Abstract
The Cannabis Abuse Screening Test (CAST) aims at screening the problematic use of cannabis. It has never been validated against the Diagnostic and Statistical Manual of Mental Disorders (DSM)‐5 and its relationships with this latter have never been studied. We used a probabilistic telephone survey collected in 2014 (1351 past‐year cannabis users aged 15–64) implementing the CAST and a DSM‐5 adaptation of the Munich Composite International Diagnostic Interview assessing cannabis use disorders. Data were weighted, and CAST items were considered categorical. Factorial structures were assessed with confirmatory factor analyses; the relationships between the instruments were studied with multiple factor analysis (MFA). One factor for the DSM‐5 and two correlated factors for the CAST were the best confirmatory factor analyses solutions. The CAST thresholds for screening moderate/severe and severe cannabis use disorders were 5 (sensitivity = 78.2% and specificity = 79.6%) and 8 (sensitivity = 86.0% and specificity = 86.7%), respectively. The MFA identified two orthogonal dimensions: The first was equally shared by both instruments; the second was the second CAST dimension (extreme frequencies of use before midday and alone, memory problems, and reproaches from friends/family). The CAST structure and screening properties were confirmed. The MFA explains its screening performances by its first dimension and identified the problematic patterns (the second dimension) that are not captured by the DSM‐5.
Keywords: cannabis problematic use, CAST, CFA, DSM‐5, multiple factor analysis, validation
1. INTRODUCTION
Cannabis use is widespread and mostly used for recreational purpose. But as recreational use itself may be linked to health and psychosocial hazards (Hall, 2014), there is a public health interest in quantifying the magnitude of the “problematic cannabis use” in the general population and not only the cannabis use disorders (CUD) defined by the International Classification of Disease or by the Diagnostic and Statistical Manual of Mental Disorders (DSM). There is no clear definition of a “problematic” cannabis use but the European Monitoring Centre for Drugs and Drug Addictions (EMCDDA) set up a working group on this topic (EMCDDA, 2007) and decided to refer to consumption patterns “ … leading to negative consequences on a social or health level, both for the individual user and for the larger community” (Beck & Legleye, 2008, p. 31). Short screening tests have thus been developed to monitor problematic cannabis use in general population surveys (Annaheim & Stéphane, 2017).
Validation of these tests in general population surveys rely on three methodologies. The classic and most common method is to validate the instrument against gold standards derived from the DSM (Bashford, Ross, & Copeland, 2010; Bastiani et al., 2013; Cuenca‐Royo et al., 2012; Fernandez‐Artamendi, Fernández‐Hermida, Muñiz‐Fernández, Secades‐Villa, & García‐Fernández, 2012; Gyepesi et al., 2014; Legleye, Piontek, & Kraus, 2011; Martin, Copeland, Gates, & Gilmour, 2006; Piontek, Kraus, & Klempova, 2008; Steiner, Baumeister, & Kraus, 2008). The second method is to explore the internal structure of the instruments, for instance using item response theory (Annaheim, Scotto, & Gmel, 2010; Langenbucher et al., 2004), exploratory factor analysis (EFA) and confirmatory factor analysis (CFA), or latent class analysis (Baillie & Teesson, 2010; Muthen, 2006; Teesson, Lynskey, Manor, & Baillie, 2002). Sometimes, latent class analysis is used to produce a new data‐driven reference for the gold standard itself (Garrett, Eaton, & Zeger, 2002; Hawkins, Garrett, & Stephenson, 2001) to be used instead. This third method is helpful when the original gold standard is challenged, as has been the case for the DSM‐IV TR (Gillespie, Neale, Prescott, Aggen, & Kendler, 2007; Legleye et al., 2015; Legleye, Piontek, Kraus, Morand, & Falissard, 2013). However, because the release of the DSM‐5 changed the conception of the CUD, some previous results obtained with the older versions of the DSM may have to be updated.
In addition, these classical methodologies do not show the concordance between the gold standard and the candidate instrument, what they have in common and to which extent they differ, a knowledge that we believe necessary to provide a correct understanding of the screening properties. False positive and false negative rates and the description of diagnostic orphans (Degenhardt, Coffey, Carlin, Swift, & Patton, 2008) only indirectly inform on the communalities of the instruments, whereas EFA/CFA are assessed separately and cannot be compared directly, because the items differ in nature. The extension of CFA to multigroup data can be used to test the invariance of a single test in various populations, but in validation studies, we encounter the opposite problem, that of comparing different sets of questions answered by the same individuals. Fortunately, multiple factor analysis (MFA; Abdi, Williams, & Valentin, 2013; Escofier & Pagès, 1990) is one method that enables analyses of this type. It exhibits the intrisic relationships between the instruments by showing how their proper dimensions are related.
Finally, although the data used for the previous validations were issued from surveys, survey weights were never considered, although not using them may bias the results and lead to erroneous statistical inferences regarding cut‐offs or and even latent variable modelling (Asparouhov, 2005).
The aim of this article is to study further the properties of the Cannabis Abuse Screening Test (CAST), one of the most used test screening for problematic cannabis use in the general population (Annaheim & Legleye, 2017). First, as in previous validations, but using now the DSM‐5, to show the internal structures of the CAST and the DSM‐5 using CFA and to determine CAST optimal thresholds for the screening of moderate/severe and severe CUD; second, to study in detail the concordance of the two instruments using a MFA, all analyses using survey weights.
2. METHODS
2.1. Sample
The sample was derived from the 2014 Health Barometer, a nationwide random telephone survey targeting non‐institutionalized French‐speaking individuals aged 15 to 75. Multiple probability inclusions resulting from the number of active (mobile or landline) phone numbers available to reach the respondents were taken into account. The main sample comprised 15,635 individuals. The response rate according to the formula RR2 of the American Association for Public Opinion Research was 57%. Data were calibrated using gender × age, diploma, and region of residence to ensure the representativeness of the sample (Richard, Gautier, Guignard, Léon, & Beck, 2014). During the interview, a random subsample of 5,294 individuals aged 15–64 answered a specific questionnaire related to drug use: among them, 1,351 were past‐year cannabis users, and their responses are those analysed in this paper.
2.2. Measures
The DSM‐5 criteria for CUD over the past 12 months were assessed to all past‐year cannabis users using the telephone version of the Munich Composite International Diagnostic Interview (Lachner et al., 1998; Wittchen et al., 1995), in which the item “legal problems” from the original version, based on the DSM‐IV TR, was replaced by two questions to produce the craving criteria in the DSM‐5 (at least one “yes” defined a positive criterion): “Wanted to smoke cannabis so badly you couldn't think of anything else?” and “Such an urge to smoke cannabis that you couldn't resist it.” Based on the classical thresholds of the DSM‐5 score (APA, 2013, 5), we retained the following thresholds for the categories of CUD symptoms in the last 12 months: 2+ (any CUD), 4+ (moderate/severe CUD), and 6+ (severe CUD).
The CAST (Legleye et al., 2011) was designed to screen for a broader spectrum of cannabis use patterns than CUD, following the EMCDDA definition of problematic use (Beck & Legleye, 2008, p. 31). It was administered to all past‐year cannabis users. The six questions are smoking before midday (C1 “Have you smoked cannabis before midday?”), smoking alone (C2 “Have you smoked cannabis when you were alone?”), memory problems (C3 “Have you had memory problems when you smoked cannabis?”), reproaches from friends/family (C4 “Have friends or family members told you that you should reduce or stop your cannabis consumption?”), unsuccessful attempts to quit (C5 “Have you tried to reduce or stop your cannabis use without succeeding?”), and problems (C6 “Have you had problems because of your cannabis use [argument, fight, accident, poor results at school, etc.]?”). All items are answered on a 5‐point scale (0 “never,” 1 “rarely,” 2 “from time to time,” 3 “fairly often,” and 4 “very often”). In population surveys, cut‐offs of the score that sums all items are used to screen for problematic use and CUD (Annaheim & Stéphane, 2017).
In the present study, there was no item nonresponse.
2.3. Statistical analyses
The structure of the CAST and the DSM‐5 was investigated using EFA and CFA. CFA model fit was examined using the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). A cut‐off of 0.95 on the CFI with a RMSEA below 0.06 was considered adequate (Hu & Bentler, 1999).
We also computed the Cronbach alpha and correlations of CAST items with the CAST score. The association between the CAST and the DSM‐5 was investigated using Pearson's correlation coefficient between scores. With regard to criterion validity, areas under receiver operating characteristic curves (area under curve [AUC]; Rey, Morris‐Yates, & Stanislaw, 1992) were computed, as well as sensitivity, specificity, and the Youden index (Y = sensitivity + specificity − 1), for each CAST score against the DSM‐5 moderate/severe and severe CUD symptoms (see Section 2.2) in order to determine the best cut‐offs.
Finally, we investigated the common underlying structure of the CAST and the DSM‐5 using a MFA (Abdi et al., 2013; Escofier & Pagès, 1990; Husson, Lê, & Pagès, 2009). MFA deals with data in which individuals are described by several groups of variables (here, the CAST items and the DSM‐5 items). Its goal is to exhibit the relations between the intrisic dimensions (i.e., components) of the groups. In our case, all items were considered categorical, and a multiple correspondence analysis (MCA) was first performed on each group to find its partial axes (i.e., components or intrisic dimensions). The first eigenvalue is used to norm each group and balance their influence, and the MFA is a MCA of this normalized common database: The individuals, variables, and partial axes can be analysed classically in the space defined by the orthogonal common dimensions. Additionally, each category of a categorical variable (e.g., a CAST item) can be represented by a “common point” (centre of gravity of all individuals with this characteristic) and by one partial point for each group of variables (the centre of gravity of the partial points representing the category according to the group, depicted in Figure 4 by the letters C and D for CAST and DSM‐5, respectively). When a category is represented in the same way by each instrument, partial points are close to the common point: The distance between the partial points reflects the divergence of the descriptions of the individuals by the two instruments.
Figure 4.
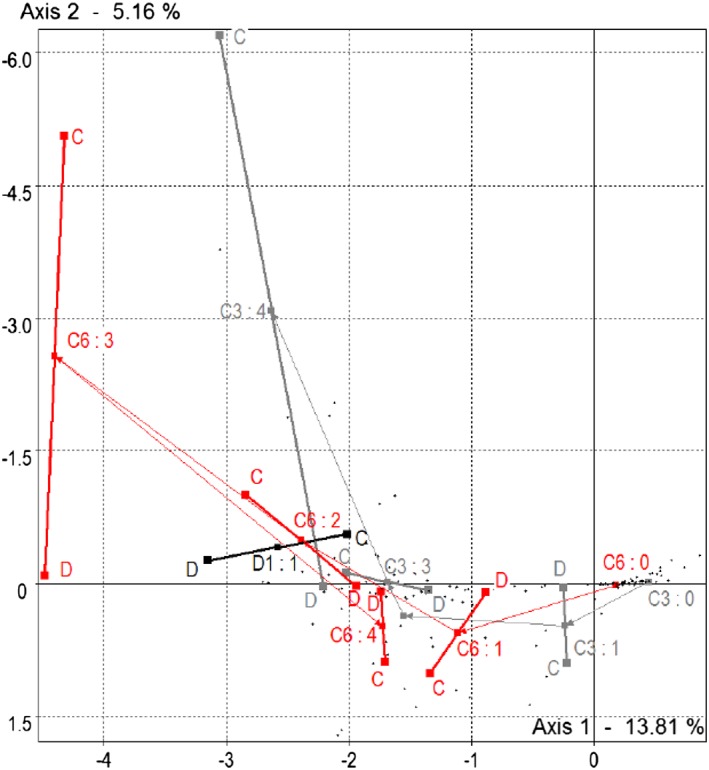
Multiple factor analysis: Partial representations (C=CAST, D=DSM‐5) of some categorical Cannabis Abuse Screening Test and Diagnostic and Statistical Manual of Mental Disorders‐5 variables in the multiple factor analysis
The global link between the CAST and the DSM‐5 is provided by the RV coefficient (Robert & Escoufier, 1976), ranging from 0 to 1 while the Lg coefficient for each group reflects its dimensionality (Abdi et al., 2013).
2.4. Methodological considerations
It is noteworthy to remind that factors obtained with CFA and dimensions obtained with MCA/MFA cannot be directly compared (Brown, 2015): The CFA seeks a reduction in dimensionality and a simplification in structure by allocating items to one factor only, while the factors remain correlated. It is based on statistical tests of a theory‐based model. The MCA/MFA provides orthogonal dimensions based on a geometrical representation of the data like in principal components analysis. All items load on all dimensions: The reduction in dimensionality is based on the explained variance.
Because CAST items are based on a 5‐point Likert scale only, we considered them as categorical variables in all analyses. In EFA/CFA, we used non‐linear factor analyses with robust estimations of weighted least‐squares means and variance for the CAST and the DSM‐5. All analyses used the survey weights.
Statistics were computed on SAS V9.4 and MPlus V7 (EFA and CFA) and SPAD8 (MCA and MFA).
3. RESULTS
The analytic sample comprised 1,351 individuals aged 15–64 (892 men [66.0%] and 459 women) who had smoked cannabis in the 12 months before the survey. Table 1 shows the distributions of the DSM‐5 and CAST items. Regarding the DSM‐5, craving (D3) is the most rarely reported behaviour (2.5%), whereas impaired control is the most prevalent (32.3%). Regarding the CAST, items related to smoking before midday (C1) and smoking alone (C2) are often reported (35.8% and 49.4%), whereas unsuccessful attempt to quit (C5) and cannabis‐related problems (C6) are rare in comparison (16.6% and 8.1%, respectively). Based on the DSM‐5, 59.9% of the sample did not satisfy the criteria for CUD, although the prevalences of any CUD, moderate/severe, and severe CUD symptoms were 34.1%, 16.0%, and 5.5%, respectively.
Table 1.
DSM‐5 criteria and CAST items (%, mean number of criteria with standard deviation; mean [SD])
| Instrument | Item | Scale | N | Prevalence (%, [SD]) | Mean (SD) |
|---|---|---|---|---|---|
| DSM‐5 | |||||
| Role impairment | D1 | 0–1 | 29 | 2.8 (0.57) | |
| Hazardous use | D2 | 0–1 | 159 | 14.2 (1.08) | |
| Craving | D3 | 0–1 | 24 | 2.5 (0.58) | |
| Social problems | D4 | 0–1 | 169 | 15.1 (1.28) | |
| Tolerance | D5 | 0–1 | 173 | 14.4 (1.18) | |
| Withdrawal | D6 | 0–1 | 112 | 9.6 (1.02) | |
| More than intended | D7 | 0–1 | 236 | 18.6 (1.29) | |
| Impaired control | D8 | 0–1 | 376 | 32.3 (1.58) | |
| Much time spent | D9 | 0–1 | 192 | 16.8 (1.30) | |
| Reduced activities | D10 | 0–1 | 71 | 6.5 (0.92) | |
| Use despite problems | D11 | 0–1 | 218 | 18.4 (1.32) | |
| Scorea | 0–11 | 1.49a (0.07) | |||
| CUDd (score ≥ 2) | 0–1 | 402 | 34.1 (1.56) | ||
| Moderate/severe CUD (score ≥ 4) | 0–1 | 181 | 16.0 (1.29) | ||
| Severe CUD (score ≥ 6) | 0–1 | 58 | 5.5 (0.81) | ||
| CAST | |||||
| Smoked before midday | C1 | 0–4 | 407 | 35.8b (1.62) | 0.68c (0.04) |
| Smoked alone | C2 | 0–4 | 615 | 49.4b (1.62) | 1.16c (0.05) |
| Memory problems | C3 | 0–4 | 317 | 26.5b (1.51) | 0.55c (0.04) |
| Reproaches from friends/family | C4 | 0–4 | 287 | 25.1b (1.50) | 0.55c (0.04) |
| Unsuccessful attempt to quit | C5 | 0–4 | 188 | 16.6b (1.30) | 0.39c (0.04) |
| Cannabis‐related problems | C6 | 0–4 | 95 | 8.0b (0.91) | 0.15c (0.02) |
| Scorec | 0–24 | 3.48c (0.15) | |||
| Score ≥ 5 | 0–1 | 357 | 32.1 (1.62) | ||
| Score ≥ 7 | 0–1 | 227 | 21.2 (1.46) | ||
| Score ≥ 8 | 0–1 | 186 | 17.3 (1.35) |
Note. N are unweighted, but means, standard deviations, and percentages are weighted. DSM = Diagnostic and Statistical Manual of Mental Disorders; CUD = cannabis use disorders; CAST = Cannabis Abuse Screening Test.
The score is computed on the binary variables scaled to 0–1.
Item is dichotomized (at least oncevs never).
The mean is computed on the Likert scale 0–4.
Cannabis use disorder.
3.1. Structures
We explored the structures of the instruments using EFA and CFA. We tested up to three factors, but as the three‐factor solutions always produced poor fit indexes, they are not reported. For the CAST (Table 2), a CFA with two correlated factors (r = .77, SD = 0.04) provides the best solution (RMSEA = 0.000, 90% CI [0.000, 0.027], p < .05 = 1.000, CFI = 1.000). Factor 1 groups C1 and C2 (uses in the morning or alone) whereas Factor 2 groups C3 to C6. The interpretation is simple: Factor 1 groups patterns of use that do not evoke fun and friends but are not directly linked to problems, that is, non‐standard use, in opposition to Factor 2 that regroups personal or social problems.
Table 2.
Exploratory and confirmatory factor analysis of the categorical CAST and the DSM‐5 criteria
| EFA | CFA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F1 | F2 | ||||||
| Loadinga | SE | Loadinga | SE | Loadinga | SE | Loadinga | SE | ||
| CAST | |||||||||
| 1 | Cannabis before midday | 0.802 | 0.438 | 0.224 | 0.210 | 0.800 | 0.027 | ||
| 2 | Cannabis when alone | 0.785 | 0.450 | 0.298 | 0.349 | 0.870 | 0.028 | ||
| 3 | Memory problems | 0.378 | 0.087 | 0.574 | 0.085 | 0.693 | 0.037 | ||
| 4 | Friends or family | 0.418 | 0.087 | 0.643 | 0.085 | 0.774 | 0.040 | ||
| 5 | Tried to reduce or stop | 0.298 | 0.077 | 0.492 | 0.088 | 0.572 | 0.049 | ||
| 6 | Problems | 0.302 | 0.084 | 0.568 | 0.087 | 0.626 | 0.048 | ||
| DSM‐5 | |||||||||
| 1 | Role impairment | 0.583 | 0.129 | 0.277 | 0.127 | 0.641 | 0.081 | ||
| 2 | Hazardous use | 0.439 | 0.087 | 0.346 | 0.092 | 0.562 | 0.053 | ||
| 3 | Craving | 0.130 | 0.120 | 0.650 | 0.155 | 0.597 | 0.078 | ||
| 4 | Social problems | 0.584 | 0.076 | 0.507 | 0.091 | 0.773 | 0.040 | ||
| 5 | Tolerance | 0.742 | 0.056 | 0.201 | 0.092 | 0.722 | 0.042 | ||
| 6 | Withdrawal | 0.625 | 0.090 | 0.478 | 0.106 | 0.789 | 0.042 | ||
| 7 | More than intended | 0.588 | 0.070 | 0.350 | 0.096 | 0.687 | 0.040 | ||
| 8 | Impaired control | 0.287 | 0.092 | 0.770 | 0.115 | 0.865 | 0.125 | ||
| 9 | Much time spent | 0.627 | 0.072 | 0.448 | 0.092 | 0.776 | 0.036 | ||
| 10 | Reduced activities | 0.688 | 0.103 | 0.214 | 0.109 | 0.692 | 0.065 | ||
| 11 | Use despite problems | 0.734 | 0.052 | 0.214 | 0.092 | 0.723 | 0.037 | ||
Note. In bold type the items chosen for each factor. Data are weighted. CAST fit indexes are 1 factor, EFA or CFA: root mean square error of approximation (RMSEA) = 0.055, 90%, confidence interval, CI [0.040, 0.072], p < .05 = .260; comparative fit index (CFI) = 0.976; 2 factors, EFA: RMSEA = 0.021, 90% CI [0.000, 0.050], p < .05 = 1.000; CFI = 0.950; and 2 factors, CFA: RMSEA = 0.000, 90% CI [0.000, 0.027], p < .05 = 1.000; CFI = 1.000. Correlation between CFA factors: r = .77, standard deviation = 0.04. DSM‐5 fit indexes are 1 factor, EFA or CFA: RMSEA = 0.014, 90% CI [0.000, 0.024], p < .05 = 1.000; CFI = 0.993; 2 factors, EFA: RMSEA = 0.000, 90% CI [0.000, 0.017], p < .05 = 1.000; CFI = 1.000; and 2 factors, CFA: RMSEA = 0.010, 90% CI [0.000, 0.022], p < .05 = 1.000; CFI = 0.996. Correlation between CFA factors: r = .91, standard deviation = 0.03. EFA = exploratory factor analysis; CFA = confirmatory factor analysis; CAST = Cannabis Abuse Screening Test; DSM = Diagnostic and Statistical Manual of Mental Disorders; SE = standard error.
Standardized loading with varimax rotation (orthogonal on EFA).
The Cronbach alpha is .71 but only .58 for the second factor, which is rather low and calls for further examination. Belonging to this factor, Items C5 and C6 have the lowest loadings in EFA and CFA (Table 2); they are rarely endorsed, especially C6 (Table 1), and their correlations with the CAST score are low, especially for C5 (r = .30 for C5 and .33 for C6, whereas the other items range from .48 [C3] to .54 [C2]). For C5, this low correlation is due to a ceiling effect at Category 1: The average CAST score are 1.1, 3.3, 3.6, 3.7, and 2.6 from Categories 0 to 4, respectively.
For the DSM‐5 (Table 2), a two‐factor solution provides the best solution, with good fit indexes in CFA (RMSEA = 0.010 90% CI [0.000, 0.022], p < .05 = 1.000, CFI = 1.000). The factors are highly correlated (r = .91, SD = 0.03). The items craving and impaired control load clearly on Factor 2, suggesting a minor dimension. The differences between the loadings on the two EFA factors were not marked for some items (social problems and hazardous use), and the single‐factor solution had also an acceptable fit (RMSEA = 0.014 90% CI [0.000, 0.024], p < .05 = 1.000, CFI = 0.993). The Cronbach alpha is .76.
3.2. Correlation between the CAST and the DSM‐5
The CAST scores range from 0 to 18 (mean = 3.5, SD = 4.3, median = 2); the corresponding values for the DSM‐5 score are 0–10 (mean = 1.5, SD = 2.1, median = 1). The Pearson correlation coefficient between the two is r = .69.
3.3. Optimal thresholds for the CAST
Table 3 shows that the discriminant power of the CAST is high (AUC = 0.91, 95% CI [0.89, 0.93]) for the screening of moderate/severe DSM‐5 CUD symptoms (score ≥ 4). On the basis of the Youden index, the optimal threshold is 5 with a sensitivity of 86.6% and a specificity of 78.2%: 79.6% of the individuals are correctly classified. For severe DSM‐5 CUD symptoms (score ≥ 6), AUC is greater (0.94, 95% CI [0.92, 0.96]) while the optimal threshold is 8 (sensitivity = 86.0%, specificity = 86.7%, 86.7% of the individuals being correctly classified). Despite these results, false positive and negative rates are rather high, and the proportion of individuals screening positive is well above that defined by the DSM‐5 thresholds (Table 1 lower panel) whereas the positive predictive values are low.
Table 3.
Screening properties of the CAST against theoretical DSM‐5 standards
| Se (%) | Sp (%) | PPV (%) | NPV (%) | FPR (%) | FNR (%) | Correct (%) | Y = Se + Sp − 1 (%) | |
|---|---|---|---|---|---|---|---|---|
| DSM‐5 moderate/severe(score ≥ 4) | ||||||||
| 1 | 98.7 | 39.7 | 23.8 | 99.4 | 60.3 | 1.3 | 49.2 | 38.4 |
| 2 | 96.7 | 55.0 | 29.1 | 98.9 | 45.0 | 3.3 | 61.7 | 51.7 |
| 3 | 92.2 | 65.8 | 34.0 | 97.8 | 34.2 | 7.8 | 70.0 | 58.0 |
| 4 | 90.1 | 72.0 | 38.1 | 97.4 | 28.0 | 9.9 | 74.9 | 62.1 |
| 5 | 86.6 | 78.2 | 43.2 | 96.8 | 21.8 | 13.4 | 79.6 | 64.8 |
| 6 | 79.5 | 83.3 | 47.7 | 95.5 | 16.7 | 20.5 | 82.7 | 62.8 |
| DSM‐5 severe(score ≥ 6) | ||||||||
| 1 | 100.0 | 35.5 | 8.3 | 100.0 | 64.5 | 0.0 | 39.0 | 35.5 |
| 2 | 100.0 | 49.4 | 10.3 | 100.0 | 50.6 | 0.0 | 52.2 | 49.4 |
| 3 | 100.0 | 59.8 | 12.6 | 100.0 | 40.2 | 0.0 | 62.0 | 59.8 |
| 4 | 97.7 | 65.6 | 14.1 | 99.8 | 34.4 | 2.3 | 67.3 | 63.3 |
| 5 | 97.7 | 71.7 | 16.7 | 99.8 | 28.3 | 2.3 | 73.1 | 69.4 |
| 6 | 93.4 | 77.1 | 19.2 | 99.5 | 22.9 | 6.6 | 78.0 | 70.5 |
| 7 | 90.1 | 82.8 | 23.4 | 99.3 | 17.2 | 9.9 | 83.2 | 73.0 |
| 8 | 86.0 | 86.7 | 27.3 | 99.1 | 13.3 | 14.0 | 86.7 | 72.8 |
| 9 | 71.1 | 90.4 | 30.2 | 98.2 | 9.6 | 28.9 | 89.4 | 61.5 |
Note. Percentages are weighted. Se = sensitivity; Sp = specificity; PPV = positive predictive value; NPV = negative predictive value; FPR = false positive rate; FNR = false negative rate; Correct = % of correctly classified individuals; CAST = Cannabis Abuse Screening Test; DSM = Diagnostic and Statistical Manual of Mental Disorders.
3.4. MFA: Preliminary separate analyses
The CAST was first studied using MCA. The first three eigenvalues account for respectively 11.1%, 6.9%, and 5.3% of the global inertia (obtained with 24 eigenvalues), and the complete histogram suggests that two or three dimensions are sufficient to describe its structure (although the Lg is 4.03). The contributions of items to the inertia of the first dimension are respectively 20.3% and 21.9% for C1 and C2, 17.1% and 17.6% for C3 and C4, and lower for C5 and C6 (13.3% and 9.6%, respectively). The main contributors to the second dimension are C1 (29.1%, with 14.6% for Category 4 alone), C2 (24.9%, with 15.6% for Categories 3 and 4 together), and C3 (20.0%, with 16.7% for Category 4 alone). The contributions of C4 and C5 are minor (12.8% and 4.8% with no major disparities between categories) as is the contribution of C6 (8.5%, with 7.0% for Category 3 alone). The main contributors to Axis 3 are C4 (30.6%, with 8.9% for Category 4) and C5 (29.0%, with 13.7% for Category 4) whereas C6 contributes only for 11.5% (9.6% for Category 4 alone).
The two first factorial diagrams are shown in Figure 1. In the first diagram, Items C1 to C4 present a classic J‐shaped pattern from left to right along the first axis from the lowest (0) to the highest category (4), with Categories 1 to 3 below the first axis and Category 4 well above. C5 and C6 behave differently: C6 diverges from this pattern for Category 4 (very often) whereas C5 diverges completely. In the second diagram (Axes 1 and 3), the pattern is a little erratic on the third axis, but the overall layout is the same for all items, with the highest categories positioned lower.
Figure 1.
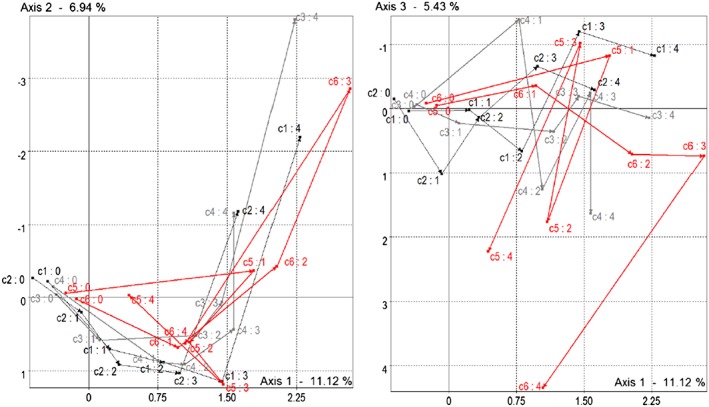
Multiple correspondence analysis of the Cannabis Abuse Screening Test, factorial plans 1 and 2
In summary, the first dimension of the CAST is a combination of all CAST items, whereas the second is driven by the extreme frequencies of non‐standard use (C1 and C2), memory problems (C3), and to a lesser extent reproaches (C4) and frequent problems (C6), as opposed to low‐intermediate frequencies (i.e., Categories 1 to 3) for these items. The third CAST axis is a mix of extreme frequencies of reproaches (C4), unsuccessful attempts to quit (C5) and problems (C6).
The MCA of the DSM‐5 provides three first eigenvalues that explain 30.0%, 10.1%, and 8.9% of the total inertia, respectively, two dimensions being sufficient for an adequate description (Lg = 1.57), the DSM‐5 being almost one‐dimensional. All items contribute to the first dimension, and all except three remain close to the second or third axis in Figure 2. The exceptions are Items D3 (craving), D1 (role impairment), and D10 (reduced activities): They are the major contributors to the second axis (39.0%, 19.2%, and 15.4%, respectively) whereas D3 is the major contributor to Axis 3 (24.0%). Craving thus has a special role in the DSM‐5, because it strongly contributes to the second and third dimensions.
Figure 2.
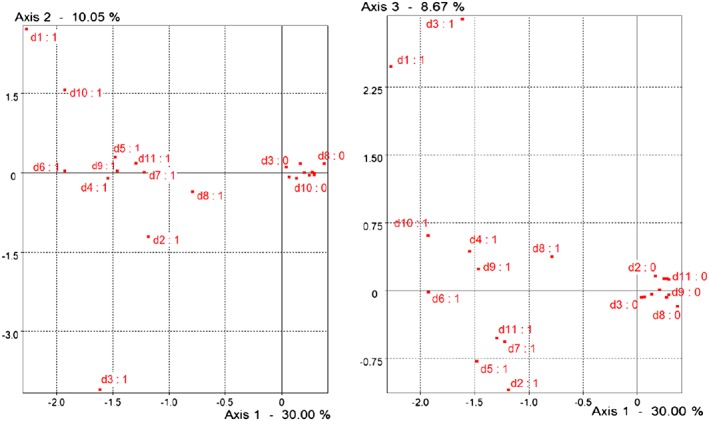
Multiple correspondence analysis of the Diagnostic and Statistical Manual of Mental Disorders‐5, factorial plans 1 and 2
3.5. MFA: Communalities of the CAST and the DSM‐5
The RV coefficient between the CAST and the DSM‐5 is .23, a rather low value due to the large difference in Lg coefficients. The first three eigenvalues of the compromise account respectively for 13.8%, 5.2%, and 4.4% of the total inertia (obtained for 35 eigenvalues), two dimensions being sufficient for an adequate description (Lg = 2.33).
Figure 3 shows the projections of the first three partial axes of the DSM‐5 and the CAST in the two first factorial plans (the subsequent partial axes are negligible and were discarded). The two instruments contribute equally to the first dimension (50%), whereas the CAST is the main contributor to the second and third dimensions (97.2% and 75.4%, respectively) through its partial axes.
Figure 3.
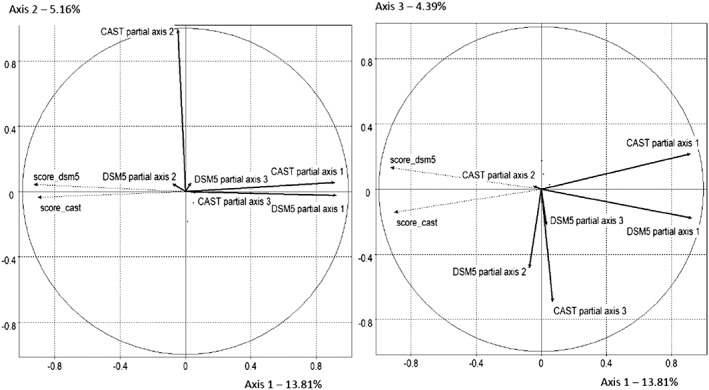
Multiple factor analysis: Partial axes of the categorical Cannabis Abuse Screening Test (CAST) and the Diagnostic and Statistical Manual of Mental Disorders (DSM)‐5
In summary, Figures 1, 2, 3 show that the CAST and the DSM‐5 have a first strong dimension in common, but that beyond, variance is almost completely due to the CAST. The DSM‐5 contributions to the second and third common dimensions are negligible.
3.6. MFA: Differences between the DSM and the CAST
Figure 4 shows the partial representations of some particular answers to the CAST and DSM‐5 items. For example, people answering “rarely” to C3 (i.e., C3 = 1) differ only slightly in the CAST and DSM‐5 spaces: They are very close on the first axis to their DSM‐5 point of view whereas their CAST point of view is clearly negative on the second axis. This is generally the case for the intermediate categories of answers to all CAST items. Conversely, representations differ markedly for the higher levels of C3: For the corresponding individuals, representations are fairly close on the first common axis, but while the DSM‐5 representations remain close, the CAST representations are well above. This is particularly clear for C3 = 4 (very often) and for C1 = C2 = C4 = 4 and C6 = 3. This means that the lower categories of these CAST items are adequately represented by the first (common) dimension (and thus by the DSM‐5) but that the higher categories are not adequately detected by the DSM‐5, with the exception of C5 = 4, which is close to 0.
4. DISCUSSION
4.1. Summary
We found that, according to CFA, the DSM‐5 could be considered unidimensionnal (although two correlated factors provided the best solution), whereas the CAST has two correlated factors, non‐standard use (C1 and C2) and problems (C3 to C6). The CAST showed high discriminant power to screen for moderate/severe and severe DSM‐5 CUD symptoms (cut‐off = 5 and 8, respectively). Using MFA, we showed that the relationships between the CAST and the DSM‐5 can be described by two orthogonal common main dimensions. The first and major common dimension is equally shared by both instruments: It may be interpreted from the CAST or the DSM‐5 point of view as a sum of intensity of use and problems or DSM‐5 symptoms and thus reflects the correlation between the scores of the two instruments. The second common dimension is the second CAST dimension exclusively. Our study explains why the CAST shows good performances in screening for DSM‐5 diagnoses: This is due to the first dimension that is common to both instruments. On the opposite, our study explains why the CAST screens individuals that are not diagnosed by the DSM‐5 although they present many behaviours that can be associated with cannabis disorders (Bastiani et al., 2017; Legleye et al., 2011) and why the proportion of false positives is high (see Table 3). Some people who report very often smoking cannabis before midday or alone (C1 and C2), having memory problems (C3), or receiving reproaches from their friends/family (C4) do not answer positively to most of the DSM‐5 items and are not detected by the DSM‐5 CUD diagnoses. This structure confirms that the CAST screens a broader spectrum of cannabis use patterns than the DSM‐5.
Despite this finding, it is noteworthy to remind that, as the DSM‐5 CUD prevalences are low (see Table 1), it is not surprising to get low positive predictive values and high false positive rates, even with high sensibility and specificity (Altman & Bland, 1994; Murphy et al., 1987).
4.2. Comparison with other studies
This study confirms some previous results obtained in adults (Cuenca‐Royo et al., 2012; Gyepesi et al., 2014; Legleye et al., 2015; Sznitman, 2016) or in adolescents (Legleye et al., 2011; Legleye et al., 2013). The CAST structure obtained using CFA is similar (same factors, similar loadings and high correlation between factors) and despite the use of the DSM‐5 instead of an empirical gold standard derived from the DSM‐IV TR, the cut‐offs for screening DSM classes of symptoms are identical, suggesting that the previous empirical classes of symptoms were very close to the DSM‐5 class of symptoms. This is an important result because it was obtained with a larger sample and with weighted analyses.
The study also sheds light on the particular behaviour of C5 and C6. Their low correlations with the CAST score have already been noted although not investigated in previous publications (Legleye et al., 2015; Legleye et al., 2011). In particular, we show that C5 has a special role within the CAST because of its ceiling effect. This may be due to its complex negative wording and thus suggests that this needs to be reviewed. Nevertheless, we show that this item contributes only to the first common axis in the MFA and thus the DSM‐5, showing that it fits its purpose, which is to capture behaviours that are strongly related to craving and dependence. Alongside, very few individuals reported extreme frequency for C6: These findings could question the rating of C5 and C6 so as to improve the CAST structure and possibly its screening properties (Bastiani et al., 2013).
In contrast, the specific, strong correlation between the non‐standard use (C1 and C2) and the DSM‐5, and its potential to improve the consistency and the screening properties of the DSM has already been noted in adolescents (Piontek, Kraus, Legleye, & Buhringer, 2011). Our study shows that memory problems (C3) could also play a similar role, because this dimension shows a very similar pattern in MFA.
Regarding DSM‐5, we found that a two‐factor solution (with craving and impaired control as secondary factor) had better fit indexes than the expected unidimensional structure. Similar results were already found in the stufy of Agrawal et al., 2014, but this calls for replications, and further research has to study whether these two items measure the same construct.
4.3. Limitations
Despite its large and representative sample, this study has a number of the classic limitations of telephone surveys. First, there is the possibility of underreporting of cannabis use because of the presence of an interviewer (even only on the phone; Beck & Peretti‐Watel, 2002), an effect known as the social desirability bias (De Leeuw, 2008). But as the Munich Composite International Diagnostic Interview and the CAST were both administered this way, this may not have altered the correlations of the instrument items. Second, as the participation rate was not 100%, it is possible that nonrespondents have different cannabis use behaviours, which could bias the estimates, despite the use of weights.
As found recently, the CAST is not fully invariant towards age (Sznitman, 2016), whereas some items in the DSM itself are not fully invariant towards gender (Agrawal & Linskey, 2007; Piontek et al., 2011) and possibly both age and gender (Legleye et al., 2015). A stratified MFA could be used to study the communalities of the CAST and the DSM in various age and gender groups, but testing the influence of age and gender on the relationships between the CAST and the DSM would require totally different methods, beyond the scope of this article.
This study used survey data collected in general population: We focussed on CUD that is usually monitored in public health. We did not consider withdrawal or intoxication that are usually of interest in clinical setting. However, a replication of the study in clinical setting, where the CUD can be administered by a trained physician, would be of great interest to describe the patterns of problematic use that are not considered in the DSM‐5. A longitudinal follow‐up may also help evaluating the concept of problematic use and its predictive power on future functioning.
5. CONCLUSION
The CAST was designed to screen for problematic use in the general population. This study confirmed its latent structure and its performance in screening for DSM‐5 CUD diagnoses. These latter are explained by the strong dimension that the CAST and the DSM‐5 have in common. On the opposite, the second CAST dimension, defined by extreme frequencies of use before midday and alone, memory problems, and reproaches from friends/family, is almost orthogonal to the DSM‐5, explaining why the CAST screens for patterns that are not detected by the DSM‐5.
CONTRIBUTORS
The author is the sole contributor.
DECLARATION OF INTEREST STATEMENT
The author does not have any conflict of interest to declare.
ACKNOWLEDGEMENTS
I would like to thank the Health Barometer team for its remarkable survey and its support, as well as Elisabeth Morand at the INED and Brigitte Gelein at the Ecole nationale de la statistique et de l'analyse de l'information (ENSAI) for their advices and remarks during the study.
Legleye S. The Cannabis Abuse Screening Test and the DSM‐5 in the general population: Optimal thresholds and underlying common structure using multiple factor analysis. Int J Methods Psychiatr Res. 2018;27:e1597 10.1002/mpr.1597
Pubmed.com agrawal cannabis dsm 2014
REFERENCES
- Abdi, H. , Williams L.J., and Valentin D.. 2013. “Multiple factor analysis: Principal component analysis for multitable and multiblock data sets.” WIREs Comput Stat https://www.utdallas.edu/~herve/abdi-WiresCS-mfa-2013.pdf.
- Agrawal, A. , & Linskey, M. T. (2007). Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the National Epidemiological Survey on alcohol and related conditions. Drug and Alcohol Dependence, 88(2–3), 300–307. 10.1016/j.drugalcdep.2006.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal, A. , Lynskey, M. T. , Bucholz, K. K. , Kapoor, M. , Almasy, L. , Dick, D. M. , … Bierut, L. J. (2014). DSM‐5 cannabis use disorder: A phenotypic and genomic perspective. Drug and Alcohol Dependence, 134, 362–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman, D. G. , & Bland, J. M. (1994). Diagnostic tests 2: Predictive values. British Medical Journal, 309, 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annaheim, B. , & Legleye, S. (2017). Short instruments to screen for “problematic” cannabis use in general population surveys In Preedy V. R. (Ed.), Handbook of cannabis and related pathologies. Biology, pharmacology, diagnosis and treatment (pp. e168–e184). London, UK: Academic Press. [Google Scholar]
- Annaheim, B. , Scotto, T. J. , & Gmel, G. (2010). Revising the cannabis use disorders identification test (CUDIT) by means of item response theory. International Journal of Methods in Psychiatric Research, 19(3), 142–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA . 2013. “Changes from DSM‐IV TR to DSM‐5.” http://www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf.
- Asparouhov, T. (2005). Sampling weights in latent variabel modeling. Structural Equation Modeling, 12(3), 411–434. [Google Scholar]
- Baillie, A. J. , & Teesson, M. (2010). Continuous, categorical and mixture models of DSM‐IV alcohol and cannabis use disorders in the Australian community. Addiction, 105(7), 1246–1253. [DOI] [PubMed] [Google Scholar]
- Bashford, J. , Ross, F. , & Copeland, J. (2010). The cannabis use problems identification test (CUPIT): Development, reliability, concurrent and predictive validity among adolescents and adults. Addiction, 105(4), 615–625. [DOI] [PubMed] [Google Scholar]
- Bastiani, L , Potente, R , Scalese, M , Siciliano, V , Fortunato, L , and Molinaro, S . 2017. “The Cannabis Abuse Screening Test (CAST) and its applications.” In Handbook of cannabis and related pathologies. Biology, pharmacology, diagnosis, and treatment, Academic Press, 971–80. London, UK: Preedy, Victor R . [Google Scholar]
- Bastiani, L. , Siciliano, V. , Curzio, O. , Luppi, C. , Gori, M. , Grassi, M. , & Molinaro, S. (2013). Optimal scaling of the CAST and of SDS scale in a national sample of adolescents. Addictive Behaviors, 38(4), 2060–2067. [DOI] [PubMed] [Google Scholar]
- Beck, F. , & Legleye, S. (2008). Measuring cannabis related problems and dependence at the population level In A cannabis reader: Global issues and local experiences (Vol. 2) (pp. 29–57). Lisbon: EMCDDA. [Google Scholar]
- Beck, F. , & Peretti‐Watel, P. (2002). The impact of data collection methodology on the reporting of mode de illicit drug use by adolescents. Population, 57(3), 571–591. [Google Scholar]
- Brown, T. A. (2015). Confirmatory factor analysis for applied research (2d ed.). Methodology in the Social Sciences. New York: The Guilford Press. [Google Scholar]
- Cuenca‐Royo, A. M. , Sánchez‐Niubó, A. , Forero, C. G. , Torrens, M. , Suelves, J. M. , & Domingo‐Salvany, A. (2012). Psychometric properties of the CAST and SDS scales in young adult cannabis users. Addictive Behaviors, 37(6). [DOI] [PubMed] [Google Scholar]
- De Leeuw, E. D. (2008). Choosing the method of data collection In De Leeuw E. D., Hox J. J., & Dillman D. A. (Eds.), International Handbook of Survey Methodology (pp. 117–135). New York: Lawrence Earlbaum Associates. [Google Scholar]
- Degenhardt, L. , Coffey, C. , Carlin, J. B. , Swift, W. , & Patton, G. C. (2008). Are diagnostic orphans at risk of developing cannabis abuse or dependence? Four‐year follow‐up of young adult cannabis users not meeting diagnostic criteria. Drug and Alcohol Dependence, 92(1–3), 86–90. [DOI] [PubMed] [Google Scholar]
- EMCDDA . 2007. Drug situation. Screening for problem or dependent cannabis use. Drugnet Europe, April–June 2007, Vol. 58 http://www.emcdda.europa.eu/html.cfm/index31435EN.html [Google Scholar]
- Escofier, B. , & Pagès, J. (1990). Multiple factor analysis. Computational Statistics and Data Analysis, 18, 121–140. [Google Scholar]
- Fernandez‐Artamendi, S. , Fernández‐Hermida, J. R. , Muñiz‐Fernández, J. , Secades‐Villa, R. , & García‐Fernández, G. (2012). Screening of cannabis‐related problems among youth: The CPQ‐A‐S and CAST questionnaires. Substance Abuse Treatment, Prevention, and Policy, 7(13), 2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett, E. S. , Eaton, W. W. , & Zeger, S. (2002). Methods for evaluating the performance of diagnostic tests in the absence of a gold standard: A latent class model approach. Statistics in Medicine, 21(9), 1289–1307. [DOI] [PubMed] [Google Scholar]
- Gillespie, N. A. , Neale, M. C. , Prescott, C. A. , Aggen, S. H. , & Kendler, K. S. (2007). Factor and item‐response analysis DSM‐IV criteria for abuse of and dependence on cannabis, cocaine, hallucinogens, sedatives, stimulants and opioids. Addiction, 102(6), 920–930. [DOI] [PubMed] [Google Scholar]
- Gyepesi, A. , Urbán, R. , Farkas, J. , Kraus, L. , Piontek, D. , Paksi, B. , … Demetrovics, Z. (2014). Psychometric properties of the Cannabis Abuse Screening Test in Hungarian samples of adolescents and young adults. European Addiction Research, 20(3), 119–128. [DOI] [PubMed] [Google Scholar]
- Hall, W. (2014). What research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction, 110(1), 19–35. [DOI] [PubMed] [Google Scholar]
- Hawkins, D. M. , Garrett, J. A. , & Stephenson, B. (2001). Some issues in resolution of diagnostic tests using an imperfect gold standard. Statistics in Medicine, 20(13), 1987–2001. [DOI] [PubMed] [Google Scholar]
- Hu, L. , & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. [Google Scholar]
- Husson, F. , Lê, S. , & Pagès, J. (2009). Exploratory multivariate analysis by example using R. London: Chapman & Hall/CRC. [Google Scholar]
- Lachner, G. , Wittchen, H. U. , Perkonigg, A. , Holly, A. , Schuster, P. , Wunderlich, U. , … Pfister, H. (1998). Structure, content and reliability of the Munich‐Composite International Diagnostic Interview (M‐CIDI) substance use sections. European Addiction Research, 4(1–2), 28–41. [DOI] [PubMed] [Google Scholar]
- Langenbucher, J. W. , Labouvie, E. , Martin, C. S. , Sanjuan, P. M. , Bavly, L. , Kirisci, L. , & Chung, T. (2004). An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM‐IV. Journal of Abnormal Psychology, 113(1), 72–80. [DOI] [PubMed] [Google Scholar]
- Legleye, S. , Guignard, R. , Richard, J. B. , Ludwig, K. , Pabst, A. , & Beck, F. (2015). Properties of the Cannabis Abuse Screening Test (CAST) in the general population. International Journal of Methods in Psychiatric Research, 24(2), 170–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legleye, S. , Piontek, D. , & Kraus, L. (2011). Psychometric properties of the Cannabis Abuse Screening Test (CAST) in a French sample of adolescents. Drug and Alcohol Dependence, 113(2–3), 229–235. [DOI] [PubMed] [Google Scholar]
- Legleye, S. , Piontek, D. , Kraus, L. , Morand, E. , & Falissard, B. (2013). A validation of the Cannabis Abuse Screening Test (CAST) using a latent class analysis of the DSM‐IV among adolescents. International Journal of Methods in Psychiatric Research, 22(1), 16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, G. , Copeland, J. , Gates, P. , & Gilmour, S. (2006). The severity of dependence scale (SDS) in an adolescent population of cannabis users: Reliability, validity and diagnostic cut‐off. Drug and Alcohol Dependence, 83(1), 90–93. [DOI] [PubMed] [Google Scholar]
- Murphy, J. M. , Berwick, D. M. , Weinstein, M. C. , Borus, J. F. , Budman, S. H. , & Klerman, G. L. (1987). Performance of screening and diagnostic tests: Application of receiver operating characteristic analysis. Archives of General Psychiatry, 44, 550–555. [DOI] [PubMed] [Google Scholar]
- Muthen, B. (2006). Should substance use disorders be considered as categorical or dimensional? Addiction, 101(Suppl 1), 6–16. [DOI] [PubMed] [Google Scholar]
- Piontek, D. , Kraus, L. , & Klempova, D. (2008). Short scales to assess cannabis‐related problems: A review of psychometric properties. Substance Abuse Treatment, Prevention, and Policy, 3, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piontek, D. , Kraus, L. , Legleye, S. , & Buhringer, G. (2011). The validity of DSM‐IV cannabis abuse and dependence criteria in adolescents and the value of additional cannabis use indicators. Addiction, 106(6), 1137–1145. [DOI] [PubMed] [Google Scholar]
- Rey, J. M. , Morris‐Yates, A. , & Stanislaw, H. (1992). Measuring the accuracy of diagnostic tests using receiver operating characteristics (ROC) analysis. International Journal of Methods in Psychatric Research, no., 2, 1–11. [Google Scholar]
- Richard, J.‐B. , Gautier, A. , Guignard, R. , Léon, C. , & Beck, F. (2014). Méthode D'enquête Du Baromètre Santé 2014. Baromètre santé, 20. [Google Scholar]
- Robert, P. , & Escoufier, Y. (1976). A unifying tool for linear multivariate statistical methods: The RV‐coefficient. Applied Statistics, 25, 257–265. [Google Scholar]
- Steiner, S. , Baumeister, S. E. , & Kraus, L. (2008). Severity of dependence scale: Establishing a cut‐off point for cannabis dependence in the German adult population. Sucht, 54(1), S57–S63. [Google Scholar]
- Sznitman, Rödner S. 2016. “The Cannabis Abuse Screening Test (CAST) revisited: Examining measurement invariance by age.” International Journal of Methods in Psychiatric Research, October. doi: 10.1002/mpr.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teesson, M. , Lynskey, M. , Manor, B. , & Baillie, A. (2002). The structure of cannabis dependence in the community. Drug and Alcohol Dependence, 68(3), 255–262. [DOI] [PubMed] [Google Scholar]
- Wittchen, H.‐U. , Beloch E., Garczynski E., Holly A., Lachner G., Perkonigg A., Pfütze E.‐M., et al. 1995. “Münchener Composite International Diagnostic Interview (M‐CIDI), Paper‐Pencil 2.2, 2/95.”


