Abstract
Prescription opioid medications are commonly used for the treatment of chronic pain. Assessments of problematic opioid use among pain patients are inconsistent across studies, partially due to differences between various measures. Therefore, the most appropriate measure to use is often unclear. In this study we assessed problematic opioid use in a sample of 551 individuals receiving treatment for chronic pain, using three questionnaires: the Alcohol Use Disorder and Associated Disabilities Interview Schedule – Fourth Edition (AUDADIS‐IV), the Current Opioid Misuse Measure (COMM) questionnaire and Portenoy's criteria (PC). These questionnaires yielded discordant positive rates of problematic use: 52.6%, 28.7%, and 17.1%, respectively, which did not change substantially when excluding AUDADIS‐IV criteria of physical symptoms of tolerance and withdrawal. Although these three questionnaires share some statistically correlated content‐based congruent questions, positive response rates to them were significantly different based on construction features, including questionnaires' referred time‐frame, wording of questions and response alternatives. The findings of the present study illustrate strengths and limitations of the AUDADIS‐IV, COMM and PC in diagnosing problematic opioid use in a population of adults suffering from chronic pain, and highlight the importance of recognizing and addressing specific questionnaire and question‐related differences when identifying problematic opioid use in this population.
Keywords: chronic pain, opioid, prevalence, problematic use, questionnaires
1. INTRODUCTION
Chronic pain is a common cause of disability among adults, as it impedes activities of daily living and work ability, and reduces quality of life (Andrew, Derry, Taylor, Straube, & Phillips, 2014; Von Korff, Kolodny, Deyo, & Chou, 2011). Over the past 25 years opioid medications have been increasingly prescribed and used for the treatment of chronic pain in many developed countries, including the United States, Canada and Australia (Dhalla, Persaud, & Juurlink, 2011; Fischer & Argento, 2012; Jamison & Mao, 2015; Roxburgh, Bruno, Larance, & Burns, 2011), and they are now among the most commonly prescribed medications for this indication (Grady, Berkowitz, & Katz, 2011; Pohl & Smith, 2011).
The increase in use of opioid medications for the treatment of chronic pain has been accompanied by reports of non‐medical use of these drugs worldwide (International Narcotics Control Board [INCB], 2015; United Nations Office on Drugs and Crime [UNODC], 2014: Kuehn, 2007), as well as repeated reports of associated harms (Manchikanti, Fellows, Ailinani, & Pampati, 2010; Roxburgh et al., 2011; Trescot et al., 2008). Exceeding the use of street narcotics in the United States (CDC, 2009; Hall et al., 2008; Manchikanti, Manchikanti, Damron, Pampati, & Fellows, 2007; Manchikanti et al., 2010) and reaching epidemic proportions, misuse of prescription opioids is an emerging public health concern that confers significant risks for overdose, unsafe drug interactions, and a wide range of adverse social and legal consequences (Wilson, 2007).
Given the high prevalence of prescription opioid use among chronic pain patients, this population may be particularly at risk for developing problems associated with long‐term use of prescription opioids such as tolerance, dependency, addiction, abnormal pain sensitivity, cognitive dysfunction, hormonal changes, immune modulation (Ballantyne & Mao, 2003), and an increased risk for fatal overdose (Sehgal, Manchikanti, & Smith, 2012). Furthermore, many patients with chronic pain who use opioids have deteriorated, rather than improved their functioning due to side effects of these potent drugs (Pohl & Smith, 2012).
The prevalence of prescription opioid use and misuse among individuals with chronic pain is unclear due to heterogeneity in findings across different studies. A systematic review conducted by Minozzi, Amato, and Davoli (2013), which aimed to assess the prevalence of prescription opioid addiction (as defined by the Diagnostic and Statistical Manual of Mental Disorders, fourth edition [DSM‐IV] or the International Classification of Diseases, 10th revision [ICD‐10]) reported prevalence rates ranging from 0 to 31%; a previous review reported rates ranging from 0 to 50% (Hojsted & Sjogren, 2007). Taken together, different studies indicate a wide range in the prevalence of opioid use disorders among chronic pain patients. This inconsistency may be explained by the use of different diagnostic criteria, assessment tools, clinical populations and research methodology (Hojsted, Nielsen, Guldstrand, Frich, & Sjogren 2010). Specifically, some assessment tools measuring problematic use of prescription opioids are specific to opioid use in pain treatment settings, such as the Prescription Drug Use Questionnaire (PDUQ, Compton, Darakjian, & Miotto 1998), the Addiction Behaviors Checklist (ABC, Wu et al., 2006), the Pain Medication Questionnaire (PMQ, Passik et al., 2004) and the Current Opioid Misuse Measure (COMM, Butler et al., 2007). Other assessment tools are designated for use in general medical settings, including the ICD‐10 (World Health Organization [WHO], 1992), the Drug Abuse Screening Test (DAST; Yudko, Lozhkina, & Fouts, 2007), the Substance Use Brief Screen (SUBS; McNeely et al., 2015) and the Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM‐IV (AUDADIS‐IV; Grant, Dawson, & Hasin, 2001). Furthermore, some questionnaires emphasize the cluster of physical symptoms as an essential feature (e.g. DSM‐IV; American Psychiatric Association [APA], 1994), while in others these do not appear at all (e.g. the COMM [Butler et al., 2007] and Portenoy's Criteria [PC; Portenoy, 1990]). Currently, the most appropriate measure for identifying problematic use of prescription opioids among chronic pain patients is still unclear, given the variety of methods applied by different questionnaires for this purpose.
The aim of the current study was to assess and compare leading tools for assessing problematic use of prescription opioids among chronic pain patients. We hypothesized that different assessment tools will produce discordant diagnostic rates within the same population; moreover, we hypothesized that architectural (e.g. the type, wording and scoring of questions) sources of variation may contribute substantially to this discordance.
2. METHODS
2.1. Participants
The study sample included chronic pain patients (N = 551) using prescription opioids and treated in the two largest pain centers in Israel: Sheba Medical Center and Sourasky Medical Center. Each patient treated at these two centers for chronic pain (i.e. pain lasting for more than three months [Elliott, Smith, Penny, Smith, & Chambers, 1999]) was approached for recruitment for the study during a six‐month period (November 2014–April 2015). The response rate was 57%. Patients were excluded from the sample if they had language barriers not allowing understating of the questionnaires or had a cognitive or motor dysfunction which prevented them from filling questionnaires. Every patient who participated in this study was required to sign an informed consent form prior to participation, which was then immediately detached from the questionnaire upon completion and indexed (in order to allow anonymous data collection and increase reliability of respondents' replies) (Harrison, 1997). This study was approved by the Institutional Review Board (IRB) committee at both medical centers.
2.2. Measures
As terminology regarding substance use disorders is dynamic and inconsistent across time and regions, and as the title of each questionnaire uses a different term to target these disorders, we collectively use the term “problematic use” for those who qualify for a positive diagnosis in any one of the questionnaires included in this study as indicated by the appropriate cutoff points listed later.
2.3. Addiction measures
We assessed prescription opioid addiction using the following three questionnaires:
AUDADIS‐IV is a designated questionnaire for the assessment of alcohol, drug, and mental disorders using DSM‐IV diagnostic criteria (Grant et al., 2001). For the objective of the current study only the DSM‐IV criteria for opioid dependence were used. Based on DSM‐IV dependence criteria, three out of seven criteria are required to consider positive for dependence. Each of the diagnostic criteria appears as one or more questions; for example, DSM‐IV criterion which refers to dose escalation is represented by the question “often use a medicine or drug in larger amounts or for a much longer period than you meant to?”, whereas the DSM‐IV criterion which refers to side effects caused or exacerbated by the drug is represented by two separate questions: “Continue to use a medicine or drug even though it was making you feel depressed, uninterested in things, or suspicious or distrustful of other people?” and “Continue to use a medicine or drug even though you knew it was causing you a health problem or making a health problem worse?”. AUDADIS‐IV consists of dichotomous items, with two possible answers for each question (yes/no). Test–retest reliability for AUDADIS‐IV diagnosis of lifetime non‐medical opioid use and dependence resulting from non‐medical opioid use in general population and clinical settings is moderate to good with kappa values ranging from 0.59 for current and lifetime dependence, and 0.66 for lifetime use (Grant, Harford, Dawson, Chou, & Pickering, 1995; Hasin, Carpenter, McCloud, Smith, & Grant, 1997). This set of criteria was elected due to its utility in clinical psychiatric setting. Though the AUDADIS is originally intended to be administered by a lay interviewer, for the purpose of this study it was adapted as a self‐administered questionnaire. The use of AUDADIS‐IV as a questionnaire rather than an interview schedule was applied in order to maintain the anonymity of the participants and to enhance the authenticity and reliability of their replies (Del Boca & Noll, 2000; Harrell, 1997) and has been practiced in previous studies (see for example Scott‐Sheldon et al., 2014).
PC questionnaire is a 10‐item self‐report questionnaire for diagnosing addiction among patients treated with opioids for the management of pain (Portenoy, 1990). Criteria for prescription opioid addiction include a positive response to both first items A (an intense desire for the drug) and B (an overwhelming concern about the drug's availability), as well as at least one additional positive reply to any of the following criteria: unsanctioned dose escalation; continued dosing despite significant side effects; use of drug to treat symptoms not targeted by therapy; unapproved use during periods of no symptoms; manipulation of the treating physician or medical system for the purpose of obtaining additional drugs; acquisition of drugs from other medical sources or from non‐medical sources and drug hoarding. The PC consists of dichotomous items, with two possible answers for each question (yes/no). It has high concurrent validity, high inter‐rater agreement (0.93), high sensitivity (0.85) and specificity (0.96); this set of criteria was elected due to its sensitivity and specificity (Hojsted et al., 2010) in chronic pain populations.
The COMM is a self‐report questionnaire designed to monitor current medication‐related aberrant behaviors during ongoing opioid treatment (Butler et al., 2007). The 17 items appearing in the COMM are scaled from 0 = never to 4 = very often (e.g. in the past 30 days, how often have you had to take more of your medication than prescribed?) with a total maximum score of 68. Test–retest reliability was 0.86 with a 95% confidence interval (CI) ranging from 0.77 to 0.92. The overall accuracy of the COMM for predicting current aberrant drug‐related behavior, as measured by the area under the curve ratio, was 0.81 (95% CI, 0.74–0.86; p < 0.001) and coefficient a (0.86) for the 17‐items suggests adequate reliability. An accumulated cutoff score of nine or higher is considered positive (Butler et al., 2007).
2.4. Psychiatric co‐morbidities
Participants were screened for psychiatric disorders using the following instruments:
Prime MD PHQ (PHQ‐9) – The depression module of the self‐administered Patient Health Questionnaire (PHQ), represents the nine DSM‐IV depression criteria using nine items (APA, 2014) scored on a three‐point scale (0 = not at all to 3 = nearly every day). Scores can range from 0 to 27 with higher scores reflecting a greater symptom severity (each score of additional five points up to 20 represents a cut‐point for mild, moderate, moderately severe and severe depression, respectively) (Spitzer, Kroenke, & Williams, 1999). The PHQ questionnaire has a good agreement between PHQ diagnoses and those of independent mental health professionals (for the diagnosis of any one or more PHQ disorder, κ = 0.65; overall accuracy, 85%; sensitivity, 75%; specificity, 90%), similar to the original Prime‐MD (administered by clinician) (Spitzer, Williams, & Kroenke, 2009).
Generalized anxiety disorder scale (GAD‐7) – a seven item measure developed to diagnose generalized anxiety disorder and to measure the severity of symptoms following DSM‐IV criteria (Spitzer, Williams, & Kroenke, 2009). Each item is rated on a 0–3 scale relating to the frequency of anxiety symptoms over the last two weeks (0 = “not at all” to 3 = “nearly every day”). Scores can range from 0 to 21 with higher scores indicating a greater severity of anxiety. Scores of 5, 10, and 15 are taken to represent mild, moderate, and severe levels of anxiety. The original validation study proposes that a cutoff score of 10 provides an optimal trade‐off between sensitivity (89%) and specificity (82%) for a diagnosis of GAD. The measure's reliability, construct validity, and factorial validity have been established in the general population (Löwe et al., 2008).
2.5. Clinical data
Medical history questionnaire – a self‐report of life‐time diagnosis of medical conditions. This questionnaire contains a list of the following common medical conditions: hypertension, liver disease, heart disease, duodenal ulcer, migraine, herniated disc, arthritis, fibromyalgia and depression.
Substance use questionnaire – a self‐administered questionnaire of past year and life‐time history of substance use and substance use disorders (including alcohol, cannabis, stimulants, hallucinogens and opioids).
2.6. Statistical analyses
We explored rates of problematic opioid use according to each of the questionnaires by calculating the portion of participants positively diagnosed by each questionnaire separately. Next, we examined the overlap between questionnaires by calculating the proportion of participants with problematic opioid use by all three questionnaires, two out of three or just one of them. Assessing agreement between questionnaires in rates of problematic opioid use was conducted using the kappa statistic.
In order to detect sources of variance in diagnosis rates according to the different questionnaires, we used an approach based on the following sets of analyses:
Simulated changes in diagnostic criteria. In order to explore the importance of physical‐based criteria as a source of variance in diagnoses rates according to the different questionnaires, we simulated a change in diagnostic criteria according to AUDADIS‐IV. Since physical symptoms of tolerance and withdrawal are an expected outcome of long‐term opioid therapy (Hojsted et al., 2010; Koch & Hollt, 2008; O'Brien, Volkow, & Li, 2006; Portenoy, 1990) and since items addressing this issue are unique to AUDADIS‐IV based criteria, we simulated omission of these physical‐based criteria and calculated rates of problematic use with and without them. Following this criteria alternation we repeated the evaluations of agreement using kappa statistic between the three questionnaires and the altered AUDADIS‐IV based diagnostic criteria.
Inter‐population sources of variance. Several risk factors for problematic use of prescription opioids have been previously described, including socio‐demographic factors, pain and drug‐related factors, anxiety, depression, chronic pain, and alcohol and substance use disorders (Liebschutz et al., 2010; Pergolizzi et al., 2012; Pohl and Smith, 2012). In order to explore inter‐population based sources of variance, we compared rates of problematic use according to each questionnaire across different socio‐demographic, clinical and medical characteristics using chi‐square tests and logistic regression analyses.
Items‐based sources of variance. The different questionnaires contain content‐based congruent questions which differ from one another in their architectural properties, including wording and scoring. In order to evaluate the contribution of inter‐item architectural differences to the variance in rates of problematic opioid use according to the different questionnaires, we initially assessed agreement between questions from different questionnaires based on content similarities using intra‐class correlation coefficient (ICC) analyses, in order to confirm their congruency. Next, we conducted a series of chi‐square tests for categorical variables in order to analyze differences in positive response rates to congruent items from different questionnaires. In order to compare COMM scaled items to PC and AUDADIS‐IV dichotomous items, we considered responses other than “never” (including rarely, sometimes, often and very often) to COMM items as positive (i.e. comparable to “yes” in the other questionnaires). This method allowed us to compare content‐based congruent items from all three questionnaires using categorical tests. For example, we compared rates of positive replies in response to the PC item “an overwhelming concern about the drug's continued availability”, and its content‐based congruent AUDADIS‐IV item “have periods when you spend a lot of time making sure you always had enough of a medicine or drug available?”
Data analyses were performed in the SPSS version 20.0 software (SPSS Inc., Chicago, IL, 2011).
3. RESULTS
3.1. Discordance in diagnoses between questionnaires
According to AUDADIS‐IV criteria 52.6% of prescription opioid users qualified for problematic opioid use, compared to 28.7% and 17.1% when using the COMM and PC, respectively. Among prescription opioid users, 21.1% qualified for problematic opioid use according to two out of the three questionnaires, and 8% qualified for problematic use according to all three questionnaires (Figure 1).
Figure 1.
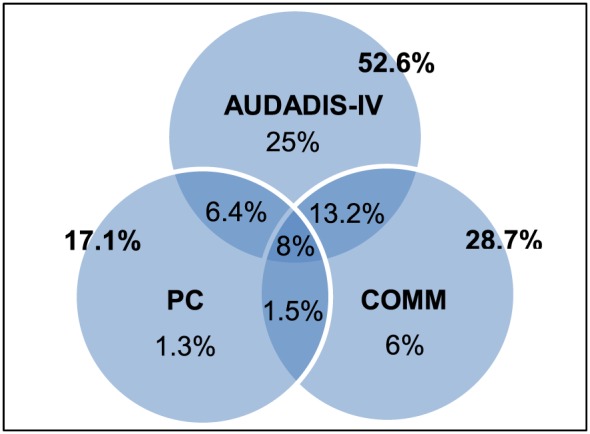
Prevalence of problematic use of prescription opioids among individuals suffering from chronic pain, as diagnosed according to: the Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (AUDADIS‐IV), Current Opioid Misuse Measure (COMM), and Portenoy's Criteria (PC)
3.2. Sources of variance between questionnaires
3.2.1. Architectural sources of inter‐instrument discordance
All questionnaires showed a fair agreement level as assessed by Kappa's measure of agreement. The best agreement was between PC and COMM (κ = 0.253, p < 0.0001), followed by AUDADIS‐IV and COMM (κ = 0.240, p < 0.0001), and PC and AUDADIS‐IV (κ = 0.207, p < 0.0001).
3.2.2. Simulated changes in diagnostic criteria
Excluding physical symptoms of tolerance and withdrawal from AUDADIS‐IV criteria did not substantially alter the prevalence of problematic opioid use according to this questionnaire. The exclusion of these questions reduced rates of diagnoses according to AUDADIS‐IV from 52.6% to 47.7%; the rate of participants diagnosed exclusively according to AUDADIS‐IV declined to 22.1%, and the overlap with COMM and PC in shared diagnoses rates decreased to 12.3% and 5.3%, respectively. The rate of participants qualifying for problematic opioid use according to all three questionnaires remained 8%.
The level of agreement between AUDADIS‐IV criteria and the altered AUDADIS‐IV criteria was excellent (κ = 0.873, p < 0.0001). The level of agreement between the altered AUDADIS‐IV and both COMM and PC remained fair and did not change substantially following the simulated changes earlier (κ = 0.271, p < 0.0001 and κ = 0.211, p < 0.0001, respectively).
3.2.3. Sources of inter‐population variance
We found several factors which increased the odds of problematic opioid use according to the different questionnaires. These included: current anxiety or depression, a history of depression and a history of alcohol use disorders (Table 1). Among participants diagnosed with current depression 69.1%, 45.7% and 25.3% were diagnosed with problematic opioid use according to AUDADIS‐IV, COMM and PC, respectively; similar rates of problematic use between AUDADIS‐IV, COMM and PC was found among those diagnosed with current anxiety (71.5%, 50% and 27.3%, respectively) and among those who reported a history of depression (67.4%, 52.6% and 33.3%, respectively). Other socio‐demographic, clinical or medical variables did not contribute significantly to the odds of problematic opioid use.
Table 1.
Odds ratio of receiving a diagnosis of problematic use of prescription opioids as diagnosed using three diagnostic criteria (The Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition [AUDADIS‐IV], Current Opioid Misuse Measure [COMM], and Portenoy's Criteria [PC]), according to socio‐demographic and clinical variables
| Pain patients using opioid prescription drugs (N = 551) | ||||||
|---|---|---|---|---|---|---|
| Problematic use of opioids | AUDADIS‐IV | PC | COMM | |||
| Odds ratio (95% CI) | Sig. | Odds ratio (95% CI) | Sig. | Odds ratio (95% CI) | Sig. | |
| Gender | ||||||
| Female | 1 | 1 | 1 | |||
| Male | .998 (.711–1.400) | .989 | 1.481 (.940–2.333) | .091 | 1.371 (.941–1.997) | .101 |
| Employment status | ||||||
| Currently not working | 1 | 1 | 1 | |||
| Currently working | .667 (.471–.944) | .022 | .650 (.402–1.052) | .080 | .679 (.458–1.006) | .054 |
| Current depressiona | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 3.053 (1.988–4.688) | .000 | 2.709 (1.402–5.235) | .003 | 5.292 (2.897–9.668) | .000 |
| Current anxietyb | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 2.501 (1.624–3.851) | .000 | 2.464 (1.363–4.456 | .003 | 4.013 (2.402–6.703) | .000 |
| DSM‐IV | ||||||
| No | 1 | 1 | ||||
| Yes | 4.790 (2.638–8.699) | .000 | 2.901 (1.899–4.433) | .000 | ||
| PC | ||||||
| No | 1 | 1 | ||||
| Yes | 4.790 (2.638–8.699) | .000 | 2.951 (1.823–4.777) | .000 | ||
| COMM | ||||||
| No | 1 | 1 | ||||
| Yes | 2.901 (1.899–4.433) | .000 | 2.951 (1.823–4.777) | .000 | ||
| Substance use disorderc | ||||||
| Alcohol | 3.288 (1.061–10.193) | .039 | 10.016 (3.613–27.764) | .000 | 9.870 (3.175–30.680) | .000 |
| Drugs | 1.878 (.564–6.252) | .304 | .439 (.093–2.070) | .298 | 1.637 (.506–5.296) | .411 |
| Medical condition | ||||||
| Hypertension | 1.052 (.698–1.585) | .810 | 1.500 (.847–2.656) | .164 | 1.682 (1.035–2.732) | .036 |
| Liver disease | 1.057 (.416–2.690) | .907 | .754 (.253–2.250) | .613 | 1.067 (.385–2.956) | .901 |
| Heart disease | 1.062 (.602–1.872) | .835 | 1.528 (.661–3.531) | .321 | 1.240 (.627–2.454) | .537 |
| Duodenal ulcer | .876 (.537–1.428) | .595 | .649 (.354–1.187) | .160 | .880 (.512–1.514) | .645 |
| Migraine | .622 (.410–.944) | .026 | 1.083 (.638–1.837) | .769 | .919 (.582–1.451) | .716 |
| Herniated disc | .797 (.551–1.153) | .228 | .972 (.591–1.597) | .910 | .812 (.529–1.246) | .340 |
| Arthritis | .751 (.494–1.144) | .182 | .694 (.406–1.185) | .181 | .752 (.471–1.203) | .235 |
| Fibromyalgia | .892 (.547–1.455) | .647 | 1.087 (.595–1.986) | .786 | .512 (.309–.847) | .009 |
| Depression | .468 (.302–.727) | .001 | .247 (.147–.413) | .000 | .266 (.170–.417) | .000 |
Current depression as measured by the Prime MD PHQ (PHQ‐9) questionnaire.
Current anxiety as measured by the Generalized Anxiety Disorder scale (GAD‐7) questionnaire.
“Substance use disorder” is a self‐report of life‐time history of alcohol or drug use disorders.
3.2.4. Items‐based sources of variance
Six of 22 AUDADIS‐IV items (27%) are shared with PC; six of 17 COMM items (35%) are shared with PC; four of 22 AUDADIS‐IV items (18%) are shared with COMM; two items are shared among all three questionnaires.
Congruent questions shared by all three questionnaires explore two important domains of problematic opioid use: worrying about drug availability and dose escalation. Congruent questions shared by PC and AUDADIS‐IV explore the following three domains of prescription drug problematic use: desire for the drug, continued use despite significant side effects, and arrests because of drug use. Congruent questions shared by PC and COMM explore the following three domains of problematic opioid use: use of drugs for the treatment of symptoms other than prescribed, manipulation of the medical system in order to obtain drugs, and obtaining drugs from unauthorized sources. Congruent questions within AUDADIS‐IV and COMM explore the following two domains of problematic opioid use: problems in important life domains and responsibilities, and having arguments with other people. Table 2 presents correlations between congruent questions among the different questionnaires.
Table 2.
Intra‐class correlation coefficient (ICC) assessment of agreement between content‐based congruent questions among different questionnaires (the Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition [AUDADIS‐IV], Current Opioid Misuse Measure [COMM], and Portenoy's Criteria [PC])
| Pain patients using opioid prescription drugs (N = 551) | |||
|---|---|---|---|
| PC item (number) | COMM item (number) | ICC (2,2) average measure | Sig. |
| Overwhelming concern about the drug's continued availability (2) | In the past 30 days, how much of your time was spent thinking about opioid medications (having enough, taking them, dosing schedule, etc.)? (6) | .223 | .002 |
| Unsanctioned dose escalation (3a) | In the past 30 days, how often have you had to take more of your medication than prescribed? (14) | .477 | .000 |
| Use of drugs to treat symptoms not targeted by therapy (3c) | In the past 30 days, how often have you used your pain medicine for symptoms other than for pain (e.g. to help you sleep, improve your mood, or relieve stress)? (16) | .362 | .000 |
| Manipulation of the treating physician or medical system for the purpose of obtaining additional drug (4a) | In the past 30 days, how often have you had to go to someone other than your prescribing physician to get sufficient pain relief from medications? (i.e. another doctor, the Emergency Room, friends, street sources) (3) | .246 | .000 |
| Acquisition of drugs from other medical sources or from non‐medical sources (4b) | In the past 30 days, how often have you needed to take pain medications belonging to someone else? (9) | .107 | .092 |
| Acquisition of drugs from other medical sources or from non‐medical sources (4b) | In the past 30 days, how often have you borrowed pain medication from someone else? (15) | .110 | .086 |
| AUDADIS‐IV item (number) | COMM item (number) | ICC (2,2) average measure | Sig. |
| Have a period when you spent a lot of time making sure you always had enough of a medicine or drug available? (13) | In the past 30 days, how much of your time was spent thinking about opioid medications (having enough, taking them, dosing schedule, etc.)? (6) | .146 | .000 |
| Often use a medicine or drug in larger amounts or for a much longer period than you meant to? (11) | In the past 30 days, how often have you had to take more of your medication than prescribed? (14) | .337 | .000 |
| Have job or school troubles as a result of your medicine or drug use – like missing too much work, not doing your work well, being demoted or losing a job, or being suspended, expelled or dropping out of school? (4) | In the past 30 days, how often do people complain that you are not completing necessary tasks? (i.e. doing things that need to be done, such as going to class, work or appointments) (2) | .046 | .298 |
| Have a period when your medicine or drug use or your being sick from your medicine or drug use often interfered with taking care of your home or family? (5) | In the past 30 days, how often do people complain that you are not completing necessary tasks? (i.e. doing things that need to be done, such as going to class, work or appointments) (2) | .156 | .027 |
| Have arguments with your spouse, boyfriend/girlfriend, family, or friends as a result of your medicine or drug use?(1) | In the past 30 days, how often have you been in an argument? (7) | .307 | .000 |
| AUDADIS‐IV item (number) | PC item (number) | ICC (2,2) average measure | Sig. |
| Felt a desire to use more drugs during the day (17) | An intense desire for the drug (1) | .374 | .000 |
| Have a period when you spent a lot of time making sure you always had enough of a medicine or drug available (13) | overwhelming concern about the drug's continued availability (2) | .510 | .000 |
| Often use a medicine or drug in larger amounts or for a much longer period than you meant to (11) | Unsanctioned dose escalation (3a) | .540 | .000 |
| Continue to use a medicine or drug even though it was making you feel depressed, uninterested in things, or suspicious or distrustful of other people (16a) | Continued dosing despite significant side effects (3b) | .355 | .000 |
| Continue to use a medicine or drug even though you knew it was causing you a health problem or making a health problem worse (16b) | Continued dosing despite significant side effects (3b) | .514 | .000 |
| Get arrested, get held at a police station or have any other legal problems because of your medicine or drug use (9) | Drug‐related arrests (4c) | .638 | .000 |
The majority of pairs of content‐based congruent questions from different questionnaires rated high in agreement, as assessed using ICC, indicating similarities in participants' overall responses to them. However, participants responded inconsistently to specific congruent questions (Table 3). For example, AUDADIS‐IV item “Often use a medicine or drug in larger amounts or for a much longer period than you meant to” had a fair agreement with COMM item “In the past 30 days, how often have you had to take more of your medication than prescribed?” (ICC (2,2) = 0.337, p < 0.0001). However, the positive response (i.e. responses other than “never”) rates significantly differed (χ 2(4,551) = 41.814, p < 0.0001) (examples provided in Figures 2 and 3).
Table 3.
Differences in response rates to content‐based congruent questions from three diagnostic criteria (The Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition [AUDADIS‐IV], Current Opioid Misuse Measure [COMM], and Portenoy's Criteria [PC])
| PC item (number) | N | Percent | COMM item (number) | N | Percent | Sig. |
|---|---|---|---|---|---|---|
| overwhelming concern about the drug's continued availability (2) | In the past 30 days, how much of your time was spent thinking about opioid medications (having enough, taking them, dosing schedule, etc.)? (6) | |||||
| No | 275 | 49.9 | Never | 455 | 82.6 | |
| Yes | 276 | 50.1 | Rarely | 47 | 8.5 | |
| Sometimes | 22 | 4 | ||||
| Often | 5 | 0.9 | ||||
| Very Often | 22 | 4 | .008 | |||
| Unsanctioned dose escalation (3a) | In the past 30 days, how often have you had to take more of your medication than prescribed? (14) | |||||
| No | 438 | 79.5 | Never | 479 | 86.9 | |
| Yes | 113 | 20.5 | Rarely | 22 | 4 | |
| Sometimes | 28 | 5.1 | ||||
| Often | 7 | 1.3 | ||||
| Very Often | 15 | 2.7 | .000 | |||
| Use of drugs to treat symptoms not targeted by therapy (3c) | In the past 30 days, how often have you used your pain medicine for symptoms other than for pain (e.g. to help you sleep, improve your mood, or relieve stress)? (16) | |||||
| No | 460 | 83.5 | Never | 487 | 88.4 | |
| Yes | 91 | 16.5 | Rarely | 27 | 4.9 | |
| Sometimes | 12 | 2.2 | ||||
| Often | 6 | 1.1 | ||||
| Very Often | 19 | 3.4 | .000 | |||
| Manipulation of the treating physician or medical system for the purpose of obtaining additional drug (4a) | In the past 30 days, how often have you had to go to someone other than your prescribing physician to get sufficient pain relief from medications? (i.e. another doctor, the Emergency Room, friends, street sources) (3) | |||||
| No | 516 | 93.6 | Never | 500 | 90.7 | |
| Yes | 35 | 6.4 | Rarely | 21 | 3.8 | |
| Sometimes | 14 | 2.5 | ||||
| Often | 8 | 1.5 | ||||
| Very Often | 8 | 1.5 | .000 | |||
| Manipulation of the treating physician or medical system for the purpose of obtaining additional drug (4a) | In the past 30 days, how often have you had to visit the Emergency Room? (17) | |||||
| No | 516 | 93.6 | Never | 497 | 90.2 | |
| Yes | 35 | 6.4 | Rarely | 37 | 6.7 | |
| Sometimes | 9 | 1.6 | ||||
| Often | 5 | 0.9 | ||||
| Very Often | 3 | 0.5 | .007 | |||
| Acquisition of drugs from other medical sources or from non‐medical sources (4b) | In the past 30 days, how often have you needed to take pain medications belonging to someone else? (9) | |||||
| No | 539 | 97.8 | Never | 524 | 95.1 | |
| Yes | 12 | 2.2 | Rarely | 10 | 1.8 | |
| Sometimes | 5 | 0.9 | ||||
| Often | 4 | 0.7 | ||||
| Very Often | 8 | 1.5 | .005 | |||
| Acquisition of drugs from other medical sources or from non‐medical sources (4b) | In the past 30 days, how often have you borrowed pain medication from someone else? (15) | |||||
| No | 539 | 97.8 | Never | 530 | 96.2 | |
| Yes | 12 | 2.2 | Rarely | 7 | 1.3 | |
| Sometimes | 5 | 0.9 | ||||
| Often | 6 | 1.1 | ||||
| Very Often | 3 | 0.5 | .008 | |||
| AUDADIS‐IV item (number) | N | Percent | COMM item (number) | N | Percent | Sig. |
| Have a period when you spent a lot of time making sure you always had enough of a medicine or drug available? (13) | In the past 30 days, how much of your time was spent thinking about opioid medications (having enough, taking them, dosing schedule, etc.)? (6) | |||||
| No | 393 | 71.3 | Never | 455 | 82.6 | |
| Yes | 158 | 28.7 | Rarely | 47 | 8.5 | |
| Sometimes | 22 | 4 | ||||
| Often | 5 | 0.9 | ||||
| Very Often | 22 | 4 | .000 | |||
| Often use a medicine or drug in larger amounts or for a much longer period than you meant to? (11) | In the past 30 days, how often have you had to take more of your medication than prescribed? (14) | |||||
| No | 433 | 78.6 | Never | 479 | 86.9 | |
| Yes | 118 | 21.4 | Rarely | 22 | 4 | |
| Sometimes | 28 | 5.1 | ||||
| Often | 7 | 1.3 | ||||
| Very Often | 15 | 2.7 | .000 | |||
| Have job or school troubles as a result of your medicine or drug use – like missing too much work, not doing your work well, being demoted or losing a job, or being suspended, expelled or dropping out of school? (4) | In the past 30 days, how often do people complain that you are not completing necessary tasks? (i.e. doing things that need to be done, such as going to class, work or appointments) (2) | |||||
| No | 424 | 82.5 | Never | 367 | 71.4 | |
| Yes | 90 | 17.5 | Rarely | 34 | 6.6 | |
| Sometimes | 48 | 9.3 | ||||
| Often | 23 | 4.5 | ||||
| Very Often | 42 | 8.2 | .452 | |||
| Have a period when your medicine or drug use or your being sick from your medicine or drug use often interfered with taking care of your home or family? (5) | In the past 30 days, how often do people complain that you are not completing necessary tasks? (i.e. doing things that need to be done, such as going to class, work or appointments) (2) | |||||
| No | 210 | 40.5 | Never | 370 | 71.4 | |
| Yes | 308 | 59.5 | Rarely | 34 | 6.6 | |
| Sometimes | 48 | 9.3 | ||||
| Often | 23 | 4.4 | ||||
| Very Often | 43 | 8.3 | .020 | |||
| Have arguments with your spouse, boyfriend/girlfriend, family, or friends as a result of your medicine or drug use? (1) | In the past 30 days, how often have you been in an argument? (7) | |||||
| No | 448 | 86.5 | Never | 375 | 72.4 | |
| Yes | 70 | 13.5 | Rarely | 60 | 11.6 | |
| Sometimes | 40 | 7.7 | ||||
| Often | 15 | 2.9 | ||||
| Very Often | 28 | 5.4 | .000 | |||
| More than once want to stop or cut down on using any of these medicines or drugs? (10a) | In the past 30 days, how often have you been worried about how you're handling your medications? (10) | |||||
| No | 145 | 26.3 | Never | 459 | 83.3 | |
| Yes | 406 | 73.7 | Rarely | 31 | 5.6 | |
| Sometimes | 27 | 4.9 | ||||
| Often | 15 | 2.7 | ||||
| Very Often | 19 | 3.4 | .962 | |||
| PC item (number) | N | Percent | AUDADIS‐IV item (number) | N | Percent | Sig. |
| An intense desire for the drug (1) | A desire to use more drugs during the day (17) | |||||
| No | 325 | 59 | No | 469 | 85.1 | |
| Yes | 226 | 41 | Yes | 82 | 14.9 | .000 |
| Overwhelming concern about the drug's continued availability (2) | Have a period when you spent a lot of time making sure you always had enough of a medicine or drug available? (13) | |||||
| No | 275 | 49.9 | No | 393 | 71.3 | |
| Yes | 276 | 50.1 | Yes | 158 | 28.7 | .000 |
| Unsanctioned dose escalation (3a) | Often use a medicine or drug in larger amounts or for a much longer period than you meant to (11) | |||||
| No | 438 | 79.5 | No | 433 | 78.6 | |
| Yes | 113 | 20.5 | Yes | 118 | 21.4 | .000 |
| Continued dosing despite significant side effects (3b) | Continue to use a medicine or drug even though it was making you feel depressed, uninterested in things, or suspicious or distrustful of other people (16a) | |||||
| No | 478 | 86.8 | No | 425 | 77.1 | |
| Yes | 73 | 13.2 | Yes | 126 | 22.9 | .000 |
| Continued dosing despite significant side effects (3b) | Continue to use a medicine or drug even though you knew it was causing you a health problem or making a health problem worse (16b) | |||||
| No | 478 | 86.8 | No | 409 | 74.2 | |
| Yes | 73 | 13.2 | Yes | 142 | 25.8 | .000 |
| Drug hoarding or sales (4c) | Get arrested, get held at a police station or have any other legal problems because of your medicine or drug use (9) | |||||
| No Yes | 512 7 | 98.7 1.3 | No Yes | 505 14 | 97.3 2.7 | .000 |
Figure 2.
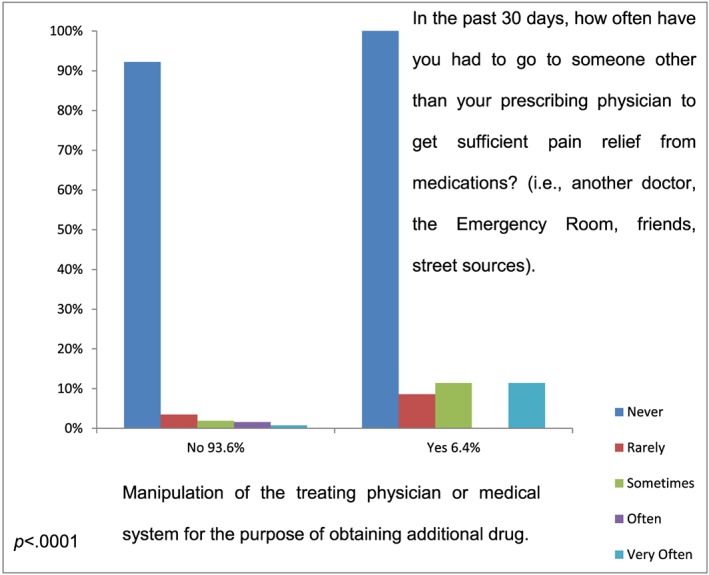
Differences in response rates to content‐based congruent questions from Portenoy's Criteria (PC; X axis) and the Current Opioid Misuse Measure (COMM; represented in bars), which refer to manipulation of the medical system in order to obtain opioids
Figure 3.
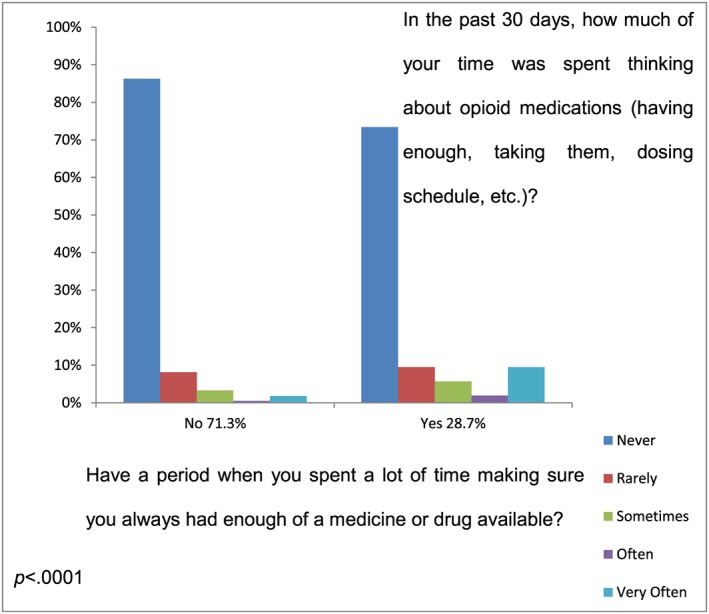
Differences in response rates to content‐based congruent questions from the Alcohol Use Disorder and Associated Disabilities Interview Schedule – Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (AUDADIS‐IV; X axis) and the Current Opioid Misuse Measure (COMM; represented in bars), which refer to worrying about drug availability
4. DISCUSSION
In this study we explored the sources of variance that contribute to discordant rates of problematic use of prescription opioids among chronic pain patients using different questionnaires. We found that prevalence rates varied substantially based on the three questionnaires used. However, each of these questionnaires overlapped partially with others; 53%, 79%, and 93% of the participants who were identified with problematic opioid use according to AUDADIS‐IV, COMM and PC, respectively, were also identified as such by an additional questionnaire. Only 8% of our sample was identified with problematic opioid use according to all three questionnaires. Simulating elimination of criteria regarding physical symptoms of tolerance and withdrawal from AUDADIS‐IV based questionnaire did not substantially alter these results or the level of agreement between the modified AUDADIS‐IV and both COMM and PC. An examination of potential sources of variance indicated that questions' architecture (including wording and scoring), and some inter‐population differences, contribute greatly to differences in diagnoses rates between questionnaires.
Utilization of different assessment tools commonly yields variance in results. For example, discordance in diagnoses rates between different questionnaires was found in alcohol use disorders (Mewton, Slade, McBride, Grove, & Teesson, 2011), tobacco dependence (Mwenifumbo & Tyndale, 2010) and other psychiatric disorders such as depression (Maske et al., 2016) and eating disorders (Segura‐Garcia et al., 2015). In the context of problematic opioid use, discordance in diagnoses rates using different questionnaires was found in several previous studies. Hojsted et al. (2010) compared diagnoses rates of opioid dependence among chronic pain patients using ICD‐10 criteria as opposed to PC. Diagnoses rates according to PC (19.3%) were similar to those found in our study (17.1%) and were higher than those found according to ICD‐10 (14.4%). The authors concluded that PC seems appropriate for diagnosing addiction in opioid treated pain patients, and seems to be more sensitive and specific than ICD‐10 for this purpose (Hojsted et al., 2010). It is possible that its sensitivity and specificity lead to similarities in diagnoses rates across different samples. Discordance in diagnoses rates was also demonstrated in a longitudinal two‐year prospective cohort study conducted by Degenhardt et al. (2015). In their study the application of DSM‐5 criteria produced much higher estimates of prescription opioid use disorders (20.8%), compared with DSM‐IV (8.9%), ICD‐10 (8.5%) and ICD‐11 (9.9%), which all produced similar prevalence rates of dependence. Though we would expect that rates of opioid use disorder would be substantially greater than those of DSM‐IV dependence (since DSM‐5 “use disorder” includes DSM‐IV abuse and dependence combined), this was not the case. Moreover, the other questionnaires used produce substantially lower prevalence rates of opioid use disorders compared to our study. These differences in results may be explained by differences in study design; while our sample was assessed directly using three questionnaires, Degenhardt et al. (2015) used an indirect diagnosing approach whereby data regarding opioid use was collected from their sample using the Composite International Diagnostic Interview, and then patients were categorized as having opioid use disorders by each set of diagnostic criteria.
It should be acknowledged that these three questionnaires measure different, though partially overlapping, phenomena. The AUDADIS‐IV is a diagnostic checklist which includes both physical and behavioral features of addiction (APA, 1994; Zacny et al., 2003), but not specifically intended for this patient population; PC is a set of criteria for diagnosing addiction in the context of patients taking opioids for chronic pain (Portenoy, 1990), and COMM measures aberrant drug‐related behaviors in patients during opioid treatment using social, emotional, and functional features (Butler et al., 2007). Hence, these are not fully overlapping concepts. Furthermore, it is important to take into consideration that respondents interpret questions in the context of the overall questionnaire, and they assume that adjacent questions are meaningfully related to one another (Schwarz, 2015). Thus, in the context of different questionnaires, it is possible that even individual questions which measure similar constructs may receive different rates of positive responses. This, in addition to specific differences in time‐frames, wording of questions and response alternatives, may have a substantial contribution to the variance in positive replies to specific questions and overall rates of problematic opioid use as seen in the different questionnaires.
Accordingly, in this study we addressed “problematic use” as the common theme underlying these different constructs. Results indicate that even when overlapping and similar constructs are measured, the attempt to measure them using different questionnaires yields different responses based on the specific questionnaires used and questions' construction (e.g. wording, time‐frame, etc.). Further analysis of possible sources of discordance between positive rates of problematic use according to the three questionnaires revealed that some inter‐population characteristics, such as differences in rates of depression, anxiety and alcohol dependence, additionally contribute to the odds of problematic opioid use. Moreover, rates of problematic opioid use were greater among those suffering from any of these three disorders. This finding is expected given that previous studies demonstrated that individuals suffering from depression (Hojsted et al., 2010; Maremmani et al., 2007) and anxiety (Martins, Keyes, Storr, Zhu, Chilcoat, 2009; Wilsey et al., 2008) are at increased risk of substance abuse, including opioid misuse. A strong association was also established between problematic opioid use and prior alcohol abuse (Ives et al., 2006; Liebschutz et al., 2010; Turk, Swanson, & Gatchel, 2008). Nevertheless, given the relatively stable proportions between diagnostic rates according to the different questionnaires among these sub‐populations, it seems the contribution of these inter‐population variables to the general variance between questionnaires is limited.
In efforts to detect and refine the sources of variance between prevalence of problematic opioid use according to the different questionnaires, we simulated exclusion of physical symptoms criteria, which did not substantially alter results. Both tolerance and withdrawal physical symptoms are common among chronic pain patients treated with opioids (Hojsted et al., 2010; Portenoy, 1996), yet these symptoms are neither crucial nor necessary for diagnosing problematic opioid use. Approximately 90% of the participants who were initially identified with problematic opioid use according to AUDADIS‐IV based criteria continued to meet diagnostic criteria after eliminating criteria regarding physical symptoms. This finding is in line with Savage et al. (2003) who propose the fundamental concept that addiction is distinct from physical dependence and tolerance, and suggest that in the context of prescription opioid treatment for chronic pain, problematic use should be viewed primarily using psychological and behavioral symptoms (Portenoy, 1990). Accordingly, it seems the focus of attention when monitoring chronic pain patients undergoing opioid treatment should be shifted to the psychological and behavioral components of problematic use.
Ultimately, our results demonstrated that the construction of questions in the various assessment tools contributed substantially to variance between questionnaires. This is in line with findings indicating that in self‐administered questionnaires the veracity of respondents' replies is influenced by characteristics of the questions, including wording, format of the response alternatives, and the context in which they are presented (Del Boca & Noll, 2000; Schwarz, 1999, 2015). In our study, the following architectural components may have contributed to the variance in response rates to content‐based congruent questions from different questionnaires.
Time‐frame differences refer to the contribution of the time‐frame referred to by questionnaire to the variance in response rates to content‐based congruent questions. While AUDADIS‐IV based criteria refer to the past 12 months (Grant et al., 2001), COMM criteria refer to the past 30 days (Butler et al., 2007) and PC refer to the past in general (Portenoy, 1990). Naturally, when questions refer to longer time periods there is a greater chance of criterion positive reply. Accordingly, in PC and AUDADIS‐IV questionnaires the respondent is more likely to reply positively (as they reflect longer periods of time) compared to the COMM. For example, among those who replied “yes” to PC item “Manipulation of the treating physician or medical system for the purpose of obtaining additional drug” there was a majority who replied “never” to COMM item “In the past 30 days, how often have you had to go to someone other than your prescribing physician to get sufficient pain relief from medications? (i.e. another doctor, the Emergency Room, friends, street sources)”. It is possible that current (past 30 days) behaviors are different than behaviors in the distant past, and thereby similar content‐based questions yield different rates of positive answers.
It is reasonable to assume that time‐based differences (lifetime/12 months/30 days) may have a central contribution to discordant rates, as one would expect that the percentage of positive replies to content‐based congruent questions with a 30‐day time‐frame would be lower than that with a 12‐month time‐frame, which would in turn be lower than those questionnaires with a lifetime time‐frame. However, our results imply that this is not always the case and that additional factors, including wording, response alternatives and the construct of the specific tool is intended to measure, are important as well. For example, in response to COMM item “In the past 30 days, how often have you been in an argument?” (30 days interval), nearly 28% of our sample provided positive responses ranging from rarely to very often, whereas only 13.5% replied positively to the congruent AUDADIS‐IV item “Have arguments with your spouse, boyfriend/girlfriend, family, or friends as a result of your medicine or drug use?” (12 months interval). Hence, the time interval defined by these questionnaires cannot serve as a sufficient explanatory of the differences in positive reply rates. Instead, these discordant rates could be better explained by differences in wording of items, their specificity and format of answer alternatives, as further discussed later.
It seems that Specificity differences, meaning the extent to which the question is detailed and includes examples aimed to clarify the question's intent, may have also contributed to the inconsistency in subjects' replies. Prima facie, COMM seems to be relatively specific, as five out of its 17 items include clarifying examples, whereas only one AUDADIS‐IV item and none of PC items include examples. However, in other cases AUDADIS‐IV items are more specific than the congruent COMM items. For example, the following AUDADIS‐IV item: “Had periods when you spent a lot of time making sure you always had enough of a medicine or drug available?” may be compared to the congruent PC item “overwhelming concern about the drug's continued availability” and COMM item: “In the past 30 days, how much of your time was spent thinking about opioid medications (having enough, taking them, dosing schedule, etc.)?” The latter provides a larger variety of possible situations which apply to this item, and therefore a respondent who replied negatively to AUDADIS‐IV item may respond otherwise to the congruent COMM item. In this manner, the inclusion of examples and details in the question can contribute to an increase or decrease in positive replies to specific questions.
An additional source of variance in positive response rates to an item is due to Wording differences, the contribution of the wording or presence of words which may be perceived in a less favorable fashion, and as a result to bias responses (Del Boca & Noll, 2000; Schwarz, 1999). For example, PC item “Manipulation of the treating physician or medical system for the purpose of obtaining additional drug”, received substantially lower rates of positive replies from participants identified with problematic opioid use compared to positive replies (any reply other than “never”) in response to the congruent COMM item “In the past 30 days, how often have you had to go to someone other than your prescribing physician to get sufficient pain relief from medications? (i.e. another doctor, the Emergency Room, friends, street sources)”. These differences in positive response rates may be partly due to social desirability, which is the tendency on the part of the respondents to present themselves in a favorable light, regardless of their true feelings or behaviors (Crowne & Marlowe, 1964), by distorting their self‐reports as a function of the perceived acceptability of the behavior in question (Edwards, 1957; Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Accordingly, it is possible that the word “manipulation” in PC item is perceived as negatively charged for some, and therefore received relatively less positive responses. In contrast, the phrase “had to” in the congruent COMM item may imply to a reduced responsibility and therefore perceived as more favorable, and as a result received more positive replies.
The three questionnaires also differ significantly in their format of possible answers. PC and AUDADIS‐IV items have two possible replies – yes/no, while answers to items included in the COMM are graded in a Likert scale of zero to four. Our findings suggest that a “no” response (to PC or AUDADIS‐IV) was not necessarily comparable to a “never” response (COMM), and that when interacting with the question's wording and especially with the time‐frame of the question, the number and format of possible answers to specific items may contribute to differences in response patterns to content‐based congruent questions in the three questionnaires. Ultimately, differences in scoring and in the time‐frame the item refers to may affect the ability of the respondent to recall specific information in a specific time‐frame (Del Boca & Noll, 2000).
Though the earlier construct‐based differences were found to contribute greatly to the discordance in positive rates of problematic opioid use according to the different questionnaires, our study design did not allow us to measure their relative contribution to the variance or their interaction with each other. Therefore, we were unable to determine which individual construction feature has a greater contribution to the discordance in results. A few limitations of the study are notable. It is important to mention the relatively low response rate in the current study (57%), which is lower than the expected response rate in the field of addiction and not reaching the recommended rate of 70% (Bowling, 1997). However, this relatively low response rate may be due to the tendency of a patients to provide incorrect information regarding current non‐medical drug use (Berndt, Maier, & Schutz, 1993; Del Boca & Noll, 2000; Fishbain, Cutler, Rosomoff, & Rosomoff 1999), and to avoid sincere replies regarding drug‐related aberrant behaviors when asked about them by their medications and prescriptions providers (Del Boca & Noll, 2000). In addition, data pertaining to problematic opioid use in this study was obtained using a limited number of three specific questionnaires. It should be taken into consideration that other addiction assessment tools are available, such as ICD‐10 (WHO, 1992), ABC (Wu et al., 2006), PDUQ (Compton et al., 1998), etc. Finally, risk factors for prescription opioid misuse among chronic opioid therapy patients are dynamic as a function of disease progression, tolerance, changes in pain quality, mental health, comorbidities, other drug therapies or drug interactions, and changes in patients' lifestyle (Pergolizzi et al., 2012). In our study we examined only some of these risk factors as possible contributors to the variance in diagnoses rates, while others may have some contribution as well. Given the fact that we conducted a cross‐sectional study, we were unable to assess the effect of these factors over time.
Nevertheless, this study presents important findings regarding tools for identifying problematic opioid use among chronic pain patients. The findings of the present study illustrate and stress strengths and limitations of the AUDADIS‐IV, COMM and PC in a population of adults suffering from chronic pain. In addition, our findings highlight the importance of the construction of questions, including the type, wording and scoring, that assemble different questionnaires used for detecting problematic opioid use, and its significance to the variance in different questionnaires' functionality. These are all important for further developing better and more reliable tools for diagnosing problematic opioid use among individuals with chronic pain.
DECLARATION OF INTEREST STATEMENT
SL has received speaking and travelling fees from Reckitt Benkiser Pharmaceuticals.
Kovatch M, Feingold D, Elkana O, Lev‐Ran S. Evaluation and comparison of tools for diagnosing problematic prescription opioid use among chronic pain patients. Int J Methods Psychiatr Res. 2017;26:e1542 10.1002/mpr.1542
REFERENCES
- American Psychiatric Association (APA) (1994). Diagnostic and Statistical Manual of Mental Disorders (Fourth ed.). Washington, DC: APA. [Google Scholar]
- Andrew, R. , Derry, S. , Taylor, R. S. , Straube, S. , & Phillips, C. J. (2014). The costs and consequences of adequately managed chronic non‐cancer pain and chronic neuropathic pain. Pain Practice: The Official Journal of World Institute of Pain, 14(1), 79–94. doi: 10.1111/papr.12050 [DOI] [PubMed] [Google Scholar]
- Ballantyne, J. C. , & Mao, J. (2003). Opioid therapy for chronic pain. The New England Journal of Medicine, 349(20), 1943–1953. doi: 10.1056/NEJMra025411 [DOI] [PubMed] [Google Scholar]
- Berndt, S. , Maier, C. , & Schutz, H. W. (1993). Polymedication and medication compliance in patients with chronic non‐malignant pain. Pain, 52(3), 331–339. [DOI] [PubMed] [Google Scholar]
- Bowling, A. (1997). Data collection methods in quantitative research: questionnaires, interviews and their response rates In Research Methods in Health: Investigating Health and Health Services. (pp. 257–272). Milton Keynes: Open University Press. [Google Scholar]
- Butler, S. F. , Budman, S. H. , Fernandez, K. C. , Houle, B. , Benoit, C. , Katz, N. , & Jamison, R. N. (2007). Development and validation of the Current Opioid Misuse Measure. Pain, 130(1–2), 144–156. doi: 10.1016/j.pain.2007.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (2009). Overdose deaths involving prescription opioids among Medicaid enrollees – Washington, 2004–2007 In Morbidity and Mortality Weekly Reports. (pp. 1171–1175). Atlanta, GA: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Compton, P. , Darakjian, J. , & Miotto, K. (1998). Screening for addiction in patients with chronic pain and “problematic” substance use: Evaluation of a pilot assessment tool. Journal of Pain and Symptom Management, 16(6), 355–363. [DOI] [PubMed] [Google Scholar]
- Crowne, D. P. , & Marlowe, D. (1964). The Approval Motive: Studies in Evaluative Dependence. New York: Wiley. [Google Scholar]
- Degenhardt, L. , Bruno, R. , Lintzeris, N. , Hall, W. , Nielsen, S. , Larance, B. , … Campbell, G. (2015). Agreement between definitions of pharmaceutical opioid use disorders and dependence in people taking opioids for chronic non‐cancer pain (POINT): A cohort study. The Lancet Psychiatry, 2(4), 314–322. doi: 10.1016/S2215-0366(15)00005-X [DOI] [PubMed] [Google Scholar]
- Del Boca, F. K. , & Noll, J. A. (2000). Truth or consequences: The validity of self‐report data in health services research on addictions. Addiction, 95(Suppl 3), S347–S360. [DOI] [PubMed] [Google Scholar]
- Dhalla, I. A. , Persaud, N. , & Juurlink, D. N. (2011). Facing up to the prescription opioid crisis. BMJ, 343, d5142. doi: 10.1136/bmj.d5142 [DOI] [PubMed] [Google Scholar]
- Edwards, A. L. (1957). Social desirability and probability of endorsement of items in the interpersonal check list. Journal of Abnormal Psychology, 55(3), 394–396. [DOI] [PubMed] [Google Scholar]
- Elliott, A. M. , Smith, B. H. , Penny, K. I. , Smith, W. C. , & Chambers, W. A. (1999). The epidemiology of chronic pain in the community. Lancet, 354(9186), 1248–1252. [DOI] [PubMed] [Google Scholar]
- Fischer, B. , & Argento, E. (2012). Prescription opioid related misuse, harms, diversion and interventions in Canada: A review. Pain Physician, 15(3 Suppl), ES191–ES203. [PubMed] [Google Scholar]
- Fishbain, D. A. , Cutler, R. B. , Rosomoff, H. L. , & Rosomoff, R. S. (1999). Validity of self‐reported drug use in chronic pain patients. The Clinical Journal of Pain, 15(3), 184–191. [DOI] [PubMed] [Google Scholar]
- Grady, D. , Berkowitz, S. A. , & Katz, M. H. (2011). Opioids for chronic pain. Archives of Internal Medicine, 171(16), 1426–1427. [DOI] [PubMed] [Google Scholar]
- Grant, B. F. , Harford, T. C. , Dawson, D. A. , Chou, P. S. , & Pickering, R. P. (1995). The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence, 39(1), 37–44. [DOI] [PubMed] [Google Scholar]
- Grant, B. , Dawson, D. , & Hasin, D. (2001). The Alcohol Use Disorders and Associated Disabilities Interview Schedule – Version for DSM‐IV (AUDADIS‐IV). Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Hall, A. J. , Logan, J. E. , Toblin, R. L. , Kaplan, J. A. , Kraner, J. C. , Bixler, D. , … Paulozzi, L. J. (2008). Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA, 300(22), 2613–2620. doi: 10.1001/jama.2008.802 [DOI] [PubMed] [Google Scholar]
- Harrell, A. V. (1997). The Validity of Self‐reported Drug Use Data: The Accuracy of Responses on confidential Self‐administered Answered Sheets,NIDA Research Monograph 167 (pp. 37–58). Bethesda, MD: National Institute on Drug Abuse. [PubMed] [Google Scholar]
- Harrison, L. (1997). The Validity of Self‐reported Drug Use in Survey Research: An Overview and Critique of Research Methods ()NIDA Research Monograph 167 (pp. 17–36). Bethesda, MD: National Institute on Drug Abuse. [PubMed] [Google Scholar]
- Hasin, D. , Carpenter, K. M. , McCloud, S. , Smith, M. , & Grant, B. F. (1997). The alcohol use disorder and associated disabilities interview schedule (AUDADIS): Reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence, 44(2–3), 133–141. [DOI] [PubMed] [Google Scholar]
- Hojsted, J. , & Sjogren, P. (2007). Addiction to opioids in chronic pain patients: A literature review. European Journal of Pain, 11(5), 490–518. doi: 10.1016/j.ejpain.2006.08.004 [DOI] [PubMed] [Google Scholar]
- Hojsted, J. , Nielsen, P. R. , Guldstrand, S. K. , Frich, L. , & Sjogren, P. (2010). Classification and identification of opioid addiction in chronic pain patients. European Journal of Pain, 14(10), 1014–1020. doi: 10.1016/j.ejpain.2010.04.006 [DOI] [PubMed] [Google Scholar]
- International Narcotics Control Board (INCB) (2015). Report of the International Narcotics Control Board for 2014. New York: INCB. [Google Scholar]
- Ives, T. J. , Chelminski, P. R. , Hammett‐Stabler, C. A. , Malone, R. M. , Perhac, J. S. , Potisek, N. M. , … Pignone, M. P. (2006). Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Services Research, 6, 46. doi: 10.1186/1472-6963-6-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison, R. N. , & Mao, J. (2015). Opioid analgesics. Mayo Clinic Proceedings, 90(7), 957–968. doi: 10.1016/j.mayocp.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Koch, T. , & Hollt, V. (2008). Role of receptor internalization in opioid tolerance and dependence. Pharmacology & Therapeutics, 117(2), 199–206. doi: 10.1016/j.pharmthera.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Kuehn, B. M. (2007). Prescription drug abuse rises globally. JAMA, 297(12), 1306. doi: 10.1001/jama.297.12.1306 [DOI] [PubMed] [Google Scholar]
- Liebschutz, J. M. , Saitz, R. , Weiss, R. D. , Averbuch, T. , Schwartz, S. , Meltzer, E. C. , … Samet, J. H. (2010). Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. The Journal of Pain: Official Journal of the American Pain Society, 11(11), 1047–1055. doi: 10.1016/j.jpain.2009.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe, B. , Decker, O. , Müller, S. , Brähler, E. , Schellberg, D. , Herzog, W. , & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD‐7) in the general population. Medical Care, 46(3), 266–274. [DOI] [PubMed] [Google Scholar]
- Manchikanti, K. , Manchikanti, L. , Damron, K. , Pampati, V. , & Fellows, B. (2007). Increasing deaths from opioid analgesics in the United States: An evaluation in an interventional pain management practice. Journal of Opioid Management, 4(5), 271–283. [DOI] [PubMed] [Google Scholar]
- Manchikanti, L. , Fellows, B. , Ailinani, H. , & Pampati, V. (2010). Therapeutic use, abuse, and nonmedical use of opioids: A ten‐year perspective. Pain Physician, 13(5), 401–435. [PubMed] [Google Scholar]
- Maremmani, I. , Pani, P. P. , Canoniero, S. , Pacini, M. , Perugi, G. , Rihmer, Z. , & Akiskal, H. S. (2007). Is the bipolar spectrum the psychopathological substrate of suicidality in heroin addicts? Psychopathology, 40(5), 269–277. doi: 10.1159/000104742 [DOI] [PubMed] [Google Scholar]
- Martins, S. S. , Keyes, K. M. , Storr, C. L. , Zhu, H. , & Chilcoat, H. D. (2009). Pathways between nonmedical opioid use/dependence and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 103(1–2), 16–24. doi: 10.1016/j.drugalcdep.2009.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maske, U. E. , Buttery, A. K. , Beesdo‐Baum, K. , Riedel‐Heller, S. , Hapke, U. , & Busch, M. A. (2016). Prevalence and correlates of DSM‐IV‐TR major depressive disorder, self‐reported diagnosed depression and current depressive symptoms among adults in Germany. Journal of Affective Disorders, 190, 167–177. doi: 10.1016/j.jad.2015.10.006 [DOI] [PubMed] [Google Scholar]
- McNeely, J. , Strauss, S. M. , Saitz, R. , Cleland, C. M. , Palamar, J. J. , Rotrosen, J. , & Gourevitch, M. N. (2015). A brief patient self‐administered substance use screening tool for primary care: two‐site validation study of the Substance Use Brief Screen (SUBS). The American Journal of Medicine, 128(7), 784–789. doi: 10.1016/j.amjmed.2015.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mewton, L. , Slade, T. , McBride, O. , Grove, R. , & Teesson, M. (2011). An evaluation of the proposed DSM‐5 alcohol use disorder criteria using Australian national data. Addiction, 106(5), 941–950. doi: 10.1111/j.1360-0443.2010.03340.x [DOI] [PubMed] [Google Scholar]
- Minozzi, S. , Amato, L. , & Davoli, M. (2013). Development of dependence following treatment with opioid analgesics for pain relief: A systematic review. Addiction, 108(4), 688–698. doi: 10.1111/j.1360-0443.2012.04005.x [DOI] [PubMed] [Google Scholar]
- Mwenifumbo, J. , & Tyndale, R. (2010). DSM‐IV, ICD‐10 and FTND: Discordant tobacco dependence diagnoses in adult smokers. Journal of Addiction Research & Therapy, 1, 105. doi: 10.4172/2155-6105.1000105 [DOI] [Google Scholar]
- O'Brien, C. P. , Volkow, N. , & Li, T. K. (2006). What's in a word? Addiction versus dependence in DSM‐V. The American Journal of Psychiatry, 163(5), 764–765. doi: 10.1176/ajp.2006.163.5.764 [DOI] [PubMed] [Google Scholar]
- Passik, S. D. , Kirsh, K. L. , Whitcomb, L. , Portenoy, R. K. , Katz, N. P. , Kleinman, L. , & Schein, J. R. (2004). A new tool to assess and document pain outcomes in chronic pain patients receiving opioid therapy. Clinical Therapeutics, 26(4), 552–561. [DOI] [PubMed] [Google Scholar]
- Pergolizzi, J. V. Jr. , Gharibo, C. , Passik, S. , Labhsetwar, S. , Taylor, R. Jr. , Pergolizzi, J. S. , & Muller‐Schwefe, G. (2012). Dynamic risk factors in the misuse of opioid analgesics. Journal of Psychosomatic Research, 72(6), 443–451. doi: 10.1016/j.jpsychores.2012.02.009 [DOI] [PubMed] [Google Scholar]
- Podsakoff, P. M. , MacKenzie, S. B. , Lee, J. Y. , & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. The Journal of Applied Psychology, 88(5), 879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- Pohl, M. , & Smith, L. (2011). Chronic pain management using buprenorphine: Questions and considerations. Journal of Global Drug Policy, 5, 1. [Google Scholar]
- Pohl, M. , & Smith, L. (2012). Chronic pain and addiction: Challenging co‐occurring disorders. Journal of Psychoactive Drugs, 44(2), 119–124. doi: 10.1080/02791072.2012.684621 [DOI] [PubMed] [Google Scholar]
- Portenoy, R. K. (1990). Chronic opioid therapy in nonmalignant pain. Journal of Pain and Symptom Management, 5(1 Suppl), S46–S62. [PubMed] [Google Scholar]
- Portenoy, R. K. (1996). Opioid therapy for chronic nonmalignant pain: A review of the critical issues. Journal of Pain and Symptom Management, 11(4), 203–217. [DOI] [PubMed] [Google Scholar]
- Roxburgh, A. , Bruno, R. , Larance, B. , & Burns, L. (2011). Prescription of opioid analgesics and related harms in Australia. The Medical Journal of Australia, 195(5), 280–284. [DOI] [PubMed] [Google Scholar]
- Savage, S. R. , Joranson, D. E. , Covington, E. C. , Schnoll, S. H. , Heit, H. A. , & Gilson, A. M. (2003). Definitions related to the medical use of opioids: Evolution towards universal agreement. Journal of Pain and Symptom Management, 26(1), 655–667. [DOI] [PubMed] [Google Scholar]
- Schwarz, N. (1999). Self‐reports: How the questions shape the answers. American Psychologist, 54(2), 93. [Google Scholar]
- Schwarz, N. (2015). Questionnaires: Cognitive approaches In International Encyclopedia of the Social & Behavioral Sciences (2nd ed.). (pp. 771–775). Amsterdam: Elsevier. [Google Scholar]
- Scott‐Sheldon, L. A. , Carey, K. B. , Carey, M. P. , Cain, D. , Simbayi, L. C. , & Kalichman, S. C. (2014). Alcohol use disorder, contexts of alcohol use, and the risk of HIV transmission among South African male patrons of shebeens. Drug and Alcohol Dependence, 140, 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura‐Garcia, C. , Aloi, M. , Rania, M. , Ciambrone, P. , Palmieri, A. , Pugliese, V. , … De Fazio, P. (2015). Ability of EDI‐2 and EDI‐3 to correctly identify patients and subjects at risk for eating disorders. Eating Behaviors, 19, 20–23. doi: 10.1016/j.eatbeh.2015.06.010 [DOI] [PubMed] [Google Scholar]
- Sehgal, N. , Manchikanti, L. , & Smith, H. S. (2012). Prescription opioid abuse in chronic pain: A review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician, 15(3 Suppl), ES67–ES92. [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , & Williams, J. B. (1999). Validation and utility of a self‐report version of PRIME‐MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA, 282(18), 1737–1744. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Williams, J. B. W. , & Kroenke, K. (2009). Instruction Manual: Instructions for Patient Health Questionnaire (PHQ) and GAD‐7 Measures. Retrieved March 25, 2014, from http://www.phqscreeners.com
- Trescot, A. M. , Helm, S. , Hansen, H. , Benyamin, R. , Glaser, S. E. , Adlaka, R. , … Manchikanti, L. (2008). Opioids in the management of chronic non‐cancer pain: An update of American Society of the Interventional Pain Physicians' (ASIPP) guidelines. Pain Physician, 11(2 Suppl), S5–S62. [PubMed] [Google Scholar]
- Turk, D. C. , Swanson, K. S. , & Gatchel, R. J. (2008). Predicting opioid misuse by chronic pain patients: A systematic review and literature synthesis. The Clinical Journal of Pain, 24(6), 497–508. doi: 10.1097/AJP.0b013e31816b1070 [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) (2014). Report of the Office on Drugs and Crime for 2013. New York: UNODC. [Google Scholar]
- Von Korff, M. , Kolodny, A. , Deyo, R. A. , & Chou, R. (2011). Long‐term opioid therapy reconsidered. Annals of Internal Medicine, 155(5), 325–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsey, B. L. , Fishman, S. M. , Tsodikov, A. , Ogden, C. , Symreng, I. , & Ernst, A. (2008). Psychological comorbidities predicting prescription opioid abuse among patients in chronic pain presenting to the emergency department. Pain Medicine, 9(8), 1107–1117. doi: 10.1111/j.1526-4637.2007.00401.x [DOI] [PubMed] [Google Scholar]
- Wilson, J. F. (2007). Strategies to stop abuse of prescribed opioid drugs. Annals of Internal Medicine, 146(12), 897–900. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) (1992). The ICD‐10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: WHO. [Google Scholar]
- Wu, S. M. , Compton, P. , Bolus, R. , Schieffer, B. , Pham, Q. , Baria, A. , … Naliboff, B. D. (2006). The addiction behaviors checklist: Validation of a new clinician‐based measure of inappropriate opioid use in chronic pain. Journal of Pain and Symptom Management, 32(4), 342–351. doi: 10.1016/j.jpainsymman.2006.05.010 [DOI] [PubMed] [Google Scholar]
- Yudko, E. , Lozhkina, O. , & Fouts, A. (2007). A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment, 32(2), 189–198. doi: 10.1016/j.jsat.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Zacny, J. , Bigelow, G. , Compton, P. , Foley, K. , Iguchi, M. , & Sannerud, C. (2003). College on problems of drug dependence taskforce on prescription opioid non‐medical use and abuse: Position statement. Drug and Alcohol Dependence, 69(3), 215–232. [DOI] [PubMed] [Google Scholar]


