Abstract
Background.
Cannabis and tobacco co-use is a growing concern, yet little is known about its developmental course or associated outcomes during emerging adulthood. This study examines developmental trajectories of cannabis and tobacco co-use from adolescence to emerging adulthood, associations of co-use trajectories with four domains of functioning, and differences across racial/ethnic groups.
Methods.
Survey data come from a racially/ethnically diverse and predominantly California-based cohort that completed 10 surveys from 2008 (wave 1: mean age 11.5; n = 6,509) to 2018 (wave 10: mean age 20.7; n = 2,429). Co-use was defined as use of both cannabis and tobacco (cigarettes or smokeless tobacco) in the past 30 days. Trajectories of use were examined using latent growth modeling in a structural equation modeling framework.
Results.
Prevalence of cannabis and tobacco co-use increased from 0.3% at wave 1 to 9.5% at wave 10, with average probabilities of co-use higher among non-Hispanic white versus Hispanic or Asian participants. Higher average probability of co-use was associated with greater delinquency, more mental health symptoms, and poorer physical health during emerging adulthood. Higher rate of change in the probability of co-use over time was associated with greater delinquency, but better social functioning and less physical ailments. There was some evidence of racial/ethnic disparities in functioning, even at similar levels of co-use.
Conclusions.
Cannabis and tobacco co-use deserves greater attention, especially regarding its effects on functioning during emerging adulthood. Results also emphasize the need for future research to focus on racial/ethnic disparities related to co-use and associated outcomes.
Keywords: cannabis, marijuana, tobacco, co-use, trajectories, race/ethnicity, emerging adults
1. INTRODUCTION
The past decade has witnessed an overall upward trend in the co-use of cannabis and tobacco among adults; that is, use of both substances at any point (and not necessarily at the same time) within a specified period such as the past month (Schauer et al., 2015). Existing research indicates a high degree of overlap between cannabis and tobacco use (Agrawal et al., 2012; Cobb et al., 2018; Ramo et al., 2012). For example, studies have found that 80%−90% of individuals who use cannabis also report using tobacco (Agrawal et al., 2011; Tucker et al., in press). In a national survey of 1,987 past 30-day cigarette smokers aged 18–25 years, 53% also reported cannabis use in that time frame (Ramo et al., 2013). Co-use is an important public health concern due to its association with greater nicotine and cannabis dependence (Panlilio et al., 2013; Schauer et al., 2017; Wang and Cataldo, 2016), and although evidence is mixed, with poorer cessation outcomes (Peters et al., 2012; Ramo et al., 2013; Vogel et al., 2018).
Cannabis and tobacco use both increase during adolescence, reaching their highest levels by emerging adulthood (Schulenberg et al., 2018). For example, data from the National Survey on Drug Use and Health (NSDUH) indicate that past month cannabis and tobacco use is reported by 6.5% and 4.9% (respectively) of 12–17 year olds (Substance Abuse and Mental Health Services Administration, 2018). Past month use of both substances (including blunts) was reported by 5% of 12–17 year olds, based on 2013–2014 NSDUH data (Schauer and Peters, 2018). In contrast, past month cannabis and tobacco use is reported by 22% and 29% (respectively) of 18–25 year olds (Substance Abuse and Mental Health Services Administration, 2018), with rates of co-use highest among emerging adults compared with other adult age groups (Schauer et al., 2015). Longitudinal data on age-related differences in cannabis and tobacco co-use is needed to better understand its developmental course from adolescence to emerging adulthood. Further, few studies have examined racial/ethnic differences in co-use and potential disparities related to consequences of co-use. Cross-sectional studies have found that young people in certain racial/ethnic minority groups, notably those who self-identify as black, are more likely than to engage in co-use (Ramo et al., 2012; see also Montgomery and Mantey, 2018). This is somewhat surprising given that epidemiological data tend to show higher rates of tobacco use among non-Hispanic white than black (and Hispanic) young people (Center for Behavioral Health Statistics and Quality, 2017). However, such studies preclude our ability to make meaningful interpretations about racial/ethnic differences in co-use over time. Longitudinal data are lacking on racial/ethnic differences in co-use that can inform efforts to reduce health disparities, especially research that includes Hispanics and Asians.
Furthermore, little attention has focused on the potential effects of co-use on functioning during emerging adulthood and whether there are disparities related to co-use. The adverse physical health effects of tobacco use, especially cigarette smoking, are well-established (U.S. Department of Health and Human Services, 2014), and there is also evidence for certain health risks associated with cannabis use (Hall, 2015). Although more research is needed, the increasing prevalence of co-use has raised concerns that it may have additive or interactive effects, compounding health risks associated with using either product alone (Meier and Hatsukami, 2016). Cannabis and tobacco co-use among adolescents and adults has also been associated with greater psychiatric disorders and psychosocial problems (Peters et al., 2014; Ramo et al., 2012), including risky behavior such as driving after using cannabis (Tucker et al., in press), and academic problems (Hernandez-Serrano et al., 2018; Pulvers et al., 2018). Although informative, this small and mostly cross-sectional literature has been limited in terms of areas of functioning that have been examined, assessment of disparities in use, and a lack of focus on emerging adults, the age group most at risk for co-use.
This study extends research on cannabis and tobacco co-use in three important respects. First, it examines trajectories of cannabis and tobacco co-use over a 10-year period from early adolescence to emerging adulthood, and tests whether racial/ethnic differences exist in the probability of co-use and rate of change in probability of co-use. Second, this study tests whether the probability of co-use, and rate of change in the probability of co-use, over the 10-year period are associated with key indicators of functioning in emerging adulthood. Finally, it focuses on disparities by examining whether there are racial/ethnic differences in functioning, given similar levels of co-use across racial/ethnic groups. We note that our prior work on trajectories of cannabis use (D’Amico et al., 2016) and cigarette smoking (Dunbar et al., 2018), which did not consider co-use of these substances, found that greater use of each substance was associated with worse functioning during late adolescence, and racial/ethnic minority youth also tended to report poorer outcomes across multiple domains compared to white youth after controlling for patterns of use. Thus, to explore whether co-use of cannabis and tobacco may pose unique risks, we compare results for cannabis and tobacco co-use to those for cannabis only use and tobacco only use. For the purposes of this study, we focus on co-use of cannabis with cigarettes and/or smokeless tobacco. E-cigarette products were not widely available or used by adolescents during the first several years of this study; as such, they were not assessed until wave 7, which precluded modeling trajectories of their use across the full study period in the present study.
2. METHODS
2.1. Sample and Procedures
Participants were from two cohorts of students who were in 6th and 7th grade in 2008 (n = 6,509), initially recruited from 16 middle schools in Southern California as part of a substance use prevention program, CHOICE (D’Amico et al., 2012). These cohorts were followed through 2018 (10 waves of data). All participants consented to the study, and all procedures were approved by the RAND IRB. Study procedures are reported in detail elsewhere (D’Amico et al., 2012). Briefly, participants completed waves 1 through 5 (wave 1: Fall 2008; wave 2: Spring 2009; wave 3: Fall 2009; wave 4: Spring 2010; wave 5: Spring 2011) during physical education classes at 16 middle schools. Follow-up rates ranged from 74–90% during this time period, excluding new youth that could have come in at a subsequent wave. Adolescents transitioned from these middle schools to over 200 high schools following wave 5 and were subsequently re-contacted and re-consented to complete annual web-based surveys. At wave 6 (Spring 2013-Spring 2014), 61% of the sample participated in the follow-up survey. At subsequent annual assessments, we retained 80% of the sample from waves 6–7, 91% of the sample from waves 7–8, 89% of the sample from waves 8–9, and 90% of the sample from waves 9–10. At wave 10, n = 2,429 participants completed the survey. Demographics (e.g., gender, race/ethnicity, employment) and substance use at the prior wave (e.g., alcohol, cigarettes, cannabis) did not predict attrition at wave 10, similar to what we have found at earlier waves (D’Amico et al., 2018; D’Amico et al., 2016).
2.2. Measures
Cannabis and tobacco use at waves 1–10.
During waves 1–10, use of cigarettes, smokeless tobacco, and cannabis were assessed by asking: “During the past month, how many days did you use cigarettes [smokeless tobacco (dip, chew or snuff)] [marijuana (pot, weed, grass, hash, bud, sins)]?” Responses ranged from 0 days to 20–30 days. Due to considerable skew and predominance of low-frequency responses in earlier waves, responses were dichotomized to indicate any (1) vs. no (0) use of each substance. Participants were classified at each wave as engaging in: tobacco use, but no cannabis use; cannabis use, but no tobacco use; or tobacco and cannabis co-use (i.e., use of both a tobacco product (cigarettes and/or smokeless tobacco) and cannabis in the past 30 days).
Socio-demographics and race/ethnicity.
Variables included self-reported age, gender, mother’s education, and race/ethnicity. Participants were classified into one of six racial/ethnic groups: non-Hispanic white (reference group), non-Hispanic Black, Hispanic, non-Hispanic Asian, multiethnic (more than one race/ethnicity), and any other race/ethnicities.
Delinquency at wave 10.
Six items asked about frequency with which participants engaged in various problem behaviors in the past year (being involved in fights, stealing, property damage, graffiti, getting into trouble with the police, being fired from a job), each rated on a 6-point scale (1 = not at all to 6 = 20 or more times). Scores were summed, with higher values indicating greater engagement in delinquent behaviors in the past year (range = 3–36, mean = 6.64, SD = 2.35).
Mental and physical health at wave 10.
Two mental health measures assessed symptoms in the past two weeks on a scale from 0 = not at all to 3 = nearly every day. The Patient Health Questionnaire – 8 item (PHQ-8; Kroenke et al., 2009; α = 0.92) assessed eight symptoms of depression such as feeling down, depressed, or hopeless and having little interest or pleasure in doing things (range = 0–24, mean = 5.76, SD = 5.73). The Generalized Anxiety Disorder – 7 item (GAD-7; Spitzer et al., 2006; α = 0.94) assessed seven symptoms of anxiety such as feeling nervous, anxious, or on edge and not being able to stop or control worrying (range = 0–21, mean = 5.25, SD = 5.56).
Physical ailments/symptoms were assessed with four items (Kroenke et al., 2002) asking participants how bothered they had been in the previous 4 weeks by four symptoms: stomach pain, headaches, feeling tired or having low energy and trouble sleeping. Responses were dichotomized as 0 = not at all bothered and 1= bothered a little or a lot, and summed, with higher scores indicating more ailments/symptoms (range = 0–3, mean = 2.01, SD = 1.42). Physical health was a combination of self-perceived overall health (1 = excellent to 5 = poor) and two items from the PROMIS pediatric physical function scale (DeWitt et al., 2011): ability to physically engage in activities that one enjoys (1 = with no trouble to 5 = not able to do), and ability to participate in sports and exercise similar to their peers (1 = with no trouble to 5 = not able to do). Items were reverse scored and summed such that higher scores indicated better physical health (range = 3–15, mean = 12.26, SD = 2.30).
Social functioning at wave 10.
Past month social functioning was assessed using eight items from the PROMIS Peer Relationships Short Form item bank (DeWalt et al., 2013). Sample items include “I was able to count on my friends” and “I felt accepted by other kids/other people my age,” each rated on a 5-point scale (0 = never to 4 = always; α = 0.96). Scores of 0 to 35 were transformed to a z-score per the scoring instructions, with higher values indicating better social functioning (range = 17.67–52.64, mean = 42.54, SD = 8.07).
2.3. Analysis
To examine trajectories of cannabis and tobacco co-use, cannabis only use, and tobacco only use we estimated separate latent growth models for each type of substance use (e.g., co-use, cannabis only use, tobacco only use) in a structural equation modeling framework, using Mplus version 8 (Muthén and Muthén, 2011). This framework allows change itself to serve as both an outcome and a predictor. We used weighted least squares with mean and variance adjusted estimator (WLSMV), which can accommodate categorical outcomes, missing data, and provide unbiased and consistent estimates as well as model fit indices (Asparouhov and Muthén, 2010). In latent growth modeling, the model intercept represents the predicted value of the outcome when the predictor is equal to zero. Due to assessment waves being unevenly spaced across years, this was set to 4.25 years after baseline assessment (i.e., time was centered at the middle of assessment waves) (D’Amico et al., 2016). There were 8.5 total years between waves 1 and 10, treated as follows in the growth models: wave 1 = −4.25 years, wave 2 = −3.75 years, wave 3 = −3.25 years, wave 4 = −2.75 years, wave 5 = −1.75 years, wave 6 = 0.25 years, wave 7 = 1.25 years, wave 8 = 2.25 years, wave 9 = 3.25 years, and wave 10 = 4.25 years. The intercept can be interpreted as the average probability of use (i.e., co-use, cannabis only, tobacco only), and the slope represents change in probability of use over time.
Longitudinal analyses then tested for intercept and slope differences by race/ethnicity (dummy coded, with white as the reference category) to determine whether group differences exist in probability of use and rate of change in probability of use for co-use, cannabis only use, and tobacco only use, separately. The next step involved testing whether slope and intercept for co-use, cannabis only use, and tobacco only use were associated with functioning at wave 10 across the full sample. Finally, we examined racial/ethnic differences in functioning by estimating models that controlled for slope and intercept of co-use, cannabis only use, and tobacco only use predicting these outcomes, looking at the direct effect of race/ethnicity on each outcome. We used a sequelae of change model (Duncan et al., 1999) which, in structural equation modeling, allows the random effect of rate of change of co-use to function as both an outcome (as it is conventionally modeled) and a predictor of subsequent outcomes. All models adjusted for age, gender, mother’s education, and intervention group at wave 1.
3. RESULTS
3.1. Sample characteristics
The wave 10 sample was 50.2% male, 15.7% white, 53.7% Hispanic, 16.1% Asian, 9.5% multiethnic, 3.2% Black, and 1.6% other races/ethnicities. Average age was 20.7 (SD = 0.70). Nearly half (48.4%) reported that their mother had a college degree. Table 1 shows cannabis and tobacco co-use, cannabis only use, and tobacco only use from waves 1–10. Across the 10 waves, average cannabis and tobacco co-use ranged from 0.3–9.5%, cannabis only use ranged from 0.4–22.4%, and tobacco only use ranged from 0.7–4.7%. Initial growth models for each type of use (e.g., tobacco only) fit the data well: co-use (χ2(50) = 102.686, RMSEA = 0.013, CFI = .98); cannabis use only (χ2(50) = 199.99, RMSEA = .021, CFI = .92); and tobacco use only (χ2(50) = 60.10, RMSEA = .006, CFI = .98). Specifically, there was a significant increase over time in the probability of co-use (slope = 0.14), cannabis only use (slope = 0.18), and tobacco only use (slope = 0.08).
Table 1.
Past month use of tobacco and cannabis by study wave (N = 6,509)
| Tobacco and Cannabis | Cannabis Only | Tobacco Only | ||||||
|---|---|---|---|---|---|---|---|---|
| Wave | % (N) | % (N) | % (N) | |||||
| 1 | 0.3% | (16) | 0.4% | (25) | 0.7% | (42) | ||
| 2 | 1.2% | (57) | 1.7% | (95) | 1.0% | (57) | ||
| 3 | 1.1% | (55) | 1.4% | (74) | 1.1% | (57) | ||
| 4 | 1.6% | (77) | 3.1% | (152) | 0.8% | (40) | ||
| 5 | 1.9% | (74) | 4.3% | (165) | 1.2% | (45) | ||
| 6 | 3.0% | (75) | 8.1% | (205) | 1.0% | (26) | ||
| 7 | 4.7% | (117) | 12.9% | (299) | 1.9% | (47) | ||
| 8 | 7.5% | (187) | 16.2% | (406) | 2.8% | (69) | ||
| 9 | 9.9% | (239) | 18.8% | (454) | 3.0% | (72) | ||
| 10 | 9.5% | (231) | 22.4% | (541) | 4.7% | (114) | ||
Note. Past month percentages generated with denominators from each respective wave (i.e., not restricted to wave 10 participants only).
3.2. Racial/ethnic differences in the intercept and slope of trajectories
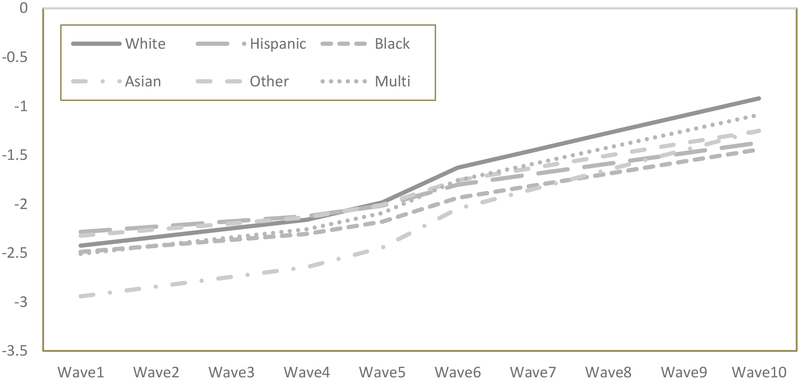
The first models examined racial/ethnic differences in the intercept and slope for co-use, cannabis only use, and tobacco only use across waves 1–10 (Table 2). In these models, the intercept represents average probability of use and slope represents change in probability of use over time, both modeled as a logistic function. Overall fit was excellent for co-use (χ2(138) = 170.41, p<.05; RMSEA = 0.006, CFI = 0.99), cannabis only use (χ2(138) = 287.10, p < .01; RMSEA = 0.013, CFI = 0.94), and tobacco only use (χ2(138) = 148.44, p = .26; RMSEA = 0.003, CFI = 0.98). For all three use types, race/ethnicity predicted average probability of use (intercept) and change in probability of use (slope) over time. Compared to white participants (the reference group), average probabilities of co-use were lower for Asians and Hispanics. Further, average probability of cannabis only use and tobacco only use were both lower for Asians compared to whites. Race/ethnicity also predicted change in probability of co-use and cannabis only use, such that Hispanic participants showed lower rates of change (i.e., less steep slopes) in their probabilities of co-use and cannabis only use compared to whites. Co-use trajectories by race/ethnicity are presented in Figure 1.
Table 2.
Parameter estimates of race/ethnicity predicting intercept and slope of cannabis and tobacco co-use, cannabis only, and tobacco only trajectories (waves 1–10)
| Cannabis and Tobacco Co-Use | Cannabis Only | Tobacco Only | ||||||
|---|---|---|---|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | Intercept | Slope | |||
| Race/ethnicity | Est. | Est. | Est. | Est. | Est. | Est. | ||
| White (reference) | -- | -- | -- | -- | -- | -- | ||
| Asian | −0.55* | 0.19 | −0.71* | 0.24 | −0.50* | 0.22 | ||
| Black | −0.38 | −0.35 | 0.20 | 0.34 | −0.08 | −0.49 | ||
| Hispanic | −0.17* | −0.29* | −0.03 | −0.24* | −0.05 | −0.25 | ||
| Multiethnic | −0.13 | 0.001 | −0.14 | −0.09 | −0.03 | −0.03 | ||
| Other | −0.17 | −0.33 | −0.30 | −0.28 | 0.10 | −0.34 | ||
Note. Est. = Standardized parameter estimate. Results are from latent growth models with logistic function examining race/ethnicity as a predictor of slope and intercept of past month use, controlling for age, gender, mother’s education, and intervention group at wave 1. Intercept represents average probability of use. Slope represents the change in probability of use over time.
p < .05.
Figure 1.
Trajectories of cannabis and tobacco co-use by racial/ethnic groups
3.3. Longitudinal associations of trajectories with outcomes at wave 10
The next models examined intercept and slopes of co-use, cannabis only use, and tobacco only use from Model 1 as predictors of outcomes at wave 10 (Table 3) in the full sample. Model fit was excellent, indicating that the linear logistic model was a good representation of the data for co-use (χ2(205) = 288.01, p < .05; RMSEA = 0.008; CFI = 0.99), cannabis only use (χ2(205) = 389.76, p < .05; RMSEA = 0.012; CFI = 0.97), and tobacco only use (χ(205) = 239.69, p = .05; RMSEA = 0.005; CFI = 0.99). For emerging adult functioning, higher average probability of use was associated with more frequent delinquency (co-use, cannabis, tobacco); more mental health symptoms and poorer health (co-use, tobacco); and more physical ailments (co-use). Higher rates of change in use were associated with better social functioning (all substances), less physical ailments (co-use), and delinquent behavior (more in the case of co-use, less in the case of cannabis use).
Table 3.
Parameter estimates for longitudinal effects of cannabis and tobacco co-use, cannabis use only, and tobacco use only at waves 1–10 on wave 10 functioning
| Cannabis and Tobacco Co-Use | Cannabis only | Tobacco only | ||||
|---|---|---|---|---|---|---|
| Functioning | Est. | Est. | Est. | Est. | Est. | Est. |
| Delinquency | 0.24* | 0.18* | 0.15* | −0.13* | 0.08* | 0.11 |
| Anxiety (GAD) | 0.10* | 0.05 | −0.01 | 0.00 | 0.09* | 0.12 |
| Depression (PHQ) | 0.14* | −0.01 | 0.03 | −0.04 | 0.15* | 0.10 |
| Physical ailments | 0.18* | −0.20* | 0.05 | −0.02 | 0.07 | 0.08 |
| Physical health | − 0.10* | 0.01 | 0.01 | −0.02 | −0.13* | 0.06 |
| Social functioning | − 0.04 | 0.20* | −0.02 | 0.21* | −0.06 | 0.18* |
Note. Est = Standardized parameter estimate. Models assessed the direct effects of both slope and intercept of use trajectories from waves 1–10 on each outcome, controlling for age, gender, race/ethnicity, mother’s education, and intervention group at wave 1.
p < .05.
3.4. Racial/ethnic differences in wave 10 outcomes controlling for trajectories of use
Finally, we examined direct effects of race/ethnicity on functioning, controlling for both the average (intercept) and the rate of change (slope) of probability of use across waves 1–10 (Table 4). For each model (i.e., cannabis and tobacco co-use, cannabis only use, tobacco only use), we controlled for corresponding intercept and slope. These models can be interpreted as a test of the association between race/ethnicity and functioning outcomes at wave 10, assuming all groups demonstrated the same trajectories (i.e., fixed intercept and slope) of probability of use over time (waves 1–10). For the cannabis and tobacco co-use model, after controlling for corresponding trajectories (intercept and slope), multiethnic participants reported greater anxiety and depression compared to whites. In addition, after controlling for co-use trajectories, Hispanic participants reported higher delinquency, poorer health, and fewer physical ailments compared to whites. We found a similar pattern for mental and physical health in the cannabis use model, and for mental health in the tobacco use model.
Table 4.
Parameter estimates for direct effects of race/ethnicity on wave 10 outcomes, controlling for trajectories of use
| Delinquency | Anxiety | Depression | Physical ailments | Physical health | Social functioning | |
|---|---|---|---|---|---|---|
| Cannabis and tobacco co-use | ||||||
| White (ref) | -- | -- | -- | -- | -- | -- |
| Hispanic | 0.13* | 0.02 | 0.04 | −0.15* | −0.14* | 0.00 |
| Black | 0.49 | 0.10 | 0.19 | −0.21 | −0.19 | −0.16 |
| Asian | −0.06 | 0.01 | 0.10 | 0.13 | −0.13 | −0.08 |
| Multiethnic | 0.01 | 0.19* | 0.20* | 0.04 | −0.14 | −0.13 |
| Other | −0.10 | −0.21 | −0.04 | −0.46 | −0.06 | 0.14 |
| Cannabis use | ||||||
| White (ref) | -- | -- | -- | -- | -- | -- |
| Hispanic | 0.01 | −0.02 | 0.01 | −0.12* | −0.13* | −0.001 |
| Black | 0.35* | 0.05 | 0.16 | −0.20 | −0.17 | −0.28* |
| Asian | −0.02 | −0.04 | 0.05 | 0.04 | −0.06 | −0.08 |
| Multiethnic | −0.01 | 0.18* | 0.18* | 0.02 | −0.13 | −0.09 |
| Other | −0.20 | −0.24 | −0.07 | −0.40* | −0.04 | 0.11 |
| Tobacco use | ||||||
| White (ref) | -- | -- | -- | -- | -- | -- |
| Hispanic | 0.07 | 0.02 | 0.05 | −0.10 | −0.12 | −0.01 |
| Black | 0.39* | 0.11 | 0.21 | −0.16 | −0.15 | −0.13 |
| Asian | −0.14 | −0.01 | 0.08 | 0.01 | −0.15* | −0.09 |
| Multiethnic | −0.01 | 0.19* | 0.18* | 0.02 | −0.13 | −0.11 |
| Other | −0.16 | −0.21 | −0.05 | −0.39 | −0.02 | 0.13 |
Note. Standardized parameter estimates. Models assessed the direct effect of race/ethnicity on each outcome (white specified as reference group), controlling for both slope and intercept of use trajectories from waves 1–10, as well as age, mother’s education, and intervention group at wave 1.
p < .05.
4. DISCUSSION
The plethora of recent literature reviews on cannabis and tobacco co-use (e.g., Agrawal et al., 2012; Meier and Hatsukami, 2016; Montgomery et al., 2017; Peters et al., 2012; Ramo et al., 2012; Schauer et al., 2017) speaks to the timeliness of this topic, given the rapidly changing recreational cannabis legalization landscape, as well as highlights gaps in existing knowledge of the developmental trajectory of co-use and its potential effects on functioning during emerging adulthood. Results from this 10-year longitudinal study show that cannabis and tobacco co-use steadily increases from middle school to emerging adulthood, with a steeper increase occurring during the transition to young adulthood than during adolescence. National data indicate that cannabis and tobacco co-use peaks between the ages of 18 and 25 (Schauer et al., 2015). In our sample, by age 21 nearly 1 in 10 participants reported engaging in co-use during the past 30 days. Cannabis and tobacco co-use is a fairly common form of substance use among emerging adults and highlights the importance of addressing co-use in intervention efforts with this population.
Prior research has shown that young people who co-use cannabis and tobacco are more likely than those who use cannabis only to engage in delinquent and other problem behaviors such as heavy alcohol use (Schauer and Peters, 2018), driving after using cannabis (Tucker et al., in press), and academic problems (Hernandez-Serrano et al., 2018; Pulvers et al., 2018). The present study extends this small and largely cross-sectional literature by utilizing 10 wave of data to show that individuals with a higher average probability of co-use, as well as those with a greater increase in the probability of co-use over time (i.e., more positive slope), also tend to report more problematic behaviors in emerging adulthood such as fighting, stealing, getting into trouble with the police, and being fired from a job. It is noteworthy that a similar finding did not emerge when considering tobacco use only or cannabis use only, especially given prior studies indicating that adolescents’ engagement in delinquency is associated with their trajectories of cannabis use and cigarette smoking (D’Amico et al., 2016; Dunbar et al., 2018). Perhaps as young people mature and “age out” of delinquency (Sweeten et al., 2013), use of each substance alone becomes less strongly related to these sorts of behavioral problems; however, individuals who co-use these two substances may continue to exhibit a range of risk behaviors. While documenting these associations is a necessary and important first step, future research should focus on better understanding why and how co-use trajectories may be associated with delinquency in emerging adulthood, including whether certain types of co-use (e.g., those who use both substances together vs. only on separate occasions) have a higher risk profile (Tucker et al., in press).
Prior research has also found that cannabis and tobacco co-use among adolescents and adults is associated with poorer self-reported health (Peters et al., 2014; Ramo et al., 2012). Results from this longitudinal study shed further light on these associations by underscoring that whether or not a person co-uses over time is important in predicting poorer mental and physical health outcomes in emerging adulthood. It is worth noting that the associations of these health outcomes with co-use trajectories generally mirror those found for tobacco use only (whereas few associations were found with cannabis use only). This may suggest that among those who are using both substances, tobacco use may be more strongly associated than cannabis use with adverse health outcomes.
Despite higher levels of depression and anxiety symptoms associated with cannabis and tobacco co-use in this study, co-use was not associated with poorer social functioning. To the contrary, a higher rate of change in co-use (as well as cannabis only use and tobacco only use) was associated with better social functioning in our sample of emerging adults. This might reflect something unique to this developmental period since neither D’Amico et al.’s (2016) study of cannabis use nor Dunbar et al.’s (2018) study of cigarette smoking reported a similar finding in late adolescence. Social smoking is common among young people (Villanti et al., 2017), and the use of cannabis typically occurs in social settings (Buckner et al., 2012; McCabe et al., 2014). Although we do not know whether emerging adults who derive social benefits from co-use generally self-identify as “social users,” those who do may be at higher risk for progression to more regular use and potential problems with cessation (Song and Ling, 2011; Villanti et al., 2017).
Finally, racial/ethnic differences in co-use trajectories showed that white emerging adults fared worse, with the average probability of co-use being higher among white versus Hispanic or Asian participants, and rate of change in co-use being higher among white versus Hispanic participants. However, after controlling for patterns of co-use, racial/ethnic minority participants reported poorer outcomes in multiple domains compared to whites. Effects were concentrated within two ethnic subgroups: multiethnic and Hispanic participants. Multiethnic participants reported greater anxiety and depression compared to whites after controlling for patterns of co-use (a result also found when adjusting for cannabis only use and tobacco only use), and Hispanic participants reported more delinquency and poorer health than whites after controlling for patterns of co-use. Results add to a growing literature indicating that substance use may differentially affect racial/ethnic subgroups (Centers for Disease Control and Prevention, 2013), and that with similar amounts of use, racial/ethnic minority groups tend to report worse outcomes, even as early as adolescence and emerging adulthood (D’Amico et al., 2016; Dunbar et al., 2018). In this case, cannabis and tobacco co-use appears to be particularly problematic for multiethnic and Hispanic young people, two of the most rapidly growing racial/ethnic groups in the U.S. (Child Trends, 2018; Jones and Bullock, 2012), emphasizing the importance of addressing co-use for these particular subgroups to address disparities in health and psychosocial functioning. Of course, it may also be the case that variables not assessed in this study (e.g., discrimination, access to care, economic instability, environmental factors) may partly account for findings. Further longitudinal research, particularly focusing on adolescents and emerging adults, is needed to identify and understand the effects of substance use on diverse groups in order to meet national priorities for reducing substance use-related disparities (U.S. Department of Health and Human Services, 2016).
In interpreting results, some limitations should be noted. Given that co-use behavior varies significantly worldwide, the use of a predominantly California-based sample limits generalizability of findings to other geographic regions. However, it also afforded us the opportunity to examine racial/ethnic differences in co-use and offered some standardization of both cannabis and tobacco policies applied to all participants in the study. Another limitation is that we did not include vaping in the current study because we did not have data to model it across all waves. The study is also limited in that the only measure of co-use available across waves was whether participants used both substances at some point during a particular period of time (in this case, the past 30 days). Although this is what is typically assessed in studies of co-use, it may obscure potentially important differences between types of co-use, such as sequential (use of one substance right after the other) or co-administration (mixing both substances together) (Tucker et al., in press). Finally, the use of dichotomized indicators of cannabis and tobacco use, while necessary for statistical analysis given the young age of the sample at earlier waves, does not allow us to account for potentially important differences between participants in frequency of using these substances.
In conclusion, this study addresses an important gap in the literature on cannabis and tobacco co-use by examining the developmental course of co-use from adolescence to emerging adulthood, demonstrating how trajectories are associated with key emerging adult outcomes, and identifying racial/ethnic disparities in both co-use and outcomes. One important direction for future research is to better understand the developmental course of co-use involving other forms of administration (e.g., vaping), as well as different subtypes of co-use (e.g., those who use both products only on separate occasions versus those who use them together in some way). Differences in how cannabis and tobacco products are used together likely has important implications for effects of co-use on functioning during adolescence and the transition to young adulthood. In addition, results indicate that cannabis and tobacco co-use may have a differential effect across subgroups of young people. As such, it is important for future research to not only continue examining racial/ethnic differences, but also to examine other disparities involving vulnerable and underserved populations such as sexual/gender minority youth and those experiencing homelessness.
HIGHLIGHTS.
Co-use prevalence increased from 0.3% at W1 (age 11.5) to 9.5% at W10 (age 20.7)
Probability of co-use was higher among White than Hispanic or Asian participants
Co-use was generally associated with poorer functioning in emerging adulthood
There is some evidence of racial/ethnic disparities in co-use related outcomes
Acknowledgements:
We thank the districts and schools who participated and supported this project. We would also like to thank Kirsten Becker and Jennifer Parker for overseeing the data collection.
Role of Funding Source. This research was supported by the California Tobacco-Related Disease Research Grants Program Office of the University of California under Grant 26IR-0011 to Tucker, as well as grants from the National Institute of Alcohol Abuse and Alcoholism (R01AA016577, R01AA020883, R01AA025848) to D’Amico.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest. No conflict declared
5. REFERENCES
- Agrawal A, Budney AJ, Lynskey MT, 2012. The co-occurring use and misuse of cannabis and tobacco: A review. Addiction. 107, 1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Scherrer JF, Lynskey MT, Sartor CE, Grant JD, Haber JR, Madden PAF, Jacob T, Bucholz KK, Xian H, 2011. Patterns of use, sequence of onsets and correlates of tobacco and cannabis. Addict Behav. 36, 1141–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, Muthén B, 2010. Weighted least squares estimation with missing data. http://www.statmodel.com/download/GstrucMissingRevision.pdf. accessed on May 22 2018.
- Buckner JD, Crosby RD, Silgado J, Wonderlich SA, Schmidt NB, 2012. Immediate antecedents of marijuana use: An analysis from ecological momentary assessment. J Behav Ther Exp Psy. 43, 647–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2017. 2016 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2013. Health disparities and inequalities report. MMWR Morb Mortal Wkly Rep. 62. [Google Scholar]
- Child Trends, 2018. Racial and ethnic composition of the child population. https://www.childtrends.org/indicators/racial-and-ethnic-composition-of-the-child-population. accessed on February 12 2019.
- Cobb CO, Soule EK, Rudy AK, Sutter ME, Cohn AM, 2018. Patterns and correlates of tobacco and cannabis co-use by tobacco product type: Findings from the Virginia Youth Survey. Subst Use Misuse. 53, 2310–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Rodriguez A, Tucker JS, Pedersen ER, Shih RA, 2018. Planting the seed for marijuana use: Changes in exposure to medical marijuana advertising and subsequent adolescent marijuana use, cognitions, and consequences over seven years. Drug Alcohol Depen. 188, 385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Ewing BA, Shih RA, Pedersen ER, 2016. Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17 years. Addiction. 111, 1825–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Zhou AJ, Shih RA, Green HD Jr., 2012. Preventing alcohol use with a voluntary after-school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prev Sci. 13, 415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Thissen D, Stucky BD, Langer M, Morgan DE, Irwin D, Lai J, Yeatts K, Gross H, Taylor O, Varni J, 2013. PROMIS pediatric peer relationships scale: Development of a peer relationships item bank as part of social health measurement. Health Psychol. 32, 1093–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWitt EM, Stucky BD, Thissen D, Irwin DE, Langer M, Varni JW, DeWalt DA, 2011. Construction of the eight item PROMIS Pediatric Physical Function Scales: Built using item response theory. J Clin Epidemiol. 64, 794–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar MS, Tucker JS, Ewing BA, Parast L, Pedersen ER, Rodriguez A, D’Amico EJ, 2018. Ethnic differences in cigarette use trajectories and health, psychosocial, and academic outcomes. J Adolescent Health. 62, 327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA, Li F, Alpert A, 1999. An introduction to latent variable growth curve modeling: Concepts, issues, and applications. Lawrence Erlbaum Associates, Mahwah, NJ. [Google Scholar]
- Hall W, 2015. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 110, 19–35. [DOI] [PubMed] [Google Scholar]
- Hernandez-Serrano O, Gras ME, Font-Mayolas S, 2018. Concurrent and simultaneous use of cannabis and tobacco and its relationship with academic achievement amongst university students. Behav Sci-Basel. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones N, Bullock J, 2012. The two or more races population: 2010. 2010 Census Brifs. U.S. Census Bureau; https://www.census.gov/prod/cen2010/briefs/c2010br-13.pdf [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH, 2009. The PHQ-8 as a measure of current depression in the general population. J Affect Disorders. 114, 163–173. [DOI] [PubMed] [Google Scholar]
- Kroenke KS, Williams RL, Janet BW, 2002. Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 64, 258–266. [DOI] [PubMed] [Google Scholar]
- McCabe SE, West BT, Veliz P, Frank KA, Boyd CJ, 2014. Social contexts of substance use among US high school seniors: A multicohort national study. J Adolescent Health. 55, 842–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier E, Hatsukami DK, 2016. A review of the additive health risk of cannabis and tobacco co-use. Drug Alcohol Depen. 166, 6–12. [DOI] [PubMed] [Google Scholar]
- Montgomery L, Mantey D, 2018. Racial/ethnic differences in prevalence and correlates of blunt smoking among adolescents. J Psychoactive Drugs. 50, 195–205. [DOI] [PubMed] [Google Scholar]
- Montgomery L, Robinson C, Seaman EL, Haeny AM, 2017. A scoping review and meta-analysis of psychosocial and pharmacological treatments for cannabis and tobacco use among African Americans. Psychol Addictive Behav. 31, 922–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B, 2011. Mplus 8. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- Panlilio LV, Zanettini C, Barnes C, Solinas M, Goldberg SR, 2013. Prior exposure to THC increases the addictive effects of nicotine in rats. Neuropsychopharmacol. 38, 1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Budney AJ, Carroll KM, 2012. Clinical correlates of co-occurring cannabis and tobacco use: A systematic review. Addiction. 107, 1404–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Schwartz RP, Wang S, O’Grady KE, Blanco C, 2014. Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence. Drug Alcohol Depen. 134, 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvers K, Ridenour C, Woodcock A, Savin MJ, Holguin G, Hamill S, Romero DR, 2018. Marijuana use among adolescent multiple tobacco product users and unique risks of dual tobacco and marijuana use. Drug Alcohol Depen. 189, 80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Delucchi KL, Hall SM, Liu H, Prochaska JJ, 2013. Marijuana and tobacco co-use in young adults: Patterns and thoughts about use. J Stud Alcohol Drugs. 74, 301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Liu H, Prochaska JJ, 2012. Tobacco and marijuana use among adolescents and young adults: A systematic review of their co-use. Clin Psychol Rev. 32, 105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M, 2015. Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addict Behav. 49, 26–32. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Peters EN, 2018. Correlates and trends in youth co-use of marijuana and tobacco in the United States, 2005–2014. Drug Alcohol Depen. 185, 238–244. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, Peters EN, 2017. Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addict Behav. 64, 200–211. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME, 2018. Monitoring the Future national survey results on drug use, 1975–2017: Volume II, College students and adults ages 19–55. Institute for Social Research, The University of Michigan, Ann Arbor. [Google Scholar]
- Song AV, Ling PM, 2011. Social smoking among young adults: Investigation of intentions and attempts to quit. Am J Public Health. 101, 1291–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Lowe B, 2006. A brief measure for assessing generalized anxiety disorder - The GAD-7. Arch Intern Med. 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSHA), 2018. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Sweeten G, Piquero AR, Steinberg L, 2013. Age and the explanation of crime, revisited. J Youth Adolescence. 42, 921–938. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Pedersen ER, Seelam R, Dunbar MS, Shih RA, D’Amico EJ, in press. Types of cannabis and tobacco/nicotine co-use and associated outcomes in young adulthood. Psychol Addict Behav. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2014. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA. [Google Scholar]
- U.S. Department of Health and Human Services, 2016. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health Office of the Surgeon General, Washington, DC: HHS. [PubMed] [Google Scholar]
- Villanti AC, Johnson AL, Rath JM, Williams V, Vallone DM, Abrams DB, Hedeker D, Mermelstein RJ, 2017. Identifying “social smoking” U.S. young adults using an empirically-driven approach. Addict Behav. 70, 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel EA, Rubinstein ML, Prochaska JJ, Ramo DE, 2018. Associations between marijuana use and tobacco cessation outcomes in young adults. J Subst Abuse Treat. 94, 69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JB, Cataldo JK, 2016. Medical marijuana legalization and co-use in adult cigarette smokers. Am J Health Behav. 40, 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]