Abstract
Objectives
No consensus has been reached regarding the theoretical dimensions underlying the Scale for Suicide Ideation (SSI) and Beck's Scale for Suicide Ideation (BSI), widely used in research and clinical practice. This undermines the understanding and management of suicidal behavior.
Methods
The factor structure of the SSI and the BSI was investigated in 201 patients visiting the emergency department of the Geneva University Hospital, Switzerland, for suicidal ideation or a suicide attempt.
Results
Exploratory factor analyses (EFAs) identified a unique theoretical dimension. Item removal based on analyses of communalities improved the explained part of variance in both scales. A joint factor analysis provided results very similar to those yielded by initial EFAs.
Conclusions
The single factor underlying the SSI and the BSI was composed of items encompassing a construct of suicide desire. Nonretained items corresponded to other elements of suicidal behavior (e.g., plans and preparations regarding the upcoming suicide attempt). These scales could not discriminate between suicide ideators and suicide attempters.
Keywords: scale for suicide ideation, Beck, dimensionality, factor analysis, suicide
1. INTRODUCTION
Scientific research on suicidal behavior has been undermined by the large variability in definitions of suicide‐related concepts, with a concrete impact on the generalization of findings (Posner, Oquendo, Gould, Stanley, & Davies, 2007; Silverman, Berman, Sanddal, O'Carroll, & Joiner, 2007a, 2007b). Suicidal behavior refers to the thoughts and behaviors related to the intention of committing suicide (O'Connor & Nock, 2014). It has been recently approached as a transition from ideation to action (Klonsky & May, 2014; Klonsky, Saffer, & Bryan, 2018), and a clear distinction between suicidal desire with and without intent to die has been established (Andriessen, 2006; Posner et al., 2007; Silverman et al., 2007a, 2007b; Van Orden et al., 2010). For example, some have specified that “ideations are purely cognitive in nature, while intent assumes, in part, an emotional component to the cognitive process, as well as a higher degree of mental engagement” (Silverman et al., 2007a, p. 257). In clinical practice, mental health professionals routinely struggle with this distinction, which directly influences the management of patients with suicidal behavior.
Scales are used in clinical settings to measure severity of suicidal behavior, and previous research has shown that current suicidal ideation is more easily disclosed via self‐report measures than clinical interviews (Kaplan et al., 1994). Though, the dimensionality of these measurement instruments is not well understood, which has led researchers to investigate their latent structure (Ghasemi, Shaghaghi, & Allahverdipour, 2015; Kodaka, Poštuvan, Inagaki, & Yamada, 2011). These instruments include not only the Scale for Suicide Ideation (SSI; Beck, Kovacs, & Weissman, 1979) and its self‐administered counterpart, the Beck Scale for Suicide Ideation (BSI; Beck, Steer, & Ranieri, 1988), but also the Modified Scale for Suicide Ideation (MSSI; Miller, Norman, Bishop, & Dow, 1986), or the SSI measuring suicidal ideation at the patient's worst point in life (SSI‐W; Beck, Brown, Steer, Dahlsgaard, & Grisham, 1999). Most studies have identified two or three dimensions underlying these instruments. Two‐factor models differentiated desire to die from preparation toward suicide (Beck, Brown, & Steer, 1997; Holden & DeLisle, 2005; Joiner, Rudd, & Rajab, 1997; Witte et al., 2006), whereas, three‐factor models usually divided this desire‐to‐die dimension into active and passive components (Beck et al., 1979; De Man, Balkou, & Iglesias, 1987; Holi et al., 2005; Steer, Rissmiller, Ranieri, & Beck, 1993). On the one hand, these findings suggest that these instruments assess suicidal behavior in an ideation‐to‐action framework in line with the theoretical approaches mentioned above; indeed, the preparation toward suicide factor was more strongly correlated to a higher degree of lethality than the suicide desire factor (Joiner et al., 1997). However, on the other hand, the preparation‐toward‐suicide factor was not consistently associated with lethality (Steer et al., 1993; Witte et al., 2006). Additionally, the items retained to form factors were not similar from one study to another, the factor distinction between active and passive desire to die is not always observed (Clum & Yang, 1995; Joiner et al., 1997), and a one‐factor solution also proposed to account for the latent structure of the BSI (Ayub, 2008).
The absence of consensus regarding the dimensional structure underlying suicidal behavior was hypothesized to be caused by differences of populations, instruments, and investigation methods (Holden & DeLisle, 2005). Therefore, the present study aimed to address these limitations in investigating the factor structure of two of the original instruments, namely the SSI and the BSI, with a similar methodology to a same population of patients visiting the emergency department of a general hospital for suicide‐related issues. These scales are similar in terms of item contents and cannot be differentiated from each other by the number of factor yielded from analyses conducted to this day and published in the literature. To the best of our knowledge, this procedure has never been attempted in previous research.
2. METHODS
2.1. Instruments
The SSI, administered by a trained psychiatrist, and the BSI, its self‐administered counterpart, include 19 items rated on a three‐point Likert scale. Each item is scored from 0 to 2 in ascending order of severity, giving a total score ranging from 0 to 38. The list of items is similar for both questionnaires, as are the anchors for each pair of items; however, anchors differ depending on the topic investigated (e.g., wish to live: 0 = Moderate to strong, 1 = Weak, 2 = None; Attitude toward ideation/wish: 0 = Rejecting, 1 = Ambivalent/Indifferent, 2 = Accepting). The 19 topics addressed in these questionnaires are as follows: wish to live (item 1), wish to die (item 2), reason for living (item 3), active attempt (item 4), passive attempt (item 5), duration of thoughts (item 6), frequency of ideation (item 7), attitude toward ideation (item 8), control over action (item 9), deterrents to attempt (item 10), reasons for attempt (item 11), specificity of planning (item 12), availability/opportunity (item 13), capability (item 14), expectancy (item 15), actual preparation (item 16), suicidal note (item 17), final acts (item 18), and deception (item 19). The BSI and SSI tend to be zero‐inflated as a score of 0 at the screening items 4 and 5 should lead to the interruption of the scales administration procedure and a total score of 0 (Beck & Steer, 1991). To attenuate this effect, we let participants fill out the entire scale even when screening items amounted to 0. The SSI has been validated in French as a self‐administered version (De Man et al., 1987; De Man, Leduc, & Labrèche‐Gauthier, 1993), which we used as equivalent to the English version BSI. We subsequently adapted this French BSI to a clinician‐administered version based on the original SSI.
2.2. Participants
The sample comprises 201 individuals (122 women and 79 men), with a mean age of 34.4 ± 14.5 years old (range: 16–82) and 0.77 ± 1.08 children on average. Most participants had the Swiss citizenship (57.7%), were single (65.7%), employed or students (57.7%), had a history of suicide attempts (63.2%), and a psychiatric diagnosis (88.6%) highlighted by the Mini‐International Neuropsychiatric Interview (Sheehan et al., 1998). The most prevalent diagnoses were major depressive episode (69.7%), alcohol dependence (16.9%), and nonalcohol substance dependence (10%). A total of 133 participants were included in the study for suicidal ideation and 68 for a suicide attempt.
2.3. Procedure
A global study on determinants of suicidal behavior was proposed to patients upon their admission to the adult psychiatric emergency department of the Geneva University Hospitals, Switzerland, for suicidal ideation or a suicide attempt. These constructs were differentiated according to the definition of Posner and colleagues (Posner et al., 2007, p. 1037). Suicidal ideation refers to “passive thoughts about wanting to be dead or active thoughts about killing oneself, not accompanied by preparatory behavior.” For the specific needs of this study, we also included in the suicidal ideation category what these authors define as “preparatory acts toward imminent suicidal behavior,” that is when an individual “takes steps to injure him‐ or herself, but is stopped by self or others from starting the self‐injurious act before the potential for harm has begun.” In contrast, a suicide attempt is described as “a potentially self‐injurious behavior, associated with at least some intent to die, as a result of the act (…) [that] may or may not result in actual injury.” After signing an information and consent form, participants were administered the SSI by a trained psychiatrist, and subsequently completed the self‐administered BSI. Other questionnaires nonrelevant for the present study were presented as well. The study procedure was approved by the Canton Geneva Ethics and Scientific Research Committee (project number 14‐168) and was conducted in compliance with the Helsinki Declaration.
2.4. Statistical analyses
Every statistical analysis was done with R version 3.3.2 (R Core Team, 2016) and we considered results to be statistically significant with a p value of 0.05 and below. In line with recommendations of Fabrigar, Wegener, MacCallum, and Strahan (1999), we considered the following five steps to conduct factor analyses.
2.4.1. Data analysis
We initially examined the structure of our data to assess their suitability for factor analyses. As the SSI and the BSI are ordinal scales, we rectified the methodological violation of the linearity assumption in conducting factor analyses from a polychoric correlation matrix obtained with the “polycor” package (Fox, 2016). Multivariate normality was assessed with Mardia's, Henze‐Zirkler's, and Royston's tests using the “multivariate normality” package (Korkmaz, Goksuluk, & Zararsiz, 2014). Data suitability for factor analysis was evaluated using Bartlett's test of homogeneity of variances with the “REdaS” package (Maier, 2015), and the Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy with the “psych” package (Revelle, 2016). We considered the communality level and the variable‐to‐factor ratio (MacCallum, Widaman, Zhang, & Hong, 1999) as well as the participant‐to‐item ratio (Costello & Osborne, 2005) as measures of factor overdetermination to assess sample size quality. As data were generally not normally distributed (see below), we chose to use nonparametric tests when available (e.g., Mann–Whitney test for mean comparison, Spearman rank‐order for correlation).
2.4.2. Type of factor analysis
Because previous studies did not agree on the number of latent variables that underlie the SSI, SSI‐W, BSI, or MSSI, we conducted exploratory factor analyses (EFAs). The EFA is appropriate to find out the dimensionality underlying a measurement instrument rather than to confirm it (Conway & Huffcutt, 2003; Osborne & Fitzpatrick, 2012).
2.4.3. Procedure
As we hypothesized that latent factors underlie SSI and BSI items, we used a common factor extraction model rather than a component extraction model (Conway & Huffcutt, 2003). We selected the type of procedure (i.e., maximum likelihood, principal axis factoring) to fit the common factor model to our data after analysis of multivariate normality (Fabrigar et al., 1999).
2.4.4. Number of factors
To estimate the number of factors retained in analyses, we observed the Cattell's scree plot (Cattell, 1966) and the parallel analysis scree plot (Horn, 1965), obtained with the “stats” package (R Core Team, 2016). We also considered comparison data analysis with the “EFA Comparison Data” program code (Ruscio & Roche, 2012).
2.4.5. Axes rotation method
On the basis of previous studies (Steer et al., 1993; Witte et al., 2006), we hypothesized that factors would be correlated and consequently adopted an oblique rotation method—the oblimin rotation, obtained with the “GPArotation” package (Bernaards & Jennrich, 2005).
We assessed replicability as an additional measure of the robustness of the extracted model, following the procedure suggested by Osborne and Fitzpatrick (2012) for internal replication, by splitting the sample into two groups randomly constituted. Simulations have shown that only 60% of EFAs led to correct factor structures when the participant‐to‐item ratio was 10:1 (Costello & Osborne, 2005). This finding has potential consequences for the analyses of this study because of the relatively small participant‐to‐item ratio of our sample (i.e., 201 participants and 19 items, resulting in a ratio of 10.6:1). Therefore, a similar factor structure in EFAs before and after internal replication would suggest that our sample size was large enough to provide reliable results.
Finally, a joint factor analysis was run to ensure that both measures captured the same latent dimensions.
3. RESULTS
3.1. Descriptive statistics
Spearman rank‐order correlations between pairs of items of the SSI and the BSI (e.g., item 1 of the SSI and item 1 of the BSI) ranged from 0.351 to 0.714. The Spearman rank‐order correlation between both scales was 0.804. Further details, means, and standard deviations for each item are summarized in Table 1. Mann–Whitney tests of mean comparisons showed that nine items of the SSI significantly differed from their BSI counterpart, specifically items 7, 8, 10, 12, 13, 14, 16, 17, and 19.
Table 1.
Descriptive statistics of the Scale for Suicide Ideation (SSI) and the Beck Scale for Suicide Ideation (BSI)
| Spearman's rank‐order correlations between SSI and BSI pairs of items | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 0.597 | 0.602 | 0.664 | 0.714 | 0.540 | 0.600 | 0.592 | 0.482 | 0.496 | 0.351 | |
| Item | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Total |
| 0.399 | 0.536 | 0.545 | 0.650 | 0.531 | 0.490 | 0.692 | 0.606 | 0.401 | 0.804 | |
| Mean and standard deviation of SSI items and total score (item score range: 0–2; total score range: 0–38) | ||||||||||
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 0.657 ± 0.589 | 1.194 ± 0.733 | 0.806 ± 0.733 | 0.841 ± 0.765 | 0.970 ± 0.774 | 0.711 ± 0.719 | 0.846 ± 0.708 | 0.925 ± 0.700 | 0.692 ± 0.703 | 0.706 ± 0.734 | |
| Item | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Total |
| 1.124 ± 0.547 | 0.915 ± 0.786 | 1.209 ± 0.870 | 0.826 ± 0.689 | 0.781 ± 0.567 | 0.358 ± 0.649 | 0.209 ± 0.496 | 0.124 ± 0.399 | 0.373 ± 0.675 | 14.269 ± 7.236 | |
| Mean and standard deviation of BSI items and total score (item score range: 0–2; total score range: 0–38) | ||||||||||
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 0.731 ± 0.646 | 1.299 ± 0.749 | 0.881 ± 0.772 | 0.945 ± 0.763 | 1.070 ± 0.791 | 0.731 ± 0.691 | 0.682 ± 0.654 | 1.070 ± 0.738 | 0.662 ± 0.696 | 0.438 ± 0.654 | |
| Item | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Total |
| 1.124 ± 0.509 | 0.692 ± 0.751 | 0.821 ± 0.882 | 1.005 ± 0.725 | 0.791 ± 0.725 | 0.662 ± 0.745 | 0.343 ± 0.638 | 0.149 ± 0.445 | 0.945 ± 0.789 | 15.039 ± 7.618 | |
| Mann–Whitney test of mean comparison between SSI and BSI pairs of items | ||||||||||
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| W = 19,128, p = 0.302 | W = 18,548, p = 0.125 | W = 19,192, p = 0.353 | W = 18,690, p = 0.166 | W = 18,800, p = 0.201 | W = 19,774, p = 0.690 | W = 22,658, p = 0.021 | W = 18,045, p = 0.045 | W = 20,658, p = 0.668 | W = 24,294, p < 0.001 | |
| Item | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Total |
| W = 20,250, p = 0.958 | W = 23,346, p = 0.004 | W = 24,898, p < 0.001 | W = 17,526, p = 0.013 | W = 20,476, p = 0.792 | W = 15,552, p < 0.001 | W = 18,390, p = 0.029 | W = 19,886, p = 0.616 | W = 12.113, p < 0.001 | W = 19,037, p = 0.318 | |
Note: In bold, tests significant at the p ≤ 0.05 threshold.
Patients incorporated in the study for suicidal ideation (n = 133) had a mean score on the BSI of 16.053 ± 7.553, and those included for a suicide attempt (n = 68) had a mean score of 13.059 ± 7.405. These means were significantly different from each other according to the Mann–Whitney test (U = 3,499.500, p = 0.009). In contrast, on the SSI, those with suicidal ideation had a mean score of 14.722 ± 7.112, and suicide attempters had a mean score of 13.382 ± 7.445, showing that scores are not significantly different (U = 4,053.500, p = 0.230). Both scales were negatively correlated with age according to the Spearman coefficient, but only the SSI correlation was statistically significant (r s = −0.147, p = 0.038). Mann–Whitney test showed gender differences in none of the questionnaires.
3.2. Scale for Suicide Ideation
Analysis of multivariate normality suggested that distribution of SSI data was not multivariate normal (Mardia's test of skewness: γ = 72.728, χ 2 = 2,436.381, p < 0.001; Mardia's test of kurtosis: γ = 429.566, z = 7.670, p < 0.001; Henze‐Zirkler's test: HZ = 1.478, p < 0.001; Royston's test: H = 1,430.058, p < 0.001). The Bartlett's test of homogeneity of variances confirmed the existence of inter‐item correlations (χ 2 = 1,295.927, df = 171, p < 0.001). The KMO had an overall measure of 0.87 for sampling adequacy, suggesting a meritorious adjustment of items to latent factors (Beavers et al., 2013). Because of the violation of multivariate normality assumption, we chose principal axis factoring to estimate the common‐factor model of the data.
One factor clearly stood out from others in both Cattell's and parallel analysis scree plots, suggesting that a one‐factor solution should be extracted from the correlation matrix. However, comparison data using the Spearman rank‐order correlations proposed to retain two factors; see Figure 1. Therefore, we decided to compute factor analyses with extraction of one and two factors using principal axis factoring and oblimin rotation. Yet, the two‐factor solution provided improper results with occurrences of the Heywood cases and cross loadings, leading us to pursue analyses with the one‐factor model only. Results of the EFA are provided in Table 2. Item communalities ranged from 0.054 to 0.714, accounting for 39.2% of the total variance.
Figure 1.
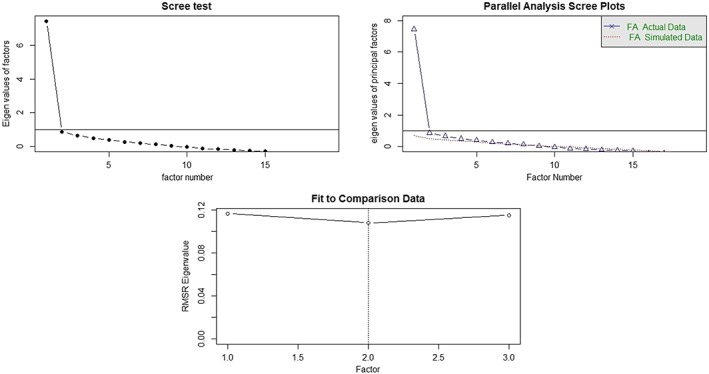
Cattell's scree plot, parallel analysis scree plot and comparison data analysis for the Scale for Suicide Ideation (SSI)
Table 2.
Exploratory factor analysis (EFA) on the Scale for Suicide Ideation (SSI) and the Beck Scale for Suicide Ideation (BSI) with principal axis factoring estimation
| SSI | BSI | ||||
|---|---|---|---|---|---|
| Items | Factor 1 | Communalities | Items | Factor 1 | Communalities |
| SSI 1 | 0.682 | 0.465 | BSI 1 | 0.733 | 0.538 |
| SSI 2 | 0.845 | 0.714 | BSI 2 | 0.851 | 0.724 |
| SSI 3 | 0.770 | 0.594 | BSI 3 | 0.789 | 0.622 |
| SSI 4 | 0.797 | 0.635 | BSI 4 | 0.775 | 0.600 |
| SSI 5 | 0.641 | 0.410 | BSI 5 | 0.576 | 0.332 |
| SSI 6 | 0.707 | 0.499 | BSI 6 | 0.726 | 0.528 |
| SSI 7 | 0.744 | 0.553 | BSI 7 | 0.773 | 0.598 |
| SSI 8 | 0.554 | 0.307 | BSI 8 | 0.751 | 0.565 |
| SSI 9 | 0.469 | 0.220 | BSI 9 | 0.402 | 0.162 |
| SSI 10 | 0.496 | 0.246 | BSI 10 | 0.543 | 0.295 |
| SSI 11 | 0.331 | 0.110 | BSI 11 | 0.155 | 0.024 |
| SSI 12 | 0.676 | 0.456 | BSI 12 | 0.607 | 0.369 |
| SSI 13 | 0.499 | 0.249 | BSI 13 | 0.593 | 0.351 |
| SSI 14 | 0.639 | 0.408 | BSI 14 | 0.641 | 0.411 |
| SSI 15 | 0.813 | 0.661 | BSI 15 | 0.842 | 0.709 |
| SSI 16 | 0.709 | 0.503 | BSI 16 | 0.740 | 0.548 |
| SSI 17 | 0.472 | 0.223 | BSI 17 | 0.436 | 0.190 |
| SSI 18 | 0.375 | 0.140 | BSI 18 | 0.201 | 0.041 |
| SSI 19 | 0.232 | 0.054 | BSI 19 | 0.188 | 0.036 |
Next, an internal replication analysis was conducted by randomly dividing participants into two subgroups of n = 101 (subgroup 1) and n = 100 (subgroup 2). In both, preliminary analyses showed that data distribution was not multivariate normal, items were intercorrelated and had a meritorious (subgroup 1), respectively middling (subgroup 2) adjustment to latent factors. Cattell's scree plot, parallel analysis scree plot, and comparison data showed that a one‐factor solution should be retained for the two subgroups.
An EFA with principal axis factoring was run, and replicability was assessed in comparing the squared differences of absolute factor loadings between subgroups. Subgroup 1 and 2 explained 38.7% and 38.8%, respectively, of the variance in the SSI. Every squared difference was below the threshold of 0.04, which suggests that item loadings were stable (i.e., with a loading difference less than 0.20) on factor 1 between the two subgroups (Osborne & Fitzpatrick, 2012). Detailed results are available online (Data S1).
3.3. Beck Scale for Suicide Ideation
Analysis of multivariate normality suggested that distribution of BSI data was not multivariate normal (Mardia's test of skewness: γ = 62.912, χ 2 = 2,107.539, p < 0.001; Mardia's test of kurtosis: γ = 431.939, z = 8.266, p < 0.001; Henze–Zirkler's test: HZ = 1.175, p < 0.001; Royston's test: H = 1,385.763, p < 0.001). The Bartlett's test of homogeneity of variances confirmed the existence of inter‐item correlations (χ 2 = 1,326.446, df = 171, p < 0.001). The KMO had an overall measure of sampling adequacy of 0.91 suggesting a marvelous adjustment of items to latent factors.
We decided to conduct an EFA with principal axis factoring estimation as data were not multivariate normal. As shown in Figure 2, results from Cattel's and parallel analysis scree tests, as well as from comparison data using the Spearman rank‐order correlations, suggested a one‐factor solution. Results from the EFA are provided in Table 2. Item communalities ranged from 0.024 to 0.724, accounting for 40.2% of the total variance.
Figure 2.
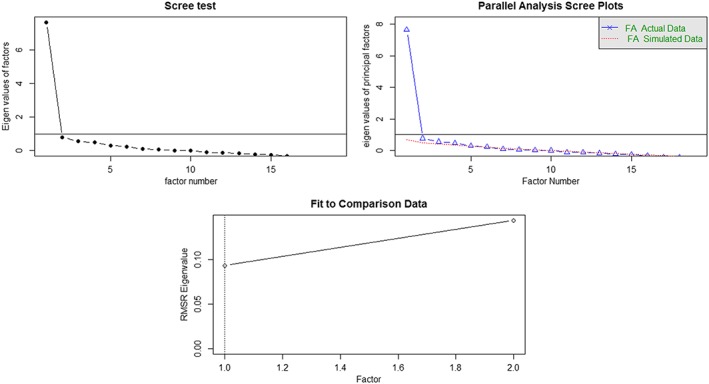
Cattell's scree plot, parallel analysis scree plot and comparison data analysis for the Beck Scale for Suicide Ideation (BSI)
Next, a replication analysis was conducted with the BSI in randomly dividing participants into two subgroups. In subgroup 1 (n = 101) and subgroup 2 (n = 100), data distribution was not multivariate normal, items were intercorrelated and had a meritorious adjustment to latent factors. One factor stood out from others in Cattell's and parallel analysis scree plots. Comparison data suggested a two‐factor solution for both subgroups; yet, for replication we chose to pursue analyses with a one‐factor model.
An EFA with principal axis factoring was run in every subgroup and replicability assessed in comparing the squared differences of absolute factor loadings between subgroups. Subgroups 1 and 2 explained 36.7% and 42.0%, respectively, of the variance in the BSI. With a squared difference of 0.068, item 11 was the only item significantly volatile according to the criterion of Osborne and Fitzpatrick (2012). Detailed results are available online (Data S2).
3.4. Reduced versions of the SSI and the BSI
Factor analyses of the SSI and the BSI identified items with communalities below 0.400, which are likely to be either not related to the extracted factor or associated with a factor that has not been extracted (Costello & Osborne, 2005). Moreover, although the 19:1 variable‐to‐factor ratio in both scales and loadings is greater than 0.50 on 11 items of the SSI and 10 items of the BSI suggest that factor 1 was highly overdetermined, heterogeneous communality values are problematic in estimating the quality of sample size (MacCallum et al., 1999). For these reasons, we decided to remove items with communalities below 0.400 from the SSI and the BSI, and conducted EFAs and replication analyses again with the remaining items of these scales following the same methodological procedure as with the 19‐item questionnaires. Thus, the reduced version of the SSI consisted of 11 items (SSI‐11), specifically items 1, 2, 3, 4, 5, 6, 7, 12, 14, 15, and 16, and the reduced version of the BSI (BSI‐10) had 10 items, specifically items 1, 2, 3, 4, 6, 7, 8, 14, 15, and 16.
Analyses of multivariate normality, homogeneity of variances and sampling adequacy provided similar results as for the full‐sized scales. On the basis of Cattell's and parallel analysis scree plots as well as comparison data, we conducted an EFA using principal axis factoring with extraction of one factor for each scale (Table 3). The model for the SSI‐11 seemed much improved in accounting for 53.9% of the total variance, displaying communalities above 0.400 with the sole exception of item 14 (0.368), and showing an 11:1 variable‐to‐factor ratio, implying that factor 1 remained highly overdetermined. Replication analyses confirmed the one‐factor structure of the SSI‐11. Subgroups 1 (n = 101) and 2 (n = 100) explained 52.1% and 54.6%, respectively, of the variance in the reduced questionnaire with no factor loading difference less than 0.20.
Table 3.
Exploratory factor analysis (EFA) on the Scale for Suicide Ideation (SSI)‐11 and the Beck Scale for Suicide Ideation (BSI)‐10 with principal axis factoring estimation
| SSI‐11 | BSI‐10 | ||||
|---|---|---|---|---|---|
| Items | Factor 1 | Communalities | Items | Factor 1 | Communalities |
| SSI 1 | 0.699 | 0.488 | BSI 1 | 0.757 | 0.573 |
| SSI 2 | 0.851 | 0.724 | BSI 2 | 0.864 | 0.746 |
| SSI 3 | 0.769 | 0.591 | BSI 3 | 0.800 | 0.639 |
| SSI 4 | 0.811 | 0.657 | BSI 4 | 0.779 | 0.607 |
| SSI 5 | 0.669 | 0.448 | BSI 6 | 0.733 | 0.537 |
| SSI 6 | 0.693 | 0.480 | BSI 7 | 0.784 | 0.614 |
| SSI 7 | 0.742 | 0.550 | BSI 8 | 0.769 | 0.592 |
| SSI 12 | 0.653 | 0.426 | BSI 14 | 0.614 | 0.377 |
| SSI 14 | 0.607 | 0.368 | BSI 15 | 0.848 | 0.720 |
| SSI 15 | 0.821 | 0.674 | BSI 16 | 0.688 | 0.474 |
| SSI 16 | 0.724 | 0.524 | |||
Similarly, the model for the BSI‐10 seemed much improved, accounting for 58.8% of the total variance, displaying only one communality below 0.400 (item 14, 0.377), and showing a 10:1 variable‐to‐factor ratio implying that factor 1 remains highly overdetermined. Replication analyses confirmed the one‐factor structure of the BSI‐10. Subgroups 1 (n = 101) and 2 (n = 100) explained 55.6% and 60.1%, respectively, of the variance in the reduced questionnaire with no factor loading difference less than 0.20.
3.5. Joint factor analysis of the SSI and the BSI
An additional investigation of the underlying structure, we conducted a joint factor analysis of the SSI and the BSI retaining one factor. The joint factor analysis explained 38% of the variance of the common scales, whereas 10 items of the SSI (i.e., items 1, 2, 3, 4, 5, 6, 7, 12, 15, and 16) and 9 items of the BSI (i.e., items 1, 2, 3, 5, 6, 7, 8, 15, and 16) had communalities of 0.400 and above. Only item 14 of the SSI (0.395) and the BSI (0.374) showed communalities that did not reach the 0.400 threshold proposed by Costello and Osborne (2005).
4. DISCUSSION
This study investigated the factor structure of the SSI and the BSI in a sample of patients visiting an adult psychiatric emergency department for suicidal ideation or a suicide attempt. Most previous studies on the factor structure of the SSI and related instruments identified two or three dimensions that usually distinguished suicide desire/motivation from preparation towards suicide. In contrast, our results suggest that a single theoretical dimension underlies the SSI and the BSI.
The one‐factor solution accounted for 39.2% of the total variance of the clinician‐rated SSI, and 40.2% in the total variance of the patient‐rated BSI. The only study proposing a unique underlying dimension found that the latter accounted for 19.2% of the variance in BSI items (Ayub, 2008). Supporting our decision to extract only one factor from EFAs, the SSI and the BSI met strong structural replication. No pair of items showing loading differences equal to or above 0.20, a criterion of stability according to Osborne and Fitzpatrick (2012), were identified in the internal replication of the SSI. In the same vein, only one item (item 11) failed to meet this criterion in replication of the BSI. These results also suggest that our sample was sufficient in size.
In both instruments, EFAs identified a number of items with communalities below 0.400, implying that removal of these items would improve the factor model (Costello & Osborne, 2005). Indeed, after eliminating eight items from the SSI and nine items from the BSI, factor solutions showed remarkable improvement with explained total variance in SSI items increasing from 39.2% to 53.9% and in BSI items from 40.2% to 58.8%. Moreover, replication analyses confirmed the stability of these reduced scales in showing no loading differences equal to or above 0.20.
These findings suggest that decreasing the number of SSI and BSI items would be beneficial to better encompass the unique latent construct of these instruments. Scrutinizing the items commonly retained in both scales—that is, items 1, 2, 3, 4, 6, 7, 14, 15, and 16—we observe that these items seem to encompass a construct of suicide desire. On the other hand, items removed from both scales—that is, items 9, 10, 11, 13, 17, 18, and 19—require participants to take a critical and active stance regarding their suicidal ideation, such as reasons for committing suicide or avoiding it (items 10 and 11), reflections regarding a method or the context, specific arrangements in prevision of their suicide (items 13, 17, 18, and 19), or considerations regarding their perceived degree of control (item 9). In other words, these nonretained items first require respondents to think about their feelings related to suicide, and; second, address concrete aspects of suicidal behavior that go beyond suicide desire. Thus, although the nonretained items did not constitute an homogeneous factor, our analyses share similarities with other studies highlighting a dichotomous suicide desire/plans and preparation factor structure (Holden & DeLisle, 2005; Joiner et al., 1997; Witte et al., 2006). Interestingly, a previous study found that written preparation for suicide—such as a note; see item 17—was negatively correlated with a factor intended to represent preparatory actions toward suicide, suggesting that thinking about reasons for committing suicide could have a protective function (Joiner et al., 1997).
In our study, the outlying items were not the same in both scales. Although items 9, 10, 11, 13, 17, 18, and 19 had low communalities in the SSI and the BSI, the 0.400 cutoff was not reached for item 8 in the SSI and for items 5 and 12 in the BSI. The SSI and the BSI differ from each other in that a clinician completes the former, whereas the latter is self‐administered. Their items are nevertheless similar in terms of contents, and we therefore expected that psychometric properties would show a high degree of similarity in both instruments. However, the correlation between the SSI and the BSI was high (r s = 0.804) and correlations between the same items of the scales were low to high (r s = 351 to 0.714), according to the criteria of Hinkle, Wiersma, and Jurs (2003). Nine item means differed from their paired item according to the Mann–Whitney test and EFAs and replication analyses did not yield to the same results in both scales. Overall, these observations suggest that the SSI and the BSI were not responded to in the same way by participants.
A few hypotheses can be advanced to address this difference between the clinician‐rated SSI and the patient‐rated BSI. First, the SSI has been validated in French into a self‐administered scale (De Man et al., 1987, 1993). In other words, the French‐validated version of the SSI corresponds to the original BSI and not the original SSI. Second, although all psychiatrists mandated for the study were provided with specific training aimed at maximizing coherence in SSI administration, the absence of strict guidelines in the scales' administration from the original authors (Beck et al., 1979) might account for a part of the variability in the score differences. Similarly, the presence of a third party—in this case, the psychiatrist—might have influenced the way participants answered questions. Third, owing to the study design, all participants were initially administered the SSI before answering the BSI. Yet, the direction of a hypothesized habituation effect remains unclear as, among the nine items differing between the two scales, four were rated more severely on the SSI (items 7, 10, 12, 13) and five on the BSI (items 8, 14, 16, 17, and 19). Fourth, we adopted a severe criterion for item selection, namely a communality above 0.400; yet, less severe criteria have been considered as acceptable in the literature, such as a factor loading of 0.400 (Matsunaga, 2010). Should we have selected items with the latter criterion, we would have proposed two scales retaining exactly the same items (removing items 11, 18, and 19).
We found that suicide attempters did not score higher than those with suicidal ideation either on the patient‐rated BSI or on the clinician‐rated SSI. This result implies that these scales are not suitable to differentiate ideators and attempters, and should rather be used as screening to discriminate between presence and absence of suicidal ideation, which was one of their initial functions (Ghasemi et al., 2015). This also suggests that suicidal ideation may not always be a necessary predictor of suicide attempt, as underlined in a recent meta‐analysis regarding suicidal behavior (Ribeiro et al., 2016). This is in line with the “ideation‐to‐action” conception of suicidal behavior that has recently given rise to several theoretical proposals (Klonsky et al., 2018). Illustrating this approach, the interpersonal‐psychological theory of suicide (Joiner, 2005; Van Orden et al., 2010) posits that an additional component, in this case the capability to act on one's suicide desire, is necessary to achieve the transition from suicidal ideation to suicide attempt.
Besides, the relevance of using the SSI and BSI global scores to assess level of suicidal behavior may be questioned because suicidal ideation is not a homogeneous theoretical construct. It has been indeed showed that suicidal ideation is composed of various components, some of them being predictors of the transition toward suicide attempt such as recency, duration, and controllability of ideation during the week where this ideation was worse, and presence of a suicidal plan (Nock et al., 2018). Similarly to what has been proposed elsewhere for the diagnosis of depression (Fried & Nesse, 2015), it might be meaningful to assess suicidal ideation not globally but with specific consideration for each of its components. Our results imply that the BSI and the SSI provide a global score of suicide desire; yet, the notion of the worst period experiencing suicidal ideation is not addressed in these scales, neither is the issue of recency or duration. Controllability is explored from a general perspective by a single item (item 9), whereas suicide planning and preparation are widely investigated through five items (i.e., items 12, 13, 16, 17, and 18). Thus, the SSI and the BSI may not be adequate to predict the ideation‐to‐action transition, as they thoroughly address only the planning component among those identified in the Nock et al. study. Similarly, if the generation of suicidal ideation does not depend on the same mechanisms as the generation of suicidal behavior, it cannot be excluded that the participants of our study responded differently to the scales depending on their inclusion criteria (i.e., suicidal ideation vs. suicide attempt).
Alternatively, the fact that suicidal ideators scored generally higher than suicide attempters in these scales might be explained by methodological reasons. First, our study design did not rule out the possibility that suicide attempters would have scored higher on these scales before they had attempted on their life than those who had only suicidal ideation. The great majority of participants were assessed immediately following their arrival at the emergency department, before discussing or analyzing their suicide attempt or suicidal ideation with a health professional. One might hypothesize that a suicide attempt as such has an alleviating effect on suicidal ideation, through either a biological response or a psychological process, such as eliciting regrets or shame regarding the gesture. Interestingly, it has been found that suicidal ideation tends to improve after hospital admission in those who did a suicide attempt in the preceding days (Russ, Kashdan, Pollack, & Bajmakovic‐Kacila, 1999). However, this hypothesis cannot be further debated as, to our knowledge, no study has yet identified an immediate, beneficial effect of unsuccessful suicide attempt on suicidal ideation. Second, it is likely that individuals visiting the emergency department of a general hospital for suicidal ideation suffer, on average, from more severe ideation than the general population of suicidal ideators (whose intensity of ideation may be strongly different from one person to another). In this regard, participants of our study included for suicidal ideation constituted a nonrepresentative subgroup of the latter population, which may restrict the generalization of our findings.
We encountered additional methodological limitations in conducting this study. First, the original versions of the SSI and BSI have not been directly validated in French; we used a version of the BSI validated in French based on the original SSI (De Man et al., 1993), and adapted a French version of the SSI from that one. Second, factor analyses were conducted on scales made of ordinal variables. Yet we conducted statistical tests commonly used in factor analyses that require continuous variables, which might have impacted our results. Finally, we acknowledge that confirmatory factor analyses (CFA) could have been conducted to further test our findings and allow model comparisons based on statistical indices. Using CFAs would be appropriate in future research aiming to confirm the results of the present study in a comparable sample.
CONFLICT OF INTEREST
All authors declare that they have no conflict of interest.
Supporting information
Data S1: Supporting Information
Data S2: Supporting Information
ACKNOWLEDGEMENTS
We are thankful to Prof. François Sarasin, Dr. Hélène Richard‐Lepouriel, and the medical team of the Geneva University Hospitals emergency department for their precious contributions to this study.
This study was funded by the Service of Liaison Psychiatry and Crisis Intervention of the Geneva University Hospitals, Switzerland. It did not benefit from any other grant or funding source.
Baertschi M, Costanza A, Canuto A, Weber K. The dimensionality of suicidal ideation and its clinical implications. Int J Methods Psychiatr Res. 2019;28:e1755 10.1002/mpr.1755
Footnotes
In the joint factor analysis, item 14 was the only one that did not reach the .400 communality threshold in both scales.
REFERENCES
- Andriessen, K. (2006). On “intention” in the definition of suicide. Suicide & Life‐Threatening Behavior, 36(5), 533–538. 10.1521/suli.2006.36.5.533 [DOI] [PubMed] [Google Scholar]
- Ayub, N. (2008). Validation of the Urdu translation of the Beck Scale for Suicide Ideation. Assessment, 15(3), 287–293. 10.1177/1073191107312240. 10.1177/1073191107312240 [DOI] [PubMed] [Google Scholar]
- Beavers, A. S. , Lounsbury, J. W. , Richards, J. K. , Huck, S. W. , Skolits, G. J. , & Esquivel, S. L. (2013). Practical considerations for using exploratory factor analysis in educational research. Practical Assessment, Research & Evaluation, 18(6), 1–13. http://doi.org/ISSN 1531–7714 [Google Scholar]
- Beck, A. T. , Brown, G. K. , & Steer, R. A. (1997). Psychometric characteristics of the Scale for suicide ideation with psychiatric outpatients. Behaviour Research and Therapy, 35(11), 1039–1046. 10.1016/S0005-7967(97)00073-9 [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Brown, G. K. , Steer, R. A. , Dahlsgaard, K. K. , & Grisham, J. R. (1999). Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide & Life‐Threatening Behavior, 29(1), 1–9. 10.1111/j.1943-278X.1999.tb00758.x [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Kovacs, M. , & Weissman, A. (1979). Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology, 47(2), 343–352. 10.1037/0022-006X.47.2.343 [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , & Steer, R. A. (1991). Manual for Beck Scale for Suicide Ideation. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck, A. T. , Steer, R. A. , & Ranieri, W. F. (1988). Scale for Suicide Ideation: psychometric properties of a self‐report version. Journal of Clinical Psychology, 44(4), 499–505. [DOI] [PubMed] [Google Scholar]
- Bernaards, C. A. , & Jennrich, R. I. (2005). Gradient projection algorithms and software for arbitrary rotation criteria in factor analysis. Educational and Psychological Measurement, 65, 676–696. 10.1177/0013164404272507 [DOI] [Google Scholar]
- Cattell, R. B. (1966). The scree test for the numbers of factors. Multivariate Behavioral Research, 1(2), 245–276. 10.1207/s15327906mbr0102 [DOI] [PubMed] [Google Scholar]
- Clum, G. A. , & Yang, B. (1995). Additional support for the reliability and validity of the modified Scale for Suicide Ideation. Psychological Assessment, 7(1), 122–125. 10.1037/1040-3590.7.1.122 [DOI] [Google Scholar]
- Conway, J. M. , & Huffcutt, A. I. (2003). A review and evaluation of Exploratory factor analysis practices in organizational research. Organizational Research Methods, 6(2), 147–168. 10.1177/1094428103251541 [DOI] [Google Scholar]
- Costello, A. B. , & Osborne, J. W. (2005). Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation, 10(7), 1–9. [Google Scholar]
- De Man, A. F. , Balkou, S. T. , & Iglesias, R. I. (1987). A French‐Canadian adaptation of the Scale for Suicide Ideation. Canadian Journal of Behavioural Science/Revue Canadienne Des Sciences Du Comportement, 19(1), 50–55. 10.1037/h0079870 [DOI] [Google Scholar]
- De Man, A. F. , Leduc, C. P. , & Labrèche‐Gauthier, L. (1993). A French‐Canadian scale for suicide ideation for use with adolescents. Canadian Journal of Behavioural Science/Revue Canadienne Des Sciences Du Comportement, 25(1), 126–134. 10.1037/h0078786 [DOI] [Google Scholar]
- Fabrigar, L. R. , Wegener, D. T. , MacCallum, R. C. , & Strahan, E. J. (1999). Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods, 4(3), 272–299. 10.1037/1082-989X.4.3.272 [DOI] [Google Scholar]
- Fox, J. (2016). Polycor: Polychoric and Polyserial Correlations. Retrieved from https://cran.r-project.org/package=polycor
- Fried, E. I. , & Nesse, R. M. (2015). Depression sum‐scores don't add up: Why analyzing specific depression symptoms is essential. BMC Medicine, 13(1), 72 10.1186/s12916-015-0325-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghasemi, P. , Shaghaghi, A. , & Allahverdipour, H. (2015). Measurement Scales of Suicidal Ideation and Attitudes: A systematic review article. Health Promotion Perspective, 5(3), 156–168. 10.15171/hpp.2015.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinkle, D. E. , Wiersma, W. , & Jurs, S. G. (2003). Applied statistics for the behavioral sciences (5th ed.). Boston: Houghton Mifflin. [Google Scholar]
- Holden, R. R. , & DeLisle, M. M. (2005). Factor analysis of the Beck Scale for Suicide Ideation with female suicide attempters. Assessment, 12(2), 231–238. 10.1177/1073191105274925 [DOI] [PubMed] [Google Scholar]
- Holi, M. M. , Pelkonen, M. , Karlsson, L. , Kiviruusu, O. , Ruuttu, T. , Heilä, H. , … Marttunen, M. (2005). Psychometric properties and clinical utility of the Scale for Suicidal Ideation (SSI) in adolescents. BMC Psychiatry, 5(1), 8 10.1186/1471-244X-5-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika, 30(2), 179–185. 10.1007/BF02289447 [DOI] [PubMed] [Google Scholar]
- Joiner, T. E. (2005). Why people die by suicide. Cambridge: Harvard University Press. [Google Scholar]
- Joiner, T. E. , Rudd, M. D. , & Rajab, M. H. (1997). The Modified Scale for Suicidal Ideation: Factors of suicidality and their relation to clinical and diagnostic variables. Journal of Abnormal Psychology, 106(2), 260–265. 10.1037/0021-843X.106.2.260 [DOI] [PubMed] [Google Scholar]
- Kaplan, M. L. , Asnis, G. M. , Sanderson, W. C. , Keswani, L. , de Lecuona, J. M. , & Joseph, S. (1994). Suicide assessment: Clinical interview vs. self‐report. Journal of Clinical Psychology, 50(2), 294–298. [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D. , & May, A. M. (2014). Differentiating suicide attempters from suicide ideators: A critical frontier for suicidology research. Suicide and Life‐threatening Behavior, 44(1), 1–5. 10.1111/sltb.12068 [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D. , Saffer, B. Y. , & Bryan, C. J. (2018). Ideation‐to‐action theories of suicide: a conceptual and empirical update. Current Opinion in Psychology, 22, 38–43. 10.1016/j.copsyc.2017.07.020 [DOI] [PubMed] [Google Scholar]
- Kodaka, M. , Poštuvan, V. , Inagaki, M. , & Yamada, M. (2011). A systematic review of scales that measure attitudes toward suicide. International Journal of Social Psychiatry, 57(4), 338–361. 10.1177/0020764009357399 [DOI] [PubMed] [Google Scholar]
- Korkmaz, S. , Goksuluk, D. , & Zararsiz, G. (2014). MVN: An R package for assessing multivariate normality. The R Journal, 6(2), 151–162. [Google Scholar]
- MacCallum, R. C. , Widaman, K. F. , Zhang, S. B. , & Hong, S. H. (1999). Sample size in factor analysis. Psychological Methods, 4(1), 84–99. 10.1037/1082-989x.4.1.84 [DOI] [Google Scholar]
- Maier, M. J. (2015). Companion package to the book “R: Einführung durch angewandte Statistik.” Retrieved from http://cran.r-project.org/package=REdaS [Google Scholar]
- Matsunaga, M. (2010). How to factor‐analyze your data right: Do's, don'ts, and how‐to's. International Journal of Psychological Research, 3(1), 97–110. 10.4090/juee.2008.v2n2.033040 [DOI] [Google Scholar]
- Miller, I. W. , Norman, W. H. , Bishop, S. B. , & Dow, M. G. (1986). The Modified Scale for Suicidal Ideation: Reliability and validity. Journal of Consulting and Clinical Psychology, 54(5), 724–725. 10.1037/0022-006X.54.5.724 [DOI] [PubMed] [Google Scholar]
- Nock, M. K. , Millner, A. J. , Joiner, T. E. , Gutierrez, P. M. , Han, G. , Hwang, I. , … Kessler, R. C. (2018). Risk factors for the transition from suicide ideation to suicide attempt: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Journal of Abnormal Psychology, 127(2), 139–149. 10.1037/abn0000317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor, R. C. , & Nock, M. K. (2014). The psychology of suicidal behaviour. The Lancet Psychiatry, 1(1), 73–85. 10.1016/S2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- Osborne, J. W. , & Fitzpatrick, D. C. (2012). Replication analysis in exploratory factor analysis: What it is and why it makes your analysis better. Practical Assessment, Research & Evaluation, 17(15), 1–8. [Google Scholar]
- Posner, K. , Oquendo, M. A. , Gould, M. , Stanley, B. , & Davies, M. (2007). Columbia Classification Algorithm of Suicide Assessment (C‐CASA): Classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. American Journal of Psychiatry, 164(7), 1035–1043. 10.1176/appi.ajp.164.7.1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2016). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Revelle, W. (2016). Psych: Procedures for personality and psychological research. Evanston, Illinois: Northwestern University. Retrieved from https://cran.r-project.org/package=psych
- Ribeiro, J. D. , Franklin, J. C. , Fox, K. R. , Bentley, K. H. , Kleiman, E. M. , Chang, B. P. , & Nock, M. K. (2016). Self‐injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta‐analysis of longitudinal studies. Psychological Medicine, 46(02), 225–236. 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio, J. , & Roche, B. (2012). Determining the number of factors to retain in an exploratory factor analysis using comparison data of known factorial structure. Psychological Assessment, 24(2), 282–292. http://doi.org/10/dhj3zz. 10.1037/a0025697 [DOI] [PubMed] [Google Scholar]
- Russ, M. J. , Kashdan, T. , Pollack, S. , & Bajmakovic‐Kacila, S. (1999). Assessment of suicide risk 24 hours after psychiatric hospital admission. Psychiatric Services, 50(11), 1491–1493. 10.1176/ps.50.11.1491 [DOI] [PubMed] [Google Scholar]
- Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. The Journal of Clinical Psychiatry, 59(Suppl 2), 22–33. quiz 34–57. Retrieved from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=9881538&retmode=ref&cmd=prlinks [PubMed] [Google Scholar]
- Silverman, M. M. , Berman, A. L. , Sanddal, N. D. , O'Carroll, P. W. , & Joiner, T. E. (2007a). Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide & Life‐Threatening Behavior, 37(3), 248–263. 10.1521/suli.2007.37.3.248 [DOI] [PubMed] [Google Scholar]
- Silverman, M. M. , Berman, A. L. , Sanddal, N. D. , O'Carroll, P. W. , & Joiner, T. E. (2007b). Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide‐related ideations, communications, and behaviors. Suicide & Life‐Threatening Behavior, 37(3), 264–277. 10.1521/suli.2007.37.3.264 [DOI] [PubMed] [Google Scholar]
- Steer, R. A. , Rissmiller, D. J. , Ranieri, W. F. , & Beck, A. T. (1993). Dimensions of suicidal ideation in psychiatric inpatients. Behaviour Research and Therapy, 31(2), 229–236. 10.1016/0005-7967(93)90090-H [DOI] [PubMed] [Google Scholar]
- Van Orden, K. A. , Witte, T. K. , Cukrowicz, K. C. , Braithwaite, S. R. , Selby, E. A. , & Joiner, T. E. (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte, T. K. , Joiner, T. E. , Brown, G. K. , Beck, A. T. , Beckman, A. , Duberstein, P. , & Conwell, Y. (2006). Factors of suicide ideation and their relation to clinical and other indicators in older adults. Journal of Affective Disorders, 94(1–3), 165–172. 10.1016/j.jad.2006.04.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1: Supporting Information
Data S2: Supporting Information


