Abstract
Objective
Feeding concerns are common in the first 2 years of life and typically reflect maternal perceptions occurring within the larger context of the parent-child relationship. We aimed to determine if: 1) Maternal depressive symptoms predicted perceived picky eating, mediated by maternal negative perceptions; 2) Receipt of the Video Interaction Project (VIP) parenting intervention impacted perceived picky eating through this pathway; and 3) Perceived picky eating was associated with child growth or subsequent dietary patterns.
Methods
We performed a partial longitudinal analysis of 187 low-income, predominantly Hispanic mother-child dyads enrolled in a randomized controlled trial of VIP. Mother-infant dyads were enrolled postpartum in an urban public hospital. Participants randomized to VIP met with an interventionist on days of well-child visits; sessions were designed to facilitate interactions in play and shared reading through provision of learning materials and review of videotaped parent-child interaction; the curriculum did not contain feeding specific elements. We used structural equation modeling to determine direct, indirect, and total effects of maternal depressive symptoms, maternal negative perceptions, and VIP on perceived picky eating. We then tested associations between perceived picky eating and: 1) child growth, using multivariable linear regression and multilevel modeling; 2) subsequent child dietary consumption using multivariable multinomial logistic regression.
Results
Maternal depressive symptoms had significant total effects on negative maternal perceptions (β=0.32, p<0.001) and perceived picky eating (β=0.21, p<0.01) after controlling for potential confounders. This effect was partially mediated by maternal negative perceptions (indirect effect: β=0.06, p=0.04). When used in the model as the predictor, VIP had a significant total effect on perceived picky eating (β=−0.16, p=0.02), which was partially mediated by maternal depressive symptoms and negative perceptions (indirect effect: β=−0.05, p=0.02). Perceived picky eating was not associated with child diet at age 2 or adiposity from 6 months to 3 years.
Conclusion
Maternal concerns about picky eating may reflect deeper depressive symptoms and negative perceptions of her child’s behavior. Interventions designed to facilitate positive parenting in general may lessen feeding specific concerns, such as picky eating. While reassurance about growth and nutritional outcomes for children perceived as picky eaters is appropriate, clinicians should also consider probing for underlying symptoms of depression that could lead to eating concerns.
Keywords: picky eating, infant feeding, maternal depression, maternal perceptions
INTRODUCTION
Maternal concern about child feeding difficulties is common; up to 50% of mothers report feeding problems in the first 2 years of a child’s life.1 One common type of feeding concern is picky eating, typically measured by maternal report of her child eating a limited variety of foods. Food neophobia, the refusal to accept new foods,2 is often thought of as an integral component of picky eating, and many measures of picky eating include questions about a child’s response to new foods as well as limitations in the variety of foods accepted.3 Though frequently concerning to parents, these behaviors can be part of normal development, and typically emerge in the second year of life, as the child begins to feed autonomously. Accordingly, when concerns about picky eating are brought to medical attention in the context of an otherwise healthy child, the guidance for clinicians is to provide reassurance that pickiness is normal and long term consequences of physiological significance are rare.4 Nevertheless, feeding has been repeatedly shown to carry great emotional weight for famlies.5 Parental concerns about child picky eating are frequently associated with feeding struggles and tantrums,6 conflicts between parents,7 and significant parental distress,8 both during and outside of mealtimes.9
Families living in poverty are exposed to a wide variety of psychosocial stressors. There are well documented socioeconomic and racial/ethnic differences in the content of parental concerns about early feeding10,11 and there is some evidence that concerns about picky eating are more common among low-income mothers.12 Maternal depression, an additional psychological vulnerability for many low-income families, is also associated with negative perceptions of infant emotions and behavior during feeding interactions.13 Transactional models of infant development posit that each partner in the maternal-infant interaction responds to the behavior and affect of the other.14 Thus, negative interpretations on the part of the mother during feeding, whether or not they are due to challenging behavior on the part of the infant, can be sensed by the infant and influence the infant’s behavioral response.15 The infant’s behavior further informs maternal perceptions and concerns in a cycle of mutually reinforcing maladaptive behavior.16 Just as a mother with depressive symptoms may be predisposed to interpret her infant’s behavior negatively, an infant with a challenging temperament can be the source of much distress for a mother in the absence of pre-existing psychosocial vulnerabilities.17 This accounts, in part, for associations between parent emotional distress and non-responsive feeding styles in low-income families.18 Interventions that target problem feeding behavior also rely heavily on supporting a healthy parent-child relationship by teaching parenting self-efficacy, skills in managing difficult child behavior, and strategies for responding to the child’s needs and cues while also providing structure and appropriate limits.19 Maternal depression has been associated with negative perceptions of infant emotions and behavior in general,16 outside of the feeding realm, and is related to a number of adverse child developmental outcomes, particularly in low-income communities. These include language and cognitive difficulties, insecure attachment, social interactive difficulties, and behavior problems.20 Consequently, this dynamic, relational aspect of parent-child interactions is the target of numerous parenting interventions for low-income families,21 a number of which have shown positive impacts on feeding related attitudes and behaviors.22 The Video Interaction Project (VIP), a parenting intervention designed to enhance parent-child interactions through shared reading and play with sustained impacts on child social-emotional development,23 has been shown to significantly reduce maternal depressive symptoms24 and maternal negative perceptions,25 though we have not examined VIP impacts on feeding behaviors or perceived picky eating through these pathways.
Most studies of maternal emotional distress and child feeding have not focused on picky eating in particular,26 and much of the literature on picky eating in young children has been cross-sectional,27 limiting interpretations of directionality. Additionally, though several studies of picky eating have included low-income samples, few have included a large number of Hispanic families,10,28 and most have had predominantly white, middle-class participants.27 This leaves several important gaps in the literature, particularly its generalizability across demographic groups. In addition to limitations in the picky eating literature related to socioeconomic and ethnic diversity, it remains unclear whether picky eating is associated with later detriment to child growth and diet,29,30 the outcomes driving most parental concerns.31 Thus, we aimed to further understand perceived picky eating in a partial longitudinal analysis of low-income, predominantly Hispanic families enrolled in a randomized controlled trial (RTC) of VIP. First, we tested pathways of association between maternal depressive symptoms at infant age 6 months, maternal negative perceptions of the child and interactions with the child at infant age 6 months, and perceived picky eating at child age 14 months while controlling for potential confounders. We hypothesized that maternal depressive symptoms would be associated with perceived picky eating, mediated by maternal negative perceptions. Second, we then analyzed the same data using VIP as a the predictor to determine if receiving VIP impacted perceived picky eating through similar pathways. Finally, we examined perceived picky eating at age 14 months in association with the child’s dietary consumption at age 2 years and growth from ages 6 months to 3 years.
METHODS
Design/Subjects
This secondary analysis of mother-child dyads was nested within an RCT of the VIP intervention, which did not target feeding behaviors as part of its curriculum. Consecutive enrollment of mother-infant dyads occurred in the postpartum unit of an urban public hospital serving low-income, primarily immigrant families, from November, 2005 through October, 2008. Mothers were English or Spanish speaking and at least 18 years of age, with healthy children born full term with planned follow up at the same institution. Full study inclusion and exclusion criteria are published elsewhere.32 After enrollment, participants were randomized to one of three conditions: usual care, VIP, and Building Blocks. Families enrolled in Building Blocks received monthly newsletters and learning materials with written information on general parenting and activity suggestions. For the purposes of the current analysis, the Building Blocks group was combined with the usual care group to constitute a single control group. Families randomized to receive VIP attended individual sessions with a trained interventionist on days of well child visits from birth to age 3 years (15 sessions total, each lasting 30–45 minutes). The interventionist facilitated interactions in play and shared reading through review of videotaped parent-child interactions and collaborative planning for parent-child interactions at home.33 This analysis was restricted to mother-child dyads with complete data for measures of maternal depressive symptoms and maternal negative perceptions at child age 6 months, and perceived picky eating at child age 14 months.
All data were collected by maternal interview in English or Spanish, with the exception of anthropometric measurements, which were obtained by medical record review. Bilingual research assistants administered the interviews at baseline (immediately postpartum), and at infant ages 6, 14, and 24 months. All survey items were read aloud to maximize validity of data obtained from mothers with low literacy. Informed, written consent was obtained prior to study participation. Approval to conduct human subjects research was granted by Institutional Review Boards at Bellevue Hospital Center and the New York University School of Medicine. The study was registered on clinicaltrials.gov ().
Measures
Perceived picky eating
Maternal perception of child picky eating was measured at child age 14 months by the Reaction to Food subscale of the Colorado Children’s Temperament Inventory.34 This subscale asked the mother to rate her child on a series of five items about the child’s typical responses to food and includes items common across picky eating scales, including items related to food neophobia.35 Items included 1) “Rarely took a new food without fussing;” 2) “Child consistently dislikes many kinds of foods;” 3) “Child makes faces at new foods;” 4) “Once the child decides he doesn’t like something, there is no getting him to like it;” and 5) “Child has strong likes and dislikes in food.” Responses were based on a 5 point Likert scale ranging from 1 (“not at all like my child”) to 5 (“a lot like my child”). Scores for each item were summed resulting in a cumulative score of 5 to 25 with higher scores indicative of more perceived pickiness.
Maternal depressive symptoms
Maternal depressive symptoms were measured by the Patient Health Questionnaire (PHQ-9)36 administered at child age 6 months. The PHQ-9 is a 9 item depression screen in which the respondent reports how frequently she has experienced symptoms such as “Little interest or pleasure in doing things” in the last 2 weeks. Response options for each item include “not at all,” “several days,” “more than half the days,” or “nearly every day,” scored as 0 to 3 points. Items are summed to give a total score that can range from 0 to 27 with a score greater than 4 representing mild to moderate depressive symptoms.
Maternal negative perceptions
Maternal negative perceptions of her child were measured using the Parent-Child Dysfunctional Interaction subscale of the Parenting Stress Index-Short Form,37 administered at child age 6 months. This assessment measures parent perceptions that the child does not meet expectations and that interactions are not rewarding. It consists of 12 items, such as “When I do things for my child, I get the feeling that my efforts are not appreciated very much” and “Sometimes my child does things that bother me just to be mean.” Each item is scored on a Likert scale of strongly disagree to strongly agree and item scores are summed, resulting in a total score ranging from 12 to 60. A score greater than 25 is considered severe dysfunction necessitating clinical attention.
Child diet composition
Child diet composition was measured at age 2 years using an adapted 17-item food frequency questionnaire (FFQ).38 The FFQ asked mothers to report how often her child eats a particular food, such as fruit, vegetables, or juice. Response options were daily, weekly, monthly, or rarely. Based on the frequency distribution of responses, we collapsed responses of monthly and rarely into a single category.
Child growth
Anthropometric data for each child were gathered from the child’s electronic medical record. We generated body mass index z-scores (BMIz) for each child at ages 6 months, 14 months, 2 years, and 3 years using the formula BMI=kg/m2 and World Health Organization (WHO) reference standards. Data flagged as biologically implausible (z scores greater than 5 standard deviations from the median) were removed.39 BMIz at ages 6 and 14 months were calculated using the closest set of paired measurements (weight and length) available within two months of those ages. BMIz at ages 2 and 3 years were calculated using the closest set of paired measurements available within three months of the 2nd or 3rd birthday, respectively.
Covariates
Family socio-demographic data were collected at the baseline interview immediately following enrollment. These included maternal age, marital status (dichotomized as single versus married or living with a partner), education (dichotomized as completed high school versus completed less than high school), and ethnicity (dichotomized as Hispanic versus non-Hispanic), as well as child sex and birth order. Measures of additional psychosocial risk factors known to affect maternal depressive symptoms and parent-child interactions were also assessed in the baseline survey. Families were considered to be at increased psychosocial risk if the mother reported one or more of the following: experienced violent victimization or had child protection agency contact in the last two years, significant financial hardship in the last 12 months, ever having been homeless, or cigarette smoking or alcohol use during pregnancy. Food insecurity was assessed at child age 6 months by items adapted from the United States Department of Agriculture core food insecurity module. Families were classified as food insecure if the mother reported that there was not enough food sometimes or often in the last four months.40
Statistical analyses
We performed univariate analyses to characterize the full analytic sample and bivariate analyses to evaluate for differences between participants who received the VIP intervention, and those who did not. We used Pearson’s correlations to examine correlations between socio-demographic covariates and our three main study variables (maternal depressive symptoms, maternal negative perceptions, and perceived picky eating). We then used this bivariate correlation matrix to guide the selection of covariates for structural equation models. The first structural equation model (Model 1A) tested our hypothesized pathway beginning with maternal depressive symptoms at infant age 6 months influencing perceived picky eating at child age 14 months, mediated by maternal negative perceptions at infant age 6 months. We then tested a similar model (Model 2A) in which receipt of the VIP intervention was treated as the predictor of perceived picky eating, operating through maternal depressive symptoms and negative perceptions. For both models, we first tested our hypothesized pathway of maternal negative perceptions mediating the relation between maternal depressive symptoms and perceived picky eating. We then tested the alternative pathway (Models 1B and 2B) in which maternal depressive symptoms mediated the relation between maternal negative perceptions and perceived picky eating. In all models we controlled for the effects of psychosocial risk and food insecurity on maternal depressive symptoms, and for the effects of maternal age, ethnicity, education, and food insecurity on negative maternal perceptions. We assessed model fit using χ2, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), comparative fit index (CFI), Akaike information criterion (AIC), and Bayes information criterion (BIC). For χ2, RMSEA, SRMR, AIC, and BIC, lower values indicate better fit. Generally accepted cutoffs for acceptable model fit include an RMSEA < 0.06, SRMR ≤ 0.08, and CFI ≥ 0.95. AIC and BIC do not have specific cutoffs and are used to compare fit between similar models.41
To answer our final research questions, we tested associations between perceived picky eating and two potential correlates of picky eating: dietary consumption at age 2 years and child BMIz from age 6 months to 3 years. For dietary analyses, we used multinomial logistic regression with food frequency of each food item (daily, weekly, monthly/rarely) as the dependent variable and perceived picky eating score as the independent variable. For growth analyses, we first used simple and multivariable linear regression to model BMIz at each of four time points (age 6 months, 14 months, 2 years, and 3 years). We then used multilevel growth curve modeling to estimate BMIz trajectories, including data from all four time points within the same model, centered at age 14 months. We performed unadjusted and adjusted multilevel analyses, each with two steps. Step 1 of the multilevel model included time, time-squared (to account for the nonlinear effect of time on BMIz) and perceived picky eating as independent predictors of BMIz. Step 2 added a time by picky eating interaction term. In this way, we were able to estimate the impact of perceived picky eating on two features that define growth over time: 1) The mean initial level (the BMIz at age 14 months) of growth trajectories in Step 1; and 2) The mean slope (the change in BMIz over time) of growth trajectories in Step 2. All multivariable models adjusted for the same set of covariates as described above. Linear regression models predicting BMIz at ages 14 months, 2 and 3 years also adjusted for the child’s BMIz at the preceding timepoint. We defined statistical significance as p<0.05 for all analyses.
RESULTS
Our analytic sample contained 187 primarily Hispanic mother-child dyads. Sample characteristics are summarized in Table 1. Mean PHQ9 score was 3 (SD 3.8) with one quarter of the sample meeting the threshold for mild depressive symptoms with a score of 5 or more. Mean maternal negative perception score was 15.4 (SD 4) and mean perceived picky eating score was 12.3 (SD 5.4), similar to distribution statistics in other healthy samples.34,37 Participants receiving the VIP intervention had significantly lower mean scores for perceived picky eating (10.9 vs 12.8, p=0.03) as compared to participants who did not receive the intervention. Pearson’s correlations between covariates and our three primary study variables are shown in Table 2. Baseline psychosocial risk and food insecurity were significantly associated with higher maternal depressive symptom scores; Hispanic ethnicity and food insecurity were significantly associated with higher maternal negative perception scores, and maternal age and high school graduation were significantly associated with lower negative perception scores.
Table 1.
Descriptive statistics for family characteristics and main study variables in 187 mother-child dyads by intervention status.
| All(n=187) | Not receiving intervention (n=134) | Receiving intervention (n=53) | |
|---|---|---|---|
| n (%) or mean (SD) | |||
| Family characteristics | |||
| Age, years | 28.0 (5.0) | 27.7 (5.2) | 28.5 (4.6) |
| Hispanic | 180 (96%) | 129 (96%) | 51 (96%) |
| Completed high school | 75 (40%) | 54 (40%) | 21 (40%) |
| Married or living as married | 161 (86%) | 117 (87%) | 44 (83%) |
| Psychosocial riska | 36 (19%) | 23 (17%) | 13 (25%) |
| Food insecureb | 20 (11%) | 13 (10%) | 7 (13%) |
| Child firstborn | 68 (36%) | 50 (37%) | 18 (34%) |
| Child female | 99 (53%) | 70 (52%) | 59 (55%) |
| Primary predictors | |||
| Maternal depressive symptomsc, d | 3.0 (3.8) | 3.3 (4.1) | 2.0 (2.6) |
| Maternal negative perceptionse, d | 15.4 (4.0) | 15.7 (4.2) | 14.4 (3.2) |
| Primary outcome | |||
| Perceived picky eatingf, d | 12.3 (5.4) | 12.8 (5.6) | 10.9 (4.9) |
Presence of one or more of the following as reported at baseline (immediately postpartum): physical abuse or child protection agency contact in the last two years, significant financial hardship in the last 12 months, ever having been homeless, or cigarette smoking or alcohol use during pregnancy
Not enough food sometimes or often in the last four months as reported at infant age 6 months.
Patient Health Questionnaire 9 administered to the mother at infant age 6 months; Possible range 0–27, with higher scores indicated more depressive symptoms.
p < 0.05 for between group difference using t-tests.
Parent-Child Dysfunctional Interaction subscale of the Parenting Stress Index – Short Form administered to the mother at infant age 6 months; Possible range 12–60, with higher scores indicating more negative perceptions.
Reaction to Food subscale of the Colorado Children’s Temperament Index administered to the mother at infant age 14 months; Possible range 5–25, with higher scores indicating more perceived pickiness.
Table 2.
Pearson’s correlations of family characteristics and main study variables.
| Maternal depressive symptoms | Maternal negative perceptions | Perceived picky eating | |
|---|---|---|---|
| Age, years | −0.01 | −0.13* | 0.07 |
| Hispanic | −0.02 | 0.10* | −0.01 |
| Completed high school | 0.05 | −0.18*** | −0.06 |
| Married or living as married | −0.04 | 0.02 | −0.04 |
| Psychosocial risk | 0.24*** | −0.02 | −0.002 |
| Food insecure | 0.19*** | 0.17*** | −0.002 |
| Child firstborn | 0.03 | 0.01 | −0.07 |
| Child female | −0.01 | 0.04 | 0.10 |
p<0.05
p<0.01
p<0.001
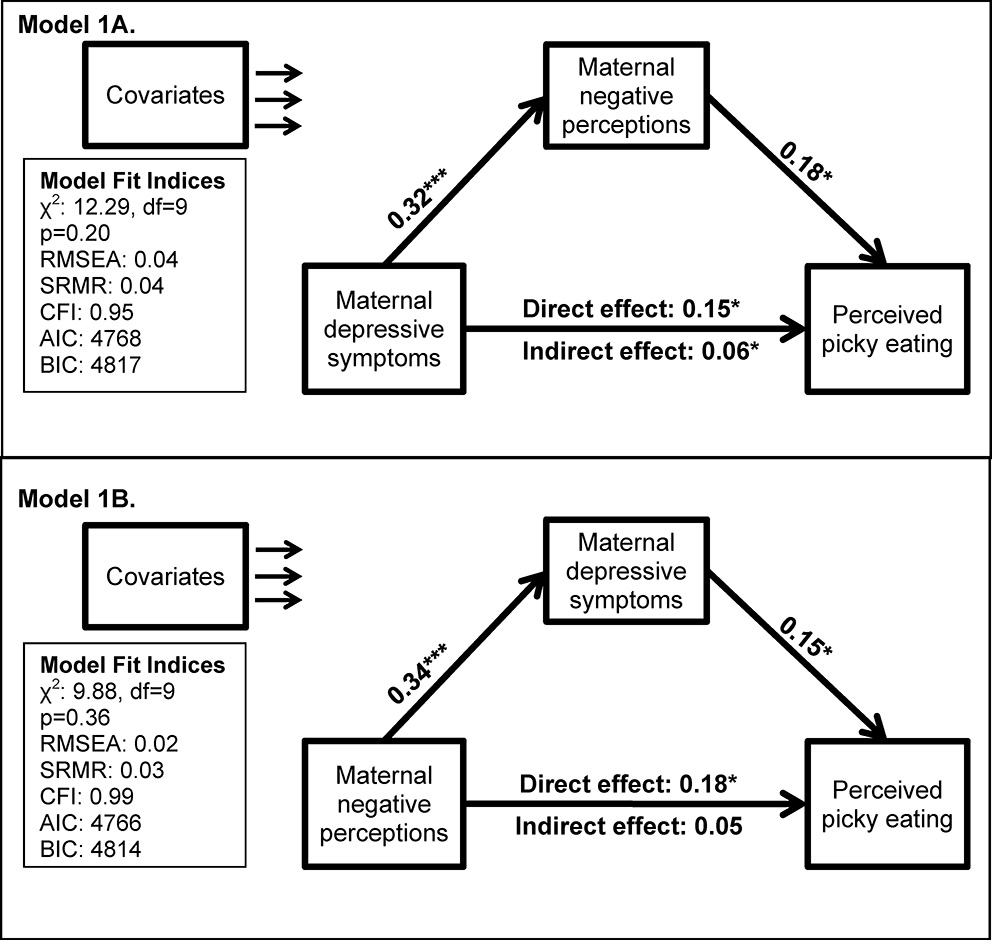
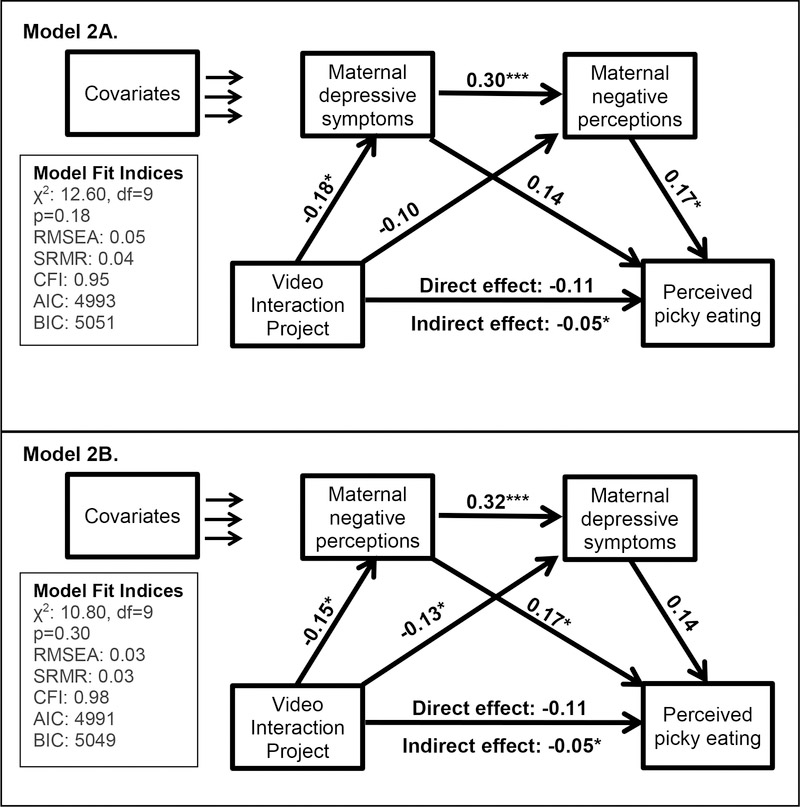
Results of our two hypothesized and two alternative structural equation models are shown in Table 3 and Figure 1. In our first hypothesized model (Figure 1: Model 1A), maternal depressive symptoms at child age 6 months had a significant and positive direct effect on perceived picky eating at child age 14 months (β=0.15, p=0.046). Maternal negative perceptions at child age 6 months also had a significant and positive direct effect on perceived picky eating at child age 14 months (β=0.18, p=0.02). The indirect effect of maternal depressive symptoms on perceived picky eating through maternal negative perceptions was small but significant (β=0.06, p=0.04), indicating partial mediation. Model fit statistics indicated acceptable fit so the model was not modified. We then tested the alternative model in which the direction of effect between depressive symptoms and negative perception was reversed (Figure 1: Model 1B). In this model, maternal negative perceptions had a significant total effect (β=0.23, p<0.01) and direct effect (β=0.18, p=0.02) on perceived picky eating but had a small indirect effect that was not statistically significant (β=0.05, p=0.06). Model fit was slightly better than that of Model 1A. Associations between depressive symptoms and perceived picky eating as well as between negative perceptions and depressive symptoms were similar in magnitude and significance to what was seen in Model 1A. When VIP was used as the predictor variable (Models 2A and 2B), similar results to the first set of models were obtained. Receipt of the VIP intervention impacted perceived picky eating through its effects on maternal depressive symptoms and negative perceptions (Model 2A: total effect: β=−0.16, p=0.02; indirect effect: β=−0.05, p=0.02). When the direction of effect between maternal depressive symptoms and negative perceptions was reversed (Model 2B), effects of VIP on perceived picky eating were the same, and model fit was slightly improved.
Table 3.
Standardized effects of maternal depressive symptoms, maternal negative perceptions, and receipt of VIP intervention on perceived picky eating and mediating variables in four structural equations modelsa
| Model 1A | Model 1B | Model 2A | Model 2B | |
|---|---|---|---|---|
| Depressive symptoms | ||||
| →Negative perceptions | 0.32*** | -- | 0.30*** | -- |
| →Perceived picky eating | ||||
| Direct | 0.15* | 0.15* | 0.14 | 0.14 |
| Indirect | 0.06* | -- | 0.05* | -- |
| Total | 0.21** | 0.15* | 0.19* | 0.14 |
| Negative perceptions | ||||
| →Depressive symptoms | -- | 0.34*** | -- | 0.32*** |
| →Perceived picky eating | ||||
| Direct | 0.18* | 0.18* | 0.17* | 0.17* |
| Indirect | -- | 0.05 | -- | 0.04 |
| Total | 0.18* | 0.23** | 0.17* | 0.21** |
| VIP intervention | ||||
| →Depressive symptoms | -- | -- | −0.18* | −0.13* |
| →Negative perceptions | -- | -- | −0.10 | −0.15* |
| →Perceived picky eating | ||||
| Direct | -- | -- | −0.11 | −0.11 |
| Indirect (via depressive symptoms and negative perceptions) | -- | -- | −0.05* | −0.05* |
| Indirect (via depressive symptoms) | -- | -- | −0.02 | −0.02 |
| Indirect (via negative perceptions) | -- | -- | −0.02 | −0.02 |
| Total | -- | -- | −0.16* | −0.16* |
| Model fit indices | ||||
| χ2 (df 9) | 12.29 | 9.88 | 12.60 | 10.80 |
| p-value | 0.20 | 0.36 | 0.18 | 0.30 |
| RMSEA | 0.04 | 0.02 | 0.05 | 0.03 |
| SRMR | 0.04 | 0.03 | 0.04 | 0.03 |
| CFI | 0.95 | 0.99 | 0.95 | 0.98 |
| AIC | 4768 | 4766 | 4993 | 4991 |
| BIC | 4817 | 4814 | 5051 | 5049 |
See Figure 1 for diagrams of the four structural equation models shown in this table
p<0.05
p<0.01
p<0.001
df: Degrees of freedom; RMSEA: Root mean square error of approximation; SRMR: Standardized root mean square residual; CFI: Comparative fit index; AIC: Akaike Information Criterion; BIC: Bayes Information Criterion.
Figure 1.
Direct and indirect effects of maternal depressive symptoms (infant age 6 months), maternal negative perceptions (infant age 6 months), and receipt of the Video Interaction Project (VIP) intervention on perceived picky eating (child age 14 months) in 187 mother-child dyads. Estimates were obtained using structural equation modeling and are presented as standardized regression coefficients (β). All models adjust for effects of maternal age, ethnicity, education, and food insecurity on maternal negative perceptions as well as effects of baseline psychosocial risk and food insecurity on maternal depressive symptoms. Model 1A. Maternal depressive symptoms had significant positive effects on perceived picky eating directly and indirectly through effects on maternal negative perceptions. Model 1B. Model fit was slightly improved by reversing the directionality of the association between maternal negative perceptions and maternal depressive symptoms in predicting perceived picky eating. While negative perceptions and depressive symptoms both have significant direct effects on perceived picky eating in this model, negative perceptions do not impact perceived picky eating through depressive symptoms. Models 2A and 2B. The VIP intervention led to lower perceived picky eating scores indirectly through protective effects on maternal depressive symptoms and maternal negative perceptions. The magnitude and significance of this effect was similar whether maternal depressive symptoms preceded negative perceptions (Model 2A) or maternal negative perceptions preceded depressive symptoms (Model 2B), with slightly improved model fit for the latter.
*p<0.05, **p<0.01, ***p<0.001; df: Degrees of freedom; RMSEA: Root mean square error of approximation; SRMR: Standardized root mean square residual; CFI: Comparative fit index; AIC: Akaike Information Criterion; BIC: Bayes Information Criterion.
Dietary data at age 2 years was available for 128 of the 187 children. These 128 families were more likely to be in the intervention group of the RCT (38% vs 9%, Chi-square 16.8, p<0.01) and were less likely to have baseline psychosocial risk (15% vs 29%, Chi-square 5.07, p=0.03) as compared to the 59 families with missing dietary data. Anthropometric data was available for construction of growth trajectories for 172 of the 187 children in the sample. The 15 subjects who had no anthropometric data within the specified time periods were not significantly different from the rest of the sample on any other study variables when compared in Chi square and t-test analyses.
Relative risk ratios of daily versus weekly versus monthly or rare consumption of each food item are reported in Table 4. There was no evidence of an association between perceived pickiness and frequency of dietary consumption of any item. Linear regression and multilevel modeling results testing associations between perceived picky eating and child growth are shown in Table 5. BMIz at age 6 months was not predictive of perceived picky eating at age 14 months in unadjusted (B=0.28, p=0.50) or adjusted analyses (B=0.26, p=0.54). Similarly, perceived picky eating was not significantly associated with BMIz at 14 months, 2 years, or 3 years when tested individually, nor was it associated with differences in level (predicted BMIz at age 14 months) or slope (change in BMIz over time) of child growth trajectories predicted by including all four time points into multilevel models.
Table 4.
Effects of perceived picky eating score at age 14 months on frequency of food consumption at age 2 years.
| N | % | RRR (95% CI)a | aRRR (95% CI)b | |
|---|---|---|---|---|
|
| ||||
| Vegetable or salad | ||||
| Daily | 58 | 45% | Ref. | Ref. |
| Weekly | 60 | 47% | 1.01 (0.95, 1.07) | 1.02 (0.95, 1.09) |
| Monthly/Rarely | 10 | 8% | 1.09 (0.42, 2.04) | 1.09 (0.96, 1.23) |
|
| ||||
| Fruit | ||||
| Daily | 115 | 90% | Ref. | Ref. |
| Weekly | 13 | 10% | 1.07 (0.97, 1.18) | 1.06 (0.96, 1.18) |
| Monthly/Rarely | 0 | -- | -- | -- |
|
| ||||
| Sugar sweetened beverages | ||||
|
| ||||
| Juice | ||||
| Daily | 93 | 73% | Ref. | Ref. |
| Weekly | 28 | 22% | 1.05 (0.98, 1.14) | 1.05 (0.97, 1.13) |
| Monthly/Rarely | 7 | 5% | 0.89 (0.75, 1.06) | 0.85 (0.69, 1.05) |
|
| ||||
| Soda, tea (including iced tea), Kool-aid | ||||
| Daily | 14 | 11% | Ref. | Ref. |
| Weekly | 37 | 29% | 0.95 (0.86, 1.06) | 0.94 (0.84, 1.06) |
| Monthly/Rarely | 77 | 60% | 0.95 (0.86, 1.05) | 0.95 (0.86, 1.05) |
|
| ||||
| Sweets | ||||
|
| ||||
| Cake, cookies, candy | ||||
| Daily | 19 | 15% | Ref. | Ref. |
| Weekly | 80 | 63% | 0.99 (0.90, 1.08) | 0.99 (0.90, 1.08) |
| Monthly/Rarely | 29 | 23% | 0.99 (0.89, 1.09) | 0.98 (0.87, 1.09) |
|
| ||||
| Added fats | ||||
|
| ||||
| Chips, nachos | ||||
| Daily | 10 | 8% | Ref. | Ref. |
| Weekly | 76 | 59% | 0.96 (0.85, 1.08) | 0.96 (0.85, 1.09) |
| Monthly/Rarely | 42 | 33% | 0.94 (0.83, 1.06) | 0.94 (0.83, 1.07) |
|
| ||||
| Fried foods | ||||
| Daily | 4 | 3% | Ref. | Ref. |
| Weekly | 73 | 57% | 1.00 (0.83, 1.19) | 1.00 (0.85, 1.18) |
| Monthly/Rarely | 51 | 40% | 0.99 (0.82, 1.18) | 0.99 (0.84, 1.18) |
RRR: Relative risk ratio predicted by multinomial logistic regression
aRRR: Adjusted relative risk ratio predicted by multivariable multinomial logistic regression, controlling for maternal ethnicity, education, marital status, social risk, food insecurity, depressive symptoms, as well as child sex and birth order.
Table 5.
Effects of perceived picky eating on BMI z-scores using multilevel modeling and linear regression.
| Unadjusted estimate | Adjusted estimatea | ||||
|---|---|---|---|---|---|
| B (95% CI) | p-value | B (95% CI) | p-value | ||
| Linear Regression Models Predicting BMIz at Each Age | |||||
| 14 monthsb | Perceived picky eating | 0.02 (−0.01, 0.05) | 0.17 | 0.02c (−0.01, 0.05) | 0.20 |
| 2 Years d | Perceived picky eating | −0.004 (−0.04, 0.03) | 0.80 | 0.004c (−0.03, 0.03) | 0.88 |
| 3 Years e | Perceived picky eating | 0.01 (−0.02, 0.05) | 0.45 | 0.001c (−0.03, 0.02) | 0.93 |
| Multilevel Model Predicting BMIz Trajectory Across Age (n=180) f | |||||
| Step 1 | Time (age in months)g | 0.03 (0.03, 0.04) | <0.01 | 0.03 (0.03, 0.04) | <0.01 |
| Perceived picky eating | 0.006 (−0.02, 0.03) | 0.61 | 0.004 (−0.02, 0.03) | 0.74 | |
| Step 2 | Time × Perceived picky eating | −0.0001 (−0.001, 0.001) | 0.88 | −0.0001(−0.001, 0.001) | 0.88 |
Controlling for maternal ethnicity, education, marital status, social risk, food insecurity, depressive symptoms, negative perceptions, as well as child sex, birth order, and intervention status.
n=154 for unadjusted analysis and n=132 for adjusted analysis.
Also controls for BMI z-score at the preceding time point.
n=140 for unadjusted analysis and n=122 for adjusted analysis.
n=113 for unadjusted analysis and n=97 for adjusted analysis.
Time is centered at 14 months so that coefficient of perceived picky eating can be interpreted as the increase in BMI z-score for every unit increase in perceived picky eating score at age 14 months.
Quadratic term (time × time) also included in the model to account for nonlinear effect of time.
DISCUSSION
In this partial longitudinal study of low-income, predominantly Hispanic families, we found that maternal depressive symptoms and negative perceptions of interactions with her child at child age 6 months were associated with perceived picky eating at child age 14 months. In all models, maternal negative perceptions of interactions with her child were directly associated with perceived picky eating, regardless of whether the negative perceptions were modeled as a cause or as a consequence of maternal depressive symptoms. VIP, a general parenting intervention without feeding related curriculum components, led to lower perceived picky eating scores, partially mediated by its beneficial effect on maternal depressive symptoms and negative perceptions. These associations were independent of maternal age, ethnicity, education, psychosocial risk, and food insecurity. Perceived picky eating at child age 14 months was not associated with excessive or inadequate dietary consumption of foods at age 2 years or with child adiposity from 6 months to 3 years.
Our findings add to the literature on child picky eating by interpreting maternal perceptions of child feeding behavior within a longitudinal transactional model of the parent-child relationship in an understudied population. This transactional model recognizes the complex interplay between individual characteristics of the mother and of the child over time.14 This is consistent with other studies of parenting and picky eating outside of the maternal depression literature. Steinsbekk et al., for example, conducted a longitudinal study of Norwegian parent-child pairs and found that parental sensitivity, defined as the parent’s awareness and responsiveness to the child’s cues, was associated with higher odds of subsequent picky eating. While parental sensitivity is typically thought of as beneficial, in the context of difficult feeding, highly sensitive parents may avoid attempting to feed new or challenging foods to their child, further contributing to the child’s pickiness.42 Our findings similarly suggest that concerns about picky eating may be influenced by the maternal psychological milieu and patterns of interactions with her infant beginning at an early age.
The current findings extend previous research linking depressive symptoms to negative perceptions of child behavior43 by showing that these negative perceptions, whether cause or result of maternal depressive symptoms, may go on to influence specific concerns about feeding and eating. Maternal depressive symptoms have also been associated with nonresponsive feeding styles, including pressuring, controlling, and restriction,13 which may further exacerbate the child’s picky eating behavior, if present.44 Our results offer empirical evidence that an intervention promoting healthy child development by enhancing the parent-child relationship can have broader effects on maternal perceptions specific to eating. Given its previously demonstrated impacts on maternal depressive symptoms24 and negative perceptions,25 it is not surprising that effects on perceived picky eating operate, in part, through this pathway.
We found that maternal perception of child picky eating at age 14 months was not associated with excessive or inadequate consumption of particular foods at age 2 or with child growth parameters from child age 6 months to 3 years. These findings are consistent with our conceptualization of perceived picky eating as a reflection, in part, of the parent-child relationship, rather than solely as a marker of problematic child feeding behavior. The absence of associations with weight and diet also suggests that on average, perceived picky eating in our primary-care, clinic-based sample, likely falls at the mild end of a spectrum of feeding behavior that ranges from common, developmentally normal, transient pickiness to rare cases of extreme food avoidance and refusal.30 Though the literature is mixed, numerous other studies of perceived pickiness in young children have also found no significant associations with subsequent growth and diet.27 In light of our findings, while it is appropriate to provide reassurance to parents whose children have normal growth trajectories and dietary intakes, reassurance alone may overlook the importance of the parental concern itself, missing an opportunity to address maternal depressive symptoms or other maladaptive strategies and perceptions that may have consequences outside of the feeding domain.
Our findings should be interpreted within the context of several limitations. Our sample was composed of low-income, primarily Hispanic families, and may not be generalizable to other populations. Our cross-sectional measurement of maternal depressive symptoms and negative perceptions make it difficult to interpret the direction of association between these two highly correlated constructs, reinforced by the fact that there was little difference in model fit between our hypothesized model and the alternative. Additionally, we did not measure maternal concerns about infant feeding prior to age 14 months, therefore, we were unable to capture whether feeding concerns may have preceded maternal depressive symptoms and negative perceptions, rather than the other way around. Indeed there are certainly child factors, such as sensory sensitivity42 and temperamental emotionality,45 that are known to correlate with picky eating. One complicating factor in assessing these child factors in our study and many others is the reliance on maternal report for measuring these constructs. Future longitudinal studies should further explore these child driven contributions to maternal infant feeding interactions using objective measures in addition to maternal report.
CONCLUSIONS
These findings have significant implications for clinicians caring for young children. Maternal concerns about picky eating are common and may reflect deeper symptoms of distress and maladaptive behavior within the family unit. Maternal depressive symptoms and dysfunction in the parent-child relationship are not frequently brought to medical attention but are amenable to treatment once identified. Therefore, clinicians should consider probing deeper about the etiology of parental concerns prior to offering reassurance about growth and nutrition. Participation in programs to enhance the parent-child relationship may lessen these concerns through impacts on maternal well-being. Further study to more deeply understand the complex interrelations between child eating behavior and maternal perceptions of child health in the context of maternal depressive symptoms is warranted, and findings could inform future interventions to enhance optimal parent-child interactions and subsequent health outcomes.
Acknowledgments
Sources of support: MK was supported in part by the Health Resources & Services Administration (T32HP22238) and the National Center for Advancing Translational Sciences (UL1TR001445 [to the NYU Langone Health CTSI]). This study was also supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (HD047740 01–04; HD047740 05–09; HD047740 08S1) and the Tiger Foundation, Marks Family Foundation, Children of Bellevue, Inc., KiDS of NYU Foundation, Inc., and the NY City Council.
Footnotes
Author disclosure statement: Authors have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Bryant-Waugh R, Markham L, Kreipe RE, et al. Feeding and eating disorders in childhood. Int J Eat Disord. 2010;40. [DOI] [PubMed] [Google Scholar]
- 2.Boquin M, Smith Simpson S, Donovan SM, et al. Mealtime behaviors and food consumption of perceived picky and nonpicky eaters through home use test. J Food Sci. 2014;79(12):S2523–S2532. [DOI] [PubMed] [Google Scholar]
- 3.Dovey TM, Staples PA, Gibson EL, et al. Food neophobia and “picky/fussy” eating in children: A review. Appetite. 2008;50(2–3):181–193. doi: 10.1016/j.appet.2007.09.009 [DOI] [PubMed] [Google Scholar]
- 4.Lumeng JC. Picky Eating. In: Parker S, Zuckerman BS, Augustyn M, eds. Developmental and Behavioral Pediatrics: A Handbook for Primary Care. 2nd ed.; 2005.
- 5.Johnson SL, Goodell LS, Williams K, et al. Getting my child to eat the right amount. Mothers’ considerations when deciding how much food to offer their child at a meal. Appetite. 2015;88:24–32. doi: 10.1016/j.appet.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 6.Mascola AJ, Bryson SW, Agras WS. Picky eating during childhood: a longitudinal study to age 11 years. Eat Behav. 2010;11(4):253–257. doi: 10.1016/j.eatbeh.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobi C, Agras WS, Bryson S, et al. Behavioral validation, precursors, and concomitants of picky eating in childhood. J Am Acad Child Adolesc Psychiatry. 2003;42(1):76–84. doi: 10.1097/00004583-200301000-00013 [DOI] [PubMed] [Google Scholar]
- 8.Harris HA, Ria-Searle B, Jansen E, et al. What’s the fuss about? Parent presentations of fussy eating to a parenting support helpline. Public Health Nutr. 2018;120(8):1–9. doi: 10.1017/S1368980017004049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goh DYT, Jacob A. Perception of picky eating among children in Singapore and its impact on caregivers: a questionnaire survey. Asia Pac Fam Med. 2012;11(1):5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evans A, Seth JG, Smith S, et al. Parental feeding practices and concerns related to child underweight, picky eating, and using food to calm differ according to ethnicity/race, acculturation, and income. Matern Child Health J. 2011;15(7):899–909. doi: 10.1007/s10995-009-0526-6 [DOI] [PubMed] [Google Scholar]
- 11.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc. 2004;104(2):215–221. doi: 10.1016/j.jada.2003.11.012 [DOI] [PubMed] [Google Scholar]
- 12.Dubois L, Farmer A, Girard M, et al. Problem eating behaviors related to social factors and body weight in preschool children: A longitudinal study. Int J Behav Nutr Phys Act. 2007;4(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savage JS, Birch LL. WIC mothers’ depressive symptoms are associated with greater use of feeding to soothe, regardless of perceived child negativity. Pediatr Obes. 2017;12(2):155–162. doi: 10.1111/ijpo.12122 [DOI] [PubMed] [Google Scholar]
- 14.Tronick EZ. Emotions and emotional communication in infants. Am Psychol. 1989;44(2):112–119. doi: 10.1037/0003-066X.44.2.112 [DOI] [PubMed] [Google Scholar]
- 15.Ammaniti M, Lucarelli L, Cimino S, et al. Maternal psychopathology and child risk factors in infantile anorexia. Int J Eat Disord. 2009;43(3). doi: 10.1002/eat.20688 [DOI] [PubMed] [Google Scholar]
- 16.Gross D, Conrad B, Fogg L, et al. A longitudinal model of maternal self-efficacy, depression, and difficult temperament during toddlerhood. Res Nurs Health. 1994;17(3):207–215. http://www.ncbi.nlm.nih.gov/pubmed/8184132. [DOI] [PubMed] [Google Scholar]
- 17.Tatano C A Meta-analysis of the relationship between postpartum depression and infant temperament. Nurs Res. 1996;45(4):225–230. [DOI] [PubMed] [Google Scholar]
- 18.Hughes SO, Power TG, Liu Y, et al. Parent emotional distress and feeding styles in low-income families. The role of parent depression and parenting stress. Appetite. 2015;92(C):337–342. doi: 10.1016/j.appet.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Satter E The feeding relationship: Problems and interventions. J Pediatr. 1990;117(2 PART 2). doi: 10.1016/S0022-3476(05)80017-4 [DOI] [PubMed] [Google Scholar]
- 20.Petterson SM, Albers AB . Effects of poverty and maternal depression on early child development. Child Development. https://onlinelibrary.wiley.com/doi/pdf/10.1111/1467-8624.00379. Accessed April 16, 2019. [DOI] [PubMed]
- 21.Cates CB, Weisleder A, Mendelsohn AL. Mitigating the effects of family poverty on early child development through parenting interventions in primary care. Acad Pediatr. 2016;16(3):S112–S120. doi: 10.1016/j.acap.2015.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerards SMPLPL, Sleddens EFCC, Dagnelie PC, et al. Interventions addressing general parenting to prevent or treat childhood obesity. Int J Pediatr Obes. 2011;6(2–2):e28–e45. doi: 10.3109/17477166.2011.575147 [DOI] [PubMed] [Google Scholar]
- 23.Cates CB, Weisleder A, Berkule Johnson S, et al. Enhancing parent talk, reading, and play in primary care: Sustained impacts of the Video Interaction Project. J Pediatr. 2018;199:49–56.e1. doi: 10.1016/j.jpeds.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkule SB, Cates CB, Dreyer BP, et al. Reducing maternal depressive symptoms through promotion of parenting in pediatric primary care. Clin Pediatr (Phila). 2014;53(5):460–469. doi: 10.1177/0009922814528033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cates CB, Weisleder A, Dreyer BP, et al. Leveraging healthcare to promote responsive parenting: Impacts of the Video Interaction Project on parenting stress. J Child Fam Stud. 2016;25(3):827–835. doi: 10.1007/s10826-015-0267-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Behadli AF, Sharp C, Hughes SO, et al. Maternal depression, stress and feeding styles: towards a framework for theory and research in child obesity. Br J Nutr. 2015;113(2015):S55–S71. doi: 10.1017/S000711451400333X [DOI] [PubMed] [Google Scholar]
- 27.Cole NC, An R, Lee SY, et al. Correlates of picky eating and food neophobia in young children: a systematic review and meta-analysis. Nutr Rev. 2017;75(7):516–532. [DOI] [PubMed] [Google Scholar]
- 28.Horodynski MA, Stommel M, Brophy-Herb H, et al. Low-income African American and non-Hispanic White mothers’ self-efficacy, “picky eater” perception, and toddler fruit and vegetable consumption. Public Health Nurs. 2010;27(5):408–417. [DOI] [PubMed] [Google Scholar]
- 29.Brown CL, Vander Schaaf EB, Cohen GM, et al. Association of picky eating and food neophobia with weight: A Systematic review. Child Obes. 2016;12(4):247–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor CM, Wernimont SM, Northstone K, et al. Picky/fussy eating in children: Review of definitions, assessment, prevalence and dietary intakes. Appetite. 2015;95:349–359. doi: 10.1016/j.appet.2015.07.026 [DOI] [PubMed] [Google Scholar]
- 31.Boquin MM, Moskowitz HR, Donovan SM, et al. Defining perceptions of picky eating obtained through focus groups and conjoint analysis. J Sens Stud. 2014;29(2):126–138. doi: 10.1111/joss.12088 [DOI] [Google Scholar]
- 32.Mendelsohn AL, Huberman HS, Berkule SB, et al. Primary Care Strategies for Promoting Parent-Child Interactions and School Readiness in At-Risk Families. Arch Pediatr Adolesc Med. 2011;165(1):33–41. doi: 10.1001/archpediatrics.2010.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mendelsohn AL, Dreyer BP, Brockmeyer CA, et al. Randomized controlled trial of primary care pediatric parenting programs: Effect on reduced media exposure in infants, mediated through enhanced parent-child interaction. Arch Pediatr Adolesc Med. 2011. doi: 10.1001/archpediatrics.2010.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rowe DC, Plomin R. Temperament in early childhood. J Pers Assess. 1977;41(2):150–156. doi: 10.1207/s15327752jpa4102_5 [DOI] [PubMed] [Google Scholar]
- 35.Wardle J, Guthrie CA, Sanderson S, et al. Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psychiatry. 2001;42(7):963–970. doi: 10.1111/1469-7610.00792 [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Whiteside-Mansell L, Ayoub C, McKelvey L, et al. Parenting stress of low-income parents of toddlers and preschoolers: Psychometric properties of a Short Form of the Parenting Stress Index. Parenting. 2007;7(1):27–56. doi: 10.1080/15295190709336775 [DOI] [Google Scholar]
- 38.Stang J, Story M. Nutrition screening, assessment and intervention In: Story M, Holt K, Sofka D, eds. Guidelines for Adolescent Nutrition Services. Center for Leadership, Education and Training in Maternal and Child Nutrition; 2005:35–54. [Google Scholar]
- 39.World Health Organization (WHO). WHO Anthro (version 3.2.2, January 2011) and macros. 2011. http://www.who.int/childgrowth/software/en/.
- 40.Bickel G, Nord M, Price C, et al. Guide to Measuring Household Food Security. USDA Econ Res Serv. 2000:1–82. [Google Scholar]
- 41.Schreiber JB, Nora A, Stage FK, et al. Reporting Structural Equation Modeling and Confirmatory Factor Analysis Results: A Review. J Educ Res. 2006;99(6):323–338. doi: 10.3200/JOER.99.6.323-338 [DOI] [Google Scholar]
- 42.Steinsbekk S, Bonneville-Roussy A, Fildes A, et al. Child and parent predictors of picky eating from preschool to school age. Int J Behav Nutr Phys Act. 2017;14(1):87. doi: 10.1186/s12966-017-0542-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Forehand R, Lautenschlager GJ, Faust J, et al. Parent perceptions and parent-child interactions in clinic-referred children: a preliminary investigation of the effects of maternal depressive moods. Behav Res Ther. 1986;24(1):73–75. doi: 10.1016/0005-7967(86)90152-X [DOI] [PubMed] [Google Scholar]
- 44.Johnson SL. Developmental and environmental influences on young children’s vegetable preferences and consumption. Adv Nutr An Int Rev J. 2016;7(9):220S–231S. doi: 10.3945/an.115.008706.preferences [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hittner JB, Faith MS. Typology of emergent eating patterns in early childhood. Eat Behav. 2011;12:242–248. doi: 10.1016/j.eatbeh.2011.06.001 [DOI] [PubMed] [Google Scholar]