Abstract
This study describes the initiation and maintenance of illicit drug use, risky behaviors, and the substance use treatment experiences of women in Georgia. Qualitative interviews with 55 drug-using women (mean age 36 years; SD = 9.52), were conducted during April-September 2011. Participants presented diverse histories of drug use initiation and substance use, risky behaviors, and drug treatment participation. All participants reported concurrent use of different substances, including home-produced injection preparations. Women described their experiences of both the positive and negative effects (physical and psychological) that they attributed to their use of drugs. Findings enrich our understanding of the environment in which substance use is initiated and maintained in a female population in Georgia, and illustrate the importance of culture and the role of social factors in the development of injection drug use. Results can provide direction for tailoring the development of interventions for substance use disorders, public policy discussions regarding the treatment of women who use drugs, and future research on substance use among women in Georgia and other post-Soviet nations.
Keywords: Caucasus region, homemade drugs, injection drug use, substance use, women-focused treatment
In Georgia, a country of 4.5 million inhabitants located in the South Caucasus, heroin and buprenorphine injection epidemics during the late 1990s to early 2000s were followed by the widespread use of home-produced injection preparations. In 2011–2012, desomorphine (“Krokodil”) and homemade amphetamine-type stimulants (“Vint” and “Jeff”) were common injection drugs. A significant proportion of people who inject drugs (PWID) use both preparations (Javakhishvili et al. 2012). Intensive policing of opioid markets resulted in PWIDs switching to alternative drugs that required less involvement in the illegal drug marketplace and were considerably cheaper. Switching to homemade drugs has often been associated with increased risk of bloodborne infections, serious physical harm, and neurological and psychiatric complications (Grund, Latypov & Harris 2013). Overall treatment coverage is as low as 6% of PWIDs, despite the fact that both drug-free and medication-assisted treatments are available in Georgia (Javakhishvili et al. 2012). Agonist maintenance with methadone or buprenorphine has been steadily expanding in recent years and, in 2011, more than 2,300 people received maintenance pharmacotherapy. In the same year, only 270 people received drug-free in-patient treatment (two-weeks detoxification with no or few cases of post-detoxification psychosocial treatment) (Javakhishvili et al. 2012).
HIV status is closely tied to the injection-drug-using community (Chkhartishvili et al. 2011) with 50% of the cumulative 4,554 HIV-positive cases registered with the National AIDS Centre by mid-2014 identified as PWIDs (Georgian AIDS and Clinical Immunology Centre 2014). Although HIV prevalence is low in the general population (0.05%), alarmingly, the number of HIV-positive registered individuals rose steadily by at least 5–10% annually between 1994 and 2009 (Government of Georgia 2010), and women comprise 26.5% out of the total number of registered cases. Although the overall HIV prevalence in Georgia is low compared to other former Soviet Union states, this rise in the number of HIV and AIDS cases remains a cause for serious concern (Buckley 2005).
Like HIV, the hepatitis C virus (HCV) infection has been associated with injection drug use. HCV prevalence among PWIDs is estimated to be 50–70% (Javakhishvili et al. 2011; Chkhartishvili et al. 2011). Bouscaillou et al. (2014) reported a 58.8% prevalence of HCV among 17 women who injected drugs in Tbilisi, the capital of Georgia. Although this sample is small, there are no other studies that have estimated HCV rates for women who inject in Georgia.
Women with substance use disorders are one of the most hidden and underserved populations in Georgia (Javakhishvili et al. 2011; 2013), and there are few opportunities for women to receive publicly funded treatment for substance use disorders. Given that drug treatment in Georgia has been designed to serve male beneficiaries, when treatment is available, it lacks sensitivity to the unique needs and challenges that injection-drug-using women face (International Harm Reduction Development Program 2009; Javakhishvili et al. 2011; Otiashvili et al. 2013; Rukhadze et al. 2009). Of the 45,000 identified systematic users of illicit and/or injecting drugs in Georgia (Sirbiladze & Tavzarashvili 2012), women may represent up to 10% of the adult drug-using population (Needle & Zhao 2010; Zaalishvili, Chavchanidze & Mchedlishvili 2013). Yet women who use drugs comprise only 1–2% of drug-related service beneficiaries in Georgia (Javakhishvili et al. 2012; Kirtadze et al. 2013).
Empirical data on drug use by women in Georgia are scarce. Our previous research has examined the factors that motivate women who inject drugs to seek health care and the barriers they encounter when they do, and identified factors that may encourage or inhibit the disclosure of substance use to health service providers by women in Georgia (Kirtadze et al. 2013; Otiashvili et al. 2013). However, little is known regarding substance use initiation and the environment in which a substance use life course of women who use drugs in Georgia develops. This study examined the attitudes, beliefs, life circumstances, and contexts of drug use among injection-drug-using women in Georgia.
METHODS
Procedure
A qualitative study was conducted during April-September 2011 in three cities: Tbilisi, Zugdidi, and Gori. These cities provide diversity in population numbers (1,152,500, 75,900, and 49,500 inhabitants, respectively) and geographic locations. Tbilisi, the capital city of Georgia, is home to one-fourth of the country’s population, and prevalence of substance use is likely reflective of the Georgian prevalence rate. Both Gori (central Georgia) and Zugdidi (west Georgia) border on two uncontrolled separatist regions (South Osetia and Abkhazia, respectively) and are characterized by a high prevalence of drug use. In all three cities, agonist treatment and low-threshold programs are available.
A Community Advisory Board (CAB), composed of 11 health care providers for women, and a Beneficiary Advisory Board (BAB), comprised of four drug-using women, informed the study. Injection-drug-using females were recruited via low-threshold programs using referrals from our CAB/BAB as well as snowball sampling.
Research staff briefly described the study to potential participants. Study-eligible and interested candidates made an appointment with staff to consent and interview them at a mutually convenient time and at a private location.
All participants provided written informed consent prior to participating in an audiotaped interview. Participants received 30 GEL ($18) as reimbursement for their time. Institutional Review Board approval was obtained from the Office of Research Protection IRB at RTI International, USA, and from the Maternal and Child Care Union IRB, Georgia.
Participants
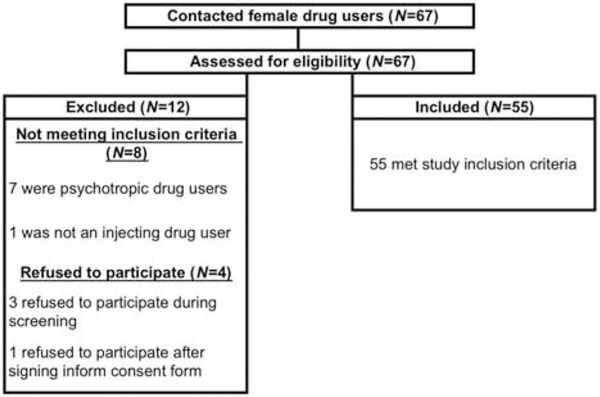
Of the 67 potential participants contacted, four refused participation during initial assessment and eight were ineligible, leaving a final sample of 55 women: 20 from Tbilisi, 20 from Gori, and 15 from Zugdidi (see Figure 1). Eligibility criteria included: conversant in Georgian; 18 years or older; able to provide informed consent; injection of illicit drugs in the past 30 days as verified by venipuncture stigmata; and sexually active at least once in the past 30 days. Four respondents were in medication-assisted treatment, 14 were participants of needle and syringe programs at the time of interview, and two women were pregnant.
FIGURE 1.
Study Flow Chart
Interviews
The data collection strategy involved in-depth interviewing (Goldstein 1979; Rosenbaum 1981; Waldorf 1973). Interviews lasted approximately 60 to 120 minutes and covered six main topics: role of women in Georgian society; initiation and consumption of tobacco, alcohol, and drugs; gender differences in drug-using individuals; forms of violence associated with drug use; what drug treatment services are needed for women; and barriers to such services. All interviews were audio-recorded with participant written consent.
Qualitative Analysis
Digital audio files were transcribed directly into Georgian in Unicode text format. Transcripts were exported as .pdf files that were then imported directly into nVivo 9 (http://www.qsrinternational.com/products_nvivo.aspx) qualitative analysis software, followed by content and thematic analyses. During the process of reading the interviews in Georgian, two coders independently coded relevant textual material that was thought to represent the opinion, statement, position, thinking mode, behavior, and/or attitudes of the respondents towards the six specific issues. The analytic process involved six key stages: (1) familiarization with the transcripts; (2) identifying a thematic framework focusing on the six specific issues; (3) coding—applying the thematic framework to the data using textual codes to identify specific statements corresponding to differing themes; (4) creating a node matrix from Matrix Coding query results and visualization; (5) mapping; and (6) interpretation, which included searching for associations, patterns, concepts, and explanations in the data, aided by visual displays such as cluster analyses, word frequency query, and connection mapping of thematic results. The aim of this procedure was to visually display ideas from the data as an aid in developing and testing interpretations.
This process was intended to create an in-depth cultural model of the social reality of the participants from their point of view, the so-called emic perspective (Pike 1990). The goal of the model was to describe how they perceived and categorized the environment in which they lived, their rules for behavior in a male-dominated network, what has meaning for them, and how they imagine and explain things.
All transcripts were translated into English to permit review and discussion with US collaborators, and then back-translated into Georgian (and the English-language transcripts corrected, if necessary), in order to ensure accuracy of translation.
RESULTS
Participants’ Characteristics
Participants’ background information is presented in Table 1. Age was about 36 years (range 18–55), and 30 participants (55%) had 11 or more years of education (equivalent to a high school degree in the United States). Approximately 62% were married or living as married. Twelve (22%) had no children (but two were pregnant at interview); 48 out of 55 (87.2%) participants were unemployed at the time of interview; those employed part- or full-time were mostly in clerical or sales positions. More than half of the sample smoked cigarettes, with 15 years being the mean age of smoking initiation. Participants indicated that their first drug experience was smoking marijuana or taking pills (e.g., ecstasy) in early adolescence. Mean age of initiation of injection drug use was 21 (SD = 4.07; range = 15–30), typically beginning with heroin or raw opium (76.5%), buprenorphine (14.5%), and/or homemade stimulants (7.3%). Home-produced amphetamine-type stimulants and opioids were the current injection drugs of use, with all respondents admitting to poly-substance use (adding sedatives, neuroleptics, and/or anticonvulsants on top of injection drug, depending on the availability of particular substances). Few participants had entered HIV-prevention programs: only 18 (33%) had ever been involved in intervention programs. Four women were in medication-assisted treatment at the time of interview, and 14 were in a syringe and needle exchange program.
TABLE 1.
Demographic and Background Characteristics of Injection-Drug-Using Women (N = 55)
| N (%) | M (SD) | |
|---|---|---|
| Ethnicity | ||
| Georgian | 53 (96.40%) | |
| Non-Georgian (Ukrainian) | 2 (3.60%) | |
| Age | 35.67 (9.52) | |
| Education | ||
| High school | 30 (54.55%) | |
| Professional education (2 years after high school education) | 5 (9.09%) | |
| Student | 1 (1.82%) | |
| University (uncompleted) | 4 (7.27%) | |
| University (completed) | 15 (27.27%) | |
| Marital status | ||
| Single | 5 (9.09%) | |
| Divorced | 15 (27.27%) | |
| Married/Remarried | 22 (40%) | |
| Co-habitation | 12 (21.82%) | |
| Widowed | 1 (1.82%) | |
| Living situation | ||
| Alone | 1 (1.82%) | |
| with children | 16 (29.09%) | |
| with children and husband | 10 (18.18%) | |
| with parents (no children) | 16 (29.09%) | |
| with partner (no children) | 12 (21.82%) | |
| Number of children | ||
| None | 12 (21.82%) | |
| 1 child | 21 (38.18%) | |
| 2 children | 15 (27.27%) | |
| 3 child | 5 (9.09%) | |
| 4 children | 2 (3.64%) | |
| Current employment status | ||
| Unemployed | 48 (87.27%) | |
| Employed part-time | 4 (7.27%) | |
| Employed full-time | 1 (1.82%) | |
| Self-employed | 2 (3.64%) | |
Thematic Content of the Interviews
This paper focuses on three main themes representing the major gaps in knowledge about the contexts surrounding substance use behavior among women in Georgia: initiation and maintenance of injection use, risk behaviors, and experience with substance use and general health services.
Drug use: Initiation, role of male partner, users’ network.
Initiation of injection drug use was typically connected with a drug-injecting sexual partner (husband or boyfriend) and happened within a social network supportive of injection drug use. Although in rare cases a woman might make a deliberate decision to initiate drug use, in most cases first drug use was encouraged by and occurred in the presence of a male significant other—sex partner, friend, or relative. The man also was typically the drug supplier. Soon, the injection-drug-using woman became dependent on the man for both financial support and drug supply. The common belief among respondents was that a man is interested in a woman becoming dependent son drugs so that she would partner with him in terms of both a sexual relationship and financing their drug use—18 respondents disclosed that their current sexual partners had been the initiators of their first injection.
W30: “ When in a family only man injects he has to think of where to get money every day, while non-user wife distributes money according to the family needs. But if a woman becomes a drug user, then both of them spend most of the money on drugs, leaving small amount for their kids.”
As a woman’s drug use advanced, a man provided a continuous drug supply and injecting occurred in privacy only with him, thus protecting the woman from undesirable exposure to either drug dealers or other individuals who injected drugs. When a woman became part of a group that injected drugs, she preferred not to inject in front of men and moved to another room. The reason for separation was that her partner often feels ashamed in front of male friends to disclose that his wife/partner injected drugs. In turn, the woman was embarrassed to inject drugs in the presence of her partners’ friends (49% of women endorsed this viewpoint).
W28: “When it comes already to injection we separate ourselves from men. Men and women don’t inject together but if a husband and a wife are injecting then men helps his wife if they are injecting alone. If he is with male friends then he won’t help her.”
When a woman lost her male partner due to arrest, death, separation, or other reason, she faced challenges and was pushed to search for alternative drug sources. She was forced to become part of a network of drug users, often desperately looking for money, and began injecting in male-dominated groups. Respondents highlighted that, due to this lack of access to drugs, women experienced more episodes of withdrawal compared to men.
W6: “When you wake up you feel very bad, you start calling around, talking with passwords, they [police] were not tapping phones so intensively in the past like now but still you needed to be cautious. You call one central figure, he would ask, ‘Do you have 50 or 100, 120 GEL, if yes we can have a great party,’ but you still don’t believe because there were cases when they lied to you. I don’t know why, but I guess, because you are weak and cannot fight that much and also there are some other guys during a day who appear and they need to be ‘satisfied,’ so because you are a woman he puts you aside.”
Respondents’ accounts indicate that networks of women who inject drugs were rare, could be created spontaneously, depending on ad-hoc needs, and were unlikely to be stable. The usual scenario suggests that, when left alone, woman lack the requisite knowledge and skills to navigate through tightly woven, male-dominated drug networks. With few possibilities to find drugs and often limited knowledge of homemade drug production, such women often ended up partnering with a new man and may become part of a male-dominated group of injectors. All members of the group had their specific roles during the pre-consumption process. Women were usually assigned to get needles and cookers, get ingredients like potassium permanganate or red phosphorus, buy pills from pharmacies (such as pregabalin, rivotril, antihistamines, cough and cold medicines), or just to be transporters of drugs. Even when a woman’s contribution to this chain of activities was substantial, it was usually a man who oversaw the process and held the decision-making power regarding the distribution of the drugs within the network.
W4: “When my husband was free I did not bother about anything, he managed everything but when he got arrested. … You have to run around and try to find drugs… . You should try hard to find some in fear of not getting arrested and cooking and preparing it or bothering someone who will cook it for you, so it’s the whole story… .”
In addition to the predetermined non-privileged status of a woman in this group, she received very little respect from the group members and was considered untrustworthy. Respondents highlighted that men, as a rule, believed that a woman was too weak and, if arrested, she would readily “squeal” and cooperate with police. Importantly, our participants shared this belief (endorsed by 60% of women).
W15: “If he [drug-using man] does not have trust that is because she is a woman, otherwise drugs have nothing to do with trust, he is not trusting a woman herself. There are a lot of men who are squealing, each of them have been divulged now, so everyone knows who were cooperating with the police. As for woman, it does not really matter whether she is a user or not, after pressure they will all squeal.”
Risky behavior: Unsafe injection practice, sexual risks, and HIV/HCV testing.
Knowledge about injection-associated risks for blood-borne infections was relatively high. Participants’ accounts suggested sufficient awareness among women who use drugs and continuous efforts to avoid sharing drug paraphernalia. However, in real-life situations, unsafe injection practice routinely occurred (International Harm Reduction Development Program 2009; Rukhadze et al. 2009). In every male-dominated injector group discussed, the person contributing the most money defined the rules. Drug distribution among group members depended on the volume of such contributions, and a woman, whose status was low enough and who was usually able to make very little financial contribution to the “obschiak” (money collected for the group’s purposes), received lower doses of drugs compared to other group members. If the group was lacking syringes, it was usually a woman who would be second in a line for the syringe; if there were not enough drugs, she would be left on “vtoriak” (a secondary product that comes out after used filters are boiled and the leftover drug is extracted).
W18: “Man can leave women on a ‘vtoriak’ because he would say that she is a woman and does not need that amount of dose. ”
W6: “I have injected from preloaded syringe in the past, but I did not inject with one needle for example in a group of friends. What I know for sure that they were sharing needles because they could not buy it in pharmacies, police were standing nearby and arresting everyone who looked suspicious, that’s why they sent me to buy all the necessary paraphernalia.”
Condom use among participants was not a usual practice. The common belief was that condoms should be used with a partner whom women trusted less, but not with a regular partner. In addition, women typically obeyed socio-cultural norms and traditions and so hardly dared to request protected intercourse, even when they knew their partner had sexual contacts outside their sexual relationship. Some respondents believed that refusal to have unprotected contact with their regular partner could lead to violence. Respondents also stated that condom use was widely perceived to be associated with commercial sex work. When used, condoms were utilized primarily for pregnancy prevention, not STI prevention.
W15: “It [condom use] depends on her partner. Some can beat their women for sexual intercourse refusal.”
W04B: “Interviewer: What can happen if a woman asks a man to use a condom? Respondent: Again violence. He’ll start asking—where did you get it, are you sleeping with others, and so on.”
Few participants were aware of female condoms (7 women out of 55). With a number of respondents indicating that it was a man’s responsibility to have a condom and not a woman’s, a female condom was viewed by the women as an alternative to a male condom.
Sexual contact in exchange for drugs or money was reported to be a frequent practice. As the vast majority of injection-drug-using women were unemployed, exchanging sex could be the only way to obtain money and/or drugs. In striking contrast with other behaviors and themes that emerged in our interviews, none of the respondents admitted ever practicing this behavior. Sex in return for drugs or money appeared in a majority of interviews, but exclusively as a behavior of others, not the respondent herself.
Most respondents (67%) had never been tested for HIV or HCV. Testing appeared to be a threat for women and they were afraid to hear positive results. Only a few participants indicated that they had been tested regularly for STIs. Similar to prior research (NCDC 2014), most of our respondents believed that having HIV/AIDS was highly stigmatizing in Georgia. Thus, hiding one’s HCV-positive status protected her from damaging social consequences and preserved her relationships with family and friends.
W06: “… I think he took the test and talked about it very lightly, saying that probably all of us have hepatitis C, so it was not a big deal; it was very widespread in Tbilisi. I shared needles and probably that’s why he was saying that all of us have HCV. I’ve never taken testing on Hep C.”
W13: “My husband has A and B and C hepatitis and I’m very afraid to go and have tests, I will die before I get the results.”
Access to drug treatment and women’s experience with health service providers.
Some participants had fragmented information about either medication-assisted withdrawal or medication-assisted treatment; others were ignorant of the types of treatment available in Georgia. Social stigma and public attitudes towards women who use drugs were viewed as playing a major role in women’s treatment-seeking desire, and were seen as a major barrier for women to seek drug treatment.
W18: “Man is always a man, he is not ashamed of going to hospital or a doctor, even in the methadone programs; women cannot go to this program because everyone would see her. … I don’t have a husband or kids so I can freely go there but I have friends who can’t. …Well you can always go on your own to a doctor or a psychologist but there are no specific services for females; there is methadone program for men but nothing for women.”
The majority of respondents indicated that there are no available treatment programs that would address the specific needs of women.
W21: “ When a female drug user would decide to quit drugs and go for treatment there is no place in Georgia I guess that she would go to.”
Lack of confidentiality represented the principal problem, and there was very little assurance that service providers would not disclose a woman’s drug-using status to others. Various issues related to the structure of programs were mentioned, such as absence of a separate entrance to the building for women, standing in a line (for agonist medication) at a dispensing area together with male patients and taking the preparation in front of them, and lack of privacy when speaking with their doctors in the presence of other patients and medical personnel.
Despite the array of structural issues related to the provision of any form of substance use treatment predominant in Georgia, the majority of respondents did share a positive perception of medication-assisted treatment (endorsed by 69% of women); no women endorsed medication-free treatment.
W06: “I like this methadone program because my friends, they were running all day long, trying to get money, without eating, drinking, and now they are calm, going to one place and taking drugs is perfect for them; some were separated and returned to their wives and now have good relationship with families.”
However, myths and prejudice towards medication-assisted treatment were common, including among the respondents who are engaged in such treatment. Some respondents noted that medication-assisted treatment was still perceived as a health-damaging intervention and for many substance-using individuals represents the “last-choice” option when treatment was sought.
W15B: “I don’t believe in methadone programs, you get more addicted after that. I prefer to ask some friend and overcome physical and psychological craving on my own.”
W01: “A methadone program affects a human body in many ways. It affects teeth, liver, stomach.”
W18: “… methadone is the first enemy of liver ”
We found that sometimes, when a woman wished to enter treatment, either a male partner or a family member made the final decision about her treatment. Having a child/wife with a substance use disorder was socially unacceptable and viewed as shameful for the family. Therefore, family members were reluctant to take any action that would risk disclosure. However, respondents indicated that, in many cases, family support might depend on the level of education and of socio-economic status of a family. In many cases, a common practice was to provide treatment at home with medical personnel visiting the patient at her residence and promising confidentiality to the family.
W32: “It depends [whether she will go to treatment facility or not], first you should get permission from husband.”
W24: “I was a tennis player in the past and then it happened … when I realized that I became dependent on drugs I first told my mom, I was afraid of course but still… . Constant fear that this information will leak. … In my case they [family] treated me secretly at home and then I left town. Secretly because it’s an embarrassment and people would start gossiping a lot about you rather than help… .”
Drug-using status was indicated as the major barrier to employment.
W04: “… you will never start working if you are a drug user. I was working on a good position and when they found out that I was using, it was spread like a rumor or something, they dismissed me next day… . I’m professional in my field … they did not dismiss me because of not fulfilling my responsibilities … they told me directly, my boss told me that she had no desire to have drug user at work.”
Furthermore, with many women having a history of imprisonment, employment opportunities were further reduced.
W05: “I am not looking for it (here: job) because I have been in a jail and nobody allows me to start working.”
W25: “They (women who use drugs and have imprisonment history) don’t need any job if they have money but if they are obliged to work then, that’s impossible to find a job, they will never find one due to state policy. Believe me, everyone would know in one week about her drug use status and prison history. In all public sectors they ask certificate of conviction, test employees several times a month, and those who have positive urine test or have imprisonment history are dismissed. Private sector won’t employ you as well, that’s impossible.”
Respondents shared a variety of experiences they had with health professionals: obstetricians and gynecologists, emergency room doctors, general practitioners, addiction physicians, psychologists, and nurses. Some comments were positive and suggested that, in certain cases women do receive appropriate treatment. However, in many instances (23 respondents), participants’ experiences were negative—breach of confidentiality and judgmental attitude of health workers following the disclosure of drug use.
W05: “I once visited a doctor, I needed some medical paper for the program [medication-assisted treatment] and it turned out that the doctor was my neighbor. When she learned that I was a user she must have felt pity for me and she thoroughly examined me. I felt very warm attitude from her, like mother and daughter attitude, but such things happen very seldom. … I once took my friend to a doctor and he noticed that she was real bad and he also noticed that I was not feeling well as well. Finally he told us to get away; otherwise he threatened to call the police.”
W07: “Yes it is considered that they [doctors] are very humane and attentive but in reality it’s on the contrary, they have the same reaction as other ordinary people towards female drug use. You can see it on their faces, how they treat you! That’s horrible! That’s why they don’t go to a doctor. ”
DISCUSSION
This study enriches our understanding of the environment in which substance use is initiated and maintained in a female population in Georgia, and illustrates the importance of culture and the role of social factors in the development of injection drug use. Results of the study provide important information about the factors that shape drug use trajectories and help-seeking behavior of women navigating a complex, male-dominated “drug world.” Similar to findings of other authors, the male partner plays a critical role in forming the substance-use-related behaviors of the woman—he supports initiation of use (Greenfield et al. 2010), is a main supplier of drugs, and often holds a decision-making power over behaviors that can put a woman under heightened risk for infection transmission (for example, used syringes and “vtoriak” for the female injector). This heightened risk of infection through unsafe injecting practices can be directly linked to the inequitable power distribution in male-dominated drug injection networks. In Georgia and elsewhere in the region, compared to men, women who use drugs have reported higher levels of sharing injecting equipment, drug paraphernalia, and needles (International Harm Reduction Development Program 2009; Rukhadze et al. 2009). While the reasons for these higher rates have yet to be elucidated, they likely reflect a power imbalance favoring male dominance and thereby increasing women’s vulnerability in many aspects of life.
The majority of respondents were unemployed and never had held a job. In general, probably reflecting the traditionally good level of literacy and education in Georgia (UNICEF 2008), our participants were comparatively well-educated; however, they lacked job skills and social or economic support. Some had criminal records that were a major barrier to finding gainful employment (Javakhishvili et al. 2012). Respondents believed it was particularly difficult for them to be hired because of what they saw as greater social stigma attached to jail time for women who use substances. With few legitimate work possibilities, women continued to find economic support engaging in sex work, increasing their risk of HIV/HCV/STI infection.
Our previous reports identified socio-cultural and personal factors shaping help-seeking behavior of women with substance use problems in Georgia (Kirtadze et al. 2013; Otiashvili et al. 2013; 2014). The present research suggests that stigmatization from the broader society, intolerance and judgmental attitudes, including on the part of health care providers, negatively affect women’s desire to admit drug use and to seek treatment. The fear of social isolation and rejection causes substance-using women to delay seeking help, not just for the treatment of their substance use, but also for their general health and psychosocial needs. Moreover, in Georgia and elsewhere, the absence of targeted women-specific services with substance use problems plays an additional demotivating role in seeking treatment (Kandall 2010; Orwin, Francisco & Bernichon 2011).
With the gradually narrowing gender gap in substance-use-related disorders, there has been increased attention from treatment providers focusing on issues related to substance use by women (Greenfield et al. 2010; Jones, O’Grady & Tuten 2011; Jones & Kaltenbach 2013). This has led to the accumulation of knowledge and development of various women-centred interventions that address specific needs of this population (Jones, Finnegan & Kaltenbach 2012; Jones et al. 2001; 2011; Greenfield et al. 2007b; Wechsberg et al. 2004; 2010; 2011; 2012) Nevertheless, according to the English language literature review of 280 articles by Greenfield and colleagues, “women with substance use disorders are less likely, over the lifetime, to enter treatment compared to their male counterparts” (Greenfield et al. 2007a). In Georgian reality, most women who use drugs do not seek treatment for their drug-related problems. Women constitute 20–40% of patients in drug dependence treatment services in the EU and in the US (EMCDDA 2005; Grella 2007), and 8% in some post-Soviet countries (CADAP 2012). In stark contrast, only 1–2% of beneficiaries in substance-use-related services in Georgia are women. The interviews underscore both the lack of and the need for the development of women-focused substance-use treatment services. The fact that a very small number of women entered such treatment may be attributed to the existing stigma against women who use drugs and the lack of availability of either women-sensitive or women-focused services in the country (Pinkham & Malinowska-Sempruch 2007). As emphasized in our previous report (Kirtadze et al. 2013), none of the specific needs that would make treatment both beneficial and attractive to women with substance-use-related problems, such as childcare, pregnancy, financial status, transportation, and reduction in social stigma (Jones & Kaltenbach 2013), were addressed in either agonist or drug-free treatment programs open to women in Georgia. Our findings confirm the critical role of the drug-using male partner and other family members in supporting or inhibiting a woman’s desire to seek treatment for her substance-use-related problems. These gender disparities help to explain the lack of women in low-threshold and drug treatment programs in Georgia.
Study limitations include a sampling approach which was purposive and not random, and the sample may not be representative of injection-drug-using women in Georgia. Findings rely on self-reports provided during in-depth interviews, creating a potential bias. However, to minimize bias, participants were guaranteed confidentiality and individual face-to-face interviews were conducted in private settings.
With these cautions in mind, our findings provide information on several major issues that can be used to shape the direction for tailoring the development of interventions for substance use disorders, public policy discussions regarding the treatment of women who use drugs, and future research on substance use among women in Georgia and other post-Soviet nations.
REFERENCES
- Bouscaillou J; Champagnat J; Luhmann N; Avril E; Inaridze I; Miollany V; Labartkava K; Kirtadze I; Butsashvili M; Kamkamidze G. & Pataut D. 2014. Hepatitis C among people who inject drugs in Tbilisi, Georgia: An urgent need for prevention and treatment. The International Journal on Drug Policy 25 (5): 871–878. [DOI] [PubMed] [Google Scholar]
- Buckley C. 2005. The socio-cultural orrelates of HIV/AIDS in the Southern Caucasus. HIV and AIDS in the Caucasus: A Socio-Cultural Approach, 11–33. [Google Scholar]
- CADAP. 2012. Kyrgyzstan Country Overview: Drug Situation 2010. The European Union’s Central Asia Drug Action Programme (CADAP), Bishkek, Kyryzstan. [Google Scholar]
- Chkhartishvili N; McNutt L-A; Smith PF & Tsertsvadze T. 2011. Characteristics of HIV-infected women and factors associated with HCV seropositivity in the Republic of Georgia. AIDS Research and Therapy 8: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMCDDA. 2005. Differences in patterns of drug use between women and men. European Drug Situation Technical Data Sheet, Lisbon, Portugal. [Google Scholar]
- Georgian AIDS and Clinical Immunology Centre. 2014. HIV/AIDS epidemiology in Georgia. Available at: http://aidscenter.ge/epidsituation_eng.html. Accessed October 2014.
- Goldstein P. 1979. Prostitution and Drug Use. Lexington, MA: Lexington Books. [Google Scholar]
- Government of Georgia. 2010. UNGASS Country Progress Report, Reporting Period 2008 – 2009 Calendar Years. Tbilisi. [Google Scholar]
- Greenfield SF; Back SE; Lawson K. & Brady KT 2010. Substance abuse in women. Psychiatric Clinics of North America 33 (2): 339–355. doi: 10.1016/j.psc.2010.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF; Brooks AJ; Gordon SM; Green CA; Kropp F; McHugh K; Lincoln M; Hien D. & Miele GM 2007a. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence 86: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF; Trucco EM; McHugh RK; Lincoln M. & Gallop RJ 2007b. The Women’s Recovery Group Study: A Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug and Alcohol Dependence 90: 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE 2007. Substance Abuse Treatment Services for Women: A Review of Policy Initiatives and Recent Research. Los Angeles: UCLA Integrated Substance Abuse Programs. [Google Scholar]
- Grund JP; Latypov A. & Harris M. 2013. Breaking worse: The emergence of krokodil and excessive injuries among people who inject drugs in Eurasia. The International Journal on Drug Policy 24 (4): 265–274. [DOI] [PubMed] [Google Scholar]
- International Harm Reduction Development Program. 2009. Women, Harm Reduction, and HIV: Key Findings from Azerbaijan, Georgia, Kyrgyzstan, Russia, and Ukraine. New York. [Google Scholar]
- Javakhishvili DJ; Balanchivadze N; Kirtadze I; Sturua L; Otiashvili D. & Zabransky T. 2012. Overview of the Drug Situation in Georgia, 2012. Tbilisi: Global Initiative on Psychiatry/Alternative Georgia. [Google Scholar]
- Javakhishvili DJ; Balanchivadze N; Kirtadze I; Sturua L; Otiashvili D.& Zabransky T. 2013. Drug Situation in Georgia (No. 978–9941-0–5129-5). Tbilisi, Georgia: Global Initiative on Psychiatry—Tbilisi & Alternative. [Google Scholar]
- Javakhishvili DJ; Sturua L; Kirtadze I; Otiashvili D. & Zabransky T. 2011. Overview of the drug situation in Georgia. Adictologie 11 (1): 42–51. [Google Scholar]
- Jones HE; Finnegan LP & Kaltenbach K. 2012. Methadone and buprenorphine for the management of opioid dependence in pregnancy. Drugs 72: 747–57. [DOI] [PubMed] [Google Scholar]
- Jones HE; Haug N; Silverman K; Stitzer M. & Svikis D. 2001. The effectiveness of incentives in enhancing treatment attendance and drug abstinence in methadone-maintained pregnant women. Drug and Alcohol Dependence 61: 297–306. [DOI] [PubMed] [Google Scholar]
- Jones HE & Kaltenbach K. 2013. Treating Women with Substance Use Disorders During Pregnancy: A Comprehensive Approach to Caring for Mother and Child. New York: Oxford University Press. [Google Scholar]
- Jones HE; O’Grady KE & Tuten M. 2011. Reinforcement-based treatment improves the maternal treatment and neonatal outcomes of pregnant patients enrolled in comprehensive care treatment. American Journal on Addictions 20: 196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandall SR 2010. Women and drug addiction: A historical perspective. Journal of Addictive Diseases 29: 117–126. [DOI] [PubMed] [Google Scholar]
- Kirtadze I; Otiashvili D; O’Grady KE; Zule WA; Krupitski EM; Wechsberg WM & Jones HE 2013. Twice stigmatized:Health service provider’s perspectives on drug-using women in the Republic of Georgia. Journal of Psychoactive Drugs 45 (1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Disease Control and Public Health (NCDC). 2014. Global AIDS Response Progress Report of Georgia 2012–2013. Available at: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/GEO_narrative_report_2014.pdf. Accessed October 2014.
- Needle R. & Zhao L. 2010. HIV Prevention among Injection Drug Users Strengthening U.S. Support for Core Interventions: A Report of the CSIS Global Health Policy Center. Washington, DC: Center for Strategic and International Studies. [Google Scholar]
- Orwin RG; Francisco L. & Bernichon T. 2011. Effectiveness of Women’s Substance Abuse Treatment Programs: A Meta-Analysis Center of Substance Abuse Treatment. Arlington, VA: SAMSHA. [Google Scholar]
- Otiashvili D; Kirtadze I; O’Grady KE; Zule W; Krupitsky E; Wechsberg WM & Jones HE 2013. Access to treatment for substance-using women in the Republic of Georgia: Socio-cultural and structural barriers. The International Journal on Drug Policy 24 (6): 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiashvili D; Kirtadze I; O’Grady KE; Zule W; Krupitsky E; Wechsberg WM & Jones HE 2014. Comprehensive women-centered treatment for substance use disorders in Georgia: Current status and future directions. Journal of Substance Use. doi: 10.3109/14659891.2014.923052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike K. 1990. On the emics and etics of Pike and Harris In: Headland T, Pike K. & Harris M (Eds.) Emic and Etics: The Insider/Outsider Debate, pp. 28–47. Newbury Park, CA: Sage. [Google Scholar]
- Pinkham S. & Malinowska-Sempruch K. 2007. Women, Harm Reduction and HIV. New York: Open Society Institute. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M. 1981. Women on Heroin. New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Rukhadze N; Chikovani I; Goguadze K; Sirbiladze T. & Tavzarashvili L. 2009. Bio-behavioral Surveillance Surveys among Injecting Drug Users in Georgia (Tbilisi, Batumi, Zugdidi, Telavi, Gori, 2008–2009): Study Report. Tbilisi: Curatio International Foundation, Public Union Bemoni. [Google Scholar]
- Sirbiladze T. & Tavzarashvili L. 2012. Estimating the Prevalence of Injection Drug Use in Georgia. Tbilisi: Bemoni Public Union. [Google Scholar]
- UNICEF. 2008. Country Profile: Education in Georgia. Available at: http://www.unicef.org/ceecis/Georgia.pdf. Accessed October 2014.
- Waldorf D. 1973. Careers in Dope. Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Wechsberg WM; Browne FA; Middlesteadt Ellerson R. & Zule WA 2010. Adapting the evidence-based women’s CoOp HIV prevention intervention in North Carolina and international settings. North Carolina Medical Journal 71 (5): 477–481. [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM; Krupitsky E; Romanova T; Zvartau E; Kline TL; Browne FA; Ellerson RM; Bobashev G; Zule WA & Jones HE 2012. Double jeopardy—drug and sex risks among Russian women who inject drugs: Initial feasibility and efficacy results of a small randomized controlled trial. Substance Abuse Treatment Prevention and Policy 7 (1). doi: 10.1186/1747-597X-7-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM; Lam WKK; Zule WA & Bobashev G. 2004. Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. American Journal of Public Health 94 (7): 1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM; Zule WA; Luseno WK; Kline TL; Browne FA; Novak SP & Ellerson RM 2011. Effectiveness of an adapted evidence-based woman-focused intervention for sex workers and non-sex workers: The Women’s Health CoOp in South Africa. Journal of Drug Issues 41 (2): 233–252. [Google Scholar]
- Zaalishvili L; Chavchanidze M. & Mchedlishvili N. 2013. Female Drug Users in Georgia: Needs Assesment. Tbilisi: Georgian Harm Reduction Network. [Google Scholar]