Abstract
Epithelial-to-mesenchymal transition (EMT) is an essential phenotypic conversion involved in cancer progression. Epidermal growth factor (EGF) and transforming growth factor (TGF)-β1 are potent inducers of the EMT. Tanshinone IIA (Tan IIA) is a phenanthrenequinone extracted from the root of Salvia miltiorrhiza Bunge, and its anticancer activity has been demonstrated in numerous studies. However, the mechanisms of action underlying Tan IIA in EGF- and TGF-β1-induced EMT in HepG2 cells remain unknown. Multiple assays were utilized in the present study, including colony formation, wound healing, Transwell invasion, immunofluorescence staining and western blotting, in order to assess the influence of Tan IIA on HepG2 cells induced by 20 ng/ml EGF and 10 ng/ml TGF-β1. The present study reported that Tan IIA treatment decreased EGF- and TGF-β1-enhanced cell colony numbers, migration and invasion, and inhibited EGF- and TGF-β1-induced decreases in the expression levels of E-cadherin, and increases in the expression levels of matrix metalloproteinase-2, N-cadherin, vimentin and Snail. In addition, it was observed that Tan IIA decreased the expression levels of phosphorylated (p)-Akt and p-ERK1/2 induced by EGF and TGF-β1. Furthermore, western blot analysis confirmed that blocking the function of PI3K/Akt and ERK with LY294002 and U0126 resulted in upregulation of E-cadherin expression, and downregulation of vimentin and Snail expression in EGF- and TGF-β1-treated HepG2 cells. In conclusion, to the best of our knowledge, the results of the present study are the first to indicate that Tan IIA may suppress EGF- and TGF-β1-induced EMT in HepG2 cells by deactivating the PI3K/Akt/ERK pathway.
Keywords: tanshinone IIA, epithelial-to-mesenchymal transition, epidermal growth factor, transforming growth factor-β1, PI3K/Akt/ERK
Introduction
Cancer, a major global public health problem, has been the first or second leading cause of mortality in the majority of countries thus far throughout the 21st century, and the incidence and mortality rates are rapidly increasing worldwide (1). Despite significant advances in the diagnosis and treatment of cancer, tumor metastasis is a major barrier to increasing life expectancy and favorable clinical outcomes, as >90% of cases of cancer-associated mortality occur as a result of metastatic disease (2,3).
In cancer, epithelial-to-mesenchymal transition (EMT) is associated with the metastatic process, tumor stemness and resistance to therapy (4). EMT is a cellular process in which cells lose their epithelial characteristics, acquire mesenchymal features and secrete matrix metalloproteinases (MMPs), which enable them to adopt more efficient motile and invasive properties. The common molecular markers of EMT include the loss of cell-cell adhesion mediated by downregulation of E-cadherin, and increased expression of mesenchymal markers (such as N-cadherin and vimentin), MMPs and transcription factors, including Twist, Slug and Snail (5). Increasing evidence has demonstrated that EMT can be induced by several growth factors, such as epidermal growth factor (EGF), the transforming growth factor (TGF) superfamily, vascular endothelial growth factor and fibroblast growth factor, produced by tumor-associated stroma (6–9). EGF activates the intrinsic protein-tyrosine kinase activity of its receptor EGFR on the cell surface and initiates signal transduction, such as the PI3K/Akt, Janus kinase and mitogen-activated protein kinase (MAPK)/ERK signaling pathways, which have been reported to serve important roles in the EMT process by regulating the expression of EMT biomarkers (10,11). TGF-β1 is one of the most potent inducers of EMT via activation of the classical Smad2/3 signaling pathway, or other downstream pathways (non-Smad signaling pathways), including the PI3K/Akt, ERK and c-Jun N-terminal kinase signaling pathways (12,13). Therefore, altering the EGF- and TGF-β1-mediated signaling pathways may be an efficient strategy to prevent EMT progression.
Tanshinone IIA (Tan IIA; C19H18O3), a phenanthrenequinone, is one of the major lipophilic components extracted from the medicinal herb Salvia miltiorrhiza Bunge (14). Over the past few decades, Tan IIA has been proven to possess potential protective effects against cardiac fibrosis, atherosclerosis, and cardiovascular and endocrine system diseases (15–18). The anticancer effects and underlying molecular mechanisms of Tan IIA have also been studied extensively in a number of different cancer cell types in vitro and tumor types in vivo (19). For example, studies have reported that Tan IIA causes apoptosis in a number of different types of cancer, including esophageal, colon, breast, lung and liver cancer (20–24). In addition, Tan IIA has been revealed to inhibit yes-associated protein 1 transcriptional activity, thereby inhibiting its effects on cervical carcinoma stem cell migration and invasion (25). Tan IIA has also been demonstrated to inhibit EMT in human bladder cancer cells via the STAT3-chemokine (C-C motif) ligand 2 signaling pathway (26). Tan IIA inhibits the migration and invasion of HNE-1NPC nasopharyngeal carcinoma cells through inhibition of MMP-2 and MMP-9 (27). However, the effects of Tan IIA on EGF- and TGF-β1-induced EMT processes and signaling molecules have not yet been investigated.
As the molecular interactions between PI3K/Akt and ERK signaling are prevalent in EGF- and TGF-β1-treated cancer cells, these interactions have significant roles in the initiation of EMT (28). Therefore, the present study aimed to investigate whether Tan IIA inhibits EMT, migration and invasion in EGF- and TGF-β1-treated HepG2 cells by deactivating these two signaling pathways, which, to the best of our knowledge, has not yet been reported. The present study could provide a novel insight into the anticancer molecular mechanisms of Tan IIA.
Materials and methods
Cell lines and reagents
The human liver cancer HepG2 cell line was purchased from the Cell Bank of the Institute of Biochemistry and Cell Biology, Chinese Academy of Sciences. The cells were grown in high-glucose DMEM supplemented with 10% FBS and 1% glutamine penicillin-streptomycin solution (all from Gibco; Thermo Fisher Scientific, Inc.) at 37°C in a 5% CO2 incubator. Tan IIA with a purity of >98% was purchased from the National Institutes for Food and Drug Control. Human recombinant EGF and TGF-β1 were purchased from PeproTech, Inc. MTT, LY294002 and U0126 were purchased from Sigma-Aldrich; Merck KGaA.
Cell viability assay
HepG2 cells were seeded in 96-well plates (5×103 cells/well) overnight in an incubator and treated with Tan IIA (0, 0.25, 0.5, 1, 2, 4 and 8 µM) for 24, 48 and 72 h at 37°C. A total of 20 µl 5 mg/ml MTT was added to each well, and the cells were incubated at 37°C for an additional 4 h in an incubator, the formazan was dissolved with 100 µl of DMSO. A microplate reader (Bio-Rad Laboratories, Inc.) was used to analyze the absorbance at a wavelength of 490 nm.
Morphology observations
HepG2 cells were seeded in 6-well plates (1×105 cells/well) overnight at 37°C, and treated with EGF (2.5, 5, 10 and 20 ng/ml) for 48 h. Cell morphology images were captured using a light microscope (magnification ×200, Olympus Corporation).
Colony formation assay
HepG2 cells were seeded in 6-well plates (1×103 cells/well) overnight, then co-treated with EGF (20 ng/ml)/TGF-β1 (10 ng/ml) and Tan IIA (0.5, 1 and 2 µM) at 37°C for 2 weeks. The cells were washed with PBS, fixed with 4% paraformaldehyde for 10 min at room temperature, and stained with 0.1% crystal violet for 20 min at room temperature. Colonies were imaged and counted using Image-Pro Plus software (version 6.0; National Institutes of Health).
Wound healing assay
HepG2 cells were seeded in a 6-well plate (3×105 cells/well) in 6-well plates and grown to 100% confluence. A wound was carefully made with a 10-µl pipette tip in the middle of the well, and the wells were washed with PBS. The cells were then incubated with fresh serum-free medium containing EGF (20 ng/ml)/TGF-β1 (10 ng/ml) with or without Tan IIA (0.5, 1.0 and 2.0 µM) for 24 h at 37°C, and images of cell migration were acquired at 0 and 24 h using an inverted light microscope (Olympus Corporation).
Transwell invasion assay
HepG2 cells (3×104 cells/well) in medium with 1% FBS containing Tan IIA (0.5, 1 and 2 µM) were cultured in the Matrigel-coated upper chamber of an 8-µm Transwell (Invitrogen; Thermo Fisher Scientific, Inc.), and 15% FBS medium containing EGF (20 ng/ml)/TGF-β1 (10 ng/ml) or not was added into the lower chamber. After 48 h of culture at 37°C in a 5% CO2 incubator, non-invasive cells on the upper side of the membrane were scraped with cotton swabs, and the cells on the lower surfaces were fixed with 4% paraformaldehyde for 10 min at room temperature and stained with 0.1% crystal violet for 20 min at room temperature. The invasive cells were imaged under a light microscope, and the crystal violet was dissolved in DMSO. The absorbance of the invasive cells was analyzed at a wavelength of 600 nm using a microplate reader (Bio-Rad Laboratories, Inc.) to indicate the invasion rates.
Immunofluorescence analysis
Cells (2×104 cells/well) in 4-well chamber slides were co-treated with EGF (20 ng/ml)/TGF- β1 (10 ng/ml) and Tan IIA (2 µM) for 48 h at 37°C. Immunofluo-rescence analysis was performed as previously described (7). After the cells were incubated overnight at 4°C with anti-E-cadherin (cat. no. 3195) and anti-vimentin (cat. no. 5741) antibodies (1:200 dilution; Cell Signaling Technology, Inc.), the cells were incubated with the corresponding secondary antibodies conjugated to fluorescein isothiocyanate (cat. no. 4412; 1:1,000; Cell Signaling Technology, Inc.) for 1 h at room temperature, and the nuclei were stained with DAPI (Beyotime Institute of Biotechnology) for 15 min at room temperature. Images were acquired using a Zeiss 880 laser confocal microscope (Zeiss AG).
Western blot analysis
Cells were seeded in 6-well culture plates (3×105 cells/well) and were untreated or co-treated with EGF (20 ng/ml)/TGF-β1 (10 ng/ml) and Tan IIA (2 µM)/LY294002 (20 µM)/U0126 (20 µM) for 48 h at 37°C. The total protein was extracted using RIPA buffer mixed with 1% PMSF (Beyotime Institute of Biotechnology), and the protein concentration was analyzed using a bicinchoninic acid protein assay kit (Nanjing KeyGen Biotech Co., Ltd.), as previously described (29). Equal amounts of total protein (30 µg) samples were separated by SDS-PAGE (8–12% gel) and transferred onto PVDF membranes (EMD Millipore). The membranes were then blocked in 5% skimmed milk for 3 h at room temperature and further incubated overnight at 4°C with primary antibodies against GAPDH (cat. no. 5174), E-cadherin (cat. no. 3195), N-cadherin (cat. no. 13116), MMP-2 (cat. no. 87809), Snail (cat. no. 3879), vimentin (cat. no. 5741), Akt (cat. no. 4691), phosphorylated (p)-Akt (cat. no. 4060), ERK1/2 (cat. no. 4695) and p-ERK1/2 (cat. no. 4376) (1:1,000 dilution; Cell Signaling Technology, Inc.). This was followed by incubation with the appropriate goat anti-rabbit IgG secondary antibodies (cat. no. AS014; 1:3,000; ABclonal Biotechnology Co., Ltd.) for 1 h at room temperature. The protein bands were visualized using an ECL reagent (EMD Millipore) and analyzed using the Tanon 5200 image acquisition system (Tanon Science and Technology Co., Ltd.), as previously described (30). The band intensity of western blotting was measured by densitometry using Image-Pro Plus J software (version 6.0; National Institutes of Health).
Statistical analysis
Data were statistically analyzed using SPSS software (version 23.0; IBM Corp.). Values are presented as the mean ± standard deviation using GraphPad Prism software (version 6.0; GraphPad Software, Inc.). One-way ANOVA followed by Duncan's post-hoc test was used for comparisons between multiple groups, while unpaired Student's t-test was used for comparisons between two groups. P<0.05 was considered to indicate a statistically significant difference.
Results
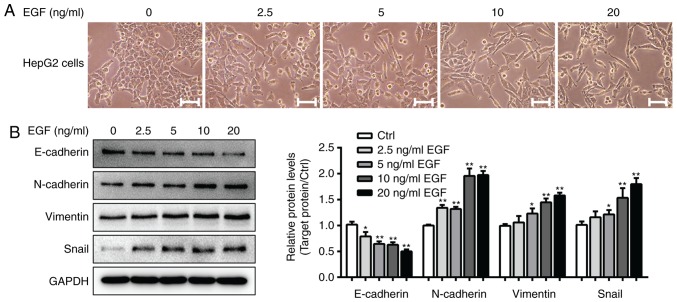
Establishment of the EGF-induced EMT model in HepG2 cells
Previous studies have demonstrated that HepG2 cells treated with 10 ng/ml TGF-β1 for 48 h exhibit fibroblast-like cell morphology, and a clearly induced EMT phenotype with significantly altered expression of EMT markers (7,31). The present study first established a model of EGF-induced EMT in HepG2 cells. As presented in Fig. 1A, control HepG2 cells grew in clusters and exhibited a classical cobblestone epithelial morphology and well-organized cell-cell associations, whereas HepG2 cells treated with EGF (5–20 ng/ml) exhibited an EMT-like cell morphology. The cells had a spindle-like mesenchymal morphology and were separated from one another. Furthermore, western blot analysis demonstrated that 20 ng/ml EGF treatment significantly decreased E-cadherin expression and increased N-cadherin, vimentin and Snail expression levels in EGF-treated cells compared with in cells from the control group (P<0.05; Fig. 1B). As a result, 20 ng/ml EGF and 10 ng/ml TGF-β1 were used to induce EMT in the subsequent experiments.
Figure 1.
EGF-induced EMT progression in HepG2 cells. (A) Morphological changes in HepG2 cells that were untreated or treated with 2.5, 5, 10 and 20 ng/ml EGF for 48 h (magnification, ×200; scale bars, 50 µm). (B) Protein expression levels of EMT biomarkers (E-cadherin, N-cadherin, vimentin and Snail) were determined via western blotting. *P<0.05, **P<0.01 vs. the control group. EGF, epidermal growth factor; EMT, epithelial-mesenchymal transition.
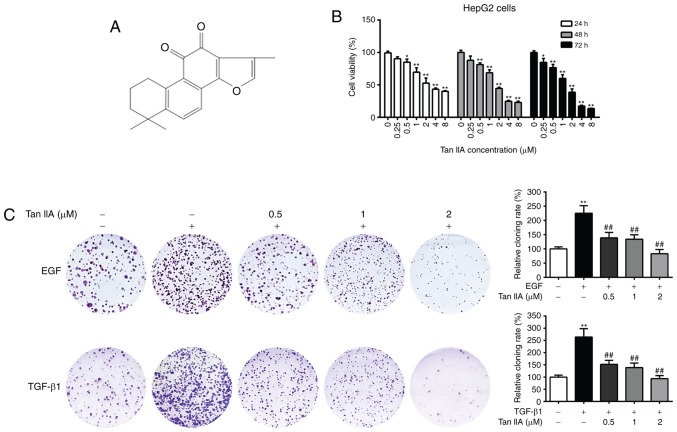
Tan IIA inhibits the viability and colony formation of HepG2 cells
The chemical structure of Tan IIA is presented in Fig. 2A. The cytotoxic effects of Tan IIA on HepG2 cells were evaluated by MTT assay. As presented in Fig. 2B, Tan IIA significantly suppressed HepG2 cell viability in a dose-dependent manner, and higher concentrations of Tan IIA (≥2 µM) time-dependently inhibited cell viability. The IC50 values of Tan IIA at 24, 48 and 72 h were 2.28, 1.62 and 1.13 µM, respectively. It has been reported that treatment with EGF and TGF-β1 promotes the malignant proliferation of cancer cells (32). In order to investigate the effects of Tan IIA on the EGF- and TGF-β1-mediated clonogenic potential of HepG2 cells, a colony formation assay was performed. The results demonstrated that EGF- and TGF-β1-treated HepG2 cells had significantly increased colony numbers compared with the untreated cells, while Tan IIA (0.5, 1 and 2 µM) treatment dose-dependently inhibited the clonogenic ability of EGF- and TGF-β1-treated HepG2 cells (P<0.05; Fig. 2C). These results indicated that Tan IIA exerted a strong inhibitory effect on the proliferation of HepG2 cells.
Figure 2.
Effects of Tan IIA on the viability and clonogenic potential of HepG2 cells. (A) Chemical structure of Tan IIA. (B) Cell viability analysis of HepG2 cells cultured in the presence of Tan IIA for 24, 48 and 72 h, by MTT assay. (C) Colony formation assay of HepG2 cells that were untreated or treated with 20 ng/ml EGF, 10 ng/ml TGF-β1 and Tan IIA (0.5, 1 and 2 µM) for 2 weeks. *P<0.05, **P<0.01 vs. the control group; ##P<0.01 vs. the EGF or TGF-β1 group. EGF, epidermal growth factor; Tan IIA, tanshinone IIA; TGF, transforming growth factor.
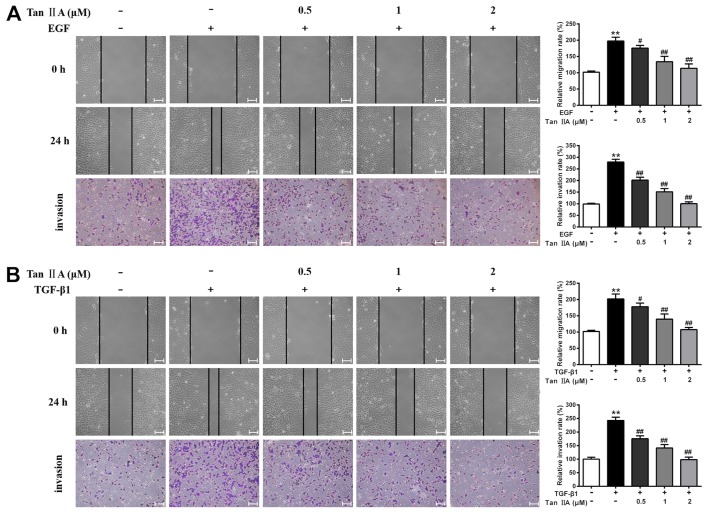
Tan IIA decreases the EGF- and TGF-β1-induced migration and invasion of HepG2 cells
Accumulating evidence has suggested that EGF and TGF-β1 can significantly enhance the motility of cancer cells (33). The present study investigated the effects of Tan IIA on the migratory and invasive abilities of EGF- and TGF-β1-treated HepG2 cells using wound healing and Transwell assays. The results revealed that the migratory and invasive potential of EGF- and TGF-β1-treated HepG2 cells was markedly higher than that of control cells, whereas Tan IIA (0.5, 1 and 2 µM) significantly inhibited EGF- and TGF-β1-enhanced cell migration and invasion in a dose-dependent manner (P<0.05; Fig. 3). In particular, treatment with 2 µM Tan IIA led to the most significant inhibition of EGF- and TGF-β1-induced proliferation, migration and invasion of HepG2 cells. Therefore, 2 µM Tan IIA was used for the subsequent experiments.
Figure 3.
Effects of Tan IIA on EGF- and TGF-β1-induced migration and invasion of HepG2 cells. The migration and invasion of HepG2 cells that were untreated or treated with (A) 20 ng/ml EGF, (B) 10 ng/ml TGF-β1 and Tan IIA (0.5, 1 and 2 µM) were analyzed by wound healing and Transwell assays, respectively. Scale bars, 100 µm. **P<0.01 vs. the control group; #P<0.05, ##P<0.01 vs. the EGF or TGF-β1 group. EGF, epidermal growth factor; Tan IIA, tanshinone IIA; TGF, transforming growth factor.
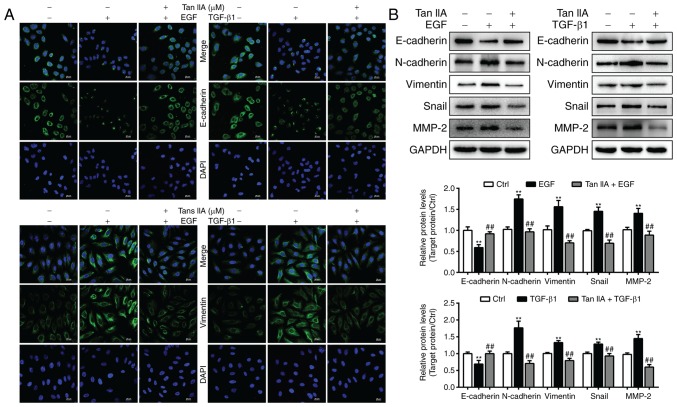
Tan IIA inhibits EGF- and TGF-β1-mediated induction of EMT biomarkers in HepG2 cells
To ascertain whether Tan IIA can inhibit EGF- and TGF-β1-induced EMT, the expression levels of the epithelial marker E-cadherin and the mesenchymal marker vimentin were analyzed in HepG2 cells by immunofluorescence staining. The results revealed that the expression levels of E-cadherin were markedly decreased in EGF- and TGF-β1-treated HepG2 cells, whereas vimentin expression was significantly elevated (Fig. 4A). Compared with in the two model groups, 2 µM Tan IIA markedly increased the expression levels of E-cadherin and decreased vimentin expression. In addition, the present study further analyzed the expression of EMT-associated biomarkers in HepG2 cells via western blotting. The results indicated that, in HepG2 cells, EGF- and TGF-β1-induced downregulation of E-cadherin expression, and upregulation of N-cadherin, vimentin, Snail and MMP-2 expression, was reversed by Tan IIA (Fig. 4B). These results confirmed that Tan IIA could effectively reverse EGF- and TGF-β1-induced EMT in HepG2 cells.
Figure 4.
Tan IIA reverses EGF- and TGF-β1-induced EMT in HepG2 cells. (A) E-cadherin and vimentin expression in HepG2 cells was determined by confocal microscopy. Scale bars, 20 µm. (B) Expression of E-cadherin, MMP-2, N-cadherin, vimentin and Snail in HepG2 cells that were untreated or treated with 20 ng/ml EGF, 10 ng/ml TGF-β1 and 2 µM Tan IIA were analyzed via western blotting. **P<0.01 vs. the control group; ##P<0.01 vs. the EGF or TGF-β1 group. EGF, epidermal growth factor; EMT, epithelial-mesenchymal transition; MMP, matrix metalloproteinase; Tan IIA, tanshinone IIA; TGF, transforming growth factor.
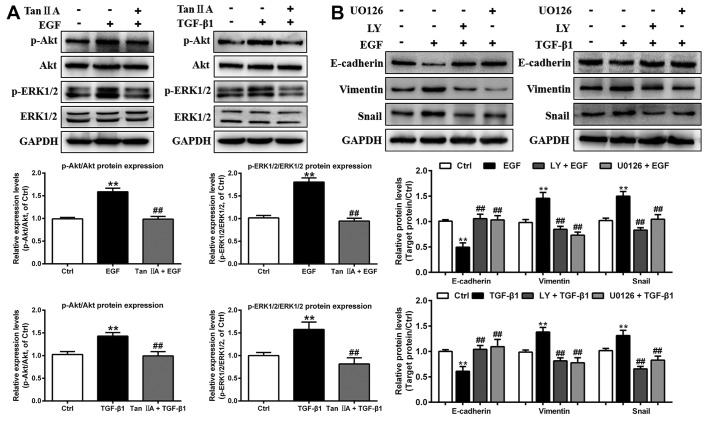
Tan IIA inhibits EGF- and TGF-β1-induced EMT in HepG2 cells by regulating the PI3K/Akt/ERK signaling pathway
In order to investigate the potential molecular mechanism underlying the inhibitory effect of Tan IIA on the EGF- and TGF-β1-induced EMT process in HepG2 cells, the expression levels of proteins in the PI3K/Akt/ERK pathway were investigated in cells treated with EGF and TGF-β1 using western blot analysis. As presented in Fig. 5A, treatment with 20 ng/ml EGF and 10 ng/ml TGF-β1 for 48 h strongly induced the phosphorylation of Akt and ERK1/2 (two downstream signaling molecules of PI3K), whereas total Akt and ERK1/2 expression levels were unchanged. However, Tan IIA treatment significantly decreased the upregulated p-Akt and p-ERK1/2 expression levels induced by EGF and TGF-β1.
Figure 5.
Tan IIA inhibits EMT by deactivating the PI3K/Akt/ERK signaling pathway in EGF- and TGF-β1-treated HepG2 cells. (A) Phosphorylation and expression of Akt and ERK1/2 in HepG2 cells that were untreated or treated with 20 ng/ml EGF, 10 ng/ml TGF-β1 and 2 µM Tan IIA were analyzed by western blotting. (B) Protein expression levels of E-cadherin, vimentin and Snail in HepG2 cells that were untreated or treated with 20 ng/ml EGF, 10 ng/ml TGF-β1, 20 µM LY, and 20 µM U0126 were analyzed by western blotting. **P<0.01 vs. the control group; ##P<0.01 vs. the EGF or TGF-β1 group. EGF, epidermal growth factor; EMT, epithelial-mesenchymal transition; LY, LY294002; p-, phosphorylated; Tan IIA, tanshinone IIA; TGF, transforming growth factor.
To further investigate the function of the PI3K/Akt/ERK signaling pathway in EGF- and TGF-β1-induced EMT in HepG2 cells, these cells were treated with the PI3K-specific inhibitor LY294002 and the MEK-specific inhibitor U0126. Compared with the groups treated with EGF or TGF-β1 alone, LY294002 and U0126 notably inhibited the protein expression levels of vimentin and Snail, and increased the protein expression levels of E-cadherin in EGF- and TGF-β1-treated HepG2 cells, consistent with the results of Tan IIA treatment (Fig. 5B). Overall, the results from the present study suggested that Tan IIA suppressed EGF- and TGF-β1-induced EMT via inhibition of the PI3K/Akt/ERK signaling pathways in HepG2 cells.
Discussion
EMT is a reversible cellular process that promotes tumor stemness, metastasis and resistance to therapy; the secretion of EGF or TGF-β1 by the tumor is associated with EMT progression (34,35). Previous studies have confirmed that TGF-β1 induces EMT in HepG2 cells (7,31); however, the association between EGF and HepG2 cells has rarely been reported. The present study first established an EMT model of HepG2 cells induced by EGF. The results demonstrated that in response to EGF, HepG2 cells lost their epithelial morphology and adopted a mesenchymal-like spindle-shaped morphology. The expression levels of two mesenchymal markers (N-cadherin and vimentin) and a transcriptional factor (Snail) were increased, whereas the expression levels of an epithelial marker (E-cadherin) were decreased. These results indicated that treatment of HepG2 cells with 20 ng/ml EGF for 48 h successfully promoted EMT.
Tan IIA, which is an effective therapeutic agent with multi-targeted actions, has been used to treat numerous human diseases in China (36). Analysis of the cancer cell death mechanism associated with Tan IIA has been provided by numerous studies. Notably, Tan IIA has been reported to significantly increase apoptotic cell death rate and decrease HepG2 cell-based tumor growth in nude mice by inhibiting CYP2J2 activity (37). Tan IIA may also cause apoptosis of HepG2 cells by inducing cell cycle arrest at the sub-G1 stages and by affecting the microRNA30b-p53-PTPN11/SHP2 signaling pathway (38). Additional reports have demonstrated that Tan IIA suppresses the invasive and migratory abilities of astrocytoma cells via the Notch-1 pathway (39), and inhibits TGF-β-induced EMT by inhibiting the Smad signaling pathway and transcription factors (40). However, the mechanism of action underlying Tan IIA in EGF- and TGF-β1-induced EMT in HepG2 cells remains unclear. The present study used HepG2 cells as a reliable model of EMT induced by EGF and TGF-β1 to investigate whether Tan IIA has antimetastatic effects in vitro. The results revealed that Tan IIA significantly inhibited the clonogenic ability of EGF- and TGF-β1-treated HepG2 cells in a dose-dependent manner. Furthermore, Tan IIA clearly inhibited the EGF- and TGF-β1-enhanced migration and invasion of HepG2 cells, as demonstrated using wound healing and Transwell assays. Immunofluorescence staining and western blotting revealed that Tan IIA rescued alterations in EMT-associated biomarker proteins (MMP-2, E-cadherin, N-cadherin, vimentin and Snail) induced by EGF and TGF-β1 in HepG2 cells, indicating that Tan IIA reversed EMT mediated by EGF and TGF-β1.
EGF binds to EGFR on the cell surface, which triggers classical EGF/EGFR signaling pathways resulting in upregulation of ERK1/2 and AKT phosphorylation (41). For example, EGF treatment induces EMT in pancreatic cancer cells via the integrin/EGFR-ERK/MAPK signaling pathway (42). Activated p-ERK1/2 and p-AKT mediate the process of EMT in human breast cancer MDA-MB-231 cells (43). Continuous EGF treatment has been demonstrated to upregulate Snail and Twist expression to induce EMT in prostate cancer PC-3 cells via the EGFR/PI3K/Akt/ERK signaling pathway (44). Despite the well-known role of the TGF-β1-induced Smad-dependent pathway in the EMT process, non-Smad signaling pathways mediated by TGF-β1 have also been demonstrated to serve a crucial role in cancer progression (7,45). In addition, the protein expression levels of p-ERK have been reported to be notably upregulated in TGF-β1-induced U-87 glioblastoma cells (46). The PI3K/Akt/mTOR signaling pathway activated by TGF-β1 is able to induce EMT in PANC-1, AsPC-1 (47) and HCT116 cells (48), consistent with the role of EGF. Therefore, it was hypothesized that deactivating the PI3K/Akt/ERK signaling pathway may reverse EMT in EGF- and TGF-β1-treated HepG2 cells. The present study demonstrated that treatment with Tan IIA significantly decreased EGF- and TGF-β1-mediated Akt and ERK phosphorylation in HepG2 cells. Furthermore, LY294002, a PI3K/Akt inhibitor, and U0126, an ERK inhibitor, increased the expression levels of E-cadherin, and inhibited the expression levels of vimentin and Snail in HepG2 cells treated with EGF and TGF-β1. Overall, the results from the present study indicated that Tan IIA may have an opposing role in EGF- and TGF-β1-induced EMT by inhibiting the activation of Akt and ERK phosphorylation. It has been reported that the Smad2/3 pathway also serves a predominant role in EMT in various types of cancer; however, the exact role of Smad proteins in TGF-β-induced EMT remains controversial and depends on an array of cofactors (49).
A limitation of the present study was that the EGF- and TGF-β1-induced EMT models used only involved the human liver cancer cell line HepG2. The value of this research could increase by performing all experiments in at least an additional authenticated liver cancer cell line. In addition, cell cycle analysis would demonstrate whether Tan IIA exerts any impact on cell proliferation in EGF- and TGF-β1-induced cell models, which would be worth investigating in further detail in future studies. Given that the anticancer activity of Tan IIA has attracted interest in the past decade, it is possible that Tan IIA also directly affects Smad signaling, and may have anti-EMT effects on other liver cancer cell lines treated with EGF or TGF-β1, as well as in animal models of metastasis in vivo. In addition, the investigation of Tan IIA alone on the proliferation and migration, as well as on the EMT markers of liver cancer cells, compared with the EGF- and TGF-β1-treated cells may also vastly increase the value of the research, which should be investigated in future studies.
In conclusion, the present study demonstrated the potential anti-EMT effects of Tan IIA in EGF- and TGF-β1-induced cell models. To the best of our knowledge, the present study is the first to suggest that Tan IIA efficiently targets the PI3K/Akt/ERK signaling pathway to suppress EGF- and TGF-β1-induced migration, invasion and EMT in HepG2 cells. Furthermore, these results suggested that Tan IIA could be developed as a potential therapeutic agent for the treatment of metastatic dissemination of cancer cells.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Special Foundation of High-Level University Construction for Valuable Chinese Herbal Medicines in China (grant no. E4640117112018).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
GW and SX conceived and designed the experiments. LZ coordinated the experiments and contributed to the interpretation of the data and manuscript writing. WL and HZ performed the immunofluorescence and western blotting assays. XC performed the cell experiments. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Mittal V. Epithelial mesenchymal transition in tumor metastasis. Annu Rev Pathol. 2018;13:395–412. doi: 10.1146/annurev-pathol-020117-043854. [DOI] [PubMed] [Google Scholar]
- 3.Mehlen P, Puisieux A. Metastasis: A question of life or death. Nat Rev Cancer. 2006;6:449–458. doi: 10.1038/nrc1886. [DOI] [PubMed] [Google Scholar]
- 4.Pastushenko I, Brisebarre A, Sifrim A, Fioramonti M, Revenco T, Boumahdi S, Van Keymeulen A, Brown D, Moers V, Lemaire S, et al. Identification of the tumour transition states occurring during EMT. Nature. 2018;556:463–468. doi: 10.1038/s41586-018-0040-3. [DOI] [PubMed] [Google Scholar]
- 5.Puisieux A, Brabletz T, Caramel J. Oncogenic roles of EMT-inducing transcription factors. Nat Cell Biol. 2014;16:488–494. doi: 10.1038/ncb2976. [DOI] [PubMed] [Google Scholar]
- 6.Said NA, Williams ED. Growth factors in induction of epithelial-mesenchymal transition and metastasis. Cells Tissues Organs. 2011;193:85–97. doi: 10.1159/000320360. [DOI] [PubMed] [Google Scholar]
- 7.Xing S, Yu W, Zhang X, Luo Y, Lei Z, Huang D, Lin J, Huang Y, Huang S, Nong F, et al. Isoviolanthin extracted from dendrobium officinale reverses TGF-β1-mediated epithelial-mesenchymal transition in hepatocellular carcinoma cells via deactivating the TGF-β/Smad and PI3K/Akt/mTOR signaling pathways. Int J Mol Sci. 2018;19(pii):E1556. doi: 10.3390/ijms19061556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fantozzi A, Gruber DC, Pisarsky L, Heck C, Kunita A, Yilmaz M, Meyer-Schaller N, Cornille K, Hopfer U, Bentires-Alj M, Christofori G. VEGF-mediated angiogenesis links EMT-induced cancer stemness to tumor initiation. Cancer Res. 2014;74:1566–1575. doi: 10.1158/0008-5472.CAN-13-1641. [DOI] [PubMed] [Google Scholar]
- 9.Mori S, Kodaira M, Ito A, Okazaki M, Kawaguchi N, Hamada Y, Takada Y, Matsuura N. Enhanced expression of integrin αvβ3 induced by TGF-β Is required for the enhancing effect of fibroblast growth factor 1 (FGF1) in TGF-β-induced epithelial-mesenchymal transition (EMT) in mammary epithelial cells. PLoS One. 2015;10:e0137486. doi: 10.1371/journal.pone.0137486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grassi ML, Palma CS, Thome CH, Lanfredi GP, Poersch A, Faca VM. Proteomic analysis of ovarian cancer cells during epithelial-mesenchymal transition (EMT) induced by epidermal growth factor (EGF) reveals mechanisms of cell cycle control. J Proteomics. 2017;151:2–11. doi: 10.1016/j.jprot.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 11.Stewart TA, Azimi I, Brooks AJ, Thompson EW, Roberts-Thomson SJ, Monteith GR. Janus kinases and Src family kinases in the regulation of EGF-induced vimentin expression in MDA-MB-468 breast cancer cells. Int J Biochem Cell Biol. 2016;76:64–74. doi: 10.1016/j.biocel.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Miyazono K. Transforming growth factor-beta signaling in epithelial-mesenchymal transition and progression of cancer. Proc Jpn Acad Ser B Phys Biol Sci. 2009;85:314–323. doi: 10.2183/pjab.85.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ren W, Zhang Y, Zhang L, Lin Q, Zhang J, Xu G. Overexpression of collagen type V α1 chain in human breast invasive ductal carcinoma is mediated by TGF-β1. Int J Oncol. 2018 Mar 15; doi: 10.3892/ijo.2018.4317. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 14.Li ZM, Xu SW, Liu PQ. Salvia miltiorrhiza Burge (Danshen): A golden herbal medicine in cardiovascular therapeutics. Acta Pharmacol Sin. 2018;39:802–824. doi: 10.1038/aps.2017.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang L, Zhu J, Zheng M, Zou R, Zhou Y, Zhu M. Tanshinone IIA protects against subclinical lipopolysaccharide induced cardiac fibrosis in mice through inhibition of NADPH oxidase. Int Immunopharmacol. 2018;60:59–63. doi: 10.1016/j.intimp.2018.04.036. [DOI] [PubMed] [Google Scholar]
- 16.Chen W, Tang F, Xie B, Chen S, Huang H, Liu P. Amelioration of atherosclerosis by tanshinone IIA in hyperlipidemic rabbits through attenuation of oxidative stress. Eur J Pharmacol. 2012;674:359–364. doi: 10.1016/j.ejphar.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 17.Gao S, Liu Z, Li H, Little PJ, Liu P, Xu S. Cardiovascular actions and therapeutic potential of tanshinone IIA. Atherosclerosis. 2012;220:3–10. doi: 10.1016/j.atherosclerosis.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 18.Lu BL, Li J, Zhou J, Li WW, Wu HF. Tanshinone IIA decreases the levels of inflammation induced by Aβ1–42 in brain tissues of Alzheimer's disease model rats. Neuroreport. 2016;27:883–893. doi: 10.1097/WNR.0000000000000618. [DOI] [PubMed] [Google Scholar]
- 19.Cao YF, Wang SF, Li X, Zhang YL, Qiao YJ. The anticancer mechanism investigation of Tanshinone IIA by pharmacological clustering in protein network. BMC Syst Biol. 2018;12:90. doi: 10.1186/s12918-018-0606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu YQ, Wang BY, Wu F, An YK, Zhou XQ. Influence of tanshinone IIA on the apoptosis of human esophageal Ec-109 cells. Nat Prod Commun. 2016;11:17–19. [PubMed] [Google Scholar]
- 21.He L, Gu K. Tanshinone IIA regulates colorectal cancer apoptosis via attenuation of Parkin-mediated mitophagy by suppressing AMPK/Skp2 pathways. Mol Med Rep. 2018;18:1692–1703. doi: 10.3892/mmr.2018.9087. [DOI] [PubMed] [Google Scholar]
- 22.Su CC, Chien SY, Kuo SJ, Chen YL, Cheng CY, Chen DR. Tanshinone IIA inhibits human breast cancer MDA-MB-231 cells by decreasing LC3-II, Erb-B2 and NF-κBp65. Mol Med Rep. 2012;5:1019–1022. doi: 10.3892/mmr.2012.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim EO, Kang SE, Im CR, Lee JH, Ahn KS, Yang WM, Um JY, Lee SG, Yun M. Tanshinone IIA induces TRAIL sensitization of human lung cancer cells through selective ER stress induction. Int J Oncol. 2016;48:2205–2212. doi: 10.3892/ijo.2016.3441. [DOI] [PubMed] [Google Scholar]
- 24.Lin CY, Chang TW, Hsieh WH, Hung MC, Lin IH, Lai SC, Tzeng YJ. Simultaneous induction of apoptosis and necroptosis by Tanshinone IIA in human hepatocellular carcinoma HepG2 cells. Cell Death Discov. 2016;2:16065. doi: 10.1038/cddiscovery.2016.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qin J, Shi H, Xu Y, Zhao F, Wang Q. Tanshinone IIA inhibits cervix carcinoma stem cells migration and invasion via inhibiting YAP transcriptional activity. Biomed Pharmacother. 2018;105:758–765. doi: 10.1016/j.biopha.2018.06.028. [DOI] [PubMed] [Google Scholar]
- 26.Huang SY, Chang SF, Liao KF, Chiu SC. Tanshinone IIA inhibits epithelial-mesenchymal transition in bladder cancer cells via modulation of STAT3-CCL2 signaling. Int J Mol Sci. 2017;18(pii):E1616. doi: 10.3390/ijms18081616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou M, Zhou G, Hu S, Zhang L. Tanshinone IIA suppress the proliferation of HNE-1 nasopharyngeal carcinoma an in vitro study. Saudi J Biol Sci. 2018;25:267–272. doi: 10.1016/j.sjbs.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu H, He Y, Qi L, Chen L, Luo Y, Chen L, Li Y, Zhang N, Guo H. cPLA2α activates PI3K/AKT and inhibits Smad2/3 during epithelial-mesenchymal transition of hepatocellular carcinoma cells. Cancer Lett. 2017;403:260–270. doi: 10.1016/j.canlet.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 29.Xing S, Zhang X, Ke H, Lin J, Huang Y, Wei G. Physicochemical properties of polysaccharides from Dendrobium officinale by fractional precipitation and their preliminary antioxidant and anti-HepG2 cells activities in vitro. Chem Cent J. 2018;12:100. doi: 10.1186/s13065-018-0471-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng Z, Wei W, Wu Z, Wang J, Ding X, Sheng Y, Han Y, Wu Q. ARPC2 promotes breast cancer proliferation and metastasis. Oncol Rep. 2019;41:3189–3200. doi: 10.3892/or.2019.7113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng G, Zeng S, Ma J, Zhang Y, Qu Y, Han Y, Yin L, Cai C, Guo C, Shen H. The anti-tumor activities of Neferine on cell invasion and oxaliplatin sensitivity regulated by EMT via Snail signaling in hepatocellular carcinoma. Sci Rep. 2017;7:41616. doi: 10.1038/srep41616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gore J, Deitz SL, Wilson JL, Korc M. Abstract 969: TGF-beta cross-talks with the EGF receptor family to promote proliferation of pancreatic cancer cells with dysfunctional RB. Cancer Res. 2014;74:969. [Google Scholar]
- 33.Xu ZH, Jiang YY, Steed H, Davidge S, Fu YX. TGFβ and EGF synergistically induce a more invasive phenotype of epithelial ovarian cancer cells. Biochem Biophys Res Commun. 2010;401:376–381. doi: 10.1016/j.bbrc.2010.09.059. [DOI] [PubMed] [Google Scholar]
- 34.Wendt MK, Allington TM, Schiemann WP. Mechanisms of the epithelial-mesenchymal transition by TGF-beta. Future Oncol. 2009;5:1145–1168. doi: 10.2217/fon.09.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu ZM, Ghosh S, Wang ZY, Hunter T. Downregulation of caveolin-1 function by EGF leads to the loss of E-cadherin, increased transcriptional activity of beta-catenin, and enhanced tumor cell invasion. Cancer Cell. 2003;4:499–515. doi: 10.1016/S1535-6108(03)00304-0. [DOI] [PubMed] [Google Scholar]
- 36.Xu S, Liu P. Tanshinone II-A: New perspectives for old remedies. Expert Opin Ther Pat. 2013;23:149–153. doi: 10.1517/13543776.2013.743995. [DOI] [PubMed] [Google Scholar]
- 37.Jeon YJ, Kim JS, Hwang GH, Wu Z, Han HJ, Park SH, Chang W, Kim LK, Lee YM, Liu KH, Lee MY. Inhibition of cytochrome P450 2J2 by tanshinone IIA induces apoptotic cell death in hepatocellular carcinoma HepG2 cells. Eur J Pharmacol. 2015;764:480–488. doi: 10.1016/j.ejphar.2015.07.047. [DOI] [PubMed] [Google Scholar]
- 38.Ren X, Wang C, Xie B, Hu L, Chai H, Ding L, Tang L, Xia Y, Dou X. Tanshinone IIA induced cell death via miR30b-p53-PTPN11/SHP2 signaling pathway in human hepatocellular carcinoma cells. Eur J Pharmacol. 2017;796:233–241. doi: 10.1016/j.ejphar.2016.11.046. [DOI] [PubMed] [Google Scholar]
- 39.Dong W, Zhang Y, Chen X, Jia Y. High-dose tanshinone iia suppresses migration and proliferation while promoting apoptosis of astrocytoma cells via Notch-1 pathway. Neurochem Res. 2018;43:1855–1861. doi: 10.1007/s11064-018-2601-0. [DOI] [PubMed] [Google Scholar]
- 40.Duan H, Ma L, Liu H, Zhang Y, Zhang Z, Yan X, Li X. Tanshinone IIA attenuates epithelial-mesenchymal transition to inhibit the tracheal narrowing. J Surg Res. 2016;206:252–262. doi: 10.1016/j.jss.2016.04.066. [DOI] [PubMed] [Google Scholar]
- 41.Pan M, Schinke H, Luxenburger E, Kranz G, Shakhtour J, Libl D, Huang Y, Gaber A, Pavšič M, Lenarčič B, et al. EpCAM ectodomain EpEX is a ligand of EGFR that counteracts EGF-mediated epithelial-mesenchymal transition through modulation of phospho-ERK1/2 in head and neck cancers. PLoS Biol. 2018;16:e2006624. doi: 10.1371/journal.pbio.2006624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sheng W, Chen C, Dong M, Wang G, Zhou J, Song H, Li Y, Zhang J, Ding S. Calreticulin promotes EGF-induced EMT in pancreatic cancer cells via Integrin/EGFR-ERK/MAPK signaling pathway. Cell Death Dis. 2017;8:e3147. doi: 10.1038/cddis.2017.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhat FA, Sharmila G, Balakrishnan S, Arunkumar R, Elumalai P, Suganya S, Raja Singh P, Srinivasan N, Arunakaran J. Quercetin reverses EGF-induced epithelial to mesenchymal transition and invasiveness in prostate cancer (PC-3) cell line via EGFR/PI3K/Akt pathway. J Nutr Biochem. 2014;25:1132–1139. doi: 10.1016/j.jnutbio.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 44.Tsai PC, Fu YS, Chang LS, Lin SR. Taiwan cobra cardiotoxin III suppresses EGF/EGFR-mediated epithelial-to-mesenchymal transition and invasion of human breast cancer MDA-MB-231 cells. Toxicon. 2016;111:108–120. doi: 10.1016/j.toxicon.2016.01.051. [DOI] [PubMed] [Google Scholar]
- 45.Liu Z, Kuang W, Zhou Q, Zhang Y. TGF-β1 secreted by M2 phenotype macrophages enhances the stemness and migration of glioma cells via the SMAD2/3 signalling pathway. Int J Mol Med. 2018;42:3395–3403. doi: 10.3892/ijmm.2018.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ouanouki A, Lamy S, Annabi B. Anthocyanidins inhibit epithelial-mesenchymal transition through a TGFβ/Smad2 signaling pathway in glioblastoma cells. Mol Carcinog. 2017;56:1088–1099. doi: 10.1002/mc.22575. [DOI] [PubMed] [Google Scholar]
- 47.Pei Z, Fu W, Wang G. A natural product toosendanin inhibits epithelial-mesenchymal transition and tumor growth in pancreatic cancer via deactivating Akt/mTOR signaling. Biochem Biophys Res Commun. 2017;493:455–460. doi: 10.1016/j.bbrc.2017.08.170. [DOI] [PubMed] [Google Scholar]
- 48.Han S, Bui NT, Ho MT, Kim YM, Cho M, Shin DB. Dexamethasone inhibits TGF-β1-induced cell migration by regulating the ERK and AKT pathways in human colon cancer cells Via CYR61. Cancer Res Treat. 2016;48:1141–1153. doi: 10.4143/crt.2015.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fuxe J, Vincent T, Garcia de Herreros A. Transcriptional crosstalk between TGF-β and stem cell pathways in tumor cell invasion: Role of EMT promoting Smad complexes. Cell Cycle. 2010;9:2363–2374. doi: 10.4161/cc.9.12.12050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.