions, two had a stressful event during the study, and two did not complete the posttest). Hence, final analysis was restricted to questionnaires returned back from 102 women [Figure 1].
Figure 1.
Consort 2010 flow diagram
Inclusion criteria were being Iranian and Muslim, having education (at least reading and writing), speaking Persian language, aged between 18 and 40 years, primary infertility confirmed by a gynecologist, getting a score <28 in the Female Sexual Function Index (FSFI) questionnaire, having no stressful trauma during the last 6 months, not using medicine for sexual function, and not taking sexual or marital course or counseling during the last 6 months. Exclusion criteria were having organized program of mental or sexual education during the study period, experiencing any traumatic stressful event during the study period, having a history of sexual disorders, having no sexual intercourse during the study period, having severe degree based on the Depression Anxiety Stress Scales-21 (DASS-21), and being absent in the instructional sessions.
To gather information, each woman guided to a quiet room. Then, they were given the written informed consent form and some oral explanation about the project and if they agreed to participate and signed the form, they were interviewed based on a checklist to see if they are eligible for the study. Besides, they were given instruction on how to fill in the required questionnaire and asked to fill in demographic checklist as well as the FSFI and DASS-21 questionnaires. In order to assess homogeneity, both intervention and control groups were examined based on these measurements. The FSFI as the main measurement tool of this study is developed by Rosen et al. It includes 19 items assessed on a 5-point Likert scale and involves six subscales including sexual desire (1 and 2), sexual stimulation (3, 4, 5, and 6), sexual lubrication (7, 8, 9, and 10), orgasm (11, 12, and 13), pain (14, 15, and 16), and sexual satisfaction (17, 18, and 19). The scores range from 0 to 5 (0 = no sexual activity, 1 = almost never or never, 2 = a few times, 3 = sometimes, 4 = most of the times, and 5 = almost always or always). Score 0 represents no sexual activity during the last 4 weeks. The maximum score for each subscale is 6 and for total scale is 36. The minimum score for the domain of sexual desire is 1.2, the minimum score for the domains of sexual stimulation, sexual lubrication, orgasm, and pain is (0), and for the domain of satisfaction is 0.8, and for the total scale is 2. A higher score represents greater level of sexual function and a score <28 represents sexual function disorder.[18] The validity and reliability of the FSFI questionnaire in Iranian culture have been assessed previously by Mohammadi et al.[19] In this study, the FSFI questionnaire had an acceptable internal consistency as its Cronbach's alpha coefficient was 0.84.
Subsequently, three 90-minute instructional sessions were administered during 1 week in a quiet and uncrowded room. Each session consisted of speaking about the project purposes and some questions about sexual issues (10 min), education through lecturing and presentation (60 min), and finally, question and answer (20 min). The instructor's competence to provide sexual education was confirmed by professional advisors in this field after taking a course in sexual education. Sessions' content was programmed to cover ten aspects of the SHM considering Iranian culture and sexual problems as follows: in the first session, talking about sex, sexual anatomy functioning, and challenges; in the second session, culture and sexual identity, sexually health care and safer sex, and positive sexuality; in the third session, body image, fantasy, relationships and intimacy, and spirituality. The control group received routine care services and administered with no intervention. However, after the study, they received all education session contents in the form of pamphlets. One month after completion of the intervention, an examiner who was not aware of the participants' groups conducted the posttest.
Statistical analysis included descriptive statistics (i.e., the means and Standard Deviations [SD]) and statistical tests such as Mann–Whitney, Independent t-test, and Wilcoxon test. All analyses were performed using SPSS (Statistical Package for the Social Sciences, version 16.0, SPSS Inc. Chicago, Illinois, USA). Significance level was set at 0.05.
Ethical considerations
An informed consent was obtained from all the participants of the study. Also, participants had the complete freedom to leave the study at any stage if they did not want to continue. This study was confirmed by ethics committee of Mashhad University of Medical Sciences (IR.MUMS.REC.1395.116).
Results
The intervention and control group were comparable in terms of demographic characteristics. The obtained results of the study showed that there was no significant difference between the two groups regarding age (p = 0.87), duration of marriage (p = 0.79), duration of infertility (p = 0.97), duration of infertility treatment (p = 0.43) [Table 1]. Results of Mann–Whitney test showed that there was also no significant difference in sexual function score between intervention and control groups before intervention as the mean (SD) of intervention and control groups were 27.41 (30) and 26.72 (2.70), respectively. However, 1 month following the intervention, there was a significant difference (p < 0.002) between the groups as the mean (SD) sexual function score of the intervention and control were 30.10 (3.31) and 27.13 (3.22), respectively. Moreover, results obtained from Wilcoxon test showed that there was a significant difference in the sexual function score in the intervention group before and after the intervention (p < 0.001), but not in control group (p = 0.07). Moreover, following 1 month of intervention, Results of Mann–Whitney test showed that there were significant difference in three dimensions of sexual function: Sexual desire (Z = −1.37, p = 0.02), sexual lubrication (Z = −2.31, p = 0.02) and sexual satisfaction (Z = −2.34, p = 0.001) between intervention and control groups. Whereas, there were no significant difference in sexual stimulation (p = 0.08), orgasm (p = 0.06) and pain between intervention and control groups after the tests [Table 2].
Table 1.
Comparison of demographic characteristics in intervention and control groups
| Variable | Intervention group | Control group | t, Z | p |
|---|---|---|---|---|
| Age of women (years), mean (SD) | 30.27 (5.80) | 30.54 (5.20) | 0.16 | 0.87* |
| Age of husbands (years), mean (SD) | 34.52 (5.98) | 34.84 (5.65) | 0.27 | 0.56* |
| Duration of marriage (years), mean (SD) | 8.52 (4.65) | 8.77 (4.76) | 0.26 | 0.79* |
| Duration of infertility (years), mean (SD) | 6.51 (4.13) | 6.60 (4.39) | 0.34 | 0.97** |
| Duration of infertility treatment (years), mean (SD) | 5.27 (3.21) | 4.88 (3.29) | 0.77 | 0.43** |
| Depression anxiety stress (DASS-21), mean (SD) | 18.66 (5.71) | 18.96 (6.76) | −0.27 | 0.81* |
| Education level, n (%) | ||||
| Reading and writing literacy | 12 (23.50) | 4 (7.81) | -1.60 | 0.11** |
| High school | 23 (45.11) | 27 (56.93) | ||
| University education | 16 (31.42) | 20 (39.22) | ||
| Husbands education level | ||||
| Reading and writing literacy | 4 (7.80) | 2 (3.90) | 0.96 | 0.33** |
| High school | 26 (51.00) | 29 (56.93) | ||
| University education | 21 (41.20) | 20 (39.22) | ||
| Income | ||||
| Lower than adequacy | 14 (27.55) | 9 (17.60) | 0.75 | 0.44** |
| Adequate | 31 (60.80) | 37 (72.50) | ||
| Higher than adequacy | 11.81 | 5 (9.83) |
*Independent t-test, **Mann–Whitney. DASS: Depression Anxiety Stress Scales, SD: Standard deviation
Table 2.
Comparison of sexual function and its dimensions in women with infertility before and after sexual education in intervention and control groups
| Mean (SD) |
Z | p | ||
|---|---|---|---|---|
| Intervention group | Control group | |||
| Sexual desire | ||||
| Before education | 4.20 (1.11) | 4.30 (1.00) | −1.14 | 0.76* |
| After education | 5.21 (0.09) | 4.62 (1.00) | −1.37 | 0.02* |
| Test result (intragroup comparison) | p<0.001**Z=−1.20 | p=0.13**Z=−2.24 | ||
| Sexual stimulation | ||||
| Before education | 4.80 (0.91) | 4.51 (0.90) | −1.31 | 0.41* |
| After education | 0.50 (8.0) | 4.60 (09) | −1.73 | 0.08* |
| Test result (intragroup comparison) | p=0.02**Z=−2.34 | p=0.18**Z=−1.36 | ||
| Sexual lubrication | ||||
| Before education | 4.65 (0.90) | 4.30 (0.80) | −1.22 | 0.21* |
| After education | 84 (8.0) | 3.4 (9.00) | −2.31 | 0.02* |
| Test result (intragroup comparison) | p=0.02**Z=−2.34 | p=0.31**Z=−1.32 | ||
| Orgasm | ||||
| Before education | 4.40 (0.81) | 4.41 (0.71) | −1.31 | 0.18 |
| After education | 4.4 (9.0) | 4.41 (0.80) | −1.86 | 0.06* |
| Test result (intragroup comparison) | p=0.001**Z=−3.36 | p=0.15**Z=−1.45 | ||
| Pain | ||||
| Before education | 4.90 (0.80) | 4.50 (1.00) | −0.95 | 0.35* |
| After education | 4.72 (0.91) | 4.46 (1.00) | −1.86 | 0.09* |
| Test result (intragroup comparison) | p=0.01**Z=−2.48 | p=0.88**Z=−1.15 | ||
| Sexual satisfaction | ||||
| Before education | 4.70 (0.90) | 4.50 (1.00) | −0.76 | 0.44* |
| After education | 4.5 (8.0) | 4.62 (0.90) | −2.34 | 0.001* |
| Test result (intragroup comparison) | p<0.001**Z=−3.88 | p=0.66**Z=−1.41 | ||
| Sexual function | ||||
| Before education | 27.41 (3.00) | 26.72 (2.70) | 0.78 | 0.21* |
| After education | 30.10 (3.31) | 27.13 (3.22) | 2.81 | <0.001* |
| Test result (intragroup comparison) | p<0.001**Z=−4.87 | p=0.07**Z=−1.86 | ||
*Mann–Whitney, **Wilcoxon test. SD: Standard deviation
Discussion
In this study, we aimed to determine the effect of sexual education based on SHM on sexual function of women with infertility attended at Milad fertility center of Mashhad. Our results showed that sexual education based on (SHM) was an effective method to increase sexual function score of women with infertility. More specifically, there was a statistically significant difference in sexual desire, sexual lubrication, and sexual satisfaction between intervention and control groups. However, the differences in sexual stimulation, pain and orgasm was not statistically significant.
The results obtained in the study conducted by Behboodi Moghadam et al. showed that after sexual health education program, except for orgasm and pain, all dimensions of sexual functions were significantly improved.[20] Moreover, Smith et al. demonstrated that participating in a group sexuality appointment improved the mean scores of sexual function. In accordance with Smith et al., our results also suggested that while the highest changes were observed in the sexual desire, excitement, sexual satisfaction and vaginal moisture, the lowest changes were detected in the sexual pain and orgasm. Regarding orgasm, one explanation is that orgasm is a skill that needs to be practiced over a long time and therefore, it is natural to observe little change after just three session's educational programs. Pain may also be due to medical issues besides the fact that women with infertility might have been forced to have sex with reduced sexual desire and reduced sexual intercourse.[21]
Several studies have reported that sexual dysfunction, especially sexual stimulation is considered as an initial problem, which was in consistent with the results of the present study.[22,23] It is worth mentioning that the sexual stimulation in women has both mental and physical aspects, and in this study the physical aspect, women's sexual lubrication, but not the mental one has increased. It seems that more time is needed to work on the mental aspect of sexual stimulation.
In a study conducted by Sasanpur et al., it was reported that after ten sessions of cognitive restructuring education, the total score of couples' sexual problems and all its dimensions were significantly reduced.[13] Accordingly, Dehkordi et al. proposed a cognitive behavioral therapy as an effective method for sexual dysfunctions. Except for pain and orgasm, the results of the aforementioned studies were in consistent with the findings of our investigation.[24] One of the reasons for the observed differences in results could be the differences in the counseling methods.
Previous studies conducted by Rostamkhani et al. and Khakbazan et al. showed that sexual counseling based on Permission-Limited Information-Specific Suggestion-Intensive Therapy (PLISSIT) model improved all dimensions of sexual function. Apart from pain and orgasm, the results of these aforementioned studies were in consistent with our investigation.[25,26] The usage of different consulting methods could be a reason for this discrepancy. In addition, PLISSIT method is individualized therapy; whereas SHM model is a group-based therapy.
The results of a clinical trial conducted by Farnam et al. using The SHM model and PLISSIT methods showed that both methods significantly increased the mean of sexual function score and decreased the mean of score of sexual function stress. They reported that regarding combined outcomes, education based on PLISSIT model and SHM model had borderline significance differences. However, considering limited human resources, time, and costs, it seems that group-based education methods could be more cost effective.[14] The similarity of their results with those of the present study could be due to fact that they, like us, incorporated socio-cultural characteristics in their programs. Moreover, the results of SHM group showed that all domains of sexual function increased significantly, the results of these aforementioned studies were in consistent with our investigation except for orgasm and stimulation. Short follow up could be a reason for this discrepancy.
One of the important factors in the success of the SHM method is that it includes different aspects like cultural, sexual identity, and spirituality. We tried to use the education method based on the Iranian culture and problems. Ibrahimpure et al. reported that the lack of correct information and premarital sexual relationships (because of our religious and cultural tradition) cause considerable stress and anxiety in couples.[27] So, it seems reasonable to suggest that in such conditions, the educational programs be designed according to the culture of the country.
Another important factor for the success of the SHM model is the dimension of body image. It has been shown that women with infertility who has a poor body image might experience more psychological problems that could affect all aspects of their life. Similarly, Khorashadizade et al. showed that the sexual performance and general well-being were improved in women with infertility after improving their body image.[28] Moreover, Marvi et al. demonstrated that the sexual education could increase genital self-image in women with infertility and there were positive association between sexual satisfaction and genital self-image among women with infertility.[29,30]
The positive therapeutic function of the grouped-based therapy is another important factor in the success of SHM model. Removing the taboo of talking about sexual problems and as a result becoming aware of the ideas and experiences of other people with similar or even more severe problems can decrease sexual concerns and normalize their thoughts and behaviors. Smith et al. have shown that group therapy can be an effective alternative option for the treatment of sexual concerns by health care facilities with limited time.[14]
Our study suggests that SHM could improve the sexual function of women with infertility and could be implemented in group therapy programs. It is more cost-effective in terms of human resources, time, and costs. Moreover, SHM includes ten necessary aspects of sexual health and aims to remove sexual concerns.
One of the limitations of the present study was that clients had some stress and concerns about counseling, treatment, and diagnosis of infertility which might influence on their answers. To control this limitation at least in part, women were asked to fill in the questionnaires when they were prepared mentally. Other limitations were individual differences in being influenced by information presented at counseling sessions, and the influences of other sources like the mass media.
Conclusions
According to the positive effects of SHM-based sexual education, this method could be considered as a subset of sexual education materials used for women with infertility suffering from sexual disorders. The results of this study could be regarded as a ground for researchers to develop and evaluate other education-centered interventions.
Financial support and sponsorship
Mashhad University of Medical Sciences
Conflicts of interest
Nothing to declare.
Acknowledgment
This study was derived from a Master's thesis in Midwifery Consultation with the code number of 941576. We would like to express our gratitude to the honorable research council, respected professors, and all the personnel working in Milad Infertility Center for their sincere cooperation.
References
- 1.Kalkhoran LF, Bahrami H, Farrokhi NA, Zeraati H, Tarahomi M. Comparing anxiety, depression and sexual life satisfaction in two groups of fertile and infertile women in Tehran. J Reprod Infertil. 2011;12:157–63. [Google Scholar]
- 2.Masoumi SZ, Garousian M, Khani S, Oliaei SR, Shayan A. Comparison of quality of life, sexual satisfaction and marital satisfaction between fertile and infertile couples. Int J Fertil Steril. 2016;10:290–6. doi: 10.22074/ijfs.2016.5045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parsanezhad ME, Jahromi BN, Zare N, Keramati P, Khalili A, Parsa-Nezhad M. Epidemiology and etiology of infertility in Iran, systematic review and meta-analysis. J Womens Health. 2013;2:2. [Google Scholar]
- 4.Golmakani N, Zare Z, Amirian M, Mzlum R, Ahangar M. Compare marital satisfaction in fertile and infertile couples and Its relationship with sexual problems. J Obstet Gynecol Iran. 2014;18:1–10. [Google Scholar]
- 5.Boivin J, Griffiths E, Venetis CA. Emotional distress in infertile women and failure of assisted reproductive technologies: Meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alirezaie S, Ozgili G, Alavi H. Compare the efficacy and sexual function in fertile and infertile women. Public Health Cent Mashhad. 2013;3:131–6. [Google Scholar]
- 7.Bayar U, Basaran M, Atasoy N, Kokturk F, Arikan II, Barut A, et al. Sexual dysfunction in infertile couples: Evaluation and treatment of infertility. J Pak Med Assoc. 2014;64:138–45. [PubMed] [Google Scholar]
- 8.Mirblouk F, Asgharnia DM, Solimani R, Fakor F, Salamat F, Mansoori S. Comparison of sexual dysfunction in women with infertility and without infertility referred to Al-Zahra hospital in 2013-2014. Int J Reprod Biomed (Yazd) 2016;14:117–24. [PMC free article] [PubMed] [Google Scholar]
- 9.Aggarwal RS, Mishrah VV, Jasani AF. Incidence and prevalence of sexual dysfunction in infertile females. Midd East Fertil Soc J. 2013;18:187–90. [Google Scholar]
- 10.Ashraf DM, Ali D, Azadeh DM. Effect of infertility on sexual function: A cross-sectional study. J Clin Diagn Res. 2015;9:QC01–3. doi: 10.7860/JCDR/2015/11148.5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winkelman WD, Katz PP, Smith JF, Rowen TS. Infertility Outcomes Program Project Group. The sexual impact of infertility among women seeking fertility care. Sex Med. 2016;4:e190–7. doi: 10.1016/j.esxm.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nourani S, Jonaidy E, Shakeri MT, Mokhber N. Sexual satisfaction in fertile and infertile women attending state clinics in Mashad. J Reprod Infertil. 2010;10:269–77. [Google Scholar]
- 13.Sasanpur M, Shahurdian G, Ahmadi A. The impact of cognitive restructuring to decrease sexual problems and increase sexual satisfaction. Armaghane Danesh. 2015;19:994–1007. [Google Scholar]
- 14.Farnam F, Janghorbani M, Raisi F, Merghati-Khoei E. Compare the effectiveness of PLISSIT and sexual health models on women's sexual problems in Tehran, Iran: A randomized controlled trial. J Sex Med. 2014;11:2679–89. doi: 10.1111/jsm.12659. [DOI] [PubMed] [Google Scholar]
- 15.Robinson BB, Munns RA, Weber-Main AM, Lowe MA, Raymond NC. Application of the sexual health model in the long-term treatment of hypoactive sexual desire and female orgasmic disorder. Arch Sex Behav. 2011;40:469–78. doi: 10.1007/s10508-010-9673-5. [DOI] [PubMed] [Google Scholar]
- 16.Robinson BB, Scheltema K, Cherry T. Risky sexual behavior in low-income African American women: The impact of sexual health variables. J Sex Res. 2005;42:224–37. doi: 10.1080/00224490509552277. [DOI] [PubMed] [Google Scholar]
- 17.Robinson BE, Walter O. Masturbation and sexual health: An exploratory study of low income African American women. J Psychol Hum Sex. 2002;14:102. [Google Scholar]
- 18.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadi kh, Heydari M, Faghihzadeh S. The Female Sexual Function Index (FSFI): validation of the Iranian version. Payesh. 2008;7:269–78. [Google Scholar]
- 20.Behboodi Moghadam Z, Rezaei E, Khaleghi Yalegonbadi F, Montazeri A, Arzaqi SM, Tavakol Z, et al. The effect of sexual health education program on women sexual function in Iran. J Res Health Sci. 2015;15:124–8. [PubMed] [Google Scholar]
- 21.Smith WJ, Beadle K, Shuster EJ. The impact of a group psychoeducational appointment on women with sexual dysfunction. Am J Obstet Gynecol. 2008;198:697, e1–6. doi: 10.1016/j.ajog.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 22.Millheiser LS, Helmer AE, Quintero RB, Westphal LM, Milki AA, Lathi RB. Is infertility a risk factor for female sexual dysfunction? A case-control study. Fertil Steril. 2010;94:2022–5. doi: 10.1016/j.fertnstert.2010.01.037. [DOI] [PubMed] [Google Scholar]
- 23.Bokaie M, Simbar M, Yassini Ardekani SM. Sexual behavior of infertile women: A qualitative study. Iran J Reprod Med. 2015;13:645–56. [PMC free article] [PubMed] [Google Scholar]
- 24.Dehkordi MA, Mohammadi A, Alipour A, Mohtashami T. The impact of cognitive behavioral sex therapy on decreasing anxiety and increasing sexual function in people with vaginismus. Int J Health Stud. 2017;3 [Google Scholar]
- 25.Rostamkhani F, Jafari F, Ozgoli G, Shakeri M. Addressing the sexual problems of Iranian women in a primary health care setting: A quasi-experimental study. Iran J Nurs Midwifery Res. 2015;20:139–46. [PMC free article] [PubMed] [Google Scholar]
- 26.Khakbazan Z, Daneshfar F, Behboodi-Moghadam Z, Nabavi SM, Ghasemzadeh S, Mehran A. The effectiveness of the permission, limited information, specific suggestions, intensive therapy (PLISSIT) model based sexual counseling on the sexual function of women with multiple sclerosis who are sexually active. Mult Scler Relat Disord. 2016;8:113–9. doi: 10.1016/j.msard.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahimpure H, Jalambadani Z, Najjar AV, Dehnavieh R. First experience of intercourse in married women of Sabzevar city. A phenomenological study. Health Med. 2012;6:453. [Google Scholar]
- 28.Khorashadizade F, Karamidehkordi A, Rahsepar A, Hashemi M, Salari M, Esmaily H, et al. Determination of the association between body image with sexual function and marital adjustment in fertile and infertile women by path analysis modeling. J North Khorasan Univ Med Sci. 2011;3:23–31. [Google Scholar]
- 29.Marvi N, Golmakani N, Esmaeli H, Shareh H. Effect of sex education on infertile females' genital self-image. J Mazandaran Univ Med Sci. 2018;27:143–53. [Google Scholar]
- 30.Marvi N, Golmakani N, Esmaily H, Shareh H. The Relationship between Sexual Satisfaction and Genital Self-image in Infertile Women. J Midwifery Reprod Health. 2018;6:1468–75. [Google Scholar]