Abstract
Objective:
We report a case of unilateral adrenal hemorrhage resulting in adrenal insufficiency in a patient on rivaroxaban for thromboprophylaxis after total knee arthroplasty.
Methods:
The clinical presentation, laboratory findings, and outcome of the case are described. An overview of the etiology, diagnosis, and treatment of adrenal hemorrhage is reviewed.
Results:
A 61-year-old male underwent bilateral total knee replacements and postoperatively was started on rivaroxaban at 10 mg daily for thromboprophylaxis. About 2 weeks after the procedure, the patient presented with abdominal pain, nausea, vomiting, and generalized weakness. Abdominal computed tomography scan identified an ill-defined heterogeneous density in the left supra-renal fossa, and an abdominal magnetic resonance imaging scan identified diffuse thickening of the left adrenal gland with periadrenal fat stranding suggestive of adrenal hemorrhage. Adrenal insufficiency was suspected and confirmed with a cosyntropin stimulation test. Pre-stimulus cortisol level was 2.7 μg/dL and 60 minutes after cosyntropin administration it was 2.5 μg/dL. The patient was started on intravenous hydrocortisone at 100 mg every 6 hours with improvement of symptoms and discharged on oral hydrocortisone at 20 mg twice daily. Follow up abdominal magnetic resonance imaging 6 weeks after discharge demonstrated resolution of the left adrenal hemorrhage.
Conclusion:
A high clinical suspicion and early detection of adrenal hemorrhage in a patient on anticoagulation can allow for earlier intervention and improved outcomes.
INTRODUCTION
Adrenal hemorrhage is a rare complication that can result from the use of anticoagulation treatments (1–3). Historically, the diagnosis had been made in postmortem examinations but the emergence of more sophisticated imaging modalities has allowed for the ability to establish the diagnosis earlier in the clinical course (4). Literature reports of adrenal hemorrhage from the use of anticoagulants has more often been associated with heparin, low-molecular-weight heparin, and warfarin (5–10). We present a case of rivaroxaban-induced adrenal hemorrhage with subsequent adrenal insufficiency following total knee arthroplasty.
CASE REPORT
A 61-year-old male with a history of osteoarthritis presented to the hospital from his primary care physician's office with abdominal pain, nausea, vomiting, and generalized weakness. The patient had undergone bilateral total knee replacements about 2 weeks prior to presentation and had been placed on rivaroxaban at 10 mg daily for thromboprophylaxis. The patient did well postoperatively and was discharged on the third postoperative day, but 2 days after discharge developed nausea and vomiting prompting a visit to the emergency department. At the time, the patient was determined to be dehydrated and treated with intravenous fluids. He improved and was discharged; however, over the next 10 days the patient developed right knee swelling, left upper quadrant abdominal discomfort, nausea, and vomiting, prompting another visit to the emergency department.
Labs at the time were significant for anemia with hemoglobin of 8.0 g/dL. The right knee swelling was determined to be secondary to hemarthrosis. Computed tomography (CT) scan of the abdomen and pelvis identified an ill-defined heterogeneous density in the left suprarenal fossa suggestive of a subacute left adrenal hemorrhage (Fig. 1). Further evaluation with an abdominal magnetic resonance imaging (MRI) scan identified diffuse thickening of the left adrenal gland with periadrenal fat stranding, the likely sequelae of adrenal hemorrhage. A random cortisol level at the time was within normal range at 16.6 μg/dL.
Fig. 1.
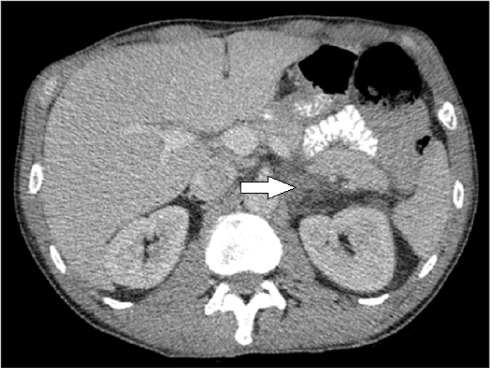
Computed tomography scan of the abdomen and pelvis showing an ill-defined heterogeneous density in the left suprarenal fossa.
During this hospitalization, the patient received Kcentra® (human prothrombin complex concentrate) and vitamin K for the right knee hemarthrosis and left adrenal hemorrhage. Two units of packed red blood cells were also transfused for the acute blood loss anemia. With consideration of the normal random cortisol level and a stable hemoglobin level, the patient was discharged on hospitalization day 3 with instruction to discontinue rivaroxaban.
Six days after leaving the hospital the patient presented to his primary care physician's office with progressive nausea, vomiting, and generalized weakness and found to be hypotensive, hyponatremic, and hyperkalemic. The patient was subsequently directed to the emergency department for further evaluation, leading to the aforementioned hospital presentation.
Following admission, laboratory values were significant for hyponatremia with sodium of 126 mmol/L and hyperkalemia with potassium of 5.6 mmol/L, consistent with adrenal insufficiency particularly when taken into account with the patient's clinical presentation. A cosyntropin stimulation test was performed to confirm adrenal insufficiency. Pre-stimulus cortisol level was 2.7 μg/dL and 60 minutes after cosyntropin administration was essentially unchanged at 2.5 μg/dL. A diagnosis of adrenal insufficiency was made. The patient was started on intravenous hydrocortisone at 100 mg every 6 hours with subsequent improvement of his symptoms and discharged on hospitalization day 3 with oral hydrocortisone at 20 mg twice daily. Follow-up abdominal MRI approximately 6 weeks after hospital discharge demonstrated resolution of the left adrenal gland hemorrhage.
DISCUSSION
Risk factors for adrenal hemorrhage include anticoagulation therapy, corticotropin stimulation, metastatic disease to the adrenal gland, adrenal tumor, trauma, severe sepsis, antiphospholipid syndrome, and recent surgery (4,5,9). The clinical presentation of adrenal hemorrhage is nonspecific and makes establishing the diagnosis a challenge. For this reason, having a high degree of clinical suspicion is important in facilitating an earlier diagnosis to avoid unfavorable outcomes. Signs and symptoms can include back or flank pain, anorexia, nausea, vomiting, hypotension, and fever (3–5). Adrenal insufficiency from adrenal hemorrhage is more often associated with bilateral adrenal hemorrhage, but in cases of unilateral adrenal hemorrhage it is suspected that the contralateral adrenal gland becomes “exhausted” with decreased or absent cortical lipid resulting in hypocortisolemia (2).
Imaging studies that can identify adrenal hemorrhage include CT, MRI, and ultrasound (5,10,11). Adrenal gland enlargement with signal attenuation greater than that seen with fluid on CT scan is suggestive of adrenal hemorrhage. A non-enhancing adrenal mass with a high T1 signal intensity visualized on MRI is indicative of adrenal hemorrhage (10,11).
Laboratory findings, if present, are usually consistent with adrenal insufficiency and include hyponatremia, hyperkalemia, hypoglycemia, leukocytosis, acidosis, and azotemia; however, these abnormalities are not always present (1,4,9). A cosyntropin stimulation test can aid in the diagnosis with cortisol measurements at baseline, 30 minutes, and 60 minutes following cosyntropin administration (5).
Treatment of adrenal insufficiency should not be delayed by waiting to confirm the diagnosis with laboratory tests in cases with high clinical suspicion. The mainstay of medical treatment for adrenal insufficiency is with corticosteroids. Rarely, adrenalectomy or embolization may be required to treat the adrenal hemorrhage (5). Complete recovery from adrenal hemorrhage may be possible and the requirement for long-term corticosteroid treatment can be re-evaluated with a cosyntropin stimulation test following the acute period.
CONCLUSION
This case demonstrates the importance of having a high clinical suspicion in diagnosing adrenal hemorrhage in a patient on anticoagulation medication presenting with nonspecific symptoms, as it can manifest with life-threatening acute adrenal insufficiency. Prompt diagnosis can allow for immediate intervention and improved outcomes.
Abbreviations:
- CT
computed tomography
- MRI
magnetic resonance imaging
Footnotes
DISCLOSURE
The authors have no multiplicity of interest to disclose.
REFERENCES
- 1.Rao RH. Bilateral massive adrenal hemorrhage. Med Clin North Am. 1995;79:107–129. doi: 10.1016/s0025-7125(16)30087-6. [DOI] [PubMed] [Google Scholar]
- 2.Vella A, Nippoldt TB, Morris JC., III Adrenal hemorrhage: a 25-year experience at the Mayo Clinic. Mayo Clin Proc. 2001;76:161–168. doi: 10.1016/S0025-6196(11)63123-6. [DOI] [PubMed] [Google Scholar]
- 3.Danese CA, Viola RM. Adrenal hemorrhage during anticoagulant therapy. Ann Surg. 1974;179:70–72. doi: 10.1097/00000658-197401000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.May CJ, Asia M, Karavitaki N, Arlt W, Guest P, O'Reilly MW. Bilateral adrenal haemorrhage. QJM. 2017;110:169–171. doi: 10.1093/qjmed/hcw212. [DOI] [PubMed] [Google Scholar]
- 5.Park KJ, Bushmiaer M, Barnes CL. Bilateral adrenal hemorrhage in a total knee patient associated with enoxaparin usage. Arthroplast Today. 2015;1:65–68. doi: 10.1016/j.artd.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Comuth W, Christiansen JJ, Bloch-Münster A, Husted S. Bilateral adrenal gland hemorrhage in a patient treated with rivaroxaban. Blood Coagul Fibrinolysis. 2017;28:102–104. doi: 10.1097/MBC.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 7.Chronopoulos E, Nikolaou VS, Masgala A, Kaspiris A, Babis GC. Unilateral adrenal hemorrhage after total knee arthroplasty. Orthopedics. 2014;37:e508–e511. doi: 10.3928/01477447-20140430-65. [DOI] [PubMed] [Google Scholar]
- 8.LaBan MM, Whitmore CE, Taylor RS. Bilateral adrenal hemorrhage after anticoagulation prophylaxis for bilateral knee arthroplasty. Am J Phys Med Rehabil. 2003;82:418–420. doi: 10.1097/01.PHM.0000064741.97586.E4. [DOI] [PubMed] [Google Scholar]
- 9.Siu SC, Kitzman DW, Sheedy PF, Jr, Northcutt RC. Adrenal insufficiency from bilateral adrenal hemorrhage. Mayo Clin Proc. 1990;65:664–670. doi: 10.1016/s0025-6196(12)65129-5. [DOI] [PubMed] [Google Scholar]
- 10.Rajamanickam A, Patel P, Anbazhagan P, Harte B. A life threatening complication of anticoagulation prophylaxis-bilateral adrenal hemorrhage. J Hosp Med. 2009;4:E25–E27. doi: 10.1002/jhm.485. [DOI] [PubMed] [Google Scholar]
- 11.Jordan E, Poder L, Courtier J, Sai V, Jung A, Coakley FV. Imaging of nontraumatic adrenal hemorrhage. Am J Roentgenol. 2012;199:W91–W98. doi: 10.2214/AJR.11.7973. [DOI] [PubMed] [Google Scholar]


