Abstract
Objectives
The purpose of this study was to evaluate the prevalence of mixed features using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5) and to examine how patients with mixed states would be classified using the DSM‐5.
Methods
In total, 12 hospitals participated in this study, and data on the demographic characteristics and clinical diagnoses of patients treated between October 2013 and September 2016 were obtained. We reviewed the data for opposite‐polarity symptoms according to the DSM‐5 criteria and the research‐based diagnostic criteria.
Results
Of the 859 patients included in the final analysis, the prevalence of mixed features in patients with major depressive episodes based on the DSM‐5 remained low. Patients with major depressive disorder were more likely to be classified as experiencing anxious distress and/or a cluster‐B personality disorder in mixed state patients not diagnosed with DSM‐5 mixed features, whereas more mixed state patients with bipolar disorder were diagnosed with mixed features using the DSM‐5.
Conclusions
The prevalence of mixed features did not increase significantly when the DSM‐5 was used, and patients with mixed states were more likely to be classified as having anxious distress and/or a cluster‐B personality disorder in addition to mixed features.
Keywords: bipolar disorder, major depressive disorder, mixed features, prevalence
1. INTRODUCTION
Anxiety and agitation have been suggested to be core symptoms of a major depressive episode (MDE) with mixed features. However, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5) excluded these conditions from the mixed features criteria (Shim, Bae, & Bahk, 2016). Koukopoulos, Sani, and Ghaemi (2013) stated that mixed depression involved marked psychomotor agitation and that intrapsychic anguish and irritability are central features of mixed depression. Also, the research‐based diagnostic criteria (RBDC; Angst et al., 2011; Angst et al., 2013; Perugi et al., 2015), as well as the empirically based criteria for mixed depression developed in Benazzi (2008a, 2008b) came to similar conclusions. Sani, Vöhringer, et al. (2014) and Sani, Napoletano, et al. (2014) and Koukopoulos et al. (2007) included hypomanic symptoms such as agitation, irritability, racing thoughts, and distractibility/lability among the core symptoms of mixed depression.
Use of the DSM‐5 diagnostic criteria, which exclude several symptoms from the definition of MDE with mixed features, would capture only subthreshold nonoverlapping symptoms of the opposite pole (Vieta & Valenti, 2013) and may consequently reduce diagnostic power (Verdolini et al., 2015). Therefore, it is assumed that some patients with mixed features are likely to be diagnosed (using other specifiers) with comorbid disorders other than mixed features. It is important to review the diagnostic classifications because they may have significant effects on illness course, treatment choice and response, and prognosis (Sani, Napoletano, et al., 2014; Seo et al., 2018; Serretti, 2018; Shim, Woo, Jun, & Bahk, 2014).
The purpose of this study was to evaluate the prevalence of mixed features in a clinical setting applying the DSM‐5 diagnostic criteria. Finally, we investigated the diagnoses given to patients who were not classified as having mixed features under the DSM‐5 diagnostic criteria despite their meeting the criteria for mixed states according to the broader research‐based criteria (RBDC).
2. METHODS
2.1. Study population
In total, 12 hospitals in Korea participated in this study. All patients hospitalized at these institutions were diagnosed in accordance with the DSM‐5 by board‐certified psychiatrists based on a clinical interview. All psychiatrists were members of the Korean Bipolar Disorders Forum and met to discuss their similar diagnostic protocols at least four times annually. Between October 2013 and September 2016, subjects in this study satisfied the DSM‐5 criteria for MDE included in the category of mood disorders (major depressive disorder [MDD] and bipolar disorder [BD]). The following inclusion criteria were used: (a) DSM‐5 diagnosis of an MDE and mood disorders (MDD and BD) and (b) >18 years of age. The following exclusion criteria were also applied: insufficient data for assessment of the symptoms of DSM‐5 or RBDC in terms of mixed features; a severe comorbid medical and/or neurological illness that could contribute to manifestation of mood symptoms; a comorbid psychiatric condition such as schizophrenia or schizoaffective disorder that could involve mood symptoms; an intellectual disability (IQ < 70); and/or the presence of a cognition‐related disorder, including dementia, that could influence mood phenomenology.
The charts of 885 subjects diagnosed with MDE were assessed at baseline, and 26 cases were excluded. Of the remaining 859 patients, patients with nonpsychotic MDE (N = 672) were further classified to examine the prevalence of mixed states according to the RBDC to reduce reviewer bias due to psychotic symptoms. Because this was a retrospective chart review, it may be that the changes in affect (mood and behavior) caused by psychotic symptoms confounded the discrimination of mixed features, although psychotic symptoms are often more prevalent in mixed than nonmixed depression (Sani, Napoletano, et al., 2014; Sani, Vöhringer, et al., 2014).
2.2. Assessments
The index episode was defined as the MDE that triggered hospitalization between October 2013 and September 2016. If a patient was hospitalized more than once during the study period, data from only the last admission were studied. Data on the following were obtained from the charts of participants with regard to the index episode: demographic characteristics, including age and sex; clinical characteristics, including diagnosis (MDD or BD, further divided into bipolar I or II disorder), specifiers (with anxious distress, with mixed features, with melancholic features, with atypical features, with psychotic features, with catatonia, with peripartum onset, and with a seasonal pattern), and comorbid disorders. We investigated the prevalence of MDE focusing on mixed features with mood disorders, using DSM‐5 for original diagnostic assessments.
To evaluate the possible prevalence of latent mixed features, we reviewed the data for opposite‐polarity symptoms according to the RBDC. These are large‐scale research‐based criteria from the Bipolar Disorders: Improving Diagnosis, Guidance and Education study distinguishing bipolarity from MDE (Angst et al., 2011; Angst et al., 2013; Perugi et al., 2015). It is meaningful to compare prevalence rates using the RBDC and DSM‐5, because the RBDC may better reflect the clinical situation, as they include more clinical manifestations, such as overlapping symptoms. Patients with at least three of the RBDC symptoms during their MDE for ≥1 week were identified as possibly exhibiting a mixed state, even though they did not meet criteria for mixed features according to the DSM‐5: (a) irritable mood, (b) emotional/mood lability, (c) distractibility, (d) psychomotor agitation, (e) impulsivity, (f) aggression (verbal or physical), (g) racing thoughts, (h) increased talkativeness/pressure to keep talking, (i) risky behavior, (j) hyperactivity, (k) increased energy, (l) euphoria, (m) grandiosity, and (n) hypersexuality.
This study was designed to compare the prevalence of mixed features applying the DSM‐5 and RBDC. On the basis of the results, we attempted to discover how patients were diagnosed in clinical practice as having mixed state conditions by reference to the RBDC although they were not diagnosed with mixed features using DSM‐5.
2.3. Statistical analysis
All statistical analyses were carried out using SPSS for Windows software (ver. 18; SPSS Inc., Chicago, IL, USA). The chi‐square or Fisher's exact tests were used to analyze categorical variables, and the t test was used to analyze continuous variables. Logistic regression analyses were used to analyze relationships between categorical variables and demographic variables, such as age or sex, and the latter were also controlled for certain analyses. P values <0.05 were considered significant.
2.4. Ethics
This study was conducted according to the Declaration of Helsinki. Approval to conduct this retrospective chart review was obtained from the institutional review board of each institution. Additionally, because the data were obtained via routine psychiatric examinations, the boards decided that informed consent was unnecessary.
3. RESULTS
3.1. Demographic characteristics and clinical diagnoses of patients with MDE
The distribution of patients satisfying the criteria for MDE in a mood disorder is shown in Table 1. Of the 859 patients who were assessed in the final analysis, 552 had MDD and 307 had BD.
Table 1.
Demographic characteristics and clinical diagnoses using Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition of patients with major depressive episodes
| Variable | Total MDEs (N = 859) | MDD (N = 552) | BD (N = 307) | Significance (MDD vs. BD) | ||
|---|---|---|---|---|---|---|
| Age, mean (SD), years | 47.3 ± 18.29 | 49.0 ± 18.82 | 44.3 ± 16.91 | <0.001* | ||
| Female sex, N (%) | 531 (61.8) | 358 (64.9) | 173 (56.4) | 0.014* | ||
| Diagnosis, N (%) | ||||||
| Bipolar I | 226 (73.6) | |||||
| Bipolar II | 81 (26.4) | |||||
| Specifiers, N (%) | 410 (47.7) | 251 (45.5) | 159 (51.8) | 0.026* | ||
| Anxious | 184 (21.4) | 151 (27.4) | 33 (10.7) | <0.001* | ||
| Mixed | 56 (6.5) | 12 (2.2) | 44 (14.3) | <0.001* | ||
| Melancholic | 29 (3.4) | 24 (4.3) | 5 (1.6) | 0.031* | ||
| Atypical | 13 (1.5) | 9 (1.6) | 4 (1.3) | 0.425 | ||
| Psychotic | 168 (19.6) | 78 (14.1) | 90 (29.3) | <0.001* | ||
| Catatonia | 1 (0.1) | 0 | 1 (0.3) | >0.999 | ||
| Peripartum | 5 (0.6) | 4 (0.7) | 1 (0.3) | 0.458 | ||
| Seasonal | 18 (2.1) | 10 (1.8) | 8 (2.6) | 0.250 | ||
| Comorbidity, N (%) | ||||||
| Anxiety disorders | 41 (4.8) | 39 (7.1) | 3 (1.0) | 0.001* | ||
| Substance use disorders | 61 (7.1) | 40 (7.2) | 21 (6.8) | 0.652 | ||
| Personality disorders (PDs) | 144 (16.8) | 103 (18.7) | 41 (13.4) | 0.004* | ||
| Cluster A | 6 (0.7) | 4 (0.7) | 2 (0.7) | 0.726 | ||
| Cluster B | 111 (12.9) | 79 (14.3) | 32 (10.4) | 0.030* | ||
| Cluster C | 18 (2.1) | 14 (2.5) | 4 (1.3) | 0.093 | ||
| Other PD | 9 (1.0) | 6 (1.1) | 3 (1.0) | 0.691 | ||
Note. MDEs: major depressive episodes; MDD: major depressive disorder; BD: bipolar disorder.
P < 0.05.
We found significant differences in age and sex between the two groups. Patients with MDD were older (P < 0.001) and more likely to be female (P = 0.014) than were patients with BD. As the clinical characteristics of the two groups differed according to demographic factors, such as age and sex, we controlled for the latter variables.
Several significant differences in the clinical diagnoses given to members of the two groups, including with regard to specifiers (anxious distress, mixed features, and psychotic features) and comorbid conditions (anxiety disorders and personality disorders), were observed. The rates of anxious distress (27.4% vs. 10.7%; P < 0.001) and melancholic features (4.3% vs. 1.6%; P = 0.031) were significantly higher in patients with MDD than in those with BD. However, the rates of mixed features (2.2% vs. 14.3%; P < 0.001) and psychotic features (14.1% vs. 29.3%; P < 0.001) were significantly higher in patients with BD than in those with MDD. The rates of comorbid anxiety disorders (7.1% vs. 1.0%; P = 0.001) and personality disorders (18.7% vs. 13.4%; P = 0.004), particularly cluster‐B personality disorders (14.3% vs. 10.4%; P = 0.030), were higher in patients with MDD than in those with BD.
3.2. Diagnosis of mixed features according to different definitions in patients with nonpsychotic MDEs
The prevalence rates of mixed features determined using the DSM‐5 and the RBDC are summarized in Table 2. Of the 672 nonpsychotic patients with MDE, 473 had MDD and 199 had BD. We found significant differences in the demographic variables, such as age (49.3 ± 18.64 vs. 45.1 ± 18.00; P = 0.007) and female sex (65.1% vs. 51.8%; P = 0.001), of patients with MDD and those with BD.
Table 2.
Diagnosis of mixed features according to different definitions in patients with nonpsychotic major depressive episodes
| Variable | Total MDEs (N = 672) | MDD (N = 473) | BD (N = 199) | Significance (MDD vs. BD) | |
|---|---|---|---|---|---|
| Age, mean (SD), years | 47.43 ± 18.46 | 49.3 ± 18.64 | 45.1 ± 18.00 | 0.007* | |
| Female sex, N (%) | 512 (61.8) | 308 (65.1) | 103 (51.8) | 0.001* | |
| Different definitions | |||||
| Mixed features according to DSM‐5 criteria (MDE + >3 nonoverlapping hypomanic criteria) | 39 (5.8) | 8 (1.7) | 31 (15.6) | <0.001* | |
| Mixed states according to RBDC criteria (MDE + >3 hypomanic criteria) | 213 (31.7) | 90 (19.0) | 123 (61.8) | <0.001* | |
Note. RBDC: research‐based diagnostic criteria; MDEs: major depressive episodes; MDD: major depressive disorder; BD: bipolar disorder; DSM‐5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
P < 0.05.
When the MDEs involved at least three nonoverlapping hypomanic symptoms of mixed features included in the DSM‐5 criteria, the diagnostic criteria were satisfied in 5.8% of all nonpsychotic patients with MDEs; the prevalence of mixed features was significantly higher in those with BD than in those with MDD after adjusting for age and sex (1.7% vs. 15.6%; P < 0.001). According to the RBDC, MDEs with mixed states involve three or more hypomanic symptoms, and 31.7% of all nonpsychotic patients with MDEs satisfied this criterion. In particular, patients with BD were diagnosed with mixed states at significantly higher rates than those with MDD (19.0% vs. 61.8%; P < 0.001) after adjusting for age and sex.
3.3. Hypomanic symptoms in patients with nonpsychotic MDEs according to RBDC mixed states
The frequencies of hypomanic symptoms in mixed states according to the RBDC are summarized in Table 3. In total, 213 patients were diagnosed with mixed states according to the RBDC; 90 of these patients had MDD, and 123 had BD. As we found significant differences between the two groups in terms of the female sex (62.2% vs. 46.3%; P = 0.022), we reanalyzed the data on hypomanic symptoms controlling for sex.
Table 3.
Hypomanic symptoms in patients with nonpsychotic major depressive episodes according to research‐based diagnostic criteria (RBDC) mixed states
| Variable | Mixed states according to RBDC (N = 213) | Nonmixed features (not meet mixed features criteria in DSM‐5) in mixed states according to RBDC (N = 174) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | MDD (N = 90) | BD (N = 123) | Significance | Total | MDD (N = 82) | BD (N = 92) | Significance | ||
| Age, mean (SD), years | 44.3 ± 17.63 | 43.8 ± 16.35 | 44.7 ± 18.57 | 0.701 | 45.3 ± 17.92 | 44.5 ± 16.41 | 46.0 ± 19.22 | 0.587 | |
| Female sex, N (%) | 113 (53.1) | 56 (62.2) | 57 (46.3) | 0.022* | 85 (48.9) | 49 (59.8) | 36 (39.1) | 0.007* | |
| Hypomanic symptoms, N (%) | Irritable mood | 172 (90.8) | 73 (81.1) | 99 (80.5) | 0.854 | 140 (80.5) | 67 (81.7) | 73 (79.3) | 0.666 |
| Emotional/mood lability | 153 (71.8) | 81 (90.0) | 72 (58.5) | <0.001* | 124 (71.3) | 75 (91.5) | 49 (53.3) | <0.001* | |
| Distractibility | 86 (40.4) | 35 (38.9) | 51 (41.5) | 0.625 | 67 (38.5) | 31 (37.8) | 36 (39.1) | 0.790 | |
| Psychomotor agitation | 112 (52.6) | 61 (67.8) | 51 (41.5) | <0.001* | 99 (56.9) | 58 (70.7) | 41 (44.6) | 0.001* | |
| Impulsivity | 137 (64.3) | 60 (66.7) | 77 (62.6) | 0.516 | 111 (63.8) | 56 (68.3) | 55 (59.8) | 0.229 | |
| Aggression (verbal or physical) | 95 (44.6) | 34 (37.8) | 61 (49.6) | 0.104 | 72 (41.4) | 28 (34.1) | 44 (47.8) | 0.096 | |
| Racing thoughts | 13 (6.1) | 4 (4.4) | 9 (7.3) | 0.336 | 8 (4.6) | 2 (2.4) | 6 (6.5) | 0.202 | |
| More talkative/pressure to keep talking | 62 (29.1) | 8 (8.9) | 54 (43.9) | <0.001* | 40 (23.0) | 5 (6.1) | 35 (38.0) | <0.001* | |
| Hyperactivity | 59 (27.7) | 7 (7.8) | 52 (42.3) | <0.001* | 41 (23.6) | 2 (2.4) | 39 (42.4) | <0.001* | |
| Increased energy | 58 (27.2) | 5 (5.6) | 53 (43.1) | <0.001* | 43 (24.7) | 1 (1.2) | 42 (45.7) | <0.001* | |
| Risky behavior | 70 (32.9) | 30 (33.3) | 40 (32.5) | 0.995 | 55 (31.6) | 27 (32.9) | 28 (30.4) | 0.777 | |
| Grandiosity | 39 (18.3) | 3 (3.3) | 36 (29.3) | <0.001* | 30 (17.2) | 2 (2.4) | 28 (30.4) | <0.001* | |
| Euphoria | 53 (24.9) | 2 (2.2) | 51 (41.5) | <0.001* | 39 (22.4) | 2 (2.4) | 37 (40.2) | <0.001* | |
| Hypersexuality | 13 (6.1) | 1 (1.1) | 12 (9.8) | 0.037* | 9 (5.2) | 0 (0) | 9 (9.8) | 0.999 | |
Note. MDD: major depressive disorder; BD: bipolar disorder; DSM: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
P < 0.05.
Of the hypomanic symptoms, emotional/mood lability (90.0% vs. 58.5%; P < 0.001) and psychomotor agitation (67.8% vs. 41.5%; P < 0.001) were significantly more common in patients with MDD than in those with BD. However, increased talkativeness/pressure to keep talking (8.9% vs. 43.9%; P < 0.001), hyperactivity (7.8% vs. 42.3%; P < 0.001), increased energy (5.6% vs. 43.1%; P < 0.001), grandiosity (3.3% vs. 29.3%; P < 0.001), euphoria (2.2% vs. 41.5%; P < 0.001), and hypersexuality (1.1% vs. 9.8%; P = 0.037) were more prevalent in patients with BD than in those with MDD.
The most common hypomanic symptoms in patients with MDD were irritable mood, emotional/mood lability, psychomotor agitation, and impulsivity, which were excluded by the DSM‐5 because they are nonspecific and overlap both poles. However, in BD, overlapping symptoms as well as the nonoverlapping hypomanic symptoms included in the DSM‐5, such as increased talkativeness/pressure to keep talking, hyperactivity, increased energy, and euphoria, were also high.
3.4. Distribution of DSM‐5 diagnoses in patients with mixed states according to the RBDC
Figure 1 shows how patients with nonpsychotic MDEs who were classified as having mixed states according to the RBDC were diagnosed using any mood disorder specifier or psychiatric comorbidity, except mood disorder, in a clinical setting based on the DSM‐5.
Figure 1.
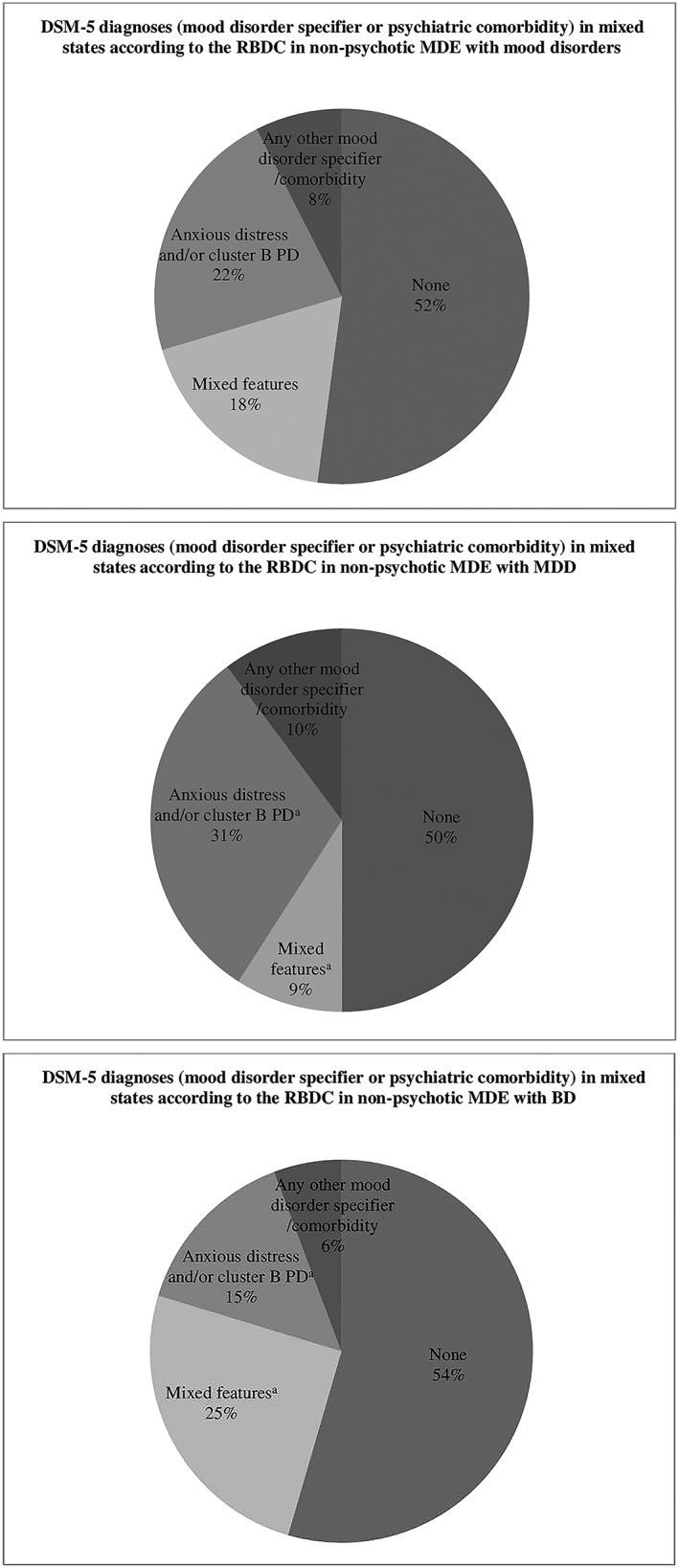
Distribution of Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5) diagnoses (mood disorder specifiers or psychiatric comorbidities) in patients with mixed states according to the research‐based diagnostic criteria (RBDC). * P < 0.05. MDE: major depressive episode; PD: personality disorder
Of the 213 patients with RBDC mixed states, 18% were diagnosed with mixed features using the DSM‐5, and an additional 22% were diagnosed with anxious distress or a cluster‐B personality disorder or with both anxious distress and a cluster‐B personality disorder. Additionally, 8% of patients received other specifiers or comorbidities (but not anxious distress) or a cluster‐B personality disorder. However, 52% were noted to have only mood disorders.
According to the DSM‐5, about 9% of patients with MDD were diagnosed with mixed features, whereas 25% of patients with BD were diagnosed with mixed features (P = 0.001). About 31% of patients with MDD who were not diagnosed with mixed features were diagnosed with anxious distress or a cluster‐B personality disorder or with both anxious distress and a cluster‐B personality disorder, but patients with BD showed a significant difference of about 15% (P = 0.005). About 50% of patients with MDD and 54% of patients with BD did not receive any further clinical diagnosis except mood disorder diagnosis.
4. DISCUSSION
This is the first study to review the classification of patients who were not diagnosed with mixed features when applying the new DSM‐5 diagnostic criteria, among patients with mixed state characteristics. This study may demonstrate the current limitations of the diagnostic criteria for mixed features presented in the DSM‐5.
This study found that 6.5% of patients with all MDEs had mixed features based on DSM‐5 criteria: This was the case for 14.3% of patients with BD and 2.2% of those with MDD (P < 0.05). According to the same criteria, the prevalence in patients with nonpsychotic MDEs was 5.8%, and it was 15.6% in those with BD and 1.7% in MDD. This is in close agreement with the low prevalence (7.5%; range, 2.6–23.3%) of mixed features overall (Perugi et al., 2015). The results of the present study show the similarity to strict criteria, such as the DSM‐IV‐Text Revision (TR; American Psychiatric Association, 2000); the Systematic Treatment Enhancement Program for Bipolar Disorder contends that 14.8% of patients with bipolar depression exhibit mixed episodes (Goldberg et al., 2009).
When the RBDC were applied, the overall prevalence of mixed states increased to 31.7%: 61.8% in BD and 19.0% in MDD. The results of the present study resemble those of an earlier study reporting that the prevalence of mixed states in those with depression was much higher according to research‐based than DSM‐based criteria (Kondo, Shinzato, & Koda, 2016). Although the prevalence of mixed states in those with depression differs among studies due to differences in the definition used, the rate has been estimated at 62.0–66.4% in BD and 12.8–32.5% in MDD, reflecting a significantly higher rate of mixed states in BD than in MDD (Benazzi, 2008b; Takeshima & Oka, 2015).
In contrast with a previous study, which predicted an increase in prevalence when comparing the DSM‐IV‐TR with the DSM‐5, the prevalence of mixed features did not significantly increase after applying the DSM‐5 in this study (McIntyre et al., 2015; Shim, Woo, & Bahk, 2015). Nevertheless, the prevalence of mixed states satisfying the RBDC was nearly identical to that in the existing data (Kondo et al., 2016). This means that the DSM did not identify patients who met the RBDC for mixed states as having mixed features. Thus, in a clinical situation, use of the DSM‐5 diagnostic criteria may render it difficult to identify mixed features even in a patient with mixed states, because these criteria exclude the overlapping hypomanic symptoms, such as anxiety or psychomotor agitation, distractibility, and irritability, which are key symptoms of mixed features. In this way, the DSM‐5 criteria exhibit lower sensitivity and higher specificity than the RBDC.
It should be noted that the prevalence of the anxious distress specifier, which was introduced in the DSM‐5, was higher than that of mixed features. In particular, the results presented in Figure 1 indicate that only 18% of the patients with mixed states according to the RBDC were diagnosed with mixed features based on the DSM‐5 and another 22% were diagnosed with anxious distress and/or a cluster‐B personality disorder. Patients with MDD were more likely than those with BD to be classified as having anxious distress rather than mixed features. This is associated with the difference in frequency of hypomanic symptoms between the two groups. Hypomanic symptoms (irritability, emotional/mood lability, psychomotor agitation, and impulsivity), which are common in MDD (Table 3), were mostly excluded from the DSM‐5 because of overlap. However, nonoverlapping hypomanic symptoms included in the DSM‐5, such as increased talkativeness/pressure to keep talking, hyperactivity, increased energy, and euphoria, were more frequent in patients with BD than in patients with MDD (Table 3). Because of this difference, those with MDD are likely to be classified as having anxious distress even though they show psychopathology similar to that shown by those with BD, who are likely to be diagnosed with mixed features. Anxious distress has some similarities to mixed features, as anxiety and psychomotor agitation are the main symptoms. Therefore, clinical evaluations of patients with anxiety or psychomotor agitation must determine whether patients have mixed or other features.
Interestingly, these results are in contrast to those of an earlier study reporting that patients with borderline personality disorder have a high prevalence of BD (Perugi et al., 2016). In this study, a cluster‐B personality disorder was more prevalent in patients with MDD than in those with BD. The low prevalence of BD II (less than 10% of the whole sample of MDE patients) in the present study could suggest that some BD II were not detected in routine clinical practice due to the difficulty of the patients to remember hypomanic symptoms when they were currently depressed. The association between borderline personality disorder and BD is stronger with BD II than BD I; it is possible that some borderline personality disorder plus BD II were in the MDD group, not in the BD group (Parker, 2014). Mixed features and a cluster‐B personality disorder seem to be consistent in that they have clinically similar psychopathologies and a high comorbidity rate (Dunayevich et al., 2000; George, Miklowitz, Richards, Simoneau, & Taylor, 2003). In this study, the incidence of cluster‐B personality disorders in patients with MDEs was >10% among those in both groups, which was higher than the prevalence of other comorbid conditions (Table 1). Additionally, patients with mixed states according to the RBDC who were not diagnosed with mixed features using the DSM‐5 were also diagnosed with a cluster‐B personality disorder at high rates in clinical settings (Figure 1). In particular, patients with both mixed features and a cluster‐B personality disorder may follow a complex course and show a reduced treatment response, warranting clinical attention (Perugi et al., 2016).
The present study has several limitations. First, because this was a retrospective study, there is a possibility that reviewer bias affected the evaluation of mixed states based on the RBDC. Some hypomanic symptoms, such as racing thoughts, might be underdetected in routine clinical practice because they were subjective symptoms. To reduce this bias, data from patients with MDEs accompanied by psychotic features that can be confused with the excitement of mixed features were excluded from the final analysis. Second, the interviews were neither structured nor semistructured and were inevitably not uniform because we performed only chart reviews. Third, we assessed only inpatients; thus, the results may not apply to outpatients. As a hospital chart contains more detailed information than an outpatient record, it might have been helpful in obtaining more detailed information.
Taken together, the data show that the prevalence of mixed features in all MDEs based on the DSM‐5 remained low, at a level similar to that obtained with DSM‐IV‐TR (mixed episode), with patients with BD showing a significantly higher prevalence than those with MDD. This suggests that the overall prevalence based on the DSM‐5 did not increase by excluding common overlapping hypomanic symptoms from the mixed features diagnostic criteria. Additionally, because the frequencies of hypomanic symptoms in patients with MDD and BD with mixed features differ, the prevalence in those with MDD was lower than that in those with BD when the same criteria were applied. Therefore, the majority of patients with MDD with mixed states according to the RBDC are likely to be classified as having anxious distress and/or a cluster‐B personality disorder according to the DSM‐5, whereas relatively more patients with BD are likely to be diagnosed with mixed features based on the DSM‐5. Future research is needed that carried out a psychometric analysis to attempt symptom clustering for mixed features empirically.
DECLARATION OF INTEREST STATEMENT
The authors declare no conflict of interest.
Shim IH, Lee J, Kim M‐D, et al. The prevalence and diagnostic classification of mixed features in patients with major depressive episodes: A multicenter study based on the DSM‐5. Int J Methods Psychiatr Res. 2019;28:e1773 10.1002/mpr.1773
Contributor Information
In Hee Shim, Email: ihshim1224@gmail.com.
Won‐Myong Bahk, Email: wmbahk@catholic.ac.kr.
REFERENCES
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, 4th edition, text version (DSM‐IV‐TR). Washington, DC: American Psychiatric Association. [Google Scholar]
- Angst, J. , Azorin, J.‐M. , Bowden, C. L. , Perugi, G. , Vieta, E. , Gamma, A. , … Group, B. S (2011). Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: The BRIDGE study. Archives of General Psychiatry, 68(8), 791–798. 10.1001/archgenpsychiatry.2011.87 [DOI] [PubMed] [Google Scholar]
- Angst, J. , Gamma, A. , Bowden, C. L. , Azorin, J. M. , Perugi, G. , Vieta, E. , & Young, A. H. (2013). Evidence‐based definitions of bipolar‐I and bipolar‐II disorders among 5,635 patients with major depressive episodes in the Bridge Study: Validity and comorbidity. European Archives of Psychiatry and Clinical Neuroscience, 263(8), 663–673. 10.1007/s00406-013-0393-4 [DOI] [PubMed] [Google Scholar]
- Benazzi, F. (2008a). Defining mixed depression. Progress in Neuro‐Psychopharmacology and Biological Psychiatry, 32(4), 932–939. 10.1016/j.pnpbp.2007.12.019 [DOI] [PubMed] [Google Scholar]
- Benazzi, F. (2008b). A tetrachoric factor analysis validation of mixed depression. Progress in Neuro‐Psychopharmacology and Biological Psychiatry, 32(1), 186–192. 10.1016/j.pnpbp.2007.08.005 [DOI] [PubMed] [Google Scholar]
- Dunayevich, E. , Sax, K. W. , Keck, P. E. Jr. , McElroy, S. L. , Sorter, M. T. , McConville, B. J. , & Strakowski, S. M. (2000). Twelve‐month outcome in bipolar patients with and without personality disorders. Journal of Clinical Psychiatry, 61(2), 134–139. 10.4088/jcp.v61n0209 [DOI] [PubMed] [Google Scholar]
- George, E. L. , Miklowitz, D. J. , Richards, J. A. , Simoneau, T. L. , & Taylor, D. O. (2003). The comorbidity of bipolar disorder and axis II personality disorders: Prevalence and clinical correlates. Bipolar Disorders, 5(2), 115–122. 10.1034/j.1399-5618.2003.00028.x [DOI] [PubMed] [Google Scholar]
- Goldberg, J. F. , Perlis, R. H. , Bowden, C. L. , Thase, M. E. , Miklowitz, D. J. , Marangell, L. B. , … Sachs, G. S. (2009). Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: Findings from the STEP‐BD. American Journal of Psychiatry, 166(2), 173–181. 10.1176/appi.ajp.2008.08050746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo, T. , Shinzato, H. , & Koda, M. (2016). Diagnostic and therapeutic considerations in depressive mixed state. Clinical Neuropsychopharmacology and Therapeutics, 7, 41–47. 10.5234/cnpt.7.41 [DOI] [Google Scholar]
- Koukopoulos, A. , Sani, G. , & Ghaemi, S. N. (2013). Mixed features of depression: Why DSM‐5 is wrong (and so was DSM‐IV). British Journal of Psychiatry, 203(1), 3–5. 10.1192/bjp.bp.112.124404 [DOI] [PubMed] [Google Scholar]
- Koukopoulos, A. , Sani, G. , Koukopoulos, A. E. , Manfredi, G. , Pacchiarotti, I. , & Girardi, P. (2007). Melancholia agitata and mixed depression. Acta Psychiatrica Scandinavica, 115(Supplementum(433)), 50–57. 10.1111/j.1600-0447.2007.00963.x [DOI] [PubMed] [Google Scholar]
- McIntyre, R. S. , Soczynska, J. K. , Cha, D. S. , Woldeyohannes, H. O. , Dale, R. S. , Alsuwaidan, M. T. , … Kennedy, S. H. (2015). The prevalence and illness characteristics of DSM‐5‐defined “mixed feature specifier” in adults with major depressive disorder and bipolar disorder: Results from the International Mood Disorders Collaborative Project. Journal of Affective Disorders, 172, 259–264. 10.1016/j.jad.2014.09.026 [DOI] [PubMed] [Google Scholar]
- Parker, G. (2014). Is borderline personality disorder a mood disorder? The British Journal of Psychiatry, 204(4), 252–253. 10.1192/bjp.bp.113.136580 [DOI] [PubMed] [Google Scholar]
- Perugi, G. , Angst, J. , Azorin, J. M. , Bowden, C. , Caciagli, A. , Mosolov, S. , … Young, A. (2016). Relationships between mixed features and borderline personality disorder in 2811 patients with major depressive episode. Acta Psychiatrica Scandinavica, 133(2), 133–143. 10.1111/acps.12457 [DOI] [PubMed] [Google Scholar]
- Perugi, G. , Angst, J. , Azorin, J. M. , Bowden, C. L. , Mosolov, S. , Reis, J. , … Young, A. H. (2015). Mixed features in patients with a major depressive episode: The BRIDGE‐II‐MIX study. Journal of Clinical Psychiatry, 76(3), e351–e358. 10.4088/jcp.14m09092 [DOI] [PubMed] [Google Scholar]
- Sani, G. , Napoletano, F. , Vohringer, P. A. , Sullivan, M. , Simonetti, A. , Koukopoulos, A. , … Ghaemi, N. (2014). Mixed depression: Clinical features and predictors of its onset associated with antidepressant use. Psychotherapy and Psychosomatics, 83(4), 213–221. 10.1159/000358808 [DOI] [PubMed] [Google Scholar]
- Sani, G. , Vöhringer, P. A. , Napoletano, F. , Holtzman, N. S. , Dalley, S. , Girardi, P. , … Koukopoulos, A. (2014). Koukopoulos' diagnostic criteria for mixed depression: A validation study. Journal of Affective Disorders, 164, 14–18. 10.1016/j.jad.2014.03.054 [DOI] [PubMed] [Google Scholar]
- Seo, J. S. , Bahk, W. M. , Wang, H. R. , Woo, Y. S. , Park, Y. M. , Jeong, J. H. , … Min, K. J. (2018). Korean Medication Algorithm for depressive disorders 2017: Third revision. Clinical Psychopharmacology and Neuroscience, 16(1), 67–87. 10.9758/cpn.2018.16.1.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serretti, A. (2018). The present and future of precision medicine in psychiatry: Focus on clinical psychopharmacology of antidepressants. Clinical Psychopharmacology and Neuroscience, 16(1), 1–6. 10.9758/cpn.2018.16.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim, I. H. , Bae, D. S. , & Bahk, W. M. (2016). Anxiety or agitation in mood disorder with mixed features: A review with a focus on validity as a dimensional criterion. Annals of Clinical Psychiatry, 28(3), 213–220. [PubMed] [Google Scholar]
- Shim, I. H. , Woo, Y. S. , & Bahk, W. M. (2015). Prevalence rates and clinical implications of bipolar disorder “with mixed features” as defined by DSM‐5. Journal of Affective Disorders, 173, 120–125. 10.1016/j.jad.2014.10.061 [DOI] [PubMed] [Google Scholar]
- Shim, I. H. , Woo, Y. S. , Jun, T. Y. , & Bahk, W. M. (2014). Mixed‐state bipolar I and II depression: Time to remission and clinical characteristics. Journal of Affective Disorders, 152‐154, 340–346. 10.1016/j.jad.2013.09.035 [DOI] [PubMed] [Google Scholar]
- Takeshima, M. , & Oka, T. (2015). DSM‐5‐defined ‘mixed features’ and Benazzi's mixed depression: Which is practically useful to discriminate bipolar disorder from unipolar depression in patients with depression? Psychiatry and Clinical Neurosciences, 69(2), 109–116. 10.1111/pcn.12213 [DOI] [PubMed] [Google Scholar]
- Verdolini, N. , Agius, M. , Ferranti, L. , Moretti, P. , Piselli, M. , & Quartesan, R. (2015). The state of the art of the DSM‐5 “with mixed features” specifier. The Scientific World Journal, 2015, 1–7. 10.1155/2015/757258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieta, E. , & Valenti, M. (2013). Mixed states in DSM‐5: Implications for clinical care, education, and research. Journal of Affective Disorders, 148(1), 28–36. 10.1016/j.jad.2013.03.007 [DOI] [PubMed] [Google Scholar]


