Abstract
We investigated differential treatment effects on specific eating disorder (ED) indicators to enhance conclusions about treatment efficacy. Profile Analysis via Multidimensional Scaling, which identifies core profiles in a population and interprets person profiles with core profile information, was utilized to identify core profiles from a sample of 5,177 patients who were repeatedly measured with the ED inventory‐2 at admission and at discharge. To assess differential treatment effects for individual ED indicators, we compared the core profiles at admission with those at discharge. Three core profiles were identified and labeled as High Body Dissatisfaction with Low Bulimia (Core Profile 1), High Interoceptive Awareness with Low Body Dissatisfaction (Core Profile 2), and High Ineffectiveness with Low Bulimia (Core Profile 3). Treatment had the greatest effects on Core Profile 2. The patients whose profile patterns were similar to that of Core Profiles 1 and 2 were positively related with weight gain. However, treatment was least on Core Profile 3, and the patients whose profile patterns were like that of Core Profile 3 were negatively related with weight gain. In conclusion, those patients who fit Core Profile 3 may benefit from different treatment modalities than those that are standard in inpatient settings.
Keywords: eating disorders, profile analysis via multidimensional scaling (PAMS), the bootstrapping method, treatment efficacy
1. INTRODUCTION
Given the potentially grave nature of eating disorders coupled with high relapse rates post‐treatment (Stice, Becker, & Yokum, 2013), isolating treatment effects for various eating disorder (ED) indicators is critical. However, prior studies have not been able to identify whether some ED indicators may be more amendable to inpatient treatment than others. The current study is designed to investigate how treatment differentially impacts patients with varying symptom profiles in terms of their observed mean scores and latent dimension scores.
Across the different diagnoses, eating disorders are marked by unhealthy eating behaviors and weight regulation as well as a wide range of adverse psychological, physical, and social consequences (Diagnostic and Statistical Manual of Mental Disorders [DSM‐5], American Psychiatric Association [APA], 2013). A high level of dysfunction accompanies eating disorders including a host of dangerous medical complications (Patrick, 2002) as well as disparate psychological correlates such as interpersonal problems (Connan et al., 2009; Hartmann, Zeeck, & Barrett, 2009), substance abuse (Courbasson & Brunshaw, 2009; Newman & Gold, 1992), and suicidality (Papadopoulos, Ekbom, Brandt, & Ekselius, 2009). Given the complexity of presenting problems, eating disorders are difficult to treat (Bulik, Berkman, Brownley, Sedway, & Lohr, 2007; Ricca, Mannucci, Zucchi, Rotella, & Faravelli, 2000) and likelihood of achieving full recovery is low (Herzog et al., 1999).
1.1. Transdiagnostic ED indicators
As a part of efforts to understand the complex nature of EDs and to effectuate their treatment, EDs have been clinically defined as several discrete entities (e.g., anorexia nervosa, bulimia nervosa, binge eating disorder, and eating disorder not otherwise specified/other specified feeding or eating disorder) that are supposed to be qualitatively different from one another according to the DSM‐5. However, this conceptualization has been challenged (Gordon, Holm‐Denoma, Smith, Fink, & Joiner, 2007). For example, taxonometrics, which is designed to classify the latent structure of phenomena (Meehl & Golden, 1982), has shown that hallmark ED indicators occur across different diagnoses rather than manifesting only in discrete categories (Gleaves, Lowe, Green, Cororve, & Williams, 2000; Tylka & Subich, 2003; Williamson et al., 2002), indicating that EDs may fall on a continuum. Discriminant function analysis has also found support for ED dimensions which may not be totally discrete (Stice, Killen, Hayward, & Taylor, 1998). Also, “cycling” between EDs appears to be common. For example, one study found that the majority of women who had been classified as anorexia nervosa were reclassified over a 7‐year period: Over half fluctuated between the restricting and binge eating/purging anorexia nervosa subtypes; one third crossed over to bulimia nervosa (Eddy et al., 2008). These results imply that there is fluidity between ED diagnoses.
As support of the fluidity between ED diagnoses, Olatunji, Kim, and Wall (2015) identified common symptom dimensions that appear across diagnoses. Identifying common symptom dimensions was an important extension of transdiagnostic theory. However, this work did not examine whether ED indicators in the common dimensions were improved or deteriorated after treatment, which would be crucial information to augment the effectiveness of current treatment approaches. Therefore, in the present study, we hypothesize that similar symptom dimensions would be found before treatment; however, we predict that there will be differences in ED indicators after standard treatments (e.g., in inpatient facilities, cognitive behavioral therapy (CBT)‐oriented psychotherapy, nutrition education, and medication), which may help to explain the variability in its effectiveness.
2. METHOD
2.1. Participants
Participants consisted of 5,193 female patients who met Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV text revision; APA, 2010) criteria for a principal eating disorder diagnosis at the Remuda Ranch Programs for EDs in Wickenburg, Arizona. Remuda had previously created a de‐identified database of patient admission and discharge body mass index (BMI) and ED inventory‐2 (EDI‐2) scores. The Institutional Review Board approval was granted from Fordham University to utilize this dataset for the present analyses. Those who had BMI below 14 or above 40 were excluded from further analyses reducing the sample to 5,177; such inputs were considered errors because values below and above these thresholds are biologically unlikely. The sample consisted of anorexia nervosa (N = 2,071, 39.7%); bulimia nervosa (N = 1632, 31.5%); and eating disorder not otherwise specified (N = 1,474, 28.5%) patients. The age range was from 12 to 68 (M = 22, SD = 8.8). The sample was 93.6% Caucasian, 2.7% Mixed/Unknown, 2.1% Hispanic, 0.9% Asian, 0.7% African American, and 0.2% Native American. For diagnoses, a team of professionals interviewed individual patients within 2 days of admission and gathered detailed information about patient backgrounds and symptoms using proprietary structured formats. To facilitate objective diagnoses, all patients received admission drug screens and completed extensive and comprehensive psychological testing to determine the specific eating disorder diagnosis as well as psychiatric comorbidity (e.g., Minnesota Multiphasic Personality Inventory‐2, Beck Depression Inventory‐II, and Yale‐Brown Obsessive Compulsive Scale); a complete listing of the assessment battery is available in Cumella, Kally, and Wall (2007). Then, a team psychiatrist and psychologist reached consensus and assigned admission diagnoses. The patients were treated with standard inpatient treatment components including CBT‐oriented psychotherapy, nutrition education and medication (Blinder, Cumella, & Sanathara, 2006). However, the majority of therapy in inpatient settings is delivered in group modalities; far less time is spent in individual psychotherapy (Frisch, Herzog, & Franko, 2006).
2.2. Measurement
Eating Disorders Inventory‐2 (Garner, 1991) is a self‐report measure of EDs that consists of 91 items organized into 11 subscales: Drive for thinness (Dt), Bulimia (Bu), Body dissatisfaction (Bd), Ineffectiveness (In), Perfectionism (Pf), Interpersonal distrust (Id), Interoceptive awareness (Ia), Maturity fears (Mf), Asceticism (As), Impulse regulation (Ir), and Social insecurity (Si). Research has shown that the 11 EDI‐2 subscales display significant test–retest reliability coefficients, ranging from 0.81 to 0.89 in an eating disorder group (Thiel & Paul, 2006), indicating that EDI‐2 has good psychometric properties. Patients completed the EDI‐2 during admission (or pre) to inpatient care and again approximately 49 days later at discharge (or post) from the program.
2.3. Introducing profile analysis via multidimensional scaling (PAMS)
To identify whether ED indicators are improved or deteriorated after treatment, we utilize profile analysis via multidimensional scaling (PAMS; e.g., Davison, Gasser, & Ding, 1996; Kim, Frisby, & Davison, 2004). PAMS estimates scale values for input variables (EDI‐2 symptom and personality measures in our study) in each dimension. However, different from ordinary multidimensional scaling (MDS), PAMS interprets an array of scale values in a dimension as their profile pattern and considers it as a core profile for person response profiles. Interpreting dimensions as core profiles has been supported and validated by numerous studies (e.g., Davison et al., 1996; Davison & Kuang, 2000; Frisby & Kim, 2008; Kim, 2010a, 2010b, 2013; Kim et al., 2004; Kim, Davison, & Frisby, 2007; McKay et al., 2014; Olatunji et al., 2015).
PAMS estimate three parameters: levels, person weights, and scale values. A level is defined as an average for a person (a person mean) or the mean of the scores in the person's profile. One level value is assigned to each person, and it determines a height of each person's profile. The person weights are analogous to correlations between person profiles and core profiles and measure how closely person profiles are related with core profiles. The scale values are elements of core profiles and their magnitudes and directions characterize dimensions as core profiles (see technical details in Kim et al., 2007).
2.3.1. PAMS for transdiagnostic ED symptom profiles
PAMS uniquely fits the transdiagnostic characteristics of ED symptom profiles (e.g., Olatunji et al., 2015), more so than other multivariate statistical methods (e.g., factor analysis). Factor analysis classifies the original input variables into small sets of homogeneous variables and defines these subsets as latent factors that characterize traits of individuals; thus, factor information is limited by a few homogenous variables. On the other hand, PAMS interprets dimensions not as single construct factors but as core profiles that include all input variables; thus, it is not necessary to classify the original variables into subsets of homogenous variables. Because all ED symptom indicators function as coordinates of profiles, the core profiles identified by PAMS are also transdiagnostic.
2.4. Data analytic strategy
2.4.1. Comparing pre‐ and post‐observed and latent scores
First, we will compare observed mean scores for the ED indicators between pre‐ and post‐treatment sessions. Second, we will examine scale value (i.e., latent score) changes for symptom indicators between pre‐ and post‐treatment sessions; there would be multiple scale value changes, depending number of dimensions. These scale value differences provide us clinically significant multidimensional information in addition to mean score differences.
2.4.2. Assessing individual patients
Also, we will conduct person‐level assessments: one for “between” and the other for “within.” For the between assessment, with information of level indexes, we will assess the overall treatment efficacy by comparing individual patients' level index scores at their admission and discharge. For the within assessment, with information of person weights, we will diagnose patients in terms of clinical information of core profiles. If patients have substantial weights on a specific core profile, we assume that ED indicators for those patients are characterized by the core profile information.
2.4.3. Simultaneous scaling
We will intentionally scale 22 EDI‐2 subscores (pre and post) all together. Because the patients were administered the same EDI‐2 subscales twice at pre and post, this simultaneous scaling allows us to compare pre and post scale values. If pre and post scores were scaled separately, PAMS (or any scaling methods) would consider pre and post as different samples, and the scale values will be normalized with a mean of zero in each sample (pre or post). Consequently, there would be no difference detected when we compare pre and post scale values.
2.4.4. Converting bootstrap mean scale values into z‐scores
The 22 bootstrap average scale values in each dimension will be converted into z‐scores (with a mean of zero and standard deviation of one) so that the scale value differences (pre–post) in a given dimension can be naturally viewed as effect sizes. The mean scale values are more reliable than the scale values from a single sample because they are averages of 2,000 bootstrap samples that contain all possible sampling variation from the original sample. We will interpret the scale value difference equal to or larger than +0.8, as corresponding to Cohen's large effect size, d ≥ 0.8 (Cohen, 1977). The positive effect sizes imply effective treatments. The effect size comparison is intended to avoid Type I errors, because a large sample (n = 5,177 in our sample) induces unreasonably small standard errors.
2.4.5. Bootstrap confidence intervals
MDS does not provide any statistics to test significance of scale values, and without statistical significance of scale values, interpreting dimensions as core profiles would be misleading. Thus, we will generate 2,000 bootstrap samples (recommended by Efron & Tibshirani, 1993) from the original sample to construct 95% bootstrap confidence intervals for scale values. To estimate the scale value confidence intervals, we used the R code developed by Kim (2010a). If the confidence intervals for scale values did not include zeros, the scale values would be statistically significant.
2.4.6. Generating a calibration and a validation sample
We will generate a calibration and a validation samples by randomly splitting the original sample into two. We will use the calibration sample to estimate the bootstrap empirical confidence intervals and mean scale values and use the validation sample to confirm the results from the calibration sample.
3. RESULTS
3.1. Paired t tests and reliability of EDI‐2
Paired t tests were conducted for the mean scores of 11 ED symptom/personality measures. The post means were statistically smaller than pre means at α = 0.01, implying that all symptoms were improved after treatment. However, the paired t‐test results did not provide differential contributions of individual symptom indicators to patient profiles (of the symptom indicator scores) but simply showed that the post means were significantly different from the pre means. The summary statistics and effect sizes are included in Table 1.
Table 1.
Observed pre and post means (standard deviations), and mean differences (pooled standard errors) of eating disorder indicators
| Pre mean (SD) | Post mean (SD) | Mean difference (pooled SE) | |
|---|---|---|---|
| Drive for thinness (Dt) | 13.75 (6.30) | 8.05 (6.64) | 5.70 (0.10) ** |
| Bulimia (Bu) | 5.81 (6.21) | 1.69 (3.10) | 4.13 (0.08) ** |
| Body dissatisfaction (Bd) | 17.32 (8.29) | 13.30 (8.72) | 4.02 (0.12) ** |
| Ineffectiveness (In) | 11.99 (7.44) | 5.89 (6.21) | 6.10 (0.10) ** |
| Perfectionism (Pf) | 8.38 (4.86) | 6.53 (4.48) | 1.85 (0.06) ** |
| Interpersonal distrust (Id) | 5.97 (4.49) | 3.35 (3.64) | 2.63 (0.06) ** |
| Interoceptive awareness (Ia) | 10.60 (6.88) | 5.37 (5.59) | 5.23 (0.10) ** |
| Maturity fear (Mf) | 5.86 (5.34) | 3.41 (4.02) | 2.45 (0.07) ** |
| Asceticism (As) | 8.29 (4.49) | 5.56 (3.89) | 2.74 (0.06) ** |
| Impulse regulation (Ir) | 4.41 (4.75) | 3.01 (4.01) | 1.41 (0.06) ** |
| Social insecurity (Si) | 8.08 (4.64) | 4.68 (4.10) | 3.41 (0.07) ** |
Note. SD , standard deviation; SE, standard error.
p ≤ 0.01.
3.2. Identifying dimensions
Because PAMS is an exploratory analysis, the appropriate dimensionality is determined by the recommended poorness‐fit‐index value (STRESS ≤ 0.05; Kruskal, 1964). Two, three, and four dimensions were compared. The STRESS values for two, three, and four dimensions were 0.075, 0.045, and 0.028, respectively. However, the third and fourth dimensions were somewhat redundant, and the three‐dimensional solution was chosen. Given the wide age range of the sample, there might be a development trends in their profiles, and we conducted exploratory analyses for each of three age groups (ages 12–20, 21–40, and 41–68) but found virtually no differences detected between them.
3.2.1. Labeling dimensions as core profiles
Figure 1 depicts the three pre and post core profiles. Although the 22 subscales were scaled together, pre and post were deliberately juxtaposed for comparison: The first 11 scale values were used to depict pre core profiles, and the other 11 scale values were used for post core profiles. We labeled core profiles mainly based on the pre core profile patterns because they were the base‐line profiles before treatment. Dimension 1 had a peak at Body dissatisfaction (Bd) and a valley at Bulimia (Bu) and was labeled as High Body Dissatisfaction with Low Bulimia. However, it was also high on Drive for thinness (Dt), which is consistent with body dissatisfaction. The first dimension usually shows the same pattern as the observed mean profile (that is an array of symptom indicator means; e.g., Kim & Lord‐Bessen, 2012) and indeed the correlation between them was perfect (r = 1.0). The second profile presents peaks in Interceptive awareness (Ia) but also in Bulimia (Bu) and Impulse regulation (Ir). Dimension 2 was labeled as High Interoceptive Awareness with Low Body Dissatisfaction. Conceptually, the second profile describes patients manifesting dysregulation; it appears to be isolating patients who are sensitive to internal cues coupled with exhibiting impulse control and related bulimia nervosa symptoms. Dimension 3 was labeled as High Bulimia with Low Ineffectiveness, but it included individuals with high Perfectionism (Pf), which may describe patients exhibiting preoccupation with self‐worth. However, Pf was not significant based on the bootstrap results, and caution is required for interpretation. Also, note that the profile labeling was based on the most pronounced and contributing ED indicators (peaks and valleys), but all other ED indicators, although they were not the most notable, were still included as characterizing the core profiles as a whole.
Figure 1.
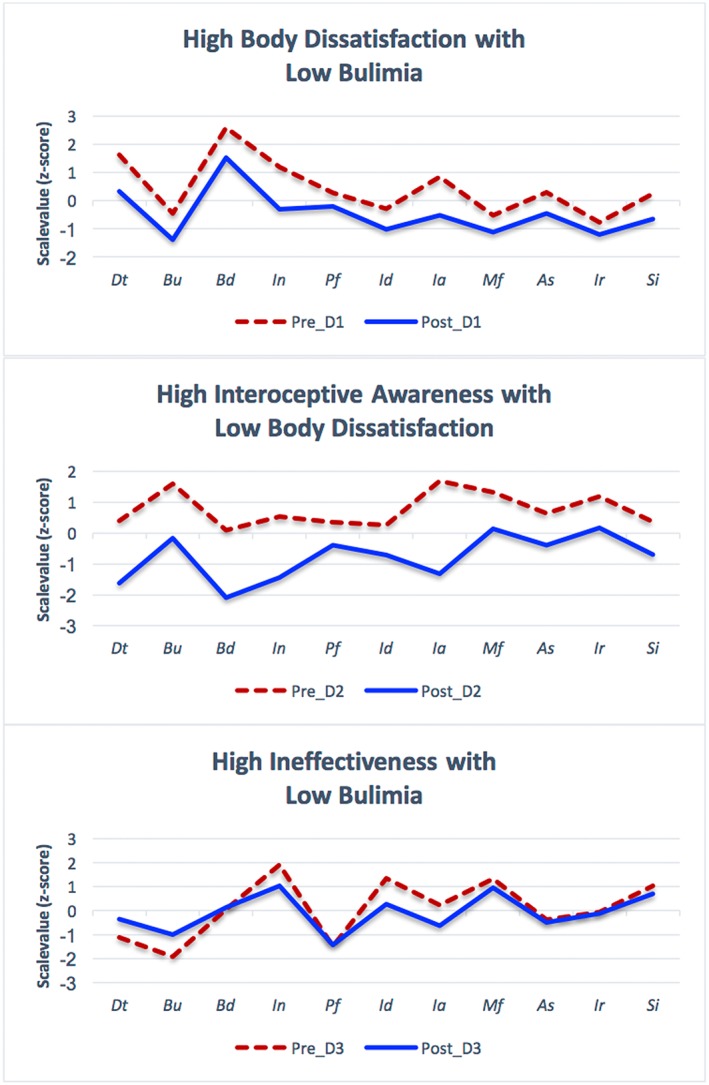
Pre and post Core profiles. Dt = Drive for thinness; Bu = Bulimia; Bd = Body dissatisfaction; In = Ineffectiveness; Pf = Perfectionism; Id = Interpersonal distrust; Ia = Interoceptive awareness; Mf = Maturity fears; As = Asceticism; Ir = Impulse regulation; and Si = Social insecurity
3.2.2. Effect sizes and contributions of ED indicators after treatment
We estimated effect sizes for each ED indicator after treatment. The treatment seemed most effective in the High Interoceptive Awareness with Low Body Dissatisfaction profile (Dimension 2) because of most effect sizes were over 1.00, except Pf (Perfectionism) and Id (Interpersonal distrust). Also, we estimated contributions (%) of the symptom indicators to the pattern variance that was accounted for by three core profiles. Because squared effect sizes (that were standard deviations in our study) were in fact variances, we estimated the symptom indicators' contributions, utilizing the pattern variance accounted for by each dimension as a weight (0.46 for Dimension 1; 0.12 for Dimension 2; and 0.07 for Dimension 3; see the last row in Table 2). As shown in Table 2, the contributions of Dt (10%), Bu (6%), Bd (7%), In (13%), and Ia (13%) were equal to or more than the average 6%. These five symptom indicators accounted for 75% (49% out of 65%) of the pattern variance explained by three core profiles.
Table 2.
Pre and post core profiles made of bootstrap mean coordinates and effect sizes
| Pre.1 | Pst.1 | Efsz (%) | Pre.2 | Pst.2 | Efsz (%) | Pre.3 | Pst.3 | Efsz (%) | Cont% | |
|---|---|---|---|---|---|---|---|---|---|---|
| Dt | 1.62 | 0.33 | 1.29 (7) | 0.39 | −1.63 | 2.02 (2) | −1.11 | −0.36 | 0.75 (1) | 10 |
| Bu | −0.45 | −1.39 | 0.94 (4) | 1.6 | −0.16 | 1.76 (1) | −1.91 | −1 | −0.91 (1) | 6 |
| Bd | 2.59 | 1.52 | 1.07 (5) | 0.10ns | −2.1 | 2.1 (2) | 0.06ns | 0.13ns | 0 (0) | 7 |
| In | 1.2 | −0.31 | 1.51 (10) | 0.53 | −1.44 | 1.97 (2) | 1.92 | 1.03 | 0.88 (1) | 13 |
| Pf | 0.28 | −0.2 | 0.49 (1) | 0.35 | −0.39 | 0.74 (0) | −1.49ns | −1.43ns | 0 (0) | 1 |
| Id | −0.29 | −1.03 | 0.74 (2) | 0.27 | −0.7 | 0.97 (0) | 1.35 | 0.28ns | 1.35 (2) | 5 |
| Ia | 0.84 | −0.52 | 1.36 (8) | 1.7 | −1.31 | 3.01 (3) | 0.23ns | −0.62 | 0.62 (1) | 13 |
| Mf | −0.52 | −1.12 | 0.6 (2) | 1.33 | 0.15ns | 1.33 (1) | 1.32ns | 0.95ns | 0 (0) | 2 |
| As | 0.29 | −0.45 | 0.74 (2) | 0.64 | −0.39 | 1.04 (0) | −0.37 | −0.5 | 0.13 (0) | 3 |
| Ir | −0.78 | −1.2 | 0.43 (1) | 1.19 | 0.17ns | 1.19 (0) | −0.07ns | −0.12ns | 0 (0) | 1 |
| Si | 0.24 | −0.66 | 0.9 (4) | 0.36 | −0.69 | 1.05 (0) | 1.03 | 0.7 | 0.33 (0) | 4 |
| Sum | 46 | 12 | 7 | 65 |
The contributions equal to or larger than the average 6% were bolded. The superscript “ns” refers to “not statistically significant” by the bootstrapping results, and the insignificant scale values were considered to be zero; thus, the effect sizes were adjusted accordingly. Cont% , contribution to pattern variance accounted for three core profiles; Dt , Drive for thinness; Bu , Bulimia; Bd , Body dissatisfaction; In , Ineffectiveness; Pf , Perfectionism; Id , Interpersonal distrust; Ia , Interoceptive awareness; Mf , Maturity fears; As , Asceticism; Ir , Impulse regulation; and Si , Social insecurity; Efsz , effect size (% , contribution for each indicator); Pre.1 , Dimension 1 from pre‐treatment; Pst.3 , Dimension 3 from post‐treatment.
3.2.3. Validation of core profile patterns
To confirm core profile patterns across samples, we correlated the core profiles identified from a validation sample (n = 2,587) with the core profiles estimated from a calibration sample (n = 2,590), and their correlations were 1.00 (for Dimension 1), 1.00 (for Dimension 2), and 0.99 (for Dimension 3). The correlational results indicate that the core profile patterns were virtually identical across the two samples. In the next section, we will empirically show utilities of the core profiles.
3.3. Diagnostic utility of PAMS
3.3.1. Relationships between BMI and core profiles
To assess how well/poorly improvement of ED indicators shown in the core profiles were related with weight recovery from a subsample of anorexia nervosa, we regressed the core profiles onto BMI at discharge. The R 2 was 0.11 (p < 0.01). The standardized coefficients were 0.10 (p < 0.01) for Core Profile 1; 0.15 (p < 0.01) for Core Profile 2; and −0.28 (p < 0.01) for Core Profile 3. Note that the standardized coefficients can be interpreted as effect sizes. Core Profiles 1 and 2 were positively related with BMI increase, but Core Profile 3 was negatively related. These results were consistent with Table 2 where the treatment effects appeared most pronounced in Core Profile 2 as indicated in its effect size (standardized coefficient). Yet in contrast, Core Profile 3 was negatively related with increase of BMI. In summary, those patients with response patterns like Core Profile 2 were expected to have greater weight gains than those who had response patterns like Core Profile 3.
3.3.2. Assessment of individual patients: Case 1
In this example, we demonstrate how to interpret patients in terms of core profile patterns. To do so, one should examine magnitudes of person weights for the patient of interest. The person weights (correlations) of Patient #82 with Core Profiles 1–3 were 0.91, −0.23, and 0.05, respectively and the three core profiles accounted for 87% (R2 = 0.87) of (within‐person) variance of Patient #82's response profile. However, because of the highest correlation with Core Profile 1, most of variance (0.912 = 0.83 or 83%) was accounted for Core Profile 1, and as shown in Figure 2, Patient #82's profile was similar to Core Profile 1. Also, we assessed the patient's overall improvement or deterioration with the profile level information: we subtracted the post level from the pre level: 1.27 − (−0.23) = 1.50, which means 1.5 standard deviation units improvement for Patient #82 after treatment in overall.
Figure 2.
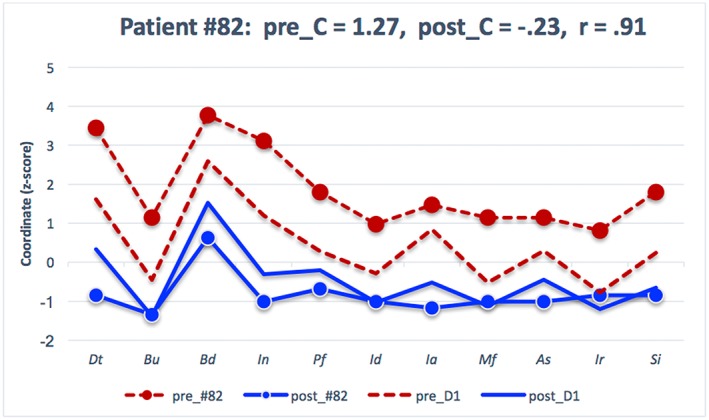
Individual‐level assessment: Pre/post patient #82's profiles juxtaposed with pre/post Core Profile 1 (dimension 1). Pre_#82 and post_#82 refer to Patient #82's response profiles in pre and post. Pre_C and post_C refer to pre and Ppst level indexes for Patient #82. pre_D1 and post_D1 refer to core response Profile 1 for pre and post. r = .91 represents correlation between Patient #82 profile and Core Profile 1. Dt = Drive for thinness; Bu = Bulimia; Bd = Body dissatisfaction; In = Ineffectiveness; Pf = Perfectionism; Id = Interpersonal distrust; Ia = Interoceptive awareness; Mf = Maturity fears; As = Asceticism; Ir = Impulse regulation; and Si = Social insecurity
3.3.3. Assessment of individual patients: Case 2
If patients have similar weights on all core profiles, how can one interpret those patients' response patterns in terms of core profile patterns? For example, Patient #56's weights on Core Profiles 1–3 were 0.65, 0.47, and 0.43, respectively, implying that this patient displayed features of all three core profiles. If these correlations were squared, Patient #56 had 42%, 22%, and 19% of shared (within person) variance with Core Profiles 1–3, respectively. Therefore, such patients would not be characterized with any single core profile pattern. Rather, those patients' profiles can be explained with one that is linearly combined by core profiles: For Patient #56, a specific profile can be made with a linear combination of the core profiles: 0.65 × 11 coordinates of Core Profile 1 +0.47 × 11 coordinates of Core Profile 2 +0.43 × 11 coordinates of Core Profile 3. There was no difference in pre and post level indexes, indicating that no overall treatment efficacy for Patient #56. When patients have similar magnitudes for the weights on certain core profiles, one can linearly combine the core profiles to make a new profile which fits to the patients' response profiles (as shown in Figure 3).
Figure 3.
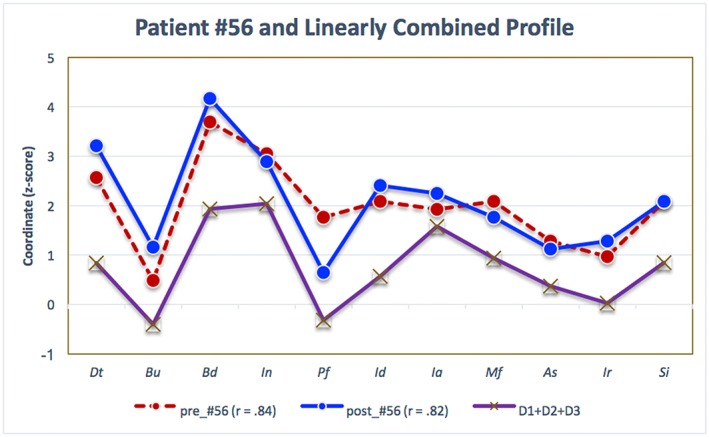
Pre and post Patient #56's profiles juxtaposed with a linearly combined profiles with three dimensions. pre_#56 (r = .84) and post_#56 (r = .82) refer to correlation of pre and post Patient #56's profiles with the linearly combined core profile (D1 + D2 + D3). Dt = Drive for thinness; Bu = Bulimia; Bd = Body dissatisfaction; In = Ineffectiveness; Pf = Perfectionism; Id = Interpersonal distrust; Ia = Interoceptive awareness; Mf = Maturity fears; As = Asceticism; Ir = Impulse regulation; and Si = Social insecurity
4. DISCUSSION
4.1. Relevancy to previous ED research
Identifying transdiagnostic core profiles has clinically meaningful implications as a better alternative to classification and potentially treatment matching (McKay et al., 2014; Olatunji et al., 2015). The previous research has shown that overevaluation of body weight and shape is a transdiagnostic process which cuts across purportedly distinct eating disorder diagnoses (Lampard, Tasca, Balfour, & Bissada, 2013). Our Core Profile 1 marked by two peaks, Drive for thinness and Body dissatisfaction, is also similar to the overevaluation of weight and shape that gives rise to many clinical characteristics of EDs. Findings derived from our profile analysis reflect the notion that common mechanisms are involved in the persistence and fluidity of anorexia nervosa, bulimia nervosa, and the atypical eating disorders (Fairburn et al., 1995; Sullivan, Bulik, Fear, & Pickering, 1998). To derive these findings, we analyzed pre and post scores separately while employing standardization techniques. Unlike ordinary scaling, we simultaneously scaled subscores from 2‐time points, pre and post, to compare changes in subscores in multidimensions. To see the subscore differences between pre and post in terms of effect sizes, we converted the simultaneously scale values (22 of them) into z‐scores in each dimension and considered the first half (11 of them) as pre subscores and the other half as post subscores. Then, we examined the differences of subscores which were in fact effect sizes; the differences of the absolute values that were larger than equal to 0.8 were considered meaningful changes.
4.2. Clinical and treatment implications
Therefore, our results shed light on how the symptom core profiles are impacted by treatment. With our profile analysis (which captures a full range of ED indicators), irrespective of diagnoses, it is possible to evaluate treatment effects generally, which is also in line with transdiagnostic cognitive behavioral accounts of eating disorders (e.g., Fairburn, 2008; Fairburn, Cooper, & Shafran, 2003). In this study, treatment appeared to be the most effective when a High Interoceptive Awareness with Low Body Dissatisfaction profile (Core Profile 2) was present because all ED indicators, except Perfectionism, were significantly alleviated after treatment. This suggests that the standard components of inpatient treatment work best for patients who are sensitive to stimuli originating within the body. Although this is speculative given limited information about the exact therapeutic techniques employed within each broader domain (e.g., CBT), it seems that features of Core Profile 2, like interoceptive awareness, are more amendable to the prominent modality of group therapy and/or ancillary modalities such as dialectical behavioral therapy which effectively addresses emotion dysregulation. Similarly, although improvements were not as robust in Core Profile 1, High Body Dissatisfaction with Low Bulimia, positive change in BMI was noted. Taken together, it appears that body dissatisfaction alone is not a strong indicator of treatment success but instead the constellation of symptoms is more important to consider.
Conversely, there was lesser improvement in High Ineffectiveness with Low Bulimia (Core Profile 3), which is characterized by global dissatisfaction with oneself and insecure relationships. Perhaps the most important take home message is that there are certain clusters of symptoms, like global dissatisfaction with oneself, which appear to be less responsive to the inpatient treatment milieu and would perhaps be better suited for empirically supported intensive individual psychotherapy. In fact, from a cost‐effectiveness perspective, an important next step suggested by these findings, is to discern if there are some patients whose symptoms profiles are less suitable to the inpatient context all together.
4.3. Advantages of PAMS
Usually, profiles are identified using data from a single time point. In our study, we profile‐analyzed individual patients with 2‐time points (pre and post) and therefore could offer insights about change over time. The similar study has been done at a single time point (e.g., Olatunji et al., 2015) but not at two time points investigated in our study. The profile comparison between pre and post allowed us to not only study overall treatment efficacy but also pinpoint improvement or deterioration of specific ED symptom indicators included in the profiles. Although we profile‐analyzed the longitudinal data with only 2‐time points, the current profile analytic paradigm can be easily applied to multiple time points. This capacity of the profile analysis can help to describe and monitor patients with multidimensional symptoms over the course of time or after intervention. This is a significant advance over the taxonomic classification. In conclusion, the profile analysis introduced here was able to elucidate differential treatment effects for ED patients in the context of a longitudinal and transdiagnostic approach. This approach has broad applications for evaluation of psychological interventions applied to polythetic presentations.
4.4. Limitations
The present study has several limitations: (a) The current findings are limited by utilization of only one treatment site, although this pattern may well be commonplace, given the relative consistency of ED inpatient treatment targets (Yager et al., 1993); (b) because of a lack of detailed information about the specific treatment techniques employed, we are unable to dissect to what extent CBT or dialectical behavioral therapy was employed versus group therapy and within each, which techniques were presented and emphasized; and lastly, (c) there was no control sample of ED patients who were not treated, which might call into question whether the treatment effect may be caused by natural recovery. However, considering the length of stay, 50 days on average, we conjecture that improvements were associated with their stay at the facility. Overall, the present findings suggest that profile analyses can be used to determine which standard treatment approaches are effective for different symptom clusters while also highlighting symptoms that may need to be targeted differently.
Kim S‐K, Annunziato RA, Olatunji BO. Profile analysis of treatment effect changes in eating disorder indicators. Int J Methods Psychiatr Res. 2018;27:e1599 10.1002/mpr.1599
REFERENCES
- American Psychiatric Association (2010). Diagnostic and statistical manual of mental disorders, Fourth edition (text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, Fifth edition (DSM‐5). Arlington, VA: American Psychiatric Association; 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Blinder, B. J. , Cumella, E. J. , & Sanathara, V. A. (2006). Psychiatric comorbidities of female inpatients with eating disorders. Psychosomatic Medicine, 68(3), 454–462. 10.1097/01.psy.0000221254.77675.f5. [DOI] [PubMed] [Google Scholar]
- Bulik, C. M. , Berkman, N. D. , Brownley, K. A. , Sedway, J. A. , & Lohr, K. N. (2007). Anorexia nervosa treatment: A systematic review of randomized controlled trials. International Journal of Eating Disorders, 40(4), 310–320. 10.1002/eat.20367. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1977). Statistical power analysis for the behavioral sciences. Routledge. [Google Scholar]
- Connan, F. , Dhokia, R. , Haslam, M. , Mordant, N. , Morgan, G. , Pandya, C. , & Waller, G. (2009). Personality disorder cognitions in the eating disorders. Behaviour Research and Therapy, 47(1), 77–82. 10.1016/j.brat.2008.10.010. [DOI] [PubMed] [Google Scholar]
- Courbasson, C. , & Brunshaw, J. M. (2009). The relationship between concurrent substance use disorders and eating disorders with personality disorders. International Journal of Environmental Research and Public Health, 6(7), 2076–2089. 10.3390/ijerph6072076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumella, E. J. , Kally, Z. , & Wall, D. A. (2007). Treatment responses of inpatient eating disorder women with and without co‐occurring obsessive‐compulsive disorder. Eating Disorders, 15(2), 111–124. 10.1080/10640260701190634. [DOI] [PubMed] [Google Scholar]
- Davison, M. L. , Gasser, M. , & Ding, S. (1996). Identifying major profile patterns in a population: An exploratory study of WAIS and GATB patterns. Psychological Assessment, 8(1), 26–31. 10.1037/1040-3590.8.1.26. [DOI] [Google Scholar]
- Davison, M. L. , & Kuang, H. (2000). Profile patterns: Research and professional interpretation. School Psychology Quarterly, 15(4), 457–464. 10.1037/h0088801. [DOI] [Google Scholar]
- Eddy, K. T. , Dorer, D. J. , Franko, D. L. , Tahilani, K. , Thompson‐Brenner, H. , & Herzog, D. B. (2008). Diagnostic crossover in anorexia nervosa and bulimia nervosa: Implications for DSM‐V. American Journal of Psychiatry, 165(2), 245–250. 10.1176/appi.ajp.2007.07060951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron, B. , & Tibshirani, R. J. (1993). An introduction to the bootstrap. New York: Chapman & Hall; 10.1007/978-1-4899-4541-9. [DOI] [Google Scholar]
- Fairburn, C. G. (2008). Eating disorders: The transdiagnostic view and the cognitive behavioral theory In Fairburn C. G. (Ed.), Cognitive behavior therapy and eating disorders (pp. 7–22). New York: The Guilford Press. [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. 10.1016/S0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Fairburn, C. G. , Norman, P. A. , Welch, S. L. , O'Connor, M. E. , Doll, H. A. , & Peveler, R. C. (1995). A prospective study of outcome in bulimia nervosa and the long‐term effects of three psychological treatments. Archives of General Psychiatry, 52(4), 304–312. 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- Frisby, C. L. , & Kim, S.‐K. (2008). Using profile analysis via multidimensional scaling (PAMS) to identify core profiles from the WMS‐III. Psychological Assessment, 20(1), 1–9. 10.1037/1040-3590.20.1.1. [DOI] [PubMed] [Google Scholar]
- Frisch, M. J. , Herzog, D. B. , & Franko, D. L. (2006). Residential treatment for eating disorders. International Journal of Eating Disorders, 39(5), 434–442. 10.1002/eat.20255. [DOI] [PubMed] [Google Scholar]
- Garner, D. M. (1991). Eating disorder inventory‐2 manual. Odessa Fla: Psychological Assessment Resources. [Google Scholar]
- Gleaves, D. H. , Lowe, M. R. , Green, B. A. , Cororve, M. B. , & Williams, T. L. (2000). Do anorexia and bulimia nervosa occur on a continuum? A taxometric analysis. Behavior Therapy, 31(2), 195–219. 10.1016/S0005-7894(00)80012-X. [DOI] [Google Scholar]
- Gordon, K. , Holm‐Denoma, J. , Smith, A. , Fink, E. , & Joiner, T. (2007). Taxometric analysis: Introduction and overview. International Journal of Eating Disorders, 40(S3), S35–S39. 10.1002/eat.20407. [DOI] [PubMed] [Google Scholar]
- Hartmann, A. , Zeeck, A. , & Barrett, M. S. (2009). Interpersonal problems in eating disorders. International Journal of Eating Disorders, 43, 619–627. [DOI] [PubMed] [Google Scholar]
- Herzog, D. B. , Dorer, D. J. , Keel, P. K. , Selwyn, S. E. , Ekeblad, E. R. , Flores, A. T. , … Keller, M. B. (1999). Recovery and relapse in anorexia and bulimia nervosa: A 7.5‐year follow‐up study. Journal of the American Academy of Child & Adolescent Psychiatry, 38(7), 829–837. 10.1097/00004583-199907000-00012. [DOI] [PubMed] [Google Scholar]
- Kim, S.‐K. (2010a). Evaluating the invariance of cognitive profile patterns derived from profile analysis via multidimensional scaling (PAMS): A bootstrapping approach. International Journal of Testing, 10(1), 33–46. 10.1080/15305050903454549. [DOI] [Google Scholar]
- Kim, S.‐K. (2010b). Comparing longitudinal profile patterns of mathematics and reading in early child longitudinal study, kindergarten (ECLS‐K): The profile analysis via multidimensional scaling (PAMS) approach. Asian Pacific Education Review, 11(2), 189–198. 10.1007/s12564-010-9074-4. [DOI] [Google Scholar]
- Kim, S.‐K. (2013). Identifying between‐person and within‐person factors to enhance understanding observed score profiles. British Journal of Mathematical and Statistical Psychology, 66, 435–451. 10.1111/j.2044-8317.2012.02055.x. [DOI] [PubMed] [Google Scholar]
- Kim, S.‐K. , Davison, M. L. , & Frisby, C. L. (2007). Confirmatory factor analysis and profile analysis via multidimensional scaling (PAMS). Multivariate Behavioral Research, 42(1), 1–32. 10.1080/00273170701328973. [DOI] [PubMed] [Google Scholar]
- Kim, S.‐K. , Frisby, C. L. , & Davison, M. L. (2004). Estimating cognitive profiles using profile analysis via multidimensional scaling (PAMS). Multivariate Behavioral Research, 39(4), 595–624. 10.1207/s15327906mbr3904_2. [DOI] [PubMed] [Google Scholar]
- Kim, S.‐K. , & Lord‐Bessen, J. (2012). Extracting longitudinal and cross‐sectional profile patterns from mathematics and reading in early child longitudinal study, kindergarten (ECLS‐K). Unpublished manuscript.
- Kruskal, J. B. (1964). Multidimensional scaling by optimizing goodness of fit to a nonmetric hypothesis. Psychometrika, 29(1), 1–27. 10.1007/BF02289565. [DOI] [Google Scholar]
- Lampard, A. M. , Tasca, G. A. , Balfour, L. , & Bissada, H. (2013). An evaluation of the transdiagnostic cognitive‐behavioural model of eating disorders. European Eating Disorders Review, 21(2), 99–107. 10.1002/erv.2214. [DOI] [PubMed] [Google Scholar]
- McKay, D. , Kim, S.‐K. , Taylor, S. , Abramowitz, J. S. , Tolin, D. F. , Coles, M. E. , … Olatunji, B. O. (2014). An examination of obsessive‐compulsive symptoms and dimensions using profile analysis via multidimensional scaling (PAMS). Journal of Anxiety Disorders, 28(4), 352–357. 10.1016/j.janxdis.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Meehl, P. E. , & Golden, R. R. (1982). Taxometric methods In Kendall P. C., & Butcher J. N. (Eds.), Handbook of research methods in clinical psychology (pp. 127–181). . New York: Wiley. [Google Scholar]
- Newman, M. M. , & Gold, M. S. (1992). Preliminary findings of patterns of substance abuse in eating disorder patients. American Journal of Drug and Alcohol Abuse, 18(2), 207–211. 10.3109/00952999208992833. [DOI] [PubMed] [Google Scholar]
- Olatunji, B. O. , Kim, S.‐K. , & Wall, D. (2015). Extracting body image symptom dimensions among eating disorder patients: The profile analysis via multidimensional scaling (PAMS) approach. Body Image, 15, 16–23. 10.1016/j.bodyim.2015.04.008. [DOI] [PubMed] [Google Scholar]
- Papadopoulos, F. C. , Ekbom, A. , Brandt, L. , & Ekselius, L. (2009). Excess mortality, causes of death and prognostic factors in anorexia nervosa. British Journal of Psychiatry, 194(1), 10–17. 10.1192/bjp.bp.108.054742. [DOI] [PubMed] [Google Scholar]
- Patrick, L. (2002). Eating disorders: A review of the literature with emphasis on medical complications and clinical nutrition. Alternative Medicine Review, 7(3), 184–202. [PubMed] [Google Scholar]
- Ricca, V. , Mannucci, E. , Zucchi, T. , Rotella, C. M. , & Faravelli, C. (2000). Cognitive‐behavioural therapy for bulimia nervosa and binge eating disorder. A review. Psychotherapy and Psychosomatics, 69(6), 287–295. 10.1159/000012410. [DOI] [PubMed] [Google Scholar]
- Stice, E. , Becker, C. B. , & Yokum, S. (2013). Eating disorder prevention: Current evidence‐base and future directions. International Journal of Eating Disorders, 46(5), 478–485. 10.1002/eat.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice, E. , Killen, J. D. , Hayward, C. , & Taylor, C. B. (1998). Support for the continuity hypothesis of bulimic pathology. Journal of Consulting and Clinical Psychology, 66(5), 784–790. 10.1037/0022-006X.66.5.784. [DOI] [PubMed] [Google Scholar]
- Sullivan, P. F. , Bulik, C. M. , Fear, J. L. , & Pickering, A. (1998). Outcome of anorexia nervosa: A case‐control study. American Journal of Psychiatry, 155(7), 939–946. 10.1176/ajp.155.7.939. [DOI] [PubMed] [Google Scholar]
- Thiel, A. , & Paul, T. (2006). Test–retest reliability of the eating disorder inventory 2. Journal of Psychosomatic Research, 61(4), 567–569. 10.1016/j.jpsychores.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Tylka, T. L. , & Subich, L. M. (2003). Revisiting the continuity‐discontinuity debate within eating disorders: Taxometric analysis using non‐behavioral indicators. Journal of Counseling Psychology, 50(3), 276–286. 10.1037/0022-0167.50.3.276. [DOI] [Google Scholar]
- Williamson, D. A. , Womble, L. G. , Smeets, M. A. M. , Netemeyer, R. G. , Thaw, J. M. , Kutlesic, V. , & Gleaves, D. H. (2002). The latent structure of eating disorder symptoms: A factor analytic and taxometric investigation. American Journal of Psychiatry, 159(3), 412–418. 10.1176/appi.ajp.159.3.412. [DOI] [PubMed] [Google Scholar]
- Yager, J. , Andersen, A. , Devlin, M. , Mitchell, J. , Powers, P. , & Yates, A. (1993). American Psychiatric Association practice guidelines for eating disorders. American Journal of Psychiatry, 150, 207–228. [Google Scholar]


