Abstract
The economic growth has paralleled the rise of diabetes and its complications in multiethnic population of United Arab Emirates (UAE). Previous studies have shown that characteristics of diabetes is variable across different ethnicities. The objective of this study was to compare diabetes prevalence and risk factors between UAE nationals and different expatriate’s ethnic groups in UAE using data from UAE National Diabetes and Lifestyle Study (UAEDIAB). The UAE nationals made one-fourth (n = 797, 25%) of total cohort and the remaining 75% belonged to immigrants. Across different ethnicities, adjusted prevalence of prediabetes ranged from 8% to 17%, while adjusted prevalence of newly diagnosed diabetes ranged from 3% to 13%. UAE nationals, Arabs non-nationals and Asians had the highest number of pre-diabetic as well as newly diagnosed diabetic patients. Adjusted prevalence of diabetes was highest in UAE nationals (male 21% and female 23%) as well as Asian non-Arabs (male 23% and female 20%), where 40% of both groups fell under the range of either prediabetes or diabetes conditions. Multivariate factors of diabetes versus non-diabetes included older age, ethnicities of Asian non-Arabs and local UAE nationals, family history of diabetes, obesity, snoring, decreased level of high density lipoprotein, elevated levels of triglycerides and blood pressure. In conclusion, diabetes prevalence and risk factors vary across the different ethnic groups in UAE, and hence interventions towards identification and prevention of diabetes should not treat all patients alike.
Subject terms: Metabolic disorders, Epidemiology, Risk factors
Introduction
The burden of diabetes is rising globally, most markedly in developing countries that are undergoing industrialization and have shifted to more sedentary lifestyle, poorer eating habits as well as less physical activity. The global number of adults with diabetes increased from 108 million in 1980 to 422 million in 20141. According to International Diabetes Federation (IDF), currently 425 million people have diabetes in the world and more than 39 million people in the Middle East and North Africa region (MENA) Region2. United Arab Emirates, one of the 19 countries of the IDF MENA region, has experienced rapid economic growth and infrastructure expansion, following the discovery of oil3. This economic burst parallels the rise of diabetes and its complications in UAE with diabetes numbers reaching over 1,185,500 cases in 20172.
The UAE population is made up around 20% local UAE nationals and the reminder non-UAE immigrants from different Arabs and non-Arabs (Asians and Westerners) ethnic backgrounds4,5. Previous studies have shown that prevalence as well as risk factors of diabetes is variable across different ethnicities6,7. Although a number of previous studies have attempted to describe diabetes in UAE8–10, these studies mainly focused on UAE nationals and few have included non-nationals in to perspective11. The UAE National Diabetes and Lifestyle Study (UAEDIAB) study was conducted in two phases; the first phase was conducted among immigrants non-UAE population and the second phase was conducted among population of UAE nationals12,13. For purpose of this study we merged the data from phase one and two.
The objective of this study was to compare the prevalence and risk factors of diabetes between UAE nationals and different expatriate’s ethnicities living across United Arab Emirates using data from the UAEDIAB.
Methods
Study design, population and settings
The UAEDIAB was a cross-sectional study conducted to investigate the prevalence and risk factors of diabetes among UAE nationals and expatriates who have been living in Sharjah, Dubai, and Northern Emirates for at least four years. The UAE multi-ethnic expatriate population were surveyed in the first phase, and the UAE Emiratis were surveyed in the second phase. Ethical approval for this study was obtained from both University of Sharjah ethics committee on 23 June 2010, and UAE Ministry of Health on 14 March 2012, and all research in this study was performed in accordance with relevant guidelines and regulations. Before the interview, every participant read a detailed information sheet and signed an informed consent form to give information as well as blood samples12.
The details of study design and sampling of the UAEDIAB investigation are described elsewhere12,14. In the first phase, the target population was all non-UAE national adults aged 18 years and older residing in UAE applying for their second or subsequent visa renewal (i.e. resident for at least 4 years). The second phase of the study involving UAE nationals had a similar inclusion criteria’s but did consider the number of years of stay in the country. People with serious physical disabilities, learning disorders, severe communication barriers, and pregnant women were excluded from both phase one and two.
During a face-to-face interview, a designed questionnaire was used to collect sociodemographic data on gender, nationality (based on country of origin), date of birth, marital status, residence, family history of diabetes in first degree relatives and lifestyle habits. After completion of the interview, measurements of weight, height, waist and hip circumference and systolic and diastolic blood pressure were obtained and a fasting blood sample was collected to test levels for plasma glucose, HbA1c and lipids12.
Variable definitions
Diabetes status was determined using measurements of FBG, HbA1c and participants self-report information. Following the WHO criteria for both of FBG and HbA1c, FBG < 6.1 mmol/l was considered normal, 6.1to 6.9 mmol/l was impaired fasting glucose (IFG), and ≥7.0 mmol/l indicated diabetes. Whereas, HbA1c, <6.5% was considered non-diabetic, and ≥6.5% diagnostic of indicated diabetes. Diabetes disease was classified into newly diagnosed diabetes mellitus (NDM) and known diabetes mellitus (KDM). Prevalence of total diabetes mellitus included both newly diagnosed and known cases of diabetes. KDM15 was assigned to those subjects who had previously been informed of having diabetes via a health professional and were either using diabetic medications or had a HbA1c ≥ 6.5% or FPG ≥ 7.0 mmol/l. Whereby participants who had FPG or HbA1c levels within the diabetes range and who had never been informed by a health professional that they had diabetes were classified as NDM following cuts off values provided by American Diabetes Association. For waist circumference different cut offs were used for Asians and the other ethnicities. For the waist circumference (WC) ethnic-specific cut offs were used where the high WC was defined as ≥90 cm in men and ≥80 cm in women from Asian ethnicity while the high WC for the rest of ethnic groups was defined as ≥102 cm in men and ≥88 cm in women. Body mass index (BMI) was obtained by dividing a participant’s weight in kilograms by the squared height in meters. To assess snoring and sleep apnoea, participants were asked whether they snore loudly or if anyone had observed them stop breathing during sleep. Hypertension was described either by a systolic blood pressure of >140 and or a diastolic blood pressure of >90. Triglycerides of >1.7 mmol/L was considered abnormal, while total cholesterol level >5.0 mmol/L was considered high. HDL < 1.0 mmol/l for males and <1.3 mmol/l for females was considered low, while LDL was categorized into three groups: <2.59, 2.59–3.34 and ≥3.34 mmol/l12.
Statistical analysis
In this study, using the direct standardization method, the age standardised prevalence of prediabetes and diabetes (known and newly diagnosed diabetes) was calculated for UAE nationals as well as each of non-UAE national immigrant ethnic group using the world mid-year population of 201316. Counts and percentages were used to present categorical variables, whereas normally distributed continuous data were presented as mean ± standard deviation (SD) and median and interquartile range (IQR) if their distribution was skewed.
In the univariate analysis, continuous data were analysed by Student t-test while the categorical data was compared using χ2test. Independent factors of DM were identified through development of a logistic regression model using enter method, which was adjusted for age, gender, and any other variables that in univariate analysis were significant at P < 0.05.The Statistical Package for Social Sciences (SPSS) version 24 (IBM Corp, New York) were used to carry out all the analysis.
Results
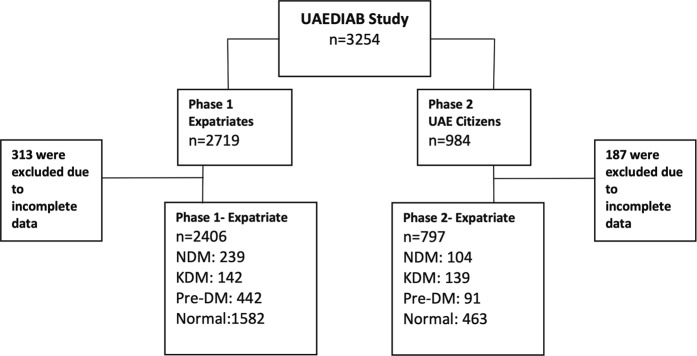
The UAEDIAB study, which consisted of two phases, has screened over 3000 patients from two populations of national Emirati and expatriate living in different cities of UAE for risk of diabetes (Fig. 1).
Figure 1.
Flow chart of subject selection from UAE National Diabetes and Lifestyle Study. UAE, United Arab Emirates; UAEDIAB, UAE National Diabetes and Lifestyle Study.
After exclusion of cases with incomplete data, 313 from phase one and 187 from phase two, the total subject included were 2406 (75%) cases from phase one and 797 (25%) cases from phase two.
The age standardised prevalence of prediabetes and diabetes (known and newly diagnosed diabetes) was calculated for UAE nationals as well as each of non-UAE national immigrant ethnic group (Fig. 2). Among UAE nationals, 42% (n = 334) were assessed to have either prediabetes or diabetes. The adjusted percentage of local female with diabetes was 23% out of which 11.5% were newly diagnosed cases while percentage of local males 21% out of which 9% were newly diagnosed cases.
Figure 2.
Age standardised prevalence of prediabetes and diabetes (known and new cases) across different ethnicities of local UAE nationals and immigrant non-UAE. UAE, United Arab Emirates.
The UAE nationals made the one-fourth (n = 797, 25%) of UAEDIAB total cohort and the remaining 75% (n = 2406) belonged to immigrants. The population of UAE expatriates was made up of the following four distinct ethnic groups: Arab non-nationals (n = 640, 20%), Asians non-Arabs (n = 1683, 52%), Westerners (n = 56, 2%) and Africans (n = 27, 1%). The total standardized prevalence of diabetes among immigrants was highest among Asians (male 23% and female 20%) followed by Arabs non-nationals (male 17% and female 18%). The fraction of population affected by either prediabetes or diabetes among Asians was nearby 40%, which was similar to UAE nationals. However, among Arab non-nationals and other ethnic minorities there was lower rate of prediabetes or diabetes.
In this study, we first compared characteristics of UAE national diabetics with diabetics from non-national ethnicities of Arabs non-nationals, Asians, African and westerners. Compared to UAE nationals, Arab non-nationals had higher numbers of males (54% versus 68%; P = 0.022), more active status (23% versus 63%; P < 0.001), higher total cholesterol (40% versus 66%; P < 0.001) but less snoring (95% versus 39%; P < 0.001). The next major immigrant ethnic group was the Asian non-Arabs, and compared to UAE nationals, Asians were on average 7 years younger: 51 ± 14 years vs 44 ± 11 years (P < 0.001), they were predominantly male (54% versus 87%; P < 0.001), reported lower family history for diabetes (64% versus 39%; P < 0.001), had lower BMI but larger waist circumference (63% versus 74%; P = 0.007), had higher levels of total cholesterol (40% versus 50%; P = 0.033) but lower levels of HDL (54% versus 43%; P = 0.014). The comparison for minor ethnic groups of Westerners and Africans are not reported here but they are displayed in the Table 1.
Table 1.
Comparison of socio-demographic and clinical characteristics of diabetes between UAE national patients and immigrant ethnic groups of Arab non-nationals, Asian non-Arabs, Westerners and African.
| Variable | DM Arab non-national n = 99 | DM UAE locals n = 243 | P value | DM Asians n = 272 | DM UAE locals n = 243 | P value | DM Westerners n = 5 | DM UAE locals n = 243 | P value | DM Africans n = 5 | DM UAE locals n = 243 | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) mean ± SD | 49 ± 10 | 51 ± 14 | 0.184 | 44 ± 11 | 51 ± 14 | <0.001 | 39 ± 16 | 51 ± 14 | 0.057 | 38 ± 13 | 51 ± 14 | 0.035 |
| Male, n (%) | 67 (68) | 131 (54) | 0.022 | 237 (87) | 131 (54) | <0.001 | 2 (40) | 131 (54) | 0.665 | 3 (60) | 131 (54) | 0.787 |
| Female, n (%) | 32 (32) | 112 (46) | 0.022 | 35 (13) | 112 (46) | <0.001 | 3 (60) | 112 (46) | 0.665 | 2 (40) | 112 (46) | 0.787 |
| Family history of diabetes, n (%) | 55 (56) | 155 (64) | 0.178 | 91 (33) | 155 (64) | <0.001 | 0 | 155 (64) | 0.007 | 3 (60) | 155 (64) | 0.862 |
| Activity, n (%) | 62 (63) | 55 (23) | <0.001 | 136 (50) | 55 (23) | <0.001 | 2 (40) | 55 (23) | 0.324 | 3 (60) | 55 (23) | 0.085 |
| Snoring, n (%) | 39 (39) | 231 (95) | <0.001 | 78 (29) | 231 (95) | <0.001 | 2 (40) | 231 (95) | 0.002 | 0 | 231 (95) | <0.001 |
| BMI (kg/m2), n (%) | 0.485 | <0.001 | 0.977 | 0.367 | ||||||||
| Normal | 13 (13) | 43 (18) | 87 (32) | 43 (18) | 1 (20) | 43 (18) | 2 (40) | 43 (18) | ||||
| Overweight | 31 (31) | 80 (33) | 117 (43) | 80 (33) | 2 (40) | 80 (33) | 0 | 80 (33) | ||||
| Obese | 55 (56) | 118 (49) | 66 (24) | 118 (49) | 2 (40) | 118 (49) | 3 (60) | 118 (49) | ||||
| Waist circumference high, n (%) | 64 (65) | 152 (63) | 0.892 | 200 (74) | 152 (63) | 0.007 | 2 (40) | 152 (63) | 0.359 | 4 (80) | 152 (63) | 0.657 |
| HDL, n (%) | 0.074 | 0.014 | 0.801 | 0.664 | ||||||||
| <1 for males & < 1.3 for females | 56 (57) | 111 (46) | 154 (57) | 111 (46) | 2 (40) | 111 (46) | 3 (60) | 111 (46) | ||||
| ≥1 for males & ≥1.3 for females | 43 (43) | 132 (54) | 118 (43) | 132 (54) | 3 (60) | 132 (54) | 2 (40) | 132 (54) | ||||
| Triglycerides, n (%) | 0.121 | 0.791 | 0.801 | 0.801 | ||||||||
| <1.7 | 44 (44) | 132 (54) | 144 (53) | 132 (54) | 3 (60) | 132 (54) | 3 (60) | 132 (54) | ||||
| ≥1.7 | 55 (56) | 111 (46) | 128 (47) | 111 (46) | 2 (40) | 111 (46) | 2 (40) | 111 (46) | ||||
| High cholesterol | 65 (66) | 98 (40) | <0.001 | 136 (50) | 98 (40) | 0.033 | 4 (80) | 98 (40) | 0.162 | 3 (60) | 98 (40) | 0.400 |
| Hypertension | 31 (31) | 97(40) | 0.142 | 126 (46) | 99 (41) | 0.213 | 1 (20) | 99 (41) | 0.651 | 2 (40) | 99 (41) | 0.073 |
| Systolic blood pressure, mean ± SD | 127 ± 18 | 130 ± 21 | 0.154 | 134 ± 22 | 130 ± 21 | 0.025 | 113 ± 12 | 130 ± 21 | 0.070 | 125 ± 17 | 130 ± 21 | 0.605 |
| Diastolic blood pressure, mean ± SD | 84 ± 10 | 83 ± 12 | 0.701 | 87 ± 13 | 83 ± 12 | 0.003 | 78 ± 12 | 83 ± 12 | 0.258 | 82 ± 13 | 83 ± 12 | 0.744 |
After comparing UAE national diabetics versus diabetics from other ethnicities, we carried a univariate analysis to compare diabetic and non-diabetic subjects within each ethnicity (Table 2). From this univariate analysis, age and gender variables together with any other variables that in univariate analysis were significant at P < 0.05 were selected for multivariate regression analysis: ethnicity, family history of diabetes, physical activity, snoring, obesity, triglyceride levels, high density lipoprotein levels, cholesterol levels, systolic and diastolic blood pressure.
Table 2.
Univariate factors of diabetes versus non-diabetes across different ethnicities of UAE national patients and immigrant ethnic groups of Arab non-nationals, Asian non-Arabs, Westerners and African.
| Variable | Arab non-national | Asian | Westerners | Africans | UAE nationals | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DM n = 99 | No DM n = 541 | P value | DM n = 272 | No DM n = 1411 | P value | DM n = 5 | No DM n = 51 | P value | DM n = 5 | No DM n = 22 | P value | DM n = 243 | No DM n = 554 | P value | |
| Age (years) mean ± SD | 49 ± 10 | 37 ± 11 | <0.001 | 44 ± 11 | 36 ± 9 | <0.001 | 39 ± 16 | 42 ± 13 | 0.649 | 38 ± 13 | 35 ± 9 | 0.546 | 51 ± 14 | 39 ± 12 | <0.001 |
| Male, n (%) | 67 (68) | 392 (72) | 0.331 | 237 (87) | 1201 (85) | 0.338 | 2 (40) | 32 (63) | 0.320 | 3 (60) | 13 (59) | 0.970 | 131 (54) | 288 (52) | 0.617 |
| Female, n (%) | 32 (32) | 149 (28) | 0.331 | 35 (13) | 210 (15) | 0.338 | 3 (60) | 19 (37) | 0.320 | 2 (40) | 9 (41) | 0.970 | 112 (46) | 266 (48) | 0.617 |
| First-degree family history of diabetes, n (%) | 55 (56) | 203 (38) | 0.001 | 91 (33) | 241(17) | <0.001 | 0 | 12 (24) | 0.221 | 3 (60) | 5 (23) | 0.099 | 155 (64) | 319 (58) | 0.100 |
| Activity, n (%) | 62 (63) | 317 (59) | 0.453 | 136 (50) | 578 (41) | 0.006 | 2 (40) | 29 (57) | 0.469 | 3 (60) | 9 (41) | 0.438 | 55 (23) | 172 (31) | 0.015 |
| Snoring, n (%) | 39 (39) | 134 (25) | 0.003 | 78 (29) | 173 (12) | <0.001 | 2 (40) | 11 (22) | 0.352 | 0 | 1 (5) | 0.627 | 231 (95) | 541 (98) | 0.053 |
| BMI (kg/m2), n (%) | 0.003 | <0.001 | 0.380 | 0.155 | <0.001 | ||||||||||
| Normal | 13 (13) | 117 (22) | 87 (32) | 629 (45) | 1 (20) | 19 (37) | 2 (40) | 9 (41) | 43 (18) | 158 (29) | |||||
| Overweight | 31 (31) | 219 (40) | 117 (43) | 596 (42) | 2 (40) | 24 (47) | 0 | 8 (36) | 80 (33) | 212 (38) | |||||
| Obese | 55 (56) | 204 (38) | 66 (24) | 182 (13) | 2 (40) | 8 (16) | 3 (60) | 5 (23) | 118 (49) | 182 (33) | |||||
| Waist circumference high, n (%) | 64 (65) | 237 (44) | <0.001 | 200 (74) | 849 (60) | <0.001 | 2 (40) | 12 (24) | 0.417 | 3 (60) | 9 (41) | 0.548 | 152 (63) | 253 (46) | <0.001 |
| High cholesterol | 65 (66) | 281 (52) | 0.012 | 136 (50) | 711 (50) | 0.906 | 4 (80) | 24 (47) | 0.160 | 3 (60) | 8 (36) | 0.332 | 98 (40) | 246 (44) | 0.285 |
| HDL, n (%) | 0.106 | 0.014 | 0.079 | 0.726 | <0.001 | ||||||||||
| <1 for males & <1.3 for females | 43 (43) | 189 (35) | 118 (43) | 501 (36) | 3 (60) | 12 (24) | 2 (40) | 7 (32) | 132 (54) | 206 (37) | |||||
| ≥1 for males & ≥1.3 for females | 56 (57) | 352 (65) | 154 (57) | 910 (64) | 2 (40) | 39 (76) | 3 (60) | 15 (68) | 111 (46) | 348 (63) ** | |||||
| Triglycerides, n (%) | <0.001 | <0.001 | 0.352 | 0.171 | <0.001 | ||||||||||
| <1.7 | 44 (44) | 362 (67) | 144 (53) | 912 (65) | 3 (60) | 40 (78) | 3 (60) | 19 (86) | 132 (54) | 432 (78) | |||||
| ≥1.7 | 55 (56) | 179 (33) | 128 (47) | 499 (35) | 2 (40) | 11 (22) | 2 (40) | 3 (14) | 111 (46) | 122 (22) | |||||
| Hypertension | 31 (31) | 110 (20) | 0.017 | 126 (46) | 477 (34) | <0.001 | 1 (20) | 14 (27) | 0.720 | 2 (40) | 5 (23) | 0.426 | 99 (41) | 103 (19) | <0.001 |
| Systolic blood pressure, mean ± SD | 127 ± 18 | 120 ± 16 | <0.001 | 134 ± 22 | 127 ± 17 | <0.001 | 113 ± 12 | 121 ± 21 | 0.463 | 125 ± 17 | 123 ± 18 | 0.751 | 130 ± 21 | 123 ± 55 | <0.001 |
| Diastolic blood pressure, mean ± SD | 84 ± 10 | 80 ± 11 | <0.001 | 87 ± 13 | 84 ± 12 | <0.001 | 78 ± 12 | 81 ± 16 | 0.660 | 82 ± 13 | 79 ± 11 | 0.676 | 83 ± 12 | 84 ± 68 | <0.001 |
BMI, body mass index; DM, diabetes mellitus; HDL, high density lipoprotein; SD, standard deviation; UAE, United Arab Emirates.
In multivariate analysis, older age was associated with increased odd ratio (OR) of diabetes with odds increasing from 2.70 (95% confidence interval [CI] 1.96–3.72) for 41–50 years age group to 6.08 (95% CI 4.28–8.64) for 51–60 years age group, and reaching OR of 8.26 (95% CI 5.32–12.82) for age group of 60 years and older. Table 3 shows the adjusted values for logistic regression analysis.
Table 3.
Multivariate factors of diabetes versus non-diabetes.
| Adjusted OR (95% CI) | P Value | |
|---|---|---|
| Male | 0.86 (0.67–1.12) | 0.864 |
| Age | ||
| 18–30 | Reference | Reference |
| 31–40 | 1.01 (0.73–1.40) | 0.951 |
| 41–50 | 2.70 (1.96–3.72) | <0.001 |
| 51–60 | 6.08 (4.28–8.64) | <0.001 |
| 60+ | 8.26 (5.32–12.82) | <0.001 |
| Ethnicity | ||
| Arab non-national | Reference | Reference |
| Asian | 1.62 (1.21–2.17) | 0.001 |
| African and westerner | 1.02 (0.48–2.17) | 0.952 |
| Arab national | 1.57 (1.10–2.22) | 0.012 |
| Family history of diabetes | 1.84 (1.48–2.27) | <0.001 |
| Physical activity | 1.09 (0. 89–1.34) | 0.403 |
| Snoring | 1.40 (1.07–1.84) | 0.015 |
| Obese | 1.60 (1.28–1.99) | <0.001 |
| High cholesterol | 0.86 (0.70–1.05) | 0.145 |
| Triglycerides (mmol/L) | 1.25 (1.15–1.35) | <0.001 |
| HDL (mmol/L) | 0.64 (0.45–0.91) | 0.013 |
| Systolic blood pressure, per increase of 10 mmHg | 1.02 (1.01–1.02) | 0.004 |
| Diastolic blood pressure, per increase of 10 mmHg | 0.99 (0.98–0.99) | 0.012 |
CI, confidence interval; HDL, high density lipoprotein; OR, odds ratio.
When comparing the OR for diabetes across the local and immigrant ethnicities, Asian non-Arabs (OR 1.62; 95% CI 1.21–2.17) and local UAE nationals (OR 1.57; 95% CI 1.10–2.22) were more likely associated with diabetes condition. In addition, family history of diabetes (OR 1.84; 95% CI 1.48–2.27), snoring (OR 1.40; 95% CI 1.07–1.84), obesity (OR 1.60; 95% CI 1.28–1.99), elevated levels of triglycerides (OR 1.25; 95% CI 1.15–1.35) as well as elevated systolic blood pressure (OR 1.02; 95% CI 1.01–1.02) was associated with increased odds of diabetes. In contrast, increased high density lipoprotein (OR 0.64; 95% CI 0.45–0.91) decreased the odds for diabetes whereas increased diastolic blood pressure (OR 0.99; 95% CI 0.98–0.99) appeared to decrease odds for diabetes but the value was close to non-significant.
Discussion
The finding of the current study displays the heterogeneity presents among prevalence and characteristics for patients with diabetes coming from different ethnic backgrounds.
In this study the variation in age standardised prevalence of prediabetes and diabetes was shown across different ethnicities of local UAE nationals and immigrant non-nationals. The UAE’s immigrant population was mainly made up of Arab non-national and Asian non-Arabs with ethnic groups of westerners and Africans as minorities. Prediabetes ranged from around 8% to 17%, while the prevalence of newly diagnosed diabetes ranged from around 3% to 13%. UAE nationals, Arabs non-nationals and Asians had the highest number of prediabetes as well as newly diagnosed diabetes. Age standardised prevalence of diabetes was highest in national UAE locals as well as Asian non-Arabs, where 40% of both groups fell under the range of either prediabetes or diabetes conditions. Likewise, the total age standardised prevalence of diabetes was highest among Asians (male 23% and female 20%) and UAE locals (male 21% and female 23%). This prevalence was higher than the UAE diabetes prevalence of 17.3% that was reported in 2017 via IDF for the whole UAE population regardless of ethnicities. Moreover, compared to other Gulf countries, the prevalence in this study was higher than 18.3% prevalence reported by Bahijri et al. from Saudi Arabia17, the 18.8% prevalence reported by Alkandari et al. from Kuwait18, and diabetes prevalence from Oman that ranged from 10.5% to 17.7%19.
Another ethnic group with high diabetes prevalence was the Asians which was consistent to high prevalence reported via previous investigations20. Compared to UAE national’s diabetics, Asians tended to have lower BMI but larger waist circumferences which could result in more visceral fat, more insulin resistance and consequently more diabetes. This finding could also explain high prevalence of diabetes among Asians despite their lower BMI, which is keeping with literature that have reported lower BMI and more visceral fat in Asians with diabetes compared to western population21.
In the logistic regression analysis, diabetes was again associated mainly with two ethnicities of Arab national and Asian non-Arab. Other multivariate factors of diabetes were consistent with previous literature and included older age22, family history of diabetes23,24, obesity25,26, snoring27 higher TG and finally raised blood pressure28.
According to IDF the UAE diabetes prevalence is growing faster than the rest of MENA regions and expected to double in number by 20402. It is recommended that health authorities in MENA regions to continue funding the research about ethnic specific diabetes characteristics and to increase the diabetes knowledge among healthcare and public sectors. The major driving factors of fast increase in diabetes prevalence among UAE local and immigrant ethnicities are the increased obesity, shift to sedentary lifestyle, decrease in physical activity and unhealthy diet29–31. There is an urgent need for increasing the knowledge and awareness of public as well as health care sector about diabetes, its risk factors and complications. The public should be encouraged to shift to healthier lifestyle, eat healthy diet that is low in sugar but high in fiber, and increase in physical and sport activities. It is important to understand that how diabetes prevalence and risk factors could vary across the different ethnic groups in UAE. Therefore, the interventions towards identification and prevention of diabetes development as well as progression should not treat all ethnicities alike. The data from this study can be used in conjunction with genetics to characterize genetic factors that might lead to prevalence to diabetes in various ethnic populations.
In summary, the prevalence and risk factors of diabetes vary across different ethnic groups in UAE. Local UAE nationals and Asians non-Arab ethnic groups have the highest prevalence of diabetes; more than one-third of these ethnic groups have either prediabetes or diabetes. Asians with diabetes have lower BMI but higher waist circumference. In addition, compared to local UAE nationals, non-nationals immigrants with diabetes tend to be younger, predominantly male and more active.
Acknowledgements
The authors are enormously grateful for the support and financial assistance provided by Ministry of Health UAE, Sharjah University, Baker IDI Heart and Diabetes Institute, and Sanofi (Dr. Hisham Mahmoud [Medical Director, Sanofi Middle East] and Dr. Mohammed Ismail [Medical Director, Sanofi Gulf Countries]). The authors also appreciate the great efforts of the members of The Diabetes Steering Committee (Professsor Hossam Hamdy and Dr. Khalid Al Jabri) for facilitating and contributing to the study. Gratitude to Dr. Shomous Nugud for her role in arranging all edits of the manuscript and reviewing the required changes. Special thanks go to Dr. Ashwini Shendge, Dr. Majd Abdel Rahim and Ms Lina Al Zarouni for their role as research assistants. This investigator-initiated study was under the auspices of the University of Sharjah and was partially supported by Sanofi and Baker IDI Heart and Diabetes Institute (Melbourne, Australia). Sanofi had no role in study design, data collection, data analysis, or writing of the manuscript. JES is supported by an Australian National Health and Medical Research Council fellowship. N.S. is funded by Al-Jalila Foundation (Grant Code: AJF150326), Diabetes and Metabolic Syndrome Research Group (University of Sharjah code 150306), National Diabetes and Lifestyle Survey (MOH Code 120301). R.H. is funded by the Sharjah Research Academy (Grant code: MED001), University of Sharjah (Grant code: 1901090254) and Al-Jalila Foundation (Grant code: AJF201741).
Author contributions
All authors have contributed to the study and to the preparation of the manuscript. Study design and data collection: N.S.S., N.S. and R.H.; Data Analysis: N.S.S., F.S.S., J.T., H.A. and R.H. Wrote the paper: F.S.S., N.S.S. and R.H.; Analyzed and revised the paper, S.A., N.S., R.H.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Rifat Hamoudi and Narjes Saheb Sharif-Askari.
References
- 1.NCD Risk Factor Collaboration Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diabetes Atlas. International Diabetes Federation. IDF Diabetes Atlas, 8th edn. Brussels, Belgium: International Diabetes Federation, 2017. Available at, http://www.diabetesatlas.org (Accessed: 23rd October 2018).
- 3.Hajat C, Harrison O, Shather Z. A profile and approach to chronic disease in Abu Dhabi. Global. Health. 2012;8:18. doi: 10.1186/1744-8603-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Government of Dubai. Dubai Statistics Center; 2017. Available at, https://www.dsc.gov.ae/Report/DSC_SYB_2017_01%20_%2003.pdf (Accessed: 9th October 2018).
- 5.Government of Abu Dhabi. Statistics Center of Abu Dhabi (SCAD); 2017. Available at, https://www.scad.gov.abudhabi/en/pages/GeneralPublications.aspx?pubid=79&themeid=7 (Accessed: 9th October 2018).
- 6.Oldroyd J, Banerjee M, Heald A, Cruickshank K. Diabetes and ethnic minorities. Postgrad Med J. 2005;81:486–90. doi: 10.1136/pgmj.2004.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi SE, Liu M, Palaniappan LP, Wang EJ, Wong ND. Gender and ethnic differences in the prevalence of type 2 diabetes among Asian subgroups in California. J. Diabetes Complications. 2013;27:429–435. doi: 10.1016/j.jdiacomp.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bani-Issa W. Evaluation of the health-related quality of life of Emirati people with diabetes: integration of sociodemographic and disease-related variables. East Mediterr Health J. 2011;17:825–830. doi: 10.26719/2011.17.11.825. [DOI] [PubMed] [Google Scholar]
- 9.Sreedharan J, et al. Incidence of Type 2 Diabetes Mellitus among Emirati Residents in Ajman, United Arab Emirates. Korean J Fam Med. 2015;36:253–257. doi: 10.4082/kjfm.2015.36.5.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saadi H, et al. Prevalence of diabetes mellitus and its complications in a population-based sample in Al Ain, United Arab Emirates. Diabetes Res Clin Pract. 2007;78:369–377. doi: 10.1016/j.diabres.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Malik M, Bakir A, Saab BA, King H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes Res Clin Pract. 2005;69:188–195. doi: 10.1016/j.diabres.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Sulaiman N, et al. High prevalence of diabetes among migrants in the United Arab Emirates using a cross-sectional survey. Sci. Rep. 2018;8:6862. doi: 10.1038/s41598-018-24312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sulaiman N, et al. Diabetes risk score in the United Arab Emirates: a screening tool for the early detection of type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2018;6:e000489. doi: 10.1136/bmjdrc-2017-000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sulaiman N, et al. Novel approach to systematic random sampling in population surveys: Lessons from the United Arab Emirates National Diabetes Study (UAEDIAB) J. Diabetes. 2015;7:642–648. doi: 10.1111/1753-0407.12270. [DOI] [PubMed] [Google Scholar]
- 15.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Census Bureau IDB. World Midyear Population by Age and Sex for 2013. U.S. Census Bureau, International Data Base; 2013. Available at, https://www.census.gov/programs-surveys/international-programs.html (Accessed: 22rd October 2018).
- 17.Bahijri SM, Jambi HA, Al Raddadi RM, Ferns G, Tuomilehto J. The Prevalence of Diabetes and Prediabetes in the Adult Population of Jeddah, Saudi Arabia- A Community-Based Survey. PLoS One. 2016;11:e0152559. doi: 10.1371/journal.pone.0152559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alkandari A, et al. The prevalence of pre-diabetes and diabetes in the Kuwaiti adult population in 2014. Diabetes Res Clin Pract. 2018;144:213–223. doi: 10.1016/j.diabres.2018.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Al-Moosa S, Allin S, Jemiai N, Al-Lawati J, Mossialos E. Diabetes and urbanization in the Omani population: an analysis of national survey data. Popul Health Metr. 2006;4:5. doi: 10.1186/1478-7954-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanaya AM, et al. Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes care. 2014;37:1621–1628. doi: 10.2337/dc13-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong AP, et al. Diabetes and its comorbidities–where East meets West. Nat. Rev. Endocrinol. 2013;9:537–547. doi: 10.1038/nrendo.2013.102. [DOI] [PubMed] [Google Scholar]
- 22.Chang AM, Halter JB. Aging and insulin secretion. Am. J. Physiol. Endocrinol. Metab. 2003;284:E7–12. doi: 10.1152/ajpendo.00366.2002. [DOI] [PubMed] [Google Scholar]
- 23.Groop L, et al. Metabolic consequences of a family history of NIDDM (the Botnia study): evidence for sex-specific parental effects. Diabetes. 1996;45:1585–1593. doi: 10.2337/diab.45.11.1585. [DOI] [PubMed] [Google Scholar]
- 24.Meigs JB, Cupples LA, Wilson PW. Parental transmission of type 2 diabetes: the Framingham Offspring Study. Diabetes. 2000;49:2201–2207. doi: 10.2337/diabetes.49.12.2201. [DOI] [PubMed] [Google Scholar]
- 25.Bray GA. Obesity increases risk for diabetes. Int. J. Obes. Relat. Metab. Disord. 16. 1992;Suppl 4:S13–17. [PubMed] [Google Scholar]
- 26.Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17:961–969. doi: 10.2337/diacare.17.9.961. [DOI] [PubMed] [Google Scholar]
- 27.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol. 2002;155:387–393. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt MI, et al. Identifying Individuals at High Risk for Diabetes. Diabetes care. 2005;28:2013. doi: 10.2337/diacare.28.8.2013. [DOI] [PubMed] [Google Scholar]
- 29.Sulaiman N, et al. Prevalence of overweight and obesity in United Arab Emirates Expatriates: the UAE National Diabetes and Lifestyle Study. Diabetology & Metabolic Syndrome. 2017;9:88. doi: 10.1186/s13098-017-0287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ng SW, et al. Nutrition transition in the United Arab Emirates. European Journal Of Clinical Nutrition. 2011;65:1328. doi: 10.1038/ejcn.2011.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wasfi AS, El-Sherbiny AA, Gurashi E, Al Sayegh FU. Sport practice among private secondary-school students in Dubai in 2004. East Mediterr Health J. 2008;14:704–714. [PubMed] [Google Scholar]