Abstract
Background:
Cardiac biomarkers soluble ST-2 (sST-2) and N-terminal prohormone B-type natriuretic peptide (NT-proBNP) may be associated with long-term survival after cardiac surgery. We explored the relationship between long-term survival after cardiac surgery and serum biomarker levels.
Methods:
Patients undergoing cardiac surgery from 2004-2007 were enrolled in a prospective biomarker cohort in the Northern New England Cardiovascular Disease Study Group Registry. Preoperative, postoperative, and the change in serum biomarker levels were categorized by quartile. We used Kaplan-Meier survival analysis and Cox regression models adjusted for variables in the STS’s ASCERT long-term survival calculator to study the association of biomarker levels with long-term survival. Following Kaplan-Meier analysis, quartiles 2 and 3 were found to have similar survival and were therefore combined into one category.
Results:
In our cohort (n=1,648), median follow-up time was 8.5 years (IQR: 7.6-9.7), during which there were 227 deaths. The 10-year survival rate was 86%. Kaplan-Meier survival analysis demonstrated a significant (p<0.001) difference across quartiles of each biomarker levels measurement. After adjustment, pre-operative, post-operative, and the change in biomarker levels in quartile 4 (highest serum levels/change) were significantly predictive of worse survival (hazard ratio range 1.77- 2.89, all p<0.05) compared to quartile 1; however, levels of sST-2 and NT-proBNP in quartiles 2-3 demonstrated a non-statistically significant trend with long-term survival.
Conclusions:
Elevated pre- and post-operative levels of sST-2 or NT-proBNP and large changes in these biomarkers’ levels are associated with increased risk of worse survival after cardiac surgery. These biomarkers can be used for risk stratification or assessing postsurgical prognosis.
Keywords: Biomarkers, Cardiac Surgery, Outcomes Research
Introduction
Biomarkers have demonstrated their value in disease detection, surveillance of clinical conditions, and prediction of response to an intervention.1-6 Yet, we have not fully explored their utility in cardiovascular care and outcomes. Despite declining mortality rates, heart disease remains the leading cause of death in the United States.7 Biomarker measurement presents a potential avenue through which we can track patient health and predict postsurgical outcomes to ultimately reduce heart disease-related mortality.
Soluble ST-2 (sST2) and N-terminal prohormone of B-type natriuretic peptide (NT-proBNP) are two promising contenders in this field. A member of the interleukin 1 receptor family, sST-2 is released from cardiomyocytes in response to mechanical strain and is involved in cardiac remodeling and fibrosis.8-12 NT-proBNP is a natriuretic peptide secreted in response to myocardial wall stress and increased cardiac workload.13-15 As such, increasing levels of serum sST-2 or NT-proBNP are associated with worse outcomes and disease severity in patients with acute myocardial infarction and chronic heart failure.8, 10-12, 14-16 The prognostic value of sST-2 and NT-proBNP in other cardiovascular conditions and their complementary properties make them suitable for study in patients undergoing cardiac surgery.
In this study, our objective was to evaluate the association of sST-2 and NT-proBNP serum levels with long-term mortality after cardiac surgery. Using data from a prospectively collected biomarker cohort, we studied preoperative, postoperative, and change in serum biomarker levels to explore their relationship to patient survival after discharge from a coronary artery bypass grafting (CABG) and/or valve replacement. Understanding the predictive ability of biomarkers measured at different stages in the surgical intervention process makes room for ways to identify and intervene for high-risk patients, thus reducing cardiovascular disease-related mortality.
Patients and Methods
Settings and Participants
The NNECDSG is a regional voluntary consortium founded in 1987 with a mission to improve outcomes for patients undergoing a cardiac procedure in Maine, New Hampshire and Vermont. Members include voluntary multi-disciplinary groups of clinicians, hospital administrators and health care research personnel from Eastern Maine Medical Center, Bangor, ME; Maine Medical Center, Portland, ME; Catholic Medical Center, Manchester, NH (affiliate Parkland Medical Center, Derry, NH), Dartmouth-Hitchcock Medical Center, Lebanon, NH; Concord Hospital, Concord, NH; and University of Vermont Medical Center, Burlington, VT.17, 18 An additional Maine and New Hampshire site are also included as they were members at the time of the study: Central Maine Medical Center, Lewiston, ME and Portsmouth Regional Hospital, Portsmouth, NH. The NNECDSG maintains a prospective registry of patient demographics, clinical characteristics, and in-hospital outcomes for cardiac surgical procedures including CABG and valve replacement.
We prospectively enrolled patients undergoing a CABG and/or valve replacement procedure from 2004-2007 in the New England Cardiovascular Disease Study Group (NNECDSG) for our biomarker study, as described in previous studies.19-22 Patients (n=1,690) had 10 mL blood samples collected preoperatively (before skin incision) and postoperatively (approximately 24 hours post-procedure). After collection, blood samples were allowed to clot and separate at room temperature for 20 minutes. Samples were then centrifuged at 3500 rpm for a further 20 mins before storage at −80°C. After freezing, sera samples were transported to the Laboratory for Clinical and Biomedical Research in Colchester, Vermont and stored at −80°C until biomarker serum level measurement by Meso Scale Discovery multiplex assay (Rockville, MD). Patients enrolled in the Biomarker study were linked to the National Death Index to determine all-cause mortality through 2015. All patients provided signed informed consent for blood collection and biomarker measurement
Forming the Analytic Cohort
For our study, we excluded patients who died prior to discharge (n=42), were missing biomarker measurements (n=122 missing preoperative, n=374 missing postoperative) or underwent a valve replacement procedure (n=5). Our final cohort includes 1,643 patients with follow-up data, for which we were able to study the effect of biomarkers levels during three time frames: preoperative (n=1,526), postoperative (n=1,256) and the change in serum levels between the preoperative and postoperative period (n=1,152). The institutional review board at each hospital approve the collection of NNECDSG data. The Committee for the Protection of Human Subjects at Dartmouth College approved this study.
Measures
The primary outcome was long-term survival after cardiac surgery, as measured by time from index discharge to death or last date known alive. Our primary exposures were preoperative, postoperative, and change in serum sST-2 and NT-proBNP biomarker levels. Change in biomarker levels was defined as the difference between preoperative and postoperative measurements. Each exposure was categorized by quartile. Following Kaplan-Meier analysis, quartiles 2 and 3 were found to have similar survival and were therefore combined into one category.
Statistical Methods
All baseline characteristics were compared using chi-squared test for categorical variables or Student’s t-test for continuous variables. The threshold for significance was a two-tailed p-value < 0.05. We also present absolute standardized differences (d) between patients that died and survived, which is a measure of the effect size (difference in means or proportions divided by the standard deviation). Based on the literature, we considered d > 0.1 as an threshold for imbalance, or significant difference, between the groups23. We used Kaplan-Meier survival analysis and Cox regression models to study the association of biomarker levels with long-term survival. As there were no deaths beyond seven years, we truncated our Kaplan-Meier survival graphs at this point. We adjusted for variables in the American College of Cardiology Foundation-Society of Thoracic Surgeons (STS) Collaboration on the Comparative Effectiveness of Revascularization Strategy (ASCERT) Long-Term Survival Probability Calculator24, 25 including age, weight, height, creatinine, ejection fraction, mean aortic gradient, sex, ethnicity, diabetes, cerebrovascular disease, cigarette smoking, congestive heart failure class, prior cardiac operation, cardiac status, number of diseased coronary vessels, myocardial infarction, and valve insufficiency. All statistical analyses were performed using Stata 15.1 (College Station, TX).
Results
Study Population
In our cohort (n=1,648), median follow-up time was 8 years (IQR: 7.5-9.7), during which there were 227 deaths. The majority of the cohort were men (78%) age 65 ± 10.1 years. Serum sST-2 and NT-proBNP levels showed substantial variability in the preoperative, postoperative, and change in levels. Mean values and cut-offs used for defining biomarker quartiles are listed in Table 1.
Table 1.
Cut-offs used for preoperative, postoperative, and change in sST-2 and NT-proBNP levels quartile categorization.
| Time Measured | Statistic | sST-2 Serum Level (in ng/mL) |
NT-proBNP Serum Level (in ng/mL) |
|---|---|---|---|
| Preoperative | Mean (SD) | 5.9 (8.5) | 7.5 (21.5) |
| Quartile 1 | < 3.2 | < 1.0 | |
| Quartile 2-3 | 3.2–5.7 | 1.0–5.6 | |
| Quartile 4 | > 5.7 | > 5.6 | |
| Postoperative | Mean (SD) | 63.8 (56.2) | 21.9 (29.4) |
| Quartile 1 | < 28.0 | < 7.9 | |
| Quartile 2-3 | 28.0–82.0 | 7.9–24 | |
| Quartile 4 | > 82.0 | > 24.0 | |
| Change | Mean (SD) | 59.4 (56.8) | 14.3 (18.1) |
| Quartile 1 | < 22.0 | < 6.0 | |
| Quartile 2-3 | 22.0–76.0 | 6.0–18.0 | |
| Quartile 4 | > 76.0 | > 18.0 |
sST-2= soluble ST-2; NT-proBNP= N-terminal prohormone of BNP
Compared to those who survived (Table 2), patients who died were older (69.6 vs 64.5, p<0.001) and more likely to have comorbidities such as atrial fibrillation (16% vs 5.6%, p<0.001) congestive heart failure (30% vs. 7.8%, p<0.001), diabetes (50% vs. 35%, p<0.001), vascular disease (42% vs. 25%, p<0.001), and any acute kidney injury (53% vs. 32%, p<0.001). During the procedure, patients who died commonly received packed red blood cells (61% vs. 34%, p<0.001), and when they did, received more units than those who survived (2.41 vs 0.95 mean units, p<0.001). The standard difference (d) for all these values were far greater than 0.10, highlighting the magnitude of imbalance between the two groups. Patients who died more commonly experienced in-hospital complications than those who survived (Table 3).
Table 2.
Characteristics of patients by survival status.
| Characteristics | Died (n=226) |
Survived (n=1,417) |
Std. Diff. (d) |
p-value‡ | |
|---|---|---|---|---|---|
| Demographics | Age, mean years (SD) | 69.5 (10.1) | 64.5 (9.9) | 0.50 | <0.001 |
| Women | 28% | 22% | 0.14 | 0.046 | |
| Body Mass Index, kg/m2 | 0.022 | ||||
| < 18.5 | 2.2% | 0.4% | 0.16 | ||
| 18.5-24.9 | 19% | 17% | 0.04 | ||
| 25.0-29.9 | 41% | 40% | 0.02 | ||
| 30.0-34.9 | 23% | 28% | 0.11 | ||
| ≥ 35.0 | 15% | 15% | 0.01 | ||
| Comorbidities | COPD | 21% | 12% | 0.25 | <0.001 |
| Smoker | 27% | 23% | 0.10 | 0.148 | |
| Diabetes | 53% | 36% | 0.36 | <0.001 | |
| Vascular Disease | 42% | 25% | 0.39 | <0.001 | |
| Preoperative serum creatinine, mg/dL (SD) | 1.29 (0.80) | 1.13 (1.05) | 0.17 | 0.030 | |
| AKI Network Stage | <0.001 | ||||
| No AKI | 47% | 68% | 0.44 | ||
| Stage 1 | 41% | 29% | 0.25 | ||
| Stage 2 | 6.0% | 2.0% | 0.21 | ||
| Stage 3 | 6.0% | 1.0% | 0.28 | ||
| Cardiac History, Function, and Anatomy | Preoperative MI | 0.008 | |||
| No | 47% | 57% | 0.22 | ||
| < 24 hours | 0.9% | 1.9% | 0.09 | ||
| > 24 hours, < 7 days | 22% | 18% | 0.10 | ||
| > 7 days, < 365 days | 15% | 9.1% | 0.17 | ||
| > 365 days | 16% | 14% | 0.07 | ||
| Prior CABG | 2.7% | 1.9% | 0.05 | 0.451 | |
| Prior PCI | 3.5% | 3.7% | 0.01 | 0.923 | |
| Hypertension | 85% | 80% | 0.12 | 0.109 | |
| Atrial Fibrillation | 16% | 5.5% | 0.33 | <0.001 | |
| Congestive heart failure | 30% | 7.8% | 0.58 | <0.001 | |
| Unstable angina | 54% | 54% | 0.004 | 0.955 | |
| Ejection Fraction (SD) | 49.1 (13.5) | 54.6 (11.5) | 0.44 | ||
| Left main, ≥ 50% stenosis | 39% | 33% | 0.14 | 0.050 | |
| Procedural Practice | Priority | 0.060 | |||
| Non-urgent | 25% | 32% | 0.14 | ||
| Urgent | 74% | 66% | 0.17 | ||
| Emergent | 0.9% | 2.1% | 0.10 | ||
| Preoperative IABP | 5.8% | 4.2% | 0.07 | <0.001 | |
| Received PRBC | 60% | 34% | 0.55 | <0.001 | |
| PRBC, units (SD) | 2.40 (3.68) | 0.95 (1.73) | 0.50 | <0.001 | |
SD= standard deviation; COPD=chronic obstructive pulmonary disease; AKI= acute kidney disease; MI= myocardial infarction; CABG= coronary artery bypass grafting; PCI= percutaneous coronary intervention; IABP= intraaortic balloon pump; PRBC= packed red blood cells
p-values calculated with chi-squared for categorical variables, Student’s t-test for continuous variables
Table 3.
In-hospital outcomes for patients by survival status.
| Outcome | Died (n=226) |
Survived (n=1,417) |
Std. Diff. (d) |
p-value‡ |
|---|---|---|---|---|
| Stroke | 8 (3.5%) | 13 (0.9%) | 0.18 | 0.001 |
| Transient Ischemic Attack | 1 (0.4%) | 4 (0.3%) | 0.03 | 0.685 |
| Mediastinis Infection | 5 (2.2%) | 6 (0.4%) | 0.15 | 0.006 |
| Pneumonia | 14 (6.2%) | 15 (1.1%) | 0.28 | <0.001 |
| Low Cardiac Output | 21 (9.4%) | 61 (4.4%) | 0.20 | 0.001 |
| Leg Infection | 2 (0.9%) | 13 (0.9%) | 0.003 | 0.962 |
| Return to Bypass Pump | 10 (4.5%) | 36 (2.6%) | 0.10 | 0.113 |
| Renal Failure | 6 (2.7%) | 2 (0.1%) | 0.21 | <0.001 |
Long-term survival
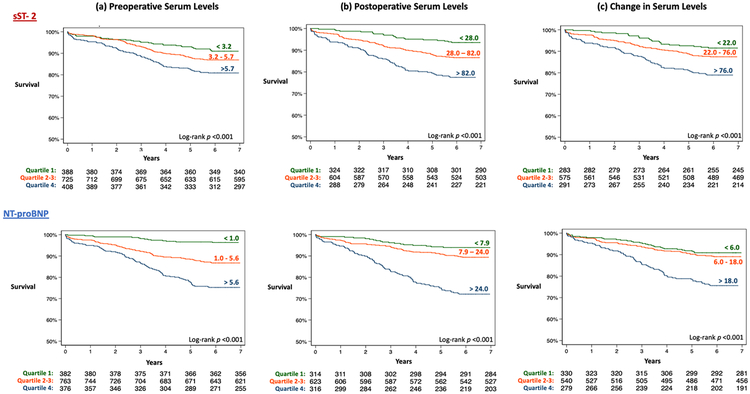
The 10-year survival rate in this cohort was 86%. The 30-day mortality was 0.9% (n=14). Kaplan-Meier survival analysis showed a dose-response relationship between sST-2 and NT-proBNP serum biomarker levels and patient survival, where increasing biomarker levels or change was associated with decreased survival rate. As such, patients in quartile 4, who are those with the highest preoperative/postoperative serum biomarker level or largest change, had the lowest survival rate (log-rank p<0.001 for all comparisons) (Figure 1).
Figure 1.
Kaplan Meier survival curves for (a) preoperative (b) postoperative and (c) change in sST-2 and NR-proBNP serum biomarker levels. This figure shows the relationship between long-term survival and quartile of biomarker serum level measured at different time points (log-rank p<0.001 for all comparisons).
We discovered this same trend in the unadjusted hazard ratios (HR) for all comparisons. Using quartile 1 as the reference group, patients in quartile 4 for preoperative, postoperative or change in biomarker levels were anywhere from 2-8 times more likely to die (p<0.05 for all comparisons) (Table 4). Though the size of the effect varied, this pattern was true for sST-2 and NT-proBNP.
Table 4.
Simple and adjusted effects of preoperative, postoperative, and chance in serum biomarker levels on long-term survival.
| Biomarker | % Dead |
Simple | Adjustedb | Adjusted + Other Biomarkerc | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | HR | 95% CI | p-value | ||
| Pre-operative (n= 1,526) | ||||||||||
| sST-2 | ||||||||||
| Quartile 1 | 10% | 1.0 (ref) | - | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - |
| Quartile 2-3 | 15% | 1.50 | 1.02-2.20 | 0.041 | 1.36 | 0.91-2.03 | 0.129 | 1.29 | 0.86–1.93 | 0.221 |
| Quartile 4 | 22% | 2.26 | 1.52-3.36 | <0.001 | 1.45 | 0.94-2.24 | 0.092 | 1.33 | 0.85-2.07 | 0.206 |
| NT-proBNP | ||||||||||
| Quartile 1 | 3.7% | 1.0 (ref) | - | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - |
| Quartile 2-3 | 15% | 3.83 | 2.19-6.70 | <0.001 | 2.43 | 1.36-4.32 | 0.003 | 2.33 | 1.31-4.16 | 0.004 |
| Quartile 4 | 28% | 7.66 | 4.37-13.43 | <0.001 | 2.89 | 1.54-5.43 | 0.001 | 2.63 | 1.38–4.99 | 0.003 |
| Post-operative (n= 1,256) | ||||||||||
| sST-2 | ||||||||||
| Quartile 1 | 7.3% | 1.0 (ref) | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - | |
| Quartile 2-3 | 14% | 2.17 | 2.35-3.51 | 0.001 | 1.49 | 0.90-2.45 | 0.117 | 1.38 | 0.83-2.27 | 0.213 |
| Quartile 4 | 27% | 3.95 | 2.42-6.44 | <0.001 | 2.57 | 1.52-4.35 | <0.001 | 2.27 | 1.33–3.86 | 0.003 |
| NT-proBNP | ||||||||||
| Quartile 1 | 6.0% | 1.0 (ref) | - | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - |
| Quartile 2-3 | 12% | 1.81 | 1.08-3.01 | 0.023 | 1.26 | 0.74-2.14 | 0.391 | 1.17 | 0.69–1.99 | 0.564 |
| Quartile 4 | 32% | 5.28 | 3.21-8.66 | <0.001 | 2.50 | 1.40-4.47 | 0.002 | 2.13 | 1.18–1.99 | 0.012 |
| Change in Serum Level (n=1,152) | ||||||||||
| sST-2 | ||||||||||
| Quartile 1 | 8.8% | 1.0 (ref) | - | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - |
| Quartile 2-3 | 13% | 1.52 | 0.96-2.40 | 0.071 | 1.09 | 0.78-1.76 | 0.710 | 1.03 | 0.63-1.67 | 0.913 |
| Quartile 4 | 25% | 2.81 | 1.76-4.47 | <0.001 | 1.77 | 1.07-2.95 | 0.027 | 1.50 | 0.87-2.53 | 0.131 |
| NT-proBNP | ||||||||||
| Quartile 1 | 9.3% | 1.0 (ref) | - | - | 1.0 (ref) | - | - | 1.0 (ref) | - | - |
| Quartile 2-3 | 12% | 1.22 | 0.78-1.89 | 0.381 | 1.12 | 0.70-1.76 | 0.632 | 1.10 | 0.69-1.74 | 0.693 |
| Quartile 4 | 28% | 2.96 | 1.93-4.54 | <0.001 | 1.85 | 1.13-3.02 | 0.014 | 1.69 | 1.02–2.79 | 0.040 |
HR= hazard ratio; CI= confidence interval; sST-2= soluble ST-2; NT-proBNP= N-terminal prohormone of BNP
Adjusted for ASCERT variables: age, weight, height, creatinine, ejection fraction, mean aortic gradient, sex, ethnicity, diabetes, cerebrovascular disease, cigarette smoking, congestive heart failure class, prior cardiac operation, cardiac status, number of diseased coronary vessels, myocardial infarction, and valve insufficiency.24,25
Adjusted for all ASCERT variables and other biomarker measure (e.g sST-2 model adjusted for NT-proBNP level at the same time point, and vice versa).
After adjustment, patients in quartile 4 of postoperative and change in sST-2 levels remained 2.6 times (HR 2.57, 9% CI: 1.52-4.35) and 1.8 times (HR 1.77, 95% CI: 1.07-2.95) more likely to die after surgery, respectively. Risk adjustment mitigated the effect of preoperative sST-2 levels and they were no longer statistically significantly predictive of death. Similarly, we found that adjusted HRs for quartile 4 NT-proBNP levels were associated with an increased likelihood of death across preoperative (HR 2.89, 95% CI: 1.54-5.43), postoperative (HR 2.50, 95% CI: 1.40-4.47), and change in levels (HR 1.85, 95% CI: 1.13-3.02). We found similar trends even after adjusting the other biomarker level at the same time point (e.g adjust for NT-proBNP level in the sST-2 model).
Comment
The use of cardiac biomarkers such as sST-2 and NT-proBNP is limited in cardiac surgery, though measuring biomarkers serum levels can potentially facilitate improved patient outcomes. Our study demonstrated that elevated preoperative and postoperative measure of sST-2 and NT-proBNP, and large changes in serum levels of these biomarkers are predictive of poorer postsurgical survival, even after adjustment for patient comorbidities and procedural characteristics. These findings can be used to identify patients at high-risk for death after CABG and/or valve replacement. Providers can then offer targeted care such as more extensive evaluation, post-discharge home visits, closer surveillance by primary care physician, or earlier post-operative follow-up appointments for these patients, actions that might mitigate future adverse outcomes.
Our results are corroborated by the cardiovascular literature. Increasing levels of sST-2 and NT-proBNP have been successfully used to identify and predict adverse outcomes for heart failure and acute myocardial infarction.8, 10-12, 14-16, 26, 27 In fact, NT-proBNP serum levels have become an established clinical practice for heart failure patients.28, 29 The most recent update of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines of the Management of Heart Failure also mentions the role of sST-2 in additive risk stratification for heart failure patients, however, calls for more validation studies in large cohorts.29 In terms of cardiac surgery, a previous study of the NNECDSG registry evaluated the added value of preoperative serum biomarker levels, including NT-proBNP, to risk prediction models for in-hospital mortality after CABG and found that there was no significant improvement in prediction ability over using patient and disease characteristics alone.19 However since then, several other studies of the NNECDSG Biomarker Study have found prognostic value for sST-2 and NT-proBNP to predict short term outcomes such as 1-year mortality and readmission, though long-term outcomes remain unstudied.20, 21, 30 There is less research available about how NT-proBNP and ST2 biomarker levels change due to intervention (e.g. the change from preoperative to postoperative level) and how this affects long-term outcomes, for which our study is a novel contribution to the published literature.
Despite the promise of our findings, there were limitations to our study. We used data from the NNECDSG Biomarker Study, a large, multicenter prospective study that enrolled patients in Northern New England. This patient population might not be generalizable across the United States, hence further studies would be required to see how the effect size changes for a potentially younger, more racially diverse population. Furthermore, the primary outcome in this study was all-cause mortality, and thus, our focus on cardiovascular comorbidities might not capture the residual confounding for predicting this outcome.
In conclusion, elevated pre- and post-operative levels of sST-2 or NT-proBNP are associated with increased risk of worse survival after cardiac surgery. Future research should expand on the generalizability of these findings to establish clinically significant thresholds for risk stratification or estimating postsurgical prognosis in order to identify and target interventions to patients at high-risk for poor survival. Early intervention in high-risk cases can ultimately improve long-term outcomes for patients undergoing CABG or valve replacement procedures.
Acknowledgments
Disclosures
This research was funded by the National Health, Lung, and Blood Institute R01HL119664 (PI: Jeremiah Brown, PhD, MS). The NNE Biomarker Study was funded in part by the NNECDSG. Donald Likosky, PhD discloses a financial relationship with Agency for Healthcare Research & Quality, National Institute of Health, and American Society of Extracorporeal Technology. Jeffery P. Jacobs, MD is the Chair of The Society of Thoracic Surgeons Workforce on National Databases.
Footnotes
Presented at the 65th Annual Meeting of the Southern Thoracic Surgical Association Amelia Island, Florida, November 7-10, 2018
References
- 1.Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clinical Pharmacology & Therapeutics. 2001;69:89–95. [DOI] [PubMed] [Google Scholar]
- 2.Ng PC, Ma TPY and Lam HS. The use of laboratory biomarkers for surveillance, diagnosis and prediction of clinical outcomes in neonatal sepsis and necrotising enterocolitis Archives of Disease in Childhood - Fetal and Neonatal Edition. 2015;100:F448–F452. [DOI] [PubMed] [Google Scholar]
- 3.Schulte PA. The use of biomarkers in surveillance, medical screening, and intervention. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 2005;592:155–163. [DOI] [PubMed] [Google Scholar]
- 4.Schütte K, Schulz C, Link A and Malfertheiner P. Current biomarkers for hepatocellular carcinoma: Surveillance, diagnosis and prediction of prognosis. World Journal of Hepatology. 2015;7:139–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kompier LC, Lurkin I, van der Aa MNM, van Rhijn BWG, van der Kwast TH and Zwarthoff EC. FGFR3, HRAS, KRAS, NRAS and PIK3CA Mutations in Bladder Cancer and Their Potential as Biomarkers for Surveillance and Therapy. PLOS ONE. 2010;5:e13821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Havrilesky LJ, Whitehead CM, Rubatt JM, Cheek RL, Groelke J, He Q, Malinowski DP, Fischer TJ and Berchuck A. Evaluation of biomarker panels for early stage ovarian cancer detection and monitoring for disease recurrence. Gynecologic Oncology. 2008;110:374–382. [DOI] [PubMed] [Google Scholar]
- 7.Prevention CDfHDaS. Heart Disease Fact Sheet. 2017.
- 8.Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie ANJ and Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. Journal of Clinical Investigation. 2007;117:1538–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinberg EO, Shimpo M, De Keulenaer GW, MacGillivray C, Tominaga SI, Solomon SD, Rouleau JL and Lee RT. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation. 2002;106:2961–2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weir RAP, Miller AM, Murphy GEJ, Clements S, Steedman T, Connell JMC, McInnes IB, Dargie HJ and McMurray JJV. Serum Soluble ST2. A Potential Novel Mediator in Left Ventricular and Infarct Remodeling After Acute Myocardial Infarction. Journal of the American College of Cardiology. 2010;55:243–250. [DOI] [PubMed] [Google Scholar]
- 11.Manzano-Fernández S, Mueller T, Pascual-Figal D, Truong QA and Januzzi JL. Usefulness of Soluble Concentrations of Interleukin Family Member ST2 as Predictor of Mortality in Patients With Acutely Decompensated Heart Failure Relative to Left Ventricular Ejection Fraction. The American Journal of Cardiology. 2011;107:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pascual-Figal DA, Manzano-Fernández S, Boronat M, Casas T, Garrido IP, Bonaque JC, Pastor-Perez F, Valdés M and Januzzi JL. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. European Journal of Heart Failure. 2011;13:718–725. [DOI] [PubMed] [Google Scholar]
- 13.Weber M and Hamm C. Role of B-type natriuretic peptide (BNP) and NT-proBNP in clinical routine. Heart. 2006;92:843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Januzzi JL, Camargo CA, Anwaruddin S, Baggish AL, Chen AA, Krauser DG, Tung R, Cameron R, Nagurney JT, Chae CU, Lloyd-Jones DM, Brown DF, Foran-Melanson S, Sluss PM, Lee-Lewandrowski E and Lewandrowski KB. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency department (PRIDE) study. The American Journal of Cardiology. 2005;95:948–954. [DOI] [PubMed] [Google Scholar]
- 15.Seino Y, Ogawa A, Yamashita T, Fukushima M, Ogata K-i, Fukumoto H and Takano T. Application of NT-proBNP and BNP measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure. European Journal of Heart Failure. 2004;6:295–300. [DOI] [PubMed] [Google Scholar]
- 16.Mueller T, Dieplinger B, Gegenhuber A, Poelz W, Pacher R and Haltmayer M. Increased Plasma Concentrations of Soluble ST2 are Predictive for 1-Year Mortality in Patients with Acute Destabilized Heart Failure. Clinical Chemistry. 2008;54:752. [DOI] [PubMed] [Google Scholar]
- 17.O’Connor GT, Plume SK, Olmstead EM and et al. A regional prospective study of in-hospital mortality associated with coronary artery bypass grafting. JAMA. 1991;266:803–809. [PubMed] [Google Scholar]
- 18.Malenka DJ and O’Connor GT. The Northern New England Cardiovascular Disease Study Group: A Regional Collaborative Effort for Continuous Quality Improvement in Cardiovascular Disease. The Joint Commission Journal on Quality Improvement. 1998;24:594–600. [DOI] [PubMed] [Google Scholar]
- 19.Brown JR, MacKenzie TA, Dacey LJ, Leavitt BJ, Braxton JH, Westbrook BM, Helm RE, Klemperer JD, Frumiento C, Sardella GL, Ross CS, O’Connor GT and for the Northern New England Cardiovascular Disease Study G. Using Biomarkers to Improve the Preoperative Prediction of Death in Coronary Artery Bypass Graft Patients. The Journal of Extra-corporeal Technology. 2010;42:293–300. [PMC free article] [PubMed] [Google Scholar]
- 20.Brown JR, Jacobs JP, Alam SS, Thiessen-Philbrook H, Everett A, Likosky DS, Lobdell K, Wyler von Ballmoos MC, Parker DM, Garg AX, Mackenzie T, Jacobs ML and Parikh CR. Utility of Biomarkers to Improve Prediction of Readmission or Mortality after Cardiac Surgery. The Annals of Thoracic Surgery. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polineni S, Parker DM, Alam SS, Thiessen-Philbrook H, McArthur E, DiScipio AW, Malenka DJ, Parikh CR, Garg AX and Brown JR. Predictive Ability of Novel Cardiac Biomarkers ST2, Galectin-3, and NT-ProBNP Before Cardiac Surgery. Journal of the American Heart Association. 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown JR, Hisey WM, Marshall EJ, Likosky DS, Nichols EL, Everett AD, Pasquali SK, Jacobs ML, Jacobs JP and Parikh CR. Acute Kidney Injury Severity and Long-Term Readmission and Mortality After Cardiac Surgery. Ann Thorac Surg. 2016;102:1482–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shahian DM, O’Brien SM, Sheng S, Grover FL, Mayer JE, Jacobs JP, Weiss JM, DeLong ER, Peterson ED, Weintraub WS, Grau-Sepulveda MV, Klein LW, Shaw RE, Garratt K, Moussa I, Shewan CM, Dangas GD and Edwards FH. Predictors of Long-Term Survival Following Coronary Artery Bypass Grafting Surgery: Results from The Society of Thoracic Surgeons Adult Cardiac Surgery Database (The ASCERT Study). Circulation. 2012;125:1491–1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lancaster TS, Schill MR, Greenberg JW, Ruaengsri C, Schuessler RB, Lawton JS, Maniar HS, Pasque MK, Moon MR, Damiano RJ and Melby SJ. Long-Term Survival Prediction for Coronary Artery Bypass Grafting: Validation of the ASCERT Model Compared With The Society of Thoracic Surgeons Predicted Risk of Mortality. The Annals of Thoracic Surgery. 2018;105:1336–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stabler ME, Rezaee ME, Parker DM, MacKenzie TA, Bohm AR, DiScipio AW, Malenka DJ and Brown JR. sST2 as a Novel Biomarker for the Prediction of In-hospital Mortality after Coronary Artery Bypass Grafting. Biomarkers : biochemical indicators of exposure, response, and susceptibility to chemicals. 2018:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lobdell KW, Parker DM, Likosky DS, Rezaee M, Wyler von Ballmoos M, Alam SS, Owens S, Thiessen-Philbrook H, MacKenzie T and Brown JR. Preoperative serum ST2 level predicts acute kidney injury after adult cardiac surgery. The Journal of thoracic and cardiovascular surgery. 2018;156:1114–1123.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morrow DA, Cannon CP, Jesse RL, Newby LK, Ravkilde J, Storrow AB, Wu AH and Christenson RH. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: Clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation. 2007;115:e356–75. [DOI] [PubMed] [Google Scholar]
- 29.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW and Westlake C. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. [DOI] [PubMed] [Google Scholar]
- 30.Jacobs JP, Alam SS, Owens SL, Parker DM, Rezaee M, Likosky DS, Shahian DM, Jacobs ML, Thiessen-Philbrook H, Wyler von Ballmoos M, Lobdell K, MacKenzie T, Everett AD, Parikh CR and Brown JR. The Association Between Novel Biomarkers and 1-Year Readmission or Mortality After Cardiac Surgery. Ann Thorac Surg. 2018;106:1122–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]