Abstract
Objectives
The current study aimed at evaluating the reliability, convergent and divergent validity, and factor structure of the Spanish Launay–Slade Hallucinations Scale‐Extended version (LSHS‐E) in people with mental disorders and healthy controls.
Methods
Four hundred and twenty‐two individuals completed the Spanish LSHS‐E and the Spanish Community Assessment of Psychic Experiences. The convergent and divergent validity of the LSHS‐E was assessed with the three dimensions of the Community Assessment of Psychic Experiences (positive, negative, and depressive dimensions) in healthy controls and people with a mental disorder. Factor structure of the LSHS‐E was assessed using confirmatory factor analysis and measurement invariance.
Results
The LSHS‐E had a good reliability in healthy controls and people with a mental disorder (Cronbach's = 0.83 and 0.91, respectively). The LSHS‐E was more strongly associated with positive psychotic‐like experiences than with depressive and negative symptoms. Four factors were found: (a) “intrusive thoughts”; (b) “vivid daydreams”; (c) “multisensory hallucination‐like experiences”; and (d) “auditory–visual hallucination‐like experiences” that were invariant between the group of healthy controls and people with a mental disorder.
Conclusion
The Spanish version of the LSHS‐E possesses adequate psychometric properties, and the confirmatory factor analysis findings provide further support for the multidimensionality of proneness to hallucination in clinical and nonclinical samples.
Keywords: factor analysis, hallucinatory proneness, Launay‐Slade Hallucination Scale, measurement invariance, sensitivity and specificity analyses
1. INTRODUCTION
Auditory hallucinations, and specifically auditory verbal hallucinations, are experienced by a large number of individuals diagnosed with psychosis, but they can also occur in other psychiatric diagnoses (Larøi et al., 2012; Sartorius, Shapiro, & Jablensky, 1974). A number of epidemiological studies support the notion that a significant minority of healthy individuals from the general population may also experience hallucinations in the absence of clear indicators of psychopathology (Beavan, Read, & Cartwright, 2011; Johns, 2005; Ochoa et al., 2008). For instance, one review (Beavan et al., 2011) has reported that the prevalence rate of voice‐hearers in the general population ranged from 0.6% to 84% (median: 13.2%). According to Beavan et al. (2011), gender and ethnic composition of the samples, methodological factors (including sample size and the tool used to assess the hallucinatory experiences), and other contextual factors might account for the large range in the prevalence of voice‐hearing in the community. In their review, Beavan et al. (2011) reported that auditory hallucinatory experiences seem to be more common in women and some non‐Western populations. In addition, these experiences may be underreported by some groups to avoid stigma discrimination. The most recent systematic review and meta‐analysis on the prevalence rates of auditory hallucinations in the general population identified 25 samples totalling 84,711 participants. Two samples were from Japan and an additional two were from African countries; all other samples were from Western countries (Maijer, Begemann, Palmen, Leucht, & Sommer, 2017). In the Maijer et al. (2017) review, children and adolescents were found to report similar lifetime prevalence rates (12.7% and 12.4%, respectively), but these were globally higher than those found in the adults (5.8%) and the elderly (4.5%).
Propensity to hallucinations is likely to be multidimensional, with factors affecting the occurrence of hallucinations proceeding from ipseity disturbances, such as thought pressure or block, perceptualization of mental stream, and spatialization of thoughts (Raballo & Larøi, 2011), enhanced imagination and propensity to vivid daydreams (Stephan‐Otto et al., 2017), the experience of nonparadigmatic hallucinations, such as those related to sleep‐hypnagogic and hypnopompic state (Waters et al., 2016), and hallucinations in one or multiple sensorial modalities.
The investigation of the multidimensionality of hallucination‐like experiences (HLEs) is important in order to explore how perceptual anomalies convert to more pathological aberrations before there is a psychotic change in the way in which the sensory world is perceived and understood by a subject (Stanghellini, 2011). There is some evidence that psychotic disorders begin with subthreshold HLEs combined with delusional ideation (Smeets, Lataster, van Winkel, et al., 2012), and studies have reported that the emergence of hallucinations (and auditory hallucinations in particular) precedes the formation of delusions in the development of psychosis (Escher, Romme, Buiks, Delespaul, & Van Os, 2002; Smeets, Lataster, Dominguez, et al., 2012; Smeets, Lataster, van Winkel, et al., 2012). Thus, the identification of these subthreshold HLEs at the very outset of their appearance would allow for preventative intervention by acting upon mentalizing abilities in these subjects, on the one hand, and working on self‐esteem and coping skills, on the other.
The Launay–Slade Hallucinations Scale (LSHS) is one of the most widely used tools to investigate the occurrence of HLEs in both clinical and nonclinical samples (Aleman, Nieuwenstein, Böcker, & De Haan, 2001, 1999; Bentall & Slade, 1985; Larøi, Marczewski, & Van der Linden, 2004; Launay & Slade, 1981; Serper, Dill, Chang, Kot, & Elliot, 2005; Siddi et al., 2017, 2016; Vellante et al., 2012). Over time, the LSHS has been repeatedly revised and improved. To account for different intensities of responding, the original binary choice (i.e., “true/false”; Launay & Slade, 1981) was replaced with a 5‐point Likert scale (Bentall & Slade, 1985). Thereafter, different authors have revised the item content of the scale (Larøi et al., 2004; Larøi & Van Der Linden, 2005; Morrison, Wells, & Nothard, 2000). For instance, Larøi and Van Der Linden (2005) reported an extended version (16 items) of the LSHS (LSHS‐E) that included items tapping into all major sensory modalities beyond the auditory modality, such as the visual, olfactory, and tactile. This version of the scale also included items on hypnagogic and hypnopompic hallucinations and on the experience of sensed presence (i.e., the experience of feeling the presence of someone close who has passed away). This study aimed at reporting the first validation study on the Spanish version of the LSHS‐E.
The LSHS was previously translated into Spanish (Fonseca‐Pedrero et al., 2010; García‐Montes, Pérez‐Álvarez, Soto Balbuena, Perona Garcelán, & Cangas, 2006), but using different versions from the LSHS‐E, and different populations (nonclinical and clinical). García‐Montes (2006) translated the version with true–false answers (Launay & Slade, 1981) and administrated it in clinical and nonclinical groups, whereas Fonseca‐Pedrero et al. (2010) validated the Spanish revised‐version with the Likert scale (Bentall & Slade, 1985) in a nonclinical group, also investigating the reliability and the factor structure of the scale. Because the LSHS‐E represents a substantial improvement with respect to the initial version of the LSHS in terms of coverage of hallucinatory experiences and of associated predisposing factors (e.g., vivid daydreams or intrusive thoughts), we think that a Spanish version of the LSHS‐E is worthwhile, as the ascertainment of its psychometric properties.
There is no agreed factor structure of the LSHS‐E. Larøi et al. (2004), working with a sample of college students, reported a four‐factor structure of the scale, characterized as representing (a) sleep‐related hallucinatory experiences; (b) vivid daydreams; (c) intrusive thoughts or realness of thought; and (d) auditory hallucinations. A five‐factor structure was also observed (Larøi & Van Der Linden, 2005), which consisted of the same four factors as those reported in the Larøi et al. (2004) study, albeit with an additional visual hallucinations factor. Finally, Vellante et al. (2012) also found (in a nonclinical sample) a four‐factor solution that did not completely overlap with the solution found by Larøi et al. (2004) and representing (a) auditory–visual HLEs; (b) multisensory HLEs; (c) intrusive thoughts; and (d) vivid daydreams. Furthermore, despite the globalization of research on the factor structure of the LSHS‐E, no previous study has explored the measurement invariance of this tool across clinical status. The establishment of measurement invariance is a prerequisite to comparing groups, because it provides evidence of whether respondents representing different clinical or sociocultural backgrounds interpret a given measure in a conceptually similar manner.
The aims of the present study were to (a) validate the LSHS‐E in a Spanish population; (b) explore the reliability, and the convergent, divergent, and the discriminant validity of the LSHS‐E; and (c) test the measurement invariance of the LSHS‐E in putatively healthy controls (HC) and people with a mental disorders.
2. METHODS
The competent institutional review boards approved the study protocol in accordance with the guidelines of the 1995 Declaration of Helsinki (as revised in Tokyo in 2004, and further revised in Fortaleza, Brazil, in 2013). The Parc Sant Joan de Déu research committee and the Sant Joan de Déu ethics committee approved the study (on 9 of July of 2014). A nonmonetary compensation for participation was offered to the participants from the general population. Participants who reported the same answers for all items were excluded.
2.1. Procedure
The study was carried out online, using the “Webropol survey” platform (https://www.webropolsurveys.com/). Participation was strictly anonymous. When participants accessed the online survey, they were first informed about the study and told that they could withdraw from the study at any time without penalty. People from the general population were invited via advertisements in social media (Facebook, Institutional websites, etc.) or via email invitations. When accessing the online survey, participants were asked to answer questions concerning their sociodemographic data (e.g., age, sex, and education) as well as their medical history (e.g., a psychiatric or neurological disorder diagnosis) and possible medication or psychological treatments received. They were required to exclude any experiences where they might have been under the effect of drugs or alcohol. Informed consent was obtained online from all participants in accordance with the requirements of the local department of data security and the local ethics committee (Sant Joan de Déu).
2.1.1. People with mental disorders
This group was composed of people with a verified psychiatric diagnosis and people who reported a psychiatric disorder in their lives. Inclusion criteria were age over 18 years old, having received a diagnosis psychosis or mood disorder and reporting a specific medication and psychological treatment for it, fluency in Spanish, and ability to provide informed consent. Exclusion criteria were a current or past diagnosis of alcohol or substance abuse disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (American Psychiatric Association, 2013), or a concurrent neurological illness. One hundred and eleven participants fulfilled the criteria (females = 73, Age mean = 40.91, SD = 11.68; Education = 25.2%, 55.0%, 19.8% for the Basic School, High School, and Bachelor or Higher, respectively).
People with a verified psychiatric diagnosis
Participants with a verified psychiatric diagnosis were recruited from the Parc Sanitari Sant Joan de Déu network of mental health services in Barcelona, Spain. They also provided written informed consent and completed the questionnaire with the help of a psychologist at the outpatient clinic where they were being treated. Data from 82 patients who fulfilled the inclusion criteria were included. Of the patients who were included, 50 had a psychotic disorder (41 with schizophrenia spectrum disorder, six with schizoaffective disorder, and three with delusional disorder) and 32 were diagnosed with a mood disorder (14 with depression disorder, 14 with bipolar disorder, three with a mixed affective disorder, and one with an anxiety disorder) according to Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria (American Psychiatric Association, 2013).
People who reported a diagnosis of mental disorder
This group included people who were recruited online from the Barcelona metropolitan and suburban areas. They reported having received a diagnosis of a mental disorder and mentioned a specific medication and psychological treatment for it. Data from 29 people (nine with depression, nine with anxiety, 10 with other psychiatric disorders such as anorexia and personality disorders, and one not classified) were included in the group of patients.
2.1.2. Putatively HC
The sample of HC consisted of 311 adults from the Barcelona metropolitan and suburban areas (females = 226; age mean = 37.49 SD = 10.89; Education1 = 1.9%, 27%, 71.1% for the Basic School, High School, and Bachelor or Higher, respectively). Inclusion criteria and exclusion criteria were the same as for the people with mental disorders except for having received a diagnosis of a mental disorder. Participants who did not complete the survey were excluded.
2.2. Measures
The survey was composed of:
2.2.1. Launay–Slade Hallucinations Scale‐Extended
The 16‐item LSHS‐E is a self‐report scale for investigating the multidimensionality of hallucinatory experiences in the general population (Larøi et al., 2004; Larøi & Van Der Linden, 2005; see Tables A1 and A2). In this version of the LSHS, items tap into sensory modalities other than auditory, such as the visual, olfactory, and tactile modalities. The scale also includes items on hypnagogic and hypnopompic hallucinations and on the experience of sensed presence (i.e., the experience of feeling the presence of someone close who has passed away). Respondents are asked to rate each item on a 5‐point Likert scale: (0) certainly does not apply to me; (1) possibly does not apply to me; (2) unsure; (3) possibly applies to me; and (4) certainly applies to me. The French version showed good internal reliability (Cronbach's α > 0.80; Larøi & Van Der Linden, 2005).
Standard translation and back‐translation procedures were followed to produce the Spanish version of the LSHS‐E. Translation accuracy was then confirmed by an independent native‐speaking translator and optimized with the help of the creator of the scale (Frank Larøi). Adaptation of the scale to Spanish culture was required to avoid potential misinterpretation, because some semantic characteristics of the scale could be slightly different from the original language.
2.2.2. Community Assessment of Psychic Experiences
The Community Assessment of Psychic Experiences (CAPE) is made up of 42 items that evaluate the Positive (20 items), Negative (14 items), and Depressive (eight items) dimensions of psychotic‐like experience in the general population (Konings, Bak, Hanssen, Van Os, & Krabbendam, 2006; Stefanis et al., 2002). It was created by van Os and coworkers and is primarily based on the PDI‐21 and PDI‐40 developed by Peters, Joseph, Day, and Garety (2004) and Peters, Joseph, and Garety (1995). Each question is answered with a 4‐point Likert‐type response scale that ranges from almost never (1) to almost always (4). In this study, the validated Spanish version (Fonseca‐Pedrero, Paino, Lemos‐Giráldez, & Muñiz, 2012; Ros‐Morente, Vilagra‐Ruiz, Rodriguez‐Hansen, Wigman, & Barrantes‐Vidal, 2011) was used (available at http://cape42.homestead.com/).
2.3. Statistics
All data were analyzed using the Statistical Package for Social Sciences, version 21. All tests were two‐tailed, and the significance threshold was set at p < 0.01 because of multiple testing. Scale reliability was evaluated using Cronbach's alpha. For group comparisons, reliability values of 0.70 are considered satisfactory, and when dealing with subscales derived from a single questionnaire, values around 0.60 are considered acceptable (Nunnally, 1978). The group with verified psychiatric disorders and the group that reported having received a diagnosis of a psychiatric disorder were fused into one group: People with mental disorders.
Continuous variables were compared between groups using Student's t test or the Mann–Whitney U test, as appropriate. Multivariate analysis of variance (MANOVA) with Wilks' lambda was used to test whether there were differences between the groups on the factors of the LSHS‐E (see below), taking into account pential confounding variables. Chi‐square tests or Fisher's exact tests were used to analyze categorical data. Cohen's d was used to calculate the effect size of the differences between means in single comparisons: Effect sizes of 0.20, 0.50, and 0.80 are considered small, medium, and large, respectively. Partial eta‐squared (ηp2) was used as a measure of effect size in the MANOVA (0.01, 0.06, 0.14 are considered small, medium, and large, respectively).
Concurrent validity was tested by assessing associations of the LSHS‐E with measures of psychotic‐like experiences (CAPE). It was hypothesized that the LSHS‐E would show greater links with items assessing (positive) psychotic‐like experiences than with items of the Negative and Depressive CAPE subscales. Correlation coefficients were compared according to Steigers' z test (Steiger, 1990).
2.3.1. Confirmatory factor analysis
Confirmatory factor analysis (CFA) was carried out with the lavaan package (Rosseel, 2012) running in R (R Development Core Team, 2012). The results obtained using this package have been shown to be consistent with other software packages (Narayanan, 2012). Maximum likelihood estimation with robust standard errors and Satorra–Bentler scaled test statistic was used to test CFA models. This method was chosen because it is robust against deviation from normality (Curran, West, & Finch, 1996). Besides the chi‐square, which is influenced by sample size, additional parameters for fit estimation were the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual. RMSEA values of 0.08 or lower, standardized root mean square residual values of 0.09 or lower, and CFI values of 0.90 or higher are considered acceptable (Browne, 1993; Hu & Bentler, 1999).
Three models were tested: the one‐factor model, assuming that all items load on a single factor; a two‐factor model, assigning items 1 to 7 to a subclinical or nonpsychopathological factor and items 8 to 16 to a clinical or psychopathological factor, by analogy with the model described in Serper et al. (2005); and a four‐factor model that distinguishes among an “auditory and visual HLEs” factor, a “multisensory HLEs” factor, an “intrusive thoughts” factor, and a “vivid daydreams” factor, as in (Vellante et al., 2012). The three‐factor model described in some past studies (Aleman et al., 2001; Paulik, Badcock, & Maybery, 2006; Waters, Badcock, & Maybery, 2003) was not tested because all these studies were conducted using the 12‐item version of the scale.
Models were compared on the basis of goodness‐of‐fit indices and the Bayesian information criterion (BIC; Schwarz, 1978), and of its derivation, the sample size adjusted BIC (Sclove, 1987). Models with the lowest BIC and sample size adjusted BIC are preferred (Kim, Yoon, Wen, Luo, & Kwok, 2015). McDonald's omega, as estimated from the model, was also reported. McDonald's omega is a reliability coefficient that has the advantage of taking into account the strength of association between items and constructs as well as item‐specific measurement errors. Therefore, it provides more realistic estimates of the true reliability of the scale. A factor loading of 0.32 (10% of the variance) was the minimum requirement for an item to be included in the final global score (Comrey & Lee, 1992). Factor mean scores were calculated by adding up item scores and then averaging the sum by the number of items for each factor. This was to compensate for the unequal number of items in the factors.
Measurement invariance by clinical status (past diagnosis of a mental disorder vs. putatively HC) was calculated according to Byrne and van de Vijver (2010), using the R semTools package (Pornprasertmanit, Miller, Schoemann, & Rosseel, 2013). Typically, a hierarchical set of steps is followed when invariance is tested, starting with the determination of a well‐fitting baseline model and then establishing successive equivalence constraints in the model parameters across groups. Configural, metric, scalar, and mean invariance was tested. Configural invariance refers to whether the same CFA model is valid in each group. Metric invariance concerns the equivalence of the factorial loadings across groups. Scalar invariance is assumed when the item intercepts and the factor loadings are equally constrained across groups. Full factor mean invariance is achieved with constraint‐latent means equal across groups. The confirmation of the invariance of the intercepts (scalar invariance) allows a comparison of the latent means in both groups. Models were compared on the basis of changes in CFI (delta‐CFI) and in RMSEA (delta‐RMSEA): delta‐CFI and delta‐RMSEA greater than 0.01 indicate deterioration in model fit. Models with the lowest BIC are preferred (Kim et al., 2015; Wicherts & Dolan, 2004).
2.3.2. Receiver operating characteristic analysis
Receiver operating characteristic (ROC) analysis was used to assess the capacity of the factors of the LSHS‐E to distinguish people with psychosis from putatively healthy people (controls). The target group included all patients with a confirmed diagnosis of psychosis within the spectrum of schizophrenia (n = 50). The HC were composed of people who denied any past or current history of a mental disorder at the online screening (n = 311).
To derive usable cutoff scores based on the reporting of HLEs as listed in the LSHS‐E, replies to each item were dichotomized, assigning a value = 1 to the responses (3) possibly applies to me and (4) certainly applies to me. All other responses received a value = 0. Scores of the four factors were recalculated by sum of occurrence = 1 (i.e., having had a HLE).
The following indicators were used to summarize the results of the ROC analysis: the area under receiver operator characteristic curve (with 95% confidence interval); sensitivity (the probability of a true positive case,i.e., probability that the score identifies a case of psychosis when compared with the confirmed psychiatric diagnosis) and specificity (the probability of a true negative case,i.e., probability that the score identifies a noncase of psychosis, someone without psychosis, when compared with the confirmed psychiatric diagnosis); positive predictive value (the probability that a person is a case of psychosis when a positive test result is observed) and negative predictive value (the probability that a person is not a case of psychosis when a negative test result is observed); and positive diagnostic likelihood ratio (the odds ratio that a positive test result will be observed in a population of people with psychosis compared with the odds that the same result will be observed among a population of people without psychosis).
Threshold for AUC were 0.80 to 0.90, good; 0.70 to 0.80, fair; <0.70, poor. Sensitivity and specificity were used to derive the cutoff that best differentiated the patients from controls. Positive and negative predictive values are better understood in cohort studies. As for the positive diagnostic likelihood ratio, the higher its value, the more useful is the test.
The ROC curves were compared with the method of DeLong, DeLong, and Clarke‐Pearson (1988).
ROC analysis was conducted with the pROC package running in R (Robin et al., 2011).
3. RESULTS
People with a mental disorder differed from the HC in age (t = −2.78 [df = 420], p = 0.006) and education (x2 = 110.99 [df = 2], p < 0.001), but not in gender ratio (x2 = 2.40 [df = 1], p = 0.121). The effect size for differences between the two groups was small for age (Cohen's d = 0.30) and large for education (Cohen's d = 1.29).
3.1. Reliability
Internal coherence, as measured by Cronbach's alpha, was acceptable for all the scales (Table 1).
Table 1.
Mean scores on the measures of psychopathology used in the study, and intercorrelation
| Putatively healthy controls (n = 311) | |||||
|---|---|---|---|---|---|
| Cronbach's α | Mean (SD) median | LSHS‐E | Positive | Depress. | |
| LSHS‐E | 0.831 | 11.78 (9.42) 25 | |||
| CAPE positive dimension | 0.866 | 25.64 (5.2.5) 24 | 0.513* | ||
| CAPE depressive dimension | 0.849 | 13.5 (3.42) 13 | 0.401* | 0.627* | |
| CAPE negative dimension | 0.873 | 23.18 (5.46) 22 | 0.388* | 0.578* | 0.744* |
| Participants with a diagnosis of a mental disorder (n = 111) | |||||
|---|---|---|---|---|---|
| Cronbach's α | Mean (SD) median | LSHS‐E | Positive | Depress. | |
| LSHS‐E | 0.911 | 23.32 (17.04) 34 | |||
| CAPE positive dimension | 0.891 | 34.09 (10.03) 31 | 0.727* | ||
| CAPE depressive dimension | 0.862 | 15.38 (4.66) 16 | 0.424* | 0.461* | |
| CAPE negative dimension | 0.859 | 27.52 (7.15) 26 | 0.492* | 0.543* | 0.803* |
Note. CAPE: Community Assessment of Psychic Experiences; LSHS‐E: Launay–Slade Hallucinations Scale‐extended version.
Pearson's r p < .0001.
3.2. Convergent and divergent validity
As expected, scores on the LSHS‐E were positively and significantly related to scores on the CAPE Positive dimension subscale (Table 1). In controls, the LSHS‐E had greater links with the CAPE Positive dimension than with the CAPE Negative (Steiger's Z = 2.75, p = 0.0059) and Depressive dimensions (Steiger's Z = 2.62, p = 0.0087). The differences were more evident in the sample of people with a mental disorder: Again, the LSHS‐E had greater links with the CAPE Positive dimension than with the CAPE Negative (Steiger's Z = 3.55, p = 0.0004) and Depressive dimensions (Steiger's Z = 4.13, p < 0.0001).
As a matter of fact, the correlation between the LSHS‐E and the CAPE Positive dimension was greater in the sample of people with mental disorder than in the sample of putatively HC: Fisher r‐to‐z transformation test: z = −3.18, p = 0.0015.
3.3. Confirmatory factor analysis
In both samples, the best fit was observed for the four‐factor model (Table 2).
Table 2.
(A) Goodness‐of‐fit indexes for the proposed models in the putatively healthy controls (sample: n = 311)
| Model | χ2 | df | CFI | RMSEA [95% CI] | SRMR | BIC | ssBIC | McDonald's omega |
|---|---|---|---|---|---|---|---|---|
| One‐factor | 214.22, p < 0.0001 | 104 | 0.815 | 0.078 [0.063–0.092] | 0.068 | 13,812.68 | 13,660.44 | 0.836 |
| Two‐factor | 173.10, p < 0.0001 | 103 | 0.882 | 0.062 [0.046–0.078] | 0.067 | 13,745.23 | 13,589.82 | 0.845 |
| Four‐factor | 114.55, p = 0.116 | 98 | 0.972 | 0.031 [0.000–0.052] | 0.051 | 13,665.06 | 13,493.79 | 0.856 |
| (B) Goodness‐of‐fit indexes for the proposed models in the participants with a diagnosis of a mental disorder (sample: n = 111) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | χ2 | df | CFI | RMSEA [95% CI] | SRMR | BIC | ssBIC | McDonald's omega |
| One‐factor | 212.57, p < 0.0001 | 104 | 0.837 | 0.109 [0.088–0.130] | 0.078 | 6,304.30 | 6,152.61 | 0.914 |
| Two‐factor | 197.87, p < 0.0001 | 103 | 0.857 | 0.103 [0.081–0.124] | 0.080 | 6,290.76 | 6,135.91 | 0.917 |
| Four‐factor | 143.10, p = 0.002 | 98 | 0.935 | 0.071 [0.044–0.096] | 0.062 | 6,237.59 | 6,066.94 | 0.928 |
Note. BIC: Bayesian information criterion; CFI: comparative fit index; RMSEA: root mean square error of approximation; SRMR: standardized root mean square residual; ssBIC: sample size adjusted BIC.
People with mental disorder had the best McDonald's omega, indicating greater reliability of their responses. In the four‐factor model, the factor loading was acceptable (>0.32) for all items except item 3 in the sample of HC (“No matter how hard I try to concentrate on my work unrelated thoughts always creep into my mind”; see Table A1).
The model with four correlated factors was therefore selected to test measurement invariance. In this model, Factor 1 can be labeled “intrusive thoughts” (Items: 1, 2, 3); Factor 2 can be seen as representing “vivid daydreams” (Items 5,6,7); Factor 3 can be labeled “multisensory HLEs” (Items: 11, 12, 13, 14, 15); and Factor 4 is related to “auditory–visual HLEs” (Items: 4, 8,9,10,16). In both samples, participants more often endorsed items related to vivid daydreams or hypnagogic and hypnopompic hallucinations than items with a clearer psychopathological nature (e.g., auditory–visual HLEs; Tables A1 and A2).
3.4. Measurement invariance
There was an overall reduction of fit with increasingly constrained models, but the models could still be considered acceptable on the basis of the global fit, with the exception of the mean invariance model (Table 3).
Table 3.
Fit indices (with corrected robust estimation) for invariance tests of the four‐factor model
| Putatively healthy controls (n = 311) versus participants with a diagnosis of a mental disorder (n = 111) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model | χ2 | df | p | CFI | RMSEA | BIC | delta‐CFI | delta‐RMSEA |
| Configural invariance | 371.63 | 196 | 0.0001 | 0.954 | 0.037 | 19,991 | ||
| Metric invariance | 428.89 | 208 | 0.0001 | 0.929 | 0.045 | 19,976 | −0.045 | +0.008 |
| Scalar invariance | 468.18 | 220 | 0.0001 | 0.908 | 0.050 | 19,963 | −0.021 | +0.005 |
| Mean invariance | 532.96 | 224 | 0.0001 | 0.869 | 0.059 | 19,983 | −0.039 | +0.009 |
Note. BIC: Bayesian information criterion; CFI: comparative fit index; RMSEA: root mean square error of approximation.
As can be seen from Table 3, the difference in the CFI between the configural and the more constrained models exceeded 0.01. However, the delta‐RMSEA was always lower than 0.01 across models. Moreover, in all comparisons, with the exception of the mean invariance model, the BIC was lower than in the preceding model, suggesting that the model had a better fit. The results support configural, metric, and strong invariance of the LSHS‐E between putatively HC and people with a mental disorder. However, the two groups were expected to differ in terms of the mean score on the four factors.
People with a mental disorder reported higher means compared with putatively HC in all four factors: intrusive thoughts (People with mental disorder: mean = 2.14, SD = 1.25; HC mean = 1.14, SD = 0.88; t = −7.77, [df = 150.57], p < 0.001), vivid daydreams (People with mental disorder: mean = 1.26, SD = 1.34; HC: mean = 0.49, SD = 0.77; t = −5.72, [df = 137.15], p < 0.001), multisensory HLEs (People with mental disorder: mean = 1.41, SD = 1.30; HC: mean = 1.05, SD = 0.93; t = −2.71, [df = 152.12], p = 0.007), and auditory–visual HLEs (People with mental disorder: mean = 1.19, SD = 1.23; HC: mean = 0.32, SD = 0.50; t = −7.25, [df = 123.10], p < 0.001). The MANOVA showed that there was a statistically significant difference in hallucination propensity between the groups: F(4, 417) = 36.32, p < 0.0005; Wilks' Λ = 0.742, partial η2 = 0.25. We can see that mental disorder has a statistically significant effect on auditory–visual HLEs F = 106.97, p < 0.0005, partial η2 = 0.20, intrusive thought F = 83.58, p < 0.0005, partial η2 = 0.16; medium effect for vivid daydreams F = 53.03, p < 0.0005, partial η2 = 0.11; and small effect for multisensory HLEs F = 10.04, p < 0.0005, partial η2 = 0.02. By taking into account education variable, the effect decreased but the significance was maintained: F(4, 416) = 20.98, p < 0.0005, partial η2 = 0.16, auditory–visual HLEs F = 58.44, p < 0.0005, partial η2 = 0.12; intrusive thoughts F = 39.77, p < 0.0005, partial η2 = 0.08; vivid daydreams F = 20.99, p < 0.0005, partial η2 = 0.04; except for multisensory HLEs F = 2.04, p = 0.154, partial η2 = 0.005.
3.5. ROC analysis
Table 4 lists the range of scores, median, and interquartile range for the four factors of the LSHS‐E in patients with psychosis and in controls. Patients were more likely to report a HLEs on the four factors of the LSHS‐E than controls (Mann–Whitney test p < 0.0001 in all comparisons).
Table 4.
Distribution of the scores on the four factors of the LSHS‐E and their predictive capacity based on ROC analysis
|
Intrusive thoughts Items: n = 3 |
Vivid daydreams Items: n = 3 |
Multisensory HLEs Items: n = 5 |
Auditory–visual HLEs Items: n = 5 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Range | Median | IQR | Range | Median | IQR | Range | Median | IQR | Range | |
| Controls (n = 311) | 1 | 1 | 0–3 | 0 | 0 | 0–3 | 1 | 2 | 0–5 | 0 | 0 | 0–5 |
| Patients with psychotic disorders (n = 50) | 2 | 2 | 0–3 | 1 | 2.25 | 0–3 | 1.5 | 4 | 0–5 | 1 | 2 | 0–3 |
| Mann–Whitney test | Z = −7.97; p < 0.0001 | Z = −7.92; p < 0.0001 | Z = −3.61; p < 0.0001 | Z = −8.23; p < 0.0001 | ||||||||
| ROC analysis | ||||||||||||
| AUC [95% CI] | 0.827 [0.767–0.888] | 0.759 [0.684–0.834] | 0.650 [0.566–0.734] | 0.780 [0.702–0.858] | ||||||||
| Cutoff | 2 | 1 | 3 | 2 | ||||||||
| Sensitivity | 0.660 | 0.640 | 0.380 | 0.600 | ||||||||
| Specificity | 0.874 | 0.829 | 0.858 | 0.948 | ||||||||
| Positive predictive value | 0.458 | 0.376 | 0.301 | 0.652 | ||||||||
| Negative predictive value | 0.941 | 0.934 | 0.895 | 0.936 | ||||||||
| Diagnostic likelihood ratio | 5.26 | 3.75 | 2.68 | 11.66 | ||||||||
Note. AUC: Area under receiver operator characteristic curve (with 95% confidence interval); HLEs: hallucination‐like experiences; IRQ: interquartile range; LSHS‐E: Launay–Slade Hallucinations Scale‐extended version; ROC: receiver operating characteristic.
ROC analysis revealed that all factors except the one on multisensory HLEs were able to differentiate patients with psychosis from controls with a fair AUC (95% CI between 0.70 and 0.80). The capacity of the multisensory HLEs factor to differentiate patients with psychosis from controls was poor. Indeed, compared with the auditory–visual HLEs factor, the multisensory HLEs factor was statistically less accurate in differentiating patients with psychosis from HC (Figure 1).
Figure 1.
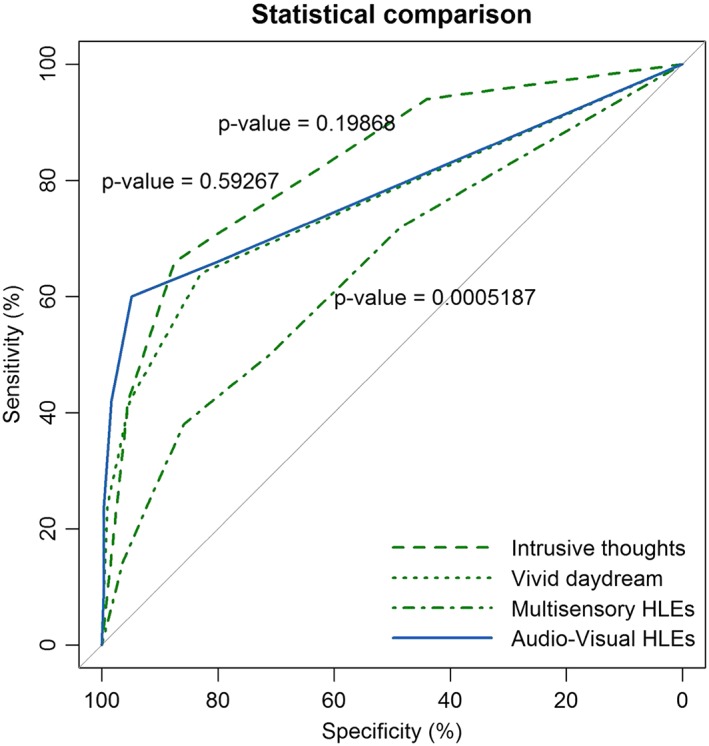
Statistical comparison of the ROC curves between the predictive capacity of the auditory and visual HLEs factors and the other three factors of the LSHS‐E in differentiating patients with psychosis from putatively healthy controls. The statistical significance of the difference between the areas under the dependent ROC curves (derived from the same cases) with the method of DeLong et al. (1988) is reported. HLEs: hallucination‐like experiences; ROC: receiver operating characteristic
The auditory–visual HLEs factor had the best diagnostic likelihood ratio, with a value above 11—that is, someone with psychosis had 11 times the chance of reporting auditory and visual HLEs than people without psychosis. Overall, the factors had high negative predictive values, suggesting that people that do not report HLEs on the LSHS‐E are very unlikely to have a psychosis. However, because the sample was not a cohort, and the proportion of people with psychosis was inflated by active enrollment, this property of the LSHS‐E remains open to further testing.
4. DISCUSSION
The present study shows that the Spanish version of the LSHS‐E possesses satisfactory psychometric properties. Indeed, the reliability of the LSHS‐E was good in both HC and people who reported or had a certified diagnosis of a mental disorder. Concurrent validity was in the expected direction, with higher correlations with measures of positive psychotic‐like experiences than with measures of depression or negative symptoms, especially in people with a mental disorder. The LSHS‐E proved able to distinguish people with psychosis within from HC. Among its factors, that on auditory–visual HLEs had the greatest capacity to differentiate people diagnosed with psychosis within the spectrum of schizophrenia from HC, whereas the multisensory HLEs factor was less accurate in differentiating the two groups. This may depend on the fact that this factor includes items on hypnagogic and hypnopompic hallucinations, which are much more frequently reported by people from the general population than subjective experiences such as auditory and visual hallucinations, which are less socially desirable (Ohayon, 2000).
In this study, the distribution of HLEs in the samples was multidimensional, with a four‐factor model showing the best fit. The multifactorial structure of the LSHS has been reported before with various versions of the scale (Aleman et al., 2001; Castiajo & Pinheiro, 2017; Fonseca‐Pedrero et al., 2010; Larøi et al., 2004; Larøi & Van Der Linden, 2005; Paulik et al., 2006; Serper et al., 2005; Vellante et al., 2012). However, structures often differed depending on the version of the LSHS that was used in the study. Fonseca‐Pedrero et al. (2010) found a four‐factor model of the Spanish version of the revised‐LSHS but with a version composed of 12 items. This study replicated the four‐factor structure of the extended 16‐item version of the LSHS‐E as reported in Vellante et al. (2012) and Preti et al. (2014), providing some consistency for four dimensions of the propensity to experience and report HLEs in nonclinical populations. Moreover, this version fully matches with the factor‐structure reported by Larøi et al. (2004) in one of the original studies, with the exception of the intrusive thought factor (called intrusive thoughts or realness of thought) that includes different items.
This study was also the first to provide evidence that the multidimensional articulation of proneness to hallucination can be reproduced across groups that differ on clinical grounds. The measurement invariance of the LSHS‐E shows that this tool is suitable for use in cross‐comparison between patients and HC. In a past investigation, Preti et al. (2014) provided evidence of configural, metric, and strong invariance of the LSHS‐E across levels of psychological distress of healthy participants. However, Preti et al. (2014) examined the measurement invariance across levels of psychological distress in a community sample of nonhelp‐seeking people. The present study is the first to formally test measurement invariance of the LSHS‐E in a mixed sample of putatively HC and people diagnosed with a mental disorder. A past study (Stanghellini, Langer, Ambrosini, & Cangas, 2012) that was based on qualitative analysis and a different version of the LSHS from the LSHS‐E suggested that some items of their scale might be described in a different way by putatively HC and patients with a diagnosis of schizophrenia. In contrast to the hypothesis advanced by Stanghellini et al. (2012), the results of the measurement invariance of the present study showed that the groups (clinical vs. nonclinical) are comparable on hallucination experiences measured by the LSHS‐E across groups. So the latent construct is equivalent in both groups; they interpret the information in the same way but the intensity with which they live these experiences is different.
As expected, people with a diagnosis of a mental disorder, especially those with psychosis, were more likely to admit having had auditory or visual HLEs than those who did not report a past diagnosis (HC). Conversely, HC rarely reported HLEs within the dimensions of psychopathology; items related to vivid daydreams or hypnagogic and hypnopompic hallucinations were more often reported by HC than items related to visual or auditory hallucinations.
Most HLEs are transitory and do not necessarily relate to psychopathology (Dhossche, Ferdinand, Van Der Ende, Hofstra, & Verhulst, 2002). However, in 10% to 25% of cases, they become persistent and may acquire some clinical relevance (van Os, Linscott, Myin‐Germeys, Delespaul, & Krabbendam, 2009). It has been suggested that differences in the prevalence of HLEs between the clinical and nonclinical group could depend on associated clinical features (Larøi et al., 2012). People of the clinical group more frequently reported negative content, less controllability, higher distress, anxiety, sadness, and disruption in their everyday life functioning compared with nonclinical groups. The co‐occurrence of other clinical conditions such as depression and anxiety, which are related per se to an increased reporting of HLEs, represents a risk factor to develop psychosis in people with a vulnerability to it (Yung et al., 2003). LSHS‐E allows some specificity in the assessment of the multidimensionality of HLEs. Indeed, scores on the LSHS‐E were more specifically related to measures of positive psychotic‐like experiences than to measures of depression or anhedonia. It would be interesting in future studies to investigate whether HLEs scored with certainty on the LSHS‐E are predictive of the risk of psychosis, as they were previously found to be related to psychological distress of clinical relevance in samples of nonhelp‐seeking people (Preti, Cella, Raballo, & Vellante, 2012). Indeed, there is some evidence that anxiety and depression influence the onset, the duration, and the recurrence of hallucination experiences (Hartley, Barrowclough, & Haddock, 2013). Early intervention may be helpful for people presenting with episodes of hallucination experiences and symptoms of anxiety or depression. This may be particularly indicated for those who report more negative voice‐hearing experiences (Powers, Kelley, & Corlett, 2017). The LSHS‐E consent to the assessment of a variety of experiences within the multidimensional continuum of hallucination experiences and might be suited for monitoring of these experiences in care routine. For its simplicity, it can also be implemented in electronic device and mobile phone applications, which are increasingly gaining popularity in the treatment of early psychosis (Kumar et al., 2018).
4.1. Limitations and strengths
The groups differed in age, but at a small effect size, not in gender ratio. However, and as expected, the HC had a higher educational level compared with people with mental disorders. Indeed, people with mental disorders, particularly with psychotic features, often do not complete the educational path, especially when they have an early onset, in childhood or adolescence (Frissen et al., 2015; Mikkonen, Moustgaard, Remes, & Martikainen, 2018).
Additional limitations need to be acknowledged. First, this is an online study and as such carries a risk of simulation. However, to detect potential simulators, we included questions that address the same information in different ways (e.g., age and date of birth) to filter out potential imposters. Second, only people who have access to the Internet could take the surveys, thereby probably excluding elderly people. Third, different cultural aspects might influence the interpretation of the content and the willingness to admit these experiences. Despite this limitation, the HLEs measured by LSHS‐E were strongly associated with positive dimensions of the CAPE, suggesting that the experiences that were measured by the Spanish LSHS‐E were within the positive psychotic dimension, as expected, and were not misinterpreted. Last but not least, the different selection used to recruit people with mental disorders could limit the generazibility of the results because a disparate range of conditions was included under the heading “mental disorders,” both with and without psychotic features. Nevertheless, online studies have a number of advantages: they are cheaper and assure the participants some sense of anonymity, making it more likely to get answers even to questions on sensitive topics, and with them, it is possible to include large numbers of people in a short time.
5. CONCLUSION
The LSHS‐E is a valid and reliable assessment tool to evaluate the multidimensionality of HLEs in nonclinical populations (Larøi et al., 2004; Vellante et al., 2012) and people at risk of psychosis. In this study, a high propensity for hallucination‐proneness was significantly associated with high psychosis proneness scores as measured by the CAPE. This version of the LSHS‐E might be particularly helpful to investigate multidimensional subthreshold HLEs that convert to more pathological aberrations, and which may eventually end up as full‐blown psychosis (Escher et al., 2002; Smeets, Lataster, Dominguez, et al., 2012; Smeets, Lataster, van Winkel, et al., 2012).
CONTRIBUTORS
Authors S. S. and A. P. managed the literature and undertook the statistical analyses. S. S. and S. O. designed the study and wrote the protocol. S. S. and A. P. wrote the first draft of the protocol. A. F., J. C., and S. S. conducted the data collection. All authors contributed to writing the final manuscript and have approved it.
ACKNOWLEDGMENTS
We would like to thank Fernando Jimenez Gomez‐Director of the Department of Personality Evaluation and Psychological Treatment of Salamanca University, and Jamila Hamidou for their help. A grant PRRMAB‐A2011‐19251 from the “Master and Back program,” Sardinia Region, was awarded to S. S. This project was financed by the Parc Sanitari Sant Joan de Déu (PSSJD: AR201404).
APPENDIX A.
Table A1.
Descriptive statistics for the items and factor analysis of the Spanish LSHS‐E with factor loading (loading <0.30 was not reported)
| Four‐factor model in the putatively healthy controls (n = 311) | |||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | % apply to mea | Factor 1 | Factor 2 | Factor 3 | Factor 4 | ||
| 1. |
Sometimes a passing thought will seem so real that it frightens me. Algunas veces tengo pensamientos pasajeros tan reales que me asustan. |
0.71 (1.06) | 1.3 | 0.539 | |||
| 2. |
Sometimes my thoughts seem as real as actual events in my life. Algunas veces mis pensamientos me parecen tan reales como los acontecimientos verdaderos de mi vida. |
0.79 (1.14) | 2.9 | 0.797 | |||
| 3. |
No matter how hard I try to concentrate on my work unrelated thoughts always creep into my mind. Aunque intente concentrarme en una actividad, me vienen a la cabeza pensamientos no relacionados con lo que estoy haciendo. |
1.93 (1.35) | 9.3 | 0.313 | |||
| 4. |
In the past I have had the experience of hearing a person's voice and then found that there was no‐one there. En el pasado he oído voces de una persona y después me he dado cuenta de que no había nadie allí. |
0.65 (1.14) | 3.5 | 0.336 | |||
| 5. |
The sounds I hear in my daydreams are generally clear and distinct. Generalmente los sonidos que oigo en mis fantasías son claros y nítidos. |
0.62 (1.06) | 3.5 | 0.614 | |||
| 6. |
The people in my daydreams seem so true to life that I sometimes think that they are. Las personas que aparecen en mis sueños despiertos son tan reales que a veces creo que realmente existen. |
0.37 (0.89) | 1.9 | 0.697 | |||
| 7. |
In my daydreams I can hear the sound of a tune almost as clearly as if I were actually listening to it. En mis fantasías puedo oír una melodía tan nítidamente que creo que la estoy escuchando realmente. |
0.48 (0.99) | 2.3 | 0.652 | |||
| 8. |
I often hear a voice speaking my thoughts aloud. Frecuentemente oigo una voz que dice mis pensamientos en voz alta. |
0.24 (0.75) | 1.3 | 0.397 | |||
| 9. |
I have been troubled by hearing voices in my head. Me he encontrado molesto por las voces que oigo en mi cabeza. |
0.09 (0.48) | 0.6 | 0.372 | |||
| 10. |
On occasions I have seen a person's face in front of me when no‐one was in fact there. En alguna ocasión he visto la cara de una persona aunque no había nadie allí. |
0.28 (0.76) | 1.0 | 0.391 | |||
| 11. |
Sometimes, immediately prior to falling asleep or upon awakening, I have had the experience of having seen, felt or heard something or someone that wasn't there, or I had the feeling of being touched even though no one was there. Algunas veces, en el momento de conciliar el sueño o al despertarme, he tenido la experiencia de ver, oír o percibir algo o a alguien que no había allí, o he tenido la impresión de ser tocado por alguien aunque no había nadie allí. |
1.16 (1.37) | 6.8 | 0.425 | |||
| 12. |
Sometimes, immediately prior to falling asleep or upon awakening, I have felt that I was floating or falling, or that I was leaving my body temporarily. Algunas veces, en el momento de conciliar el sueño o al despertarme, he tenido la impresión de flotar en el aire, caer o separarme del cuerpo temporalmente. |
1.61 (1.56) | 14.1 | 0.496 | |||
| 13. |
On certain occasions I have felt the presence of someone close who had passed away. Algunas veces he tenido la sensación de la presencia de una persona cerca de mí que había fallecido. |
0.86 (1.25) | 4.5 | 0.294 | |||
| 14. |
In the past, I have smelt a particular odour even though there was nothing there. En el pasado he sentido un olor particular aunque no había nada. |
0.88 (1.31) | 6.4 | 0.416 | |||
| 15. |
I have had the feeling of touching something or being touched and then found that nothing or no‐one was there. He tenido la sensación de tocar algo, o ser tocado por alguien y después descubrir que no había nada. |
0.76 (1.21) | 4.2 | 0.549 | |||
| 16. |
Sometimes, I have seen objects or animals even though there was nothing there. Algunas veces he visto objetos o animales aunque no había nada. |
0.36 (0.85) | 1.3 | 0.641 | |||
Note. LSHS‐E: Launay–Slade Hallucinations Scale‐extended version.
% Apply to me includes those who reply possibly (3) or certainly (4) apply to me on the item.
Table A2.
Descriptive statistics for the items and factor analysis of the Spanish LSHS‐E with factor loading (loading <0.30 was not reported)
| Four‐factor model in the participants with a diagnosis of a mental disorder (n = 111) | |||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | % apply to mea | Factor 1 | Factor 2 | Factor 3 | Factor 4 | ||
| 1. |
Sometimes a passing thought will seem so real that it frightens me. Algunas veces tengo pensamientos pasajeros tan reales que me asustan. |
1.98 (1.62) | 25.2 | 0.539 | |||
| 2. |
Sometimes my thoughts seem as real as actual events in my life. Algunas veces mis pensamientos me parecen tan reales como los acontecimientos verdaderos de mi vida. |
1.91 (1.71) | 27.9 | 0.797 | |||
| 3. |
No matter how hard I try to concentrate on my work unrelated thoughts always creep into my mind. Aunque intente concentrarme en una actividad, me vienen a la cabeza pensamientos no relacionados con lo que estoy haciendo. |
2.55 (1.55) | 36.0 | 0.313 | |||
| 4. |
In the past I have had the experience of hearing a person's voice and then found that there was no‐one there. En el pasado he oído voces de una persona y después me he dado cuenta de que no había nadie allí. |
0.76 (1.78) | 30.6 | 0.336 | |||
| 5. |
The sounds I hear in my daydreams are generally clear and distinct. Generalmente los sonidos que oigo en mis fantasías son claros y nítidos. |
1.50 (1.66) | 20.7 | 0.614 | |||
| 6. |
The people in my daydreams seem so true to life that I sometimes think that they are. Las personas que aparecen en mis sueños despiertos son tan reales que a veces creo que realmente existen. |
1.27 (1.64) | 17.1 | 0.697 | |||
| 7. |
In my daydreams I can hear the sound of a tune almost as clearly as if I were actually listening to it. En mis fantasías puedo oír una melodía tan nítidamente que creo que la estoy escuchando realmente. |
1.02 (1.53) | 13.5 | 0.652 | |||
| 8. |
I often hear a voice speaking my thoughts aloud. Frecuentemente oigo una voz que dice mis pensamientos en voz alta. |
1.04 (1.53) | 15.3 | 0.397 | |||
| 9. |
I have been troubled by hearing voices in my head. Me he encontrado molesto por las voces que oigo en mi cabeza. |
1.19 (1.65) | 18 | 0.372 | |||
| 10. |
On occasions I have seen a person's face in front of me when no‐one was in fact there. En alguna ocasión he visto la cara de una persona aunque no había nadie. |
1.22 (1.63) | 18 | 0.391 | |||
| 11. |
Sometimes, immediately prior to falling asleep or upon awakening, I have had the experience of having seen, felt or heard something or someone that wasn't there, or I had the feeling of being touched even though no one was there. Algunas veces, en el momento de conciliar el sueño o al despertarme, he tenido la experiencia de ver, oír o percibir algo o a alguien que no había allí, o he tenido la impresión de ser tocado por alguien aunque no había nadie allí. |
1.59 (1.67) | 21.6 | 0.425 | |||
| 12. |
Sometimes, immediately prior to falling asleep or upon awakening, I have felt that I was floating or falling, or that I was leaving my body temporarily. Algunas veces, en el momento de conciliar el sueño o al despertarme, he tenido la impresión de flotar en el aire, caer o separarme del cuerpo temporalmente. |
1.50 (1.68) | 18.9 | 0.496 | |||
| 13. |
On certain occasions I have felt the presence of someone close who had passed away. Algunas veces he tenido la sensación de la presencia de una persona cerca de mí que había fallecido. |
1.48 (1.79) | 28.8 | 0.294 | |||
| 14. |
In the past, I have smelt a particular odour even though there was nothing there. En el pasado he sentido un olor particular aunque no había nada. |
1.25 (1.66) | 19.8 | 0.416 | |||
| 15. |
I have had the feeling of touching something or being touched and then found that nothing or no‐one was there. He tenido la sensación de tocar algo, o ser tocado por alguien y después descubrir que no había nada. |
1.29 (1.69) | 19.8 | 0.549 | |||
| 16. |
Sometimes, I have seen objects or animals even though there was nothing there. Algunas veces he visto objetos o animales aunque no había nada. |
0.79 (1.39) | 9 | 0.641 | |||
Note. LSHS‐E: Launay–Slade Hallucinations Scale‐extended version.
% Apply to me includes those who reply possibly (3) or certainly (4) apply to me on the item.
Siddi S, Ochoa S, Farreny A, et al. Measurement invariance of the Spanish Launay–Slade Hallucinations Scale‐Extended version between putatively healthy controls and people diagnosed with a mental disorder. Int J Methods Psychiatr Res. 2018;27:e1741 10.1002/mpr.1741
Footnotes
Educational level based on the following classification: 1 = Basic School (no studies; primary studies); 2 = High school (high school; uncompleted university studies); 3 = Bachelor or Higher (Bachelor, Master, and PhD).
REFERENCES
- Aleman, A. , Nieuwenstein, M. R. , Böcker, K. B. , & De Haan, E. H. (1999). Temporal stability of the Launay‐Slade Hallucination Scale for high‐ and low‐scoring normal subjects. Psychological Reports, 85(3 Pt 2), 1101–1104. 10.2466/pr0.1999.85.3f.1101 [DOI] [PubMed] [Google Scholar]
- Aleman, A. , Nieuwenstein, M. R. , Böcker, K. B. E. , & De Haan, E. H. F. (2001). Multi‐dimensionality of hallucinatory predisposition: Factor structure of the Launay–Slade Hallucination Scale in a normal sample. Personality and Individual Differences, 30(2), 287–292. 10.1016/S0191-8869(00)00045-3 [DOI] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, 5th edition (DSM‐5). Diagnostic and Statistical Manual of Mental Disorders 4th Edition TR (ed., Vol. 280). Washington: American Psychiatry Publishing; 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- Beavan, V. , Read, J. , & Cartwright, C. (2011). The prevalence of voice‐hearers in the general population: A literature review. Journal of Mental Health (Abingdon, England), 20(3), 281–292. 10.3109/09638237.2011.562262 [DOI] [PubMed] [Google Scholar]
- Bentall, R. P. , & Slade, P. D. (1985). Reality testing and auditory hallucinations: A signal detection analysis. The British Journal of Clinical Psychology/the British Psychological Society, 24(Pt 3), 159–169. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/4052663 [DOI] [PubMed] [Google Scholar]
- Browne, M. C. R. (1993). Alternative ways of assessing model fit In Bollen J. S. (Ed.), Testing structural equation models (pp. 136–161). Newbury Park: Sage. [Google Scholar]
- Byrne, B. M. , & van de Vijver, F. J. R. (2010). Testing for measurement and structural equivalence in large‐scale cross‐cultural studies: Addressing the issue of nonequivalence. International Journal of Testing, 10(2), 107–132. 10.1080/15305051003637306 [DOI] [Google Scholar]
- Castiajo, P. , & Pinheiro, A. P. (2017). On “hearing” voices and “seeing” things: Probing hallucination predisposition in a Portuguese nonclinical sample with the Launay‐Slade Hallucination Scale‐revised. Frontiers in Psychology, 8(JUL). 10.3389/fpsyg.2017.01138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comrey, A. L. , & Lee, H. B. (1992). A first course in factor analysis (2nd ed.). Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc; 10.1037/0011756 [DOI] [Google Scholar]
- Curran, P. J. , West, S. G. , & Finch, J. F. (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1(1), 16–29. 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- DeLong, E. R. , DeLong, D. M. , & Clarke‐Pearson, D. L. (1988). Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics, 44(3), 837–845. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/3203132 [PubMed] [Google Scholar]
- Dhossche, D. , Ferdinand, R. , Van Der Ende, J. , Hofstra, M. B. , & Verhulst, F. (2002). Diagnostic outcome of self‐reported hallucinations in a community sample of adolescents. Psychological Medicine, 32(4), 619–627. 10.1017/S003329170200555X [DOI] [PubMed] [Google Scholar]
- Escher, S. , Romme, M. , Buiks, A. , Delespaul, P. , & Van Os, J. (2002). Formation of delusional ideation in adolescents hearing voices: A prospective study. American Journal of Medical Genetics ‐ Neuropsychiatric Genetics, 114(8), 913–920. 10.1002/ajmg.10203 [DOI] [PubMed] [Google Scholar]
- Fonseca‐Pedrero, E. , Lemos‐giráldez, S. , Paino, M. , Sierra‐Baigrie, S. , Villazón‐garcía, Ú. , González, P. G. , … Muniz, J. (2010). Dimensionality of hallucinatory predisposition: Confirmatory factor analysis of the Launay‐Slade Hallucination Scale‐revised in college students. Anales De Psicologia, 26, 41–48. [Google Scholar]
- Fonseca‐Pedrero, E. , Paino, M. , Lemos‐Giráldez, S. , & Muñiz, J. (2012). Validation of the community assessment psychic experiences‐42 (CAPE‐42) in Spanish college students and patients with psychosis. Actas Españolas de Psiquiatría, 40(4), 169–176. [PubMed] [Google Scholar]
- Frissen, A. , Lieverse, R. , Marcelis, M. , Drukker, M. , Delespaul, P. , & GROUP Investigators (2015). Psychotic disorder and educational achievement: A family‐based analysis. Social Psychiatry and Psychiatric Epidemiology, 50(10), 1511–1518. 10.1007/s00127-015-1082-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García‐Montes, J. M. , Pérez‐Álvarez, M. , Soto Balbuena, C. , Perona Garcelán, S. , & Cangas, A. J. (2006). Metacognitions in patients with hallucinations and obsessive‐compulsive disorder: The superstition factor. Behaviour Research and Therapy, 44(8), 1091–1104. 10.1016/j.brat.2005.07.008 [DOI] [PubMed] [Google Scholar]
- Hartley, S. , Barrowclough, C. , & Haddock, G. (2013). Anxiety and depression in psychosis: A systematic review of associations with positive psychotic symptoms. Acta Psychiatrica Scandinavica 10.1111/acps.12080, 128, 327–346. [DOI] [PubMed] [Google Scholar]
- Hu, L. , & Bentler, P. M. (1999). Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Johns, L. C. (2005). Hallucinations in the general population. Current Psychiatry Reports, 7(3), 162–167. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15935129 [DOI] [PubMed] [Google Scholar]
- Kim, E. S. , Yoon, M. , Wen, Y. , Luo, W. , & Kwok, O. M. (2015). Within‐level group factorial invariance with multilevel data: Multilevel factor mixture and multilevel MIMIC models. Structural Equation Modeling, 22(4), 603–616. 10.1080/10705511.2014.938217 [DOI] [Google Scholar]
- Konings, M. , Bak, M. , Hanssen, M. , Van Os, J. , & Krabbendam, L. (2006). Validity and reliability of the CAPE: A self‐report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatrica Scandinavica, 114(1), 55–61. 10.1111/j.1600-0447.2005.00741.x [DOI] [PubMed] [Google Scholar]
- Kumar, D. , Tully, L. M. , Iosif, A.‐M. , Zakskorn, L. N. , Nye, K. E. , Zia, A. , & Niendam, T. A. (2018). A mobile health platform for clinical monitoring in early psychosis: Implementation in community‐based outpatient early psychosis care. JMIR Mental Health, 5(1), e15 10.2196/mental.8551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larøi, F. , Marczewski, P. , & Van der Linden, M. (2004). Further evidence of the multi‐dimensionality of hallucinatory predisposition: Factor structure of a modified version of the Launay‐Slade hallucinations scale in a normal sample. European Psychiatry: The Journal of the Association of European Psychiatrists, 19(1), 15–20. 10.1016/S0924-9338(03)00028-2 [DOI] [PubMed] [Google Scholar]
- Larøi, F. , Sommer, I. E. , Blom, J. D. , Fernyhough, C. , Ffytche, D. H. , Hugdahl, K. , … Waters, F. (2012). The characteristic features of auditory verbal hallucinations in clinical and nonclinical groups: State‐of‐the‐art overview and future directions. Schizophrenia Bulletin, 38(4), 724–733. 10.1093/schbul/sbs061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larøi, F. , & Van Der Linden, M. (2005). Nonclinical participants' reports of hallucinatory experiences. Canadian Journal of Behavioural Science 10.1037/h0087243, 37, 33–43. [DOI] [Google Scholar]
- Launay, G. , & Slade, P. (1981). The measurement of hallucinatory predisposition in male and female prisoners. Personality and Individual Differences, 2(3), 221–234. 10.1016/0191-8869(81)90027-1 [DOI] [Google Scholar]
- Maijer, K. , Begemann, M. J. H. , Palmen, S. J. M. C. , Leucht, S. , & Sommer, I. E. C. (2017). Auditory hallucinations across the lifespan: A systematic review and meta‐analysis. Psychological Medicine, 48, 1–10. 10.1017/S0033291717002367. [DOI] [PubMed] [Google Scholar]
- Mikkonen, J. , Moustgaard, H. , Remes, H. , & Martikainen, P. (2018). The population impact of childhood health conditions on dropout from upper‐secondary education. The Journal of Pediatrics, 196, 283–290.e4. 10.1016/j.jpeds.2018.01.034 [DOI] [PubMed] [Google Scholar]
- Morrison, A. P. , Wells, A. , & Nothard, S. (2000). Cognitive factors in predisposition to auditory and visual hallucinations. British Journal of Clinical Psychology, 39(1), 67–78. 10.1348/014466500163112 [DOI] [PubMed] [Google Scholar]
- Narayanan, A. (2012). A review of eight software packages for structural equation modeling. The American Statistician, 66(2), 129–138. 10.1080/00031305.2012.708641 [DOI] [Google Scholar]
- Nunnally, J. C. (1978). Psychometric theory (2nd. ed.). New York: McGraw‐Hill. [Google Scholar]
- Ochoa, S. , Haro, J. M. , Torres, J. V. , Pinto‐Meza, A. , Palacín, C. , Bernal, M. , … Autonell, J. (2008). What is the relative importance of self reported psychotic symptoms in epidemiological studies? Results from the ESEMeD‐Catalonia Study. Schizophrenia Research, 102(1–3), 261–269. 10.1016/j.schres.2008.04.010 [DOI] [PubMed] [Google Scholar]
- Ohayon, M. M. (2000). Prevalence of hallucinations and their pathological associations in the general population. Psychiatry Research, 97(2–3), 153–164. 10.1016/S0165-1781(00)00227-4 [DOI] [PubMed] [Google Scholar]
- Paulik, G. , Badcock, J. C. , & Maybery, M. T. (2006). The multifactorial structure of the predisposition to hallucinate and associations with anxiety, depression and stress. Personality and Individual Differences, 41(6), 1067–1076. 10.1016/j.paid.2006.04.012 [DOI] [Google Scholar]
- Peters, E. , Joseph, S. , Day, S. , & Garety, P. (2004). Measuring delusional ideation: The 21‐item Peters et al. Delusions Inventory (PDI). Schizophrenia Bulletin, 30(4), 1005–1022. [DOI] [PubMed] [Google Scholar]
- Peters, E. R. , Joseph, S. A. , & Garety, P. A. (1995). The measurement of delusional ideation in the normal population—Introducing the PDI (PEters et al. delusions inventory). Schizophrenia Research, 15(1–2), 19 10.1016/0920-9964(95)95071-G [DOI] [PubMed] [Google Scholar]
- Pornprasertmanit, S. , Miller, P. , Schoemann, A. , & Rosseel, Y. (2013). SemTools: Useful tools for structural equation modeling. R package version 0.3–2.
- Powers, A. R. , Kelley, M. S. , & Corlett, P. R. (2017). Varieties of voice‐hearing: Psychics and the psychosis continuum. Schizophrenia Bulletin, 43(1), 84–98. 10.1093/schbul/sbw133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti, A. , Cella, M. , Raballo, A. , & Vellante, M. (2012). Psychotic‐like or unusual subjective experiences? The role of certainty in the appraisal of the subclinical psychotic phenotype. Psychiatry Research, 200(2–3), 669–673. 10.1016/j.psychres.2012.07.014 [DOI] [PubMed] [Google Scholar]
- Preti, A. , Sisti, D. , Rocchi, M. B. L. , Siddi, S. , Cella, M. , Masala, C. , … Carta, M. G. (2014). Prevalence and dimensionality of hallucination‐like experiences in young adults. Comprehensive Psychiatry, 55(4), 826–836. 10.1016/j.comppsych.2014.01.015 [DOI] [PubMed] [Google Scholar]
- R Development Core Team (2012). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3‐900051‐07‐0, URL http://www.r-project.org/. R Foundation for Statistical Computing, Vienna, Austria.
- Raballo, A. , & Larøi, F. (2011). Murmurs of thought: Phenomenology of hallucinatory consciousness in impending psychosis. Psychosis, 3(2), 163–166. 10.1080/17522439.2010.529617 [DOI] [Google Scholar]
- Robin, X. , Turck, N. , Hainard, A. , Tiberti, N. , Lisacek, F. , Sanchez, J.‐C. , & Müller, M. (2011). pROC: An open‐source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics, 12(1), 77 10.1186/1471-2105-12-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ros‐Morente, A. , Vilagra‐Ruiz, R. , Rodriguez‐Hansen, G. , Wigman, J. H. , & Barrantes‐Vidal, N. (2011). Process of adaptation to Spanish of the Community Assessment of Psychic Experiences (CAPE). Actas Españolas de Psiquiatría, 39(2), 95–105. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21404148 [PubMed] [Google Scholar]
- Rosseel, Y. L. (2012). An R Package for structural equation modeling. Journal of Statistical Software, 48, 1–36. [Google Scholar]
- Sartorius, N. , Shapiro, R. , & Jablensky, A. (1974). The international pilot study of schizophrenia. Schizophrenia Bulletin, 1(11), 21–34. 10.1093/schbul/1.11.21 [DOI] [PubMed] [Google Scholar]
- Schwarz, G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. Retrieved from http://projecteuclid.org/euclid.aos/1176344136 [Google Scholar]
- Sclove, S. L. (1987). Application of model‐selection criteria to some problems in multivariate analysis. Psychometrika, 52(3), 333–343. 10.1007/BF02294360 [DOI] [Google Scholar]
- Serper, M. , Dill, C. A. , Chang, N. , Kot, T. , & Elliot, J. (2005). Factorial structure of the hallucinatory experience: Continuity of experience in psychotic and normal individuals. Journal of Nervous and Mental Disease, 193(4), 265–272. 10.1097/01.nmd.0000158374.54513.a0 [DOI] [PubMed] [Google Scholar]
- Siddi, S. , Petretto, D. R. , Burrai, C. , Scanu, R. , Baita, A. , Trincas, P. , … Preti, A. (2017). The role of set‐shifting in auditory verbal hallucinations. Comprehensive Psychiatry, 74 10.1016/j.comppsych.2017.01.011, 162–172. [DOI] [PubMed] [Google Scholar]
- Siddi, S. , Petretto, D. R. , Scanu, R. , Burrai, C. , Baita, A. , Trincas, P. , … Preti, A. (2016). Deficits in metaphor but not in idiomatic processing are related to verbal hallucinations in patients with psychosis. Psychiatry Research, 246 10.1016/j.psychres.2016.09.024, 101–112. [DOI] [PubMed] [Google Scholar]
- Smeets, F. , Lataster, T. , Dominguez, M. ‐d.‐G. , Hommes, J. , Lieb, R. , Wittchen, H.‐U. , & van Os, J. (2012). Evidence that onset of psychosis in the population reflects early hallucinatory experiences that through environmental risks and affective dysregulation become complicated by delusions. Schizophrenia Bulletin, 38(3), 531–542. 10.1093/schbul/sbq117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeets, F. , Lataster, T. , van Winkel, R. , de Graaf, R. , ten Have, M. , & van Os, J. (2012). Testing the hypothesis that psychotic illness begins when subthreshold hallucinations combine with delusional ideation. Acta Psychiatrica Scandinavica, 127(1), 34–47. 10.1111/j.1600-0447.2012.01888.x [DOI] [PubMed] [Google Scholar]
- Stanghellini, G. (2011). Phenomenological psychopathology, profundity, and sschizophrenia. Philosophy, Psychiatry, & Psychology, 18(2), 163–166. https://doi.org.ezproxy1.lib.asu.edu/10.1353/ppp.2011.0022 [Google Scholar]
- Stanghellini, G. , Langer, A. I. , Ambrosini, A. , & Cangas, A. J. (2012). Quality of hallucinatory experiences: Differences between a clinical and a non‐clinical sample. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 11(2), 110–113. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22654943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanis, N. C. , Hanssen, M. , Smirnis, N. K. , Avramopoulos, D. a. , Evdokimidis, I. K. , Stefanis, C. N. , … Van Os, J. (2002). Evidence that three dimensions of psychosis have a distribution in the general population. Psychological Medicine, 32(2), 347–358. 10.1017/S0033291701005141 [DOI] [PubMed] [Google Scholar]
- Steiger, J. H. (1990). Some additional thoughts on components, factors, and factor indeterminancy. Multivariate Behavioral Research 10.1207/s15327906mbr2501_4, 25, 41–45. [DOI] [PubMed] [Google Scholar]
- Stephan‐Otto, C. , Siddi, S. , Senior, C. , Muñoz‐Samons, D. , Ochoa, S. , Sánchez‐Laforga, A. M. , & Brébion, G. (2017). Visual imagery and false memory for pictures: A functional magnetic resonance imaging study in healthy participants. PLoS One, 12(1), e0169551 10.1371/journal.pone.0169551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os, J. , Linscott, R. J. , Myin‐Germeys, I. , Delespaul, P. , & Krabbendam, L. (2009). A systematic review and meta‐analysis of the psychosis continuum: Evidence for a psychosis proneness‐persistence‐impairment model of psychotic disorder. Psychological Medicine, 39(2), 179–195. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- Vellante, M. , Larøi, F. , Cella, M. , Raballo, A. , Petretto, D. R. , & Preti, A. (2012). Hallucination‐like experiences in the nonclinical population. The Journal of Nervous and Mental Disease, 200(4), 310–315. 10.1097/NMD.0b013e31824cb2ba [DOI] [PubMed] [Google Scholar]
- Waters, F. , Blom, J. D. , Dang‐Vu, T. T. , Cheyne, A. J. , Alderson‐Day, B. , Woodruff, P. , & Collerton, D. (2016). What is the link between hallucinations, dreams, and hypnagogic‐hypnopompic experiences? Schizophrenia Bulletin 10.1093/schbul/sbw076, 42, 1098–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters, F. A. V. , Badcock, J. C. , & Maybery, M. T. (2003). Revision of the factor structure of the Launay‐Slade Hallucination Scale (LSHS‐R). Personality and Individual Differences, 35(6), 1351–1357. 10.1016/S0191-8869(02)00354-9 [DOI] [Google Scholar]
- Wicherts, J. M. , & Dolan, C. V. (2004). A cautionary note on the use of information fit indexes in covariance structure modeling with means. Structural Equation Modeling: A Multidisciplinary Journal, 11(1), 45–50. 10.1207/S15328007SEM1101_3 [DOI] [Google Scholar]
- Yung, A. R. , Phillips, L. J. , Yuen, H. P. , Francey, S. M. , McFarlane, C. A. , Hallgren, M. , & McGorry, P. D. (2003). Psychosis prediction: 12‐Month follow up of a high‐risk (“prodromal”) group. Schizophrenia Research, 60(1), 21–32. 10.1016/S0920-9964(02)00167-6 [DOI] [PubMed] [Google Scholar]


