Abstract
Background
The relationship between morbid obesity and long-term patient outcomes after primary total hip arthroplasty (THA) has been understudied. The purpose of this study was to determine the association between morbid obesity and 10-year complications (revision surgery, reoperation, dislocation) and mortality in patients undergoing primary THA.
Methods
We conducted a population-based cohort study of patients aged 45–74 years who underwent primary THA for osteoarthritis between 2002 and 2007 using Ontario administrative health care databases. Patients were followed for 10 years. We estimated risk ratios (RRs) of mortality, reoperation, revision and dislocation in patients with body mass index (BMI) greater than 45 kg/m2 (morbidly obese patients) compared with patients with a BMI of 45 kg/m2 or less (nonmorbidly obese patients).
Results
There were 22 251 patients in the study cohort, of whom 726 (3.3%) were morbidly obese. Morbid obesity was associated with higher 10-year risk of death (RR 1.38, 95% confidence interval [CI] 1.18–1.62). Risks of revision (RR 1.43, 95% CI 0.96–2.13) and dislocation (RR 2.38, 95% CI 1.38–4.10) were higher in morbidly obese men than in nonmorbidly obese men; there were no associations between obesity and revision or dislocation in women. Risk of reoperation was higher in morbidly obese women than in nonmorbidly obese women (RR 1.59, 95% CI 1.05–2.40); there was no association between obesity and reoperation in men.
Conclusion
Morbidly obese patients undergoing primary THA are at higher risk of long-term mortality and complications. There were differences in complication risk by sex. The results of this study should inform perioperative counselling of patients considering THA.
Abstract
Contexte
Le lien entre l’obésité morbide et les issues à long terme des patients ayant subi une arthroplastie totale primaire de la hanche (ATH) est sous-étudié. Cette étude visait à caractériser l’association entre l’obésité morbide et les complications (chirurgie de révision, réintervention, dislocation) et la mortalité sur 10 ans chez les patients ayant subi une ATH.
Méthodes
Nous avons mené une étude de cohorte basée sur la population auprès de patients de 45 à 74 ans atteints d’arthrose ayant subi une ATH primaire entre 2002 et 2007 en utilisant les bases de données administratives en santé de l’Ontario. Les patients ont été suivis pour une période de 10 ans. Nous avons estimé des rapports de risque (RR) pour la mortalité, la réintervention, la chirurgie de révision et la dislocation chez les patients ayant un indice de masse corporelle (IMC) de plus de 45 kg/m2 (obésité morbide) en comparaison avec les patients ayant un IMC de 45 kg/m2 ou moins.
Résultats
L’étude de cohorte comptait 22 251 patients, dont 726 (3,3 %) étaient atteints d’obésité morbide. L’obésité morbide a été associée à un risque de mortalité sur 10 ans accru (RR 1,38; intervalle de confiance [IC] de 95 % 1,18–1,62). Le risque de chirurgie de révision (RR 1,43; IC de 95 % 0,96–2,13) et de dislocation (RR 2,38; IC de 95 % 1,38–4,10) était plus élevé chez les hommes atteints d’obésité morbide que chez les autres hommes; aucune association n’a été observée entre l’obésité et la chirurgie de révision ou la dislocation chez les femmes. Par contre, le risque de réintervention était accru chez les femmes atteintes d’obésité morbide (RR 1,59; IC de 95 % 1,05–2,40), mais aucune association n’a été établie entre l’obésité et la réintervention chez les hommes.
Conclusion
Les patients atteints d’obésité morbide qui subissent une ATH primaire courent un risque plus élevé de complications et de mortalité à long terme. Des différences ont été observées dans les risques de complications selon le sexe. Les résultats de cette étude devraient guider l’offre de conseils aux patients qui envisagent l’ATH.
Obesity is a worldwide epidemic that is associated with increased morbidity and mortality and a substantial burden to health care systems.1 Obesity is typically defined as a body mass index (BMI) of 30 kg/m2 or higher, but this simple definition can obscure the vast heterogeneity of patients within this group.2 As such, the World Health Organization (WHO) further categorizes 3 classes of obesity: patients in class I have a BMI between 30.0 and 34.9 kg/m2, patients in class II have a BMI between 35.0 and 39.9 kg/m2 and patients in class III have a BMI of 40.0 kg/m2 or higher. Patients with class III obesity are also classified as having clinically severe, or morbid, obesity, which is associated with more comorbidities and higher health care utilization.2 Interestingly, the groups with the highest BMIs are growing faster than any other weight group.2
Obesity is associated with several comorbidities, including osteoarthritis.1,3 Obese patients comprise an increasing portion of the population of patients who undergo total joint arthroplasty; morbidly obese patients are 8.5 times more likely to undergo total hip arthroplasty (THA) than people of normal weight.4–7 Obesity’s association with other comorbidities that increase perioperative risk following total joint arthroplasty is well-documented in the literature. Furthermore, morbid obesity has been linked to postoperative complications after THA, including superficial and deep infection, hip dislocation, aseptic loosening and early revision.8–32 However, few studies have looked at long-term outcomes, and to our knowledge no study to date has examined the association between morbid obesity and long-term survival after primary THA.32
The purpose of this population-based study was to determine the association between morbid obesity and 10-year mortality and postoperative complications, including revision surgery, reoperation for infection and dislocation, in patients undergoing primary THA. A secondary objective was to determine if there were sex-related differences in risk of complication and mortality in this population.
Methods
Study design
Provincial-level health care data were used for this population-based retrospective cohort study. With more than 14 million residents, Ontario is the most populous province in Canada. The Ontario Health Insurance Plan (OHIP) provides permanent residents with universal health care coverage.
ICES holds province-wide, individual-level health care data and has the capacity to link multiple databases. For this study, data sets containing diagnostic, procedural and physician billing information (Appendix 1, available at canjsurg.ca/017318-a1) were linked using unique encoded identifiers and analyzed at ICES. The study was approved by the University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board.
Study population
The study cohort included Ontario patients between the ages of 45 and 74 years who underwent primary THA for osteoarthritis between Apr. 1, 2002, and Mar. 31, 2007. Date of surgery was recorded as the index date. This accrual window allowed for 10 years of follow-up after primary THA. Patients who underwent bilateral THA (2 records of physician billing for primary THA on the same day) were excluded, because simultaneous bilateral THA is independently associated with increased mortality after surgery.33 Patients with a diagnosis of rheumatoid arthritis, osteomyelitis or septic arthritis in the year preceding joint replacement were also excluded, because the disease process and risk of complication may differ for these patients compared with patients with osteoarthritis. Patients who lost OHIP eligibility during the follow-up period were excluded. Lastly, for patients who underwent more than 1 primary THA during the study period, the date of the first arthroplasty was recorded as the index date.
Baseline characteristics
Patient age, sex and income quintile at the index date were obtained. Baseline comorbidity was measured using health care encounter data for the year before the index date and represented by the Johns Hopkins Aggregated Diagnosis Groups (ADG) Index.34 Having diagnoses in 3 or more ADGs over a specified period is considered a significant morbidity burden. The mean number of total ADGs and major ADGs was calculated for each obesity class. Neighbourhood income quintile compares the average income within a given postal code against all other postal codes in the census area or census metropolitan area; this measure was used as a surrogate for socioeconomic status. A higher percentile indicates that people living in that neighbourhood have a higher average income relative to people living in neighbourhoods with other postal codes in the area.
Morbid obesity was identified using premiums billed by either surgeons or anesthetists for procedures performed on patients with a BMI greater than 45 kg/m2. Patients without such a code were classified as having a BMI of 45 kg/m2 or less (nonmorbidly obese). This method has been used in related literature.35 In 2009 and 2010, the criteria for these premiums were altered to include patients with a BMI greater than 40 kg/m2 in accordance with the definition of morbid obesity; given that this change falls outside our accrual period, it would not cause exposure misclassification in our cohort. The available data do not include actual BMI values, and consequently we were not able to divide patients into more discrete categories.
Outcome measures
The outcomes of interest were 10-year all-cause death, revision surgery, reoperation for infection and hip dislocation. The specific physician billing codes we used are included in Appendix 1. Revision surgery was identified through OHIP physician billing codes for revision THA or implant removal. Revision procedures that occurred on the index date were included. Reoperation for infection was identified through physician billing codes for any of the following procedures: joint incision and drainage, joint synovectomy/débridement, soft tissue (muscle) excision, or replacement of acetabular liner and/or femoral head. To limit misclassification, only the latter procedure was allowed to occur on the same date as the index date; all other reoperations must have occurred after the index date. In practice, these reoperation codes are used primarily for management of superficial and/or deep joint infections. Our definition of reoperation for infection did not include revision THA, which was estimated separately. Hip dislocation was identified through physician billing codes for closed or open reduction of hip dislocation. Dislocation was allowed to occur on the same date as the index date.
Statistical analysis
We used χ2 tests and Student t tests to statistically assess differences in patient characteristics by morbid obesity for categorical and continues variables, respectively. Differences in time to death, revision THA, reoperation for infection and hip dislocation were examined using Kaplan–Meier survival curves. The log-rank test was used to test statistical significance. Modified Poisson regression models were used to calculate 10-year risks of death, hip dislocation, revision THA and reoperation for infection. Patients were included in the 10-year risk of death models if they retained OHIP eligibility coverage through 10 years of follow-up or if they died before 10 years of follow-up. Likewise, patients were included in the 10-year risk of revision models if they retained their OHIP eligibility coverage through 10 years of follow-up or if they had revision before 10 years of follow-up. A priori confounders of morbid obesity and THA outcomes included age, sex, socioeconomic status and comorbidities as measured by the Johns Hopkins ADGs.36 Modification of the risk ratios (RRs) by sex was examined. Statistical analyses were performed using SAS version 9.3.
Results
Baseline characteristics are described in Table 1. One hundred and ninety-seven patients were excluded because they lost OHIP eligibility during the follow-up period; the distribution of morbid obesity did not vary between patients who lost OHIP eligibility and patients included in the study. There were 22 251 patients in the study cohort, of whom 726 (3.3%) were morbidly obese. We linked multiple databases to follow the cohort over 10 years with minimal loss to follow-up. There was high coding consistency and agreement for both diagnostic and intervention codes, meaning high specificity in defining the cohort and low risk of outcome misclassification.37,38
Table 1.
Baseline (preoperative) characteristics of patients in Ontario who underwent primary total hip arthroplasty in 2002 to 2007 by BMI category
| Characteristic | No. (%) of patients | p value | ||
|---|---|---|---|---|
| BMI > 45 n = 726 |
BMI ≤ 45 n = 21 525 |
Total n = 22 251 |
||
| Sex | ||||
| Female | 464 (63.9) | 11 297 (52.5) | 11 761 (52.9) | < 0.001 |
| Male | 262 (36.1) | 10 228 (47.5) | 10 490 (47.1) | |
| Age, yr | ||||
| Mean ± SD | 60.62 ± 7.74 | 63.43 ± 7.87 | 63.34 ± 7.88 | < 0.001 |
| 45–54 | 174 (24.0) | 3491 (16.2) | 3665 (16.5) | < 0.001 |
| 55–64 | 303 (41.7) | 6926 (32.2) | 7229 (32.5) | |
| 65–74 | 249 (34.3) | 11 108 (51.6) | 11 357 (51.0) | |
| SES, percentile | ||||
| 0–20 | 146 (20.1) | 3318 (15.4) | 3464 (15.6) | 0.002 |
| 21–40 | 135 (18.6) | 3998 (18.6) | 4133 (18.6) | |
| 41–60 | 132 (18.2) | 4244 (19.7) | 4376 (19.7) | |
| 61–80 | 154 (21.2) | 4571 (21.2) | 4725 (21.2) | |
| 81–100 | 154 (21.2) | 5335 (24.8) | 5489 (24.7) | |
| Missing | < 6 | 59 (0.3) | 64 (0.3) | |
| Sum of all ADGs, mean ± SD | 6.36 ± 2.94 | 6.31 ± 2.81 | 6.31 ± 2.82 | 0.67 |
| Sum of major ADGs, mean ± SD | 1.23 ± 1.08 | 1.24 ± 1.13 | 1.24 ± 1.12 | 0.79 |
ADGs = Johns Hopkins Aggregated Diagnosis Groups; BMI = body mass index, measured in kg/m2; SD= standard deviation; SES = socioeconomic status.
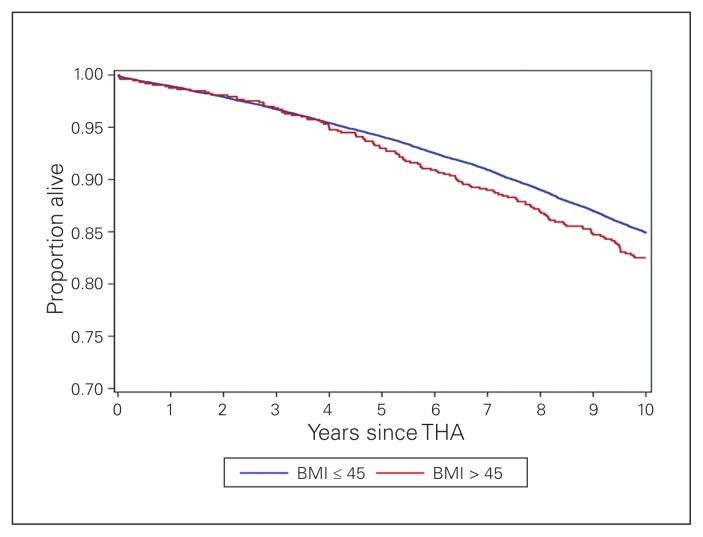
Ten-year mortality status
Kaplan–Meier curves demonstrated that morbidly obese patients had a slightly higher crude risk of death at 10 years that approached statistical significance (BMI > 45 kg/m2, 17.5%; BMI ≤ 45 kg/m2, 15.1%, p = 0.07, Fig. 1). In regression models, the 10-year unadjusted risk of death was higher in morbidly obese patients (RR 1.16, 95% confidence interval [CI] 0.99–1.36, Table 2). After we adjusted for age, sex, socioeconomic status and ADG, the 10-year risk of death following THA was 38% higher in patients classified as morbidly obese than in patients who were nonmorbidly obese (RR 1.38, 95% CI 1.18–1.62, Table 2). There was no modification of RR by sex (adjusted RR 1.37, 95% CI 1.07–1.75, for men; adjusted RR 1.39, 95% CI 1.14–1.70, for women) (Table 3).
Fig. 1.
Kaplan–Meier curves for length of time from index procedure to death by body mass index (BMI) category. THA = total hip arthroplasty.
Table 2.
Crude and adjusted 10-year risk ratios of death, revision, reoperation, dislocation and all-cause reoperation in morbidly obese compared with nonmorbidly obese patients in Ontario who underwent primary total hip arthroplasty
| Outcome | No. (%) of patients | Unadjusted RR (95% CI) | Adjusted* RR (95% CI) | ||
|---|---|---|---|---|---|
| BMI > 45 kg/m2 | BMI ≤ 45 kg/m2 | Total | |||
| Death | 127 (3.8) | 3250 (96.2%) | 3377 (15.2) | 1.16 (0.99–1.36) | 1.38 (1.18–1.62) |
| No death | 599 (3.2) | 18 275 (96.8%) | 18 874 (84.8) | ||
| Revision THA | 58 (4.1) | 1354 (95.9%) | 1412 (6.3) | 1.27 (0.99–1.63) | 1.21 (0.94–1.56) |
| No revision THA | 688 (3.2) | 20 171 (96.8%) | 20 839 (93.7) | ||
| Reoperation† | 31 (4.5) | 661 (95.5%) | 692 (3.1) | 1.39 (0.98–1.98) | 1.37 (0.96–1.94) |
| No reoperation | 695 (3.2) | 20 864 (96.8%) | 21 559 (96.9) | ||
| Dislocation | 32 (5.4) | 561 (94.6%) | 593 (2.7) | 1.69 (1.19–2.40) | 1.65 (1.16–2.34) |
| No dislocation | 694 (3.2) | 20 964 (96.8%) | 21 658 (97.3) | ||
BMI = body mass index; CI = confidence interval; RR = risk ratio; THA = total hip arthroplasty.
Adjusted for age, sex, socioeconomic status, and Johns Hopkins Aggregated Diagnosis Groups.
Includes the following surgical procedures: joint incision and drainage, joint synovectomy/débridement, soft tissue (muscle) excision, or replacement of acetabular liner and/or femoral head.
Table 3.
Effect modification of associations between morbid obesity and death, revision, reoperation, dislocation and all-cause reoperation by sex
| Comparison | Adjusted* RR (95% CI); sex | |
|---|---|---|
| Women | Men | |
| Death in morbidly obese v. nonmorbidly obese patients | 1.39 (1.14–1.70) | 1.37 (1.07–1.75) |
| Revision THA in morbidly obese v. nonmorbidly patients | 1.10 (0.79–1.53) | 1.43 (0.96–2.13) |
| Reoperation† in morbidly obese v. nonmorbidly patients | 1.59 (1.05–2.40) | 0.98 (0.49–1.95) |
| Dislocation in morbidly obese v. nonmorbidly patients | 1.36 (0.87–2.13) | 2.38 (1.38–4.10) |
CI = confidence interval; RR = risk ratio; THA = total hip arthroplasty.
Adjusted for age, sex, socioeconomic status and Johns Hopkins Aggregated Diagnosis Groups.
Includes the following surgical procedures: joint incision and drainage, joint synovectomy/débridement, soft tissue (muscle) excision, or replacement of acetabular liner and/or femoral head.
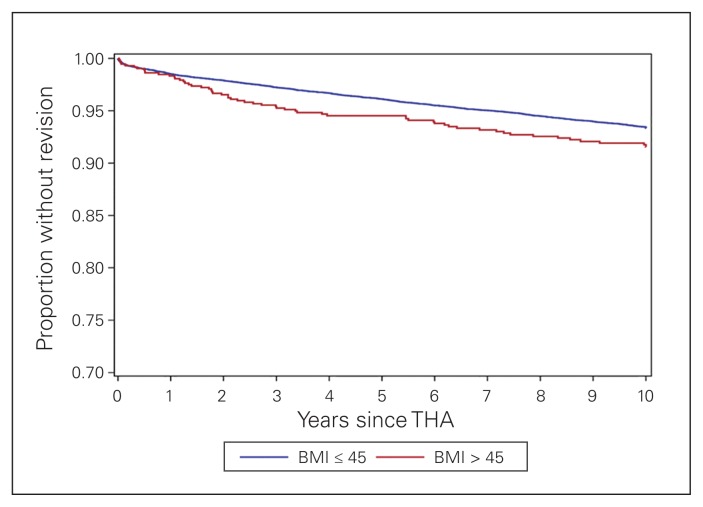
Ten-year revision rate
Kaplan–Meier curves demonstrated that morbidly obese patients had a higher crude risk of revision that approached statistical significance (BMI > 45 kg/m2, 8.0%; BMI ≤ 45 kg/m2, 6.3%, p = 0.05, Fig. 2). The 10-year unadjusted RR of revision surgery was 1.27 (95% CI 0.99–1.63) in morbidly obese patients compared with nonmorbidly obese patients (Table 2). Adjustment for potential confounders did not affect the estimate (RR 1.21, 95% CI 0.94–1.57, Table 2). The risk of revision surgery in morbidly obese patients varied by sex (adjusted RR 1.43, 95% CI 0.96–2.13 for men; adjusted RR 1.10, 95% CI 0.79–1.53 for women) (Table 3).
Fig. 2.
Kaplan–Meier curves for length of time from index procedure to revision total hip arthroplasty by body mass index (BMI) category. THA = total hip arthroplasty.
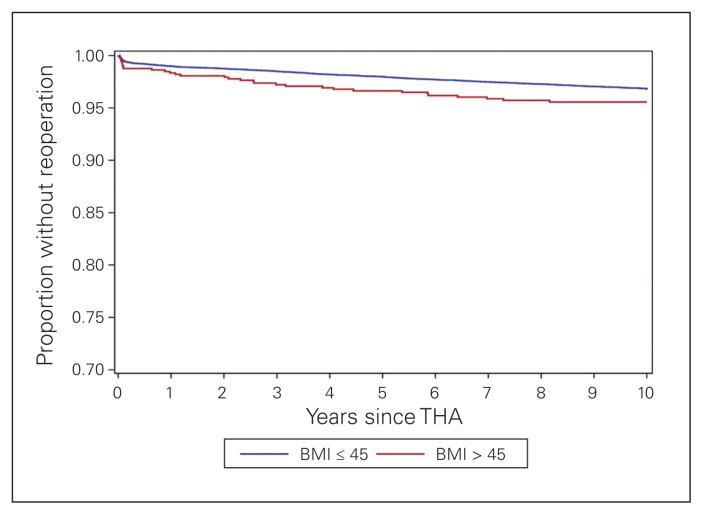
Ten-year risk of reoperation for infection
Kaplan–Meier curves demonstrated that morbidly obese patients had a higher crude risk of reoperation for infection that approached statistical significance (BMI > 45 kg/m2, 4.3%; BMI ≤ 45 kg/m2, 3.1%, p = 0.06, Fig. 3). In the regression models, the 10-year unadjusted RR of reoperation for infection was 1.39 (95% CI 0.98–1.98) in morbidly obese patients compared with nonmorbidly obese patients (Table 2). The association was unchanged after adjustment for potential confounders (RR 1.37, 95% CI 0.96–1.94, Table 2). The risk of reoperation for infection was 60% higher in morbidly obese women than in nonmorbidly obese women (adjusted RR 1.60, 95% CI 1.05–2.40, Table 3); for men, there was no increased risk associated with obesity (adjusted RR 0.98, 95% CI 0.49–1.95, Table 3).
Fig. 3.
Kaplan–Meier curves for length of time from index procedure to reoperation for infection by body mass index (BMI) category. THA = total hip arthroplasty.
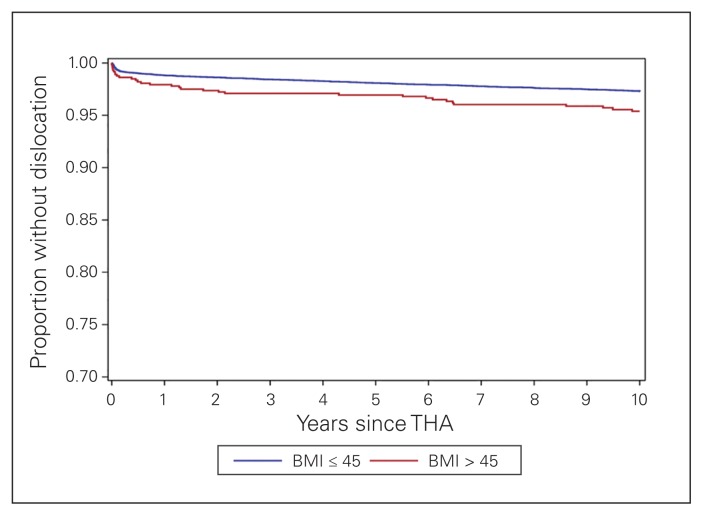
Ten-year dislocation risk
Kaplan–Meier curves demonstrated that morbidly obese patients had a higher crude risk of hip dislocation (BMI > 45 kg/m2, 4.4%, BMI ≤ 45 kg/m2, 2.6%, p = 0.003, Fig. 4). In the regression models, the 10-year unadjusted RR of dislocation was 1.69 (95% CI 1.19–2.40) in morbidly obese patients compared with nonmorbidly obese patients (Table 2). The association was unchanged after adjustment for potential confounders (RR 1.65, 95% CI 1.16–2.34, Table 2). There was evidence of moderate modification of the risk of dislocation by sex (adjusted RR 2.38, 95% CI 1.38–4.10, for men; adjusted RR 1.36, 95% CI 0.87–2.13, for women) (Table 3).
Fig. 4.
Kaplan–Meier curves for length of time from index procedure to hip dislocation by body mass index (BMI) category. THA = total hip arthroplasty.
Discussion
To our knowledge, this is the first large population-based cohort study to examine the effect of morbid obesity on long-term survival and outcomes following THA. Our use of a BMI cut-off of greater than 45 kg/m2 to categorize patients as morbidly obese probably attenuated effect estimates. Patients with BMI less than or equal to 45 kg/m2 include those who are classified as non-obese (BMI < 30 kg/m2) and obese (BMI between 30 and 40 kg/m2) and some who are classified as morbidly obese (BMI between 40 and 45 kg/m2) according to WHO definitions. Patients from the latter 2 BMI categories would have been included in our nonmorbidly obese group, along with patients of normal weight; this would probably have increased the risk of adverse outcomes in the nonmorbidly obese group, thus attenuating associations between obesity and the outcomes of interest. Unfortunately, further refinement of exposure categories is not possible with our existing data sources. Laterality (right- or left-sided THA) cannot be established with the available diagnostic and procedure codes. In patients who underwent primary THA on both hips, either during or before the study period, we were unable to specify if the revision or reoperation code was related to their index procedure (first THA) or the contralateral THA. As in a related study using similar methodology to assess the effect of morbid obesity on total knee arthroplasty, we do not expect this coding limitation to have a significant impact on our results.35 All patients were followed for up to 10 years from the date of their first THA.
Morbidly obese patients were 38% more likely than nonmorbidly obese patients to die within 10 years, after adjusting for baseline differences in age, sex, socioeconomic status and comorbidity. To our knowledge, our study is the first to report long-term survival differences in morbidly obese and nonmorbidly obese patients undergoing THA. We are aware of only 1 other study that compared mortality by obesity in patients undergoing THA. In 2015, Ward and colleagues found that patients who were morbidly obese were over twice as likely to die in the year following total joint arthroplasty (THA or total knee arthroplasty) as nonmorbidly obese patients.39 A large meta-analysis with a combined sample size of over 2.88 million patients estimated an all-cause mortality hazard ratio of 1.29 for class II and III obesity, relative to normal weight.40 Thus, the increased risk of death observed in our study may be explained, at least in part, by the increased risk of mortality from obesity irrespective of THA. It would be valuable to compare the long-term mortality risk in morbidly obese patients who undergo primary THA with that of morbidly obese patients who do not undergo arthroplasty. This research question warrants future investigation.
We showed an obesity effect for revision surgery after primary THA, with further evidence suggesting that this risk is higher in morbidly obese men than in morbidly obese women. These findings are in keeping with a number of studies.8,12–14,16,22,29,41 Interestingly, Goodnough and colleagues showed higher odds of revision surgery for obese and morbidly obese patients in the first 5 years following primary THA, but lower odds after 10 years.8 They attributed the increased early risk to aseptic loosening, which has been shown in several other studies as well.8,13,22,27 For example, Electricwala and colleagues found that the risk of early revision THA increased by 4.7 times in obese patients because of aseptic loosening.13 A few studies showed no statistically significant difference in revision risk by obesity. 26,28,32 These studies, however, still showed a trend toward an obesity effect. A lower BMI cut-off for obesity and lack of study power because of small sample sizes probably explains the nonsignificant results.26,28,32
We demonstrated an obesity effect for risk of nonrevision reoperation following primary THA, with some indication that this risk was higher in morbidly obese women. This measure is our surrogate for infections requiring operative management, but given the billing codes used it could potentially include ball/liner exchanges for early instability or polyethylene wear. However, these probably represent a small proportion of the patients in this group. These results are in keeping with existing literature showing an increased risk of superficial and deep joint infection associated with obesity.8,14,16,17,19,21,24–27,30,31,39,42,43 Lübbeke and colleagues also commented on effect modification by sex.41 Although their method for measuring infection was markedly different than ours (chart review and ongoing surveillance), they also described increased an risk of infection only in obese women, compared with non-obese women, following primary THA. They suggested differences in body fat distribution and metabolic response as possible explanations for the higher risk of infection in morbidly obese women following THA.
We showed an obesity effect for risk of dislocation following primary THA, with a 65% increased risk of dislocation in morbidly obese patients. In addition, risk of dislocation was higher for morbidly obese men than for morbidly obese women. These results are consistent with results from the literature, which show an increased risk of dislocation in obese, morbidly obese and superobese (defined as BMI > 50 kg/m2) patients undergoing primary THA.12,15,21,26,41 For example, Davis and colleagues found a 114% increase in risk of dislocation for every additional 10 BMI units.26 To our knowledge, our study is the first to examine effect modification by sex in risk of dislocation in morbidly obese patients. The increased dislocation risk may be associated with difficult surgical exposure because of body habitus, which can compromise implant positioning. Furthermore, in their biomechanical analysis, Elkins and colleagues described other obesity-related conditions, such as thigh soft tissue impingement, that compromise stability of THA.44
Morbidly obese patients undergo THA on average 3 years earlier than nonmorbidly obese patients. Similar demographic differences have been reported in the literature. 5,7,10,15,22,31,42,45 In our study and in others, women comprise a larger proportion of the population of morbidly obese patients undergoing THA than of the population of non-morbidly obese patients undergoing this procedure.10,22,28,42
Conclusion
We described long-term trends related to morbid obesity in patients undergoing primary THA. Morbid obesity was associated with a 38% increase in 10-year mortality in patients undergoing primary THA. It was also associated with a 43% increased risk of revision surgery and a 138% increased risk of dislocation in men, but there was no increased risk of these outcomes in women. Finally, morbid obesity was associated with a 60% increased risk of reoperation for infection in women, but there was no association between obesity and reoperation in men. The effect of sex on risk of complication has been described by few studies thus far and requires further investigation. The results of this population-based study have important implications for this growing patient population and can be used to counsel morbidly obese patients about risks following THA.
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the authors and not necessarily those of CIHI. Funding for this project was provided by the Department of Surgery, Queen’s University.
Footnotes
Competing interests: None declared.
Contributors: M. Tohidi, S. Brogly, M. Harrison, A. Campbell and S. Mann designed the study. K. Lajkosz acquired and analyzed the data, which M. Tohidi, S. Brogly, E. VanDerKerkhof and S. Mann also analyzed. M. Tohidi wrote the article, which all authors reviewed and approved for publication. All authors agreed to be accountable for all aspects of the work.
References
- 1.Smith KB, Smith MS. Obesity statistics. Prim Care. 2016;43:121–35. doi: 10.1016/j.pop.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121:492–6. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sturmer T, Gunther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol. 2000;53:307–13. doi: 10.1016/s0895-4356(99)00162-6. [DOI] [PubMed] [Google Scholar]
- 4.Workgroup of the American Association of Hip and Knee Surgeons Evidence Based Committee. Obesity and total joint arthroplasty: a literature based review. J Arthroplasty. 2013;28:714–21. doi: 10.1016/j.arth.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Bourne R, Mukhi S, Zhu N, et al. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007;465:185–8. doi: 10.1097/BLO.0b013e3181576035. [DOI] [PubMed] [Google Scholar]
- 6.Singh JA, Lewallen DG. Increasing obesity and comorbidity in patients undergoing primary total hip arthroplasty in the U.S.: a 13-year study of time trends. BMC Musculoskelet Disord. 2014;15:441. doi: 10.1186/1471-2474-15-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vasarhelyi EM, MacDonald SJ. The influence of obesity on total joint arthroplasty. J Bone Joint Surg Br. 2012;94:100–2. doi: 10.1302/0301-620X.94B11.30619. [DOI] [PubMed] [Google Scholar]
- 8.Goodnough LH, Finlay AK, Huddleston JI, et al. Obesity is independently associated with early aseptic loosening in primary total hip arthroplasty. J Arthroplasty. 2018;33:882–6. doi: 10.1016/j.arth.2017.09.069. [DOI] [PubMed] [Google Scholar]
- 9.Zusmanovich M, Kester BS, Schwarzkopf R. Postoperative complications of total joint arthroplasty in obese patients stratified by BMI. J Arthroplasty. 2017;33:856–64. doi: 10.1016/j.arth.2017.09.067. [DOI] [PubMed] [Google Scholar]
- 10.Deakin AH, Iyayi-Igbinovia A, Love GJ. A comparison of outcomes in morbidly obese, obese and non-obese patients undergoing primary total knee and total hip arthroplasty. Surgeon. 2018;16:40–5. doi: 10.1016/j.surge.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Hanna SA, McCalden RW, Somerville L, et al. Morbid obesity is a significant risk of failure following revision total hip arthroplasty. J Arthroplasty. 2017;32:3098–101. doi: 10.1016/j.arth.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Werner BC, Higgins MD, Pehlivan HC, et al. Super obesity is an independent risk factor for complications after primary total hip arthroplasty. J Arthroplasty. 2017;32:402–6. doi: 10.1016/j.arth.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Electricwala AJ, Narkbunnam R, Huddleston JI, 3rd, et al. Obesity is associated with early total hip revision for aseptic loosening. J Arthroplasty. 2016;31:217–20. doi: 10.1016/j.arth.2016.02.073. [DOI] [PubMed] [Google Scholar]
- 14.George J, Piuzzi NS, Ng M, et al. Association between body mass index and thirty-day complications after total knee arthroplasty. J Arthroplasty. 2018;33:865–71. doi: 10.1016/j.arth.2017.09.038. [DOI] [PubMed] [Google Scholar]
- 15.Haynes J, Nam D, Barrack RL. Obesity in total hip arthroplasty: Does it make a difference? Bone Joint J. 2017;99-B:31–6. doi: 10.1302/0301-620X.99B1.BJJ-2016-0346.R1. [DOI] [PubMed] [Google Scholar]
- 16.Issa K, Harwin SF, Malkani AL, et al. Bariatric orthopaedics: total hip arthroplasty in super-obese patients (those with a BMI of >=50 kg/m2) J Bone Joint Surg Am. 2016;98:180–5. doi: 10.2106/JBJS.O.00474. [DOI] [PubMed] [Google Scholar]
- 17.Lübbeke A, Zingg M, Vu D, et al. Body mass and weight thresholds for increased prosthetic joint infection rates after primary total joint arthroplasty. Acta Orthop. 2016;87:132–8. doi: 10.3109/17453674.2015.1126157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adhikary SD, Liu W-M, Memtsoudis SG, et al. Body mass index more than 45 kg/m(2) as a cutoff point is associated with dramatically increased postoperative complications in total knee arthroplasty and total hip arthroplasty. J Arthroplasty. 2016;31:749–53. doi: 10.1016/j.arth.2015.10.042. [DOI] [PubMed] [Google Scholar]
- 19.Ma Z, Guo F, Qi J, et al. Meta-analysis shows that obesity may be a significant risk factor for prosthetic joint infections. Int Orthop. 2016;40:659–67. doi: 10.1007/s00264-015-2914-4. [DOI] [PubMed] [Google Scholar]
- 20.Ward DT, Metz LN, Horst PK, et al. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015;30:42–6. doi: 10.1016/j.arth.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 21.Liu W, Wahafu T, Cheng M, et al. The influence of obesity on primary total hip arthroplasty outcomes: a meta-analysis of prospective cohort studies. OrthopTraumatol Surg Res. 2015;101:289–96. doi: 10.1016/j.otsr.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Murgatroyd SE, Frampton CMA, Wright MS. The effect of body mass index on outcome in total hip arthroplasty: early analysis from the New Zealand Joint Registry. J Arthroplasty. 2014;29:1884–8. doi: 10.1016/j.arth.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 23.Wallace G, Judge A, Prieto-Alhambra D, et al. The effect of body mass index on the risk of post-operative complications during the 6 months following total hip replacement or total knee replacement surgery. Osteoarthritis Cartilage. 2014;22:918–27. doi: 10.1016/j.joca.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Friedman RJ, Hess S, Berkowitz SD, et al. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin Orthop Relat Res. 2013;471:3358–66. doi: 10.1007/s11999-013-3049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamsen E, Nevalainen P, Eskelinen A, et al. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94:e101. doi: 10.2106/JBJS.J.01935. [DOI] [PubMed] [Google Scholar]
- 26.Davis AM, Wood AM, Keenan ACM, et al. Does body mass index affect clinical outcome post-operatively and at five years after primary unilateral total hip replacement performed for osteoarthritis? A multivariate analysis of prospective data. J Bone Joint Surg Br. 2011;93:1178–82. doi: 10.1302/0301-620X.93B9.26873. [DOI] [PubMed] [Google Scholar]
- 27.Haverkamp D, Klinkenbijl MN, Somford MP, et al. Obesity in total hip arthroplasty — does it really matter? A meta-analysis. Acta Orthop. 2011;82:417–22. doi: 10.3109/17453674.2011.588859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCalden RW, Charron KD, MacDonald SJ, et al. Does morbid obesity affect the outcome of total hip replacement?: an analysis of 3290 THRs. J Bone Joint Surg Br. 2011;93:321–5. doi: 10.1302/0301-620X.93B3.25876. [DOI] [PubMed] [Google Scholar]
- 29.Chee YH, Teoh KH, Sabnis BM, et al. Total hip replacement in morbidly obese patients with osteoarthritis: results of a prospectively matched study. J Bone Joint Surg Br. 2010;92:1066–71. doi: 10.1302/0301-620X.92B8.22764. [DOI] [PubMed] [Google Scholar]
- 30.Malinzak RA, Ritter MA, Berend ME, et al. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24:84–8. doi: 10.1016/j.arth.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 31.Andrew JG, Palan J, Kurup HV, et al. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90:424–9. doi: 10.1302/0301-620X.90B4.20522. [DOI] [PubMed] [Google Scholar]
- 32.McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg Br. 2006;88:1286–92. doi: 10.1302/0301-620X.88B10.17660. [DOI] [PubMed] [Google Scholar]
- 33.Otte KS, Husted H, Ørsnes T, et al. Bilateral simultaneous total hip arthroplasty in a fast track setting. Hip. 2018;21:336–9. doi: 10.5301/HIP.2011.8393. [DOI] [PubMed] [Google Scholar]
- 34.Weiner JP, Abrams C. The Johns Hopkins ACG® System, technical reference guide, version 10.0. Baltimore (MD): Johns Hopkins University; 2011. Dec, [Google Scholar]
- 35.Tohidi M, Brogly SB, Lajkosz K, et al. Ten-year mortality and revision after total knee arthroplasty in morbidly obese patients. J Arthroplasty. 2018;33:2518–23. doi: 10.1016/j.arth.2018.03.049. [DOI] [PubMed] [Google Scholar]
- 36.Austin PC, van Walraven C, Wodchis WP, et al. Using the Johns Hopkins Aggregated Diagnosis Groups (ADGs) to Predict mortality in a general adult population cohort in Ontario, Canada. Med Care. 2011;49:932–9. doi: 10.1097/MLR.0b013e318215d5e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Juurlink D, Preya C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: a validation study. Toronto: ICES; 2006. [Google Scholar]
- 38.Canadian Institute for Health Information. CIHI data quality study of the 2009–2010 Discharge Abstract Database. Ottawa: Canadian Institute for Health Information; 2012. [Google Scholar]
- 39.Ward DT, Metz LN, Horst PK, et al. Complications of Morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015;30:42–6. doi: 10.1016/j.arth.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 40.Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lübbeke A, Stern R, Garavaglia G, et al. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–34. doi: 10.1002/art.22542. [DOI] [PubMed] [Google Scholar]
- 42.Namba RS, Paxton L, Fithian DC, et al. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 43.Wallace G, Judge A, Prieto-Alhambra D, et al. The effect of body mass index on the risk of post-operative complications during the 6 months following total hip replacement or total knee replacement surgery. Osteoarthritis Cartilage. 2014;22:918–27. doi: 10.1016/j.joca.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 44.Elkins JM, Daniel M, Pedersen DR, et al. Morbid obesity may increase dislocation in total hip patients: a biomechanical analysis. Clin Orthop Relat Res. 2013;471:971–80. doi: 10.1007/s11999-012-2512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guenther D, Schmidl S, Klatte TO, et al. Overweight and obesity in hip and knee arthroplasty: evaluation of 6078 cases. World J Orthop. 2015;6:137–9. doi: 10.5312/wjo.v6.i1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]