Abstract
The current study examined the reliability and validity of a Danish adaptation of “Darryl”, a cartoon‐based measure of DSM‐IV symptoms of post‐traumatic stress disorder (PTSD) in a sample of Danish children and adolescents. Exposure to potentially traumatizing events, PTSD symptoms and diagnostic status were assessed in 65 children between the ages of 7 and 17 years old. Participants were recruited from a crisis centre for battered women and a school for children with emotional and behavioural problems. The study revealed that Darryl has good internal consistency for the overall scale and adequate reliability for each DSM‐IV symptom cluster. Scores from Darryl were significantly correlated with the Clinician Administered PTSD Scale for Children and Adolescents (CAPS‐CA) scores and receiver operating characteristic (ROC) analysis showed that it could significantly predict the presence of a PTSD diagnosis according to the CAPS‐CA. In comparison to the CAPS‐CA, Darryl has comparable psychometric properties and assesses PTSD symptoms in a developmentally appropriate manner. Furthermore, Darryl is quick to administer and was easier for the children in this sample to comprehend than the more traditional measure of PTSD. Overall, Darryl is an effective instrument for screening children at risk of a PTSD diagnosis. The relatively high specificity suggests that screening positive for PTSD using Darryl merits further diagnostic assessment. Copyright © 2016 John Wiley & Sons, Ltd.
Keywords: Darryl cartoon test, children, PTSD, validity, CAPS‐CA
Introduction
Exposure to traumatic events can lead to the development of post‐traumatic stress disorder (PTSD) which in turn can have serious consequences for a child's psychological and physiological wellbeing (Fairbank and Fairbank, 2009). It is therefore worrying that most child maltreatment and other potentially traumatic events remain undetected by local authorities and hospital wards (Christoffersen, 2010). Evidence from a Danish birth cohort indicated that while 5.6% reported experiencing physical abuse, only 1.1 % were known to the local authorities, and only 0.1% were registered at a hospital ward (Christoffersen, 2010). Routine screening for PTSD during an initial mental health assessment is therefore recommended by the American Academy of Child and Adolescent Psychiatry (Cohen et al., 2010). Exposure to traumatic events and the consequent development of PTSD symptoms can be very distressing for the child. It can influence normal development negatively and may result in cognitive, emotional, and behavioural difficulties (Margolin and Vickerman, 2007). This can lead to disruptions in both the social and the school environment.
Age‐specific features of PTSD in children
Children can develop PTSD either through direct exposure to, witnessing, or learning about potentially traumatizing events (McNally, 1996). A recent meta‐analysis which included 72 studies (N = 3563) reported an overall rate of 16% of PTSD in trauma exposed children and adolescents. This review highlighted the variability across studies in terms of type of trauma exposure and gender with interpersonal trauma and being female presenting with a higher risk (Alisic et al., 2014).
Children often express age‐specific features of PTSD that in some respect differ from adult PTSD symptomology (McNally, 1996). The Diagnostic and Statistical Manual for Metal Disorders (DSM‐IV: American Psychiatric Association, 2000), states that PTSD follows a traumatic event, which causes intense fear and/or perceived helplessness in an individual. This criterion has led to controversy regarding the classification of PTSD in children as many may not be able to self‐report these reactions (Scheeringa et al., 2012) but may instead show signs of disorganized or agitated behaviour. In regards to the individual PTSD symptom clusters outlined in the DSM‐IV (re‐experiencing, avoidance and hyperarousal), there are differences in how these symptoms may manifest in children. Children may express re‐experiencing symptoms through nightmares related to the trauma which over time can change into generalized nightmares involving threats to themselves or significant others. Likewise, intrusive memories are not always only manifested cognitively but can manifest through repetitive play re‐enacting the traumatic event (American Psychiatric Association, 2000). Symptoms of avoidance for children and adolescents include a sense of foreshortened future, where they believe they will not live long enough to become adults (Terr, 1990). Verbalizing and detecting avoidance symptoms can be difficult especially for younger children (Geller et al., 2007) and often information is needed from teachers or parents to establish the presence of these symptoms. Hyperarousal symptoms for children and adolescents include insomnia, irritability, and difficulties in concentrating. Additionally, children often exhibit somatic symptoms, such as headaches and stomach aches (Anthony et al., 1999). Thus, children exhibit PTSD in a different way to adults and it can be difficult for the child to understand and verbalize their psychological symptoms. Children are often assessed through parental report but it may be difficult for parents to detect symptoms due to their internal nature. Consistent with this research has shown that PTSD symptoms are often underreported by parents (Charuvastra et al., 2010). Combining parent and child reports when assessing children has been found to result in significantly higher endorsement rates of re‐experiencing, avoidance and hyperarousal symptoms when compared to using parent reports only (Meiser‐Stedman et al., 2008; Scheeringa et al., 2006).
Measures of PTSD in children
To date there are several existing interview forms and questionnaires designed to diagnose PTSD in children, e.g. the Schedule for Affective Disorders and Schizophrenia for School‐Age Children (K‐SADS; Puig‐Antich and Chambers, 1987), the Diagnostic Interview for Children and Adolescents‐Revised (DICA‐R; Reich et al., 1994), the Anxiety Disorder Interview Schedule Child (ADIS‐C; Silverman and Albano, 1996), and the Children's Post‐traumatic Stress Disorder Inventory (CPSDI: Saigh, 1998, cited in Yasik et al., 2001). Although some of these measures rely solely on abstract verbal or written material and are often very lengthy, studies have shown that children with PTSD often show lower neurocognitive outcomes (De Bellis et al., 1999) and in particular can have difficulties relating to executive functioning including attention (DePrince et al., 2009). Therefore, brief and effective screening measures for detecting PTSD symptomology especially for younger children are needed to identify children at risk and consequently offer them a more comprehensive diagnostic assessment and treatment. These screening instruments must incorporate PTSD symptoms as typically manifested in younger children. Furthermore, cognitive theory suggests that using a combination of visual and auditory stimuli (as opposed to only visual or auditory) is useful for maintaining the child's attention and focusing the child's interest. This is likely to lead to more effective information‐processing and a better understanding of abstract concepts (Valla et al., 2000). A combination of both visual and auditory stimuli have been utilized in cartoon tests, such as the Young Children's Critical Illness Impact Scale (Y‐CCIIS; Rennick et al., 2014) used to measure psychological distress in school‐aged children admitted to paediatric intensive care units and the “Darryl” (Neugebauer et al., 1999) which measures PTSD symptoms in school‐aged children.
Validation of the Darryl cartoon test
In this study, the psychometric properties of “Darryl”, a cartoon based measure of DSM‐IV PTSD symptoms in children, are explored. “Darryl” was developed by Neugebauer et al. (1999) to assess PTSD symptoms in school aged children exposed to community violence. The original study which examined the reliability and validity of the Darryl in a non‐clinical sample of 110 children (aged seven to nine) found that it had an excellent overall internal consistency (α = 0.92) and was significantly associated with child (r = 0.48, p < 0.0001) and adult (r = 0.29, p < 0.006) reports of exposure to community violence. Using a sample of 49 children and adolescents from an outpatient psychiatry clinic, Geller et al. (2007) found that the Darryl had demonstrated excellent internal consistency (r = 0.90). Furthermore, overall scores of the Darryl were significantly correlated with the overall scores of the Child's Post‐traumatic Stress Disorder – Reaction Index (r = 0.64, p = 0.001) and the child measure of exposure to violence (rho = 0.28, p < 0.05). Lastly, the utility of the Darryl as a screening tool was explored using the Childhood Disorders Version of the Structured Clinical Interview for DSM‐IV (KID‐SCID). However, only 2% (n = 2) of the sample were diagnosed with PTSD using the KID‐SCID, and 16% of the sample (n = 8) screened positive for PTSD using the Darryl. A sensitivity of 100% and specificity of 83% was found for the Darryl in relation to the KID‐SCID module. Given the limited number of PTSD diagnoses in the sample, further evidence concerning the specificity and sensitivity of the Darryl is needed.
The Danish version of the Darryl has been credited with validity as a screening measure for identifying childhood PTSD symptomatology (Elklit et al., 2013; Rønholt et al., 2013). The current study aims to examine the Darryl's reliability and validity in a sample of children exposed to family violence. The current study will also provide an opportunity for an initial evaluation of Darryl's sensitivity and specificity as a screening tool for PTSD in comparison to a semi‐structured clinical interview using a Danish version of the Clinician Administered PTSD Scale for Children and Adolescents (CAPS‐CA).
Method
Participants
The study included two samples of children between 7 and 17 years. Altogether, 65 children (25 girls and 40 boys) with a mean age of 11.3 years [standard deviation (SD) 2.7] at assessment participated in the study. Nineteen children were between seven and nine years of age, 27 children were 10–12 years, and 28 children were between 13 and 17 years of age.
The first sample consisted of 43 children (19 girls, 24 boys) with a mean age 10.86 years (SD 2.79) from a large crisis centre for battered women located in the southern region of Denmark. These children were admitted to the crisis centre along with their mother and siblings and had experienced a history of family violence. The second sample consisted of 22 children (six girls, 16 boys) with a mean age of 12.61 (SD 2.34) attending an all‐day school in the southern region of Denmark for children with emotional and/or behavioural problems. The samples were significantly different in relation to age (F (1, 69) 7.50; p < 0.01) and there was no significant difference in terms of gender. Almost half (18), of the children from the crisis centre and only one child from the all‐day school had parents who had not been born in Denmark. A previous study (Laursen and Elklit, 2009) found that pupils attending this type of school had often been exposed to a considerable number of potentially traumatic events during childhood such as domestic violence, alcohol and drug abuse, parental mental health problems, divorce, step fathers, and temporary foster homes. Participants were recruited from the all‐day school and the crisis centre due to the high rates of exposure to domestic violence.
Procedure
Sample 1
All mothers of children between 7 and 17 years old who were admitted to the crisis centre from January 2010 until December 2011 were invited to participate in the study. If the mother provided informed consent and the child agreed to participate, the two study measures were administered to the children by a trained and highly experienced psychologist employed by the crisis centre. Children who did not have sufficient language capabilities or children who were strongly emotionally affected by the family violence and the admittance to the crisis centre were omitted from the study. Children in a crisis centre face many environmental challenges. For example, their family situations are often chaotic and their placement within the crisis centre may only last a few days. Whilst in the centre families are also in contact with health, social and public services. These factors therefore limit the opportunities the psychologist has to interact with the child in an environment that is both suitable for research purposes and for the child to be comfortable and able to concentrate on the task. All measures in this sample were scored by two independent individuals.
Sample 2
All parents of children attending the school in January 2012 received written information about the study and were invited to participate. If the parents provided informed consent and the child agreed to participate, the two study measures were administered by a trained psychologist from the Danish National Centre for Psychotraumatology. The project was approved by the Regional Scientific Ethical Committees for Southern Denmark.
Measures
Darryl
Darryl (“Thomas” in Danish) is a cartoon‐based instrument, designed to measure all the central DSM‐IV PTSD symptoms among school‐age children who have experienced one or more potentially traumatic events (Neugebauer et al., 1999). The pictures illustrate emotional, cognitive, or behavioural symptoms of PTSD (see Figure 1). The Darryl does not measure flashbacks or dissociation symptoms of PTSD as these are difficult to convey to young children. The cartoons feature Darryl, a young boy of indeterminate ethnicity, and each cartoon depicts a different PTSD symptom. The interviewer reads aloud a short script describing the symptom content. The response choices are “never”, “some of the time” or “a lot of the time” and are coded as zero, one or two, respectively (Neugebauer et al., 1999). The scoring algorithm for Darryl entails summing responses across items that correspond to DSM‐IV criteria. Therefore, the possible range of scores is 0–38.
Figure 1.
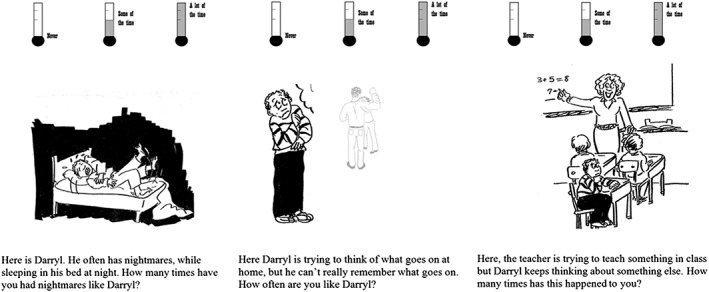
Items from the Danish version of the Darryl cartoon‐based measure of PTSD exemplifying symptoms of re‐experiencing, avoidance, and hyperarousal.
Due to prior knowledge that the sample was victims of family violence they were not asked specifically about any other type of trauma. The version utilized in the present study adapted illustrations to depict domestic scenes rather than the original illustrations which captured community violence. A sample question relating to domestic violence or alcohol consumption was illustrated with the caption “When Darryl's parents fight or drink” which follows an illustration capturing this image. The theme of domestic violence and an unsafe family environment was introduced and repeated several times.
The Darryl version employed in the present study contained 20 items designed to measure DSM‐IV PTSD symptomology in children. The symptoms were divided into the following core symptom clusters: re‐experiencing (six items), avoidance (seven items), and hyperarousal (five items). The nightmare criterion in the re‐experiencing cluster was divided into two questions: a trauma‐related nightmare item and a general nightmare item as children may find it difficult to differentiate between the two. Two somatic items (headache and stomach ache), which are common trauma symptoms in children were also included. Participants met the DSM‐IV diagnostic criteria for PTSD if they endorsed at least: (a) one re‐experiencing symptom; (b) three avoidance symptoms; and, (c) two hyperarousal symptoms, corresponding to the DSM‐IV criteria. The two somatic items were not included in the criteria for the diagnosis. Darryl took between 15 and 20 minutes to administer in this sample.
CAPS‐CA
The PTSD symptoms were also assessed using the Danish version of the CAPS‐CA (Landolt et al., 2009; Nader et al., 1996). The CAPS–CA is a child and adolescent version of the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995). Like the CAPS, it is a semi‐structured clinical interview that employs standardized prompt questions and supplementary follow‐up questions. The CAPS‐CA assesses all DSM‐IV criteria for PTSD. Specifically, it assesses exposure to a traumatic event, the individual's experience of the event, the 17 symptoms for PTSD in DSM‐IV, as well as the one‐month duration requirement, and the impact of symptoms on daily functioning. The frequency and intensity of each of the symptoms are rated via behaviourally anchored ratings. Each symptom is rated between zero and four for both the frequency and the intensity and the two values are then summed. In the present study a frequency score of one or greater as well as an intensity score of two or greater was required in order to qualify as a symptom (Weathers et al., 1999). The CAPS‐CA includes opportunities to practice with the format prior to questions, and a standard procedure for identification of time frames to increase the utility of this instrument with children. The CAPS‐CA has been found to have good internal consistency (coefficient α ranging from 0.73 to 0.81 for the symptom clusters and 0.89 for the full scale; Landolt et al., 2009). Using this sample, the CAPS‐CA administration time was between 45 and 60 minutes.
Statistical analyses
Internal consistencies of the Darryl, the CAPS‐CA overall and the three symptom clusters were examined using Cronbach's alpha. The validity of Darryl was examined by comparing the total amount of PTSD symptoms reported on Darryl to the total amount of PTSD symptoms on CAPS‐CA using Pearson's r. Furthermore, the association between the total number of potentially traumatic events and PTSD symptoms on the Darryl was examined using Spearman's rho since the numbers of experienced events were markedly skewed. Receiver operating characteristic (ROC) analysis was used to assess the ability of the Darryl to identify PTSD diagnosis according to the CAPS‐CA. The performance of the Darryl in terms of sensitivity and specificity was assessed using different cutoff scores. Sensitivity indicates the probability that someone with the PTSD diagnosis according to CAPS‐CA will have tested positive using the Darryl. Specificity indicates the probability that someone without a PTSD diagnosis according to CAPS‐CA will have tested negative using the Darryl. Positive and negative predictive power of the Darryl was also calculated. Positive predictive power reflects the proportion of children with positive test results who are correctly diagnosed as having PTSD. Negative predictive power reflects the proportion of children with negative results who are correctly diagnosed as not having PTSD. The overall efficiency of the Darryl was measured in terms of the percentage of cases correctly classified as having or not having a possible PTSD diagnosis.
Results
Descriptive findings
All participants in the study reported exposure to at least one potentially traumatic event with an average of 4.6 different types of incidents (range 1–12; SD = 2.93).Only one child did not report any PTSD symptoms on the CAPS‐CA scale. The average number of PTSD symptoms in this sample was 9.2 and the highest was 17. No statistically significant differences in symptoms on the CAPS‐CA were found in regards to age or sex.
On the Darryl, participants reported between one and 17 symptoms. The average number of symptoms reported was 8.9. The most frequently experienced symptom on the Darryl was avoidance of thoughts and feelings which was reported by 72.3% of the children, as shown in Table 1. Intrusive recollections were reported by 70.7% of participants. At the other end of the spectrum, the most infrequently reported symptom was play re‐enactment of the trauma which was only reported by 12.5% of the children. No statistically significant differences in symptoms on the Darryl were found in regards to age or sex.
Table 1.
Frequency of PTSD items from Darryl and CAPS‐CA from 65 child respondents
| Darryl | CAPS‐CA | |||
|---|---|---|---|---|
| n | % | N | % | |
| B. Re‐experiencing | ||||
| B1 Intrusive recollections | 46 | 70.7 | 29a | 44.6 |
| B1c Play re‐enactment of the trauma | 8 | 12.5 | 8a | 12.3 |
| B2 Nightmares about the trauma | 30 | 46.2 | 16 | 24.6 |
| B2c Nightmares in general | 24 | 36.9 | — | — |
| B3 Acting/feeling as if the event is recurring (including dissociative flashbacks) | — | — | 13 | 20 |
| B4 Psychological distress at reminders | 32 | 49.2 | 25 | 38.5 |
| B5 Physiological distress at reminders | 26 | 40 | 10 | 15.4 |
| C. Avoidance | ||||
| C1 Avoidance of thoughts and feelings | 47 | 72.3 | 24 | 36.9 |
| C2 Avoidance of people and activities | 31 | 47.7 | 14 | 21.5 |
| C3 Inability to recall an important aspect of the event | 41 | 64 | 19 | 29.2 |
| C4 Loss of interest in usual activities | 25 | 39 | 17 | 26.2 |
| C5 Detachment/social withdrawal | 22 | 34.4 | 14 | 21.5 |
| C6 Restricted range of affect | 19 | 29.2 | 10 | 15.4 |
| C7 Sense of foreshortened future | 20 | 31.3 | 5 | 7.7 |
| D. Hyperarousal | ||||
| D1 Difficulty initiating and/or sustaining sleep | 38 | 58.4 | 13 | 20 |
| D2 Irritability | 34 | 52.3 | 20 | 30.8 |
| D3 Decreased concentration | 44 | 67.6 | 26 | 40 |
| D4 Hypervigilance | 37 | 56.9 | 22 | 33.8 |
| D5 Exaggerated startle response | 28 | 43.1 | 6 | 9.2 |
| Somatic pain | ||||
| Stomach ache | 25 | 38.5 | — | — |
| Headache | 24 | 36.9 | — | — |
Note: B1c and B2c: “c” = a criterion adapted to fit a PTSD symptom of a child according to the DSM‐IV.
In CAPS‐CA, the item for the B1 criterion comprises one question about intrusive recollections and one question about play re‐enactment of the trauma and counts as one symptom. In the Darryl, intrusive recollections and play re‐enactment are two different items (B1 and B1c, respectively). In this table, the CAPS‐CA reports on the item of intrusive recollections and/or play re‐enactment has been split in two rows for comparison with the two items in the Darryl.
To calculate the cases of PTSD identified using the Darryl, the diagnostic algorithm for PTSD from DSM‐IV requiring one symptom from the re‐experiencing cluster, three symptoms from the avoidance cluster and two symptoms from the hyperarousal cluster was applied. In order to meet the symptom criteria the responses either “some of the time” or “a lot of the time” had to be endorsed. To calculate the cases of PTSD identified by the CAPS‐CA the diagnostic algorithm for PTSD from DSM‐IV was applied to the symptoms endorsed in the CAPS‐CA. Reports of a symptom frequency score of one or greater as well as reports of an intensity score of two or greater met the symptom criteria. On this basis, 19% of the sample (n = 12) screened positive for PTSD using the CAPS‐CA, compared to 57% (n = 37) of the sample who screened positive for DSM‐IV‐PTSD according to the Darryl. All the PTSD cases identified by the CAPS‐CA also screened positive for PTSD according to the Darryl.
Reliability
The overall internal consistency of the Darryl was 0.88 and that of the CAPS‐CA was 0.93. The three Darryl subscales, re‐experiencing, avoidance, and hyperarousal also had good reliability but were slightly lower than the corresponding results for the CAPS‐CA subscales, as seen in Table 2.
Table 2.
Reliability and validity of Darryl relative to CAPS‐CA
| a | ||
|---|---|---|
| Reliability | Darryl | 0.88 |
| Re‐experiencing subscale | 0.78 | |
| Avoidance subscale | 0.69 | |
| Hyperarousal subscale | 0.75 | |
| CAPS‐CA | 0.93 | |
| Re‐experiencing subscale | 0.85 | |
| Avoidance subscale | 0.80 | |
| Hyperarousal subscale | 0.87 | |
| r | ||
| Validity | Correlation of Darryl and CAPS‐CA | 0.73* |
| Re‐experiencing subscales | 0.63* | |
| Avoidance subscales | 0.62* | |
| Hyperarousal subscales | 0.69* |
p < 0.001.
Validity
Overall scores on the Darryl and on the CAPS‐CA were substantially and significantly correlated (r = 0.73, p < 0.000). The corresponding subscales of the Darryl and the CAPS‐CA were also significantly correlated with each other (Table 2). Furthermore, there was a significant association between the Darryl scores and the number of potentially traumatic events reported using the event list in CAPS‐CA (rho = 0.48, p < 0.03). No age or gender specific findings were found in this regard.
The utility of the Darryl as a screening tool for detecting cases of PTSD was assessed using the CAPS‐CA diagnoses for comparative purposes. We examined the area under the curve (AUC) using ROC. The AUC is proportional to the overall ability of the scale across its range to correctly identify both cases and non‐cases of PTSD. The AUC for Darryl was 0.84. This indicates that high scores on the Darryl test are a good indicator of a PTSD diagnosis, as shown in Figure 2. The optimal cutoff point when using the Darryl as a continuous measure to predict a PTSD diagnosis was a score of 17 or more. The performance of the Darryl using different cutoff scores was then calculated and this is presented in Table 3. Each cutoff score gives an overall efficiency ranging from 69% to 82%. The best predictive value was achieved when using a cutoff score of 19. This revealed a sensitivity of 70%, a specificity of 84% and an overall efficiency of 82%. When the Darryl is used as a screening tool for detecting children in need of further diagnostic evaluation a cutoff score of 15 or more yields a very high sensitivity of 90%, a specificity of 65% and an overall efficiency of 69%.
Figure 2.
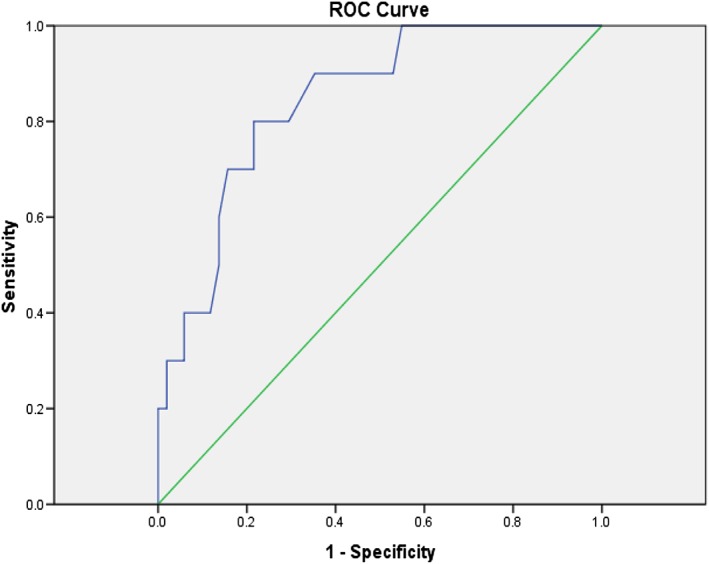
ROC curve for the Darryl and CAPS‐CA.
Table 3.
Sensitivity, specificity, positive and negative predictive power of the Darryl across different cutoff scores using the CAPS‐CA diagnosis as reference
| Cutoff score | Sensitivity | Specificity | Positive predictive power | Negative predictive power | Overall efficiency |
|---|---|---|---|---|---|
| 15 | 0.90 | 0.65 | 0.33 | 0.97 | 0.69 |
| 16 | 0.80 | 0.71 | 0.35 | 0.95 | 0.72 |
| 17 | 0.80 | 0.78 | 0.42 | 0.95 | 0.79 |
| 18 | 0.70 | 0.78 | 0.39 | 0.93 | 0.77 |
| 19 | 0.70 | 0.84 | 0.47 | 0.94 | 0.82 |
| 20 | 0.60 | 0.86 | 0.46 | 0.92 | 0.82 |
| 21 | 0.50 | 0.86 | 0.42 | 0.90 | 0.80 |
Discussion
The aim of this study was to assess the psychometric properties of the Darryl using a Danish sample of children exposed to family violence. The American version of the Darryl measures PTSD symptoms following exposure to community violence, whereas the Danish version was adapted to assess PTSD symptoms of children exposed to family violence.
Consistent with previous studies of American children (Geller et al., 2007; Neugebauer et al., 1999), the Darryl exhibited good internal consistency for the full scale and adequate reliability for the symptom subscales in this sample of Danish children and adolescents. Furthermore, this study found support for the construct and criterion validity of Darryl. The study adds to the existing validation studies of the Darryl. The current study found that the scores correlated significantly with a widely used instrument for assessing PTSD symptoms in children, the CAPS‐CA, and with the number of potentially traumatic events reported. Moreover, the study reported Darryl's sensitivity and specificity relative to the CAPS‐CA.
Initial support for the utility of the Darryl as a screening instrument in this high risk sample of children has also been presented using the CAPS‐CA for comparison. ROC analysis showed that overall the Darryl was a good predictor of a PTSD diagnosis. The statistical analysis suggested that when using the Darryl as a continuous measure, a cutoff score of 19 or more was a valid method to detect probable PTSD cases. When using Darryl as a screening measure, a cutoff score of 15 or more ensures a very high sensitivity (90%). Based on the current analyses, it is recommended that a cutoff of 15 is used to screen for further assessment (e.g. CAPS‐CA), and a cutoff of 19 in the absence of a diagnostic instrument.
Impairment of intellectual abilities and concentration skills are common symptoms in traumatized children. The CAPS‐CA is a well‐established and thorough assessment tool however, it is very time consuming and demanding for young children with average or below average language skills or intellectual ability. The administration time of the CAPS‐CA took between 45 and 60 minutes whereas the administration of the Darryl only took between 15 and 20 minutes. During the administration of the CAPS‐CA many of the children reported and displayed signs of concentration difficulties, for example, difficulty following the questions, restlessness, distraction, or suddenly talking about something else. Notably, no differences were observed between the two samples in relation to concentration difficulties. Furthermore, the intensity rating format used in the CAPS‐CA was very difficult for the children to comprehend and use, resulting in many children rating the intensity at the extreme ends of the spectrum. This may have contributed to the relatively lower number of PTSD cases according to the CAPS‐CA, as an intensity rating of at least two was required for the item to count as a PTSD symptom.
Furthermore, the CAPS‐CA questions appeared more abstract, making it more difficult for the younger children to comprehend. For example, the questions relating to avoidance behaviour require that a child must firstly understand that they are exhibiting avoidance behaviour, secondly remember how often they engage in this behaviour in the past month and in his/her lifetime, and finally rate both the frequency and intensity of the behaviour on two separate five level scales. Adding up each PTSD symptom plus an additional 16 items rated on two dimensions results in some 500 questions. This is a demanding task for most people and young children who have been exposed to trauma making this especially difficult. On the contrary, the Darryl was found to be easy and quick to administer and was very well tolerated by the children in this study. Another advantage of the Darryl is the playful tone of the wording and the cartoon format which is developmentally appropriate for children. Qualitative interviewing of the children in this sample suggested that the children in the lowest age group especially preferred the Darryl when compared to the CAPS‐CA because it was easier for them to understand the wording and the response coding. The Darryl appears very effective in screening for PTSD symptoms in trauma populations with a known trauma (or suspicion of a particular trauma) as the pictures depict a specific trauma such as interpersonal violence or witnessing a fire. However, when screening more widely for a range of possible traumas the Darryl might not be the optimal assessment tool.
We have developed six versions of the Darryl, respectively for violence in the family, death, war, childhood sexual abuse, illness, and fire. In most cases, the clinician has prior knowledge about the trauma experiences before the initial assessment. In this case the appropriate version could be selected. If the clinician has no knowledge of any trauma beforehand or learns about the trauma unexpectedly he/she would do a normal interview with the parents and the child. The clinician could then come back after learning about the trauma and do a thorough PTSD assessment specific to the type of trauma experienced. Inevitably, there will be a number of trauma types that are not covered by the Darryl. However, the successful use of the Darryl in previous studies highlights the applicability of the measure in a wide range of traumatized samples. Additionally, the CAPS‐CA can be exhausting and even contraindicative for children aged 8–10 to complete. It is proposed that measures such as the Darryl are more developmentally appropriate and less intrusive to the child. Additionally, the use of illustrations can help the child to identify with the emotions and symptoms that are being portrayed. It could be argued that the use of pictures is less threatening when compared to a format which relies solely on questions.
The findings of the present study must be interpreted in the context of some limitations. The sample was relatively small with a wide age range and children aged seven to nine were underrepresented. Future research should address these limitations by using larger samples of children and adolescents. Additionally, there was no access to specific information relating to the frequency or the recency of the potential violent episodes. It is possible that these may have been confounding factors. Placement in a crisis shelter may constitute a safe haven and promote avoidant coping mechanisms during this time. Moreover, due to practical considerations at the crisis centre and the all‐day school the psychologists who administered the measures were not blind to the CAPS‐CA results during admission of the Darryl. Additionally, whereas the applied version of the Darryl assessed PTSD symptoms related to family violence, the CAPS‐CA assessed PTSD symptoms based on a screening list for exposure to 17 potentially traumatic events where several of the events included some form of exposure to violence. The CAPS‐CA was applied as diagnostic instrument of PTSD, whereas the Darryl screened for the presence of PTSD symptoms after exposure to family violence. When investigating the validity of the family violence version of the Darryl, the CAPS‐CA should assess the reactions on the events only related to family violence. This was not explicitly done in the study because the recruitment of the children was done based on the inclusion criterion of the children's high exposure to family violence. Furthermore, this sample consisted of children who had a potentially traumatic home environment and the results may not be transferrable to the general population. Finally, the type of trauma reported in this sample was interpersonal violence which precludes generalizing the findings to a wider childhood trauma population.
Conclusion
The Darryl has been found to be a promising tool for assessing PTSD symptoms in a sample of Danish children and adolescents who experienced interpersonal violence. This study contributes to the literature in several ways. Firstly, the Darryl has shown its ability as a screening measure. It can also identify children with a probable PTSD diagnosis when used as a continuous measure. Secondly, it has been recommended that child and adolescent screening measures are brief, easy to administer, understand and complete (Prins et al., 2004) therefore the brevity of the Darryl adds to its utility for assessing childhood and adolescent PTSD. Thirdly, this method of assessment is considered to have an advantage over other measures of childhood PTSD as it is more developmentally appropriate and less intrusive.
Declaration of interest statement
The authors have no competing interests.
Acknowledgements
Thanks to Dr Richard Neugebauer for giving the authors permission to use the Darryl and elaborate new version. This research was supported by a grant from the Egmont Foundation (831‐2174).
Schandorph Løkkegaard, S. , Rønholt, S. , Karsberg, S. , and Elklit, A. (2017) Validation of the PTSD screening cartoon test “Darryl” in a Danish clinical sample of children and adolescents. Int J Methods Psychiatr Res, 26: e1514. doi: 10.1002/mpr.1514.
References
- Alisic E., Zalta A.K., Van Wesel F., Larsen S.E., Hafstad G.S., Hassanpour K., Smid G.E. (2014) Rates of post‐traumatic stress disorder in trauma‐exposed children and adolescents: meta‐analysis. The British Journal of Psychiatry, 204(5), 335–340. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision). Washington, DC: American Psychiatric Association. [Google Scholar]
- Anthony J.L., Lonigan C.J., Hecht S.A. (1999) Dimensionality of posttraumatic stress disorder symptoms in children exposed to disaster: results from confirmatory factor analyses. Journal of Abnormal Psychology, 108(2), 326–336. [DOI] [PubMed] [Google Scholar]
- Blake D.D., Weathers F.W., Nagy L.M., Kaloupek D.G., Gusman F.D., Charney D.S., Keane T.M. (1995) The development of a clinician‐administered PTSD scale. Journal of Traumatic Stress, 8(1), 75–90. [DOI] [PubMed] [Google Scholar]
- Charuvastra A., Goldfarb E., Petkova E., Cloitre M. (2010) Implementation of a screen and treat program for child posttraumatic stress disorder in a school setting after a school suicide. Journal of Traumatic Stress, 23(4), 500–503. DOI: 10.1002/jts.20546. [DOI] [PubMed] [Google Scholar]
- Christoffersen M.N. (2010) Børnemishandling i hjemmet, København: SFI. [Google Scholar]
- Cohen J.A., Bukstein O., Walter H., Benson S.R., Chrisman A., Farchione T.R., Issues A.W.G.O.Q. (2010) Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 49(4), 414–430. [PubMed] [Google Scholar]
- De Bellis M.D., Keshavan M.S., Clark D.B., Casey B.J., Giedd J.N., Boring A.M., Ryan N.D. (1999) Developmental traumatology part II: brain development. Biological Psychiatry, 45(10), 1271–1284. [DOI] [PubMed] [Google Scholar]
- DePrince A.P., Weinzierl K.M., Combs M.D. (2009) Executive function performance and trauma exposure in a community sample of children. Child Abuse and Neglect, 33(6), 353–361. DOI: 10.1016/j.chiabu.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Elklit A., Nielsen L.H., Lasgaard M., Duch C. (2013) A cartoon‐based measure of PTSD symptomatology in children exposed to a disaster. Journal of Loss and Trauma, 18(1), 54–63. DOI: 10.1080/15325024.2012.679125. [DOI] [Google Scholar]
- Fairbank J.A., Fairbank D.W. (2009) Epidemiology of child traumatic stress. Current Psychiatry Reports, 11(4), 289–295. [DOI] [PubMed] [Google Scholar]
- Geller P.A., Neugebauer R., Possemato A.K., Walter P., Dummit E.S.E., Silva R.R. (2007) Psychometric properties of darryl, a cartoon based measure to assess community violence‐related PTSD in children. Psychiatric Quarterly, 78(2), 157–168. DOI: 10.1007/s11126-006-9035-6. [DOI] [PubMed] [Google Scholar]
- Landolt M.A., Buehlmann C., Maag T., Schiestl C. (2009) Brief report: quality of life is impaired in pediatric burn survivors with posttraumatic stress disorder. Journal of Pediatric Psychology, 34(1), 14–21. DOI: 10.1093/jpepsy/jsm088. [DOI] [PubMed] [Google Scholar]
- Laursen H., Elklit A. (2009) Traumer hos børn på en heldagsskole. Pædagogisk Psykologisk Tidsskrift, 46(1–2), 9–24. [Google Scholar]
- Margolin G., Vickerman K.A. (2007) Posttraumatic stress in children and adolescents exposed to family violence: I. Overview and issues. Professional Psychology:Research and Practice, 38(6), 613–619. DOI: 10.1037/0735-7028.38.6.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally R.J. (1996) Assessment of posttraumatic stress disorder in children and adolescents. Journal of School Psychology, 34(2), 147–161. DOI: 10.1016/0022-4405(96)00004-0. [DOI] [Google Scholar]
- Meiser‐Stedman R., Smith P., Glucksman E., Yule W., Dalgleish T. (2008) The PTSD diagnosis in preschool‐ and elementary school‐age children exposed to motor vehicle accidents. American Journal of Psychiatry, 165(10), 1326–1337. DOI: 10.1176/appi.ajp.2008.07081282. [DOI] [PubMed] [Google Scholar]
- Nader K.O., Kriegler J.A., Blake D.D., Pynoos R.S., Newman E., Weather F.W. (1996) Clinician Administered PTSD Scale, Child and Adolescent Version, White River Junction: National Center for PTSD. [Google Scholar]
- Neugebauer R., Wasserman G.A., Fisher P.W., Kline J., Geller P.A., Miller L.S. (1999) Darryl, a cartoon‐based measure of cardinal posttraumatic stress symptoms in school‐age children. American Journal of Public Health, 89(5), 758–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Cameron R.P., Hugelshofer D.S., Shaw‐Hegwer J., Sheikh J.I. (2004) The primary care PTSD screen (PC‐PTSD): development and operating characteristics. Primary Care Psychiatry, 9(4), 9–14. [Google Scholar]
- Puig‐Antich J., Chambers W. (1987) The Schedule for Affective Disorder and Schizophrenia for School Age Children (kiddy‐SADS), New York: New York State Psychiatric Institute. [Google Scholar]
- Reich W., Leacock N., Shanfield C. (1994) Diagnostic Interview for Children and Adolescents‐revised (DICA‐R), St Louis, MO: Washington University. [Google Scholar]
- Rennick J., Rashotte J., Stevens B., Stremler R., Chambers C., Stack D., Wood‐Dauphinee S. (2014) The Young Children's Critical Illness Impact Scale (Y‐CCIIS): Psychometric Testing of an Illustrated Measure of Post‐PICU Psychological Distress, Paper presented at the The 7th World Congress on Pediatric Critical Care, Istanbul, Turkey.
- Rønholt S., Karsberg S., Elklit A. (2013) Preliminary evidence for a classroom based psychosocial intervention for disaster exposed children with posttraumatic stress symptomatology. Child & Youth Care Forum, 42(6), 617–631. DOI: 10.1007/s10566-013-9220-3. [DOI] [Google Scholar]
- Scheeringa M.S., Wright M.J., Hunt J.P., Zeanah C.H. (2006) Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. American Journal of Psychiatry, 163(4), 644–651. DOI: 10.1176/ajp.2006.163.4.644. [DOI] [PubMed] [Google Scholar]
- Scheeringa M.S., Myers L., Putnam F.W., Zeanah C.H. (2012) Diagnosing PTSD in early childhood: an empirical assessment of four approaches. Journal of Traumatic Stress, 25(4), 359–367. DOI: 10.1002/jts.21723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman W.K., Albano A.M. (1996) The Anxiety Disorder Interview Schedule for DSM‐IV: Child Interview Schedule, San Antonio, TX: Graywind. [Google Scholar]
- Terr L. (1990) Too Scared to Cry: Psychic Trauma in Childhood, New York: Basic Books. [Google Scholar]
- Valla J.P., Bergeron L., Smolla N. (2000) The Dominic‐R: a pictorial interview for 6‐ to 11‐year‐old children. Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 85–93. DOI: 10.1097/00004583-200001000-00020. [DOI] [PubMed] [Google Scholar]
- Weathers F.W., Ruscio A.M., Keane T.M. (1999) Psychometric properties of nine scoring rules for the clinician‐administered posttraumatic stress disorder scale. Psychological Assessment, 11(2), 124–133. DOI: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]
- Yasik A.E., Saigh P.A., Oberfield R.A., Green B., Halamandaris H., McHugh M. (2001) The validity of the children's PTSD inventory. Journal of Traumatic Stress, 14(1), 81–94. [DOI] [PubMed] [Google Scholar]


