Abstract
Burnout and depression pose significant threats to emotional and occupational functioning; however, questions exist over how these two conditions are associated with each other over time, and how they are related to underlying job stressors. The Job Demands-Resources model (JD-R) provides a useful framework for understanding how job demands and job resources may lead to burnout, but questions remain about their distinct association with depression symptoms. The current study examined these questions in a sample of 402 nursing workers. The Exhaustion subscale of the Oldenburg Burnout Inventory (OLBI), the Patient Health Questionnaire-9 (PHQ-9) depression assessment, and items reflecting job demands and job resources from the Copenhagen Psychosocial Questionnaire were assessed at baseline; additionally, OLBI Exhaustion and PHQ-9 depression were assessed over 12 monthly follow-ups. Linear mixed models assessed longitudinal bidirectional associations between burnout and depression in both concurrent and lagged models. Longitudinal models found bidirectional relationships between burnout and depression symptoms over time, with relatively stronger associations for concurrent models relative to lagged models. Job demands and job resources each predicted unique variance in burnout and depression symptoms over time. Results provide evidence that burnout and depression symptoms change in the same direction, in tandem, rather than one condition having a distinctly stronger temporal association over the other. Results also indicate that both job demands and job resources are associated with depression symptoms independent from their association with burnout symptoms. Our results highlight the importance of considering burnout symptoms, depression symptoms, and job stressors concurrently in evaluating worker mental health.
Keywords: burnout, depression, nursing, Job Demands-Resources
If a leading goal of occupational health is to foster well-being in the work environment, then workplace burnout and depression present a major barrier to this objective. Burnout, which is characterized as a behavioral reaction to the cumulative effects of workplace stressors (Demerouti, Bakker, Nachreiner, & Schaufeli, 2001; Maslach, Schaufeli, & Leiter, 2001; Shirom, 2003), has been associated with multiple adverse outcomes related to health and work ability (Ahola et al., 2009; Borritz et al., 2010; Fragoso et al., 2016; Melamed, Shirom, Toker, Berliner, & Shapira, 2006). Depression presents an even greater health and disability risk than burnout; it is the world’s leading cause of poor health and disability (World Health Organization, 2017), and its most prevalent single mental disorder (Murray et al., 2013). Both burnout and depression are manifestations of chronic stress, with similarities and differences in underlying stressors. Like burnout, depression can be caused by occupational stressors (EU-OSHA, 2014), but it is also influenced by a broader range of interpersonal and social stressors, as well as by biological factors (American Psychiatric Association, 2013). In both cases, burnout and depression are associated with economic loss and adverse effect on worker well-being (EU-OSHA, 2014). In order to improve occupational outcomes related to mental health, it is important to better understand the associations among burnout, depression, and underlying contributions of psychosocial stressors in the workplace.
Burnout
Among the first and most enduring models of burnout has been articulated by Maslach and colleagues (Maslach et al., 2001), who identified burnout as composed of symptoms related to exhaustion, depersonalization, and reduced sense of personal accomplishment. These symptoms were seen as the result of job-related stressors, most often occurring in human service professions like nursing, medicine, and social work. In addition to Maslach’s model of burnout, there are several alternative models involving varying and overlapping dimensions (Demerouti et al., 2001; Shirom, 2003). One systematic review examined multiple models of burnout and found the common construct across these models to be exhaustion (Seidler et al., 2014). The exhaustion dimension of burnout has been described as a loss of emotional and energetic resources resulting from a long-term adaptive failure to resolve mismatches between job demands and worker resources (Bianchi, Schonfeld, & Laurent, 2015). Prevailing models of burnout share the assumption that exhaustion-related burnout is largely precipitated by chronic exposure to workplace stressors, including workload demands, emotional burden, low job autonomy, and lack of organizational leadership (Demerouti et al., 2001; Maslach et al., 2001; Shirom, 2003).
Depression
Depressive symptoms are often associated with the clinical diagnosis of MDD, which is characterized by sad mood and loss of motivation, as well as by symptoms that can include impaired concentration and decision making, guilt, sleep problems, appetite dysregulation, fatigue or loss of energy, and suicidal thoughts. The diagnosis of MDD is also marked by impairments in social and occupational functioning (American Psychiatric Association, 2013). Whereas burnout is largely conceptualized as a response to workplace stressors, research suggests that depression is more strongly associated with non-work-related life stressors than is burnout (Plieger, Melchers, Montag, Meermann, & Reuter, 2016). Additionally, depression can vary in clinical expression based on the underlying stressor (Keller, Neale, & Kendler, 2007). These findings support a common argument that burnout arises in the context of work, whereas the source of depression symptoms is context free (Bakker et al., 2000). Pertinent to the current study, it is important to recognize that many individuals experiencing depressive symptoms do not meet full criteria for MDD, but still experience similar distress and threats to well-being. Research suggests that subsyndromal depressive symptoms are comparable in prevalence to MDD (Pietrzak et al., 2013) and comparably impair health and work performance (Beck et al., 2011; Cuijpers et al., 2013); thus, as in the current study, elevated depression symptoms are themselves an important barrier to worker well-being even if they do not reflect a formal diagnosis.
The Relationship Between Burnout and Depression
One unresolved issue in the association between burnout and depression is the extent to which one condition precedes the other. To date, a limited number of studies have examined longitudinal associations between burnout and depression. Some longitudinal studies have found that burnout predicts depression Armon (Armon, Melamed, Toker, Berliner, & Shapira, 2014), while others have found that depression predicts burnout (Armon, Shirom, & Melamed, 2012; Campbell, Prochazka, Yamashita, & Gopal, 2010). The majority of studies, however, did not examine whether these associations were bidirectional. Among the studies that have examined a bidirectional relationship between burnout and depression symptoms, several have attempted to identify a temporal sequence between the two conditions, with mixed results. Several of these studies used longitudinal cross-lagged analysis, over periods from 18 months to 7 years, in samples ranging from healthcare workers, to teachers, to adolescent students. This group of studies found that burnout symptoms predicted later depression symptoms, but the association was not bidirectional; that is, depression symptoms did not similarly predict burnout (Hakanen & Schaufeli, 2012; Hakanen, Schaufeli, & Ahola, 2008; Salmela-Aro, Savolainen, & Holopainen, 2009; Shin, Noh, Jang, Park, & Lee, 2013). Four other studies examined the longitudinal association between burnout and depression, and found varying patterns of bidirectionality. Toker and Shirom (Toker & Biron, 2012) studied a multi-occupational sample over six years (N= 1632), and using a latent difference score model found that increased burnout from Time 1 to Time 2 predicted increased depression from Time 2 to Time 3. Notably, they found a bidirectional association of depression predicting increased burnout over the same waves. Ahola and colleagues (Ahola & Hakanen, 2007) followed a group of dentists over 3 years (N = 2,555), and based on a path analysis found reciprocal associations of burnout predicting depression symptoms from baseline to follow-up. Ahola and colleagues later examined the same cohort after a longer follow-up period, using a growth-mixture model to identify clusters of individuals with similar trajectories of burnout and depression over time (Ahola, Hakanen, Perhoniemi, & Mutanen, 2014). They found that burnout and depression symptoms clustered together at similar levels of severity, and increased and decreased in tandem over time. Based on these results, the authors concluded that burnout and depression symptoms are equivalent within the context of work. Another study followed a sample of nurses (N = 100) over two years and found evidence of a bidirectional association between burnout and depression symptoms without identifying an a priori temporal sequence (McKnight & Glass, 1995). The study did, however, explore concurrent change scores over time, which suggested concurrent rather than temporal change in the relationship between burnout and depression symptoms. Studies like these, which identify concurrent changes in burnout and depressive symptoms over time, may strengthen arguments for the mutuality of burnout and depression by showing that the symptoms of each construct change in tandem over time. In contrast, studies finding a clear temporal relationship in the development of burnout and depression symptoms may suggest that one of these constructs has a distinctly stronger association relative to the other. While acknowledging that true causality cannot be established via observational research, important considerations in judgements about causality can include the strength, consistency, and specificity of associations (Hill, 1965). The mixed evidence reviewed above suggests that more comprehensive approaches are needed to better understand whether meaningful conclusions can be drawn about temporal or concurrent associations between burnout and depression symptoms.
A Conceptual Framework for Occupational Burnout and Depression
A final area to consider is the process by which workplace stressors can lead to burnout and depression symptoms individually, which in turn may provide insight into how they are associated with each other. Several models of job stress have shown the association between work-related factors and adverse health outcomes, including the Job Demands-Control Model (JDC: Karasek, 1979; Karasek & Theorell, 1990) and the Effort-Reward Imbalance Model (ERI: Siegrist, 1996); however, one model that has focused more specifically on burnout is the Job Demands-Resources model (JD-R: Bakker & Demerouti, 2007; Demerouti et al., 2001). The JD-R model theorizes a dynamic balance between job demands and job resources: job demands reflect work characteristics requiring sustained physical or psychological effort, which can result in physical or psychological costs when this effort is overtaxed; job resources, in contrast, are characteristics that aid in the management of demands, help achieve work goals, or foster personal growth and learning. The JD-R assumes every workplace has a distinct work culture, and it allows the flexibility to assimilate a wide range of job demands and job resources across intra-personal, interpersonal, and organizational levels. As such, it has been argued that the JD-R can encompass content of both JDC and ERI models (Schaufeli & Taris, 2014). Indeed, a prior study with a group of call center workers found that a JD-R-based model accounted for more variance in emotional exhaustion than the JDC and ERI models alone (Lewig & Dollard, 2003).
In the JD-R framework, burnout is a unitary construct reflecting a health impairment process caused by energetic depletion from stressors that can include chronic high job demands as well as low job resources (Bakker & Demerouti, 2007). Burnout is viewed as the endpoint of this health impairment process, (Schaufeli & Taris, 2014), but depression is a plausible endpoint as well. Few studies have examined the associations among burnout, depression, and job stressors in a longitudinal design; fewer still tested bidirectional relationships between burnout and depression symptoms. To our knowledge, there is only one study to have undertaken such an approach (Ahola & Hakanen, 2007), which was a 3-year follow-up study of Finnish dentists that tested whether job stress was associated with depression symptoms and mediated by burnout. The authors defined job stress specifically as “job strain” based on the JDC model (operationalized as a ratio of Job Demands to Job Control as measured by Job Content Questionnaire). They found that a higher job-strain ratio predicted depressive symptoms, but the association was no longer significant after adjusting for the effects of burnout. Job strain was associated with depression symptoms only indirectly via burnout; in contrast, job strain was directly associated with burnout, and also indirectly associated with burnout via depression symptoms. This study appears to support an argument that burnout is distinct from depression because of its direct association with high job strain, whereas job strain may not be related to depression in the absence of the mediating influence of burnout symptoms. While this study suggests a potentially important distinction about temporal and bidirectional relationships between burnout and depression symptoms with respect to job stress, it does not examine concurrent change, and because it uses the JD-C model of job strain, it does not consider the separate contributions of job demands and job resources. Given these limitations, it is important to evaluate the association of burnout and depression symptoms from the perspective an alternative model such as the JD-R, while also extending understanding of their longitudinal relationship by testing both temporal and concurrent associations.
The Current Study
The preceding review highlights unresolved questions about how burnout and depression symptoms are related over time, and moreover the contribution of job demands and job resources to both conditions. The main focus of the current study is on better understanding the association of these two conditions to each other over time; that is, whether the associations are unidirectional versus bidirectional, and whether these associations are more strongly indicated to be temporal versus concurrent. Unidirectional effects would indicate that one condition is disproportionately influential over the other, while bidirectional effects would indicate that burnout and depression symptoms are mutually influential. Stronger effects for temporal associations would support arguments that burnout conceptually precedes depression (Hakanen & Schaufeli, 2012; Hakanen et al., 2008; Salmela-Aro et al., 2009; Shin et al., 2013), or possibly vice versa (Campbell et al., 2010) Associations that are stronger for concurrent associations, however, would support arguments that burnout and depression symptoms are mutually reciprocal, with no predominant direction of association across individuals (Ahola et al., 2014). The second focus of the study is on separate and distinct contributions of job demands and job resources to burnout and depression symptoms. Most theoretical models of job stress and burnout suggest job demands are a necessary contributor to burnout, but devote less attention to their role in depression symptoms independent of burnout (Schaufeli & Taris, 2014). While the JD-R model articulates that high job demands and low job resources are a pathway to health impairment, as manifest in burnout, finding that depression symptoms are also an endpoint to this pathway would provide a useful extension of the JD-R framework.
In the current study, we used a cohort of actively working individuals assessed monthly for one year to examine temporal and concurrent associations between burnout and depression symptoms. This examination can provide answers to important unresolved questions about the extent to which burnout and depression symptoms are related to each other in different temporal contexts, and whether job demands and resources have unique associations to one or both constructs. Similar to prior research, we predicted a bidirectional association between burnout and depression symptoms, as well as concurrent change between the two conditions across the monthly follow-up periods (Ahola et al., 2014; McKnight & Glass, 1995):
Hypothesis 1: Higher levels of burnout symptoms will predict higher levels of depression symptoms over 12 months; in turn, higher levels of depression symptoms will predict higher levels of burnout symptoms over the same follow-up period.
Hypothesis 2: Effect sizes predicting burnout and depression symptoms in models of concurrent change will be larger than effect sizes in models of lagged change.
Hypothesis 3: Higher job demands and lower job resources each will be associated separately with higher levels of burnout over 12 months, independent of the association of depression symptoms to burnout symptoms. Correspondingly, higher job demands and lower job resources each will be associated separately with higher levels of depression symptoms over 12 months, independent of the association of depression symptoms to burnout symptoms. That is, across lagged and concurrent models, job demands and job resources will each contribute unique variance to the prediction of burnout and depression symptoms over time.
Methods
Participants
The current study was conducted using a single-occupation sample of nursing workers. This fits our study objectives well, as nurses are exposed to high levels of cognitive and emotional stressors (Aiken, Sloane, Bruyneel, Van den Heede, & Sermeus, 2013) and are thus vulnerable to burnout (Demerouti, Bakker, Nachreiner, & Schaufeli, 2000) and depression (Letvak, Ruhm, & McCoy, 2012). Participants actively working in the nursing field were recruited from an academic health system in the southeast United States to reach a target sample of 400. Email addresses were requested and obtained from nursing administration. Emails requesting participation also contained a link with screening questions to determine eligibility. To be eligible, individuals had to be actively working in the nursing field; that is, not on medical leave, disability leave, or family leave. Participants were also required to have at least two years’ experience in the nursing field and to be at least 25 years old. This was done in order to exclude participants just starting their nursing career, as these individuals may experience work stressors differently than those established in the field. Recruitment was closed at 402 participants, which consisted of 375 Registered Nurses and 27 other nursing workers, including Licensed Practical Nurses, Certified Nursing Assistants, and Medical Assistants. The mean age was 41.7 years, with a standard deviation of 11.4 years. Ethnicity was 78% white, 14% African American, 5% Asian, and 3% Other. The proportion of women was 92.79%. The gender and ethnicity composition of the sample was similar to that of the nursing population as a whole (United States Department of Health and Human Services, 2010), with the exception that it over-represented Black/African-American persons (14.1%, compared to 5.4% in U.S. registered nurses). Though nursing administration supplied email addresses of nurses, they were blinded to the identity of those who participated.
Design
This study used a longitudinal design, with assessments completed at baseline and across 12 monthly follow-ups. Assessments were gathered via self-report, and consisted of demographic information collected at baseline, select questions on job demands and resources variables collected at baseline, and formal questionnaires on burnout and depression symptoms collected at baseline and each monthly follow-up. This allows for testing of bidirectional associations between burnout and depression symptoms over time. A trained research technician was present during the baseline assessment to provide instructions and answer questions, but was positioned so as to be blind to participants’ responses. Participant data was collected and maintained using Research Electronic Data Capture (REDCap), which is designed to establish user authentication and participant confidentiality (Harris et al., 2009). Follow-up assessments were requested via email. Completion rates at each month ranged from 87–98% (mean: 91%). The Institutional Review Board of Duke University approved this study.
Measures
Burnout.
Burnout was assessed using the Oldenburg Burnout Inventory (OLBI; Demerouti et al., 2001). The OLBI has scales for Exhaustion and Disengagement, however, only the Exhaustion scale was used in the current study. The Exhaustion scale assesses the extent to which one’s emotional, physical, and cognitive resources have been compromised, and includes items such as “I can tolerate the pressure of my work very well” and “during my work, I often feel emotionally drained”. Items are scored on a four-point Likert scale ranging from “strongly agree” to “strongly disagree”. Scores on negatively worded items are reversed before items are averaged, yielding a score ranging from one to four. OLBI Exhaustion was collected at baseline and each monthly follow-up. Internal consistency of this measure at baseline was found to be good (α=.81), with monthly values ranging from .81–.87 (see supplemental materials).
Depression.
The Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001) was used to assess depression symptoms in this study. This self-report measure assesses the frequency of nine depression symptoms over the previous two weeks (diminished interest in pleasurable activities, feeling down, sleep problems, diminished energy, appetite problems or overeating, feelings of failure, concentration problems, slowed speech or actions, and suicidal thoughts). Each item assesses symptom frequency, on a 0–3 scale (‘not at all’, ‘several days’, ‘more than half the days’, ‘nearly every day’), resulting in a total score with a possible range of 0–27. The validity of the PHQ-9 has been demonstrated, with studies indicating that a cutoff score of 10 achieved good sensitivity and specificity in relation to clinical diagnosis (Kroenke et al., 2001; Manea, Gilbody, & McMillan, 2015). The PHQ-9 was assessed at baseline and each monthly follow-up. Internal consistency of this measure at baseline was found to be good (α=.86), with monthly values ranging from .85–.89 (see supplemental materials).
Job Demands and Resources.
The Copenhagen Psychosocial Questionnaire, (COPSOQ:Kristensen, Hannerz, Hogh, & Borg, 2005; Pejtersen, Kristensen, Borg, & Bjorner, 2010) is a multiscale assessment of psychosocial work characteristics associated with job-related stress. Selected items were drawn from the 1st and 2nd versions of the questionnaire, and the names of the dimensions reflecting these items were retained as well (see supplemental materials for item content). Job demands was operationalized by 6 items from the Quantitative Demands scale, which was calculated by averaging the individual items (range of 0–100). Based on our previous work (Duan-Porter et al., 2018), job resources was operationalized by a single factor score derived from confirmatory factor analysis (CFA) of items from the following job resource scales from the COPSOQ: Influence at Work, Degree of Freedom, Possibilities for Development, Role Clarity, Quality of Leadership, and Social Support. Although the Job Resources factor-score from this CFA was our a priori assessment of the job resources construct, we planned to also analyze the individual resource variables for exploratory purposes. The COPSOQ was completed at baseline. Factor loadings from the CFA and individual scale items, and internal consistency are available in supplemental materials.
Analysis
Frequency distributions and measures of central tendency were used to describe the sample, and chi-square tests and Pearson correlations were used to assess bivariate relationships between covariates and study variables.
To assess longitudinal relationships between burnout and depression symptoms, we used linear mixed models. This analysis is a type of multilevel model that controls for variation within individuals by nesting repeated observations. To assess the degree of correlation in these repeated observations, random effects ANOVA models were used to obtain intra-class correlations (ICCs) for measures of each outcome (PHQ-9 Depression and OLBI Exhaustion) at baseline and the 12 monthly follow-ups. Including the baseline measures of the outcomes in our models is designed to control for the effect of initial levels of these variables on the follow-up assessments. To test the assumption of homoscedastic error variance across time points, a likelihood ratio test (LRT) was used to compare a model with one residual modeled across time points with a model that allowed a separate residual to be modeled at each time point. This revealed significant improvement in models allowing a separate residual at each time for both outcomes (PHQ-9 Depression: χ2(12)=44.7, p<.001; OLBI Exhaustion: χ2(12)= 53.3, p<.01), indicating that this assumption was not met. To adjust for this, models were specified to allow a separate residual at each time point. Although this added 12 parameters to each model, convergence was achieved in all models. We also tested for statistical significance in random intercept and slope terms, and the covariance between these. This was done to test for the presence of individual differences in baseline burnout and depression symptoms and individual differences in trajectories of these symptoms over time. It also tests whether individual differences in baseline levels of burnout and depression symptoms were related to the trajectory of these symptoms across the follow-up assessments, which provides additional control for the association of the baseline symptoms on the trajectory of the longitudinal symptoms. Burnout and depression symptoms were both modeled as outcomes, in separate models, in order to test for bidirectionality.
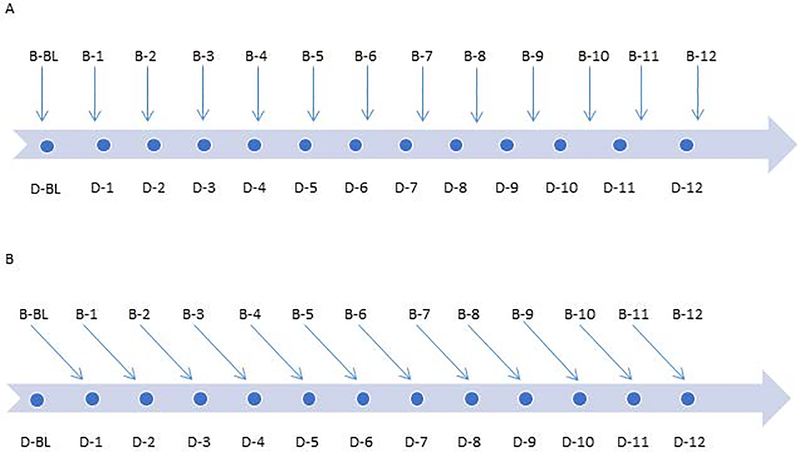
To examine the differences of tandem vs. temporal (concurrent or lagged) associations between burnout and depression symptoms, we modeled burnout using two types of time-variant predictors (see Figure 1). To assess concurrent burnout, burnout and depression symptoms were entered for the same month. To assess lagged burnout, burnout one month previous to depression at each month (i.e. burnout lagged one month) was entered. These models were conducted in three steps. In the first step, burnout (concurrent or lagged) was entered, along with age and sex as covariates. Time was also included, in order to estimate monthly rate of change in depression symptoms. In the second step, Quantitative Demands and the unitary Job Resources factor were added. Contingent on the Job Resources factor being significant, we also conducted a third step for exploratory purposes, in which the Job Resources factor was removed, and replaced by the individual resource scales. Lacking specific hypotheses regarding individual resource scales, we sought to better understand not just whether the global construct of job resources was significant, but also whether distinct types of job resources were significant contributors to the associations between burnout and depression symptoms. Standardized coefficients (denoted b*) are reported. Restricted maximum likelihood was used to estimate parameters. Mplus version 7 (Muthén & Muthén, 1998–2015) was used for CFA models and SAS version 9.3 (SAS Institute Inc., 2012) was used for descriptive statistics and linear mixed models.
Figure 1.
Schematic of Concurrent (A) and Lagged (B) models for 12-month follow up
A. Concurrent burnout: burnout concurrent with depression at each month. B. Lagged burnout: burnout lagged one month to depression at each month. Letter (B) = burnout symptoms. Letter (D) = depression symptoms.
Results
Sample Characteristics
Means and correlations among study measures are reported in Table 1. The mean OLBI burnout score at baseline was 2.61 (SD = 0.46) and the mean PHQ-9 score at baseline was 5.54 (SD = 4.85); however, approximately 20% of baseline PHQ-9 scores were above a score of 10, which indicates moderate and higher levels of symptom severity (Kroenke et al., 2001). Female gender was significantly associated with higher burnout symptoms (t=3.62, p<.01), but not with depression symptoms. Older age was associated with lower levels of burnout (r=−.10, p=.045), but not with depression symptoms (r=−.06, p=.27). There was a significant medium-sized correlation between baseline burnout and depression symptoms (r=.57, p<.01). There were significant small- to medium-sized correlations between burnout symptoms and nearly all of the job demands/resources variables, with the exception of a nonsignificant association with the Possibilities for Development variable. There were significant small- to medium-sized correlations between depression symptoms and all of the job demand/resource variables. For both burnout and depression symptoms, higher Quantitative Demands was associated with higher symptom severity, whereas higher levels of the job resources variables were associated with lower symptom severity. Overall, the magnitude of correlations with job demands/job resources was higher for burnout than for depression symptoms.
Table 1.
Baseline Sample Characteristics and Bivariate Correlations
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | ||||||||||
| 2. Gender | .01 | - | |||||||||
| 3. Exhaustion | −.10* | −.18** | - | ||||||||
| 4. Depression | −.06 | −.09 | .57** | - | |||||||
| 5. Quantitative Demands | .08 | .02 | .41** | .19** | - | ||||||
| 6. Influence at Work | .11* | .03 | −.30** | - 19** | −.05 | - | |||||
| 7. Degree of Freedom | .21** | .08 | −.28** | −.18** | −.10 | .46** | - | ||||
| 8. Possibilities for Development | −.13* | .10* | −.09 | −.14** | .01 | .24** | .22** | - | |||
| 9. Role Clarity | .04 | .06 | −.31** | −.29** | −.20** | .34** | .30** | .28** | - | ||
| 10. Quality of Leadership | .05 | .10* | −.40** | −.29** | −.20** | .35** | .31** | .28** | .44** | - | |
| 11. Social Support | −.09 | .06 | −.28** | −.26** | −.17** | .21** | .23** | .25** | .39** | .31** | - |
| M | 41.72 | 2.6 | 5.5 | 47.4 | 34.2 | 39.1 | 73.7 | 70.1 | 55.3 | 70.4 | |
| SD | 11.36 | 0.5 | 4.8 | 14.5 | 18.8 | 20.0 | 16.5 | 16.1 | 24.4 | 18.7 |
p<.05,
p<.01
Note. N = 402. Mean (M) and standard deviation (SD) reported for continuous variables. Point biserial correlations used for gender (0=female, 1=male; 92.8% female). Exhaustion= Oldenburg Burnout Inventory, Exhaustion subscale; Depression= Patient Health Questionnaire-9 Depression scale.
Longitudinal Burnout and Depression
Findings from linear mixed models revealed intra-class correlations of 0.69 and 0.75 for burnout and depression symptoms, respectively. Models of burnout and depression symptoms regressed on time revealed statistically significant random intercept and slope terms (burnout: b*=0.86, t=13.21, p<.001 and b*=0.003, t=9.52, p<.001; depression: b*=0.81, t=12.93, p<.001 and b*=0.003, t=9.35, p<.001), indicating individual differences in baseline values and slopes of exhaustion and depression, and significant covariances between random intercepts and slopes (burnout: b*=−0.02, t=−5.01, p<.001; depression: b*=−0.02, t=−5.36, p<.001). That the coefficients for these are negative indicates an inverse relation between these two regression components, in that higher baseline scores were associated with greater decline in symptoms over time.
Longitudinal Depression and Burnout on Concurrent Burnout and Depression
Models of longitudinal depression and burnout regressed on concurrent burnout and depression are presented in Table 2. Step 1 results indicate significant, medium-sized effects for concurrent burnout in predicting longitudinal depression symptoms (b*=0.38, t=18.77, p<.001), and concurrent depression symptoms in predicting longitudinal burnout (b*=0.35, t=19.53, p<.001). Interactions between concurrent predictors and time revealed non-significant interactions for concurrent exhaustion in predicting longitudinal depression (b*=0.004, t=1.51, p=.13), and a significant interaction for concurrent depression in predicting longitudinal exhaustion (b*=0.006, t=2.24, p=.03). To interpret this, simple slopes of longitudinal burnout at conditional values of concurrent depression symptoms were conducted. This indicated greater increases in burnout over time in those higher in concurrent depression symptoms (one standard deviation below the mean: b*=−0.004, t=−1.17, p=.24; mean: b*=0.001, t=0.51, p=.61; one standard deviation above the mean: b*=0.007, t=1.86, p=.06.
Table 2.
12-Month Longitudinal Depression and Burnout on Concurrent Burnout and Depression
| Variables | b* | 95% CI | t value | p-value | b* | 95% CI | t value | p-value | b* | 95% CI | t value | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression | ||||||||||||
| Burnout | 0.38 | 0.34, 0.41 | 18.77 | <.001 | 0.37 | 0.33, 0.41 | 17.95 | <.001 | 0.37 | 0.33, 0.41 | 17.92 | <.001 |
| Time, in months | 0.004 | −0.002, 0.009 | 1.33 | .18 | 0.004 | −0.002, 0.009 | 1.34 | .18 | 0.004 | −0.002, 0.009 | 1.34 | .18 |
| Age | 0.02 | −0.04, 0.07 | 0.59 | .55 | 0.02 | −0.03, 0.08 | 0.82 | .41 | 0.01 | −0.05, 0.07 | 0.46 | .64 |
| Sex | −0.08 | −0.28, 0.12 | −0.79 | .43 | −0.04 | −0.24, 0.16 | −0.43 | .67 | −0.04 | −0.24, 0.16 | −0.38 | .71 |
| Demands | 0.01 | −0.04, 0.07 | 0.43 | .67 | 0.004 | −0.06, 0.06 | 0.12 | .91 | ||||
| Resources | −0.11 | −0.17, −0.04 | −3.63 | <.001 | ||||||||
| Influence | 0.009 | −0.07, 0.07 | 0.03 | .98 | ||||||||
| Freedom | 0.01 | −0.05, 0.08 | 0.38 | .71 | ||||||||
| Development | −0.01 | −0.07, 0.05 | −0.25 | .81 | ||||||||
| Role Clarity | −0.04 | −0.11, 0.03 | −0.99 | .32 | ||||||||
| Leadership | −0.07 | −0.14, −0.004 | −2.07 | .04 | ||||||||
| Social Support | −0.06 | −0.13, 0.001 | −1.94 | .05 | ||||||||
| AIC | 7337 | 7333 | 7353 | |||||||||
| Burnout | ||||||||||||
| Depression | 0.35 | 0.32, 0.39 | 19.53 | <.001 | 0.34 | 0.30, 0.37 | 19.15 | <.001 | 0.34 | 0.30, 0.37 | 19.10 | <.001 |
| Time, in months | 0.001 | −0.004, 0.006 | 0.46 | .65 | 0.002 | −0.004, 0.007 | 0.57 | .57 | 0.002 | −0.004, 0.007 | 0.57 | .57 |
| Age | −0.09 | −0.16, −0.02 | −2.44 | .02 | −0.10 | −0.17, −0.04 | −3.16 | .002 | −0.09 | −0.16, −0.02 | −2.67 | .008 |
| Sex | −0.38 | −0.66, −0.11 | −2.72 | .007 | −0.35 | −0.60, −0.10 | −2.80 | .005 | −0.38 | −0.62, −0.13 | −3.02 | .003 |
| Demands | 0.27 | 0.21, 0.34 | 8.25 | <.001 | 0.27 | 0.20, 0.33 | 8.07 | <.001 | ||||
| Resources | −0.17 | −0.23, −0.10 | −5.08 | <.001 | ||||||||
| Influence | −0.13 | −0.21, −0.06 | −3.57 | <.001 | ||||||||
| Freedom | −0.02 | −0.10, 0.05 | −0.56 | .58 | ||||||||
| Development | 0.05 | −0.01, 0.12 | 1.54 | .13 | ||||||||
| Role Clarity | 0.01 | −0.07, 0.08 | 0.16 | .88 | ||||||||
| Leadership | −0.08 | −0.150, −0.003 | −2.05 | .04 | ||||||||
| Social Support | −0.07 | −0.141, −0.001 | −1.99 | .047 | ||||||||
| AIC | 6707 | 6618 | 6629 | |||||||||
Note. Depression= Patient Health Questionnaire-9 (PHQ-9) Depression scale; Burnout = Oldenburg Burnout Inventory Exhaustion scale; selected scales from the Copenhagen Psychosocial Questionnaire (COPSOQ): Demands = Quantitative Demands; Resources = factor score of the following scales; Influence = Influence at Work, Freedom = Degree of Freedom at Work; Development = Possibilities for Development; Role Clarity, Leadership = Quality of Leadership, Social Support, Social Support at Work
AIC= Akaike Information Criterion.
Results from Step 2 models revealed that after entering Quantitative Demands and the unitary Job Resources factor, concurrent exhaustion and depression symptoms remained significant (b*=0.37, t=17.95, p<.001; b*=0.34, t=19.15, p<.001). In these models, Quantitative Demands was significant in predicting longitudinal burnout only (b*=0.27, t=8.25, p<.001), and the unitary Job Resources factor was significant in predicting both longitudinal burnout and depression (b*=−0.11, t=−3.63, p<.001; b*=−0.17, t=−5.08, p<.001). Step 3 results revealed that after entering Quantitative Demands and the individual job resources variables, concurrent burnout and depression symptoms remained significant (b*=0.37, t=17.92, p<.001; b*=0.34, t=19.10, p<.001). In these models, Quantitative Demands was significant in predicting longitudinal burnout only (b*=0.27, t=8.07, p<.001). Among individual scales, Leadership Quality was significant in predicting longitudinal depression (b*=−0.07, t=−2.07, p=.04), and Influence at Work, Leadership Quality, and Social Support were significant in predicting longitudinal burnout (b*=−0.13, t=−3.57, p<.001; b*=−0.08, t=−2.05, p=.04; b*=−0.07, t=−1.99, p=.047).
Longitudinal Depression and Burnout on Lagged Burnout and Depression
Table 3 presents models of longitudinal depression and burnout regressed on lagged burnout and depression. This indicated a significant but small association between lagged burnout and longitudinal depression (b*=0.11, t=5.83, p<.001). A similar association was found between lagged depression and longitudinal burnout (b*=0.12, t=6.74, p<.001). Findings also revealed non-significant interactions between lagged predictors and time: for lagged burnout in predicting longitudinal depression (b*=0.0, t=0.01, p=.99), and for lagged depression in predicting longitudinal burnout (b*=0.002, t=0.87, p=.38). After entering Quantitative Demands and the unitary Job Resources factor in the individual models (Step 2), lagged burnout and depression both remained significant (burnout: b*=0.11, t=5.83, p<.001; depression: b*=0.12, t=6.74, p<.001). In these models, Quantitative Demands was significant in predicting longitudinal depression and burnout (depression: b*=0.12, t=3.24, p=.001; burnout: b*=0.28, t=7.72, p<.001), and the unitary Job Resources factor was significant in both outcomes as well (b*=−0.21, t=−5.56, p<.001; b*=−0.24, t=−6.35, p<.001). Following Step 3 of entering Quantitative Demands and the individual job resources variables, lagged burnout and depression remained significant (b*=0.09, t=4.94, p<.001; b*=0.11, t=6.15, p<.001). In these models, Quantitative Demands was significant in predicting both outcomes (depression: b*=0.11, t=2.78, p=.006; exhaustion: b*=0.28, t=7.54, p<.001). Among the individual job resources variables, Role Clarity and Leadership Quality were significant in predicting longitudinal depression (b*=−0.09, t=−1.97, p=.049; b*=−0.13, t=−2.93, p=.004), while and Influence at Work and Leadership Quality were significant in predicting longitudinal burnout (b*=−0.16, t=−3.93, p<.001; b*=−0.10, t=−2.46, p=.01).
Table 3.
12-Month Longitudinal Depression and Burnout on Lagged Burnout and Depression
| Variables | b* | 95% CI | t value | p-value | b* | 95% CI | t value | p-value | b* | 95% CI | t value | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression | ||||||||||||
| Burnout | 0.11 | 0.07, 0.14 | 5.83 | <.001 | 0.09 | 0.06, 0.13 | 4.99 | <.001 | 0.09 | 0.05, 0.13 | 4.94 | <.001 |
| Time, in months | 0.005 | −0.002, 0.01 | 1.47 | .14 | 0.005 | −0.002, 0.01 | 1.42 | .16 | 0.005 | −0.002, 0.012 | 1.42 | .16 |
| Age | −0.02 | −0.10, 0.05 | −0.55 | .58 | −0.02 | −0.09, 0.06 | −0.46 | .64 | −0.02 | −0.10, 0.05 | −0.65 | .52 |
| Sex | −0.20 | −0.48, 0.08 | −1.39 | .17 | −0.14 | −0.40, 0.13 | −0.99 | .32 | −0.14 | −0.41, 0.13 | −0.99 | .32 |
| Demands | 0.12 | 0.05, 0.20 | 3.24 | .001 | 0.11 | 0.03, 0.18 | 2.78 | .006 | ||||
| Resources | −0.21 | −0.29, −0.14 | −5.56 | <.001 | ||||||||
| Influence | −0.04 | −0.12, 0.04 | −0.93 | .36 | ||||||||
| Freedom | 0.02 | −0.06, 0.11 | 0.48 | .63 | ||||||||
| Development | 0.01 | −0.07, 0.09 | 0.29 | .77 | ||||||||
| Role Clarity | −0.09 | −0.176, −0.0003 | −1.97 | .049 | ||||||||
| Leadership | −0.13 | −0.22, −0.04 | −2.93 | .004 | ||||||||
| Social Support | −0.08 | −0.164, 0.0005 | −1.95 | .051 | ||||||||
| AIC | 7318 | 7315 | 7331 | |||||||||
| Burnout | ||||||||||||
| Depression | 0.12 | 0.08, 0.15 | 6.74 | <.001 | 0.11 | 0.07, 0.14 | 6.10 | <.001 | 0.11 | 0.07, 0.14 | 6.15 | <.001 |
| Time, in months | 0.003 | −0.003, 0.009 | 0.93 | .35 | 0.003 | −0.003, 0.009 | 0.97 | .33 | 0.003 | −0.003, 0.009 | 0.97 | .33 |
| Age | −0.08 | −0.16, 0.0001 | −1.95 | .052 | −0.09 | −0.16, −0.02 | −2.53 | .01 | −0.08 | −0.150, −0.003 | −2.05 | .04 |
| Sex | −0.36 | −0.67, −0.05 | −2.26 | .02 | −0.31 | −0.59, −0.04 | −2.23 | .03 | −0.34 | −0.61, −0.07 | −2.44 | .02 |
| Demands | 0.28 | 0.21, 0.36 | 7.72 | <.001 | 0.28 | 0.21, 0.35 | 7.54 | <.001 | ||||
| Resources | −0.24 | −0.31, −0.16 | −6.35 | <.001 | ||||||||
| Influence | −0.16 | −0.25, −0.08 | −3.93 | <.001 | ||||||||
| Freedom | −0.03 | −0.11, 0.06 | −0.62 | .54 | ||||||||
| Development | 0.06 | −0.02, 0.14 | 1.58 | .11 | ||||||||
| Role Clarity | −0.02 | −0.11, 0.06 | −0.56 | .58 | ||||||||
| Leadership | −0.10 | −0.19, −0.02 | −2.46 | .01 | ||||||||
| Social Support | −0.08 | −0.156, 0.001 | −1.95 | .052 | ||||||||
| AIC | 6595 | 6498 | 6507 | |||||||||
Note. Depression= Patient Health Questionnaire-9 (PHQ-9) Depression scale; Burnout = Oldenburg Burnout Inventory Exhaustion scale; selected scales from the Copenhagen Psychosocial Questionnaire (COPSOQ): Demands = Quantitative Demands; Resources = factor score of the following scales; Influence = Influence at Work, Freedom = Degree of Freedom at Work; Development = Possibilities for Development; Role Clarity, Leadership = Quality of Leadership, Social Support, Social Support at Work
AIC= Akaike Information Criterion
Discussion
Summary of Key Findings
The results of the current study most strongly support the idea that burnout and depression symptoms have both bidirectional and concurrent relationships to each other, as assessed on a month-to-month basis over a period of one year. A limitation of many prior studies of the association between burnout and depression is that they did not examine bidirectional associations; the current study makes a novel contribution by testing bidirectional associations in both concurrent and lagged models. Findings revealed medium-sized, bidirectional effects of concurrent burnout symptoms predicting longitudinal depression symptoms, and of concurrent depression symptoms predicting longitudinal burnout symptoms. Smaller bidirectional effect sizes were found for lagged models, suggesting that relative to the concurrent models, the strength of the bidirectional associations between burnout and depression symptoms weakened with temporal separation. We believe this is a novel finding in support of the argument that burnout and depression symptoms change in the same direction, in tandem, rather than one condition having a distinctly stronger temporal association relative to the other. Rather, we argue that changes in either burnout or depression symptom severity are associated with changes in the other symptom dimension in the same direction for a given individual. Another novel finding from the current study is that job resources contributed separate and unique variance to the prediction of both burnout and depression symptoms over time. This is important because the majority of studies focus on risk factors for burnout and depression symptoms, while the current study also highlights potential protective factors attributable to higher job resources. Job demands also contributed uniquely to burnout and depression symptoms over time, but more consistently for burnout symptoms. This suggests that the adverse effects of high job demands and low job resources are not specific to burnout over time, but also contribute independently to depression symptoms over time.
Comparison with Previous Findings
Results from the current study are important to consider in the context of previous research. Our results align with arguments that burnout and depression symptoms are highly inter-related in the context of work (Ahola et al., 2014), finding that they have bidirectional and concurrent effects on each other. In our comparison of two analytic approaches, findings for concurrent models were stronger and more consistent than for temporal models. If burnout symptoms were clearly casual to depression symptoms, or vice versa, a stronger case for temporality and consistency would be expected (Hill, 1965). The relatively smaller effects of lagged predictors is also consistent with previous evidence showing time-lagged relationships between burnout and depression to be non-significant (Armon et al., 2014; Toker & Biron, 2012). This suggests the contemporaneous effect of burnout symptoms on depression symptoms (and vice versa) is more robust than their delayed effects.
The current research also raises questions about findings that burnout symptoms mediate the associations between job stressors and depression symptoms, given that our findings indicate effects of both job demands and job resources on longitudinal depression symptoms independent from variance attributable to burnout symptoms. This result differs from a prior study finding that the association between job stress and depression was mediated by burnout (Ahola & Hakanen, 2007), in which job stress was conceptualized more narrowly as job strain according to the JDC model (operationalized as a quotient of Job Demands by Job Control as measured by Job Content Questionnaire). The JD-R model, in contrast, conceptualizes job stress as reflecting a more multi-dimensional balance between job demands and job resources, in this case operationalized by items from the COPSOQ.
The current results support the JD-R model with respect to burnout symptoms (Bakker & Demerouti, 2007; Demerouti et al., 2001), but also extend it with respect to depression symptoms. In the JD-R framework, job demands are theorized to contribute to a health impairment pathway that leads to burnout (Schaufeli & Taris, 2014); however, our results suggest depression is a likely endpoint to this pathway as well. In addition, our findings suggest that job resources independently contribute to this health impairment pathway for both burnout and depression symptoms. We do note that jobs demands had small but significant associations with longitudinal depression symptoms in the lagged models, but not in the concurrent models. We do not have a conclusive explanation for this discrepancy, though it may be that unmeasured changes in job demands- which were not assessed on a monthly basis- were specifically influential on depression symptoms in the lagged models in ways that we unfortunately cannot test in the context of the current study.
Practical Implications
Findings from this study have practical implications for occupational health psychology. One implication is that monitoring of workplace mental health should include not only assessments both burnout and depression symptoms, but also comprehensive assessment workplace stressors. While burnout and depression symptoms are highly related, they are still distinct constructs (Armon et al., 2014; Bakker et al., 2000; Toker & Biron, 2012), and screening only for one condition could lead to overlooking important symptoms of the other condition that are important for wellbeing and safety. In an employee health setting, for instance, assessing only for a presenting complaint of burnout may lead to overlooking more serious depression-related symptoms like suicidality, which occurs at a higher rate than the general population in some health professions (Sheikhmoonesi & Zarghami, 2014; Silva et al., 2015). As another example, failing to consider the contribution of burnout symptoms when treating depression may lead to a less effective treatment outcome by overlooking emotional exhaustion and potentially modifiable sources of job stress. Following this logic, it also appears important to assess both job demands and job resources to obtain a better understanding of where sources of stress and potential resilience may exist for emotionally distressed employees. With respect to individual intervention for workers, the results argue for an approach to therapy that assesses and targets burnout and depression conjointly by limiting the adverse impact of person-specific job demands, and augmenting the beneficial impact of person-specific job related resources, whether by problem solving, cognitive re-appraisal, behavioral activation, or other approaches. At the organizational level, it is again important to assess for both burnout and depression when assessing for psychosocial risks, as they may have different relationships to work productivity and health-related costs. As with the individual employee, assessment of job demands and job resources within an organization or work unit can provide an important guide to intervention strategies. The current study suggests the JD-R model is a useful framework for understanding burnout and depression at the individual and organizational levels, and the COPSOQ appears to be a useful assessment instrument, albeit one that was designed to assess at the organizational rather than individual level.
The results of the current study make a strong case that factors at the organizational level are related to mental well-being in the workforce, particularly burnout and depression symptoms. Consistent with previous research using the COPSOQ, individuals who report being unable to keep ahead of their workload are susceptible to persistent symptoms of burnout and depression (Borritz et al., 2006; Duan-Porter et al., 2018), which is consistent with adverse effects of high demand and effort in multiple models of job stress (Demerouti et al., 2001; Karasek, 1979; Siegrist, 1996). In nursing, for instance, organizational changes to better match staffing ratios to workload demands may pay dividends via improved patient health outcomes and higher levels of nurse well-being (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002). The current study also suggests that the quality of job resources within an organization may also be associated with lower levels of burnout and depression. The significant association for an overall Job Resources factor to levels of burnout and depression symptoms may be a proxy for impact of an organizational culture that intentionally values mental well-being in the workplace. In exploratory models, we found that quality of leadership is particularly important to levels of burnout and depression symptoms. Given that billions of dollars per year are spent on the development of leadership skills in the U.S. alone (Kaiser & Curphy, 2013), a comprehensive definition of leadership is beyond the scope of the current study; however, as operationalized in our measure, high quality of leadership was characterized by effective planning of work tasks, effective conflict resolution, promotion of employee development, and a priority on job satisfaction. Along with articulating clear work goals and responsibilities and providing a level of input and autonomy to employees, these job resources may be important objectives in establishing an organizational culture that supports emotional well-being.
Strengths and Limitations
One strength of the study is that participants were homogeneous with respect to occupational sector and organizational characteristics, which can reduce variance that occurs between different occupations and workplaces. A limitation to this, however, is difficulty appraising how the results from the current study generalize to other occupations, though we expect job stressors associated with burnout and depression symptoms among nurses to be similar among other health care professions and even other human service jobs. Ultimately, these relationships between burnout and depression symptoms remain to be examined in other occupational samples. We also note that while PHQ-9 scores are associated with the clinical diagnosis of MDD (Kroenke et al., 2001), our operational definition of depression was based on symptom severity and not a formal psychiatric diagnosis. The PHQ-9 is a useful clinical tool for tracking changes in depression symptom severity, as done in the current study; however, it is possible that different results may be obtained among individuals meeting formal diagnostic criteria for MDD.
One strength of our study was the longitudinal design, which assessed symptoms on a monthly schedule over the course of the year. Prior studies have used fewer individual assessments over a longer follow-up period, which may be less reliable in estimating concurrent change. Our design was well-suited to assess dynamic changes in burnout and depression symptoms over one year, which may be a more clinically relevant timeframe than longer follow-up periods, given that average resolution of both minor and major depression episodes occur over 6–12 months (Ten Have et al., 2017). Longer time intervals between assessment and a longer follow-up period may yield different results, including more divergent courses of burnout and depression over longer intervals, which may be disproportionately influenced by changes in unmeasured occupational and personal factors over time. We acknowledge that monthly assessments of burnout and depression may have led participants to become increasingly familiar with assessment items. In addition, the PHQ-9 and OLBI Exhaustion scale have different frames of temporal reference; the PHQ-9 asks about symptoms over the preceding two weeks, while the OLBI does not have a specific time frame for symptom reporting. While these characteristics may influence the accuracy monthly assessment of symptoms, the magnitude of correlations between measures at adjacent months did not appear to increase over time. This suggests participants were not increasingly biased toward responses they had given at previous months, and suggests that they were responding to symptoms they were experiencing contemporaneously rather than cumulatively or chronically.
Conclusions
The current study provides evidence supporting a close bidirectional relationship between burnout and depression symptoms and their concurrent associations with each other over time. Results favor the argument that burnout and depression symptoms change in the same direction, in tandem, rather than in a distinct temporal sequence. Job demands and job resources both uniquely predict burnout and depression symptoms over time. The results provide a strong argument for optimizing job demands and job resources to promote an organizational climate of emotional well-being.
Supplementary Material
Acknowledgements
This work was supported by funding from the German Federal Institute for Occupational Safety and Health and the National Institutes of Health under Grant T32-AG000029. The authors have no disclosures to report. The authors would like to recognize members of our study team, and the participants who took part in our study.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ahola K, Gould R, Virtanen M, Honkonen T, Aromaa A, & Lonnqvist J (2009). Occupational burnout as a predictor of disability pension: A population-based cohort study. Occupational and Environmental Medicine, 66, 284–290. 10.1136/oem.2008.038935 [DOI] [PubMed] [Google Scholar]
- Ahola K, & Hakanen J (2007). Job strain, burnout, and depressive symptoms: A prospective study among dentists. Journal of Affective Disorders, 104, 103–110. 10.1016/j.jad.2007.03.004 [DOI] [PubMed] [Google Scholar]
- Ahola K, Hakanen J, Perhoniemi R, & Mutanen P (2014). Relationship between burnout and depressive symptoms: A study using the person-centered approach. Burnout Research, 1, 29–37. 10.1016/j.burn.2014.03.003 [DOI] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, & Silber JH (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association, 288, 1987–1993. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, & Sermeus W (2013). Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. International Journal of Nursing Studies, 50, 143–153. http://dx.doi.org/j.ijnurstu.2012.11.009 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Armon G, Melamed S, Toker S, Berliner S, & Shapira I (2014). Joint effect of chronic medical illness and burnout on depressive symptoms among employed adults. Health Psychology, 33, 264–272. 10.1037/e577572014-258 [DOI] [PubMed] [Google Scholar]
- Armon G, Shirom A, & Melamed S (2012). The Big Five personality factors as redictors of changes across time in burnout and its facets. Journal of Personality, 80, 403–427. p 10.1111/j.1467-6494.2011.00731.x [DOI] [PubMed] [Google Scholar]
- Bakker AB, & Demerouti E (2007). The Job Demands-Resources model: State of the art. Journal of Managerial Psychology, 22, 309–328. 10.1108/02683940710733115 [DOI] [Google Scholar]
- Bakker AB, Schaufeli WB, Demerouti E, Janssen PPM, Van der Hulst R, & Brouwer J (2000). Using equity theory to examine the difference between burnout and depression. Anxiety Stress and Coping, 13, 247–268. 10.1080/10615800008415727 [DOI] [Google Scholar]
- Beck A, Crain AL, Solberg LI, Unutzer J, Glasgow RE, Maciosek MV, & Whitebird R (2011). Severity of depression and magnitude of productivity loss. Annals of Family Medicine, 9, 305–311. 10.1370/afm.1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi R, Schonfeld IS, & Laurent E (2015). Burnout-depression overlap: A review. Clinincal Psychology Review, 36, 28–41. http://dx.doi.org/j.cpr.2015.01.004 [DOI] [PubMed] [Google Scholar]
- Borritz M, Christensen KB, Bultmann U, Rugulies R, Lund T, Andersen I, … Kristensen TS (2010). Impact of burnout and psychosocial work characteristics on future long-term sickness absence. Prospective results of the Danish PUMA Study among human service workers. Journal of Occupational and Environmental Medicine, 52, 964–970. 10.1097/jom.0b013e3181f12f95 [DOI] [PubMed] [Google Scholar]
- Borritz M, Rugulies R, Bjorner JB, Villadsen E, Mikkelsen OA, & Kristensen TS (2006). Burnout among employees in human service work: Design and baseline findings of the PUMA study. Scandinavian Journal of Public Health, 34, 49–58. 10.1080/14034940510032275 [DOI] [PubMed] [Google Scholar]
- Campbell J, Prochazka AV, Yamashita T, & Gopal R (2010). Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Academic Medicine, 85, 1630–1634. http://dx.doi.org/acm.0b013e3181f0c4e7 [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, & Penninx BW (2013). Differential mortality rates in major and subthreshold depression: Meta-analysis of studies that measured both. British Journal of Psychiatry, 202, 22–27. 10.1192/bjp.bp.112.112169 [DOI] [PubMed] [Google Scholar]
- Demerouti E, Bakker AB, Nachreiner F, & Schaufeli WB (2000). A model of burnout and life satisfaction amongst nurses. Journal of Advanced Nursing, 32, 454–464. 10.1046/j.1365-2648.2000.01496.x [DOI] [PubMed] [Google Scholar]
- Demerouti E, Bakker AB, Nachreiner F, & Schaufeli WB (2001). The job demands-resources model of burnout. Journal of Applied Psychology, 86, 499–512. 10.1037//0021-9010.86.3.499 [DOI] [PubMed] [Google Scholar]
- Duan-Porter W, Hatch D, Pendergast JF, Freude G, Rose U, Burr H, … Potter G (2018). 12-month trajectories of depressive symptoms among nurses-Contribution of personality, job characteristics, coping, and burnout. Journal of Affective Disorders, 234, 67–73. 10.1016/j.jad.2018.02.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragoso ZL, Holcombe KJ, McCluney CL, Fisher GG, McGonagle AK, & Friebe SJ (2016). Burnout and Engagement: Relative Importance of Predictors and Outcomes in Two Health Care Worker Samples. Workplace Health and Safety. 10.1177/2165079916653414 [DOI] [PubMed] [Google Scholar]
- Hakanen JJ, & Schaufeli WB (2012). Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. Journal of Affective Disorders, 141, 415–424. 10.1016/j.jad.2012.02.043 [DOI] [PubMed] [Google Scholar]
- Hakanen JJ, Schaufeli WB, & Ahola K (2008). The Job Demands-Resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work and Stress, 22, 224–241. 10.1080/02678370802379432 [DOI] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AB (1965). The environment and disease: Association or Causation? Bulletin of the World Heatlh Organization, 83, 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser RB, & Curphy G (2013). Leadership development: The failure of an industry and the opportunity for consulting psychologists. Consulting Psychology Journal: Practice and Research, 65, 294–302. 10.1037/a0035460 [DOI] [Google Scholar]
- Karasek RA (1979). Job Demands, Job Decision Latitude, and Mental Strain - Implications for Job Redesign. Administrative Science Quarterly, 24, 285–308. 10.2307/2392498 [DOI] [Google Scholar]
- Karasek RA, & Theorell T (1990). Healthy work: Stress, productivity, and the reconstruction of working life. New York: Basic Books, Inc. [Google Scholar]
- Keller MC, Neale MC, & Kendler KS (2007). Association of different adverse life events with distinct patterns of depressive symptoms. American Journal of Psychiatry, 164, 1521–1529. 10.1176/appi.ajp.2007.06091564 [DOI] [PubMed] [Google Scholar]
- Kristensen TS, Hannerz H, Hogh A, & Borg V (2005). The Copenhagen Psychosocial Questionnaire--a tool for the assessment and improvement of the psychosocial work environment. Scandinavian Journal of Work and Environmental Health, 31, 438–449. 10.5271/sjweh.948 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letvak S, Ruhm CJ, & McCoy T (2012). Depression in Hospital-Employed Nurses. Clinical Nurse Specialist, 26, 177–182. 10.1097/nur.0b013e3182503ef0 [DOI] [PubMed] [Google Scholar]
- Lewig KA, & Dollard MF (2003). Emotional dissonance, emotional exhaustion and job satisfaction in call centre workers. European Journal of Work and Organizational Psychology, 12, 366–392. 10.1080/13594320344000200 [DOI] [Google Scholar]
- Manea L, Gilbody S, & McMillan D (2015). A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. General Hospital Psychiatry, 37, 67–75. 10.1016/j.genhosppsych.2014.09.009 [DOI] [PubMed] [Google Scholar]
- Maslach C, Schaufeli WB, & Leiter MP (2001). Job burnout. Annual Review of Psychology, 52, 397–422. 10.1146/annurev.psych.52.1.397 [DOI] [PubMed] [Google Scholar]
- McKnight JD, & Glass DC (1995). Perceptions of control, burnout, and depressive symptomatology: a replication and extension. Journal of Consulting and Clinical Psychology, 63, 490–494. 10.1037//0022-006x.63.3.490 [DOI] [PubMed] [Google Scholar]
- Melamed S, Shirom A, Toker S, Berliner S, & Shapira I (2006). Burnout and risk of cardiovascular disease: Evidence, possible causal paths, and promising research directions. Psychological Bulletin, 132, 327–353. 10.1037/e538922013-203 [DOI] [PubMed] [Google Scholar]
- Murray CJL, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, … Lopez AD (2013). The State of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA - Journal of the American Medical Association, 310(6), 591–608. 10.1001/jama.2013.13805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2015). Mplus User’s Guide (Seventh ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pejtersen JH, Kristensen TS, Borg V, & Bjorner JB (2010). The second version of the Copenhagen Psychosocial Questionnaire. Scandinavian Journal of Public Health, 38, 8–24. http://dx.doi.org/10.1017/s003329171200230910.1177/140349480934985810.1177/1403494809349858 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Kinley J, Afifi TO, Enns MW, Fawcett J, & Sareen J (2013). Subsyndromal depression in the United States: Prevalence, course, and risk for incident psychiatric outcomes. Psychological Medicine, 43, 1401–1414. 10.1017/s0033291712002309 [DOI] [PubMed] [Google Scholar]
- Plieger T, Melchers M, Montag C, Meermann R, & Reuter M (2016). Life stress as potential risk factor for depression and burnout. Personality and Individual Differences, 101, 505–505. 10.1016/j.paid.2016.05.255 [DOI] [Google Scholar]
- Salmela-Aro K, Savolainen H, & Holopainen L (2009). Depressive symptoms and school burnout during adolescence: evidence from two cross-lagged longitudinal studies. Journal of Youth and Adolescence, 38, 1316–1327. 10.1007/s10964-008-9334-3 [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. (2012). SAS Release 9.3. Cary, NC. [Google Scholar]
- Schaufeli WB, & Taris TW (2014). A critical review of the Job Demands-Resources Model: Implications for improving work and health In Bauer GF & Hammig O (Eds.), Bridging Occupational, Organizational, and Public Health: A Transdisciplinary Approach (pp. 43–68). Dordrecht, The Netherlands: Springer Science + Business Media. [Google Scholar]
- Seidler A, Thinschmidt M, Deckert S, Then F, Hegewald J, Nieuwenhuijsen K, & Riedel-Heller SG (2014). The role of psychosocial working conditions on burnout and its core component emotional exhaustion - a systematic review. Journal of Occupational Medicine and Toxicology, 9, 10 10.1186/1745-6673-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikhmoonesi F, & Zarghami M (2014). Prevention of physicians’ suicide. Iranian Journal of Psychiatry and Behavioral Sciences, 8, 1–3. [PMC free article] [PubMed] [Google Scholar]
- Shin H, Noh H, Jang Y, Park YM, & Lee SM (2013). A longitudinal examination of the relationship between teacher burnout and depression. Journal of Employment Counseling, 50(3), 124–137. 10.1002/j.2161-1920.2013.00031.x [DOI] [Google Scholar]
- Shirom A (2003). Job-related burnout In Quick JC & Tetrick LE (Eds.), Handbook of Occupational Health Psychology (pp. 245–265). Washington, DC: American Psychological Association. [Google Scholar]
- Siegrist J (1996). Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology, 1, 27–41. 10.1037//1076-8998.1.1.27 [DOI] [PubMed] [Google Scholar]
- Silva DDD, Tavares NVD, Alexandre ARG, Freitas DA, Breda MZ, de Albuquerque MCD, & Neto VLD (2015). Depression and suicide risk among Nursing professionals: An integrative review. Revista Da Escola De Enfermagem Da Usp, 49, 1023–1031. 10.1590/s0080-623420150000600020 [DOI] [PubMed] [Google Scholar]
- Ten Have M, Penninx B, Tuithof M, van Dorsselaer S, Kleinjan M, Spijker J, & de Graaf R (2017). Duration of major and minor depressive episodes and associated risk indicators in a psychiatric epidemiological cohort study of the general population. Acta Psychiatrica Scandinavica, 136(3), 300–312. doi: 10.1111/acps.12753 [DOI] [PubMed] [Google Scholar]
- Toker S, & Biron M (2012). Job burnout and depression: unraveling their temporal relationship and considering the role of physical activity. Journal of Applied Psychology, 97, 699–710. 10.1037/a0026914 [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. (2010). The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses. Retrieved from http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf.
- World Health Organization. (2017). Depression Fact Sheet. Retrieved from Geneva, Switzerland: http://www.who.int/mediacentre/factsheets/fs369/en/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.