Abstract
Objectives
Internet‐ and mobile‐based interventions (IMIs) offer the opportunity to deliver mental health treatments on a large scale. This randomized controlled trial evaluated the efficacy of an unguided IMI (StudiCare SAD) for university students with social anxiety disorder (SAD).
Methods
University students (N = 200) diagnosed with SAD were randomly assigned to an IMI or a waitlist control group (WLC) with full access to treatment as usual. StudiCare SAD consists of nine sessions. The primary outcome was SAD symptoms at posttreatment (10 weeks), assessed via the Social Phobia Scale (SPS) and the Social Interaction Anxiety Scale (SIAS). Secondary outcomes included depression, quality of life, fear of positive evaluation, general psychopathology, and interpersonal problems.
Results
Results indicated moderate to large effect sizes in favor of StudiCare SAD compared with WLC for SAD at posttest for the primary outcomes (SPS: d = 0.76; SIAS: d = 0.55, p < 0.001). Effects on all secondary outcomes were significant and in favor of the intervention group.
Conclusion
StudiCare SAD has proven effective in reducing SAD symptoms in university students. Providing IMIs may be a promising way to reach university students with SAD at an early stage with an effective treatment.
Keywords: internet‐based treatment, social anxiety disorder, unguided self‐help, university students
1. INTRODUCTION
Social anxiety disorder (SAD) is the most common anxiety disorder in the general population (Kessler, Chiu, Demler, & Walters, 2005). Prevalence estimates for SAD in university students show a wide range from 3.4% (12 months) in the United States (Blanco et al., 2008) to 16.1% (point prevalence) in Sweden (Tillfors & Furmark, 2007).
University students with SAD face a number of adverse effects including problems with identity formation (Gültekin & Dereboy, 2011), increased consumption of alcohol (Gilles, Turk, & Fresco, 2006), higher levels of suicidal ideation (Olfson, 2000), and lower quality of life (Mendlowicz, 2000). In addition, emotional distress due to SAD triggers dysfunctional avoidance strategies (Tillfors & Furmark, 2007), which are associated with underachievement and may lead to university dropout. The resulting lower qualification and social impairment (Kessler, 2003; Magee, Eaton, Wittchen, McGonagle, & Kessler, 1996) may subsequently lead to a high economic burden for those affected as well as for society at large. Thus, treatment of SAD is of interest to the public health care system and health services in and outside of the university setting (Wittchen & Jacobi, 2005; Wittchen, Jacobi, Rehm, & Gustavsson, 2011), particularly as SAD can manifest as a chronic condition when untreated (Chartier, Hazen, & Stein, 1998).
However, only a fraction of those in need (Runge, Beesdo, Lieb, & Wittchen, 2008; Wang et al., 2005) receive help. Reasons for this unmet need include shortage in available clinicians and fear of stigmatization. Furthermore, the fear of negative evaluation (FNE; Rapee & Heimberg, 1997; Stangier, Heidenreich, & Peitz, 2009), the expectation that others might judge one's behavior as embarrassing (Kessler, 2003; King & Poulos, 1998), a key feature of SAD, prevents university students from seeking professional advice (Kessler, 2003; King & Poulos, 1998).
Internet‐ and mobile‐based interventions (IMIs) are a promising strategy to overcome treatment barriers by offering a low‐access threshold, anonymous, flexible, and effective treatment option (Ebert, Cuijpers, Muñoz, & Baumeister, 2017; Griffiths, Lindenmeyer, Powell, Lowe, & Thorogood, 2006). IMIs have been shown to be effective in the treatment of a broad range of disorders (Ebert, Van Daele, et al., 2018b). The latest systematic review on IMIs for SAD found a mean standardized effect size of g = 0.84 (0.72–0.97) compared with untreated control groups and g = 0.38 (0.13–0.62) compared with active control conditions (Kampmann, Emmelkamp, & Morina, 2016).
Most studies to date that targeted SAD evaluated guided IMIs. However, once developed, costs of IMIs are substantially linked to professional guidance time, which clearly limits their possible reach and consequently lowers the potential to reduce the negative consequences of SAD at population level. Thus, in light of technological developments that allow them to mimic some functions of human support, unguided IMIs have received more attention. The most recent meta‐analysis found an average effect of g = 0.78 (95% confidence interval [CI] [0.50, 1.05]) for unguided IMIs compared with passive controls (n = 8) and of g = 0.19 (95% CI [−0.08, 0.46]) compared with active conditions (n = 7; Kampmann et al., 2016).
However, effect sizes of unguided treatment vary widely (95% CI [0.28, 1.47]; Berger et al., 2011; Botella et al., 2010; Furmark et al., 2009; Gallego, Emmelkamp, Maria, van der Kooij, & Mees, 2011; Lopez, Botella, Quero, Gomez, & Baños, 2014; Titov et al., 2010; Titov, Andrews, Choi, Schwencke, & Johnston, 2009; Titov, Andrews, Choi, Schwencke, & Mahoney, 2008) and high dropout >40% at posttreatment (Botella et al., 2010; Gallego et al., 2011). Therefore, additional research is needed to investigate the efficacy of unguided IMIs as treatment of SAD.
We are aware of two studies that evaluated internet‐based cognitive behavioral therapy (iCBT) for SAD in university students. A small open trial (n = 38) that delivered PDFs with self‐help material and offered minimal contact with a psychotherapist resulted in large pre–post within‐group effects (Social Interaction Anxiety Scale [SIAS]: d = 0.81; Social Phobia Scale [SPS]: d = 1.18) for both the iCBT group and the iCBT group with additional in vivo group exposure (Tillfors et al., 2008). Another unguided web‐based intervention that was personalized to each user's symptoms yielded smaller pre–post effect sizes in a non‐clinical sample of psychology students (e.g., SIAS: d = 0.72; McCall, Richardson, Helgadottir, & Chen, 2018).
Although the efficacy of cognitive behavioral therapy (CBT) in the treatment of SAD is well documented (Kampmann et al., 2016), there is still room for improvement. Recent findings suggest that FNEs are a central feature of SAD and document a strong link between SAD and the fear of positive evaluation (FPE; Hedman et al., 2011; Weeks, Heimberg, & Rodebaugh, 2008; Weeks, Heimberg, Rodebaugh, Goldin, & Gross, 2012). According to Weeks and Howell's (2012) bivalent fear of evaluation model of social phobia, fear of evaluation in general is the core component of SAD, including not only FNE but also FPE. Empirical evidence shows that FPE and FNE are related but distinct factors contributing to social anxiety, with FPE explaining a unique and independent proportion of variance in the fear of social interactions (Weeks, Jakatdar, & Heimberg, 2010). Even though established treatments for SAD do not address FPE directly, there is evidence that CBT can reduce FPE, albeit with smaller effect sizes compared with FNE (Weeks et al., 2012). Neglecting this component of SAD in the treatment may impede treatment progress, such as when clients still feel anxious after successful exposures that received positive feedback (Weeks & Howell, 2014). Even though research has shown that FPE is sensitive to CBT (Fergus et al., 2009), to our knowledge, no intervention exists that systematically addresses this as a treatment component of SAD. Thus, the intervention used in our study was enhanced by one module on FPE.
The current study evaluated whether an unguided internet‐based intervention complemented by one module on FPE is effective in treating SAD in university students when compared with a waitlist control group (WLC). This study is part of the recently launched World Health Organization World Mental Health Surveys International College Student Project (WMH‐ICS; http://www.hcp.med.harvard.edu/wmh/college_student_survey.php; Bruffaerts et al., 2018; Mortier et al., 2017). The WMH‐ICS was initiated to obtain accurate longitudinal data on the prevalence and correlates of mental disorders among university students, assess unmet needs for treatment, evaluate a wide range of interventions (a number of them developed in the context of WMH‐ICS) to prevent and treat these disorders, and develop precision medicine clinical decision support tools to match the right students to the most appropriate treatments.
2. METHODS
2.1. Design and procedure
Using a two‐arm randomized controlled design, N = 200 participants were randomly allocated (block size of 8, varying ratio) to an internet‐based unguided CBT (n = 100) or to a 6‐month WLC group (n = 100). Both groups had full access to treatment as usual. Randomization was performed using an internet‐based randomization program (Randlist) and carried out by an independent researcher not otherwise involved in the study. All questionnaires were assessed online at baseline (T0), 10 weeks (T1, posttreatment), and 6 months (T2) after randomization. The WLC group received access to the intervention following T2. In this study, we only report pretreatment and posttreatment data. The trial was registered at the German Clinical Trials Register (DRKS00011424). More details on the study design can be found in the study protocol (Kählke et al., 2018). All procedures involved in the study were consistent with the generally accepted standards of ethical practice and were approved by the ethical committee of the University of Erlangen–Nuremberg (reference number 260_16 B, 13.09.2016).
2.2. Participants
Participants had to be at least 18 years of age, enrolled as university students, scoring above predefined cutoff scores on the SPS (>21) or SIAS (>32), and meeting diagnostic criteria of SAD according to the Structured Clinical Interview for DSM‐IV Axis I Disorders. The interviews were conducted by trained interviewers via telephone (Rohde, Lewinsohn, & Seeley, 1997). Interrater reliability was evaluated in 20% of randomly selected cases. Cohen's kappa was κ = 0.78, which indicates good agreement across raters (Landis & Koch, 1977).
We excluded applicants who were either at risk of suicide (Beck Suicide Item > 1) or receiving psychotherapy at the time of entering the study or had a known diagnosis of a psychotic, bipolar, or another severe mental disorder. Prescription medications for anxiety and depression lead to an exclusion if the dosage had changed within 1 month before the beginning of the study. Participants were recruited in Germany, Austria, and Switzerland from January 2017 to February 2018 primarily through circular e‐mails sent to enrolled students at a number of German, Austrian, and Swiss universities.
2.3. Intervention
The intervention is based on the cognitive behavioral treatment model for social phobia by Clark and Wells (1995). This model has been shown to be efficacious in previous studies in general population samples (Berger et al., 2011; Berger, Hohl, & Caspar, 2009, 2010; Boettcher, Berger, & Renneberg, 2012; A. Schulz et al., 2016; Stolz et al., 2018). The original intervention was specifically adapted to the university setting, for example, by providing case examples of socially anxious students. The intervention consisted of nine text‐based sessions, various exercises (e.g., attention training), and diaries (such as a diary aimed to identify and challenge negative thoughts). Participants were asked to work on one session weekly, to revise the exercises, and to fill in the diaries. The approximate time required to complete one session was 60 min plus the time required to implement treatment strategies in their daily life routine.
The first three intervention sections are composed of motivational enhancement (Session 1), psycho‐education (Session 2), and identification and modification of negative thoughts through a thought diary (Session 3). The fourth session consists of a module not in the original Clark and Wells model that teaches participants how to identify and modify FPE‐related cognitions (Session 4). This module provides information on the definition and etiology of FPE regarding the bivalent fear of evaluation model (Weeks & Howell, 2012), the evolutionary model (Gilbert, 2014), and FPE‐related cognitive strategies such as the disqualification of positive social outcomes. Identification and modification of FPE‐related cognitions as well as perceived costs and advantages of positive evaluation are supported by a thought diary and complemented by exercises that facilitate self‐compassion and the experience and acceptance of positive emotions, both of which have been linked to a reduction of FPE (Werner, Goldin, Ball, Heimberg, & Gross, 2011). In Sessions 5–7, participants are then introduced to exercises to reduce self‐focused attention, including behavioral experiments such as in vivo exposures. Session 8 includes information about healthy lifestyle (e.g., sports and nutrition) and conveyed problem solving skills. Finally, Session 9 provides strategies to maintain the acquired skills and to prepare for relapses.
Although the intervention does not include any therapeutic guidance, participants receive standardized automatic messages aiming to promote adherence. Adherence reminders follow procedures used in a number of previously conducted studies (Ebert et al., 2016; Ebert, Buntrock, et al., 2018; Zarski et al., 2016) consisting of one positive reinforcement per session completion and one automatic reminder if participants do not log into the platform for more than one week. These automated reminders contain standardized motivational messages that encourage participants to continue to work with the program. A more detailed description of the StudiCare SAD can be found in the protocol of the trial (Kählke et al., 2018).
2.4. Primary outcome measures
The primary outcome measures assess SAD symptoms with the SPS and the SIAS (Stangier, Heidenreich, Berardi, Golbs, & Hoyer, 1999). These two self‐report questionnaires complement one another and are usually administered together. The SIAS assesses more general fears of social interaction (e.g., “I tense up if I meet an acquaintance in the street”), whereas the SPS focuses on fears of being judged by others during daily activities (e.g., “I become anxious if I have to write in front of others.”). Each scale consists of 20 items rated on a 5‐point Likert scale (0 = “not at all” to 4 = “extremely”). These two measures have been found to be valid, reliable, and useful for clinical and research purposes (Mattick & Clarke, 1998). Cronbach's α for the SIAS and SPS ranges from 0.90 to 0.94 (Heinrichs et al., 2002). In the present study, Cronbach's α at T1 was 0.91 for the SPS and 0.92 for the SIAS.
2.5. Secondary outcome measures
Fear of positive social feedback was assessed using the Fear of Positive Evaluation Scale (FPES; Weeks, Heimberg, Rodebaugh, & Norton, 2008). The FPES is a self‐report instrument, which consists of 10 items and has shown good psychometric properties in clinical and healthy samples (Fergus et al., 2009; Weeks, Heimberg, Rodebaugh, & Norton, 2008). The disqualification of positive social outcomes is a cognitive strategy that has been related to FPE (Weeks, Heimberg, Rodebaugh, & Norton, 2008; Weeks & Howell, 2012). This cognitive tendency is assumed to represent a mental safety behavior in the context of FPE and was measured using the Disqualification of Positive Social Outcomes Scale (DPSOS; Weeks, 2010). The DPSOS comprises 13 items and measures disqualification of positive outcomes towards other‐oriented and self‐oriented attributions. Cronbach's α in the current sample for FPE was 0.78, and for DPSOS, it was 0.91.
Depression severity was assessed using the Beck Depression Inventory II (Hautzinger, Keller, & Kühner, 2006). The scale consists of 21 items each rated on a 4‐point Likert scale. Prior research has shown high reliability and validity in SAD clients (Berger et al., 2011). Cronbach's α in the present study was 0.89.
General psychopathology was assessed using the Brief Symptom Inventory, which spans nine dimensions, including insecurity in social situations, anxiety, depressiveness, and compulsivity (Franke, 2000). The Brief Symptom Inventory assesses symptoms within the past week and has shown robust psychometric properties (Schlarb & Hautzinger, 2011). Cronbach's α in the current sample was 0.96.
The Liebowitz Social Anxiety Scale (Liebowitz, 1987; Stangier & Heidenreich, 2003) assesses self‐reported fear and avoidance in 24 different situations. Thirteen of the situations relate to performance and the remaining items to situations within the context of social interactions. Prior research has shown good to excellent reliability and validity (Stangier & Heidenreich, 2003). In this study, Cronbach's α was 0.95.
Difficulties in interpersonal behavior and causes of relational distress as indicated assertiveness and passivity of participants were assessed using the Inventory of Interpersonal Problems. The instrument has eight dimensions and shown adequate psychometric properties (Horowitz, Rosenberg, Baer, Ureño, & Al, 1988; Horowitz, Strauß, & Kordy, 2000). Cronbach's α in the present study was 0.94.
The Assessment of Quality of Life (AQoL; Richardson, Iezzi, Khan, & Maxwell, 2014) measured quality of life. The AQoL‐8D comprises 35 items on eight dimensions (independent living, pain, senses, mental health, happiness, coping, relationships, and self‐worth) and allows for the calculation of separate sum scores for each dimension. The AQoL is a reliable and valid instrument (Richardson et al., 2014; Cronbach's α = 0.96). In this sample α was 0.93.
The German Client Satisfaction Questionnaire (Schmidt, Lamprecht, & Wittmann, 1989) adapted to the online training context was administered to examine the acceptance of internet‐based interventions and global client satisfaction on the intervention (Boß et al., 2016).
2.6. Sample size calculation
The study was powered to detect small to medium effect sizes of d = 0.4 between the conditions in the intention‐to‐treat (ITT) analysis, using a one‐sided test, with 80% power, adjusted for multiple testing due to two primary outcome tests. Hence, 100 participants were included per condition.
2.7. Statistical analyses
All analyses are reported according to the Consolidated Standards of Reporting Trials statement (K. F. Schulz, Altman, & Moher, 2010) using ITT procedures. Additionally, study completer, that is, including only those that provided data at follow‐up, were reported as sensitivity analysis. Analyses were performed using IBM SPSS version 25 (IBM SPSS, 2017). Multiple imputation using a Markov chain Monte Carlo multivariate imputation algorithm was used to handle missing data (Little & Rubin, 2002). Ten single estimations of the missing values were calculated based on the valid data for all available data at all assessment points (T0 and T1).
The intervention group (IG) and WLC were compared at 10 weeks (T1) using analysis of covariance (ANCOVA) with baseline levels as covariates. The primary outcome analyses were adjusted for multiple testing; hence, α was set at <0.025 for the primary outcome tests and <0.05 for all other tests. Cohen's d with 95% CIs was calculated based on the imputed dataset by comparing the means and SDs of the IG and WLC groups at posttest. According to Cohen (1988), d = 0.2 can be considered a small effect, d = 0.5 a medium effect, and d = 0.8 a large effect.
To determine the numbers of participants achieving a reliable, positive outcome, we coded participants as responders or non‐responders according to the widely used Reliable Change Index of Jacobson and Truax (1991) using the following formula: 1.96 × SD × sqrt(2) × sqrt(1 − rel). Therefore, we used the standard deviation of the whole sample at T0 (SD SPS = 12.68, SD SIAS = 12.16) and the retest reliability of the SPS (r tt = 0.96) and SIAS (r tt = 0.92) according to the test authors (Stangier et al., 1999). The participants were defined as having reliably changed if their SPS score differed more than (−)7.03 points and their SIAS score more than (−)9.53 points from T0 to T1. To investigate potential negative effects on individual level, we also calculated the number of participants that displayed a reliable symptom deterioration from baseline to posttreatment (+7.03) using the Reliable Change Index.
Participants were rated as symptom‐free if they scored 17 or below on the SPS and 26 or below on the SIAS (Stangier et al., 1999). Additionally, the numbers needed to treat (NNT), indicating the number of participants that have to be treated to generate one additional treatment response/symptom‐free status as compared with the control group, were calculated (Altman, 1998; Cook & Sackett, 1995).
3. RESULTS
3.1. Participants
A total of 603 individuals were screened for eligibility, and 387 were excluded primarily because they either scored below the cutoff (109/603) or because of a lack of informed consent/baseline (175/603). Subsequently, 16 participants were excluded due to no SAD diagnosis (n = 10), other mental disorders that require treatment (n = 5), and suicidal ideation (n = 16). Overall, 7.5% (n = 15) of participants did not provide data at T1. No significant differences were found between the IG (n = 9, 9%) and WLC (n = 6, 6%) with regard to missing data, χ 2(1) = 0.649, p = 0.421. The study flow is illustrated in Figure 1.
Figure 1.
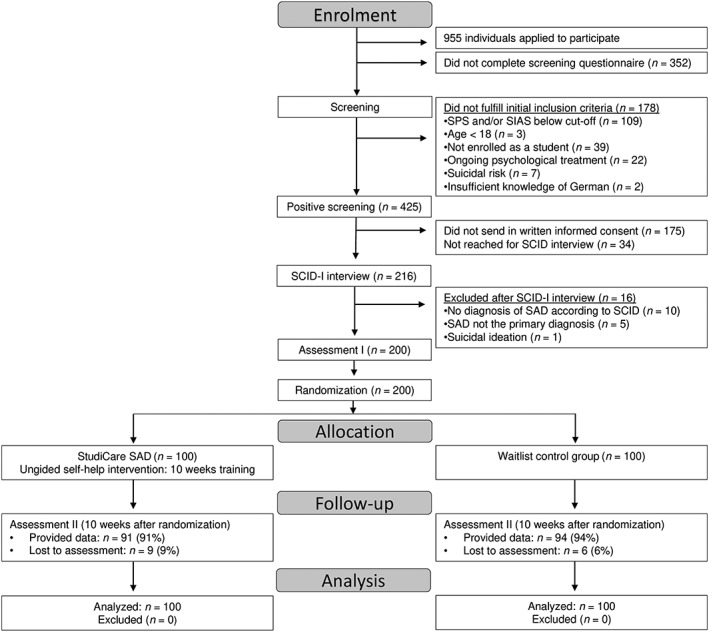
Flow of participants. SPS: Social Phobia Scale; SIAS: Social Interaction Anxiety Scale; SAD: social anxiety disorder; SCID‐I: Structured Clinical Interview for DSM‐IV Axis I Disorders
Baseline socio‐demographic and clinical characteristics were balanced across groups and are displayed in Table 1. The average age of the participants was 26.70 years (SD = 6.34). The sample was primarily female (124/200, 62%) and consisted mostly of full‐time students (n = 170, 85%), who were related to medical fields (n = 77, 39.1%). Half of them were married or in a relationship (n = 102, 51.0%). Having received psychotherapy in the past was endorsed by 68 persons (34.0%). Table 2 summarizes all means and SDs for all outcome measures.
Table 1.
Baseline sample characteristics
| Characteristic | All participants (N = 200) | IG (n = 100) | WLC (n = 100) |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Sociodemographic characteristics | |||
| Age (M, SD) | 26.70 (6.34) | 26.71 (6.08) | 26.68 (6.61) |
| Gender, female | 124 (62.0%) | 63 (63.0%) | 61 (61.0%) |
| Married or in a relationship | 102 (51.0%) | 52 (52.0%) | 50 (50.0%) |
| Citizenship | |||
| Germany | 150 (75.0%) | 74 (74.0%) | 76 (76.0%) |
| Switzerland | 40 (20.0%) | 21 (21.0%) | 19 (19.0%) |
| EEA member | 3 (1.5%) | 1 (1.0%) | 2 (2.0%) |
| No EEA member | 7 (3.5%) | 4 (4.0%) | 3 (3.0%) |
| Study characteristics | |||
| Full‐time student | 170 (85.0%) | 86 (86.0%) | 84 (84.0%) |
| Part‐time student | 30 (15.0%) | 14 (14.0%) | 16 (16.0%) |
| Semester (M, SD) | 5.09 (3.38) | 4.65 (3.15) | 5.53 (3.56) |
| Taking less classes due to SAD | 40 (20.0%) | 15 (15.0%) | 25 (25.0%) |
| ECTS taken less on average (M, SD) | 2.14 (5.73) | 1.49 (4.97) | 2.79 (6.36) |
| Field of study | |||
| Psychology | 53 (26.9%) | 33 (33.3%) | 20 (20.4%) |
| Medicine & Pharmaceutics | 24 (12.2%) | 9 (9.1%) | 15 (15.3%) |
| Business & Law | 35 (17.8%) | 16 (16.2%) | 19 (19.4%) |
| Literature & Media | 8 (4.1%) | 2 (2.0%) | 6 (6.1%) |
| Educational sciences | 13 (6.6%) | 4 (4.0%) | 9 (9.2%) |
| Engineering | 30 (15.2%) | 18 (18.2%) | 12 (12.2%) |
| Linguistics, culture, and social studies | 15 (7.6%) | 10 (10.1%) | 5 (5.1%) |
| Mathematics and other sciences | 19 (9.6%) | 7 (7.1%) | 12 (12.2%) |
| Work characteristics | |||
| Employed | 106 (53.0%) | 58 (58.0%) | 48 (48.0%) |
| Full‐time employed | 17 (8.5%) | 9 (9.0%) | 8 (8.0%) |
| Chronic conditions | |||
| Any chronic condition | 127 (64.0%) | 66 (66.0%) | 61 (61.0%) |
| Treatment utilization | |||
| Previous psychotherapy | 68 (34.0%) | 38 (38.0%) | 30 (30.0%) |
| Medication at T0 | 5 (2.5%) | 3 (3.0%) | 2 (2.0%) |
Note. ECTS: European Credit Transfer System; EEA: European Economic Area; SAD: social anxiety disorder.
Table 2.
Means and standard deviations for the IG and the WLC groups (ITT sample)
| T0 | T1a | |||||||
|---|---|---|---|---|---|---|---|---|
| IG | WLC | IG | WLC | |||||
| Outcome | M | SD | M | SD | M | SD | M | SD |
| Primary outcome | ||||||||
| SPS | 34.36 | 11.79 | 35.71 | 13.54 | 21.03 | 11.54 | 30.63 | 13.72 |
| SIAS | 51.47 | 11.23 | 48.71 | 12.92 | 36.72 | 13.86 | 44.36 | 14.05 |
| Secondary outcome | ||||||||
| BDI‐II | 12.68 | 8.23 | 12.97 | 7.71 | 8.12 | 6.71 | 11.88 | 8.16 |
| BSI | 0.86 | 0.49 | 0.92 | 0.56 | 0.56 | 0.40 | 0.81 | 0.57 |
| LSAS | 77.61 | 16.87 | 76.96 | 19.57 | 58.82 | 20.45 | 72.51 | 22.17 |
| IIP‐64 | 1.71 | 0.39 | 1.66 | 0.43 | 1.34 | 0.47 | 1.5 | 0.48 |
| FPES | 43.82 | 11.00 | 39.90 | 13.00 | 36.17 | 13.49 | 39.95 | 14.6 |
| DPSOS‐Self | 16.76 | 4.91 | 15.85 | 5.68 | 14.35 | 5.42 | 16.06 | 5.89 |
| DPSOS‐Others | 42.51 | 11.93 | 40.16 | 12.56 | 36.11 | 14.81 | 40.60 | 14.81 |
| AQoL | 0.57 | 0.14 | 0.58 | 0.17 | 0.68 | 0.16 | 0.61 | 0.18 |
| CSQ‐8 | — | — | — | — | 25.15 | 3.77 | — | — |
Note. M: means; SD: standard deviations; IG: intervention group; WTL: waitlist control group; ITT: intention‐to‐treat; SPS: Social Phobia Scale; SIAS: Social Interaction Anxiety Scale; BDI‐II: Beck Depression Inventory II; BSI: Brief Symptom Inventory; LSAS: Liebowitz Social Anxiety Scale; IIP‐64: Inventory of Interpersonal Problems; FPES: Fear of Positive Evaluation Scale; DPSOS: Disqualification of Positive Social Outcomes Scale; AQoL: Assessment of Quality of Life; CSQ‐8: Client Satisfaction Questionnaire.
Missing data imputed by multiple imputation.
The most common reason that participants indicated why they applied for participation in the internet‐based treatment was that they found an internet‐based intervention easier to integrate into daily life than an regular outpatient therapy (63.5%, n = 127) followed by a general interest in such a new treatment approach (56%, n = 112). Approximately one third (34.5%, n = 69) indicated that they were not willing to use any outpatient face‐to‐face psychotherapy. Only one fifth (20%, n = 43) of the participants stated that the most important reason for getting involved in the study was that waiting times for psychological therapy were too long. Only the minority of the participants were unsatisfied with former treatment (10.5%, n = 21) or indicated a limited access to treatment (2%, n = 4).
3.2. Treatment adherence and other treatment
On average, participants in the IG completed 5.18 (SD = 2.65) of the nine sessions (58% of the intervention). Of the 100 individuals participating in the IG, Session 1 was completed by 96 of the participants (96%), Session 2 by 92 (92%), Session 3 by 85 (85%), Session 4 by 71 (71%), Session 5 by 58 (58%), Session 6 by 40 (40%), Session 7 by 31 (31%), Session 8 by 24 (24%), and Session 9 by 21 (21%) of the participants.
In the WLC condition, three participants (3.0%) indicated at T1 that they had received other help within the previous 10 weeks (e.g., psychotherapy and health training other than the StudiCare SAD) as opposed to two participants (2.0%) in the IG condition.
3.3. Primary outcome analyses
3.3.1. Intervention effect
Changes from baseline to posttest in the IG were large for both primary outcomes according to Cohen's criteria (SPS: d = 1.14, 95% CI [0.84, 1.44]; SIAS: d = 1.17, 95% CI [0.87, 1.47]), whereas within‐group changes in the WLC were small to moderate (SPS: d = 0.37, 95% CI [0.09, 0.65]; SIAS: d = 0.32, 95% CI [0.04, 0.6]).
As shown in Table 3, a significant group effect in the ANCOVA indicated lower scores on both primary outcome measures for the IG relatively to the WLC at T1, SPS: F(1, 197) = 94.65, p < 0.001; SIAS: F(1, 197) = 122.51, p < 0.001. Effect sizes for differences between the groups were moderate for the SIAS (d = 0.55, 95% CI [0.27, 0.83]) and moderate to large for the SPS (d = 0.76, 95% CI [0.47, 1.04]).
Table 3.
Results of the ANCOVAs and Cohen's d for the primary and secondary outcome measures (ITT sample) at posttest (T1)
| T1 between‐groups effect | T1 within‐group effect | |||
|---|---|---|---|---|
| d (95% CI) | ANCOVAa | |||
| Outcome | F(1, 197) | p | ||
| Primary outcome | ||||
| SIAS | 0.55 [0.83, 0.27] | 46.22 | <0.001 | 1.17 [0.87, 1.47] |
| SPS | 0.76 [0.47, 1.04] | 40.30 | <0.001 | 1.14 [0.84, 1.44] |
| Secondary outcome | ||||
| BDI‐II | 0.50 [0.22, 0.78] | 16.77 | <0.001 | 0.61 [0.32, 0.89] |
| BSI | 0.49 [0.21, 0.77] | 16.66 | <0.001 | 0.66 [0.37, 0.94] |
| LSAS | 0.64 [0.36, 0.92] | 15.71 | <0.001 | 1.00 [0.70, 1.29] |
| IIP‐64 | 0.34 [0.06, 0.61] | 16.55 | <0.001 | 0.86 [0.56, 1.14] |
| FPES | 0.27 [0.01, 0.55] | 16.66 | <0.001 | 0.62 [0.34, 0.90] |
| DPSOS‐Self | 0.30 [0.02, 0.58] | 12.56 | <0.001 | 0.47 [0.18, 0.74] |
| DPSOS‐Others | 0.30 [0.02, 0.58] | 12.58 | <0.001 | 0.48 [0.19, 0.75] |
| AQoL | 0.41 [0.13, 0.69] | 19.45 | <0.001 | 0.73 [0.44, 1.01] |
Note. ANCOVA: analysis of covariance; ITT: intention‐to‐treat; SPS: Social Phobia Scale; SIAS: Social Interaction Anxiety Scale; BDI‐II: Beck Depression Inventory II; BSI: Brief Symptom Inventory; LSAS: Liebowitz Social Anxiety Scale; IIP‐64: Inventory of Interpersonal Problems; FPES: Fear of Positive Evaluation Scale; DPSOS: Disqualification of Positive Social Outcomes Scale; AQoL: Assessment of Quality of Life.
Controlling for pretreatment scores (T0).
3.3.2. Treatment response, symptom‐free status and symptom deterioration
At T1, more participants in the IG showed reliable improvement compared with those in the WLC based on both the SPS (IG: n = 68, 68%; WLC: n = 32, 32%), χ 2(1) = 25.92, p < 0.001, NNT: 2.78, 95% CI [2.04, 4.33], and the SIAS (IG: n = 60, 60%; WLC: n = 24, 24%), χ 2(1) = 26.60, p < 0.001, NNT: 2.78, 95% CI [2.05, 4.30].
Compared with WLC, more participants in the IG met the symptom‐free criterion at T1 (IG: n = 43, 43%; WLC: n = 19, 19%), χ 2(1) = 13.46, p = 0.0155, NNT = 4.17, 95% CI [2.75, 8.61], on both the SPS and the SIAS (IG: n = 24, 24%; WLC: n = 11, 11%), χ 2(1) = 5.85, p < 0.001, NNT = 7.70, 95% CI [4.28, 38.12].
At T1, fewer participants in the IG showed reliable deterioration compared with those in the WLC based on both the SPS (IG: n = 12, 12%; WLC: n = 20, 20%), χ 2(1) = 2.38, p = 0.12, and the SIAS (IG: n = 10, 10%; WLC: n = 18, 18%), χ 2(1) = 2.66, p = 0.10, although these differences did not reach statistical significance.
3.4. Secondary outcome analyses
Table 3 shows the results of the ITT analyses for the secondary outcomes, interpersonal problems, depression, somatic symptoms, FPE, and quality of life. The ANCOVAs showed significant between‐group effects on all outcomes at the postassessment point, with effect sizes ranging from d = 0.27 (95% CI [0.01, 0.55]) for the FPES to d = 0.64 (95% CI [0.36, 0.92]) for the Liebowitz Social Anxiety Scale.
3.4.1. Client satisfaction
Client satisfaction with the training was high, as 83% of the participants (n = 70) were “very or mostly satisfied” in general. Most of the participants in the IG group (82%, n = 69) rated the quality of the training as being “good” or “excellent.” The majority of the participants indicated that the training met “almost all” or “most” of their needs (79%, n = 66) and that they have received the kind of training they wanted (80%, n = 67; “yes, definitely” or “yes, generally”). Overall, they were satisfied with the amount of training they received (83%, n = 70; “very satisfied” or “mostly satisfied”), that the training has helped them “a great deal” or at least “helped” to deal more effectively with their problems (82%, n = 69), and that they would use the training again if needed (83%, n = 70; “yes, definitely” or “yes, I think so”). In closing, 88% (n = 74) of the participants would recommend the IMI to a friend (“yes, definitely” or “yes, I think so”).
3.4.2. Sensitivity analyses
Results of the study completers, including only those participants that provided data, were very similar to those of the ITT analysis, with significant effects on all assessed outcomes and effect sizes at least as large as in the ITT analysis for all outcomes. The between‐group effects were smallest for FPES (d = 0.25, 95% CI [−0.03, 0.53]) and highest for SPS (d = 0.72, 95% CI [0.43, 1.02]).
4. DISCUSSION
This study evaluated the efficacy of an internet‐based unguided self‐help intervention for university students with SAD. We found moderate to large effects on social anxiety symptoms for the IG compared with the WLC. The intervention also showed significant effects on all secondary outcome measures including FPE, depression, and quality of life, thus providing evidence for unguided internet‐based self‐help as an effective format to treat SAD in university students.
The effects found in the present study are in line with the few previous studies targeting SAD symptoms in university students. The only other study on unguided self‐help in a sample of students with a confirmed SAD diagnoses and fear of public speaking found significant effects compared with a WLC (Botella et al., 2010). A small pilot study (N = 38) on therapist guided self‐help found comparable effects for changes in SAD on the SPS (d = 1.18 vs. 1.14 in the present study) but somewhat smaller effects with regard to changes on the SIAS (d = 0.81 vs. d = 1.17 in the present study; Tillfors et al., 2008). Recently, McCall et al. (2018) reported somewhat smaller within‐group changes for unguided self‐help in a non‐clinical student sample with SAD symptoms (SIAS: d = 0.72), where between‐group effects were comparable with the present study (d = 0.56). However, the authors reported completer data only, and the dropout rate in the study was substantial (>35%).
Furthermore, the findings are in concordance with those found for unguided internet‐based self‐help for SAD in general population samples. The latest meta‐analysis on this topic found an average effect of g = 0.78 (95% CI [0.50, 1.05]; Kampmann et al., 2016), but with substantial heterogeneity between studies. Effects (d = 1.14–1.17, 95% CI [0.84, 1.46]) are also in the range of what is typically found for state‐of‐the‐art face‐to‐face CBT for SAD (Bandelow et al., 2015; d = 1.10, 95% CI [0.93, 1.28]).
Comparing effects on FPE with previous studies is not possible, as we are not aware of any other study that evaluated an intervention that directly targeted FPE. However, Weeks and colleagues reported large pre–post effects for face‐to‐face CBT that were not specifically targeting FPE. They found a reduction in FPE scores from baseline to posttreatment with a corresponding effect size of d = 1.38 (95% CI [1.24, 1.52]) compared with 0.62 (95% CI [0.34, 0.90]) in the present study. As we did not include a comparison condition without a module on FPE, it is not possible to conclude whether the additional FPE module had any incremental effect to the standard treatment, which should be tested in future studies.
Another important finding is that one third (34.5%) of the participants indicated that they would not be willing to utilize traditional available treatment formats such as face‐to‐face psychotherapy, further highlighting the potential of internet‐based treatments for reaching people who were previously not reached by the current health care system (Ebert, Van Daele, et al., 2018a). This finding is in line with studies on barriers of treatment utilization in university students that found attitudinal barriers, such as a preference for self‐help or fear of stigma, to be more relevant than structural barriers, such as non‐availability, high costs, or long waiting times, in both university students (Ebert, Mortier, et al., 2018) and general population samples (Andrade et al., 2014).
The study has a number of limitations: First, common in randomized trials, there were a small number of cases that did not provide data at follow‐up. However, missing data were handled using multiple imputations, and dropout was very low (IG: 9% and CG: 6% after 10 weeks). Therefore, it is unlikely that this has biased the results.
Second, one needs to keep in mind that the evidence provided by the present study is based on a randomized controlled trial (RCT) that is typically characterized by high structuring of participants and a high research attention. As the securing of participants' commitment represents an adherence‐promoting element in self‐help interventions, it may be the case that the effect sizes are an overestimation of what can be expected when implementing such an intervention into routine care. Hence, a clear concept for ensuring adherence in unguided self‐help under routine conditions, such as through minimal guidance, seems favorable (Ebert & Baumeister, 2017).
Third, the elaborated study inclusion process typical for an RCT (i.e., completion of two self‐report assessments and sending of informed consent) might have led to the greater inclusion of above‐average motivated students, than one could expect outside of the controlled research context. This is a common limitation of RCTs on psychological interventions but may have a particularly high impact on the results of trials on unguided interventions. As a result, the findings might not generalize to unguided self‐help without such an inclusion process.
Fourth, although findings clearly indicate that unguided internet‐based self‐help can result in substantial benefits for students with SAD, it may very well be the case that students are less willing to participate in such a mental health intervention if no support from a health care professional is provided, compared with interventions that include professional guidance. As the effect of any intervention depends on the utilization of the target population, lower overall effects at population level would result, if this should be the case. Thus, future studies should compare the acceptability of different guidance formats as well as the comparable effects at population level.
Finally, a WLC design with unrestricted access to treatment as usual has been chosen, which may cause some participants in the control condition being less motivated to initiate health‐related behavior changes and thus may overaccentuate effects (Ebert & Baumeister, 2017). Finally, follow‐up of the results at 6 months will provide information about the sustainability of our internet‐based approach.
This study demonstrated that StudiCare SAD is effective in treating SAD when compared with a waitlist control condition. Given the barriers of treatment utilization and high number of untreated university students, it would be worthwhile to integrate such IMIs into routine university health care. Future studies should focus on evaluating effects under routine care conditions.
FUNDING
This study is cofunded by the BARMER, a German statutory health insurance company. The funders did not have a role in study design, data collection, analysis, interpretation of results, or the decision to publish the study results.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved on 13.09.2016 by the Ethics Committee of the Friedrich‐Alexander‐Universität Erlangen‐Nürnberg (ref. no. 260_16 B, 13.09.2016). A written consent was obtained by all participants.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIAL
The dataset used in the present study is available from DDE.
DECLARATION OF INTEREST STATEMENT
D. D. E. reports to have received consultancy fees or served in the scientific advisory board from several companies such as Minddistrict, Sanofi, Lantern, Schön Kliniken, German health insurance companies (BARMER and Techniker Krankenkasse), and chambers of psychotherapists. D. D. E. and M. B. are also stakeholders of the Institute for health trainings online (GET.ON), which aims to implement scientific findings related to digital health interventions into routine care. H. B. reports to have received consultancy fees and fees for lectures or workshops from chambers of psychotherapists and training institutes for psychotherapists. In the past 3 years, R. C. K. received support for his epidemiological studies from Sanofi Aventis, was a consultant for Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, and Takeda, and served on an advisory board for the Johnson & Johnson Services, Inc., and Lake Nona Life Project. R. C. K. is a co‐owner of DataStat, Inc., a market research firm that carries out health care research.
AUTHORS' CONTRIBUTIONS
D. D. E. and H. B. obtained funding for this study. F. K., D. D. E., T. B., and A. S. have contributed to the study design. F. K. drafted the manuscript, supervised by D. D. E. All authors contributed to the further writing of the manuscript and interpretation of data. All authors read and approved the final manuscript.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the contribution of all participants, research assistants, therapists, and all others who contributed to our study.
Kählke F, Berger T, Schulz A, et al. Efficacy of an unguided internet‐based self‐help intervention for social anxiety disorder in university students: A randomized controlled trial. Int J Methods Psychiatr Res. 2019;28:e1766 10.1002/mpr.1766
REFERENCES
- Altman, D. G. (1998). Confidence intervals for the number needed to treat. BMJ, 317(7168), 1309–1312. 10.1136/bmj.317.7168.1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade, L. H. , Alonso, J. , Mneimneh, Z. , Wells, J. E. , Al‐Hamzawi, A. , Borges, G. , … Kessler, R. C. (2014). Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychological Medicine, 44(6), 1303–1317. 10.1017/S0033291713001943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandelow, B. , Reitt, M. , Rover, C. , Michaelis, S. , Gorlich, Y. , & Wedekind, D. (2015). Efficacy of treatments for anxiety disorders: A meta‐analysis. International Clinical Psychopharmacology, 30(4), 183–192. 10.1097/YIC.0000000000000078 [DOI] [PubMed] [Google Scholar]
- Berger, T. , Caspar, F. , Richardson, R. , Kneubühler, B. , Sutter, D. , & Andersson, G. (2011). Internet‐based treatment of social phobia: A randomized controlled trial comparing unguided with two types of guided self‐help. Behaviour Research and Therapy, 49(3), 158–169. 10.1016/j.brat.2010.12.007 [DOI] [PubMed] [Google Scholar]
- Berger, T. , Hohl, E. , & Caspar, F. (2009). Internet‐based treatment for social phobia: A randomized controlled trial. Journal of Clinical Psychology, 65(10), 1021–1035. 10.1002/jclp.20603 [DOI] [PubMed] [Google Scholar]
- Berger, T. , Hohl, E. , & Caspar, F. (2010). Internetbasierte Therapie der sozialen Phobie: Ergebnisse einer 6‐Monate‐Katamnese. Zeitschrift für Klinische Psychologie und Psychotherapie, 39(4), 217–221. 10.1026/1616-3443/a000050 [DOI] [Google Scholar]
- Blanco, C. , Okuda, M. , Wright, C. , Hasin, D. S. , Grant, B. F. , Liu, S.‐M. , & Olfson, M. (2008). Mental health of college students and their non–college‐attending peers. Archives of General Psychiatry, 65(12), 1429 10.1001/archpsyc.65.12.1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boettcher, J. , Berger, T. , & Renneberg, B. (2012). Does a pre‐treatment diagnostic interview affect the outcome of Internet‐based self‐help for social anxiety disorder? A randomized controlled trial. Behavioural and Cognitive Psychotherapy, 40(05), 513–528. 10.1017/s1352465812000501 [DOI] [PubMed] [Google Scholar]
- Boß, L. , Lehr, D. , Reis, D. , Vis, C. , Riper, H. , Berking, M. , & Ebert, D. D. (2016). Reliability and validity of assessing user satisfaction with web‐based health interventions. Journal of Medical Internet Research, 18(8), e234 10.2196/jmir.5952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botella, C. , Gallego, M. J. , Garcia‐Palacios, A. , Guillen, V. , Baños, R. M. , Quero, S. , & Alcañiz, M. (2010). An Internet‐based self‐help treatment for fear of public speaking: A controlled trial. Cyberpsychology, Behavior and Social Networking, 13(4), 407–421. 10.1089/cyber.2009.0224 [DOI] [PubMed] [Google Scholar]
- Bruffaerts, R. , Mortier, P. , Kiekens, G. , Auerbach, R. P. , Cuijpers, P. , Demyttenaere, K. , … Kessler, R. C. (2018). Mental health problems in college freshmen: Prevalence and academic functioning. Journal of Affective Disorders, 225, 97–103. 10.1016/j.jad.2017.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier, M. J. , Hazen, A. L. , & Stein, M. B. (1998). Lifetime patterns of social phobia: A retrospective study of the course of social phobia in a nonclinical population. Depression and Anxiety, 7(3), 113–121. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9656091. [DOI] [PubMed] [Google Scholar]
- Clark, D. , & Wells, A. (1995). A cognitive model of social phobia. New York: Guilford Press. [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Cook, R. J. , & Sackett, D. L. (1995). The number needed to treat: A clinically useful measure of treatment effect. BMJ, 310(6977), 452–454. 10.1136/bmj.310.6977.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert, D. D. , & Baumeister, H. (2017). Internet‐based self‐help interventions for depression in routine care. JAMA Psychiatry, 1(4), 205–215. 10.1001/jamapsychiatry.2017.1394 [DOI] [PubMed] [Google Scholar]
- Ebert, D. D. , Buntrock, C. , Lehr, D. , Smit, F. , Riper, H. , Baumeister, H. , … Berking, M. (2018). Effectiveness of web‐ and mobile‐based treatment of subthreshold depression with adherence‐focused guidance: A single‐blind randomized controlled trial. Behavior Therapy, 49(1), 71–83. 10.1016/j.beth.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Ebert, D. D. , Cuijpers, P. , Muñoz, R. F. , & Baumeister, H. (2017). Prevention of mental health disorders using internet‐ and mobile‐based interventions: A narrative review and recommendations for future research. Frontiers in Psychiatry, 8 10.3389/fpsyt.2017.00116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert, D. D. , Lehr, D. , Heber, E. , Riper, H. , Cuijpers, P. , & Berking, M. (2016). Internet‐ and mobile‐based stress management for employees with adherence‐focused guidance: Efficacy and mechanism of change. Scandinavian Journal of Work, Environment and Health, 42(5), 382–394. 10.5271/sjweh.3573 [DOI] [PubMed] [Google Scholar]
- Ebert, D. D. , Mortier, P. , Kaehlke, F. , Bruffaerts, R. , Baumeister, H. , Auerbach, R. P. , … Kessler, R. C. (2018). Barriers of mental health treatment utilization among first year college students: First cross‐national results from the WHO World Mental Health International College Student Initiative. [DOI] [PMC free article] [PubMed]
- Ebert, D. D. , Van Daele, T. , Nordgreen, T. , Karekla, M. , Compare, A. , Zarbo, C. , … Taylor, J. (2018a). Internet‐ and mobile‐based psychological interventions: Applications, efficacy, and potential for improving mental health. European Psychologist, 23, 167–187. 10.1027/1016-9040/a000318 [DOI] [Google Scholar]
- Ebert, D. D. , Van Daele, T. , Nordgreen, T. , Karekla, M. , Compare, A. , Zarbo, C. , … Taylor, J. (2018b). Internet‐ and mobile‐based psychological interventions: Applications, efficacy, and potential for improving mental health: A report of the EFPA E‐Health Taskforce. European Psychologist. Hogrefe Publishing, 23, 167–187. 10.1027/1016-9040/a000318 [DOI] [Google Scholar]
- Fergus, T. A. , Valentiner, D. P. , McGrath, P. B. , Stephenson, K. , Gier, S. , & Jencius, S. (2009). The Fear of Positive Evaluation Scale: Psychometric properties in a clinical sample. Journal of Anxiety Disorders, 23(8), 1177–1183. 10.1016/j.janxdis.2009.07.024 [DOI] [PubMed] [Google Scholar]
- Franke, G. (2000). BSI, Brief Symptom Inventory von L. R. Derogatis (Kurzform der SCL‐90‐R) ‐ deutsches Manual. Beltz Test GmbH .
- Furmark, T. , Carlbring, P. , Hedman, E. , Sonnenstein, A. , Clevberger, P. , Frykman, M. , … Andersson, G. (2009). Guided and unguided self‐help for social anxiety disorder: Randomised controlled trial. The British Journal of Psychiatry, 195, 440–447. 10.1192/bjp.bp.108.060996. [DOI] [PubMed] [Google Scholar]
- Gallego, M. J. , Emmelkamp, G. , Maria, P. , van der Kooij, M. , & Mees, H. (2011). The effects of a Dutch version of an Internet‐based treatment program for fear of public speaking: A controlled study. International Journal of Clinical and Health Psychology, 11(3), 459–472. Retrieved from http://www.redalyc.org/articulo.oa?id=33719289003 [Google Scholar]
- Gilbert, P. (2014). Evolutionary models: Practical and conceptual utility for the treatment and study of social anxiety disorder In The Wiley blackwell handbook of social anxiety disorder. Chichester: John Wiley & Sons, Ltd; 10.1002/9781118653920.ch2 [DOI] [Google Scholar]
- Gilles, D. M. , Turk, C. L. , & Fresco, D. M. (2006). Social anxiety, alcohol expectancies, and self‐efficacy as predictors of heavy drinking in college students. Addictive Behaviors, 31(3), 388–398. 10.1016/j.addbeh.2005.05.020 [DOI] [PubMed] [Google Scholar]
- Griffiths, F. , Lindenmeyer, A. , Powell, J. , Lowe, P. , & Thorogood, M. (2006). Why are health care interventions delivered over the Internet? A systematic review of the published literature. Journal of Medical Internet Research, 8(2), e10 10.2196/jmir.8.2.e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gültekin, B. K. , & Dereboy, F. (2011). The prevalence of social phobia, and its impact on quality of life, academic achievement, and identity formation in university students. Turk Psikiyatri Dergisi. Retrieved from http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L363008230%5Cnhttp://www.turkpsikiyatri.com/PDF/C22S3/en/150-158en.pdf%5Cnhttp://sfx.libis.be/sfxlcl3?sid=EMBASE&issn=13002163&id=doi:&atitle=The+prevalence+of+social+phobia%2C+and+i [PubMed]
- Hautzinger, M. , Keller, F. , & Kühner, C. (2006). Beck Depressions‐Inventar (BDI‐II). Frankfurt am Main: Harcourt Test Services. [Google Scholar]
- Hedman, E. , Andersson, G. , Ljótsson, B. , Andersson, E. , Rück, C. , Mörtberg, E. , & Lindefors, N. (2011). Internet‐based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non‐inferiority trial. PLoS One, 6(3), e18001 10.1371/journal.pone.0018001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrichs, N. , Hahlweg, K. , Fiegenbaum, W. , Frank, M. , Schroeder, B. , & von Witzleben, I. (2002). Validität und Reliabilität der Social Interaction Anxiety Scale (SIAS) und der Social Phobia Scale (SPS). Verhaltenstherapie, 12(1), 26–35. 10.1159/000056690 [DOI] [Google Scholar]
- Horowitz, L. , Rosenberg, S. E. , Baer, B. A. , Ureño, G. , & Al, E. (1988). Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology, 56(6), 885–892. 10.1037//0022-006x.56.6.885 [DOI] [PubMed] [Google Scholar]
- Horowitz, L. , Strauß, B. , & Kordy, H. (2000). Inventar zur Erfassung interpersonaler Probleme: IIP‐D; deutsche Version. Weinheim: Beltz. [PubMed] [Google Scholar]
- Jacobson, N. S. , & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. 10.1037//0022-006x.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kählke, F. , Berger, T. , Schulz, A. , Baumeister, H. , Berking, M. , Cuijpers, P. , … Ebert, D. D. (2018). Efficacy and cost‐effectiveness of an unguided, internet‐ and mobile‐based self‐help intervention for social anxiety disorder in university students: Protocol of a randomized controlled trial. Manuscript under Review. [DOI] [PMC free article] [PubMed]
- Kampmann, I. L. , Emmelkamp, P. M. G. , & Morina, N. (2016). Meta‐analysis of technology‐assisted interventions for social anxiety disorder. Journal of Anxiety Disorders, 42, 71–84. 10.1016/j.janxdis.2016.06.007 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. (2003). The impairments caused by social phobia in the general population: Implications for intervention. Acta Psychiatrica Scandinavica, 108(s417), 19–27. 10.1034/j.1600-0447.108.s417.2.x [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Chiu, W. T. , Demler, O. , & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12‐month DSM‐IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617 10.1001/archpsyc.62.6.617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, S. A. , & Poulos, S. T. (1998). Using the Internet to treat generalized social phobia and avoidant personality disorder. CyberPsychology and Behavior, 1(1), 29–36. 10.1089/cpb.1998.1.29 [DOI] [Google Scholar]
- Landis, J. R. , & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159 10.2307/2529310–174. [DOI] [PubMed] [Google Scholar]
- Liebowitz, M. (1987). Social phobia. Modern Problems of Pharmacopsychiatry, 22, 141–173. 10.1159/000414022 [DOI] [PubMed] [Google Scholar]
- Little, R. J. A. , & Rubin, D. B. (2002). Statistical analysis with missing data. Hoboken: John Wiley & Sons, Inc; 10.1002/9781119013563 [DOI] [Google Scholar]
- Lopez, G. C. , Botella, C. , Quero, S. , Gomez, A. R. , & Baños, R. (2014). Telepsychology program to treat public‐speaking anxiety among the Mexican population. Psicología Iberoamericana, 22, 45–55. [Google Scholar]
- Magee, W. J. , Eaton, W. W. , Wittchen, H.‐U. , McGonagle, K. A. , & Kessler, R. C. (1996). Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Archives of General Psychiatry, 53(2), 159–168. 10.1001/archpsyc.1996.01830020077009 [DOI] [PubMed] [Google Scholar]
- Mattick, R. P. , & Clarke, J. C. (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36(4), 455–470. 10.1016/S0005-7967(97)10031-6 [DOI] [PubMed] [Google Scholar]
- McCall, H. C. , Richardson, C. G. , Helgadottir, F. D. , & Chen, F. S. (2018). Evaluating a web‐based social anxiety intervention among university students: Randomized controlled trial. Journal of Medical Internet Research, 20 10.2196/jmir.8630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendlowicz, M. V. (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry, 157(5), 669–682. 10.1176/appi.ajp.157.5.669 [DOI] [PubMed] [Google Scholar]
- Mortier, P. , Demyttenaere, K. , Auerbach, R. P. , Cuijpers, P. , Green, J. G. , Kiekens, G. , … Bruffaerts, R. (2017). First onset of suicidal thoughts and behaviours in college. Journal of Affective Disorders, 207, 291–299. 10.1016/j.jad.2016.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson, M. (2000). Barriers to the treatment of social anxiety. American Journal of Psychiatry, 157(4), 521–527. 10.1176/appi.ajp.157.4.521 [DOI] [PubMed] [Google Scholar]
- Rapee, R. M. , & Heimberg, R. G. (1997). A cognitive‐behavioral model of anxiety in social phobia. Behaviour Research and Therapy, 35(8), 741–756. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9256517. 10.1016/S0005-7967(97)00022-3 [DOI] [PubMed] [Google Scholar]
- Richardson, J. , Iezzi, A. , Khan, M. A. , & Maxwell, A. (2014). Validity and reliability of the Assessment of Quality of Life (AQoL)‐8D multi‐attribute utility instrument. The Patient ‐ Patient‐Centered Outcomes Research, 7(1), 85–96. 10.1007/s40271-013-0036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde, P. , Lewinsohn, P. M. , & Seeley, J. R. (1997). Comparability of telephone and face‐to‐face interviews in assessing axis I and II disorders. American Journal of Psychiatry, 154(11), 1593–1598. 10.1176/ajp.154.11.1593 [DOI] [PubMed] [Google Scholar]
- Runge, A. J. , Beesdo, K. , Lieb, R. , & Wittchen, H.‐U. (2008). How frequent is psychotherapy utilisation by adolescents and young adults with anxiety disorders? Verhaltenstherapie, 18(1), 26–34. 10.1159/000113890 [DOI] [Google Scholar]
- Schlarb, A. , & Hautzinger, M. (2011). Klinisch‐psychiatrische Ratingskalen für das Kindes‐und Jugendalter. Göttingen: Hogrefe. [Google Scholar]
- Schmidt, J. , Lamprecht, F. , & Wittmann, W. (1989). Zufriedenheit mit der stationären Versorgung. Entwicklung eines Fragebogens und erste Validitätsuntersuchungen. Psychotherapie, Psychosomatik, Retrieved from http://cat.inist.fr/?aModele=afficheN&cpsidt=7320939 [PubMed]
- Schulz, A. , Stolz, T. , Vincent, A. , Krieger, T. , Andersson, G. , & Berger, T. (2016). A sorrow shared is a sorrow halved? A three‐arm randomized controlled trial comparing internet‐based clinician‐guided individual versus group treatment for social anxiety disorder. Behaviour Research and Therapy, 84, 14–26. 10.1016/j.brat.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Schulz, K. F. , Altman, D. G. , & Moher, D. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ, 340 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangier, U. , & Heidenreich, T. (2003). Die Liebowitz Soziale Angst‐Skala (LSAS) In Collegium Internationale Psychiatriae Scalarum (Ed.), Internationale Skalen für Psychiatrie. Göttingen: Hogrefe. [Google Scholar]
- Stangier, U. , Heidenreich, T. , Berardi, A. , Golbs, U. , & Hoyer, J. (1999). Die Erfassung sozialer Phobie durch die Social Interaction Anxiety Scale (SIAS) und die Social Phobia Scale (SPS). Zeitschrift F {ü} r Klinische Psychologie Und Psychotherapie, 28(1), 28–36. 10.1026//0084-5345.28.1.28 [DOI] [Google Scholar]
- Stangier, U. , Heidenreich, T. , & Peitz, M. (2009). Soziale Phobien: ein kognitiv‐verhaltenstherapeutisches Behandlungsmanual; mit CD‐ROM. Weinheim: Beltz. [Google Scholar]
- Stolz, T. , Schulz, A. , Krieger, T. , Vincent, A. , Urech, A. , Moser, C. , … Berger, T. (2018). A mobile app for social anxiety disorder: A three‐arm randomized controlled trial comparing mobile and PC‐based guided self‐help interventions. Journal of Consulting and Clinical Psychology, 86(6), 493–504. 10.1037/ccp0000301 [DOI] [PubMed] [Google Scholar]
- Tillfors, M. , Carlbring, P. , Furmark, T. , Lewenhaupt, S. , Spak, M. , Eriksson, A. , … Andersson, G. (2008). Treating university students with social phobia and public speaking fears: Internet delivered self‐help with or without live group exposure sessions. Depression and Anxiety, 25(8), 708–717. 10.1002/da.20416 [DOI] [PubMed] [Google Scholar]
- Tillfors, M. , & Furmark, T. (2007). Social phobia in Swedish university students: Prevalence, subgroups and avoidant behavior. Social Psychiatry and Psychiatric Epidemiology, 42(1), 79–86. 10.1007/s00127-006-0143-2 [DOI] [PubMed] [Google Scholar]
- Titov, N. , Andrews, G. , Choi, I. , Schwencke, G. , & Johnston, L. (2009). Randomized controlled trial of web‐based treatment of social phobia without clinician guidance. Australian & New Zealand Journal of Psychiatry, 43(10), 913–919. 10.1080/00048670903179160 [DOI] [Google Scholar]
- Titov, N. , Andrews, G. , Choi, I. , Schwencke, G. , & Mahoney, A. (2008). Shyness 3: Randomized controlled trial of guided versus unguided Internet‐based CBT for social phobia. The Australian and New Zealand Journal of Psychiatry, 42(12), 1030–1040. 10.1080/00048670802512107 [DOI] [PubMed] [Google Scholar]
- Titov, N. , Andrews, G. , Schwencke, G. , Robinson, E. , Peters, L. , & Spence, J. (2010). Randomized controlled trial of Internet cognitive behavioural treatment for social phobia with and without motivational enhancement strategies. The Australian and New Zealand Journal of Psychiatry, 44(10), 938–945. 10.3109/00048674.2010.493859 [DOI] [PubMed] [Google Scholar]
- Wang, P. S. , Berglund, P. , Olfson, M. , Pincus, H. A. , Wells, K. B. , & Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 603 10.1001/archpsyc.62.6.603–613. [DOI] [PubMed] [Google Scholar]
- Weeks, J. W. (2010). The Disqualification of Positive Social Outcomes Scale: A novel assessment of a long‐recognized cognitive tendency in social anxiety disorder. Journal of Anxiety Disorders, 24(8), 856–865. 10.1016/j.janxdis.2010.06.008 [DOI] [PubMed] [Google Scholar]
- Weeks, J. W. , Heimberg, R. G. , & Rodebaugh, T. L. (2008). The Fear of Positive Evaluation Scale: Assessing a proposed cognitive component of social anxiety. Journal of Anxiety Disorders, 22(1), 44–55. 10.1016/j.janxdis.2007.08.002 [DOI] [PubMed] [Google Scholar]
- Weeks, J. W. , Heimberg, R. G. , Rodebaugh, T. L. , Goldin, P. R. , & Gross, J. J. (2012). Psychometric evaluation of the Fear of Positive Evaluation Scale in patients with social anxiety disorder. Psychological Assessment, 24(2), 301–312. 10.1037/a0025723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks, J. W. , Heimberg, R. G. , Rodebaugh, T. L. , & Norton, P. J. (2008). Exploring the relationship between fear of positive evaluation and social anxiety. Journal of Anxiety Disorders, 22(3), 386–400. 10.1016/j.janxdis.2007.04.009 [DOI] [PubMed] [Google Scholar]
- Weeks, J. W. , & Howell, A. N. (2012). The bivalent fear of evaluation model of social anxiety: Further integrating findings on fears of positive and negative evaluation. Cognitive Behaviour Therapy, 41(2), 83–95. 10.1080/16506073.2012.661452 [DOI] [PubMed] [Google Scholar]
- Weeks, J. W. , & Howell, A. N. (2014). Fear of positive evaluation: The neglected fear domain in social anxiety In The Wiley Blackwell handbook of social anxiety disorder. John Wiley & Sons, Ltd; 10.1002/9781118653920.ch20 [DOI] [Google Scholar]
- Weeks, J. W. , Jakatdar, T. A. , & Heimberg, R. G. (2010). Comparing and contrasting fears of positive and negative evaluation as facets of social anxiety. Journal of Social and Clinical Psychology, 29(1), 68–94. 10.1521/jscp.2010.29.1.68 [DOI] [Google Scholar]
- Werner, K. H. , Goldin, P. R. , Ball, T. M. , Heimberg, R. G. , & Gross, J. J. (2011). Assessing emotion regulation in social anxiety disorder: The emotion regulation interview. Journal of Psychopathology and Behavioral Assessment, 33(3), 346–354. 10.1007/s10862-011-9225-x [DOI] [Google Scholar]
- Wittchen, H.‐U. , & Jacobi, F. (2005). Size and burden of mental disorders in Europe—A critical review and appraisal of 27 studies. European Neuropsychopharmacology, 15(4), 357–376. 10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]
- Wittchen, H.‐U. , Jacobi, F. , Rehm, J. , & Gustavsson, A. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21, 655–679. 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- Zarski, A.‐C. , Lehr, D. , Berking, M. , Riper, H. , Cuijpers, P. , & Ebert, D. D. (2016). Adherence to internet‐based mobile‐supported stress management: A pooled analysis of individual participant data from three randomized controlled trials. Journal of Medical Internet Research, 18(6), e146, 1–15. 10.2196/jmir.4493 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used in the present study is available from DDE.


