Abstract
Objectives
The CZEch Mental health Study (CZEMS) was launched to inform the ongoing mental health care reform. This paper describes rationale, methods, and the plan for the future analyses of this project.
Methods
A cross‐sectional survey on a representative sample of the general adult noninstitutionalized population of the Czech Republic was conducted. Two‐stage sampling was utilized and respondents were interviewed by centrally trained staff using a paper and pencil interviewing. The presence of mental disorders was assessed by The Mini‐International Neuropsychiatric Interview. The study also collected information about disability, self‐identification of having a mental illness, medical history, and help‐seeking behaviour.
Results
This survey had a 75% response rate, and the final sample consisted of 3,306 persons aged from 18 to 96 years (mean age 49 years old, 54% women) that were interviewed in their homes. The final sample is representative for the Czech Republic in terms of age, gender, education, and region.
Conclusions
CZEMS will provide up‐to‐date evidence about a prevalence of mental disorders in the Czech Republic, associated disability, and treatment gap. This will help informed decision‐making about the current mental health care reform and future mental health care development in the Czech Republic.
Keywords: disability, epidemiology, methodology, public mental health, treatment gap
1. INTRODUCTION
Mental health care has long been neglected in the Czech Republic (Höschl, Winkler, & Pěč, 2012). The Czech government is currently developing a reform that aims to modernize the care of patients affected with mental disorders. One of the main goals is to shift the locus of care from large psychiatric hospitals towards communities where currently existing network of outpatient psychiatrist should be complemented with newly established community mental health centres (Winkler, Mladá, et al., 2016; Pěč, 2018). This is the process known as deinstitutionalization, which has been associated with better outcomes for people with severe mental illness (SMI) but is yet to be pursued in countries from Central and Eastern Europe (CEE; Knapp, Beecham, McDaid, Matosevic, & Smith, 2011; Kunitoh, 2013; Winkler, Barret, et al., 2016; Winkler et al., 2017). In the Czech Republic, this process has only been recently launched, but a lack of reliable epidemiological data is an important obstacle.
The burden of mental disorders differs greatly across Europe. For example, the prevalence of major depressive disorder in adults varies between 2% and 8% in different European countries (Paykel, Brugha, & Fryers, 2005). Similarly, estimates on the occurrence of anxiety disorders reach from 4% in Finland (Pirkola et al., 2005) to 15% in Germany (Jacobi et al., 2004). The variance in the prevalence of common mental disorders (CMD) could not only be explained by methodological differences in individual studies. For example, Pirkola et al. (2005) and Jacobi et al. (2004) had both used the same version of Composite International Diagnostic Interview, conducted their surveys in approximately the same period, and achieved high response rates.
The heterogeneity of prevalence rates of mental disorders was also reflected in the critical appraisals of European epidemiological studies, where substantial differences were found for both CMD and SMI (Wittchen et al., 2011; Wittchen & Jacobi, 2005). Evidence about mental disorders from countries in CEE is largely lacking. In the above‐mentioned review of European epidemiological studies, there were only two conducted in CEE, one of them was an unpublished study from the Czech Republic performed in 2005, and the other one came from Hungary (Wittchen & Jacobi, 2005). No study from CEE was added in the following review 6 years later (Wittchen et al., 2011). A considerable lack of epidemiological studies was also found in a recent review of 25 years of development of mental health care for people with SMI in CEE (Winkler et al., 2017).
It is estimated that CEE is the region with the highest level of disability and mortality rates due to mental disorders (Charlson et al., 2015; Whiteford et al., 2013). A large gap between the number of affected persons and those that receive evidence‐based treatment, down prioritization of their somatic care, and high rates of alcohol abuse and unhealthy life style habits may be the main reasons (Charlson et al., 2015; Whiteford et al., 2013). Furthermore, long hospitalizations in large institutions and practically non‐existent care in the community may hinder successful recovery from mental disorders (Höschl, Winkler, & Pěč, 2012). Last but not least, the level of stigma seems to be high in the region, and this is likely to negatively influence not only mental health policy, funding, and service quality, but also help‐seeking behaviour and early detection of people with mental disorders (Link, Struening, Rahav, Phelan, & Nuttbrock, 1997; Winkler et al., 2017).
The CZEch Mental health Study (CZEMS) has been conducted to support the mental health care reform in the Czech Republic by providing up‐to‐date evidence about mental disorders. The aims of CZEMS are the following: (a) Estimate the current and lifetime prevalence of mental disorders in general adult population and its sociodemographic and somatic correlates. (b) Examine the disability associated with mental disorders. (c) Assess the treatment gap, which is understood as the proportion of people screened positive for a mental disorder but not receiving any care.
2. METHOD
2.1. Sampling
Data for this study was collected from October 16 to November 20, 2017, by centrally trained staff using a face‐to‐face paper and pencil interviewing. A two‐stage sampling method was employed to obtain a sample of Czech adults representative for age, gender, education, and region of residence. The persons eligible for the interview were chosen using a random‐route procedure and a first‐birthday method. Specifically, in the first stage, a random sample of 850 voting districts was selected from all voting districts. Second, a random starting address was chosen in all of the selected voting districts. From these starting addresses, the interviewers operated according to the following instructions: They had to stand with the right hand next to a house and had to find the fourth house on the way. If there were more apartments in the house, they had to choose a household from the fourth apartment when counting from the top of the house.
The interviewer asked the door‐opening member of the household for a number of people living there and their age. In single‐member households, a person who was at least 18 years old was eligible for interviewing. In households with more members, the person who was at least 18 years old and had their birthday closest to the date of the interviewer's visit was chosen for the interview. If nobody opened the door or if the eligible person from a multi‐member household was not at home, the interviewer would come back, twice at most, in order to reach the household member. All participants provided an oral informed consent. They have been informed about the purpose of the study and the storage and use of the data, and their data were anonymized. This study was approved by the Ethics Committee of the National Institute of Mental Health, Czech Republic.
2.2. Measurements
2.2.1. Characteristics of participants and their attitudes towards mental health problems
A complete list of questions concerning multiple characteristics of the participants is provided in Table S1. The questionnaire was self‐developed; following sociodemographic information was gathered: gender, age, size of residence, the highest obtained education, occupation, marital status, and number of children. The respondent's current and past health status was assessed through a battery of questions. Moreover, information about health behaviour concerning the use of tobacco, alcohol, drugs, and physical activity as well as social contacts and serious life events during the five past years was collected. Questions on help‐seeking behaviour, examining attitudes towards mental health professionals, and experience with mental health services, which are presented in Table S2, were complemented with the item on social distance towards people with different types of mental disorders, such as schizophrenia, depression, dementia, and others.
2.2.2. Mini‐International Neuropsychiatric Interview
The fifth version of Mini‐International Neuropsychiatric Interview (MINI) was used for detection of mental disorders. MINI is a brief, fully structured interview for the assessment of major psychiatric disorders included in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders and the 10th version of the International Classification of Diseases (Sheehan et al., 1998). It allows administration by trained nonspecialized interviewers (Sheehan et al., 1998) and has been used in numerous previous population‐based studies (Faravelli et al., 2004; Kadri et al., 2010; Leray et al., 2011; Stylianidis, Pantelidou, Chondros, Roelandt, & Barbato, 2014; Vrublevska et al., 2017). A Czech version of MINI is based on an expert translation conducted by a professor of psychiatry Petr Zvolský; it has been used in clinical practice in the Czech Republic for many years, and it was also used in the unpublished epidemiological survey in 2005. We checked the accuracy of the translation before we conducted the survey, and we found it very good.
It consists of 16 modules, each of them referring to a diagnostic category, allowing for determining the diagnoses of 30 mental disorders. In the present study, three modules have not been included (M: Anorexia nervosa, N: Bulimia nervosa, P: Antisocial personality disorder), leaving 13 modules with 25 possible diagnoses of mental disorders. In this study, a part of the Module L (Psychotic disorders) was modified. Because the administrators were not trained to assess whether the respondents' answers are bizarre, the answers to questions L1 to L5 were written down and then separately examined by five experts to assess whether they are bizarre or not. Inconsistencies in ratings were solved through discussion.
2.2.3. The Psychosis Screening Questionnaire
As an addition to the psychotic disorders module contained in MINI, the Psychosis Screening Questionnaire was used to assess psychotic symptoms (Bebbington & Nayani, 1995). The Psychosis Screening Questionnaire consists of 17 items that are categorized into five sections related to hypomania, thought insertion, paranoia, strange experiences, and hallucinations. In the original version, the reference period for reporting psychotic symptoms was 12 months before conducting the interview. In this study, the reference period was changed to “ever in life,” thus examining the lifetime occurrence of psychotic symptoms.
2.2.4. Self‐identification as Mentally Ill
The Self‐identification as Mentally Ill scale was administered to measure self‐identification with a group of persons with a mental illness (Stolzenburg et al., 2017). This scale was developed by Schomerus et al. and originally termed “Mental Health Problem Appraisal Scale” (Schomerus et al., 2012). It consists of five items, rated on a 5‐point Likert scale spanning from 1 (don't agree at all) to 5 (agree completely), with higher scores reflecting a higher extent of self‐identification. The results in the original paper indicate that the scale possesses good internal consistency (Cronbach's α = 0.84; Stolzenburg et al., 2017). In our study, the Cronbach's α for this scale was 0.86, indicating good internal consistency as well.
2.2.5. The World Health Organization Disability Assessment Schedule
The World Health Organization Disability Assessment Schedule (WHODAS) was used to assess disability. WHODAS captures the level of a person's functioning in the following domains: cognition, mobility, self‐care, getting along, life activities, and participation. For all domains, WHODAS 2.0 provides a profile and summary measure of functioning and disability. It is an etiologically neutral instrument, meaning it allows to assess functioning independently from specific diseases. In the present study, a 12‐item version was used, which was suggested to explain 81% of the variance of the full 36‐item version (Üstün, 2010).
2.3. Fieldwork
In total, 279 persons were employed for the data collection. They had at least 2 years of experience working as interviewers for the agency that performed the fieldwork. The age of interviewers was distributed equally over all age categories. Interviewers and supervisors for each region were centrally trained in two phases and acquainted with the aim of research, ethical issues, instructions to participants, the structure of the questionnaire, and measurement tools. Support materials for interviewers following the guidelines of https://en.wikipedia.org/wiki/European_Society_for_Opinion_and_Marketing_Research were provided (Bowers, 1998). As a part of training, 72 pilot interviews were performed, lasting on average 50 min (the shortest interview was 30 min and the longest 105 min long). The comments on interviewers were incorporated into the questionnaire, if appropriate.
2.4. Quality control
The quality of each interviewer's work was controlled in four steps: The regional supervisor was present during certain parts of the interviews and visual control of completed questionnaire was conducted after it's delivery. The Data Entry SPSS software with control of logical links was used for converting data from paper form into dataset. The entry of data was done independently by two workers, and additional control was performed by supervisors. Finally, the performance of the interviews was checked retrospectively in 1,488 participants via e‐mail, mail, phone, or by the regional supervisor.
2.5. Statistical methods
We present descriptive data as mean ± standard deviation (SD) or n (%), where appropriate. To compare characteristics of the sample with data from the general population acquired from the Czech Statistical Office, chi‐square goodness of fit test was used to assess if data are consistent with a specified distribution.
3. RESULTS
3.1. Response rate
In total, 5,531 households were initially contacted; however, nobody was reached at home in 1,112 households (20%), thus 4,419 visits took place. From them, 756 (17%) households decided not to participate in the survey, 280 (6%) target participants refused to be interviewed, and 38 (1%) were not found. In addition, 39 (1%) respondents aborted the interview, which resulted in 3,306 completed interviews (response rate 75%). Flowchart is presented on Figure 1.
Figure 1.
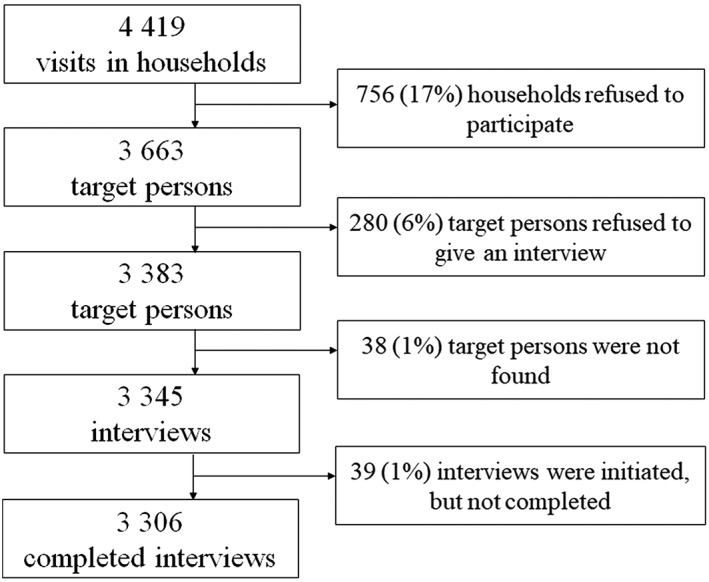
Selection of the study sample
3.2. Respondent characteristics
The final sample (mean age 48.8 ± SD 17.2) consisted of 1,774 women (54%) and 1,532 men (46%, Table 1). Eleven percent of the sample completed university education, 58% had paid work, and 21% lived in communities with more than 100,000 inhabitants. Sixty percent of the sample were married or cohabiting. Compared with the general population of the Czech Republic, there were no statistically significant differences related to the distribution of age, gender, and education (Table 2).
Table 1.
Characteristics of respondents
| Characteristics | n (%) |
|---|---|
| Gender | |
| Women | 1,774 (54) |
| Men | 1,532 (46) |
| Age | |
| 18–29 | 553 (17) |
| 30–39 | 589 (18) |
| 40–49 | 586 (18) |
| 50–64 | 817 (24) |
| 65+ | 761 (23) |
| Education | |
| Basic | 278 (8) |
| Vocational | 1,292 (39) |
| High school graduation | 1,178 (36) |
| Higher professional education, bachelor degree | 203 (6) |
| University | 355 (11) |
| Marital status | |
| Married | 1,495 (45) |
| Cohabiting | 497 (15) |
| Widowed | 372 (11) |
| Divorced | 422 (12) |
| Separated | 30 (1) |
| Single | 490 (15) |
| Had children | |
| Yes | 2,539 (77) |
| No | 767 (23) |
| Size of community (number of inhabitants) | |
| 1–99,999 | 2,598 (79) |
| 100,000+ | 708 (21) |
| Employment status | |
| Paid work | 1,927 (58) |
| Unemployed (looking for work) | 112 (3) |
| Unemployed (not looking for work) | 17 (0.5) |
| In household | 12 (0.5) |
| Parental leave | 120 (4) |
| Not working due to illness | 7 (0.5) |
| Disability pension | 107 (3) |
| Retired | 872 (26) |
| Student | 128 (4) |
| Other | 4 (0.5) |
Table 2.
Comparison between CZEMS study sample and general population
| CZEMS population (n = 3,306) | General population (n = 10,565,284) | p value | |
|---|---|---|---|
| Gender | |||
| Males | 1,532 (46.3) | 5,193,012 (49.2) | 0.6 |
| Females | 1,774 (53.7) | 5,372,272 (50.8) | |
| Age | |||
| 18–34 years | 815 (24.7) | 2,178,698 (25.2) | 1.0 |
| 35–54 years | 1,175 (35.5) | 3,159,015 (36.5) | |
| 55–74 years | 1,081 (32.7) | 2,564,780 (29.6) | |
| 75–94 years | 233 (7.1) | 747,340 (8.6) | |
| 95 years and more | 1 (0.0) | 7,181 (0.1) | |
| Size of community | |||
| 0–4,999 inhabitants | 1,264 (38.2) | 4,108,872 (38.9) | 1.0 |
| 5,000–19,999 inhabitants | 609 (18.4) | 1,943,878 (18.4) | |
| 20,000–99,999 inhabitants | 725 (21.9) | 2,196,266 (20.8) | |
| 100,000 and more | 708 (21.5) | 2,316,268 (21.9) | |
| Education | |||
| Basic | 278 (8.4) | 1,101,075 (14.0) | 0.4 |
| Vocational | 1,292 (39.2) | 2,913,253 (37.0) | |
| High school graduation | 1,178 (35.6) | 2,626,320 (33.4) | |
| Higher professional education, bachelor degree | 203 (6.1) | 296,188 (3.7) | |
| University | 355 (10.7) | 934,687 (11.9) |
Note. CZEMS: CZEch Mental health Study. Data is presented as n (%); p values are derived from chi‐square goodness of fit test assessing if data are consistent with a specified distribution.
4. DISCUSSION
CZEMS is a representative survey of mental disorders in the Czech Republic, a country situated in the region of CEE, where a reform of mental health care has just been launched. This study will provide detailed epidemiological data along with information about the patients' experience with mental health services, on which new policies for the development of mental health care in the Czech Republic can be built and evaluated. Results of the study will be vrelevant for other countries in CEE that share similarities in history, health behaviour, and system of mental health care. Details about the study methods could be adapted by other investigators in CEE to conduct a similar survey in their own settings.
The analyses will focus on the main project objectives. First, the prevalence of mental disorders and their comorbid combination will be assessed. The primary comorbid combination of interest will be alcohol abuse or dependence with CMD and SMI, owing to the frequent heavy alcohol consumption in the Czech Republic (Popova, Rehm, Patra, & Zatonski, 2007). Since an unpublished survey using the same methodology as in CZEMS was conducted in 2005, we will be able to estimate a possible change in the occurrence of mental disorders in the Czech Republic over the past 12 years. The second main goal of CZEMS is to assess the treatment gap and explore factors associated with it. Third, we aim to understand the level of disability associated with mental disorders, and we will analyse how behavioural risk factors, somatic comorbidities, sociodemographic, and family characteristics modify the burden of mental disorders, help seeking, and the intensity of service used by persons with different disability levels. Fourth, we aim to look at the association between attitudes towards mental health problems and help‐seeking behaviour.
This study has several strengths. The sample is representative to the population of the Czech Republic with respect to age, gender, and education. Rigorous sampling and quality control was adopted to optimize the quality of the data. Interviewers were trained in order to maximize participation and increase the likelihood that respondents would share personal information with them. The study used several previously validated and well accepted measurement tools. MINI is a widely used instrument for the detection of mental disorders and has been shown to have good validity and reliability (Lecrubier et al., 1997; Sheehan et al., 1997). Uniquely for a country in CEE, the administration of the Self‐identification as Mentally Ill scale and WHODAS within this study will enable us to explore whether self‐identification as a mentally ill person and disability play a role in seeking help for mental health problems. The results will serve as a basis for interventions aiming at decreasing the treatment gap in the Czech Republic.
Several limitations of this study need to be mentioned. Data in CZEMS is self‐reported and is a subject to potential misclassification (Althubaiti, 2016). Furthermore, information about lifetime mental health conditions was collected retrospectively and is affected by recall bias, which may lead to underestimation of the lifetime prevalence of mental disorders (Moffitt et al., 2010; Wells & Horwood, 2004). As previously reported (de Graaf, Ten Have, & van Dorsselaer, 2010; Kessler & Üstün, 2004), non‐participants in studies differed from the respondents in several sociodemographic characteristics. In a Dutch survey NEMESIS (Bijl, Van Zessen, Ravelli, De Rijk, & Langendoen, 1998), the non‐participants were suggested to have a higher rate of mental disorders than respondents, whereas there was no such a difference in another study from the United States (Kessler et al., 2004). Characteristics of nonrespondents in the present study are not known.
If there was a higher rate of mental disorders in individuals that refused to participate in the study, were not found at home or did not complete the initiated interview, the prevalence of mental disorders would be underestimated in CZEMS. It needs to be acknowledged that the deinstitutionalization process has only recently been launched in the Czech Republic, meaning that a fair number of persons with mental disorders in the Czech Republic are hospitalized. Therefore, the true prevalence of mental disorders in the Czech Republic is likely higher than what will be suggested by CZEMS, and results of this study are only generalizable to community‐dwelling individuals. Despite the limitations, CZEMS is a valuable dataset for researchers and policy makers in the Czech Republic and other countries in CEE. The study will give new insights into the burden of mental disorders and the use of mental health services, which is crucial information for the ongoing mental health care reform in the Czech Republic.
DECLARATION OF INTEREST STATEMENT
None declared.
Supporting information
Table S1 Sociodemographic, behavioural and clinical characteristics of participants: items in the questionnaire
Table S2 Help‐seeking behaviour: items in the questionnaire
ACKNOWLEDGEMENTS
We thank the MindBridge agency, the interviewers who performed the fieldwork and all study participants. We also thank Prof Lucie Bankovská Motlová, MD, PhD, and Jiří Renka, MD. for their contribution to assessment of mental disorders. The CZEch Mental health Study (CZEMS) was supported by the project “Sustainability for the National Institute of Mental Health” (grant LO1611), with a financial support from the Ministry of Education, Youth and Sports of the Czech Republic; as well as by the project “MERRPS”, CZ.03.3.X/0.0/0.0/15_124/0006067, with a financial support from the Ministry of Labour and Social Affairs of the Czech Republic.
Winkler P, Formánek T, Mladá K, Cermakova P. The CZEch Mental health Study (CZEMS): Study rationale, design, and methods. Int J Methods Psychiatr Res. 2018;27:e1728 10.1002/mpr.1728
REFERENCES
- Althubaiti, A. (2016). Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 9, 211–217. 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bebbington, P. , & Nayani, T. (1995). The psychosis screening questionnaire. International Journal of Methods in Psychiatric Research, 5(1), 11–19. [Google Scholar]
- Bijl, R. , Van Zessen, G. , Ravelli, A. , De Rijk, C. , & Langendoen, Y. (1998). The Netherlands Mental Health Survey and Incidence Study (NEMESIS): Objectives and design. Social Psychiatry and Psychiatric Epidemiology, 33(12), 581–586. [DOI] [PubMed] [Google Scholar]
- Bowers, D. K. (1998). The new research tool. Marketing Research, 10(3), 34. [Google Scholar]
- Charlson, F. J. , Baxter, A. J. , Dua, T. , Degenhardt, L. , Whiteford, H. A. , & Vos, T. (2015). Excess mortality from mental, neurological and substance use disorders in the Global Burden of Disease Study 2010. Epidemiology and Psychiatric Sciences, 24(2), 121–140. 10.1017/s2045796014000687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faravelli, C. , Abrardi, L. , Bartolozzi, D. , Cecchi, C. , Cosci, F. , D'Adamo, D. , … Truglia, E. (2004). The Sesto Fiorentino study: Point and one‐year prevalences of psychiatric disorders in an Italian community sample using clinical interviewers. Psychotherapy and Psychosomatics, 73(4), 226–234. [DOI] [PubMed] [Google Scholar]
- de Graaf, R. , Ten Have, M. , & van Dorsselaer, S. (2010). The Netherlands Mental Health Survey and Incidence Study‐2 (NEMESIS‐2): Design and methods. International Journal of Methods in Psychiatric Research, 19(3), 125–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höschl, C. , Winkler, P. , & Pěč, O. (2012). The state of psychiatry in the Czech Republic. International Review of Psychiatry, 24(4), 278–285. [DOI] [PubMed] [Google Scholar]
- Jacobi, F. , Wittchen, H.‐U. , Hölting, C. , Höfler, M. , Pfister, H. , Müller, N. , & Lieb, R. (2004). Prevalence, co‐morbidity and correlates of mental disorders in the general population: Results from the German Health Interview and Examination Survey (GHS). Psychological Medicine, 34(04), 597–611. [DOI] [PubMed] [Google Scholar]
- Kadri, N. , Agoub, M. , Assouab, F. , Tazi, M. , Didouh, A. , Stewart, R. , & Moussaoui, D. (2010). Moroccan national study on prevalence of mental disorders: A community‐based epidemiological study. Acta Psychiatrica Scandinavica, 121(1), 71–74. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund, P. , Chiu, W. T. , Demler, O. , Heeringa, S. , Hiripi, E. , … Zaslavsky, A. (2004). The US National Comorbidity Survey Replication (NCS‐R): Design and field procedures. International Journal of Methods in Psychiatric Research, 13(2), 69–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , & Üstün, T. B. (2004). The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp, M. , Beecham, J. , McDaid, D. , Matosevic, T. , & Smith, M. (2011). The economic consequences of deinstitutionalisation of mental health services: Lessons from a systematic review of European experience. Health & Social Care in the Community, 19(2), 113–125. [DOI] [PubMed] [Google Scholar]
- Kunitoh, N. (2013). From hospital to the community: The influence of deinstitutionalization on discharged long‐stay psychiatric patients. Psychiatry and Clinical Neurosciences, 67(6), 384–396. [DOI] [PubMed] [Google Scholar]
- Lecrubier, Y. , Sheehan, D. V. , Weiller, E. , Amorim, P. , Bonora, I. , Sheehan, K. H. , … Dunbar, G. C. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. [Google Scholar]
- Leray, E. , Camara, A. , Drapier, D. , Riou, F. , Bougeant, N. , Pelissolo, A. , … Millet, B. (2011). Prevalence, characteristics and comorbidities of anxiety disorders in France: Results from the “Mental Health in General Population” survey (MHGP). European Psychiatry, 26(6), 339–345. [DOI] [PubMed] [Google Scholar]
- Link, B. G. , Struening, E. L. , Rahav, M. , Phelan, J. C. , & Nuttbrock, L. (1997). On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior, 38, 177–190. [PubMed] [Google Scholar]
- Moffitt, T. E. , Caspi, A. , Taylor, A. , Kokaua, J. , Milne, B. J. , Polanczyk, G. , & Poulton, R. (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40(6), 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel, E. S. , Brugha, T. , & Fryers, T. (2005). Size and burden of depressive disorders in Europe. European neuropsychopharmacology: the journal of the European College of Neuropsychopharmacology, 15(4), 411–423. 10.1016/j.euroneuro.2005.04.008 [DOI] [PubMed] [Google Scholar]
- Pěč, O. (2018). Mental Health Reforms in the Czech Republic. BJPsych International. Published Online, 15 March 2018, pp., 1–3. 10.1192/bji.2017.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkola, S. P. , Isometsä, E. , Suvisaari, J. , Aro, H. , Joukamaa, M. , Poikolainen, K. , … Lönnqvist, J. K. (2005). DSM‐IV mood‐, anxiety‐and alcohol use disorders and their comorbidity in the Finnish general population. Social Psychiatry and Psychiatric Epidemiology, 40(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Popova, S. , Rehm, J. , Patra, J. , & Zatonski, W. (2007). Comparing alcohol consumption in central and eastern Europe to other European countries. Alcohol & Alcoholism, 42(5), 465–473. [DOI] [PubMed] [Google Scholar]
- Schomerus, G. , Auer, C. , Rhode, D. , Luppa, M. , Freyberger, H. J. , & Schmidt, S. (2012). Personal stigma, problem appraisal and perceived need for professional help in currently untreated depressed persons. Journal of Affective Disorders, 139(1), 94–97. [DOI] [PubMed] [Google Scholar]
- Sheehan, D. , Lecrubier, Y. , Sheehan, K. H. , Janavs, J. , Weiller, E. , Keskiner, A. , … Dunbar, G. (1997). The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID‐P and its reliability. European Psychiatry, 12(5), 232–241. [Google Scholar]
- Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. The Journal of Clinical Psychiatry, 59(Suppl 20), 22–33;quiz 34–57. [PubMed] [Google Scholar]
- Stolzenburg, S. , Freitag, S. , Evans‐Lacko, S. , Muehlan, H. , Schmidt, S. , & Schomerus, G. (2017). The stigma of mental illness as a barrier to self labeling as having a mental illness. The Journal of Nervous and Mental Disease, 205(12), 903–909. [DOI] [PubMed] [Google Scholar]
- Stylianidis, S. , Pantelidou, S. , Chondros, P. , Roelandt, J. , & Barbato, A. (2014). Prevalence of mental disorders in a Greek island. Psychiatrike= . Psychiatriki, 25(1), 19–26. [PubMed] [Google Scholar]
- Üstün, T. B. (2010). Measuring health and disability: Manual for WHO disability assessment schedule WHODAS 2.0. World Health Organization. [Google Scholar]
- Vrublevska, J. , Trapencieris, M. , Snikere, S. , Grinberga, D. , Velika, B. , Pudule, I. , & Rancans, E. (2017). The 12‐month prevalence of depression and health care utilization in the general population of Latvia. Journal of Affective Disorders, 210, 204–210. 10.1016/j.jad.2016.12.031 [DOI] [PubMed] [Google Scholar]
- Wells, J. E. , & Horwood, L. J. (2004). How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychological Medicine, 34(6), 1001–1011. [DOI] [PubMed] [Google Scholar]
- Whiteford, H. A. , Degenhardt, L. , Rehm, J. , Baxter, A. J. , Ferrari, A. J. , Erskine, H. E. , … Vos, T. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet (London, England), 382(9904), 1575–1586. 10.1016/s0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Winkler, P. , Barrett, B. , McCrone, P. , Csémy, L. , Janous̆ková, M. , & Höschl, C. (2016). Deinstitutionalised patients, homelessness and imprisonment: Systematic review. The British Journal of Psychiatry, 208(5), 421–428. [DOI] [PubMed] [Google Scholar]
- Winkler, P. , Krupchanka, D. , Roberts, T. , Kondratova, L. , Machů, V. , Höschl, C. , … Thornicroft, G. (2017). A blind spot on the global mental health map: A scoping review of 25 years' development of mental health care for people with severe mental illnesses in central and eastern Europe. The Lancet Psychiatry, 4(8), 634–642. [DOI] [PubMed] [Google Scholar]
- Winkler, P. , Mladá, K. , Krupchanka, D. , Agius, M. , Ray, M. K. , & Höschl, C. (2016). Long‐term hospitalizations for schizophrenia in the Czech Republic 1998‐2012. Schizophrenia Research, 175(1–3), 180–185. [DOI] [PubMed] [Google Scholar]
- Wittchen, H.‐U. , & Jacobi, F. (2005). Size and burden of mental disorders in Europe—A critical review and appraisal of 27 studies. European Neuropsychopharmacology, 15(4), 357–376. [DOI] [PubMed] [Google Scholar]
- Wittchen, H. U. , Jacobi, F. , Rehm, J. , Gustavsson, A. , Svensson, M. , Jonsson, B. , … Steinhausen, H. C. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21(9), 655–679. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Sociodemographic, behavioural and clinical characteristics of participants: items in the questionnaire
Table S2 Help‐seeking behaviour: items in the questionnaire


