Abstract
There have been several attempts to identify individuals potentially at high risk for psychotic‐spectrum disorders using brief screening measures. However, relatively few studies have tested the psychometric properties of the psychosis screening measures in representative samples of adolescents. The main purpose of the present study was to analyse the prevalence, factorial structure, measurement invariance across gender, and reliability of the Youth Psychosis At‐Risk Questionnaire – Brief (YPARQ‐B) in a community‐derived sample of adolescents. Additionally, the relationship between YPARQ‐B, depressive symptoms, psychopathology, stress manifestations, and prosocial skills was analysed. One thousand and twenty students from high schools participated in a cross‐sectional survey. The YPARQ‐B, the Reynolds Adolescent Depression Scale, the Strengths and Difficulties Questionnaire, and the Student Stress Inventory – Stress Manifestations were used. A total of 85.1% of the total sample self‐reported at least one subclinical psychotic experience. We observed a total of 10.9% of adolescents with a cutoff score of ≥11 or 6.8% with a cutoff score of ≥13. The analysis of internal structure of the YPARQ‐B yielded an essentially unidimensional structure. The YPARQ‐B scores showed measurement invariance across gender. The internal consistency of the YPARQ‐B total score was 0.94. Furthermore, self‐reported subclinical psychotic experiences were associated with depressive symptoms, emotional and behavioural problems, poor prosocial skills, and stress manifestations. These results would appear to indicate that YPARQ‐B is a brief and easy tool to assess self‐reported subclinical psychotic experiences in adolescents from the general population. The assessment of these experiences in community settings, and its associations with psychopathology, may help us to enhance the possibility of an early identification of adolescents potentially at risk for psychosis and mental health problems.
Keywords: early detection, psychosis, risk, screening, YPARQ‐B
1. INTRODUCTION
During the last two decades, the early identification of individuals potentially at‐risk for psychotic‐spectrum disorders has become an extensive focus of research and debate (Addington, Stowkowy, & Weiser, 2015; Kline & Schiffman, 2014). Reliable identification of individuals at‐high risk and timely prophylactic intervention may delay, ameliorate, or prevent the onset to frank psychotic symptoms and other mental health disorders as well as reduce its possible impact on many levels (e.g. personal, familiar, educational, occupational) (Fusar‐Poli, Carpenter, Woods, & McGlashan, 2014). Moreover, it opens up the possibility of examining and understanding risk markers, protective factors, and possible etiological mechanisms of psychotic‐spectrum disorder prior to the clinical expression of the clinical disorder with the aim to conduce prophylactic treatments that may improve outcome (Fonseca‐Pedrero, Gooding, Ortuño‐Sierra, & Paino, 2016). These are key points within the Roadmap for Mental Health Research in Europe (ROAMER) (Wittchen, Knappe, & Schumann, 2014).
Psychotic symptoms and signs usually display their onset during late adolescence or early adulthood, many years before the clinical diagnosis is made (Fusar‐Poli et al., 2012a; Häfner & An Der Heiden, 1999). These preceding symptoms to the imminent clinical expression are usually called prodromal symptoms (Yung & McGorry, 1996). This phase is prospectively called “at‐risk mental state” (ARMS) or clinical high risk (CHR) state (Fusar‐Poli et al., 2014). Follow‐up studies carried out show that those individuals who report attenuated psychotic symptoms (APS), or psychotic‐like experiences (PLEs) have a greater probability of psychiatric outcome, particularly non‐affective psychotic disorders (Debbané et al., 2015; Fusar‐Poli et al., 2012a) as well as other mental problems (Fisher et al., 2013; Fusar‐Poli et al., 2014).
Moreover, these subclinical experiences and symptoms have been associated with the same demographic, environmental, and genetic risk factors (Linscott & van Os, 2013) and show similar deficits (e.g. neurocognitive, structural and functional brain abnormalities) to those found in patients with psychosis (Calkins et al., 2014; Fusar‐Poli et al., 2012b; Fusar‐Poli et al., 2007; Wolf et al., 2015). From the extended psychosis continuum model, the expression of psychosis phenotype fluctuates from a normal state of functioning, going from subclinical psychotic experiences and symptoms, toward its clinical manifestation in the form of certain psychotic‐spectrum disorder (Linscott & van Os, 2013; van Os, Linscott, Myin‐Germeys, Delespaul, & Krabbendam, 2009). The subclinical experiences which do not reach clinical threshold for psychosis state, that are not related with associated distress, help‐seeking behaviour and/or functional impairment, and that are continuously distributed across the general population, are known as PLEs.
At present there are several measurement instruments available for clinicians and researchers to document the presence, frequency, and severity of APS and PLEs (Addington et al., 2015; Kline & Schiffman, 2014). These measures have shown to be valid and efficient in identifying and recruiting high‐risk samples (Kline & Schiffman, 2014), To date, however, there is no gold standard of self‐report measure to assess CHR symptoms. The PRIME Screen (Miller, Cicchetti, Markovich, McGlashan, & Woods, 2004), the Prodromal Questionnaire (PQ) (Loewy, Bearden, Johnson, Raine, & Cannon, 2005), and the Youth Psychosis At‐Risk Questionnaire (YPARQ) or its brief version (YPARQ‐B) (Myles‐Worsley et al., 2007; Ord, Myles‐Worsley, Blailes, & Ngiralmau, 2004), are good examples of self‐report psychosis risk screening measures.
The YPARQ in particular, is a 92‐item tool specifically developed for screening CHR symptoms in adolescents. Based upon the Comprehensive Assessment of At‐Risk Mental States (CAARMS) (Yung et al., 2005), the YPARQ items assess positive, negative, and affective domains of psychosis phenotype. It was validated on 648 high school students in Palau, a region where familial cases of schizophrenia have been followed‐up extensively (Myles‐Worsley et al., 2007; Ord et al., 2004). There is also a brief version, the YPARQ‐B, which contains only 28 items. This abbreviated tool was derived from the most discriminating questions from the positive symptoms (Ord et al., 2004) of the CAARMS (Yung et al., 2005) in combination with criteria from the Personal Assessment and Crisis Evaluation (PACE) clinic of the Early Psychosis Prevention and Intervention Centre at the University of Melbourne, Australia.
Previous studies conducted showed that YPARQ‐B is a good measure to screen CHR symptoms and sublinical psychotic experiences in adolescents as well as young adults. The scores of this tool have demonstrated good internal consistency coefficients and temporal stability as well as adequate levels of sensitivity and specificity (Bedwell & Donnelly, 2005; Kline et al., 2014; Kline et al., 2015; Kline et al., 2012a, 2012b; Lee, Cho, Cho, Jang, & Kim, 2012). Furthermore, this tool has shown good correspondence with the most recognized interviews, such as the Structured Interview for Psychosis Risk Syndromes (SIPS) (Miller et al., 2003) and other psychosis risk screening measures. For instance, Kline et al. (2012a, 2012b) recommended that a screening threshold of (≥ 11) yielded sensitivity of 0.65, specificity of 0.76, and PPV of 0.65 with regard to SIPS CHR/psychosis diagnoses. However, the within‐sample optimized threshold was slightly higher (≥ 13) and yielded sensitivity of 0.65, specificity of 0.90, and positive predictive value (PPV) of 0.81. In another study, Kline et al. (2015), using the threshold of ≥13 found a sensitivity of 1.00, specificity of 0.80, PPV of 0.29, negative predictive value (NPV) of 1.00, and accuracy of 81%.
There is evidence indicating that APS and PLEs are relatively common during adolescence (Calkins et al., 2014; Kelleher et al., 2012c; Linscott & van Os, 2013; Schultze‐Lutter, Michel, Ruhrmann, & Schimmelmann, 2014). Epidemiological studies have demonstrated that the mean annual prevalence of the PLEs among adolescents aged 13 to 18 is 7.5% (Kelleher et al., 2012a). In addition, individuals with APS or PLEs show overlapping yet less severe deficits and impairments to those found in clinical samples. Adolescents with APS or sublinical psychotic experiences for instance, reported a high prevalence of mental axis I diagnoses as well as psychopathology symptoms related with depression, anxiety, suicide attempts, and internalizing and externalizing problems. Moreover, functional and social impairments and neurocognitive deficits have been also reported (Calkins et al., 2014; Fusar‐Poli et al., 2014; Fusar‐Poli et al., 2012b; Kelleher, Cederlöf, & Lichtenstein, 2014; Kelleher, Clarke, Rawdon, Murphy, & Cannon, 2013a; Kelleher et al., 2012c; Thompson et al., 2015). In this regard, the assessment of subclinical psychotic symptoms or experiences and their relationship with other mental health indicators, during adolescence and in community settings, may provide a window to the reliable identification of those at heightened risk for psychosis spectrum disorders. More accurate and comprehensive psychosis risk detection efforts under a close‐in strategy, may improve psychosis prevention within this age group.
Despite several efforts to define and measure psychotic symptoms and experiences, inadequate attention has been specifically directed towards samples of adolescents (Schimmelmann, Michel, Martz‐Irngartinger, Linder, & Schultze‐Lutter, 2015; Schimmelmann & Schultze‐Lutter, 2012). The current study will focus on the validity of YPARQ‐B to assess self‐reported subclinical psychotic experiences and its associations with several psychopathological psychometric indicators in a large sample of non‐clinical adolescents. To date, there have been several attempts to identify adolescents potentially at high risk for psychosis using brief psychosis risk screening measures; however, to the best of our knowledge, no previous studies have validated the YPARQ‐B in this age group. For instance, the factorial validity of the YPARQ‐B or the analysis of the reliability of the scores using modern psychometric approaches such us Item Response Theory (IRT) (Hambleton, Swaminathan, & Rogers, 1991) has not been conducted.
Within this research framework, the main purpose of the present study was to analyse the psychometric properties of the YPARQ‐B scores, as well as the relationship between self‐reported subclinical psychotic experiences and psychopathology in a community‐derived sample of adolescents. Deriving from this general goal are the following specific objectives: (a) to analyse the prevalence of the self‐reported subclinical psychotic experiences using the YPARQ‐B; (b) to test the factorial structure and measurement invariance across gender of the YPARQ‐B scores; (c) to examine the internal consistency and precision, through IRT, of the YPARQ‐B scores; (d) to analyse the relationship between self‐reported subclinical psychotic experiences and depression symptoms, behavioural and emotional problems, and stress manifestations.
Based on previous research, we hypothesized that subclinical psychotic experiences would be able to be reliably assessed, and found to be relatively common albeit low levels in this community sample. This tool is based on the most discriminating positive symptom questions of the CAARMS. Those items were used to calculate a positive symptom score in previous studies (Ord et al., 2004). Thus, we expected that the YPARQ‐B would be characterized by a one‐dimensional structure equivalent across gender. We also predicted that YPARQ‐B scores would be associated with psychopathology in this sample.
2. METHOD
2.1. Participants
In order to obtain a representative community sample, we recruited participants from different cities and different types of secondary schools (e.g. public, funded, and private) and vocational/technical schools belonging to Navarra and La Rioja (regions located in the north of Spain). Both rural and urban areas were represented, as well as a range of socio‐economic levels. We recruited students from a total of 10 schools, including educational and training centres. The initial sample included 1071 students, and we discarded data from participants who presented: (a) omissions of any demographics or items without responding (n = 31); and (b) scores in the range of outliers (n = 20) (e.g. scores higher than 2.5 standard deviations (SDs) in the subscales of the measures used). The final sample consisted of 1020 students, of which 392 were male (38.4%). The age of the participants ranged from 13 to 21 years‐old [mean [M] = 16.12 years; SD = 2.12). The age distribution of the sample was the following: 13 years (n = 60; 5.9%), 14 years (n = 171; 16.8%), 15 years (n = 253; 24.8%), 16 years (n = 169; 16.6%), 17 years (n = 118; 11.6%), 18 years (n = 126; 12.4%), and 19–21 years (n = 102; 12.1%).
2.2. Instruments
2.2.1. The YPARQ‐B
The YPARQ‐B is a 28‐item self‐report instrument (“yes”, “no”, or “unknown”), specifically developed to screen CHR symptoms during adolescence. In this study “yes” was scored as “1” and “no” or “unknown” as “0”. The Spanish adaptation of the YPARQ‐B was made in accordance with the international guidelines for test translation and adaptation (Muñiz, Elosua, & Hambleton, 2013).
2.2.2. The Reynolds Adolescent Depression Scale (RADS)
The Reynolds Adolescent Depression Scale (RADS) (Reynolds, 1987) assesses the severity of depressive symptoms in adolescents. It is composed of 30 items in a Likert response format with four options (1 = “almost never”, 2 = “hardly ever”, 3 = “sometimes”, 4 = “most of the time”). The RADS encompasses four empirically derived scales: anhedonia, somatic complaints, negative self‐evaluation, and dysphoric mood. The validated Spanish version of the RADS was used in the present study (Fonseca‐Pedrero et al., 2010).
2.2.3. The Strengths and Difficulties Questionnaire (SDQ)
The Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997) is a self‐report questionnaire that is widely used for the assessment of different emotional and behavioural problems related to mental health in adolescents. The SDQ is made up of a total of 25 statements distributed across five subscales: emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behaviour. The first four subscales yield a total difficulties score. In this study we used a Likert‐type response format with three options (0 = “Not true”, 1 = “Somewhat true”, 2 = “Certainly true”). The validated Spanish version of the SDQ was used in the present study (Ortuño‐Sierra, Chocarro, Fonseca‐Pedrero, Sastre i Riba, & Muñiz, 2015).
2.2.4. The Student Stress Inventory – Stress Manifestations (SSI‐SM)
The Student Stress Inventory – Stress Manifestations (SSI‐SM) (Fimian, Fastenau, Tashner, & Cross, 1989) is composed of a total of 22 items in a Likert‐type response format with five options (1 = “absolutely not”, 2 = “few times”, 3 = “sometimes”, 4 = “often”, and 5 = “a lot of times”). Items are grouped in three subscales: physiological responses (six items), emotional responses (10 items), and behavioural responses (six items). The total score is the sum of each subscale. In this study we used the validated Spanish version of the SSI‐SM (Escobar, Blanca, Fernández‐Baena, & Trianes, 2011; Ortuño‐Sierra, Fonseca‐Pedrero, Aritio‐Solana, & Chocarro de Luis, 2016).
2.3. Procedure
The questionnaires were administered collectively, in groups of 10 to 35 students, during normal school hours and in a classroom specially prepared for this purpose. For participants under 18, parents were asked to provide a written informed consent in order for their child to participate in the study. Participants were informed of the confidentiality of their responses and of the voluntary nature of the study. No incentive was provided for their participation. Administration took place under the supervision of the researchers. The study was approved by the research and ethic committee at the University of La Rioja.
2.4. Data analyses
First, we calculated descriptive statistics and the prevalence of the self‐reported subclinical psychotic experiences. Second, in order to analyse the internal structure of the YPARQ‐B scores confirmatory factor analysis (CFA) was used. Due to the fact that (a) no previous research have tested the underlying structure of the YPARQ‐B scores in adolescents, and (b) this tool map has only a positive dimension of psychotic symptoms (see Ord et al., 2004), thus a one‐dimensional factor model was tested. The weighted least squares means and variance adjusted (WLSMV) estimator for dichotomous items was used. The following goodness‐of‐fit indices were used: chi‐square (χ 2), Comparative Fit Index (CFI), Tucker–Lewis Index (TLI), root mean square error of approximation (RMSEA), and weighted root mean square residual (WRMR). Hu and Bentler (1999) suggested that RMSEA should be 0.06 or less for a good model fit and CFI and TLI should be 0.95 or more, though any value over 0.90 tends to be considered acceptable. For WRMR, values less than 0.95 indicate good model fit (for dichotomous outcomes) (Yu, 2002). Fourth, in order to test measurement invariance across gender, successive multigroup CFAs were conducted. Using Delta parameterization in Mplus, two steps on measuring invariance need to be considered: configural and strong invariance models (Muthén & Muthén, 1998–2012). The ΔCFI were used to determine in cases where nested models were practically equivalent.
Third, we examined internal consistency and test information function of the YPARQ‐B scores. To obtain a measure of the reliability of the scores, we calculated Ordinal alpha coefficients for categorical data (Zumbo, Gadermann, & Zeisser, 2007). Ordinal alpha is conceptually equivalent to Cronbach's alpha and it performs well for dichotomous data (Zumbo et al., 2007). Furthermore, the test information function was estimated. The information function is an extension of the reliability in Classical Test Theory, within IRT framework (Hambleton et al., 1991). Test information functions are related to the measurement precision (less error of measurement) and show the degree of precision at different levels of theta or latent trait (e.g. subclinical psychotic experiences). Theta scores are measured on an interval scale (M = 0; S 2 = 1).
Fifth, the associations between self‐reported YPARQ‐B scores and psychopathology were examined using two analyses: (a) Pearson's correlations, and (b) multiple logistic regression. The YPARQ‐B scores were dichotomized using the cutoff of ≥13, and RADS, SDQ, and SSI‐SM scores were used as predictor variables. Age and gender showed no significant associations with YPARQ‐B scores, these variables were not used as covariates.
3. RESULTS
3.1. Descriptive statistics and prevalence of subclinical psychotic experiences
Descriptive statistics for the subscales and total scores of the measuring instruments used are shown in Table 1. Descriptive statistics of the YPARQ‐B items are depicted in Table 2. As can be seen in Table 2, the prevalence of self‐reported subclinical psychotic experiences ranged from 0.06 (item 26, “Do things sound louder than usual to you?”) to 0.37 (item 15, “Have you noticed any unusual bodily sensations such as tingling, pulling, pressure, burning, cold, vibrations, drilling tearing or electricity?”). A total of 85.1% of the sample reported at least one item of the YPARQ‐B. We observed 10.9% of adolescents with a cutoff score of ≥11 (standard cutoff) and 6.8% with a cutoff score of ≥13. The norms for the YPARQ‐B scores were for the following percentiles 10, 20, 30, 40, 50, 60, 70, 80, 90, and 95, were 0, 1, 2, 3, 4, 5 7, 9, 12, and 14, respectively. No statistically significant differences were found by gender in the YPARQ‐B total score (t = 1.352; p = 0.187). Age was negatively associated with YPARQ‐B total score (r = −0.14, p < 0.05).
Table 1.
Descriptive statistics for the self‐report measures
| M | SD | Skewness | Kurtosis | Range | Ordinal alpha | |
|---|---|---|---|---|---|---|
| YPARQ‐B total score | 5.11 | 4.86 | 1.30 | 1.78 | 0–28 | 0.94 |
| RADS | ||||||
| Dysphoric mood | 16.18 | 4.39 | 0.60 | 0.02 | 8–32 | 0.76 |
| Anhedonia | 11.45 | 2.84 | 0.96 | 1.11 | 7–25 | 0.70 |
| Negative self‐evaluation | 12.77 | 4.24 | 1.12 | 1.13 | 8–32 | 0.83 |
| Somatic complains | 15.52 | 3.46 | 0.26 | –0.09 | 7–28 | 0.78 |
| SDQ | ||||||
| Emotional symptoms | 3.21 | 2.38 | 0.62 | –0.31 | 0–10 | 0.75 |
| Conduct problems | 2.02 | 1.70 | 1.05 | 1.26 | 0–10 | 0.72 |
| Peer problems | 1.88 | 1.84 | 1.33 | 2.00 | 0–10 | 0.74 |
| Hiperactive | 4.46 | 2.12 | 0.18 | –0.30 | 0–10 | 0.71 |
| Prosocial | 8.34 | 1.76 | –1.42 | 2.42 | 0–10 | 0.75 |
| Total dificultes | 11.57 | 5.51 | 0.55 | 0.00 | 0–30 | 0.84 |
| SSI‐SM | ||||||
| Emotional | 23.67 | 7.24 | 0.54 | 0.20 | 10–50 | 0.90 |
| Physiological | 10.96 | 3.47 | 1.08 | 1.83 | 6–27 | 0.78 |
| Behavioural | 10.37 | 3.20 | 1.04 | 1.98 | 6–29 | 0.79 |
Note: YPARQ‐B, Youth Psychosis At‐Risk Questionnaire – Brief; RADS, Reynolds Adolescent Depression Scale; SDQ, Strengths and Difficulties Questionnaire; SSI‐SM, Student Stress Inventory – Stress Manifestations.
Table 2.
Descriptive statistics and standardized factorial loadings for the Youth Psychosis At‐Risk Questionnaire – Brief (YPARQ‐B) items
| Standardized factorial loadings | |||||
|---|---|---|---|---|---|
| Item | M | SD | Total sample | Male | Female |
| 1 | 0.22 | 0.41 | 0.30 | 0.30 | 0.31 |
| 2 | 0.27 | 0.44 | 0.52 | 0.51 | 0.54 |
| 3 | 0.25 | 0.43 | 0.50 | 0.49 | 0.50 |
| 4 | 0.19 | 0.39 | 0.66 | 0.71 | 0.63 |
| 5 | 0.25 | 0.43 | 0.58 | 0.69 | 0.53 |
| 6 | 0.24 | 0.43 | 0.46 | 0.51 | 0.42 |
| 7 | 0.22 | 0.41 | 0.64 | 0.70 | 0.61 |
| 8 | 0.18 | 0.38 | 0.39 | 0.56 | 0.33 |
| 9 | 0.30 | 0.46 | 0.60 | 0.64 | 0.54 |
| 10 | 0.08 | 0.27 | 0.51 | 0.47 | 0.54 |
| 11 | 0.11 | 0.31 | 0.41 | 0.40 | 0.41 |
| 12 | 0.16 | 0.37 | 0.67 | 0.62 | 0.71 |
| 13 | 0.10 | 0.29 | 0.73 | 0.73 | 0.75 |
| 14 | 0.16 | 0.36 | 0.51 | 0.57 | 0.46 |
| 15 | 0.37 | 0.48 | 0.62 | 0.57 | 0.67 |
| 16 | 0.22 | 0.41 | 0.58 | 0.54 | 0.61 |
| 17 | 0.17 | 0.38 | 0.66 | 0.77 | 0.58 |
| 18 | 0.10 | 0.30 | 0.51 | 0.55 | 0.48 |
| 19 | 0.20 | 0.40 | 0.74 | 0.74 | 0.74 |
| 20 | 0.13 | 0.34 | 0.67 | 0.68 | 0.67 |
| 21 | 0.12 | 0.33 | 0.72 | 0.75 | 0.69 |
| 22 | 0.08 | 0.28 | 0.75 | 0.75 | 0.75 |
| 23 | 0.12 | 0.33 | 0.72 | 0.79 | 0.68 |
| 24 | 0.19 | 0.39 | 0.72 | 0.69 | 0.76 |
| 25 | 0.25 | 0.43 | 0.70 | 0.70 | 0.71 |
| 26 | 0.06 | 0.24 | 0.60 | 0.66 | 0.57 |
| 27 | 0.28 | 0.45 | 0.63 | 0.57 | 0.67 |
| 28 | 0.09 | 0.29 | 0.74 | 0.73 | 0.75 |
Note: For categorical items, the number of adolescents who responding affirmatively one item of the YPARQ‐B is the equal to the mean value × 100.
3.2. Factorial structure and measurement invariance of the YPARQ‐B scores across gender
Table 3 shows the goodness‐of‐fit indices for the one‐factorial model tested. This model yielded adequate goodness‐of‐fit indices for the total sample as well as for males and females. Due the fact that no previous studies have tested the factorial structure of the YPARQ‐B, and YPARQ‐B items are based in the positive dimension of psychosis phenotype, only a unidimensional model was tested. The standardized factor loadings for the whole sample as well as for males and females are shown in Table 2. The range of the factor loadings, for the total sample was from 0.30 (item 1) to 0.75 (item 22). All standardized factor loadings estimated were statistically significant (p < 0.01)
Table 3.
Goodness‐of‐fit indices for the hypothetical models tested and measurement invariance across gender
| Model | χ2 | df | CFI | TLI | RMSEA (90% IC) | WRMR | ΔCFI |
|---|---|---|---|---|---|---|---|
| One‐factor | 760.856 | 350 | .943 | .939 | .034 (.031–.037) | 1.279 | |
| Measurement invariance | |||||||
| Male (n = 392) | 525.837 | 350 | .937 | .932 | .036 (.029–.042) | 1.081 | |
| Female (n = 628) | 538.579 | 350 | .954 | .950 | .029 (.024–.034) | 1.079 | |
| Configural invariance | 1063.15 | 700 | .946 | .941 | .032 (.028–.036) | 1.527 | |
| Strong invariance | 1053.79 | 728 | .950 | .948 | .030 (.026–.034) | 1.559 | –.01 |
Note: χ2 = chi square; df = degrees of freedom; CFI = Comparative Fit Index; TLI = Tucker–Lewis Index; RMSEA = root mean square error of approximation; IC = interval confidence; WRMR = weighted root mean square residual; ΔCFI = change in Comparative Fix Index.
Given that the one‐factor model evidenced good model fit, we therefore tested the measurement invariance of the YPARQ‐B scores across gender. Prior to the analysis of measurement invariance across gender, we tested whether the one‐factor model showed a reasonably good fit to the data in each group separately (see Table 3). Goodness‐of‐fit indices for males and females were adequate. The configural invariance model in which no equality constraints across groups were imposed showed an adequate fit to the data. Next, a strong invariance model was tested with the item thresholds and factor loadings constrained to be equal across groups. The ΔCFI between the constrained and unconstrained models was under 0.01, indicating that strong measurement invariance across gender was supported for the YPARQ‐B scores.
3.3. Reliability estimation and accuracy of the YPARQ‐B scores
The internal consistency of the YPARQ‐B total scores, estimated with ordinal alpha, was 0.94. According to IRT framework, the study of measurement precision of the YPARQ‐B scores indicated that the information function provides an optimal estimation at the high latent‐trait (values between 0 and 2.8) (see Figure 1). The tool reduces its accuracy around the lowest level of the latent trait (< −2).
Figure 1.
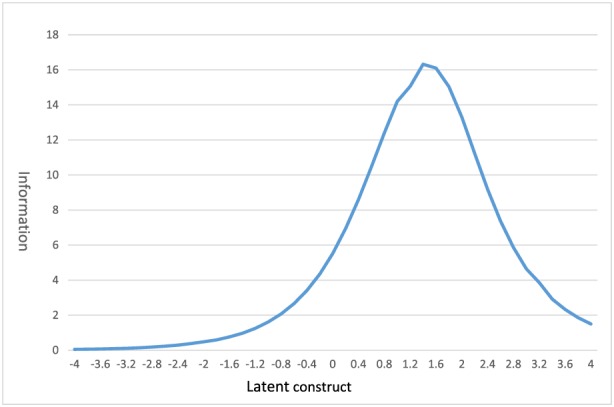
Test information function of the Youth Psychosis At‐Risk Questionnaire – Brief.
3.4. Associations between subclinical psychotic experiences and depressive symptoms, psychopathology, and stress manifestations
We calculated the Pearson's correlation between YPARQ‐B total score and the RADS, the SDQ, and the SSI‐SM scores. As shown in Table 4, all of the associations between YPARQ‐B scores and RADS, SDQ, and SSS‐SM subscales were statistically significant (p < 0.01). Only the correlation between YPARQ‐B and SDQ prosocial subscale was negatively associated. The multiple logistic regression model showed that the total score of the SDQ, negative self‐evaluation (RADS), prosocial (SDQ), and physiological manifestations (SSI‐SM) subscales predicted the YPARQ‐B scores of the high‐risk group (see Table 5). The adjusted R 2 for this regression model was 0.278. The Nagelkerke R 2 values were 0.222 (step 1), 0.249 (step 2), 0.264 (step 3), and 0.278 (step 4).
Table 4.
Pearson's correlations between Youth Psychosis At‐Risk Questionnaire – Brief (YPARQ‐B) and the Reynolds Adolescent Depression Scale (RADS), the Strengths and Difficulties Questionnaire (SDQ), and the Student Stress Inventory – Stress Manifestations (SSI‐SM) subscales
| Dysphoric mood | Anhedonia | Negative self‐evaluation | Somatic complains | |||
|---|---|---|---|---|---|---|
| YPARQ‐B/ RADS | 0.33** | 0.24** | 0.39** | 0.30** | ||
| Emotional | Conduct | Peer problems | Hiperactive | Prosocial | Total | |
| YPARQ‐B/ SDQ | 0.38** | 0.35** | 0.36** | 0.24** | –0,16** | 0.49** |
| Emotional | Physiological | Behavioural | ||||
| YPARQ‐B/ SSI‐SM | 0.36** | 0.34** | 0.28** |
p < 0.01.
Table 5.
Logistic regression model
| B | SE | Wald | p | OR | OR 95% CI | |||
|---|---|---|---|---|---|---|---|---|
| Step | Variable | Inferior | Superior | |||||
| 1 | SDQ total score | 0.206 | 0.022 | 89.23 | 0.001 | 1.229 | 1.177 | 1.283 |
| Constant | –5.274 | 0.376 | 196.42 | 0.001 | 0.005 | |||
| 2 | Negative self‐evaluation (RADS) | 0.098 | 0.027 | 13.19 | 0.001 | 1.103 | 1.046 | 1.163 |
| SDQ total score | 0.166 | 0.025 | 45.92 | 0.001 | 1.181 | 1.125 | 1.239 | |
| Constant | –6.125 | 0.459 | 178.36 | 0.001 | 0.002 | |||
| 3 | Negative self‐evaluation (RADS) | 0.115 | 0.028 | 17.14 | 0.001 | 1.122 | 1.063 | 1.185 |
| Prosocial (SDQ) | –0.171 | 0.060 | 8.22 | 0.004 | 0.843 | 0.749 | 0.947 | |
| SDQ total score | 0.147 | 0.025 | 34.11 | 0.001 | 1.159 | 1.103 | 1.217 | |
| Constant | –4.745 | 0.648 | 53.67 | 0.001 | 0.009 | |||
| 4 | Physiological (SSI‐SM) | 0.090 | 0.033 | 7.19 | 0.007 | 1.094 | 1.024 | 1.168 |
| Negative self‐evaluation (RADS) | 0.105 | 0.029 | 13.17 | 0.001 | 1.110 | 1.049 | 1.175 | |
| Prosocial (SDQ) | –0.202 | 0.062 | 10.78 | 0.001 | 0.817 | 0.724 | 0.922 | |
| SDQ total score | 0.125 | 0.027 | 21.79 | 0.001 | 1.133 | 1.075 | 1.195 | |
| Constant | –5.104 | 0.670 | 58.05 | 0.001 | 0.006 | |||
Note: The YPARQ‐B scores were dichotomized using the cutoff of >13.
4. DISCUSSION
The knowledge of the validity of YPARQ‐B scores is relevant in order to use it as a psychosis screening measure in community settings during adolescence, a developmental stage of special risk for the development of the first symptoms of psychosis and other mental disorders and symptoms. Furthermore, reliable assessment of subclinical psychotic experiences and symptoms in adolescents is essential for psychosis screening purposes in order to allow for the early identification of those potentially at‐risk for psychotic‐spectrum disorders (Addington et al., 2015; Kline & Schiffman, 2014) and in this way, allow for the implementation of prevention strategies such as further evaluation or early intervention to improve the outcome. To date, however, we have little information about the psychometric properties of the YPARQ‐B, as a psychosis risk screening tool in a community‐derived sample of adolescents. Moreover, the phenotypic expression of subclinical psychotic experiences and their associations with psychopathology have scarcely been analysed.
The main goal of the present study was to examine the prevalence, factorial structure, measurement invariance across gender, and reliability of the YPARQ‐B scores, as well as its associations with depression symptoms, psychopathology, and stress manifestations in a large sample of non‐clinical adolescents. If the main goal is to examine the liability for psychosis or to identify individuals potentially at‐high risk, then analysing the associations between subclinical psychotic experiences and psychopathology below clinical threshold, may help us to enhance the prediction of clinical outcome. It may be useful in the identification of clinical precursors and perhaps also to facilitate the study of etiopathogenic mechanisms for psychotic‐spectrum disorders. These are relevant issues in the ROAMER work (Wittchen et al., 2014).
The results revealed that YPARQ‐B is an easy, and brief tool to use for screening purposes. The psychometric properties of this measure were adequate in this sample. The internal consistency level, estimated with ordinal alpha, was good. Good use was also made of IRT as a modern psychometric approach, the tool measured with high accuracy individuals who scored at the high latent‐trait. Furthermore, the results suggested that subclinical psychotic experiences, using YPARQ‐B, is better considered as a unidimensional factor structure equivalent across gender. It is worth mentioning, that the YPARQ‐B was developed taking into account only the most discriminating items of the positive dimensions of the psychosis phenotype assessed by CAARMS interview (see Ord et al., 2004). This is, to our knowledge, the first empirical test of the factorial structure of the YPARQ‐B scores in a non‐clinical sample of adolescents, thus new research studies should be conducted in order to validate these findings. For instance, Fonseca‐Pedrero et al. (2016) using the brief version of the PQ‐Brief in a sample of non‐clinical adolescents, found a unidimensional factor structure.
Previous studies showed that YPARQ‐B is a good measure for screening CHR states and demonstrated adequate levels of predictive validity in adolescents and young adults at CHR for psychosis as well as convergence with other psychosis screening measures (e.g. SIPS, PQ), as well as good reliability coefficients (Kline & Schiffman, 2014; Kline et al., 2012a, 2012b, 2015; Myles‐Worsley et al., 2007; Ord et al., 2004). This empirical evidence suggests that this tool could be useful for more comprehensive identifying and recruiting strategies of individuals at CHR (Kline et al., 2015) as well as to expand its use to the non‐clinical population, such as educational and primary care settings, where a required specialized training (i.e. costs, time) is not possible. To date, not surprisingly, the psychometric data on self‐report measures is markedly variable across studies and are in their nascent stage (Fonseca‐Pedrero et al., 2016; Kline & Schiffman, 2014). They have also been criticized (Schultze‐Lutter et al., 2013). Thus, new empirical studies need to replicate the findings established here and define to what extent the new samples of the general population would be an important factor in future research.
The results showed that subclinical psychotic experiences are common in non‐clinical samples of adolescents. Although a total of 85.1% of the total sample reported at least one psychotic experience, only 6.8% scored higher using the standardized cutoff score (≥ 13 points). Prior studies have found similar results using self‐reports and interviews (Calkins et al., 2014; Kelleher et al., 2012a, 2012c). In particular, Kelleher et al. (2012a), conducted a meta‐analysis of PLEs during childhood and adolescence and found mean prevalence rates of around 17% in children from 9 to 12 years of age and 7.5% in adolescents from 13 to 18. For instance, Calkins et al. (2014) in a US representative sample of 7054 adolescents, revealed that between 3.8% and 17.6% of the sample endorsed “Definitely agree” on some psychotic symptom items. In another study, Fonseca‐Pedrero et al. (2016) using the PQ‐Brief found that 16% of the adolescents scored above the standardized cutoff. As it can be seen, previous empirical research have demonstrated that the frontiers of the psychosis phenotype extends beyond the traditional borders proposed by the international classification systems (e.g. ICD‐10; DSM‐5), which offers support to the existence of a psychometric phenotypic continuity between the clinical and subclinical psychosis phenotypes. Moreover, this set of experiences fall within a spectrum of “normal” developmental experiences and in most of the cases disappear over time and never progress to a clinical disorder (Linscott & van Os, 2013).
In addition, YPARQ‐B scores were moderate associated with a range of psychopathology symptoms at non‐clinical level such as depression, stress responses, emotional and behavioural problems and poor prosocial skills. In particular, emotional and behavioural symptoms, negative self‐evaluation, low prosocial skills, and physiological stress manifestations were the variables that predicted YPARQ‐B. It is important to bear in mind that all measures and the correlations between measures showed non‐normal distribution that may have several implications in the results found. Previous studies revealed similar results to those found in this study. For instance, adolescents who reported PLEs indicated a wide range of mental health problems, such as depressive symptoms (Armando et al., 2010; Yung et al., 2009), distress (Armando et al., 2010), emotional and behavioural problems (Wigman et al., 2011), sleep disturbances (Lee et al., 2012), childhood trauma and bullying (Kelleher et al., 2008, 2013b), suicidal behaviour (ideation, attempts) (Kelleher et al., 2014), cannabis used (Hides et al., 2009), and increase risk for multiple co‐occurring Axis I mental disorders (Kelleher et al., 2012b). For instance, Lee et al. (2012), in a sample of 8530 students, found that the YPARQ‐Q was positively correlated with the Beck Depression Inventory (r = 0.48, p < 0.001).
Furthermore, co‐morbidity with depression and emotional symptoms is one of the most replicate findings regarding CHR symptoms, APS, and PLEs in both clinical high risk samples and general population and predicted poorer clinical outcome (Krabbendam et al., 2005; Yung, Philips, Pan Yuen, & McGorry, 2004). The presence of self‐reported subclinical experiences during adolescence is associated with multiple concurrent psychopathology symptoms, and it appears to be a fundamental part of the CHR picture. These results have clear implications in the understanding of links between risk factors for psychosis before clinical debut and may help us to enhance the possibility of an early identification of adolescents at risk for psychosis.
According to the psychosis–proneness–persistence–impairment model formulated by van Os et al. (2009), the presence of schizotypal traits or PLEs during adolescence is not a necessary or sufficient condition for the later development of a psychotic disorder. Nonetheless, it is true that in a small group of adolescents such subclinical experiences and traits may interact synergistically or additively with genetic (e.g. family members with psychosis), environmental (e.g. trauma, migration, urbanicity, cannabis use), and/or psychological factors (e.g. depression, stress, anxiety, avoidance coping), becoming abnormally persistent and clinically relevant, leading to the development of clinical psychosis and need for care. The Gene‐x‐Environment interaction combined with the presence of other factors, such as, for example, the occurrence, severity, persistence, and associated distress of these traits and experiences, as well as associated social dysfunction and functional impairment, would explain the transition to the clinical outcome. The study of the extended psychosis phenotype from multiple levels of analyses and multiple indicators is essential in the new era of studies. For instance, it is possible that sequential screening uses the combination of several risk factors and multiple screening measures, from different levels of analyses (from genomics to self‐reports, as follow the guidelines of the Research Domain Criteria) to detect the early emergence of first onset psychosis. In a seminal comparison of two recruitment strategies, Rietdijk et al. (2012) found that sequential screening detected three times more individuals at risk of developing psychosis than the traditional case‐recruitment strategy.
The results obtained in the present study must be interpreted in light of the following limitations. First, adolescence is a developmental period in which personality is still consolidating. The present results must thus be further evaluated in order to understand their natural developmental course. Second, in the present study, we only investigated the YPARQ‐B as a psychosis risk screening measure in non‐clinical samples of adolescents. A new cross‐validation research could be recommended for further study. This tool is a self‐reporting tool with the problems inherent to any research based on these type of measures. Third, the extent to which screening measures for psychotic symptoms and experiences of psychosis may be associated with false positives in community samples is unclear. Fourth, these measures have been associated with stigmatization, negative labelling, and stereotypes (Schimmelmann & Schultze‐Lutter, 2012).
5. CONCLUSION
The results indicated that (a) YPARQ‐B scores showed adequate psychometric properties in this sample, and (b) self‐reported subclinical psychotic experiences and psychopathology are related during adolescence. Thus, the YPARQ‐B seems to be an interesting psychosis screening risk tool to measure this set of experiences in non‐clinical adolescents. More research is needed in order to establish reliable norms and screening thresholds for different settings, samples, and cultures. The role of the PLEs in the prediction of psychotic disorders and non‐psychotic disorders should continue to be explored in greater depth through independent longitudinal studies in both non‐clinical adolescent and participants potentially at‐high risk for psychosis.
DECLARATION OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ACKNOWLEDGEMENTS
The authors wish to thank the schools and students for their participation in this project. This research was funded by the Spanish Ministry of Science and Innovation (MICINN) (PSI2014‐56114‐P), 2015 edition of the BBVA Foundation Grants for Researchers and Cultural Creators, and by the Instituto Carlos III, Centre for Biomedical Research in Mental Health Network (CIBERSAM).
Fonseca‐Pedrero E, Ortuño‐Sierra J, Chocarro E, Inchausti F, Debbané M, Bobes J. Psychosis risk screening: Validation of the youth psychosis at‐risk questionnaire – brief in a community‐derived sample of adolescents. Int J Methods Psychiatr Res. 2017;26:e1543 10.1002/mpr.1543
REFERENCES
- Addington, J. , Stowkowy, J. , & Weiser, M. (2015). Screening tools for clinical high risk for psychosis. Early Intervention in Psychiatry, 9(5), 345–356. doi: 10.1111/eip.12193 [DOI] [PubMed] [Google Scholar]
- Armando, M. , Nelson, B. , Yung, A. R. , Ross, M. , Birchwood, M. , Girardi, P. , & Nastro, P. F. (2010). Psychotic‐like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophrenia Research, 119, 258–265. [DOI] [PubMed] [Google Scholar]
- Bedwell, J. S. , & Donnelly, R. S. (2005). Schizotypal personality disorder or prodromal symptoms of schizophrenia? Schizophrenia Research, 80, 263–269. [DOI] [PubMed] [Google Scholar]
- Calkins, M. E. , Moore, T. M. , Merikangas, K. R. , Burstein, M. , Satterthwaite, T. D. , Bilker, W. B. , … Gur, R. E. (2014). The psychosis spectrum in a young U.S. community sample: Findings from the Philadelphia Neurodevelopmental Cohort. World Psychiatry, 13(3), 296–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debbané, M. , Eliez, S. , Badoud, D. , Conus, P. , Flückiger, R. , & Schultze‐Lutter, F. (2015). Developing psychosis and its risk states through the lens of schizotypy. Schizophrenia Bulletin, 41, S396–S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar, M. , Blanca, M. J. , Fernández‐Baena, F. J. , & Trianes, M. V. (2011). Adaptación española de la escala de manifestaciones de estrés del Student Stress Inventory (SSI‐SM) [Spanish adaptation of the Stress Manifestations Scale of the Student Stress Inventory (SSI‐SM)]. Psicothema, 23, 475–485. [PubMed] [Google Scholar]
- Fimian, M. J. , Fastenau, P. A. , Tashner, J. H. , & Cross, A. H. (1989). The measure of classroom stress and burnout among gifted and talented students. Psychology in the Schools, 26, 139–153. [Google Scholar]
- Fisher, H. L. , Caspi, A. , Poulton, R. , Meier, M. H. , Houts, R. , Harrington, H. , … Moffitt, T. E. (2013). Specificity of childhood psychotic symptoms for predicting schizophrenia by 38 years of age: A birth cohort study. Psychological Medicine, 43, 2077–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca‐Pedrero, E. , Gooding, D. C. , Ortuño‐Sierra, J. , & Paino, M. (2016). Assessing self‐reported clinical high risk symptoms in community‐derived adolescents: A psychometric evaluation of the Prodromal Questionnaire – Brief. Comprehensive Psychiatry, 66, 1–8. [DOI] [PubMed] [Google Scholar]
- Fonseca‐Pedrero, E. , Wells, C. , Paino, M. , Lemos‐Giráldez, S. , Villazón‐García, U. , Sierra, S. , … Muñiz, J. (2010). Measurement invariance of the Reynolds Depression Adolescent Scale across gender and age. International Journal of Testing, 10, 133–148. [Google Scholar]
- Fusar‐Poli, P. , Bonoldi, I. , Yung, A. R. , Borgwardt, S. , Kempton, M. J. , Valmaggia, L. , … McGuire, P. (2012a). Predicting psychosis: Meta‐analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry, 69, 220–229. doi: 10.1001/archgenpsychiatry.2011.1472 [DOI] [PubMed] [Google Scholar]
- Fusar‐Poli, P. , Carpenter, W. T. , Woods, S. W. , & McGlashan, T. H. (2014). Attenuated Psychosis Syndrome: Ready for DSM‐5.1? Annual Review of Clinical Psychology, 10, 155–192. [DOI] [PubMed] [Google Scholar]
- Fusar‐Poli, P. , Deste, G. , Smieskova, R. , Barlati, S. , Yung, A. R. , Howes, O. , … Borgwardt, S. (2012b). Cognitive functioning in prodromal psychosis: A meta‐analysis. Archives of General Psychiatry, 69, 562–571. doi: 10.1001/archgenpsychiatry.2011.1592 [DOI] [PubMed] [Google Scholar]
- Fusar‐Poli, P. , Perez, J. , Broome, M. , Borgwardt, S. , Placentino, A. , Caverzasi, E. , … McGuire, P. (2007). Neurofunctional correlates of vulnerability to psychosis: A systematic review and meta‐analysis. Neuroscience and Biobehavioral Reviews, 31(4), 465–484. [DOI] [PubMed] [Google Scholar]
- Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. [DOI] [PubMed] [Google Scholar]
- Häfner, H. , & An Der Heiden, W. (1999). The course of schizophrenia in the light of modern follow‐up studies: The ABC and WHO studies. European Archives of Psychiatry and Clinical Neuroscience, 249(Suppl. 4), IV14–IV26. [DOI] [PubMed] [Google Scholar]
- Hambleton, R. K. , Swaminathan, H. , & Rogers, H. J. (1991). Fundamentals of Item Response Theory. Beverly Hills, CA: Sage Publications. [Google Scholar]
- Hides, L. , Lubman, D. I. , Buckby, J. , Yuen, H. P. , Cosgrave, E. , Baker, K. , & Yung, A. R. (2009). The association between early cannabis use and psychotic‐like experiences in a community adolescent sample. Schizophrenia Research, 112, 130–135. [DOI] [PubMed] [Google Scholar]
- Hu, L.‐T. , & Bentler, P. M. (1999). Cut off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Kelleher, I. , Cederlöf, M. , & Lichtenstein, P. (2014). Psychotic experiences as a predictor of the natural course of suicidal ideation: A Swedish cohort study. World Psychiatry, 13, 184–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelleher, I. , Clarke, M. C. , Rawdon, C. , Murphy, J. , & Cannon, M. (2013a). Neurocognition in the extended psychosis phenotype: Performance of a community sample of adolescents with psychotic symptoms on the MATRICS neurocognitive battery. Schizophrenia Bulletin, 39, 1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelleher, I. , Connor, D. , Clarke, M. C. , Devlin, N. , Harley, M. , & Cannon, M. (2012a). Prevalence of psychotic symptoms in childhood and adolescence: A systematic review and meta‐analysis of population‐based studies. Psychological Medicine, 9, 1–7. [DOI] [PubMed] [Google Scholar]
- Kelleher, I. , Harley, M. , Lynch, F. , Arseneault, L. , Fitzpatrick, C. , & Cannon, M. (2008). Associations between childhood trauma, bullying and psychotic symptoms among a school‐based adolescent sample. British Journal of Psychiatry, 193, 378–382. [DOI] [PubMed] [Google Scholar]
- Kelleher, I. , Keeley, H. , Corcoran, P. , Lynch, F. , Fitzpatrick, C. , Devlin, N. , … Cannon, M. (2012b). Clinicopathological significance of psychotic experiences in non‐psychotic young people: Evidence from four population‐based studies. British Journal of Psychiatry, 201, 26–32. doi: 10.1192/bjp.bp.1111.101543 [DOI] [PubMed] [Google Scholar]
- Kelleher, I. , Keeley, H. , Corcoran, P. , Ramsay, H. , Wasserman, C. , Carli, V. , … Cannon, M. (2013b). Childhood trauma and psychosis in a prospective cohort study: Cause, effect, and directionality. American Journal of Psychiatry, 170, 734–741. [DOI] [PubMed] [Google Scholar]
- Kelleher, I. , Murtagh, A. , Molloy, C. , Roddy, S. , Clarke, M. C. , Harley, M. , & Cannon, M. (2012c). Identification and characterization of prodromal risk syndromes in young adolescents in the community: A population‐based clinical interview study. Schizophrenia Bulletin, 38, 239–246. doi: 10.1093/schbul/sbr1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, E. , & Schiffman, J. (2014). Psychosis risk screening: A systematic review. Schizophrenia Research, 158, 11–18. [DOI] [PubMed] [Google Scholar]
- Kline, E. , Thompson, E. , Demro, C. , Bussell, K. , Reeves, G. , & Schiffman, J. (2015). Longitudinal validation of psychosis risk screening tools. Schizophrenia Research, 165, 116–122. [DOI] [PubMed] [Google Scholar]
- Kline, E. , Wilson, C. , Ereshefsky, S. , Denenny, D. , Thompson, E. , Pitts, S. C. , … Schiffman, J. (2012a). Psychosis risk screening in youth: A validation study of three self‐report measures of attenuated psychosis symptoms. Schizophrenia Research, 141, 72–77. [DOI] [PubMed] [Google Scholar]
- Kline, E. , Wilson, C. , Ereshefsky, S. , Tsuji, T. , Schiffman, J. , Pitts, S. , & Reeves, G. (2012b). Convergent and discriminant validity of attenuated psychosis screening tools. Schizophrenia Research, 134, 49–53. [DOI] [PubMed] [Google Scholar]
- Krabbendam, L. , Myin‐Germeys, I. , Hanssen, M. , de Graaf, R. , Vollebergh, W. , Bak, M. , & van Os, J. (2005). Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. British Journal of Clinical Psychology, 44, 113–125. [DOI] [PubMed] [Google Scholar]
- Lee, Y. J. , Cho, S. J. , Cho, I. H. , Jang, J. H. , & Kim, S. J. (2012). The relationship between psychotic‐like experiences and sleep disturbances in adolescents. Sleep Medicine, 13, 1021–1027. [DOI] [PubMed] [Google Scholar]
- Linscott, R. J. , & van Os, J. (2013). An updated and conservative systematic review and meta‐analysis of epidemiological evidence on psychotic experiences in children and adults: On the pathway from proneness to persistence to dimensional expression across mental disorders. Psychological Medicine, 43, 1133–1149. [DOI] [PubMed] [Google Scholar]
- Loewy, R. L. , Bearden, C. E. , Johnson, J. K. , Raine, A. , & Cannon, T. D. (2005). The prodromal questionnaire (PQ): Preliminary validation of a self‐report screening measure for prodromal and psychotic syndromes. Schizophrenia Research, 79(1), 117–125. [PubMed] [Google Scholar]
- Miller, T. , Cicchetti, D. , Markovich, P. , McGlashan, T. , & Woods, S. (2004). The SIPS Screen: A brief self‐report screen to detect the schizophrenia prodrome. Schizophrenia Research, 70(Suppl. 1), 78. [Google Scholar]
- Miller, T. J. , McGlashan, T. H. , Rosen, J. L. , Cadenhead, K. , Ventura, J. , McFarlane, W. , … Woods, S. W. (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin, 29(4), 703–715. [DOI] [PubMed] [Google Scholar]
- Muñiz, J. , Elosua, P. , & Hambleton, R. K. (2013). Directrices para la traducción y adaptación de los tests: segunda edición [International Test Commission Guidelines for test translation and adaptation: Second edition]. Psicothema, 25, 151–157. [DOI] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (1998–2012). Mplus User's Guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Myles‐Worsley, M. , Blailes, F. , Ord, L. M. , Weaver, S. , Dever, G. , & Faraone, S. V. (2007). The Palau Early Psychosis Study: Distribution of cases by level of genetic risk. American Journal of Medical Genetics, Part B (Neuropsychiatric Genetics), 144B, 5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ord, L. M. , Myles‐Worsley, M. , Blailes, F. , & Ngiralmau, H. (2004). Screening for prodromal adolescents in an isolated high‐risk population. Schizophrenia Research, 71, 507–508. [DOI] [PubMed] [Google Scholar]
- Ortuño‐Sierra, J. , Chocarro, E. , Fonseca‐Pedrero, E. , Sastre i Riba, S. , & Muñiz, J. (2015). The assessment of emotional and behavioural problems: Internal structure of the Strengths and Difficulties Questionnaire. International Journal of Clinical and Health Psychology, 15, 265–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortuño‐Sierra, J. , Fonseca‐Pedrero, E. , Aritio‐Solana, R. , & Chocarro de Luis, E. (2016). Stress assessment during adolescence: Psychometric properties and measurement invariance of the Student Stress Inventory – Stress Manifestations. The European Journal of Developmental Psychology, 13(5), 529–544. [Google Scholar]
- Reynolds, W. M. (1987). Reynolds Adolescent Depression Scale. Professional Manual. Odessa: Psychological Assessment Resources. [Google Scholar]
- Rietdijk, J. , Klaassen, R. , Ising, H. , Dragt, S. , Nieman, D. H. , van de Kamp, J. , … van der Gaag, M. (2012). Detection of people at risk of developing a first psychosis: Comparison of two recruitment strategies. Acta Psychiatrica Scandinavica, 126, 21–30. [DOI] [PubMed] [Google Scholar]
- Schimmelmann, B. G. , Michel, C. , Martz‐Irngartinger, A. , Linder, C. , & Schultze‐Lutter, F. (2015). Age matters in the prevalence and clinical significance of ultra‐high‐risk for psychosis symptoms and criteria in the general population: Findings from the BEAR and BEARS‐kid studies. World Psychiatry, 14, 189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimmelmann, B. G. , & Schultze‐Lutter, F. (2012). Early detection and intervention of psychosis in children and adolescents: urgent need for studies. European Child & Adolescent Psychiatry, 21, 239–241. [DOI] [PubMed] [Google Scholar]
- Schultze‐Lutter, F. , Michel, C. , Ruhrmann, S. , & Schimmelmann, B. G. (2014). Prevalence and clinical significance of DSM‐5‐attenuated psychosis syndrome in adolescents and young adults in the general population: The Bern Epidemiological At‐Risk (BEAR) study. Schizophrenia Bulletin, 40, 1499–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultze‐Lutter, F. , Renner, F. , Paruch, J. , Julkowski, D. , Klosterkötter, J. , & Ruhrmann, S. (2013). Self‐reported psychotic‐like experiences are a poor estimate of clinician‐rated attenuated and frank delusions and hallucinations. Psychopathology, 47, 194–201. [DOI] [PubMed] [Google Scholar]
- Thompson, E. , Kline, E. , Ellman, L. M. , Mittal, V. , Reeves, G. M. , & Schiffman, J. (2015). Emotional and behavioral symptomatology reported by help‐seeking youth at clinical high‐risk for psychosis. Schizophrenia Research, 162, 79–85. [DOI] [PubMed] [Google Scholar]
- van Os, J. , Linscott, R. J. , Myin‐Germeys, I. , Delespaul, P. , & Krabbendam, L. (2009). A systematic review and meta‐analysis of the psychosis continuum: Evidence for a psychosis proneness–persistence–impairment model of psychotic disorder. Psychological Medicine, 39, 179–195. [DOI] [PubMed] [Google Scholar]
- Wittchen, H.‐U. , Knappe, S. , & Schumann, G. (2014). Introduction to the ROAMER work package 5 consensus document: The psychological perspective on mental health and mental disorder research. International Journal of Methods in Psychiatric Research, 23(Suppl. 1), 15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigman, J. T. , Vollebergh, W. A. , Raaijmakers, Q. A. , Iedema, J. , van Dorsselaer, S. , Ormel, J. , … van Os, J. (2011). The structure of the extended psychosis phenotype in early adolescence – a cross‐sample replication. Schizophrenia Bulletin, 37, 850–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, D. H. , Satterthwaite, T. D. , Calkins, M. E. , Ruparel, K. , Elliott, M. A. , Hopson, R. D. , … Gur, R. E. (2015). Functional neuroimaging abnormalities in youth with psychosis spectrum symptoms. JAMA Psychiatry, 72, 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, C. Y. (2002). Evaluating Cutoff Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes, Doctoral dissertation . Los Angeles, CA: University of California.
- Yung, A. , Philips, L. J. , Pan Yuen, H. , & McGorry, P. D. (2004). Risk factors for psychosis in an ultra high‐risk group: Psychopathology and clinical features. Schizophrenia Research, 67, 131–142. [DOI] [PubMed] [Google Scholar]
- Yung, A. R. , & McGorry, P. O. (1996). The prodromal phase of first‐episode psychosis: Past and current conceptualizations. Schizophrenia Bulletin, 22(2), 353–370. [DOI] [PubMed] [Google Scholar]
- Yung, A. R. , Nelson, B. , Baker, K. , Buckby, J. A. , Baksheev, G. , & Cosgrave, E. M. (2009). Psychotic‐like experiences in a community sample of adolescents: Implications for the continuum model of psychosis and prediction of schizophrenia. Australian and New Zealand Journal of Psychiatry, 43, 118–128. doi: 10.1080/00048670802607188 [DOI] [PubMed] [Google Scholar]
- Yung, A. R. , Yuen, H. P. , McGorry, P. D. , Phillips, L. J. , Kelly, D. , Dell'Olio, M. , … Buckby, J. (2005). Mapping the onset of psychosis – the Comprehensive Assessment of At Risk Mental States (CAARMS). Australian and New Zealand Journal of Psychiatry, 39, 964–971. [DOI] [PubMed] [Google Scholar]
- Zumbo, B. D. , Gadermann, A. M. , & Zeisser, C. (2007). Ordinal versions of coefficients alpha and theta for Likert rating scales. Journal of Modern Applied Statistical Methods, 6, 21–29. [Google Scholar]


