Abstract
With the decrease in PSA screening based on the 2011 United States Preventive Services Task Force guidelines and the potential approval of highly sensitive imaging techniques over the next few years, we are likely to see an increasing trend of metastatic prostate cancer diagnosis. Traditional therapy for nonmetastatic prostate cancer (nmPC) has consisted of androgen deprivation therapy (ADT) followed by other hormonal therapy maneuvers, such as anti-androgen withdrawal, herbal preparations, low dose steroids, or ketoconazole. Androgen receptor-axis-targeted therapies (ARAT) were previously only approved for patients with metastatic castration resistant prostate cancer (mCRPC). This has recently changed after reporting of results from the SPARTAN and PROSPER trials, which were conducted in nonmetastatic CRPC (nmCRPC) patients. These studies demonstrated improved metastasis-free survival with apalutamide and enzalutamide, each compared to placebo in a double blind randomized setting. In 2017, the LATITUDE and STAMPEDE studies demonstrated marked survival benefit with early abiraterone and prednisone in patients with metastatic hormone sensitive prostate cancer (mHSPC) in addition to ADT. Other second-generation AR antagonists are currently in phase 3 trials in mHSPC and nmCRPC. This article summarizes the key clinical trials that led to FDA approval of ARAT in the mHSPC and nmCRPC settings and highlights potential limitations, future directions, and treatment-algorithms when selecting patients for early therapy in mHSPC and NMPC.
1. Introduction
For decades, the controversy of early versus delayed treatment had been raging in prostate cancer therapy. Prior to the routine acceptance of therapy in asymptomatic disease, studies such as the Medical Research Council trial were conducted comparing early versus delayed androgen deprivation therapy (ADT), even in the metastatic setting [1]. Now systemic androgen receptor (AR)-axis-targeted therapies (ARAT) are approved by the FDA even in the setting of prostate cancer with no evidence of metastases. Two second-generation androgen receptor antagonists, enzalutamide and apalutamide, demonstrated a metastasis free survival (MFS) benefit compared to placebo in patients with nonmetastatic castration resistant prostate cancer (nmCRPC) [2, 3]. Abiraterone, an inhibitor of CYP17A1, showed an overall survival (OS) benefit in metastatic hormone sensitive prostate cancer (mHSPC) and received FDA approval for this indication [4]. A subset of patients within the STAMPEDE trial [5] had high-risk nonmetastatic hormone sensitive prostate cancer and also showed a treatment benefit.
Between 1950 and 2000, ADT had been the only systemic therapy available for advanced prostate cancer, and it was primarily used in the therapy of metastatic disease. Subsequently, systemic therapy was evaluated after failure of ADT, and this disease state was defined as hormone refractory, androgen independent, or castration resistant prostate cancer. Mitoxantrone and docetaxel chemotherapies were approved by the FDA given their palliative benefit and OS benefit in mCRPC, respectively [5, 6]. Over the last decade, sipuleucel-T, cabazitaxel, and radium-223 each showed an OS benefit in metastatic castration resistant prostate cancer (mCRPC) patients and were approved by the FDA [7, 8]. A better understanding of mechanisms of castration resistance, such as i) inappropriate restoration of androgen receptor signaling, ii) intratumoral and extragonadal androgen synthesis, and iii) androgen receptor mutations, has led to the development of new targeted therapies, initially for mCRPC patients [9]. Now, multiple clinical trials in prostate cancer are investigating the role of these contemporary therapies in earlier disease, starting with mHSPC, and culminating with the recently completed and reported trials in nmCRPC and in high-risk hormone sensitive nonmetastatic prostate cancer (nmHSPC).
We review the levels of evidence and the nuances of considering therapy early in nonmetastatic prostate cancer. We discuss the pivotal trials supporting the new indications in terms of efficacy and safety and present potential treatment algorithms. The importance of a careful risk/benefit discussion with the patient and shared decision-making are emphasized. A discussion of potential pitfalls of the earlier introduction of androgen receptor-targeting drugs is included along with pointers for patient and tumor characteristics that can be factored into guiding therapeutic selection.
2. ARAT Therapies in mCRPC
Testosterone is synthesized from weakly active dehydroepian-drosterone and androstenedione by cytochrome P450 (CYP) 11A1 and CYP17A1 [10]. Abiraterone is a selective and irreversible inhibitor of CYP17A1 and impairs AR signaling by depleting adrenal and intratumoral androgens [10]. In the phase 3 COU-AA301 trial, abiraterone plus prednisone was compared against placebo in patients with mCRPC who had progressed on docetaxel. The study showed improved OS with a median of 14.8 months compared to 10.9 months [hazard ratio (HR) = 0.65, 95% CI 0.54–0.77,p <0.001] [11]. This led to the FDA approval of abiraterone for mCRPC patients in 2011. Subsequently, in 2013, the phase 3 COU-AA 302 trial reported OS and radiographic progression benefit by abiraterone in chemotherapy naive mCRPC patients [12].
Enzalutamide (formerly MDV3100) is an inhibitor of AR signaling that exerts its activity by binding to the ligand-binding domain of the AR, competing with and displacing the natural ligands of the receptor (testosterone and dihydrotestosterone) while also inhibiting the translocation of the androgen receptor into the nucleus and impairing transcription of its target genes [13]. It lacks the androgen agonist activity seen with first generation AR blockers. In the AFFIRM phase 3 trial, enzalutamide was compared to placebo in patients with chemotherapy-refractory mCRPC at a dose of 160 mg daily in 2:1 randomization. At the interim analysis, improved OS with a median of 18.4 months with enzalutamide compared to 13.6 months for placebo was seen [14]. This resulted in FDA approval in 2012 for chemotherapy-refractory mCRPC. The results of the PREVAIL trial reported in 2014 led to the approval of enzalutamide for the chemotherapy-naïve patient population based on an OS difference and delay in initiation of cytotoxic chemotherapy compared to placebo [15].
With a tolerable safety profile and remarkable efficacy in mCRPC, ARAT therapies were rapidly moved to earlier settings of evaluation and therapy.
3. Metastatic Hormone-Sensitive Prostate Cancer
ADT had been the mainstay of treatment for newly diagnosed mHSPC patients until 2014. Resistance to ADT occurs after approximately 24 months; hence, attempts were made to improve outcomes by incorporating cytotoxic chemotherapy earlier in the treatment plan [16]. The results of the CHAARTED [17], STAMPEDE Arm C [18], and GETUG-AFU 15 [19] phase 3 studies brought forth docetaxel plus ADT as a new standard of care in mHSPC patients who are fit to receive chemotherapy, with significant improvement in OS (51 vs 34 months in CHAARTED) (Table 1). The subset of patients with high volume/extensive (four or more bone lesions or visceral involvement) disease, which constituted 62% of the patients enrolled in CHAARTED, had a large magnitude of benefit with median survival changing from 32.2 to 49.2 months (p < 0.001) [17]. However, barriers, such as advanced age, neurotoxicity, co-existing illnesses, and lack of social and family support, pose challenges to the administration of cytotoxic chemotherapy. In addition, chemotherapy related deaths, including complications, such as hepatotoxicity, neutropenic infections, and myelosuppression, were observed in all of these studies [17–19].
Table 1.
Recently completed phase 3 trials of ARAT in the hormone-sensitive and nmCRPC settings
| Trial | Patient population | Treatment arms | Outcomes |
|---|---|---|---|
| Hormone-sensitive | |||
| CHAARTED [17] (for comparison) | mHSPC (high volume [visceral metastases or ≥ 4 bone lesions with ≥>1 beyond the vertebral bodies and pelvis] vs. low volume). | • ADT (n = 393) • ADT plus docetaxel (n = 397) |
• Significant improvement in OS with the addition of chemotherapy of 57.6 vs 44months with HR of 0.61 and p < 0.001 |
| LATITUDE [20] | High-risk mHSPC (2/3 criteria: Gleason score of ≥8), at least three bone lesions, and the presence of measurable visceral metastasis) | • ADT (n = 602) • ADT plus abiraterone (n = 597) |
• Significant improvement in OS with the addition of abiraterone to ADT (NR vs. 34.7 mo; HR 0.62; 95% CI 0.51–0.76; p <0.001). |
| STAMPEDE G [21] | nmHSPC (high-risk locally advanced with 2/3 features: i)T3 or T4, ii) Gleason score of ≥8 iii) a PSA level ≥ 40 ng/ml and high-risk relapsed with i)PSA ≥4 ng/ml with PSADT<6 months or ii) PSA ≥ 20 ng/ml) and mHSPC | • ADT (n = 957) • ADT plus abiraterone (n = 960) |
• Significant improvement in three-year OS with the addition of abiraterone to ADT (83 vs. 76%; HR 0.63; 95% CI 0.52–0.76; p <0.001). • OS significantly improved in the mHSPC but not in the nmHSPC patients |
| Nonmetastatic CRPC | |||
| PROSPER [2] | nmCRPC (PSADT<10 months) | • ADT(n = 468) • ADT plus enzalutamide(n =933) |
• Median MFS improved 36.6 months vs 14.7 months with HR of 0.29, p <0.0001 • Median PFS 33.3 months versus 3.9 months |
| SPARTAN [3] | nmCRPC (PSADT<10 months) | • ADT(n =401) • ADT plus apalutamide (n = 806) |
• Median MFS improved 40.5 vs. 16.2 months, respectively, with HR of 0.28 and p <0.001 • Median PFS 40.5 vs. 14.7 months |
| STRIVE [26] | mCRPC and nmCRPC | • ADT plus bicalutamide in nmCRPC (n = 69) • ADT plus enzalutamide in nmCRPC (n =70) |
• Median PFS and median time to PSA progression were not reached with enzalutamide and were 8.6 months and 11.1 months with bicalutamide, respectively, in nmCRPC patients • p < 0.001 for both endpoints, • HR = 0.24 for PFS and 0.19 for PSA progression |
ADT, androgen deprivation therapy; ARAT, androgen-receptor-axis targeted therapy; mHSPC, metastatic hormone sensitive prostate cancer; nmCRPC, nonmetastatic castration resistant prostate cancer
In 2017, two pivotal phase 3 trials using abiraterone shifted the paradigm once again toward utilizing ARAT therapy in mHSPC. The LATITUDE study enrolled patients with at least two high-risk prognostic features; Gleason score of ≥8, the presence of ≥3 bone lesions, or the presence of measurable visceral metastasis. The study randomized patients with the above eligibility criteria to receive a combination of abiraterone and prednisone plus ADT vs ADT alone (Table 1). OS was significantly higher among those who received ADT plus abiraterone and prednisone than among those who received ADT plus placebo (median NR vs 34.7 months). A 38% lower relative risk of death was noted (HR 0.62) in the abiraterone group [20]. Radiographic progression-free survival (PFS) was prolonged in the abiraterone arm, with a median of 33 months compared to 14.8 months in the placebo arm (HR 0.47). Other than grade 3 hypertension and hypokalemia, no major safety concerns were noted in this trial. Only 27% of the placebo treated patients to date have received abiraterone or enzalutamide at progression to mCRPC [20]. Hence, follow up is inadequate to detect the impact on outcomes of patients in the castrate resistant setting.
In arm G of the STAMPEDE trial, 1917 patients with newly diagnosed metastatic, node-positive, or high-risk locally advanced (defined as at least two of the following prognostic criteria: T3/ T4 stage, Gleason score of 8 to 10, or PSA ≥ 40 ng/mL) or previously treated, relapsing disease with high-risk features (in men no longer receiving therapy, a PSA level > 4 ng per milliliter with a doubling time of <6 months, a PSA level > 20 ng per milliliter, nodal or metastatic relapse, or <12 months of total ADT with an interval of >12 months without treatment) were eligible. Enrolled patients were randomized to ADT vs ADT plus abiraterone and prednisone in a 1:1 ratio (Table 1). The majority of patients were newly diagnosed and were classified with metastatic disease (n = 941), node-positive nonmetastatic disease (n = 369), or node negative nonmetastatic disease (n =509) [21]. The primary outcome measure was OS. The intermediate primary outcome was failure-free survival (FFS), defined as the time to radiologic, clinical, or PSA progression, or death from prostate cancer. Abiraterone plus ADT increased the 3-year OS rate of patients by 7 % (83% vs. 76%, HR: 0.63, 95% CI: 0.52 to 0.76, p < 0.001) and the 3-year FFS rate by 30% (75% to 45%, HR: 0.29, 95% CI: 0.25 to 0.34, p< 0.001) [21]. Preplanned analysis of OS of metastatic disease patients showed an improved OS with an HR of 0.61 and 95% CI of 0.49–0.75. The OS data for nonmetastatic disease subset are currently immature, but preliminary results are trending to show an OS benefit favoring the abiraterone arm. Decreased rates of biochemical relapse were noted with addition of abiraterone therapy. In a subgroup analysis, patients with Gleason score < 8 and age > 70 did not benefit in terms of OS. However, the endpoint of FFS showed benefit with addition of abiraterone therapy across all the sub-groups. Grade 3–5 adverse events were low in incidence, and hypertension and ALT increase were the predominant treatment related adverse events [21].
Other ARAT therapies, such as ortorenel/TAK-700 and darolutamide, were evaluated in mHSPC patients. The recently completed SWOG 1216 trial enrolled 1300 + patients and is designed to evaluate OS outcomes with the addition of TAK-700 to ADT as compared to bicalutamide and ADT.
Enzalutamide monotherapy was investigated in a phase 2 trial in the hormone-sensitive setting in men with metastatic and nonmetastatic disease with a primary end point of an 80% or greater decline in PSA at week 25 [22]. In this study, 24% of patients had a Gleason score of 8 or higher and 39% had metastasis at the study entry; 92.5% of the total population achieved the primary end point without any new safety signals related to therapy. Enzalutamide is currently being investigated in the phase 3 randomized ENZAMET trial in patients with metastatic HSPC with randomization to enzalutamide vs nonsteroidal antiandrogen (NSAA), such as bicalutamide or flutamide, in combination with ADT (Table 2). A more contemporary trial called ARCHES, is allowing previous use of docetaxel chemotherapy in mHSPC cancer patients and randomizing them to either ADT alone or ADT plus enzalutamide (Table 2).
Table 2.
Ongoing phase 3 trials of ARAT in the nonmetastatic and metastatic setting
| Trial | Patient population | Treatment arms | Primary endpoint |
|---|---|---|---|
| Nonmetastatic | |||
| ENZARAD NCT02446444 | nmHSPC(high risk locally advanced) | •RT + ADT and enzalutamide for 2 years •RT + ADT for 2 years + NSAA for 6 months |
OS |
| EMBARK NCT02319837 | nmHSPC (high-risk relapsed) | •ADT •ADT plus enzalutamide enzalutamide |
MFS |
| ARAMIS | nmCRPC | •ADT •ADT plus darolutamide |
MFS |
|
NCT02200614 Metastatic | |||
| SWOG 1216 | mHSPC | •ADT + TAK-700 •ADT + bicalutamide |
OS |
| ENZAMET NCT02446405 | mHSPC | •ADT plus NSAA •ADT plus enzalutamide |
OS |
| ARCHES NCT02677896 | mHSPC with ± previous DOC | •ADT plus placebo •ADT plus enzalutamide |
rPFS |
| TITAN NCT02489318 | mHSPC with ± previous DOC | •ADT plus placebo •ADT plus apalutamide |
OS and rPFS |
| ARASENS NCT02799602 | mHSPC | •ADT plus docetaxel plus darolutamide •ADT plus aocetaxel |
OS |
ADT, androgen deprivation therapy; ARAT, androgen-receptor-axis targeted therapy; DOC, docetaxel, MFS, metastasis free survival; mHSPC, metastatic hormone sensitive prostate cancer; nmHSPC, nonmetastatic hormone sensitive prostate cancer; rPFS, radiographic progression free survival
4. Nonmetastatic Prostate Cancer
For patients who are at low risk with a long relapse free interval, low Gleason score, low absolute PSA level, or prolonged PSA doubling time, salvage local therapy alone can be considered. Novel imaging techniques, such as fluciclovine/axumin scans or choline PET scans, help identify sites of metastasis that were previously not detectable with conventional CT scan and bone scan imaging. Stereotactic body radiation therapy (SBRT), cryoablation, radiofrequency ablation, or resection are local options that can be considered. The noninvasive nature of some of these options has made the consideration of local therapy applicable even to elderly patients with comorbidities.
Almost all patients who are started on ADT therapy eventually become castrate resistant, with a median time of 14–20 months [23]. Until recently, no standard of care drugs were available for nmCRPC. Usual practice was to add bicalutamide or other secondary hormonal agents to ADT based on nonrandomized studies, which resulted in a modest benefit with >50% PSA decline in only 20% of patients without any correlated quality of life benefit [24]. Moreover, the androgen receptor agonist activity of bicalutamide can some-times worsen disease progression, which leads to discontinuation of the drug in a majority of the cases. Denosumab showed an improvement in metastasis-free survival (MFS) of >6 months; however, none of these agents have showed improvement OS [25]. Enzalutamide was compared to bicalutamide in the nonmetastatic and metastatic castrate resistant setting in the STRIVE trial [26]. In patients with nm CRPC, median PFS and median time to PSA progression were not reached with enzalutamide compared with 8.6 months and 11.1 months with bicalutamide, respectively (p < 0.001 for both, HR 0.24 for PFS and 0.19 for PSA progression) [26]. Both the PFS and PSA progression benefits were higher in the nonmetastatic setting compared to the metastatic setting, owing to the low tumor burden in the nonmetastatic setting. This was the first study to indicate a benefit of AR receptor blockade in the nonmetastatic setting.
4.1. High-Risk nmCRPC
Given the success of ARAT in the mCRPC setting, phase 3 trials were conducted to treat high-risk disease in the nmCRPC setting. Castrate resistance is followed by metastasis to the bones and other organs, which represent a major reason for complications and death in prostate cancer with an average survival of only 16 to 18 months [27]. A shorter PSA doubling time in nmCRPC patients is directly associated with a shorter time to metastasis or death [27]. A large meta-analysis of 19 randomized trials in localized prostate cancer, and a systematic literature review of nonmetastatic prostate cancer conducted between 1999 and 2014, provide support for MFS as a valid clinical end point and a surrogate for OS [28, 29]. Thus, MFS, defined as the time from randomization to the first detection of distant metastasis or death, whichever occurred first, has been validated as a primary end point for this population.
Enzalutamide was compared to ADT alone in the phase III PROSPER trial in the nmCRPC setting with the primary end point of MFS. Baseline PSA doubling time of less than 6 months was present in 77% of the population in both arms [Table 1]. The results were presented in February 2018 and showed that the use of enzalutamide plus ADT significantly reduced the risk of developing metastases or death by 71% compared to ADT alone. Median MFS was 36.6 months for men who received enzalutamide compared to 14.7 months with ADT alone [2]. There was a 93% reduction in the relative risk of PSA progression and median time to PSA progression was increased by 33.3 months (37.2 months [95% CI: 33.1-NR] versus 3.9 months with ADT alone [95% CI: 3.8–4.0]). Time to first use of new antineoplastic therapy was delayed by 21.9 months versus ADT alone [2]. No new major safety signals were found with a 10% discontinuation rate in the experimental arm, and the drug was approved by the FDA in July 2018.
Apalutamide is a second-generation nonsteroidal antiandrogen agent that binds directly to the ligand binding domain of the AR and works in a similar fashion as enzalutamide [30]. Apalutamide has a low affinity for the gamma-aminobutyric acid type A receptor (IC50 = 3.0 μmol/L) and fourfold lower levels in the brain than enzalutamide, suggesting a lower seizure potential for apalutamide [31]. In the international, randomized, placebo-controlled phase 3 SPARTAN trial, men with a PSA doubling time of 10 months or less were randomized to 240 mg apalutamide daily vs placebo in a 2:1 fashion in the nmCRPC setting (Table 1). All patients received ADT throughout the clinical trial. Baseline median PSA doubling time of less than 6 months was present in about 71% of the population in both arms. Men with nmCRPC treated with apalutamide (n = 806) had a significantly longer median MFS compared with placebo recipients (n = 401) of 40.5 vs. 16.2 months, respectively, with an HR of 0.28 [3]. In subgroup analyses, there was consistent benefit observed across all sub-groups based on age, race, region from which enrolled, prior hormonal therapy, baseline PSA value, as well as stratification factors at study entry [PSA doubling time (<6 vs. ≥ 6 months), use of bone-targeted agents (yes vs. no), and classification of local or regional nodal disease (N0 vs. N1)]. Apalutamide was associated with a significantly longer median time to metastasis (40.5 vs. 16.6 months) and median PFS (40.5 vs.14.7 months). At the time of the primary analysis, the median time to symptomatic progression and the median time to the initiation of cytotoxic chemotherapy were not reached in the apalutamide or placebo treatment groups [3]. After progression, secondary PFS was also higher in the apalutamide group compared to the placebo arm (median not reached vs 39 months). Treatment-related AEs (all grades) included fatigue (30.4% of apalutamide recipients vs. 21.1% of placebo recipients), rash (23.8 vs. 5.5%), falls (15.6 vs. 9.0%), fractures (11.7 vs. 6.5%), hypothyroidism (8.1 vs. 2.0%), and seizures (0.2 vs. 0%). Grade 3 or 4 treatment-related AEs reported in the apalutamide and placebo groups were rash (5.2 vs. 0.3%), fractures (2.7 vs. 0.8%), falls (1.7 vs. 0.8%), and fatigue (0.9 vs. 0.3%) [3]. Based on this data, after an FDA priority review, apalutamide was approved in early 2018 at the 240 mg daily dose with concomitant ADT therapy. Currently, apalutamide is being tested in multiple phase 3 trials in the mCRPC, mHSPC (TITAN trial), and in locally advanced prostate cancer settings (Table 2).
Darolutamide is a novel, oral next-generation AR antagonist with a high affinity for the AR receptor. In contrast to enzalutamide and apalutamide, darolutamide also inhibits mutated AR in preclinical models, such as F877 L, W742 L, and T877A, which have been implicated in conferring treatment resistance to CRPC therapies [32, 33]. Moreover, darolutamide has negligible blood-brain barrier penetration. Owing to its good safety profile with low drug-drug interactions and decreased CNS penetration, combined with robust PSA responses seen in phase 2 trials, it is currently being investigated in phase 3 trials. ARAMIS is a placebo controlled randomized trial in nmCRPC patients (positive results for MFS were announced in a press release in October 2018), and ARASENS is a trial for mHSPC patients (Table 2).
4.2. Low-Risk nmCRPC
The study population of PROSPER and SPARTAN only applies to about a third of patients with nmCRPC patients as both of these trials included only patients with a PSA doubling time of 10 months or less [34]. For patients who are at low risk with long relapse free interval, low Gleason score, low absolute PSA level, or prolonged PSA doubling time of greater than 10 months, salvage local therapy alone can be considered. Novel imaging techniques with F-18 choline, F-18 fluciclovine, and F-18/PSMA tracers can help identify sites of local recurrence or metastasis that were previously not detectable with conventional CT scan and bone scan imaging in patients with very low PSA values. For example F-18/PSMA PET scans can detect potential sites of recurrence in a median of 51.4% of patients with PSA levels of less than 1 ng/mL, in 74% of patients with PSA between 1 to 2 ng/mL, and in 90.5% of patients when the PSA level is less than 2 ng/mL [35]. Focal cryoablation, high intensity focused ultrasound (HIFU), low-dose brachytherapy, and radiation of the prostate bed are local options to be considered. With focal cryoablation, biochemical disease free survival rates ranging from 69 to 100% at 1 year, 50–72.4% at 3 years, and 46.5–54.4% at 5 years have been reported [36]. Crouzet et al. described a cohort of 290 patients who achieved disease-specific and MFS rates of close to 80% using HIFU, at 48-month follow-up [37]. The noninvasive nature of some of these options has made the therapy applicable even to elderly patients with comorbidities. If radiation to the prostate bed is being considered then randomized trial data indicate that combining with 6 months of androgen deprivation therapy produces better outcomes. [38].
5. Ongoing Trials
The open-label phase 2IMAAGEN trial also demonstrated a possible benefit of abiraterone acetate plus prednisone in patients with nmCRPC. The rates of PSA reduction >50% from the baseline and the median PSA-PFS were 87% and 28.7 months, respectively [39]. No subsequent phase 3 trials of CYP17 inhibitors in the nmCRPC population have been reported to date. ENZARAD is a phase 3 study evaluating the use of enzalutamide vs NSAA in high-risk locally advanced prostate cancer patients in combination with conventional radiation and ADT therapy (Table 2). EMBARK is a phase 3 study assessing early use of enzalutamide in high-risk (PSA doubling time < 9 months) biochemically recurrent nonmetastatic prostate cancer progressing after radical prostatectomy or radiotherapy or both in the castration sensitive setting by randomizing patients to enzalutamide plus ADT vs enzalutamide alone vs LHRH therapy (Table 2).
6. Discussion
With the results of the LATITUDE and STAMPEDE trials in 2017, now there are two different standard-of-care treatment options available for mHSPC patients, including abiraterone and prednisone, or docetaxel chemotherapy. Due to the lack of a direct comparison in clinical trials, multiple attempts have been made to compare these two options through meta-analysis, ad-hoc analysis, and cross-trial comparisons. A recent meta-analysis of three docetaxel plus ADT phase 3 studies, including CHAARTED, STAMPEDE arm C, GETUG-AFU 15, and the two abiraterone plus ADT phase 3 studies, including LATITUDE and STAMPEDE arm G, did not demonstrate a significant difference in OS between abiraterone and docetaxel [40]. Similarly, post hoc analysis of STAMPEDE arm C (docetaxel vs ADT) and STAMPEDE arm G (abiraterone vs ADT) found similar OS, indicating no significant difference between the two treatments [41].
The CHAARTED trial with docetaxel plus ADT in mHSPC stratified patients based on high vs low volume disease and a benefit of chemotherapy was only seen in those with high volume [17]. LATITUDE for abiraterone plus ADT in mHSPC only included patients that were high-risk [20]. Although the definition of high volume and high risk are not exactly similar, given that the comparison arm with ADT did quite similar in both studies, cross-trial comparisons have been made. HR for the experimental arms in both studies are 0.62 and 0.60 for abiraterone and docetaxel, respectively, indicating that either of the treatment options in this specific populations is appropriate [17, 20]. LATITUDE did not enroll patients with low-risk metastatic disease and the STAMPEDE G study did not stratify patients based on high vs low risk disease [20, 21]. However, in STAMPEDE G the OS benefit was seen in all of the patients who had metastatic disease. Although FFS was improved in all the subgroups, including patients with nonmetastatic disease in STAMPEDE G, the OS data are not mature and longer follow up is needed. About 77% of the patients in STAMPEDE G were still alive at the time of publication; thus, further analysis of patients based on their subsequent treatments will be helpful in deriving the exact benefit of using abiraterone early in this setting [21].
Currently there is one retrospective analysis showing an OS benefit of early use of ARAT in nmCRPC vs mCRPC. The study demonstrated better OS from the time of diagnosis of CRPC in Kaplan-Meier analysis (median OS of 86 months vs 40 months; p = 0.004), with significant improvement observed for PFS (p =0.048) and PSA response (p =0.0014) [42]. Multivariate analysis demonstrated nonmetastatic status, low PSA, and long PSA doubling time at ARAT initiation as significant predictors of longer OS (p =0.044, 0.0001, and 0.026, respectively) [42]. However, the study had a low number of patients, imbalance in imaging schedules between the two groups, and patients in the mCRPC group had higher-risk features. MFS has been proposed as the surrogate for OS based on retrospective studies in the nonmetastatic and castrate sensitive setting. Whether the benefits in MFS in the nmCRPC patients seen in the SPARTAN and PROSPER trials will hold up to translate into improved OS remains to be seen with time as OS is a secondary endpoint in both the studies.
6.1. Resistance to ARAT
Approximately 20–40% of patients may exhibit primary resistance to abiraterone or enzalutamide [43]. A well described AR mutation is the AR-V7 splice variant. The AR isoform encoded by this splice-variant lacks the ligand-binding domain, which is the target of enzalutamide and apalutamide (and indirectly also of abiraterone), but remains constitutively active as a transcription factor [43]. Retrospective and prospective studies have shown that patients expressing the ARV7 mutation have poor responses to both agents compared to patients without the AR-V7 mutation [44]. However, response to taxane-based chemotherapy is preserved in AR-V7 mutated mCRPC patients [45]. Given the differences in the genotype and phenotype between CRPC and HSPC patients, the significance of the AR-V7 mutation remains to be seen in the CSPC setting. However, since the testing for AR-V7 mutation is still not a standard-of-care, a potential pitfall of applying androgen receptor axis blockade early in the prostate cancer treatment is selecting those with AR-V7 mutation for a treatment strategy that will not be beneficial.
Conversely, ERG is a transcription factor that affects several parameters of microtubule dynamics and inhibits effective drug-target engagement of docetaxel or cabazitaxel with tubulin [46]. An analysis of a cohort of 34 men with metastatic CRPC treated with docetaxel chemotherapy revealed that ERG-overexpressing prostate cancers had twice the chance of docetaxel resistance than ERG-negative cancer [47]. This mechanism has not been validated in patients with mHSPC but can be a potential biomarker to make decisions between secondary hormonal therapy vs chemotherapy in this setting.
6.2. Toxicity of ARAT
Early use of ARAT comes with a different toxicity profile compared to systemic chemotherapy and must be individualized based on comorbidities. Abiraterone requires concomitant use of prednisone and results in side effects, such as hypertension, hyperkalemia, and hyperglycemia. In both the STAMPEDE G and LATITUDE trials, most common grade 3–4 side effects in the abiraterone arms included hypertension, hypokalemia, AST/ALT elevation, and other cardiac disorders [20, 21]. SPARTAN reported side effects of rash, fatigue, and fractures and hypothyroidism, which were more common in the apalutamide arm [3]. Enzalutamide is known to cause neurocognitive issues, such as fatigue, falls, and seizures, which is a concern especially in the elderly population. In addition to ADT and docetaxel, now there are also reports of abiraterone and enzalutamide induced neuroendocrine differentiation (NED), which is associated with poor prognosis [48]. Whether applying ARAT drugs earlier in the prostate cancer setting will cause more long term remissions is not known and needs to be investigated further. Duration of treatment with ARAT is much longer compared to systemic chemotherapy and requires prolonged commitment of patient compliance. Cost of ARAT drugs is undoubtedly more than chemotherapy agents. Whether potential reductions in hospitalizations, and individual suffering from toxicity of chemotherapy, would justify ARAT over chemotherapy remains to be investigated with a formal cost-based analysis.
6.3. Algorithm for ARAT Use
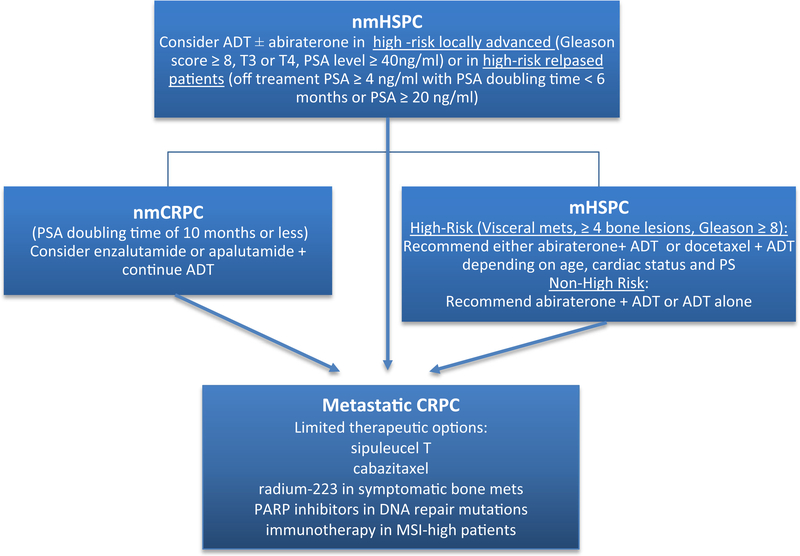
Based on available data, for patients with high-volume or high-risk metastatic HSPC, both abiraterone and docetaxel are considered standard-of care. There is no evidence to support the use of both together but future trials will likely investigate this. The choice between the two therapies should be individualized based on patient and physician preferences, cost-analysis, duration of treatment, and side effect profiles. Patients who are considered unfit for chemotherapy due to poor performance status or pre-existing neuropathy should be considered for abiraterone (Fig. 1). For patients with diabetes, heart failure, swallowing difficulties, and those at risk of noncompliance or lack of resources, finite therapy with docetaxel is favored. A select few patients might be not able to tolerate either of the therapies due to comorbidities, and ADT therapy alone remains an option. If information on bio-markers, such as ARV7 mutation or ERG gene fusion status, is available, those with ARV7 mutation should be considered for docetaxel and those with ERG over-expression may preferentially be considered for abiraterone. In patients with high-volume or high-risk metastatic prostate cancer, abiraterone is the new standard-of-care due to the OS benefit seen in the STAMPEDE G trial, acknowledging that most of the benefit in OS was driven by the high-tumor burden population. Second-generation AR antagonists, such as enzaluatmide, apalutamide, and darolutamide, (Table 2) are currently in phase 3 trials (some allowing previous docetaxel use) and will likely enhance the already available armamentarium to treat mHSPC patients.
Fig. 1.
Proposed treatment algorithm with recent ARAT approvals. Patients with high-risk features with locally advanced prostate cancer can be considered for abiraterone both in relapsed and in upfront setting. Patient with high-risk mHSPC can be considered for ADT plus abiraterone or ADT plus docetaxel based on patient characteristics. Both enzaluatmide and apalutamide are an equal option for patients with nmCRPC with PSA doubling time of less than 10 months. ARAT, androgen-receptor-axis targeted therapy; nmHSPC, nonmetastatic hormone sensitive prostate cancer; mHSPC, metastatic hormone sensitive prostate cancer; nmCRPC, nonmetastatic castration resistant prostate cancer; metastatic CRPC, metastatic castrate resistant prostate cancer; ADT, androgen deprivation therapy; PSADT, PSA doubling time
Use of ARAT therapy in high-risk locally advanced and high-risk relapsed settings is an evolving field. The data from the STAMPEDE G trial show an improved FFS, but OS results are not mature enough to adopt the early use of abiraterone (Fig. 1). The ENZARAD and EMBARK trials compare enzalutamide to standard-of-care in both high-risk locally advanced and high-risk relapsed settings, respectively (Table 2).
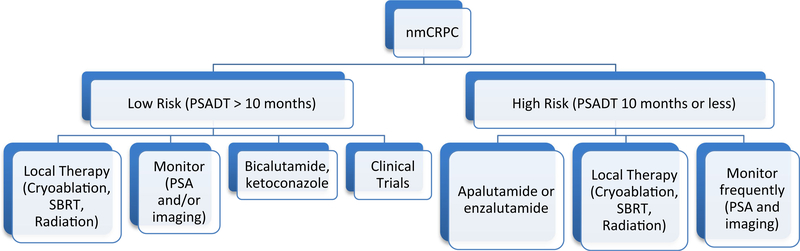
Based on the phase 3 data of SPARTAN and PROSPER, both apalutamide and enzalutamide are appropriate therapies in nmCRPC patients with PSA doubling time of 10 months or less (Figs. 1 and 2). The MFS is better with apalutamide (40.5 months) compared to enzalutamide (36.6 months); however, the SPARTAN study enrolled fewer patients with PSA doubling time of 6 months or less [2, 3]. Important adverse effects of rash, fractures, and hypothyroidism related to apalutamide should be taken into account before making a therapeutic decision. Results of the ARAMIS phase 3 trial utilizing darolutamide (a strong second generation AR inhibitor with less blood-brain barrier penetration) in the same setting are eagerly awaited (positive results for MFS were announced in a press release in October 2018) to see if the toxicity profile can be improved upon without losing efficacy. Future comparison trials between the AR antagonists and investigation of predictive biomarkers will enable more efficient therapeutic selection.
Fig. 2.
Treatment in nmCRPC. Patients with PSA doubling time of greater than 10 months can be treated with local therapy, conservative management with frequent PSA/imaging, NSAAs or clinical trials. Patients with PSA doubling time of less than 10 months should be considered for either local therapies or ARATs based on recent approvals. nmCRPC, nonmetastatic castration resistant prostate cancer; PSADT, PSA doubling time; SBRT, Stereotactic body radiotherapy
7. Conclusions
The results of randomized studies, such as SPARTAN and PROSPER, in nmCRPC patients confirmed the intuitive fact that early therapy will produce a higher chance of response (87% PSA response) for a longer duration (median 40.1 months); however, the impact on clinical outcomes and OS remains a question. The cost and toxicity ramifications in a largely asymptomatic patient population should not be underestimated. A careful assessment of the comorbidity risk score and estimated life expectancy of the patient is essential before conducting a balanced discussion regarding starting therapy in nmCRPC. Patients with a PSA doubling time of greater than 10 months can be managed conservatively with local therapies and close monitoring (Fig. 2). Decades of follow up will be required to establish the true benefits of mortality and morbidity, and the comparison remains based on a presumption that the placebo patients will receive ARAT therapy appropriately early within the metastatic disease course. The mental and cardiac effects are likely to be underestimated as delayed toxicity data is not yet available. After 50+ years of ADT use, the metabolic syndrome and dementia effects were noticed and publicized and a similar phenomenon can be predicted for long durations of ARAT use.
Patient selection and shared decision making remain critical components of the process of selecting early ARAT therapy in the nonmetastatic setting, and pros and cons should be considered with each clinical scenario (Table 3).
Table 3.
Pros and cons of ARAT therapies in nmCRPC
| Pros | Cons |
|---|---|
| Delaying occurrence of metastatic disease | Decreased therapy options and refractory disease, when symptomatic metastatic disease occurs |
| Improved OS | Increased morbidity within metastatic disease |
| High magnitude of clinical benefit | Small proportion progress to metastatic neuroendocrine prostate cancer with limited therapy options and attenuated OS |
| Avoid the stress of prolonged monitoring for occurrence of metastatic disease | Prolonged toxicity, such as cognitive effects and rash |
| May reduce morbidity and hospitalization | High cost of prolonged administration of agents |
| Study used conventional imaging | Newer imaging techniques not incorporated which will impart a bigger lead time bias |
| Selection of patients with a likelihood of developing metastasis within 16 months as seen in placebo arm. | Patients likely to receive abiraterone and prednisone very early, in nmHSPC based on results of STAMPEDE trial |
Some of the pros of using ARAT in nmCRPC patients include increased MFS, OS, and decreased stress regarding prolonged monitoring. Cons include decreased therapy options in the metastatic setting, toxicity, and cost of therapy
Key Points.
The treatment paradigm in prostate cancer has shifted with the FDA approvals of abiraterone in metastatic hormone sensitive prostate cancer and of enzalutamide and apalutamide in non metastatic castrate resistant prostate cancer.
Longer follow-up and overall survival data of early androgen-receptor axis targeted therapy use in non-metastatic setting is awaited.
Pros and cons for earlier use of androgen-receptor axis targeted therapy should be considered for each patient before treatment initiation in the metastatic and non-metastatic settings.
Acknowledgments
Funding No external funding was used in the preparation of this manuscript.
Footnotes
Compliance with Ethical Standards
Conflict of Interest Dr. Ulka Vaishampayan declares research support and consulting for Astellas Inc. and honoraria from Pfizer Inc. and Bayer Inc. Dr. Harsh Shah declares that he has no conflicts of interest that might be relevant to the contents of this manuscript.
References
- 1.Walsh PC . Initial results of the Medical Research Council Trial. The Medical Research Council Prostate Cancer Working Party Investigators Group. Br JUrol. 1997;79(2):235–46. [DOI] [PubMed] [Google Scholar]
- 2.Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2018;378(26):2465–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med. 2018;378(15):1408–18. [DOI] [PubMed] [Google Scholar]
- 4.Elkon JM, Millett RL, Millado KF, Lin J. Abiraterone is effective and should be considered for the treatment of metastatic castrate-naïve prostate cancer. Expert Opin Pharmacother. 2018;19(5):507–9. [DOI] [PubMed] [Google Scholar]
- 5.Berry W, Dakhil S, Modiano M, Gregurich M, Asmar L. Phase III study of mitoxantrone plus low dose prednisone versus low dose prednisone alone in patients with asymptomatic hormone refractory prostate cancer. J Urol. 2002;168(6):2439–43. [DOI] [PubMed] [Google Scholar]
- 6.Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. [DOI] [PubMed] [Google Scholar]
- 7.de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54. [DOI] [PubMed] [Google Scholar]
- 8.Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fossa SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23. [DOI] [PubMed] [Google Scholar]
- 9.Dai C, Heemers H, Sharifi N. Androgen signaling in prostate cancer. Cold Spring Harb Perspect Med. 2017;7:a030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Attard G, Belldegrun AS, de Bono JS. Selective blockade of androgenic steroid synthesis by novel lyase inhibitors as a therapeutic strategy for treating metastatic prostate cancer. BJU Int. 2005;96: 1241–6. [DOI] [PubMed] [Google Scholar]
- 11.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364(21):1995–2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy N Engl J Med. 2013;368(2):138–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nadal R, Bellmunt J. The evolving role of enzalutamide on the treatment of prostate cancer. Future Oncol. 2016;12(5):607–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy N Engl J Med. 2012;367(13):1187–97. [DOI] [PubMed] [Google Scholar]
- 15.Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy N Engl J Med. 2014;371(5):424–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santer FR, Erb HH, McNeill RV. Therapy escape mechanisms in the malignant prostate. Semin Cancer Biol. 2015;35:133–44. [DOI] [PubMed] [Google Scholar]
- 17.Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373: 737–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multi-stage, platform randomised controlled trial. Lancet. 2016;387: 1163–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gravis G, Boher JM, Joly F, Soulie M, Albiges L, Priou F, et al. Androgen deprivation therapy (ADT) plus docetaxel versus ADT alone in metastatic non castrate prostate cancer: impact of metastatic burden and long-term survival analysis of the randomized phase 3 GETUG-AFU15 trial. Eur Urol. 2016;70:256–62. [DOI] [PubMed] [Google Scholar]
- 20.Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60. [DOI] [PubMed] [Google Scholar]
- 21.James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP, et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N Engl J Med. 2017;377:388–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tombal B, Borre M, Rathenborg P, Werbrouck P, Van Poppel H, Heidenreich A, et al. Enzalutamide monotherapy in hormone-naive prostate cancer: primary analysis of an open-label, single-arm, phase 2 study Lancet Oncol. 2014;15:592–600. [DOI] [PubMed] [Google Scholar]
- 23.Sharifi N, Gulley JL, Dahut WL. Androgen deprivation therapy for prostate cancer. JAMA. 2005;294:238–44. [DOI] [PubMed] [Google Scholar]
- 24.Kucuk O, Fisher E, Moinpour CM, Coleman D, Hussain MH, Sartor AO, et al. Phase II trial of bicalutamide in patients with advanced prostate cancer in whom conventional hormonal therapy failed: a southwest oncology group study (SWOG 9235). Urology. 2001;58(1):53–8. [DOI] [PubMed] [Google Scholar]
- 25.Smith MR, Saad F, Oudard S, Shore N, Fizazi K, Sieber P, et al. Denosumab and bone metastasis-free survival in men with nonmetastatic castration-resistant prostate cancer: exploratory analyses by baseline prostate-specific antigen doubling time. J Clin Oncol. 2013;31:3800–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Penson DF, Armstrong AJ, Concepcion R, Agarwal N, Olsson C, et al. Enzalutamide versus bicalutamide in castration-resistant prostate cancer. J Clin Oncol. 2016;34(18):2098–106. [DOI] [PubMed] [Google Scholar]
- 27.Smith MR, Kabbinavar F, Saad F, Hussain A, Gittelman MC, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23(13):2918–25. [DOI] [PubMed] [Google Scholar]
- 28.Li T, Thompson M, Tran D. Metastatic-free survival and overall survival in prostate cancer [abstract]. Presented at: International Society for Pharmacoeconomics and Outcomes Research; 16–20 May 2015; Philadelphia, PA: Abstract PRM22. [Google Scholar]
- 29.Xie W, Sweeney C, Regan M, Nakabayashi M, Buyse M, Clarke N, et al. Metastasis free survival (MFS) is a surrogate for overall survival (OS) in localized prostate cancer (CaP). Ann Oncol. 2016;27(suppl 6):7170. [Google Scholar]
- 30.Clegg NJ, Wongvipat J, Joseph JD, Tran C, Ouk S, et al. ARN-509: a novel antiandrogen for prostate cancer treatment. Cancer Res. 2012;72(6):1494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al Salama ZT. Apalutamide: first global approval. Drugs. 2018;78(6):699–705. [DOI] [PubMed] [Google Scholar]
- 32.Moilanen AM, Riikonen R, Oksala R, Ravanti L, Aho E, Wohlfahrt G, et al. Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep. 2015;5: 12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shore ND. Darolutamide (ODM-201) for the treatment of prostate cancer. Expert Opin Pharmacother. 2017;18(9):945–52. [DOI] [PubMed] [Google Scholar]
- 34.Howard LE, Moreira DM, De Hoedt A, Aronson WJ, Kane CJ, Amling CL, et al. Thresholds for PSA doubling time in men with non-metastatic castration-resistant prostate cancer. BJU Int. 2017;120:E80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evans JD. Prostate cancer-specific PET radiotracers: a review on the clinical utility in recurrent disease. Pract Radiat Oncol. 2018;8: 28–39. [DOI] [PubMed] [Google Scholar]
- 36.Duijzentkunst DA, Peters M, van der Voort van Zyp JR, Moerland MA, van Vulpen M. Focal salvage therapy for local prostate cancer recurrences after primary radiotherapy: a comprehensive review. World JUrol. 2016;34(11):1521–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crouzet S, Murat FJ, Pommier P, Poissonnier L, Pasticier G, Rouviere O, et al. Locally recurrent prostate cancer after initial radiation therapy: early salvage high-intensity focused ultrasound improves oncologic outcomes. Radiother Oncol. 2012;105:198–202. [DOI] [PubMed] [Google Scholar]
- 38.Carrie C, Hasbini A, de Laroche G, Richaud P, Guerif S, Latorzeff I, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): a randomised, multicentre, open-label phase 3 trial. Lancet Oncol. 2016;17(6):747–56. [DOI] [PubMed] [Google Scholar]
- 39.Ryan CJ, Crawford ED, Shore ND, Underwood W 3rd, Taplin ME, Londhe A, et al. The IMAAGEN study: effect of abiraterone acetate and prednisone on prostate specific antigen and radiographic disease progression in patients with nonmetastatic castration resistant prostate cancer. JUrol. 2018;200(2):344–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Messina C, Messina M, Boccardo F. Abiraterone or docetaxel for castration-sensitive metastatic prostate cancer? That is the question! EurUrol. 2018;73:145–8. [DOI] [PubMed] [Google Scholar]
- 41.Sydes MR, Spears MR, Mason MD, Clarke NW, Dearnaley DP, de Bono JS, et al. Adding abiraterone or docetaxel to long-term hormone therapy for prostate cancer: directly randomised data from the STAMPEDE multi-arm, multi-stage platform protocol. Ann Oncol. 2018;29(5):1235–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mori K, Kimura T, Ito K, Onuma H, Tanaka M, Matsuura T, et al. Earlier use of androgen receptor-axis-targeted drugs may improve overall survival in patients with non-metastatic castration-resistant prostate cancer. Prostate. 2018;78(10):766–72. [DOI] [PubMed] [Google Scholar]
- 43.Crona DJ, Milowsky MI, Whang YE. Androgen receptor targeting drugs in castration-resistant prostate cancer and mechanisms of resistance. Clin Pharmacol Ther. 2015;98:582–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Antonarakis ES, Lu C, Luber B, Wang H, Chen Y, Nakazawa M, et al. Androgen receptor splice variant 7 and Efficacy of Taxane chemotherapy in patients with metastatic castration-resistant prostate cancer. JAMA Oncol. 2015;1(5):582–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Galletti G, Matov A, Beltran H, Fontugne J, Miguel Mosquera J, Cheung C, et al. ERG induces taxane resistance in castration-resistant prostate cancer. Nat Commun. 2014;5:5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galletti G, Leach BI, Lam L, Tagawa ST. Mechanisms of resistance to systemic therapy in metastatic castration-resistant prostate cancer. Cancer Treat Rev. 2017;57:16–27. [DOI] [PubMed] [Google Scholar]
- 48.Hu C-D, Choo R, Huang J. Neuroendocrine differentiation in prostate cancer: a mechanism of radioresistance and treatment failure. Front Oncol. 2015;5:90. [DOI] [PMC free article] [PubMed] [Google Scholar]