Abstract
Objectives
To evaluate whether there are distinct childhood sleep problem trajectories from birth to 10–11 years and to assess associations with cumulative socio-ecological risks (child, family, context).
Study design
Participants were 5,107 children from the Longitudinal Study of Australian Children—Birth Cohort. At birth, cumulative risk indexes were generated for birth, parenting, family, socioeconomic, and neighborhood risks. Parent-reported child sleep problems were assessed biennially from ages 0–1 to 10–11 years. Sleep problem trajectories were derived using latent class analysis. Multivariable logistic regression was used to examine associations with risk indexes.
Results
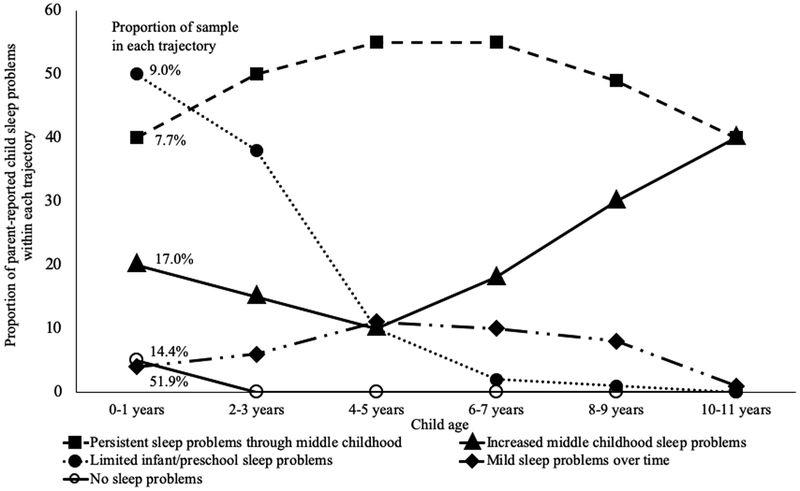
Five distinct trajectories emerged: persistent sleep problems through middle childhood (7.7%), limited infant/preschool sleep problems (9.0%), increased middle childhood sleep problems (17.0%), mild sleep problems over time (14.4%), and no sleep problems (51.9%). Cumulative mother- and father-reported family risks (distress; marital/relational hostility) were linked to nearly all of the trajectories, whereas father- and mother-reported parenting risks were associated with fewer trajectories. Birth risks were associated with increased middle childhood sleep problems. Neighborhood risks were not associated with any trajectories. Socioeconomic risks were linked to mild and persistent sleep problem trajectories. Cumulative risk indexes were most associated with increased middle childhood sleep problems.
Conclusions
This study identified distinct longitudinal sleep problem trajectories, suggesting the need for continuous sleep screening over development. Cumulative risks assessed at birth—primarily maternal and paternal family risks—predicted these trajectories, especially for the sleep problems in middle childhood trajectory. Preventive interventions targeting modifiable factors, especially caregiver distress and marital/relational hostility, could benefit child sleep.
Identifying children at-risk for persistent sleep problems through childhood is critical, as sleep difficulties are associated with subsequent deficits in social-emotional and behavioral skills (1, 2), neurocognitive functioning (3, 4), and brain morphology(5). Sleep problems in infancy have been found to persist through early childhood (6–10), but few studies have examined the developmental course of sleep problems beyond ages 5–6 years. One study identified children with persistent sleep problems (10.6% of the sample) and their corresponding behavioral issues, from ages 5 to 14 years (11). Another study examined longitudinal patterns of insomnia symptoms over seven years, from middle childhood to adolescence (12).. Understanding the trajectories of sleep problems can lead to anticipatory guidance for families This research can also provide a basis for future work that identifies children on distinct sleep problem trajectories that should be differentially targeted for preventive intervention.
To further inform targeted screening and prevention efforts, as well as natural pathways to target during intervention delivery, cumulative risk factors across socio-ecological (13) domains that are associated with persistent childhood sleep problems and those that remit over time should be identified. Bronfenbrenner socio-ecological model (13), recently applied to understand factors linked to adult sleep duration (14), consists of multiple, interacting systems that vary in proximity to the individual and impact development and functioning. These systems include the individual microsystem (eg, biological and psychological factors), the mesosystem (e.g., parenting and other family factors; the school context); and the macrosystem (e.g., the broader physical environment; public policy). Many studies have separately identified risk factors for sleep problems at various socio-ecological levels (13). These include individual child factors such as prematurity (15) and temperament (16, 17), parent and family factors such as maternal depression (18, 19), parenting practices (20–22), inter-parental conflict (23) and household chaos (24, 25), and contextual factors, such as family socioeconomic status (26, 27) and neighborhood disadvantage (28, 29).
Studies using cumulative risk models, which combine multiple and highly intercorrelated risk factors into a risk exposure index (30, 31), to predict other aspects of child development have shown that increased exposure to cumulative socio-ecological risks robustly predicts adverse outcomes such as behavioral health diagnoses, school dropout, substance use, and physical illnesses (32–34). Some emerging research suggests that cumulative exposure to risks related to family adversity is linked to decreased sleep duration (35) and increased sleep problems (36) in childhood. However, linkages with exposure to familial and other cumulative risks on child sleep have not been examined longitudinally or in relation to sleep problem trajectories.
To address these gaps, the primary aim of this study was to identify distinct trajectories of child sleep problems from infancy to middle childhood. The second aim was to examine whether indexes of cumulative risks at multiple socio-ecological levels assessed at birth at the individual child, parent and family, and neighborhood levels were associated with sleep problem trajectories.
METHODS
Data were drawn from the first 6 waves of the prospective Growing up in Australia: The Longitudinal Study of Australian Children (LSAC)—Birth Cohort (B-cohort). Technical details about the study design and methods have been described elsewhere (37). In 2004, LSAC employed a two-stage cluster sampling design to enroll the cohort. In the first stage, Australian postcodes were sampled after stratifying by state and urban/rural status to ensure proportional geographic representation. Within each postcode, children registered on the Australian Medicare database (which includes 98% of all children) were randomly selected to participate. Children not registered on the Medicare database are those who do not have Australian citizenship or whose family members have not applied for a permanent residency (38). Follow-up waves have occurred biennially. The B-cohort includes 5,107 infants aged 0–1 years who were enrolled in 2004 (Wave 1), of whom 3,764 (73.7%) remained in the study at Wave 6 (age 10 to 11 years). The final analytic sample for this study was 4,517 participants. Retention was marginally lower for children with less highly educated parents and from non-English speaking backgrounds (39). Written informed consent for study participation was obtained from children’s primary parent/legal guardian. The study was approved by the Australian Institute of Family Studies Ethics Committee.
Procedure
At each data collection wave researchers administered a face-to-face interview with the primary parent (usually the mother) in the family home (37). When possible, both parents reported on study outcomes.
Measures
Sleep problems.
At each time point, child sleep problems were defined using the parent-reported question, How much is your child’s sleeping pattern or habits a problem for you?(40) The primary parent indicated whether their child’s sleep was a large problem, a moderate problem, a small problem, no problem at all, or not sure/don’t know. Responses were dichotomized according to previous longitudinal and intervention research (41–43), with a sleep problem defined as those who had a moderate or large problem, and no sleep problem defined as no problem or a small problem. Not sure/don’t know responses were coded as missing. This dichotomous approach has shown high correspondence with other measures of caregiver-identified problematic sleep behaviors (44, 45).
Cumulative socio-ecological risk indexes (measured during infancy).
Five separate cumulative risk indexes were theoretically derived and constructed according to Bronfenbrenner socio-ecological framework (13), previous LSAC studies examining socio-ecological risks (31, 46), and previous research on socio-ecological predictors of pediatric sleep problems. Indexes included: a birth risk index (46, 47) to reflect the individual child socio-ecological level; a family risk index and a parenting risk index (31) to reflect aspects of the family socio-ecological level; and a socioeconomic risk index and a neighborhood risk index (48–51) to reflect the broader socio-cultural context. Table I shows the variables in each index. Within each index, each risk variable was dichotomously coded as 1 for high risk and 0 for low risk, and then averaged to generate a total risk index score (between 0 to 1) where more than half the risk variables were available, consistent with cumulative risk coding procedures (30) (see Table 2 and Table 3 (available at www.jpeds.com) for coding of cumulative risk variables and for correlations among risk indexes). Higher index scores indicate higher risk levels. When both maternal and paternal reports were available, we generated a separate risk index by reporter, (family risk and parenting indexes; Table 1 shows included variables by reporter). Of note, the maternal family risk index contained a depressed mood variable and the maternal parenting risk index contained a co-parenting, whereas the corresponding paternal indexes did not as these variables were not included in the LSAC data collection for paternal participants. For single parent families, where a score was not available for the partner, the partner index was treated as missing data.
Table 1.
Variables included in cumulative risk indexes
| Cumulative risk index and relevant citations | Variables |
|---|---|
| Birth risks (43, 46, 47) | Prenatal maternal antidepressant use |
| Prenatal maternal alcohol use | |
| Prenatal cigarette use | |
| Prematurity (<37 weeks gestation) | |
| Low birth weight (<2500g) | |
| Postnatal intensive care | |
| Child special health care needs (78) | |
| Family risks (18, 23, 31, 64)* | Marital hostility |
| Parental psychological distress (Kessler K-6 scale (79)) | |
| Parental depression+ | |
| Parental exposure to stressful life events | |
| Parenting risks (21, 22, 31)* | Low parental warmth |
| Hostile parenting | |
| Low parenting self-efficacy | |
| Poor co-parenting+ | |
| Socioeconomic risks (26, 48, 49) | Financial hardship |
| Low socioeconomic position (SEP) composite (parental income, education, and occupational prestige) | |
| Neighborhood risks (28, 50, 51) | Poor neighborhood facilities |
| Poor neighborhood livability (safety; cleanliness; traffic noise) | |
| Low neighborhood level socio-economic status composite |
Indicates separate mother- and father-reported indexes were generated when available.
Indicates that father-reported index does not include this variable.
Table 2.
Coding information for risk indexes (online only)
| Index | Variable | Reporter | Procedure/question | Coding |
|---|---|---|---|---|
| Birth | Prenatal antidepressant use | Mother | Retrospective report of whether mother had taken any antidepressants during their pregnancy with the child participating in the study, on a yes/no scale. | “Yes” = 1; “no” = 0. |
| Prenatal alcohol use | Mother | Retrospective response to the question, “During the pregnancy with the study child, did you drink alcohol?” on a 3-point scale: “yes, most days”; “yes, occasionally”; “no.” | Any “yes” = 1; “no” = 0. | |
| Prenatal cigarette use | Mother | Retrospective response to the question, “During the pregnancy with the study child, did you smoke cigarettes?” on a 3-point scale: “yes, most days”; “yes, occasionally”; “no.” | Any “yes” = 1; “no” = 0. | |
| Prematurity | Mother | Retrospective report of number of weeks at which child was born. | <37 weeks = 1; 37 weeks or greater = 0. | |
| Low birth weight | Mother | Retrospective report of child birth weight. | Very low (<1500g) and low (1500g - 2500g) birth weight = 1; 2500g or greater = 1(47). | |
| Postnatal intensive care | Mother | Retrospective report of whether there was intensive care at birth, rated on a 3-point scale (“yes”; “no”; “I don’t know”). | “Yes” = 1; “no” and “I don’t know” = 0. | |
| Child special health care needs | Mother | Response on Children with Special Health Care Needs screener—Short Form; response to whether children had a medial, behavioral, or other health condition that has lasted at least 1 year or who required (1) additional medical, mental health, or educational services or (2) prescription medication as a result of their condition. | Any “yes” = 1; “no” = 0 | |
| Family (separate for mothers and fathers) | Marital hostility | Mother; father | Response to 5 items on a 5-point Likert scale ranging from “never” (1) to “always” (5). Items included the frequency of disagreements between partners about child-rearing, stressful or awkward conversations, anger or hostility, or arguments that ended in an individual pushing, hitting, kicking, or shoving. | Items were averaged to generate a total score; 20% of the sample with the highest levels of martial hostility =1; rest of sample = 0; based on Hancock et al. (31). |
| Psychological distress | Mother; father | Response to 6-item Kessler K6 scale (79) on a 5-point Likert scale ranging “all of the time” (0) to “none of the time” (4). Items asked how often reported had felt the following over the past 4 weeks: nervous; hopeless; restless or fidgety; that everything was an effort; so sad that nothing would cheer you up; worthless. | Items were reversed coded as needed and summed to generate a total score; 20% of the sample with the highest scores = 1; rest of sample = 0. | |
| Depression | Mother | Response to one item on a dichotomous yes/no scale asking whether reporter had felt depressed for ≥2 weeks. | Yes = 1; no = 0. | |
| Stressful life events | Mother; father | Response to one items asking reporter the extent to which they were having difficulties with life stress on a 4-point Likert scale ranging from “no stressors” (0) to “many stressors” (3). | Some or many stressors = 1; no or few stressors = 0; based on Giallo et al. (46). | |
| Parenting (separate for mothers and fathers) | Parental warmth | Mother; father | Response to 6 items on a 5-point Likert scale ranging from “never/almost never” (1) to “always/almost always” (5). Items asked parents the frequency with which they expressed affection by: hugging, kissing, and holding the child; hugging or holding the child for no particular reason; telling the child how happy he/she makes you; having warm, close times together with the child; feeling close to the child when they are happy and upset. | Items were summed to generate a total score; 20% of the sample with the lowest scores = 1; rest of sample = 0. |
| Hostile parenting | Mother; father | Response to 5 items on a 10-point Likert scale ranging from “not at all” (1) to “all the time” (1). Items asked parents how often in the previous 4 weeks they: had been angry with the study child; had raised their voice or shouted at the study child; felt the study child got on their nerves when the child cried; had lost their temper with the study child; has left the study child alone in his/her bedroom when they were irritable or upset. | Items were summed to generate a total score; 20% of the sample with the highest scores = 1; rest of sample = 0. | |
| Parenting self-efficacy | Mother; father | Response to four items rated on a 5-point Likert scale ranging from “never/almost never” (1) to “always/almost always” (5). Items asked how good parents felt they were at: performing routine caregiving tasks; keeping the study child amused; calming the study child; keeping the study child busy. | Items were summed to generate a total score; 20% of the sample with the lowest scores = 1; rest of sample = 0. | |
| Co-parenting | Mother | Response to 3 items on a 5-point Likert scale ranging from “never” (1) to “always” (5). Parents rated how often their partner is a resource or support to them in raising their children; how often they are a resource or support to their partner; and how often they feel their partner understands and is supportive of their needs. Items were summed to generate an overall score | Items were summed to generate a total score; 20% of the sample with the lowest scores = 1; rest of sample = 0. | |
| Socioeconomic | Financial hardship | Mother | Report of financial hardship in the previous 12 months using a 6-item measure that asked about the family’s ability to pay their bills and mortgage on time, and whether the family had gone without meals, had been unable to heat or cool their home, had pawned or sold something, or sought out welfare or community-based assistance. | 20% of the sample with the highest financial hardship scores = 1; rest of sample = 0. |
| Socioeconomic Position (SEP) | Mother | Composite variable consisting of parent-reported parental income, education, and occupational prestige. Blakemore et al. generated the SEP was generated using the following steps (48). Annual income for each caregiver (maternal and paternal) were summed and log-transformed. Each parent reported on their number of years of education attainment, which ranged from those who had no formal schooling (0 years) to those who had completed a post-graduate degree (20 years). Parents reported on their most recent occupational status, which was then rated using the ANU4, an index of occupational skill level and type. The income, educational attainment, and occupational prestige variables were then standardized, summed, and divided by the number of caregivers in the home. The resulting score was restandardized with a mean of 0 and a standard deviation of 1. The SEP was further categorized into low, medium, and high SEP categories reflecting low, medium, and high SEP. | Low SEP category = 1; middle and high SEP = 0. | |
| Neighborhood | Neighborhood facilities | Mother | Response to six statements on a 4-point Likert scale ranging from “strongly agree” (1) to “strongly disagree” (4). Statements asked parents the extent to which they agreed that the following existed in their neighborhood: good parks, playgrounds, and play spaces in their neighborhood; good street lighting; good footpaths and roads’ access to close, affordable, regular public transport; access to basic shopping facilities; access to basic services such as banks, medical clinics, etc. | Lowest 20% of scores = 1; rest of sample = 0. |
| Neighborhood livability | Mother | Response to three statements on a 4-point Likert scale ranging from “strongly disagree” (1) to “strongly agree” (4). The ask parents about the livability of their neighborhood, being “This is a safe neighborhood”, “This is a clean neighborhood” and “There is heavy traffic on my street or road” | Lowest 20% of scores = 1; rest of sample = 0. | |
| Neighborhood-level socioeconomic status | Administrative data | Socioeconomic Indices for Areas (SEIFA) Index of Advantage/Disadvantage; the SEIFA has been validated by the Australian Bureau of Statistics, and consists of 31 variables drawn from administrative data, including neighborhood-level rates of income, unemployment, occupation, and education (50, 51). Scores range from disadvantaged (1) to advantaged (10). | Lowest 20% of scores = 1; rest of sample = 0. |
Table 3.
Correlations between cumulative risk indexes (online only)
| Risk indexes | Birth | Family (mother) | Family (father) | Parenting (mother) | Parenting (father) | Socioeconomic |
|---|---|---|---|---|---|---|
| Family (mother) | 0.13 | . | ||||
| Family (father) | 0.06 | 0.28 | . | |||
| Parenting (mother) | 0.02 | 0.18 | 0.04 | . | ||
| Parenting (father) | 0.03 | 0.12 | 0.38 | 0.12 | . | |
| Socioeconomic | 0.07 | 0.11 | 0.08 | 0.01 | 0.08 | . |
| Neighborhood | 0.01 | 0.01 | 0.04 | 0.03 | 0.04 | 0.19 |
Note. Mother = mother-reported; father = father-reported.
This cumulative risk approach indexes the number of risk factor exposures. Although some risk factors may be strongly intercorrelated, others are not (30, 31); this approach maximizes the likelihood of capturing diverse risk exposures linked with child sleep problems in previous research. Tables 4–8 (available at www.jpeds.com) show the correlations among variables in the risk indexes, which ranged from small to moderate across indexes, with the exception of the birth risk index. In that index, some variables such as maternal prenatal use of teratogenic substances and intensive postnatal care were not associated. This index was created on the basis of previous pediatric sleep and LSAC research (47), and theoretically represents a spectrum of risky birth complications. Reliability and validity for the continuous variables, such as the parenting scales, are strong (alpha >.70) and are described in detail elsewhere (52).
Table 4.
Correlations among variables in birth risk index (online only)
| Risk variables | Prenatal antidepressant use | Prenatal alcohol use | Prenatal cigarette use | Prematurity | Low birthweight | Postnatal intensive care |
|---|---|---|---|---|---|---|
| Prenatal alcohol use | 0.00 | |||||
| Prenatal cigarette use | 0.03 | 0.01 | ||||
| Prematurity (<37 weeks gestation) | 0.02 | −0.02 | 0.05 | |||
| Low birthweight (<2500g) | 0.01 | −0.05 | 0.07 | 0.54 | ||
| Postnatal intensive care | −0.01 | −0.03 | 0.02 | 0.41 | 0.37 | |
| Child special healthcare needs | 0.03 | −0.03 | 0.01 | 0.08 | 0.07 | 0.10 |
Table 8.
Correlations among variables included in the neighborhood risk index (online only)
| Neighborhood socioeconomic status | Poor neighborhood livability | |
|---|---|---|
| Poor neighborhood livability | 0.21 | . |
| Poor neighborhood facilities | 0.14 | 0.26 |
Note. The neighborhood socioeconomic status variable is a standardized index created by the LSAC study team.
Confounders.
Child sex was entered as confounder in all statistical analyses. We also included three primary caregiver-reported child sleep behaviors in all statistical analyses as confounders: difficulty getting off to sleep at night; not happy to sleep alone; and waking during the night. Caregivers rated whether these items occurred 4 or more nights per week (yes/no).
Statistical Analyses
We used survey methods in all analyses to account for the unequal probability of participant selection into the sample and sample attrition, and the multi-stage, clustered sampling design (53, 54). To identify whether there were distinct trajectories of child sleep problems over time, we conducted latent class analysis in Mplus version 8 (55). Children were grouped based on the repeatedly measured parent-reported child sleep problem across the 6 study waves. The number of trajectories classified was determined on the basis of the minimum Bayesian Information Criterion (=7870.9) and a significant Lo-Mendell-Rubin Likelihood Ratio Test (<0.05). This technique estimates the number of groups that best represent the data, and whether extracting additional groups would significantly improve model fit. Estimation was by maximum likelihood with robust standard errors, which handles missing data by inferring on the basis of available measures.
We then used Stata version 15 (56) to examine whether cumulative socio-ecological risk indexes measured at birth were differentially predictive of the latent sleep problem trajectories. Associations between the risk indexes and derived sleep trajectories were determined using multinomial logistic regression to estimate the unadjusted and adjusted odds ratios between groups with the “no sleep problems” group (see below) as the reference. Only adjusted models are presented as the estimates attenuated only slightly on including the a priori confounders. Finally, we conducted multivariable logistic regression for each trajectory, with only indexes with a P < .05 in the multinomial logistic regressions included as predictors in the multivariable models.
RESULTS
Table 9 shows the birth cohort demographic information. There were similar proportions of girls and boys (51.1% male). The mother served as the primary reporter for the majority of children (96.1%). Most families were two-parent families (90.6%), spoke English as the primary language at home (85.6%) and had parents who had completed at least high school (68.3% of mothers; 59.8% of fathers). Mean cumulative risk scores for each index are also presented in Table 9. The correlations between risk indexes are available in Table 3.
Table 9.
Participant demographic characteristics and mean risk index scores
| B cohort | |
|---|---|
| N = 5107 | |
| Child (baseline) | |
| Male, % | 51.1 |
| Age (months), mean (SD); range | 8.8 (2.5); 3 – 19 |
| Primary parent (baseline) | |
| Female, % | 96.1 |
| Age (years), mean (SD); range | 31.0 (5.5); 15–63 |
| Born in Australia/New Zealand, % | 81.4 |
| English main language spoken at home, % | 85.6 |
| Education status, % | |
| Did not complete high school | 31.7 |
| Completed high school only | 35.5 |
| Completed tertiary/postgraduate degree | 32.9 |
| Married/de facto, % | 90.6 |
| Secondary parent (baseline) | N = 4629 |
| Male, % | 98.3 |
| Age (years), mean (SD); range | 33.7 (6.0); 16–65 |
| Born in Australia/New Zealand, % | 79.4 |
| Education status, % | |
| Did not complete high school | 40.2 |
| Completed high school only | 23.1 |
| Completed tertiary/postgraduate degree | 36.7 |
| Cumulative risk index score, mean (SD) | |
| Birth risks | 0.14 (0.15) |
| Family risks | |
| Mother-reported | 0.27 (0.31) |
| Father-reported | 0.28 (0.33) |
| Parenting risks | |
| Mother-reported | 0.38 (0.19) |
| Father-reported | 0.10 (0.15) |
| Socioeconomic risks | 0.37 (0.36) |
| Neighborhood risks | 0.19 (0.25) |
Sleep problem trajectories
The Figure depicts the results of latent class analysis, in which 5 distinct sleep problem trajectories emerged across the 6 time points. Spanning ages 0–1 to 10–11 years, 51.9% of children were classified as having “no sleep problems” over time. Seventeen percent of children showed minimal sleep problems in early childhood with increased sleep problems through middle childhood (“increased middle childhood sleep problems”). Another 9.0% of children showed increased sleep problems during the infancy and preschool periods, with substantial decreases around ages 4–5 years and continued decreases during middle childhood (“limited infant/preschool sleep problems”). A total of 14.4% showed mild sleep problems with minor increases in middle childhood (“mild sleep problems over time”), and 7.7% of children were categorized as having a persistently high level of sleep problems from infancy through middle childhood (“persistent sleep problems through middle childhood”).
Cumulative risk indexes at birth and sleep problem trajectories
Table 10 provides results of multinomial models examining associations between each cumulative risk index assessed at birth and each sleep problem trajectory. The birth risk index was associated with “increased middle childhood sleep problems” and the “limited infant/preschool sleep problems” trajectories. Both the mother-reported family risk index and parenting risk index were associated with nearly all of the trajectories; only the association between the mother-reported parenting risk index and the “mild sleep problems over time” trajectory was non-significant. Father-reported family risk was also associated with all of the trajectories, but father-reported parenting risks were only linked to the “increased middle childhood sleep problems” and “persistent sleep problems” trajectories. Whereas neighborhood risks were only associated with “mild sleep problems over time,” socioeconomic risks were linked to all sleep problem trajectories.
Table 10.
Associations among cumulative socio-ecological risk indexes and child sleep problem trajectories
| Multinomial regression models | ||||||||
|---|---|---|---|---|---|---|---|---|
| Risk Indexes | Mild sleep problems over time | Increased middle childhood sleep problems | Limited infant/preschool sleep problems | Persistent sleep problems through middle childhood | ||||
| OR 95% CI | p-value | OR 95% CI | p-value | OR 95% CI | OR 95% CI | p-value | ||
| Birth risks | 1.35 (0.67, 2.71) | 0.394 | 2.44 (1.41, 4.25) | 0.002 | 1.99 (1.01, 3.92) | 0.046 | 1.74 (0.77, 3.93) | 0.18 |
| Family risks | ||||||||
| Mother-reported | 2.27 (1.64, 3.12) | <0.001 | 3.03 (2.21, 4.14) | <0.001 | 3.07 (2.16, 4.36) | <0.001 | 5.85 (4.01, 8.52) | <0.001 |
| Father-reported | 1.76 (1.29, 2.39) | <0.001 | 1.99 (1.49, 2.67) | <0.001 | 2.13 (1.49, 3.05) | <0.001 | 2.62 (1.72, 3.99) | <0.001 |
| Parenting risks | ||||||||
| Mother-reported | 0.79 (0.49, 1.29) | 0.362 | 2.36 (1.61, 3.44) | <0.001 | 1.92 (1.22, 3.04) | 0.005 | 1.80 (1.04, 3.11) | 0.034 |
| Father-reported | 1.15 (0.58, 2.27) | 0.677 | 2.56 (1.45, 4.50) | 0.001 | 0.69 (0.32, 1.47) | 0.341 | 2.73 (1.17, 6.40) | 0.020 |
| Socioeconomic risks | 2.33 (1.82, 2.99) | <0.001 | 1.40 (1.10, 1.78) | 0.006 | 1.42 1.05, 1.93) | 0.022 | 3.09 (2.21, 4.32) | <0.001 |
| Neighborhood risks | 1.47 (1.04, 2.06) | 0.026 | 1.11 (0.81, 1.53) | 0.482 | 1.15 0.75, 1.76) | 0.497 | 1.30 (0.82, 2.08) | 0.257 |
| Multivariate logistic regression models | ||||||||
| Risk Indexes | Mild sleep problems over time | Increased middle childhood sleep problems | Limited infant/preschool sleep problems | Persistent sleep problems through middle childhood | ||||
| OR 95% CI | p-value | OR 95% CI | p-value | OR 95% CI | p-value | OR 95% CI | p-value | |
| Birth risks | - | - | 2.15 (1.07, 4.32) | 0.031 | 1.32 (0.56, 3.08) | 0.515 | - | - |
| Family risks | ||||||||
| Mother-reported | 1.84 (1.24, 2.72) | 0.002 | 2.38 (1.60, 3.54) | <0.001 | 2.47 (1.64, 3.72) | <0.001 | 4.41 (2.69, 7.24) | <0.001 |
| Father-reported | 1.45 (1.03, 2.05) | 0.032 | 1.41 (1.00, 1.96) | 0.045 | 1.56 (1.06, 2.29) | 0.022 | 1.49 (0.90, 2.46) | 0.113 |
| Parenting risks | ||||||||
| Mother-reported | - | - | 1.93 (1.08. 3.46) | 0.026 | 1.25 (0.66, 2.33) | 0.486 | 1.05 (0.51, 2.15) | 0.889 |
| Father-reported | - | - | 1.56 (0.844, 2.87) | 0.155 | 1.55 (0.59, 4.09) | 0.368 | ||
| Socioeconomic risks | 2.06 (1.50, 2.83) | <0.001 | 1.22 (0.92, 1.62) | 0.158 | 1.30 (0.93, 1.83) | 0.121 | 2.14 (1.41, 3.28) | <0.001 |
| Neighborhood risks | 1.03 (0.66, 1.61) | 0.882 | - | - | - | - | - | - |
Note. OR = odds ratio. Multivariate logistic regressions include only those risk indexes associated with trajectories at p<.05 in multinomial analyses.
In multivariable logistic regressions, which only included the risk indexes in multinomial models with a p<.05 (Table 10), all of the associations were attenuated and some were no longer significant. Birth risks continued to be associated with “increased middle childhood sleep problems.” Mother-reported family risks also continued to be associated with all of the trajectories, as in the multinomial models, and father-reported family risks were associated with all trajectories except “persistent sleep problems through middle childhood.” Mother-reported parenting risks were only associated with “increased middle childhood sleep problems.” Father-reported parenting risks were not associated with any sleep problem trajectories. Neighborhood risks similarly were not associated with any of the trajectories. The socioeconomic risk index, however, continued to be associated with the “mild sleep problems over time” and the “persistent sleep problems through middle childhood” trajectories.
Overall, the “increased middle childhood sleep problems” trajectory had the greatest number of associated cumulative socio-ecological risk indexes. As shown in Table 10, in the multivariable models, this trajectory had four associated cumulative risk indexes, whereas other trajectories were associated with a maximum of three risk indexes. Indexes associated with the “increased middle childhood sleep problems” trajectory were the cumulative birth risk, mother-reported and father-reported family risk, and mother-reported parenting risk indexes.
DISCUSSION
This study identifies distinct sleep problem trajectories from birth to middle childhood and examines associations with cumulative socio-ecological risks assessed at birth. In line with previous studies (6, 11, 57) about one-half of children showed no sleep problems, and 9% showed only early childhood sleep problems and 14% exhibited mild increases in sleep problems through ages 10–11 years. Three of the five trajectories included sleep problems in the first year of life. Interestingly, 17% of the sample had minimal sleep problems in early childhood but developed sleep problems in middle childhood. These trajectories correspond with and extend research showing that 12–20% of infants with sleep problems have continued early childhood difficulties (6, 8) and with research indicating a sleep problem persistence of 4–10% in middle childhood (11, 58). A recent study of sleep problems from ages 10–14 years found evidence for only 2 trajectories—troubled (10.6%) and normal sleepers (11), compared with the 5 found here. A proportion of the “normal” sleepers may have had early sleep problems that resolved or mild middle childhood sleep problems, consistent with the “limited infant/preschool sleep problems” and the “mild increases over time” trajectories that we found (Figure). Studies that do not include the early years likely miss identifying children with early sleep problems.
Figure 1.
Sleep problem trajectories from birth to age 10–11 years
Mother-reported family risk variables, which included marital/relational hostility, stress exposure, psychological distress, and depression, were consistently associated with sleep problem trajectories. The more limited associations among sleep problem trajectories and father-reported family and especially parenting risk variables may be due to differences in parental practices and the division of childcare. Mothers may have more exposure to infant sleep problems due to longer postpartum family leave, which could lead to continued maternal management of sleep problems in later development. Indeed, mothers are more involved than fathers in nighttime caregiving during both early infancy (59) and toddlerhood (60). A study of 9- to 10-year-olds found that maternal, but not paternal, sleep was linked to child sleep duration and quality (61), suggesting greater maternal involvement in sleep regulation.
In the present study father-reported family risks at birth were associated with all trajectories except “persistent sleep problems through middle childhood,” but father-reported parenting risks were not. Other research (60) has found that paternal family risks and parenting practices are more strongly linked to concurrent or at least less distal sleep problems. Father-reported parenting risks may also have an indirect as opposed to a direct influence on persistent child sleep problems, as found in a longitudinal study showing that maternal marital hostility in infancy directly influenced later sleep problems, whereas paternal marital hostility had an indirect effect (62). Marital/relational hostility, which was a risk factor included in the maternal and paternal family risk indexes, may interact with child emotional and behavioral factors to influence sleep problems over time (63).
It is noteworthy that both mother and father-reported family risks in a child’s first year of life are linked with proximal sleep problems in infancy and early childhood and with more distal sleep problems that extend through or emerge in middle childhood. It could be that caregivers struggling with family risks such as marital/relational hostility or psychological distress during their child’s infancy are more likely to experience a recurrence of these concerns over time, leading to continued difficulty with child sleep problems (64). At the same time, persistent child sleep problems may also cause continued parental depressive symptoms and marital/relational stress. A recent study found such bidirectional effects, with child sleep problems robustly impacting maternal depression longitudinally (19); additional research is needed with fathers.
Child birth risks and mother-reported parenting risks were associated only with the “increased sleep problems in middle childhood” trajectory. This is surprising as early birth risks have been linked to sleep problems (43) and poor parenting has been found to impact early childhood sleep via bedtime limit setting difficulties, low parental self-efficacy, and negative parent-child interactions (21, 22, 62). The effects of birth risks and maternal parenting practices in the first year of life may accumulate over time and be exacerbated by other child factors, resulting in a greater impact on sleep in later development. Unmeasured child factors such as temperament and behavioral concerns can also interact with parent behavior and impact the etiology and persistence of child sleep difficulties (16, 23, 62, 63). Future research should examine child temperament, mood, and behavior concerns, which have been linked to poor sleep in middle childhood (11, 58, 65). Research is also needed on how maternal and paternal family and parenting processes unfold over time to influence child sleep and related outcomes (19, 23).
Collectively, these findings support a personalized and developmentally-tailored approach to child sleep problem screening, prevention, and intervention. The high number of cumulative risk indexes associated with the “increased middle childhood sleep problems” trajectory suggests that anticipatory guidance about the development of later sleep problems may be necessary for families contending with child birth risks, maternal and paternal family risks, and maternal parenting risks in a child’s first year of life. It could be that children with this combination of cumulative risk factors at multiple socio-ecological levels at birth show later sleep problems that are comorbid with behavioral health conditions, given that internalizing and externalizing disorders tend to co-occur with pediatric sleep problems (58, 66).
Screening for caregiver psychological distress, stress exposure, and marital/relational conflict during infancy may also identify children at-risk for early and persistent sleep problems. Although neighborhood-level risks such as safety and noise were not associated with sleep problem trajectories, family-level socioeconomic risks were linked to both mild and persistent sleep problems, consistent with previous research linking socioeconomic disadvantage and poor sleep (26, 27). The American Academy of Pediatrics recommends that pediatricians screen for parent and child adverse experiences, including caregiver mental health and stress exposure, to identify children at-risk for poor developmental outcomes (67, 68).
Aspects of the caregiver family and parenting risks are modifiable intervention targets that could be leveraged to prevent child sleep problems. With an increased postpartum depression prevalence (69), maternal mood screening is recommended as a part of maternity and infant care in Australia and other Western contexts (70, 71). Unfortunately, few mothers who screen positively for postpartum depression receive treatment (70), despite accessing medical care for themselves and for their children (72). Given these service delivery gaps, treatment for maternal mood concerns could be integrated into child behavioral sleep programs. Such programs have had ancillary benefits on maternal mood (41, 73) and marital satisfaction (74), and children with a depressed caregiver show diminished sleep intervention outcomes (75). Integrated services should also be extended to paternal postpartum mood concerns, which impact 10% of fathers and are correlated with maternal mood (76), Incorporating evidence-based strategies to improve caregiver distress, marital/relational hostility, and enhance parenting practices could further augment sleep intervention effects, benefit families who may not respond to sleep intervention, or reduce the risk of sleep problem recurrence (8, 65) One study found that combining behavioral parent training with sleep intervention increased pre-to-posttreatment child behavior effect sizes (77).
Study limitations include the use of subjective reports of child sleep as well as a single item used to assess problematic sleep, which may not fully capture the range, nuances, or presence of a diagnosed child sleep disorder such as insomnia. In addition, this item does not capture objective aspects of child sleep including sleep timing and duration. Future research using objective measures would reduce the potential in the present study for significant linkages between caregiver-reported, and especially maternally-reported, cumulative risks as well as child sleep problems. In particular, caregiver mood concerns could impact caregiver-reported child sleep, although it is noteworthy that father-reported family risks were still linked to mostly maternally-reported child sleep problems in this study. This study used a large, representative Australian sample, but findings may not generalize to other racial/ethnic backgrounds, cultures, parenting and marital/romantic partnership arrangements, and socio-ecological contexts, especially given cross-cultural variation in parent-defined sleep problems (57). The study design precludes any assessment of causality, however, findings may inform future causal research examining cumulative risk indexes and child sleep. Research should also assess cumulative risk indexes at multiple time points in relation to child sleep, with consistent reporting of mother-versus father-reported risk variables and expansion of caregiver report to families with other parenting arrangements (i.e., relatives; maternal primary and secondary caregivers; etc). Genetic factors may also confer increased risk for or resilience to sleep problems.
Additional research should examine the interplay of socio-ecological risks, sleep problems, and child factors longitudinally, as well as the direct and indirect effects of maternal and paternal risk factors. Screening for maternal and paternal family risks, particularly in socio-economically disadvantaged families, can help to identify risk for persistent sleep problems. Screening can also elucidate modifiable intervention targets, such as caregiver distress or marital/relational concerns that could be delivered to caregivers or incorporated into child sleep treatment. These efforts could buffer against the development or persistence of pediatric sleep problems, augment the effects of behavioral sleep intervention, and potentially mitigate the negative effects of familial and environmental risk factors on broad child and family functioning.
Table 5.
Correlations among variables in family risk indexes (online only)
| Mother-reported risk variables | Marital hostility | Psychological distress | Depression |
|---|---|---|---|
| Psychological distress (Kessler-6) | 0.25 | . | |
| Depression | 0.20 | 0.37 | . |
| Stress exposure | 0.25 | 0.37 | 0.26 |
| Father-reported risk variables | Marital hostility | Psychological distress | |
| Psychological distress (Kessler-6) | 0.23 | . | |
| Stress exposure | 0.24 | 0.37 | . |
Note. Father-reported family risk index did not include depression variable as this item was not measured for fathers.
Table 6.
Correlations among variables in parenting risk indexes (online only)
| Mother-reported risk variables | Self-efficacy | Warmth | Hostile parenting |
|---|---|---|---|
| Warmth | 0.24 | . | |
| Hostile parenting | 0.21 | 0.11 | . |
| Co-parenting | 0.21 | 0.25 | 0.12 |
| Father-reported risk variables | Self-efficacy | Warmth | |
| Warmth | 0.21 | . | |
| Hostile parenting | 0.17 | 0.22 | . |
Note. Father-reported family risk index did not include hostile parenting variable as this item was not measured for fathers.
Table 7.
Correlations among variables included in the socioeconomic risk index (online only)
| Risk variables | Socioeconomic position |
|---|---|
| Financial hardship | 0.24 |
Note. The socioeconomic position (SEP) variable is a standardized index consisting of family income, education, and occupational prestige. The variable was created by the LSAC study team.
Acknowledgments
Supported by the National Heart, Lung, and Blood Institute (T32HL007953–17 [to A.W.]); the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD094905 [to A.W.]); the Sleep Research Society Foundation (to A.W.); the National Health and Medical Research Council (Practitioner Fellowship, 1136222 [to H.H.]); and the Victorian Government’s Operational Infrastructure Support Program (to J.Q.). The authors declare no conflicts of interest.
Abbreviations:
- LSAC
Longitudinal Study of Australian Children
- OR
odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this study were presented at the International Paediatric Sleep Association Congress, << >>, 2018, << >>; and the Pediatric Academic Societies annual meeting, May 5–8, 2018, Toronto, Canada.
REFERENCES
- 1.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA pediatrics. 2015;169:575–82. [DOI] [PubMed] [Google Scholar]
- 2.Williams KE, Berthelsen D, Walker S, Nicholson JM. A developmental cascade model of behavioral sleep problems and emotional and attentional self-regulation across early childhood. Behavioral sleep medicine. 2017;15:1–21. [DOI] [PubMed] [Google Scholar]
- 3.Kocevska D, Rijlaarsdam J, Ghassabian A, Jaddoe VW, Franco OH, Verhulst FC, et al. Early childhood sleep patterns and cognitive development at age 6 years: the Generation R Study. Journal of pediatric psychology. 2016:jsv168. [DOI] [PubMed] [Google Scholar]
- 4.Taveras EM, Rifas-Shiman SL, Bub KL, Gillman MW, Oken E. Prospective Study of Insufficient Sleep and Neurobehavioral Functioning among School-Age Children. Academic Pediatrics. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocevska D, Muetzel RL, Luik AI, Luijk MP, Jaddoe VW, Verhulst FC, et al. The Developmental Course of Sleep Disturbances Across Childhood Relates to Brain Morphology at Age 7: The Generation R Study. Sleep. 2017;40:1–9. [DOI] [PubMed] [Google Scholar]
- 6.Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129:e276–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kataria S, Swanson MS, Trevathan G. Persistence of sleep disturbances in preschool children. The Journal of pediatrics. 1987;110:642–6. [DOI] [PubMed] [Google Scholar]
- 8.Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics. 2003;111:e203–e7. [DOI] [PubMed] [Google Scholar]
- 9.Reynaud E, Forhan A, Heude B, de Lauzon-Guillain B, Charles M-A, Plancoulaine S. Night-waking trajectories and associated factors in French preschoolers from the EDEN birth-cohort. Sleep medicine. 2016;27:59–65. [DOI] [PubMed] [Google Scholar]
- 10.Williams KE, Nicholson JM, Walker S, Berthelsen D. Early childhood profiles of sleep problems and self-regulation predict later school adjustment. British journal of educational psychology. 2016;86:331–350. [DOI] [PubMed] [Google Scholar]
- 11.Wang B, Isensee C, Becker A, Wong J, Eastwood PR, Huang R-C, et al. Developmental trajectories of sleep problems from childhood to adolescence both predict and are predicted by emotional and behavioral problems. Frontiers in psychology. 2016;7:1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Combs D, Goodwin JL, Quan SF, Morgan WJ, Shetty S, Parthasarathy S. Insomnia, health-related quality of life and health outcomes in children: a seven year longitudinal cohort. Scientific reports. 2016;6:27921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bronfenbrenner U Toward an experimental ecology of human development. American psychologist. 1977;32:513. [Google Scholar]
- 14.Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep medicine reviews. 2010;14:191–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Björkqvist J, Paavonen J, Andersson S, Pesonen A-K, Lahti J, Heinonen K, et al. Advanced sleep–wake rhythm in adults born prematurely: confirmation by actigraphy-based assessment in the Helsinki Study of Very Low Birth Weight Adults. Sleep medicine. 2014;15:1101–6. [DOI] [PubMed] [Google Scholar]
- 16.Cremone A, Jong DM, Kurdziel LB, Desrochers P, Sayer A, LeBourgeois MK, et al. Sleep Tight, Act Right: Negative Affect, Sleep and Behavior Problems During Early Childhood. Child Development. 2017;89:e42–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Molfese VJ, Rudasill KM, Prokasky A, Champagne C, Holmes M, Molfese DL, et al. Relations between toddler sleep characteristics, sleep problems, and temperament. Developmental neuropsychology. 2015;40:138–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Jong DM, Cremone A, Kurdziel LB, Desrochers P, LeBourgeois MK, Sayer A, et al. Maternal depressive symptoms and household income in relation to sleep in early childhood. Journal of pediatric psychology. 2016;41:961–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ystrom H, Nilsen W, Hysing M, Sivertsen B, Ystrom E. Sleep problems in preschoolers and maternal depressive symptoms: An evaluation of mother-and child-driven effects. Developmental psychology. 2017;53:2261. [DOI] [PubMed] [Google Scholar]
- 20.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep medicine reviews. 2010;14:89–96. [DOI] [PubMed] [Google Scholar]
- 21.Teti DM, Kim B-R, Mayer G, Countermine M. Maternal emotional availability at bedtime predicts infant sleep quality. Journal of Family Psychology. 2010;24:307. [DOI] [PubMed] [Google Scholar]
- 22.Johnson N, McMahon C. Preschoolers’ sleep behaviour: associations with parental hardiness, sleep-related cognitions and bedtime interactions. Journal of Child Psychology and Psychiatry. 2008;49:765–73. [DOI] [PubMed] [Google Scholar]
- 23.El-Sheikh M, Kelly RJ, Bagley EJ, Wetter EK. Parental depressive symptoms and children’s sleep: The role of family conflict. Journal of Child Psychology and Psychiatry. 2012;53:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boles RE, Halbower AC, Daniels S, Gunnarsdottir T, Whitesell N, Johnson SL. Family chaos and child functioning in relation to sleep problems among children at risk for obesity. Behavioral sleep medicine. 2017;15:114–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spilsbury JC, Patel SR, Morris N, Ehayaei A, Intille SS. Household chaos and sleep-disturbing behavior of family members: results of a pilot study of African American early adolescents. Sleep health. 2017;3:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychology. 2013;32:849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychology. 2014;33:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bagley EJ, Kelly RJ, Buckhalt JA, El-Sheikh M. What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment. Sleep medicine. 2015;16:496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheehan C, Powers D, Margerison-Zilko C, McDevitt T, Cubbin C. Historical neighborhood poverty trajectories and child sleep. Sleep health. 2018;4:127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychological Bulletin. 2013;139:1342. [DOI] [PubMed] [Google Scholar]
- 31.Hancock KJ, Christensen D, Zubrick SR. Development and Assessment of Cumulative Risk Measures of Family Environment and Parental Investments in the Longitudinal Study of Australian Children. Social Indicators Research. 2017:1–30. [Google Scholar]
- 32.Atkinson L, Beitchman J, Gonzalez A, Young A, Wilson B, Escobar M, et al. Cumulative risk, cumulative outcome: A 20-year longitudinal study. PloS one. 2015;10:e0127650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evans GW. A multimethodological analysis of cumulative risk and allostatic load among rural children. Developmental psychology. 2003;39:924. [DOI] [PubMed] [Google Scholar]
- 34.Rutter M Protective factors in children’s responses to stress and disadvantage. Ann Acad Med Singapore. 1979;8:324–38. [PubMed] [Google Scholar]
- 35.Bagley EJ, El-Sheikh M. Familial risk moderates the association between sleep and zBMI in children. Journal of pediatric psychology. 2013;38:775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alkon A, Boyce WT, Neilands TB, Eskenazi B. children’s autonomic nervous system reactivity Moderates the relations between Family adversity and sleep Problems in latino 5-Year Olds in the CHAMACOS study. Frontiers in public health. 2017;5:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soloff C, Lawrence D, Jonstone R. Longitudinal Study of Australian Children Technical Paper No. 1: Sample Design. Melbourne, Victoria: Australian Institute of Family Studies; 2005. [Google Scholar]
- 38.Australian Government. Medicare Commonwealth of Australia [Available from: https://www.health.gov.au/internet/main/publishing.nsf/Content/health-medicarebenefits-index.htm.
- 39.Norton A, Monahan K. The Longitudinal Study of Australian Children: LSAC technical Paper No. 15, Wave 6 Weighting and Non-Response. 2015.
- 40.Australian Government Department of Families, Housing, Community Services and Indigenous Affairs [AGDF]. Growing up in Ausralia: The Longitudinal Study of Australian Children 2009–10 Annual Report. Australia: New Millennium Print; 2011. [Google Scholar]
- 41.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Efficacy of an internet-based intervention for infant and toddler sleep disturbances. Sleep. 2011;34:451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics. 2011;128:692–701. [DOI] [PubMed] [Google Scholar]
- 43.Quach J, Mensah FK, Hiscock H. Differential outcomes of sleep problems in children with and without special health care needs: Australian population study. Journal of Developmental & Behavioral Pediatrics. 2016;37:415–23. [DOI] [PubMed] [Google Scholar]
- 44.Lycett K, Mensah FK, Hiscock H, Sciberras E. Comparing subjective measures of behavioral sleep problems in children with ADHD: a cross-sectional study. Sleep medicine. 2015;16:1377–80. [DOI] [PubMed] [Google Scholar]
- 45.Williamson AA, Mindell JA, Hiscock H, Quach J. Child sleep behaviors and sleep problems from infancy to school-age. Sleep Medicine. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Giallo R, Cooklin A, Nicholson JM. Risk factors associated with trajectories of mothers’ depressive symptoms across the early parenting period: an Australian population-based longitudinal study. Archives of women’s mental health. 2014;17:115–25. [DOI] [PubMed] [Google Scholar]
- 47.Sciberras E, Ukoumunne OC, Efron D. Predictors of parent-reported attention-deficit/hyperactivity disorder in children aged 6–7 years: A national longitudinal study. Journal of Abnormal Child Psychology. 2011;39:1025–34. [DOI] [PubMed] [Google Scholar]
- 48.Blakemore T, Strazdins L, Gibbings J. Measuring family socio-economic position. Australian Social Policy Journal. 2009;8:121. [Google Scholar]
- 49.Nicholson JM, Lucas N, Berthelsen D, Wake M. Socioeconomic inequality profiles in physical and developmental health from 0–7 years: Australian National Study. Journal of Epidemiology & Community Health. 2010:jech. 2009.103291. [DOI] [PubMed] [Google Scholar]
- 50.Edwards B, Bromfield LM. Neighborhood influences on young children’s conduct problems and pro-social behavior: Evidence from an Australian national sample. Children and Youth Services Review. 2009;31:317–24. [Google Scholar]
- 51.Trewin D Census of population and housing: Socio-economic indexes for areas (SEIFA). Canberra, Australia: Australian Bureau of Statistics; 2001. [Google Scholar]
- 52.Zubrick SR, Lucas N, Westrupp EM, Nicholson JM. Parenting measures in the Longitudinal Study of Australian Children: Construct validity and measurement quality, Waves 1 to 4. Canberra: Department of social services; 2014. [Google Scholar]
- 53.Soloff C, Lawrence D, Johnstone R. LSAC technical reference paper number 1: sample design. Available at: www.aifs.gov.au/growingup/pubs/techpapers/tp1.pdf. 2005. [
- 54.Misson S, Sipthorp M, Studies AIoF. Wave 2 weighting and non-response: Australian Institute of Family Studies; 2007. [Google Scholar]
- 55.McCutcheon AL. Latent class analysis: Sage; 1987. [Google Scholar]
- 56.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 57.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep medicine. 2011;12:478–82. [DOI] [PubMed] [Google Scholar]
- 58.Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:964–71. [DOI] [PubMed] [Google Scholar]
- 59.Tikotzky L, Sadeh A, Glickman-Gavrieli T. Infant sleep and paternal involvement in infant caregiving during the first 6 months of life. Journal of Pediatric Psychology. 2010;36:36–46. [DOI] [PubMed] [Google Scholar]
- 60.Millikovsky-Ayalon M, Atzaba-Poria N, Meiri G. The role of the father in child sleep disturbance: child, parent, and parent–child relationship. Infant Mental Health Journal. 2015;36:114–27. [DOI] [PubMed] [Google Scholar]
- 61.Kouros CD, El-Sheikh M. Within-family relations in objective sleep duration, quality, and schedule. Child development. 2017;88:1983–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rhoades KA, Leve LD, Harold GT, Mannering AM, Neiderhiser JM, Shaw DS, et al. Marital hostility and child sleep problems: direct and indirect associations via hostile parenting. Journal of Family Psychology. 2012;26:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kelly RJ, El-Sheikh M. Longitudinal relations between marital aggression and children’s sleep: The role of emotional insecurity. Journal of Family Psychology. 2013;27:282. [DOI] [PubMed] [Google Scholar]
- 64.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. Journal of Family Psychology. 2007;21:67. [DOI] [PubMed] [Google Scholar]
- 65.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep medicine reviews. 2012;16:129–36. [DOI] [PubMed] [Google Scholar]
- 66.Van Dyk TR, Becker SP, Byars KC. Mental Health Diagnoses and Symptoms in Preschool and School Age Youth Presenting to Insomnia Evaluation: Prevalence and Associations with Sleep Disruption. Behavioral sleep medicine. 2018:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Garner AS, Shonkoff JP, Siegel BS, Dobbins MI, Earls MF, McGuinn L, et al. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129:e224–e31. [DOI] [PubMed] [Google Scholar]
- 68.Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131:319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Frontiers in psychiatry. 2018;8:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kallem S, Matone M, Boyd RC, Guevara JP. Mothers’ Mental Health Care Use After Screening for Postpartum Depression at Well-Child Visits. Academic pediatrics. 2018;18:20761–7. [DOI] [PubMed] [Google Scholar]
- 71.Reilly N, Harris S, Loxton D, Chojenta C, Forder P, Austin M-P. The impact of routine assessment of past or current mental health on help-seeking in the perinatal period. Women and Birth. 2014;27:e20–e7. [DOI] [PubMed] [Google Scholar]
- 72.Schmied V, Langdon R, Matthey S, Kemp L, Austin M-P, Johnson M. Antenatal psychosocial risk status and Australian women’s use of primary care and specialist mental health services in the year after birth: a prospective study. BMC women’s health. 2016;16:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hiscock H, Bayer JK, Hampton A, Ukoumunne OC, Wake M. Long-term mother and child mental health effects of a population-based infant sleep intervention: cluster-randomized, controlled trial. Pediatrics. 2008;122:e621–e7. [DOI] [PubMed] [Google Scholar]
- 74.Adams LA, Rickert VI. Reducing bedtime tantrums: comparison between positive routines and graduated extinction. Pediatrics. 1989;84:756–61. [PubMed] [Google Scholar]
- 75.Sciberras E, Mulraney M, Mensah F, Oberklaid F, Efron D, Hiscock H. Sustained impact of a sleep intervention and moderators of treatment outcome for children with ADHD: a randomised controlled trial. Psychological medicine. 2019:1–10. [DOI] [PubMed] [Google Scholar]
- 76.Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. Jama. 2010;303:1961–9. [DOI] [PubMed] [Google Scholar]
- 77.Nelson TD, Van Dyk TR, McGinnis JC, Nguyen AV, Long SK. Brief sleep intervention to enhance behavioral parent training for noncompliance: Preliminary findings from a practice-based study. Clinical Practice in Pediatric Psychology. 2016;4:176. [Google Scholar]
- 78.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2:38–48. [DOI] [PubMed] [Google Scholar]
- 79.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-L, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological medicine. 2002;32:959–76. [DOI] [PubMed] [Google Scholar]