Abstract
The university system and students are rapidly growing and changing in low‐ and middle‐income countries (LMICs). This growth can facilitate enhanced national productivity yet it can also bring potential risks to student mental health. The World Mental Health Surveys International College Student (WMH‐ICS) initiative could increase information and support in a relatively low‐cost manner for university students in LMICs—a group that is particularly vulnerable to mental health problems and who live in an environment where few targeted resources may be available. Effective implementation of the WMH‐ICS initiative, however, requires long‐term planning and consideration of the specific challenges present in LMIC settings. Planning as to what types of interventions would be needed and achievable in the next 10 to 15 years and consideration of local issues related to uptake, acceptability, appropriateness, feasibility, fidelity, and sustainability from the very beginning would be needed to ensure that the initiative would be useful in the future.
1. INTRODUCTION
Mental health problems, in particular depression and anxiety, are as or more prevalent among university students compared with the general population (Auerbach et al., 2018; Ibrahim, Kelly, Adams, & Glazebrook, 2013). Transitioning to a new environment at university can provide not only increased opportunities for independence but also less structured time with greater potential to engage in risky behaviours, often while living far away from family and friends. These new and sometimes challenging circumstances emerge alongside increased pressures for academic achievement, all of which can contribute to a higher risk for mental health problems.
For students from low‐ and middle‐income countries (LMICs), these adjustments and pressures may be particularly severe given that so many of these students come from families in which neither of their parents attended university and in which pressures on the students are great to help elevate the socio‐economic positions of their entire families. And all this occurs in the context of the human and financial resources to support students in LMICs being highly constrained (Oppong Asante & Andoh‐Arthur, 2015; Shamsuddin et al., 2013). Given the potential impact of mental health problems on academic achievement and hence future life opportunities of these students, and the critical importance of nurturing a generation of university graduates for societal development, it is critical to understand how young people in LMICs can be supported so that their mental health problems do not undermine their educational attainment. Mental health related risk and protective factors, effective intervention strategies, and how best to implement them for university students in LMICs are all under‐researched issues. The aim of this viewpoint paper is to consider key questions related to the implementation of evidence for this target group.
2. CURRENT TRENDS IN HIGHER EDUCATION IN LMICs
The number of universities and university students has been steadily increasing worldwide, but this growth has been particularly great in many LMICs (Mullan et al., 2011). Between 2000 and 2016, for example, the proportion of adults enrolled in tertiary education increased 122% in low‐income countries (from 3.4% to 7.5%) and by 195% in upper middle‐income countries (from 17.2% to 50.7%; UNESCO Institute for Statistics, 2017). Indeed, in China, the increase in university students was over 500% during this time period. High‐income countries already have a much greater proportion of individuals enrolled in tertiary education compared with LMICs and showed a smaller increase of only of 33% between 2000 and 2016 (from 56.4% to 75% of young people; UNESCO Institute for Statistics, 2017; see Figure 1).
Figure 1.
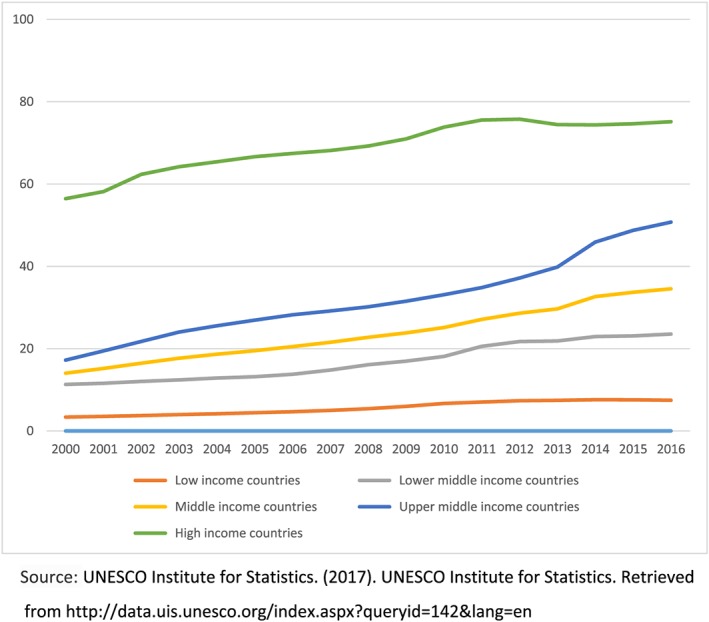
Percentage of adults enrolled in tertiary education since 2000 by World Bank country income classification
These enrolment figures are likely to continue growing given the prominence of higher education in the United Nations Sustainable Development Goals and in particular target 4.3, which focuses on increasing equitable access to tertiary education, including university (United Nations, 2015). The push for university expansion in LMICs may well also lead to changes in the types of students attending university in these countries (Schendel & McCowan, 2016). Although university education in LMICs was traditionally limited to a relatively small sector of elite families, it is anticipated that the expansion will lead to universities enrolling more students from socio‐economically deprived backgrounds in addition to higher numbers of women (Schendel & McCowan, 2016). This increased diversity at the university level in LMICs could have important consequences in terms of increasing equity in future leadership roles.
3. MENTAL HEALTH CONSEQUENCES OF UNIVERSITIES IN TRANSITION IN LMICs
Although such growth in the knowledge economy is undoubtedly a positive consequence of higher education expansion, the increased pressures on students and families associated with this transition can also increase vulnerability to mental health problems. Students from socio‐economically deprived backgrounds, in particular, are likely to have lower levels of preparation from primary and secondary school education, lower levels of financial resources, and a more limited social support network with knowledge of the skills needed to negotiate the demands of university life (Ibrahim, Kelly, & Glazebrook, 2012; Shamsuddin et al., 2013). Moreover, given the investment made by these individuals and families to attend university, the pressures under which students are operating to manifestly succeed may be intense. These conditions can make maintaining good mental health difficult because of the perceived stakes whereby obtaining a degree could secure the long‐term financial viability of the student and family, while the penalty of failure could have serious negative social and economic impacts. Under these circumstances, students who do develop mental illness may be reluctant to disclose this to their family, or to seek help if this may not be done confidentially.
There is a body of literature, mostly from high‐income countries, which demonstrates the particular challenges faced by individuals who are the “first in their family” to attend university (Brosnan et al., 2016; Southgate et al., 2017). These students may experience some similar challenges to students from LMICs around financial stress and lack of practical support from their family. This literature argues that these students may need additional support at university to be able to successfully complete their education. Most universities in LMICs, however, are ill equipped to deal with mental health challenges and faculty are often already fully stretched and have limited training about how to provide social or emotional support to students (Hakim et al., 2018; Mullan et al., 2011).
4. HOW CAN THE WORLD MENTAL HEALTH SURVEYS INTERNATIONAL COLLEGE STUDENT (WHO WMH‐ICS) INITIATIVE RESULTS BENEFIT STUDENTS WITH MENTAL HEALTH PROBLEMS IN LMICs?
Effective interventions exist for mental health promotion, prevention, and early intervention (Harrer et al., 2018), which can enormously improve outcomes for young people and hence alter trajectories in a way that lead to immediate as well as longer term benefits (Das et al., 2016; Davies, Morriss, & Glazebrook, 2014; Regehr, Glancy, & Pitts, 2013; Sandler et al., 2014). The WHO WMH‐ICS (Cuijpers, Ebert, Auerbach, Bruffaerts, & Karyotaki, 2018) provides an infrastructure to deliver evidence‐based, internet‐delivered interventions for mental health that are inexpensive and scalable. This platform uses a stepped‐care approach and also allows for monitoring of mental health and associated risk and protective factors over time alongside the intervention. The data collected from participants could therefore allow for stratifying the interventions based on which types of intervention demonstrate the greatest effectiveness for specific individuals or student groups, including those with less social or financial support.
The WHO WMH‐ICS also has potential to provide new evidence on how to improve access to effective interventions in order to improve mental health among university students in LMICs. The intervention is relatively low cost to the user—mainly relying on access to a mobile device and internet connectivity with relatively inexpensive coaching provided by trained laypersons. This means that the interventions will not require a high degree of specialised training or burden the health care workforce available in most LMICs. If the intervention did lead to greater recognition of mental health problems and increased help‐seeking, this could result in increased costs to the health and education sectors in the short term. However, appropriate intervention could also positively impact upon educational achievement and societal costs in the long term. The WHO WMH‐ICS interventions could also increase earlier access to support and reduce the stigma related barriers to accessing support (Clement et al., 2013; Semrau, Evans‐Lacko, Koschorke, Ashenafi, & Thornicroft, 2014) as the individual would not have to visit a mental health service and disclose their problems in person. This possible increase in the proportion of individuals with mental disorders who receive timely treatment has the potential not only to reduce the duration of untreated mental illness but also could have a positive impact on treatment effectiveness and reduce subsequent disorder persistence and severity.
5. IMPLEMENTATION CHALLENGES OF THE WHO WMH‐ICS IN LMICs
There are clearly potential benefits which could result from implementing the WHO WMH‐ICS in LMICs. At a minimum, implementation in LMICs would allow collection of data about the feasibility and effectiveness of e‐health intervention in LMIC contexts, where robust data are often limited (Das et al., 2016). The resulting impacts, however, would rely on effective implementation and uptake of the programme and recognition of the particular challenges that exist in LMICs. Indeed, the interventions are still at an early pilot stage, and evidence of feasibility, uptake, and effectiveness is still needed.
The WHO WMH‐ICS is currently being field tested. Although this is mainly being done in a selected number of high‐income countries, there are also data available from upper middle‐income countries: South Africa and Mexico (Auerbach et al., 2018; Benjet et al., in press; Mall et al., 2018; Mortier et al., 2018). Thus, even if intervention effectiveness were established in the pilot countries, this would not address whether and how the intervention works in other LMIC contexts. Additionally, the incentives for universities to participate in high‐income countries might not translate to LMIC settings. Given that few young people attend universities in LMICs, it may also be helpful to broaden the target group in LMIC contexts (including low‐income contexts) and consider other settings or training and apprenticeship programmes which are more commonly attended by young people in LMICs.
Additionally, given several key implementation issues require consideration. There is substantial heterogeneity between and within sites and attention needs to be taken to consider how to specifically adapt the WHO WMH‐ICS for participating LMICs sites or countries from the initial planning stages. First, although the programme would provide support for individuals to self‐manage their problems, a subset of those with more severe problems would require more intensive treatment, for example, from a specialist and appropriate referral systems would need to be put in place for this (Keynejad, Dua, Barbui, & Thornicroft, 2017). Given the lack of professional health care staff in LMICs, this would likely require additional effort to identify resources already available in that community. It may also need closer collaboration with health care professionals in that setting given that the intervention could increase demand for mental health treatment where the resources are limited. The university might also experience increased demands for support and given the likely pressures to expand quickly, careful discussions may be needed to make a case as to why they might invest in the WHO WMH‐ICS and divert limited resources from competing demands. The educational and economic advantages of student support need to be made clear to senior management at universities to support their decisions to invest in student mental health services. To this end, it is important for the initial waves of WMH‐ICS surveys to determine the strength of associations between mental disorders and subsequent school performance among students in LMICs.
In addition to such service supply side issues impacting on limited university or community resources, there would be another set of contextual factors, which would require consideration for tailoring and adaption to the country and/or university context. There are likely to be legal, ethical, technical, and cultural issues that may influence engagement, uptake, and even effectiveness of the intervention in different contexts. At the legal or regulatory level, there are likely differences in consent procedures and privacy policies, which would need to be addressed, for example, consideration of when, if at all, parents of students with mental illness would be informed of the condition. Students in some countries may also be less familiar with research and thus would require detailed explanation about the meaning of the trial and implications of their participation. Some religious beliefs and cultural values may also conflict with traditional therapeutic approaches (Scorzelli & Reinke‐Scorzelli, 1994; Shefer et al., 2013) and thus require adaptation to facilitate engagement and effectiveness (Bhugra & Bhui, 2006; Lewer, O'Reilly, Mojtabai, & Evans‐Lacko, 2015; Moodley & Palmer, 2014). Finally, limited internet connectivity in some countries may require a platform with a lower bandwith. Although the mobile health platform may mitigate stigma and privacy barriers to uptake, local factors to facilitate engagement should be considered given that it is largely a self‐management tool. The possibility might be considered, for example, of expanding the existing coaching aspects of the guided versions of the e‐interventions used in WMH‐ICS to include, that is, blended interventions, that is, combinations of internet and face‐to‐face interventions (Erbe, Eichert, Riper, & Ebert, 2017) and including, for example, social skills training related to the special demands of student life.
6. CONCLUSIONS
The WHO WMH‐ICS initiative is an exciting undertaking by virtue of the fact that is has potential to increase information and support for university students in LMICs—a group that is particularly vulnerable to mental health problems and who live in an environment where few targeted resources may be available. Moreover, data gathered from the WHO WMH‐ICS platform could help to distinguish key target groups that could benefit from interventions offered by the initiative and to identify ways of optimising the effects of these interventions in areas with limited data and resources for research. Achieving these targets requires long‐term planning considering implementation factors such as uptake, acceptability, appropriateness, feasibility, fidelity, and sustainability (Peters, Adam, Alonge, Agyepong, & Tran, 2013) from the very beginning in order to ensure that the programme is useful in the future.
Implementation and testing in LMICs will require recognition of the specific challenges present in those settings based on currently available evidence, but also planning as to what types of interventions are most needed and would be achievable over a time horizon of 10 to 15 years. It may be useful to consider how a “whole school” approach, which has been shown to be cost‐effective in secondary school settings in LMICs, could be integrated (Patel, 2018). Given the rapid expansion and changing demographics of universities in LMICs, the programme will need to plan for new types of users, circumstances, and potentially different types of mental health problems and changes in mental health resources available. These issues will need to be kept in mind right from the beginning and will require concerted collaboration with university structures and individuals working at the top, middle management, and ground levels to understand relevant policies and practices and ensure that people are on board to ensure the sustainability of this promising programme.
ACKNOWLEDGEMENTS
We would also like to thank Professors Vikram Patel, Ron Kessler, Corina Benjet, and Pim Cuijpers and Drs David Ebert and Randy Auerbach for their helpful feedback on the paper. GT is supported by the Medical Research Council and the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King's College London NHS Foundation Trust, and the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. S. E. L. is supported by the European Research Council under the European Union's Seventh Framework Programme (FP7/2007‐2013)/ERC grant agreement (337673), Medical Research Council, Economic and Social Research Council, and Global Challenges Research Fund.
Evans‐Lacko S, Thornicroft G. Viewpoint: WHO World Mental Health Surveys International College Student initiative: Implementation issues in low‐ and middle‐income countries. Int J Methods Psychiatr Res. 2019;28:e1756 10.1002/mpr.1756
REFERENCES
- Auerbach, R. P. , Mortier, P. , Bruffaerts, R. , Alonso, J. , Benjet, C. , Cuijpers, P. , … Kessler, R. C . (2018). Mental disorder risk profiles in the World Health Organization World Mental Health Surveys International College Student Project. International Journal of Methods in Psychiatric Research, (This issue). [Google Scholar]
- Benjet et al. (in press). Psychopathology and suicidality among incoming first year students in six Mexican universities. Salud Publica de Mexico [DOI] [PubMed]
- Bhugra, D. , & Bhui, K. (2006). Psychotherapy for ethnic minorities: Issues, context and practice. British Journal of Psychotherapy, 14(3), 310–326. 10.1111/j.1752-0118.1998.tb00385.x [DOI] [Google Scholar]
- Brosnan, C. , Southgate, E. , Outram, S. , Lempp, H. , Wright, S. , Saxby, T. , … Kelly, B. (2016). Experiences of medical students who are first in family to attend university. Medical Education, 50(8), 842–851. 10.1111/medu.12995 [DOI] [PubMed] [Google Scholar]
- Clement, S. , Schauman, O. , Graham, T. , Maggioni, F. , Evans‐Lacko, S. , Bezborodov, N. , … Thornicroft, G. (2013). Mental health stigma and access to care: A systematic review of quantitative and qualitative studies. In Press. [DOI] [PubMed] [Google Scholar]
- Cuijpers, P. , Ebert, D. D. , Auerbach, R. P. , Bruffaerts, R. , Karyotaki, E. , & Kessler, R . (2018). The WHO World Mental Health Initiative International College Student (WMH‐ICS) project: A systematic support system for mental health problems in college students. International Journal of Methods in Psychiatric Research, (This issue). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das, J. K. , Salam, R. A. , Lassi, Z. S. , Khan, M. N. , Mahmood, W. , Patel, V. , & Bhutta, Z. A. (2016). Interventions for adolescent mental health: An overview of systematic reviews. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 59(4S), S49–S60. 10.1016/j.jadohealth.2016.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies, E. B. , Morriss, R. , & Glazebrook, C. (2014). Computer‐delivered and web‐based interventions to improve depression, anxiety, and psychological well‐being of university students: A systematic review and meta‐analysis. Journal of Medical Internet Research, 16(5), e130 10.2196/jmir.3142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbe, D. , Eichert, H.‐C. , Riper, H. , & Ebert, D. D. (2017). Blending face‐to‐face and internet‐based interventions for the treatment of mental disorders in adults: Systematic review. Journal of Medical Internet Research, 19(9), e306 10.2196/jmir.6588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakim, J. G. , Chidzonga, M. M. , Borok, M. Z. , Nathoo, K. J. , Matenga, J. , Havranek, E. , … Campbell, T. B. (2018). Medical education partnership initiative (MEPI) in Zimbabwe: Outcomes and challenges. Global Health, Science and Practice, 6(1), 82–92. 10.9745/GHSP-D-17-00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer, M. , Adam, S. H. , Baumeister, H. , Cuijpers, P. , Karyotaki, E. , Auerback, R. P. , … Berking, M. E. D. (2018). Internet interventions for mental health in university students: A meta‐analysis. International Journal of Methods in Psychiatric Research, (This issue). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim, A. K. , Kelly, S. J. , Adams, C. E. , & Glazebrook, C. (2013). A systematic review of studies of depression prevalence in university students. Journal of Psychiatric Research, 47(3), 391–400. 10.1016/j.jpsychires.2012.11.015 [DOI] [PubMed] [Google Scholar]
- Ibrahim, A. K. , Kelly, S. J. , & Glazebrook, C. (2012). Analysis of an Egyptian study on the socioeconomic distribution of depressive symptoms among undergraduates. Social Psychiatry and Psychiatric Epidemiology, 47(6), 927–937. 10.1007/s00127-011-0400-x [DOI] [PubMed] [Google Scholar]
- Keynejad, R. C. , Dua, T. , Barbui, C. , & Thornicroft, G. (2017). WHO Mental Health Gap Action Programme (mhGAP) Intervention Guide: A systematic review of evidence from low and middle‐ income countries. Evid Based Mental Health Month, 0(0), 30–34. 10.1136/eb-2017-102750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewer, D. , O'Reilly, C. , Mojtabai, R. , & Evans‐Lacko, S. (2015). Antidepressant use in 27 European countries: Associations with sociodemographic, cultural and economic factors. British Journal of Psychiatry, 207(3), 221–226. 10.1192/bjp.bp.114.156786 [DOI] [PubMed] [Google Scholar]
- Moodley, R. , & Palmer, S. (2014). Race, culture and psychotherapy: Critical perspectives in multicultural practice Taylor and Francis; Retrieved from https://books.google.co.uk/books?hl=en&lr=&id=lbGOAwAAQBAJ&oi=fnd&pg=PA46&dq=related:f2UQ-mk-nO0J:scholar.google.com/&ots=9mGDwBxHx9&sig=oEAJrMbLVFMcxBq_QGf4ReOYSLI&redir_esc=y#v=onepage&q&f=false [Google Scholar]
- Mall, S. , Mortier, P. , Taljaard, L. , Roos, J. , Stein, D. J. , & Lochner, C. (2018). The relationship between childhood adversity, recent stressors, and depression in college students attending a South African university. BMC Psychiatry, 18(1), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier, P. , Auerbach, R. P. , Alonso, J. , Bantjes, J. , Benjet, C. , Cuijpers, P. , … WHO WMH‐ICS Collaborators . (2018). Suicidal thoughts and behaviors among first‐year college students: Results from the WMH‐ICS Project. Journal of the American Academy of Child & Adolescent Psychiatry, 57(4), 263–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullan, F. , Frehywot, S. , Omaswa, F. , Buch, E. , Chen, C. , Greysen, S. R. , … Neusy, A.‐J. (2011). Medical schools in sub‐Saharan Africa. The Lancet, 377(9771), 1113–1121. 10.1016/S0140-6736(10)61961-7 [DOI] [PubMed] [Google Scholar]
- Oppong Asante, K. , & Andoh‐Arthur, J. (2015). Prevalence and determinants of depressive symptoms among university students in Ghana. J Affect Disord. 15(171), 161–166. 10.1016/j.jad.2014.09.025. [DOI] [PubMed] [Google Scholar]
- Patel, V. (2018). SEHER trial. Lancet. [Google Scholar]
- Peters, D. H. , Adam, T. , Alonge, O. , Agyepong, I. A. , & Tran, N. (2013). Implementation research: What it is and how to do it. BMJ (Clinical Research Ed.), 347, f6753 10.1136/BMJ.F6753 [DOI] [PubMed] [Google Scholar]
- Regehr, C. , Glancy, D. , & Pitts, A. (2013). Interventions to reduce stress in university students: A review and meta‐analysis. Journal of Affective Disorders, 148(1), 1–11. 10.1016/j.jad.2012.11.026 [DOI] [PubMed] [Google Scholar]
- Sandler, I. , Wolchik, S. A. , Cruden, G. , Mahrer, N. E. , Ahn, S. , Brincks, A. , & Brown, C. H. (2014). Overview of meta‐analyses of the prevention of mental health, substance use, and conduct problems. Annual Review of Clinical Psychology, 10(1), 243–273. 10.1146/annurev-clinpsy-050212-185524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schendel, R. , & McCowan, T. (2016). Expanding higher education systems in low‐ and middle‐income countries: The challenges of equity and quality. Higher Education, 72(4), 407–411. 10.1007/s10734-016-0028-6 [DOI] [Google Scholar]
- Scorzelli, J. F. , & Reinke‐Scorzelli, M. (1994). Cultural sensitivity and cognitive therapy in India. The Counseling Psychologist, 22(4), 603–610. 10.1177/0011000094224006 [DOI] [Google Scholar]
- Semrau, M. , Evans‐Lacko, S. , Koschorke, M. , Ashenafi, L. , & Thornicroft, G. (2014). Stigma and discrimination related to mental illness in low‐ and middle‐income countries. Epidemiology and Psychiatric Sciences, 24(5), 382–394. 10.1017/S2045796015000359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamsuddin, K. , Fadzil, F. , Ismail, W. S. W. , Shah, S. A. , Omar, K. , Muhammad, N. A. , … Mahadevan, R. (2013). Correlates of depression, anxiety and stress among Malaysian university students. Asian Journal of Psychiatry, 6(4), 318–323. 10.1016/j.ajp.2013.01.014 [DOI] [PubMed] [Google Scholar]
- Shefer, G. , Rose, D. , Nellums, L. , Thornicroft, G. , Henderson, C. , & Evans‐Lacko, S. (2013). Our community is the worst: The influence of cultural beliefs on stigma, relationships with family and help‐seeking in three ethnic communities in London. International Journal of Social Psychiatry, 59(6), 535–544. 10.1177/0020764012443759 [DOI] [PubMed] [Google Scholar]
- Southgate, E. , Brosnan, C. , Lempp, H. , Kelly, B. , Wright, S. , Outram, S. , & Bennett, A. (2017). Travels in extreme social mobility: How first‐in‐family students find their way into and through medical education. Critical Studies in Education, 58(2), 242–260. 10.1080/17508487.2016.1263223 [DOI] [Google Scholar]
- UNESCO Institute for Statistics . (2017). UNESCO Institute for Statistics. Retrieved from http://data.uis.unesco.org/index.aspx?queryid=142&lang=en
- United Nations . (2015). Transforming our world: The 2030 agenda for sustainable development. Retrieved from https://sustainabledevelopment.un.org/post2015/transformingourworld


