Abstract
Investigation of the prevalence, incidence, and determinants of post‐traumatic stress disorders (PTSD) and other mental disorders associated with military deployment in international missions poses several methodological and procedural challenges. This paper describes the design and sampling strategies, instruments, and experimental procedures applied in a study programme aimed to examine military deployment‐related mental health and disorders (prevalence and trajectories) and to identify vulnerability and risk factors (e.g. age, gender, type of mission, rank, and duration of deployment and a wide range of neurobiological, psychological, social, and behavioural factors).
The study comprised two components. The first component, a cross‐sectional study, included 1483 deployed and 889 non‐deployed German soldiers (response rate, 93%) who served during the 2009 International Security Assistance Force (ISAF) mission. A standardized diagnostic instrument (Composite International Diagnostic Interview, CIDI) coupled with established questionnaires was administered to detect and diagnose PTSD and a broad spectrum of mental disorders and mental health problems. The second component, a prospective‐longitudinal study, included 621 soldiers examined before (2011) and after return (2012) from the ISAF mission. In addition to the CIDI and questionnaires, several experimental behavioural tests and biological markers were implemented to probe for incident mental disorders, mental health problems and risk factors. Our methods are expected to provide greater precision than previous studies for estimating the risk for incident deployment‐related and non‐deployment‐related disorders and their risk factors. We expect the findings to advance our understanding of a wide spectrum of adverse mental health outcomes beyond PTSD. Copyright © 2012 John Wiley & Sons, Ltd.
Keywords: PTSD, combat, trauma mental disorders, prevalence, incidence, risk factors, comorbidity
Introduction
Substantial evidence from a range of studies has shown that soldiers deployed for foreign military missions are at increased risk for mental health problems and post‐traumatic stress disorders (PTSD, Fear and Jones, 2010; Hoge et al., 2006; Sundin et al., 2010). Many studies have examined risk factors, and consequences associated with military mission‐related PTSD (Iversen et al., 2008; LeardMann et al., 2009; Vasterling et al., 2010). However, the prevalence of mission‐related mental health problems and PTSD vary widely between nations and between studies with relatively comparable samples. Recent reviews have indicated that this variability may be due to a range of socio‐political and cultural factors related to the nature of the disorders and to the methodological factors employed (Frueh et al., 2010; Stein et al., 2009; Wittchen et al., 2009). Relevant methodological factors include design (one/two stage designs, with/without control groups), the sampling strategy (inclusion of reservists/combat‐only), the assessment strategy (screening tools, self‐report, clinical scales, diagnostic interviews), and the study time‐frame (i.e. cross‐sectional, 12‐month, lifetime).
Studies that rely exclusively on screening methods and self report are generally associated with higher prevalence rates (Kulka et al., 1991) than studies based on clinically structured or standardized diagnostic interviews. The latter are generally accepted as the best currently available standard (Richardson et al., 2010; Wittchen et al., 2009). Self‐report methods typically reflect symptom severity, but do not allow derivation of specific diagnoses, according to the generally accepted guidelines, like the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM‐IV‐TR). Variability in prevalence among studies may also be due to other factors, like the type of mission, deployment location, duration, type and intensity of stressful events, and the timing of assessment (e.g. the number of months after the mission). PTSD and other mental disorders subsequent to military events might have a delayed onset, perhaps several months after a traumatic event (Meewisse et al., 2011).
A major limitation of studies in this field is that they rarely cover the full range of potentially relevant mental health problems and disorders. Available studies typically focus on one or a few disorders, most frequently PTSD, but also depression, suicidal tendencies, substance (ab)use, or sleep disorders (i.e. Capaldi et al., 2011; Jacobson et al., 2008; Wells et al., 2010). Only a few studies have highlighted the association between deployment and military mission and the risk for psychopathological conditions beyond PTSD (Iversen et al., 2008), but to our knowledge no study has yet included a full range of DSM‐IV disorders. Exclusive focus on one particular disorder inherently neglects the possibility that stressful, traumatic deployment events may trigger the onset of mental disorders beyond PTSD, including depressive and anxiety disorders or other forms of mental disorders or aggravate their course. Furthermore, focus on one disorder precludes proper evaluation mandatory diagnostic exclusion rules and differential diagnostic considerations; this can lead to both over‐ and under‐estimation of the true prevalence of PTSD and other mission‐related disorders. Also, studies with a restricted diagnostic focus are unable to examine the complex interrelationships between disorders (comorbidity); e.g. the potential effects of past or pre‐existing mental health conditions on incident traumatic disorders or subsequent mental disorders. These problems are particularly critical in cross‐sectional or 12‐month prevalence studies, but do also apply to the few existing prospective, longitudinal studies designed to investigate the trajectories of symptom development and identify risk and resilience factors for one or several disorders. Thus, study designs that ignore comorbidity and the potential effects of pre‐existing mental disorders on deployment‐related mental health problems from a longitudinal perspective, are overall of limited value to derive preventive interventions.
Aims
We launched a comprehensive study programme, labelled PID‐PTSD+3, to extend our understanding of the consequences of military deployment in the German Army on mental health and mental disorders, and to identify factors associated with adverse mental health outcomes. The programme included representative samples of deployed and never deployed German soldiers and covered an unprecedented broad spectrum of mental disorders and mental health problems beyond PTSD. It consisted of two major components. The first was a large scale, cross‐sectional study of soldiers that served in 2009 as part of the International Security Assistance Force (ISAF) mission compared to a control group of soldiers never deployed. The second was a prospective‐longitudinal study of another sample of soldiers examined before (2011) and after (2012) an ISAF mission. The major aims of these study programmes were to examine:
the frequency of stressful, traumatic mission events; the trajectories, incidence, and prevalence of mission and non‐mission related PTSD; and the incidence of a wide range of other mental disorders according to the criteria of DSM‐IV‐TR (APA, 2000);
the patterns and measures of mission‐related mental disorders (comorbidity), symptom severity, and mental health problems beyond threshold mental disorders;
the risk for PTSD and mental disorders, based on age, gender, type of mission, rank, deployment location, and duration of deployment;
the associated disabilities, quality of life, and rates of seeking help and treatment;
more specific factors associated with increased risk for PTSD and mental disorders beyond those mentioned in (3);
the longitudinal contributions of a wide range of neurobiological, psychological, social, and behavioural risk factors associated with the onset or persistence of mental disorders and PTSD.
The examination of these complex issues posed a range of methodological and procedural challenges. This paper describes the design and sampling strategies, instruments, and experimental procedures applied in the cross‐sectional and prospective‐longitudinal components of this programme.
Design and methods of the cross‐sectional study
Overview
The cross‐sectional component of the PID‐PTSD+3 addressed a broad spectrum of research questions. Trained clinical psychologists performed personal interviews and computer‐assisted, standardized, clinical diagnostic assessments in two representative samples. The first was a random, stratified sample of n = 1483 German soldiers that had been deployed to Afghanistan in the German ISAF mission the year before the study assessment. The second was a “control” group of n = 889 soldiers that had not been deployed. Deployed soldiers were sampled from the 20th and 21st German ISAF mission contingents (the reference population). The control group of soldiers were matched to the same home base locations as the deployed soldiers. All participants were approached and assessed at their respective home bases by trained clinical assessors from our research field teams. For deployed soldiers, the assessment took place about 12 months after return from the mission. The assessments started in May 2009 at the first location and ended in December 2010 at the last location.
Sampling of soldiers
According to deployment lists provided by the German Army Operations Command, the 20th and 21st German contingents of the 2009/2010 ISAF mission in Afghanistan comprised a total of 10,055 soldiers. Close examination of the enlisted deployed soldiers revealed that there were 438 apparent errors (i.e. double counting, anticipated deployment did not take place, information missing about home base location, or gender). Thus, the total reference population for sampling deployed soldiers consisted of n = 9617 soldiers. Logistical and funding constraints did not allow assessment of all deployed soldiers; therefore, we employed a sampling strategy. Power calculations indicated that sufficient resolution of prevalence rates for PTSD could be achieved with a 36% (n = 3493) random sample of the total of 9617 soldiers, with assumed non‐eligibility and refusal rates. This included oversampling combat soldiers, assumed to be a high risk group. Thus, combat soldiers were sampled at about twice the rate of that used for support units and medical personnel. The random sampling procedure was performed by Operations Command according to our strict sampling protocol, because confidentiality and data protection regulations did not allow direct access to soldier personal contact information before written informed consent was provided.
Recruitment and eligibility
Operations Command and staff from the German Center of Military Mental Health in Berlin checked the eligibility of the 3493 sampled deployed soldiers. Personal letters of invitation to participate were sent to all sampled eligible subjects. In the letter, subjects were asked to schedule a face‐to‐face meeting with our research staff. This personalized information and recruitment strategy was chosen to ensure complete independence from any Army‐related body. We allowed no access to the data outside the study personnel. We ensured absolute privacy and confidentiality of assessments, including information on whether the selected soldiers actually participated or refused participation. Furthermore, this procedure avoided potential cluster refusal effects within a location, which might occur with group information sessions. The personalized strategy required that our trained clinical research field teams were installed in all home base locations prior to the assessment periods. This was necessary to be able to approach eligible subjects, inform them about the study, obtain informed consent, and ultimately conduct the assessments. The eligibility criteria were: (a) the soldiers sampled from the total reference population had to be present in their home base during the respective study assessment period; (b) our logistical and financial constraints restricted recruitment to locations that held a significant number of deployed soldiers that were eligible for interview. Only locations with a sufficiently high number of eligible deployed soldiers (> 50) were considered.
The German Center of Military Mental Health in Berlin negotiated with army command to determine appropriate time slots for the assessments and re‐examinations of sampled subjects. From the total of 3493 soldiers originally sampled, n = 1559 were eligible. These subjects were distributed over a total of 18 locations nationwide. These 1599 (=100%) soldiers constituted the basis for the subsequent sample description and the results of the study (Figure 1).
Figure 1.
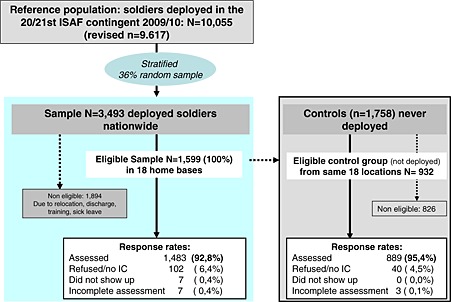
Cross‐sectional study component: reference population, sampling and completion rates in deployed and never‐deployed soldiers.
Of the 1894 ineligible soldiers, 5.5% were not stationed in one of the 18 target locations, 20.6% had been relocated, 23.9% were discharged, 5.2% were on holiday, 15.7% were attending training courses, and 5.9% were on sick leave. Of note, there were some indications that, among the ineligible soldiers, there was an over‐representation of both lower and higher ranked soldiers that did not serve in Kunduz, Afghanistan. This was most likely due to the fact that many enlisted soldiers had left the army before the study period. Special care was taken to examine soldiers that were ineligible due to sickness; we noted whether the sickness status might be directly or indirectly related to injuries or medical disorders, including PTSD that resulted from deployment. An internal review was conducted by the German Center of Military Mental Health to examine all available medical files of ineligible subjects for indications that these subjects may have sustained mental disorders or PTSD. Out of 110 participants that were ineligible due to sick leave, 54 medical files could be analysed. Indications for probable deployment‐related psychological health problems, including PTSD, were ascertained for only three of the 54 subjects examined; thus, selective non‐participation effects were unlikely.
Deployed soldiers: refusal and completion rates
Of the 1599 eligible soldiers (100%), 102 (6.4%) refused to participate, and seven (0.4%) did not appear at the time their examination was scheduled. Thus, a total of 1483 eligible participants (92.8% response rate) were enrolled and examined. Figure 1 summarizes the recruitment and sampling process. Table 1 shows the frequency of soldiers stratified by combat/non‐combat, gender, and service location (Kunduz/non‐Kunduz province). The numbers of soldiers are shown for the total reference population, the 36.3% sample, the non‐eligible and eligible subjects, and the sample ultimately interviewed. The frequencies reflected the oversampling of combat soldiers. Associations between eligibility criteria and some noteworthy differences in some of the strata were observed. Therefore, we adjusted the final sample to account for these effects by post‐stratification weighting to match the total reference population (last column Table 1). Details about weighting and adjustment procedures are described in detail later.
Table 1.
Sampling strata in the reference population and sample of deployed soldiers
| Reference population | 36.3% samplec | Not eligible | Eligible | Sample assessed (unweighted) | Sample, weightedd | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sampling strata | N = 9617 | N = 3493 | N = 1894 | N = 1599 | N = 1483 | N = 1483 | |||||||||
| Sex | Unit | Rank | Location | N | % | N | % | N | % | N | % | N | % | N | % |
| Male | Combat | Lowera | Kunduz | 381 | 4.0 | 281 | 8.0 | 59 | 3.1 | 222 | 13.9 | 219 | 14.8 | 58 | 3.9 |
| Non‐Kunduz | 897 | 9.3 | 563 | 16.1 | 362 | 19.1 | 201 | 12.6 | 177 | 11.9 | 138 | 9.3 | |||
| Higherb | Kunduz | 237 | 2.5 | 183 | 5.2 | 27 | 1.4 | 156 | 9.8 | 150 | 10.1 | 36 | 2.4 | ||
| Non‐Kunduz | 664 | 6.9 | 316 | 9.1 | 178 | 9.4 | 138 | 8.6 | 128 | 8.6 | 102 | 6.9 | |||
| Total | 2179 | 22.7 | 1343 | 38.5 | 626 | 33.1 | 717 | 44.8 | 674 | 45.5 | 334 | 22.5 | |||
| Support/medical | Lowera | Kunduz | 198 | 2.1 | 74 | 2.1 | 34 | 1.8 | 40 | 2.5 | 37 | 2.5 | 31 | 2.1 | |
| Non‐Kunduz | 783 | 8.1 | 246 | 7.0 | 144 | 7.6 | 102 | 6.4 | 91 | 6.1 | 121 | 8.2 | |||
| Higherb | Kunduz | 907 | 9.4 | 315 | 9.0 | 197 | 10.4 | 118 | 7.4 | 114 | 7.7 | 141 | 9.5 | ||
| Non‐Kunduz | 5050 | 52.5 | 1371 | 39.3 | 799 | 42.2 | 572 | 35.8 | 523 | 35.3 | 779 | 52.5 | |||
| Total | 6938 | 72.1 | 2006 | 57.4 | 1174 | 62.0 | 832 | 52.0 | 765 | 51.6 | 1071 | 72.2 | |||
| Female | Kunduz | 86 | 0.9 | 31 | 0.9 | 22 | 1.2 | 9 | 0.6 | 7 | 0.5 | 14 | 0.9 | ||
| Non‐Kunduz | 414 | 4.3 | 113 | 3.2 | 72 | 3.8 | 41 | 2.6 | 37 | 2.5 | 64 | 4.3 | |||
| Total | 1483 | 100.0 | 1483 | 100.0 | |||||||||||
Other enlisted ranks.
Commissioned and non‐commissioned officers.
Combat was sampled at twice the rate as other groups.
Adjusted to the reference population of 9617.
Control group of non‐deployed soldiers
To compare morbidity rates between deployed and non‐deployed soldiers, the control and deployed groups were sampled from the same locations and selected with the same strata and eligibility criteria. The Army Command, jointly with the German Center of Military Mental Health, provided a random sample of 1758 non‐deployed soldiers. Of those, 932 were eligible (53.0%), and 40 refused, resulting in 889 participants (95.4% of eligible). It should be noted that, unexpectedly, 25 of these soldiers had actually been deployed abroad prior to the assessment, but they were not part of the 2009/2010 ISAF contingency. Therefore, these remained in the sample.
Field teams
Sixty‐four trained clinical psychologists approached the selected subjects, scheduled appropriate time slots, completed informed consent procedures, and conducted the assessments. Army personnel were not involved in any of these tasks. However, assigned personnel of the German Center of Military Mental Health assisted in preparing the logistics of the study at each location (lodging and food for assessors, training the assessors to behave according to the rules of each location, etc.). At each location, field teams comprised two coordinators, several supervisors, and up to nine assessors, depending on the number of interviews conducted at each location. Field teams spent up to three weeks at the study locations. The field team coordinators arranged the onsite visits and organized team resources in each location; for example, they reserved the appropriate numbers of assessment rooms, secured housing, established personal contact with Army support staff, and ensured a proper logistical flow (arrival time, security issues, etc.). The field team supervisors (n ≤ 3) monitored strict adherence to the study protocol, correct administration of study instruments, appropriate data editing, and confidential data transmission to the Centre for Epidemiological Studies (TU‐Dresden).
Assessors
Assessors were clinical psychologists with training and skills in at least the core parts of the assessment package or previous participation as an interviewer in a similar epidemiological study. Prior to conducting the interviews, assessors completed the mandatory 2–3‐day interviewer training programme, based on a study procedure manual. The training covered all steps of assessment, including behavioural rules in army locations, standardized information, informed consent procedures, the interview components, and protocols for data editing and data quality control. The training was repeated at each new location, and, when necessary, supervisors provided additional on‐site training. After interviewers had completed the training and passed a real life interview test without any protocol violations, they were licensed for the study. Interviews were videotaped and checked for errors or inconsistencies in the use of the computer‐assisted assessment package. This included automatic testing for plausibility of information obtained and timing protocols to identify atypically fast or slow interviewers. In cases of serious misconduct or violations of the study procedure manual, assessors were excluded from the study. No interviewers had to be excluded based on theses criteria. On average, each interviewer was expected to complete 2–3 interviews per day during a typical assessment week (Monday to Friday). This included immediate editing with the standard editing programme and transferring data to the data bank. The average interview lasted 120 minutes, including informed consent and the core assessment interview [mean = 106.2, standard deviation (SD) = 35.9 minutes]. Up to seven interviews were typically conducted in parallel to minimize study duration at each location.
Assessment procedures
In the week prior to the start of the assessment period in each location, a pseudoanonymous list of target respondents was used to schedule a suitable time slot for each subject. Prior to testing, all scheduled respondents had received a personalized information letter signed by the study directors (HUW and SS) via the German Bundeswehr “Center of Military Mental Health”. The letter informed the subject about the background, procedures, and aims of the study, and invited them to attend a personal information session. Invited participants were required to attend the meeting, irrespective of their willingness to participate. The invitation letter emphasized that only the interviewer was to know whether they had ultimately participated in the study, and that they would not report to a supervising officer until the full assessment time slot ended, regardless of whether they participated. Before participation, soldiers were informed about the study by the interviewer and asked for informed consent. In case of refusal, a short questionnaire was completed (data not reported due to the low refusal rate). The interview started immediately after receiving informed consent. All interviews were conducted in separate rooms, face‐to‐face, via a computer‐assisted‐personal interview (CAPI) platform. All instructions and questions were standardized and, with few exceptions, presented verbatim according to prompts on the screen. A separate response booklet was placed in front of the participant that included all scales, response lists, visual aids, and written instructions that were presented verbally by the interviewer throughout the session. The interview included questions that probed commitment and instructions for completing self‐reported assessments that involved rating scales and itemised lists. The interviewer entered all responses directly into his/her laptop computer.
Assessment instruments
The core modular assessment component was the computer‐assisted version of the Munich‐Composite International Diagnostic Interview (DIA‐X/M‐CIDI, Wittchen and Pfister, 1997). The mandatory CIDI respondent‐booklet contained self‐report questionnaires, other response lists, and visual aids. Table 2 displays all the measures covered in this study, organized by CIDI section (A to X).
Table 2.
Measures and assessment instruments (DIA‐CIDI, military version)
| Section | Domain/questionnaire | Abbrev. | Domain | Authors |
|---|---|---|---|---|
| A | a) Standard CIDI demographic information | CIDI‐A | a) Age, gender, family status, education, income, etc. | Wittchen and Pfister, 1997 |
| b) Military specific information | b) Rank, carrier, service, deployments, etc. | Wittchen et al., 2009 | ||
| c) Problem‐list | c) Recent somatic, psychological, psychosocial problems (domain‐score) | |||
| World Mental Health Social Support Scale | WMH‐SPS | Social network, social support (score) | Kessler et al., 2008 | |
| Concerns about Life and Family Disruption Scale | DRRI | Worries about home and family (disruption in relationship, missing important events at home, etc.) | King et al., 2003 | |
| Difficult Living and Working Environment Scale | DRRI | Living and working environment (climate, clothing, equipment, etc.) | King et al., 2003 | |
| Combat Experiences Scale & Exposure to Aftermath of Battle Scale | DRRI | Combat experiences, dealing with aftermath of combat (attacks, corpses, injured, refugees, destroyed homes) | King et al., 2003 | |
| Sense of Preparedness Scale | DRRI | Feeling prepared (information, equipment, training, etc.) | King et al., 2003 | |
| Positive effects of deployment | MHAT IV | Perceived positive effects of deployment | Based on Mental Health Advisory Team (MHAT IV), 2006; German: Wittchen et al., 2009 | |
| World Health Organization Disability Assessment Schedule 2.0 | WHO‐DAS II | Disability total and subscale scores (communication, mobility, self‐care, interpersonal, life activities, participation | Üstün et al., 2010 | |
| B | Smoking and DSM‐IV nicotine dependency | CIDI‐B | quantity, frequency, onset and recency symptoms of dependency, therapy, changes associated with deployment) | Wittchen and Pfister, 1997 |
| C | WHO‐Quality of Life Questionnaire | WHOQOL‐bref | Subjective rating of quality of health and life | WHOQOL Group, 1998 |
| WHOQOL total and domain scores | ||||
| Physical status | CIDI‐CX | 16 medically confirmed diagnosed illnesses, and status of medical treatment, (in general and associated with deployment) | Wittchen and Jacobi, 2008 | |
| DSM‐IV somatoform disorders | CIDI‐C | DSM‐IV somatoform disorders, SSI4/6, pain disorder, undifferentiated somatoform disorder; onset and recency, total score | Wittchen and Pfister, 1997 | |
| D | DSM‐IV anxiety disorders | CIDI‐D | Panic attacks, panic disorder, GAD, agoraphobia, social phobia, specific phobia, all onset und recency, severity scores, changes associated with deployment | Wittchen and Pfister, 1997 |
| Hospital Anxiety and Depression Scale | HADS | Degree of symptoms of anxiety and depression | Zigmond and Snaith, 1983 | |
| N | N1 distressing and traumatic events | CIDI‐N1 | 29 events categorized in three main categories, mission and non‐mission‐related | Wittchen et al., 2009 |
| N2 number of combat experiences | MHAT IV mod. | 33 combat‐related events, frequency (respectively and total) | Based on Hoge et al., 2004; German: Wittchen et al., 2009 | |
| DSM‐IV Post‐traumatic Stress Disorder (PTSD) | CIDI‐N | PTSD, acute stress disorder, onset und recency, number of symptoms | Wittchen and Pfister, 1997 | |
| Post‐traumatic Diagnostic Scale | PDS | Frequency and intensity of PTSD symptoms within last month | Ehlers et al., 1996 (English: Foa, 1995) | |
| E | Depression Screening Questionnaire (DSQ −34) | DSQ‐34 | 34 item version of the DSQ, dimensional measure of depression symptoms, allows diagnosis of adjustment disorder as MDD | Wittchen and Pfister, 1997; Wittchen et al., 2009 |
| DSM‐IV Depressive Disorders | CIDI‐E | DSM‐IV major depression, dysthymia, and subtypes, onset and recency, course, changes associated with deployment | Wittchen and Pfister, 1997 | |
| Pittsburgh Sleep Quality Index | PSQI | Quality of sleep, sleep disorders | Riemann and Backhaus, 1996 (English: Buysse et al., 1989) | |
| Fatigue Scale for Motor and Cognitive Functions | FSMC | Cognitive and physiological fatigue | Penner et al., 2005
. |
|
| F | DSM‐IV bipolar disorders | CIDI‐F | Manic and hypomanic episode, onset and recency, course, changes associated with deployment | Wittchen and Pfister, 1997 |
| G | DSM‐IV psychosis | CIDI‐G | Type and number of psychotic symptoms (25), and likelihood of presence of psychosis | Wittchen and Jacobi, 2008 |
| I | DSM‐IV alcohol abuse and dependence | CIDI‐I | Standard drinks – recent, lifetime, quantity, frequency, onset and recency, course, symptoms of dependency, therapy, changes associated with deployment | Wittchen and Pfister, 1997 |
| K | DSM‐IV OCD | CIDI‐K | DSM‐IV OCD (obsessions and compulsions) onset and recency, changes associated with deployment | Wittchen and Pfister, 1997 |
| L | DSM‐IV abuse and dependency of drugs | CIDI‐L | Quantity, recency, onset and recency, changes associated with deployment | Wittchen and Pfister, 1997 |
| Q | Usage of medical services and interventions | CIDI‐Q | Services of different facilities within and outside the army, frequency, type of service and their evaluation | Wittchen et al., 2009 |
| Barriers to Care scale | BAC | Barriers to care | Wittchen and Jacobi, 2008 | |
| X1 | Perceived Threat Scale | DRRI | Perceived threat (death, serious injuries, chemical and biological weapons, etc.) | King et al., 2003 |
| X2 | Deployment Social Support Scale | DRRI | Social support in the work environment (unit cohesion, respect) | King et al., 2003 |
| X3 | General (1–7) + Sexual Harassment Scale | DRRI | bullying and sexual harassment (extreme criticism, devaluation, inappropriate sexual comments or actions) | King et al., 2003 |
| X4 | Work environment | MHAT IV‐mod | Atmosphere within the unit, support by unit/seniors | Based on Mental Health Advisory Team (MHAT IV), 2006; German: Wittchen et al., 2009 |
| X5 | Work environment | MHAT IV‐mod | Behaviour and perceived competence of seniors | Based on MHAT 2006; German: Wittchen et al., 2009 |
| X6 | Social support after homecoming | Appreciation and support after homecoming | Based on Maercker and Bromberger, 2005; Iversen et al., 2009; Wittchen et al., 2009 | |
| X7 | Response to Intrusions Questionnaire | RIQ | Dysfunctional coping with intrusive memories (rumination, thought suppression, distraction, dissociation) | Clohessy and Ehlers, 1999 |
| X8 | Post‐traumatic Cognitions Inventory‐r | PTCI‐r | Dysfunctional cognitions about traumatic event and its sequel | Foa et al., 1999 |
The military version of the DIA‐X/M‐CIDI is a fully standardized, diagnostic interview designed to assess a wide range of mental disorders and symptoms according to the diagnostic criteria of the DSM‐IV‐TR (APA, 2000). The validity and reliability of substance use disorders diagnosed with the DIA‐X/M‐CIDI have been established (Lachner et al., 1998; Wittchen et al., 1998). In this study, we used the combined 12‐month and lifetime versions of the interview; thus, we could estimate 12‐month, pre‐12‐month‐lifetime, and overall lifetime threshold and subthreshold disorders. The respondent‐booklets were supplemented with interviewer and self‐report questions and modules relevant to the study aims and the military context. Modifications were introduced that retained all CIDI standard diagnostic algorithms for potential future DSM‐V diagnoses, as follows: (a) dimensional measures were incorporated (Shear et al., 2007); (b) the socio‐demographic section was extended with relevant items regarding military ranks, tasks, employment history, and deployment characteristics; (c) the mood disorder section was supplemented with modules for subthreshold depressive disorders, adjustment disorders, fatigue, and sleep disorders; (d) the trauma and PTSD section (Perkonigg et al., 2005) was considerably enlarged by separating military from non‐military stressful (DSM‐IV A1) and traumatic (DSM‐IV A2) events, and by separating recent mission from non‐mission events; (e) dimensional scales were added, including combat experience scales (Table 2) from the Mental Health Advisory Team VI (MHAT‐VI) report by Operation Iraqi Freedom VI (2006) and the Post‐traumatic Diagnostic Scale (PDS, Ehlers et al., 1996); these allowed dimensional and comparative analyses; (f) finally, the CIDI section on seeking help and treatment (CICI‐Q) was enlarged to include all pre‐ and post‐deployment services and interventions available to soldiers.
Outcome measures
The core categorical diagnostic measures, derived from the DIA‐X/M‐CIDI, were:
threshold DSM‐IV‐TR PTSD and acute stress disorders;
threshold DSM‐IV‐TR diagnoses of mood disorders [major depressive episode (MDE), bipolar disorder (BIP), dysthymia (Dys)], anxiety disorders (panic disorder, agoraphobia, social, and specific phobia, generalized anxiety disorder (GAD)], obsessive‐compulsive disorder (OCD), somatoform disorders (pain, somatization, hypochondrias), any psychotic disorder (probable), and substance use disorders (nicotine dependence, abuse of alcohol, and use of drugs or medication).
For each of these disorders, the diagnostic algorithms used information about age of onset, recency, and duration to compute:
the lifetime incidence, defined as the proportion of subjects that met the criteria at any point in life, from childhood to the day of the interview;
the 12‐month (post‐mission) prevalence, defined as the proportion of subjects that met the diagnostic criteria within the past 12 months;
the post‐mission incidence, defined as the proportion of subjects that met the 12‐month criteria, but had not been affected by the disorder previously at any point in life.
Additionally we computed the incidence of:
any disorder (overall incidence);
specific comorbidity patterns;
subthreshold disorders; subjects that lacked one criterion required for diagnosis by the DSM‐IVTR criteria;
current fatigue; derived from the Fatigue Scale for Motor and Cognitive Functions (FSMC, Penner et al., 2005);
sleep problems; based on the Pittsburgh Sleep Quality Index (PSQI, Buysse et al., 1989).
For most diagnostic domains, additional dimensional scales were implemented. These included the Hamilton Anxiety and Depression Scale (HADS, Zigmond and Snaith, 1983); the revised CIDI‐Depression Screening Questionnaire (DSQ) scale, for measuring current severity of depressive symptoms; the German version of the Difficult Living and Working Environment (DRRI) scale (King et al., 2003); the Reaction to Intrusion Questionnaire (RIQ, Clohessy and Ehlers, 1999); and the Post‐traumatic Cognitions Inventory (PTCI, Foa et al., 1999). The latter assessed trauma and symptom related cognitions. The primary non‐diagnostic outcome measures were: the number, type, and frequency of military (MHAT‐VI) and non‐military events (CIDI) that were rated “traumatic” (based on A1 and A2 criteria of the DSM‐IV for PTSD).
Data analyses for the cross‐sectional study
Design weights and adjustments
All statistical analyses were performed with weighted data. Design and sampling weights were applied to account for the higher probability of sampling soldiers that experienced combat and were deployed to Kunduz, Afghanistan. Post‐stratification weights were used to account for differences that occurred due to the joint effects of sampling, eligibility, and response (Table 1); these were applied in the first step only to deployed subjects. The weight calculation procedure was based on the inverse sample versus the reference population frequency count per stratum (results for non‐deployed soldiers are available upon request).
Because ineligibility was primarily due to reasons unrelated to the study context, we assumed it was independent of the main study outcomes, and therefore, the weighted study sample accurately reflected the total reference population in the core strata of interest. The design variables and other military and socio‐demographic characteristics of non‐deployed subjects were adjusted to those of the deployed subjects. The adjustments accounted for military rank (low, middle, high), unit (combat, support, medical), number of years spent in the military (< 2, 2–4, 5–7, 8–9, 10+ years), operational area (army, air force, basic fighting forces, marine, medical), gender, age (18–24, 25–29, 30–39, 40+ years), educational level (low, middle, high), number of years spent at school, and whether they had children (no/yes). First, we used logistic regression to determine the relationships between the true deployment status and these variables; then, we calculated the model‐based probability of deployment for each participant. This probability is called propensity score (Rosenbaum and Rubin, 1983), and it served as the basis for weighting (Kurth et al., 2006). The PSCORE procedure (Becker and Ichino, 2002) in Stata 12 (StataCorp, 2011) was used to categorize the propensity score into quartile‐based blocks. The predictor variables were balanced as evenly as possible within the blocks. This categorization reduced the variance in the weighting variable, which would otherwise yield unnecessarily broad confidence intervals and low statistical power (Hoefler et al., 2005). Here, eight blocks provided the best coverage. Next, weights were calculated as the inverse ratios of non‐deployed to deployed relative frequencies within these blocks. The block frequencies for the deployed were weighted as described earlier to maintain the adjustment to the population frequencies.
Finally, the weighting variables in both deployed and non‐deployed soldiers were scaled to make the average weight equal to unity. The weighting variables in deployed and non‐deployed soldiers had standard deviations (SDs) of 0.51 and 1.40, respectively.
Diagnostic algorithms and analyses
All diagnostic data were based on the CIDI‐DSM‐IV‐TR diagnostic algorithms. The standard, edited CIDI data file was the input. Thus, the diagnostic procedure was regarded reliable and objective in the sense that assessors had no influence on diagnostic decisions.
Statistical analyses
We used two types of comparisons to estimate the prevalence of mission‐related traumatic events, PTSD, and other mental disorders. First, comparisons within subjects were used to compare the rate of incident 12‐month diagnoses to the total lifetime rate. Second, comparisons of rates between deployed soldiers and matched non‐deployed soldiers were used to assess excess morbidity due to deployment for both lifetime and incident 12‐month rates. Incidence rates for disorders were calculated based on the CIDI standard age of onset questions. Subjects were defined as incident cases when they fulfilled the criteria for a lifetime disorder and reported onset within the past 12 months. Because the interviews took place at approximately 12 months after return from deployment, this convention covered part of the deployment period (average four months) and the interval between the return from deployment and the interview date.
The frequencies (N values) were unweighted, and the other results (percentages, means, SDs, and test or regression results) were weighted. Global comparisons of categorical outcomes with more than two categories were examined with a design‐based modification of the Chi squared test of independence, which follows an F distribution (Choi and McHugh, 1989). Differences in binary outcomes between cases and controls were expressed with odds ratios (ORs) from logistic regressions; for outcomes with more than two categories, multinomial logistic regressions were fitted. In cases of dimensional outcomes, linear regressions were applied with regression coefficients that represented estimates of the mean difference between cases and controls (using a dummy‐coded variable). Statistical inference in regressions was based on the robust, Huber–White, sandwich estimator of standard errors for weighted data (e.g. Royall, 1986). Statistical significance was evaluated at the two‐sided, 0.05 level. Analyses were conducted with Stata 12 (StataCorp, 2011) and the SVY‐procedures (procedures for survey data) for statistical inference.
Design and methods of the prospective‐longitudinal study
Overview
The soldiers for the prospective‐longitudinal study were sampled in the same way as described earlier for the cross‐sectional study. Soldiers were sampled from the disposition list of Army Operations Command, which comprised all soldiers scheduled for an upcoming deployment as part of the 26th and 27th contingencies in the 2011/2012 ISAF mission in Afghanistan. All eligible soldiers were invited to participate twice (Figure 2): once for a pre‐deployment examination and then for a re‐examination about 12 months after return from the mission, in 2012 (follow‐up assessments are ongoing).
Figure 2.
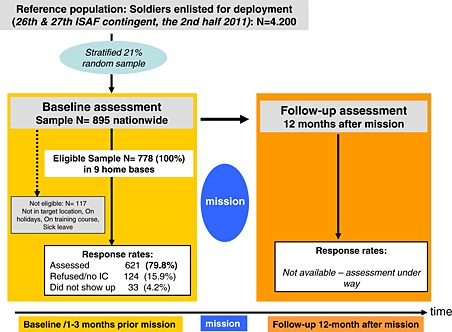
Design of the prospective‐longitudinal study.
Sampling and eligibility of the baseline wave
The German Army Operations Command sampled a total of 895 soldiers. Sample size was determined based on the refusal rates in the cross‐sectional study and power calculations for achieving statistical significance based on trajectory modelling of traumatic events and PTSD data from the cross‐sectional study. The sampling procedure was performed by Operations Command, due to the confidentiality and data protection regulations stated earlier. As in the cross‐sectional study, recruitment and eligibility checks were conducted by the Operations Command and staff from the “Center of Military Mental Health”, Berlin, in conjunction with the study staff.
Refusal and completion rates for the baseline wave
From the total of 895 soldiers sampled, n = 778 subjects were eligible. Subjects were distributed over a total of nine locations nationwide. These soldiers constituted the basis for the baseline sample description. Of the 117 ineligible soldiers, 2.6% were not stationed in one of the nine target locations, 23.1% were on holiday, 34.2% were at training courses, and 7.7% were on sick leave. Of the 778 eligible soldiers (100%), a total of n = 124 (15.9%) refused to participate and 33 (4.2%) did not appear at the time their examination was scheduled. Thus, 621 participants (79.8% of those eligible) were enrolled and examined. The response rate was slightly lower than that of the cross‐sectional study.
Instruments and assessments
This study used the same phenotypic and clinical assessment battery that was used in the cross‐sectional study (Table 2). However, in the baseline assessment of this study, we implemented a number of additional constructs and experimental psychological measures relevant to predicting incident PTSD and other mental disorders that occurred subsequent to deployment.
Experimental psychological paradigms
Four paradigms were implemented, as described later. All tests were used twice; once before the mission at baseline and a second time in the follow‐up assessment.
Autobiographical memory
Memory plays a prominent role in the development of post‐traumatic mental disorders (Kleim and Ehlers, 2008; Sutherland and Bryant, 2005). In the present study, we will test whether the ability to remember specific autobiographical events predicts PTSD and trauma‐related depression. We used the Autobiographical Memory Test (AMT, Williams & Broadbent, 1986; Figure 3). In this test, a cue word was acoustically presented and participants were required to recall a specific event that lasted a day or less and occurred at a certain place and time, but not during the last seven days. They had 30 seconds to recall a specific event. When a non‐specific memory was named, and sufficient time remained, they were asked to recall a specific event. Before the test started, participants received a training session with three neutral cue words. The test phase did not begin until the subject demonstrated a clear understanding of the task by recalling at least one specific event in the training phase. During the test phase, five positive and five negative words were presented alternately in a randomized order. In compliance with the coding system of Williams and Broadbent (1986), the experimenter classified the answers as semantically associated, categorical, extended, or specific memories. According to the participant's consent, responses were recorded and coded. Finally, participants were asked whether they had reported traumatic events during the test. We calculated the proportions of specific responses given after the negative and positive cues.
Figure 3.
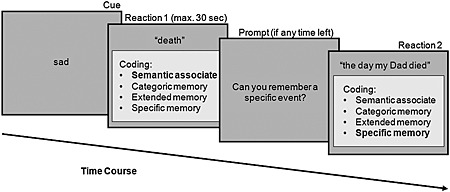
Sequence of events in one trial of the Autobiographical Memory Test.
Cognitive flexibility
Rumination is a powerful predictor of persistent PTSD (Clohessy and Ehlers, 1999; Ehlers et al., 1998; Steil and Ehlers, 2000). One potential explanation for this is that rumination is a manifestation of a tendency toward cognitive inflexibility (Davis and Nolen‐Hoeksema, 2000). Cognitive flexibility was measured with a task switch paradigm, similar to the tasks used by Rogers and Monsell (1995). Participants performed the tasks on a laptop computer. Each trial (Figure 4) started with a fixation cross, followed by the instruction “letter” or “digit”. The next screen showed a letter and a digit. Depending on the instruction (“letter”/“digit”), participants indicated whether the letter was a vowel or consonant or whether the digit was odd or even. After providing feedback, the next trial began. Before the experimental trials (64), participants received a training session, where the responses were practiced separately (12 trials) and together (24 trials). The cost of switching paradigms was calculated as the difference between response times to switched and repeated cues.
Figure 4.
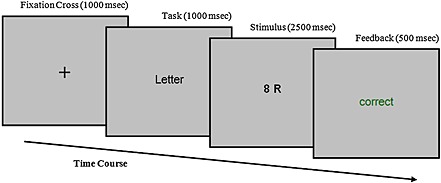
Sequence of events in one task switch trial.
Attention biases
Attention plays an important role in the aetiology and maintenance of anxiety disorders (Bar‐Haim et al., 2007). We will examine whether an attention bias to threat‐related material predicts the development of anxiety disorders; i.e. PTSD. We measured attention biases to threat‐related material with the dot‐probe paradigm of Pérez‐Edgar et al. (2010), which was modified from the original dot‐probe paradigm (MacLeod et al., 1986). Participants performed 120 experimental trials; each trial (Figure 5) started with a fixation cross, followed by two pictures of a face. One facial expression was always neutral; the other was either happy or angry. Immediately after presenting the pictures, the probe (letter E or F) appeared at one of the two positions of the pictures. The participant identified the letter by pressing a specified key; this initiated a blank screen, which was followed by the next trial. The attention bias to threat‐related material was calculated as the average difference between the response times to neutral and threat‐related pictures.
Figure 5.
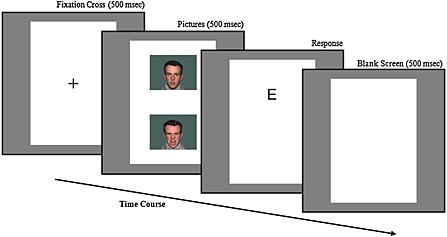
Sequence of events in a dot‐probe task trial.
Almost the same paradigm was used in the last (fourth) experiment to examine a more specific, Afghanistan‐related attention bias. This test followed the same dot‐probe format, but it comprised different pictures and 220 trials. Here, the pictures displayed scenes of soldiers at home and in Afghanistan with neutral, happy, or negative content. The same calculations were used to evaluate the Afghanistan‐related attention bias.
Stress‐paradigm (TSST)
The Trier Social Stress Test (TSST, Kirschbaum et al., 1993), which assesses acute stress response, was conducted before military deployment. The TSST is a standardized laboratory protocol for measuring saliva cortisol to evaluate reliably acute psychosocial stress. The test consists of a brief preparation period, a five‐minute speech, and a five‐minute mental arithmetic task in front of an audience. The audience is trained to abstain from verbal or non‐verbal feedback (for a review see Foley and Kirschbaum, 2010; Figure 6). Based on a meta‐analysis (Dickerson and Kemeny, 2004), the TSST leads to robust changes in the hypothalamus‐pituitary‐adrenal (HPA) axis stress response compared to other laboratory paradigms. Reported effects ranged from 0.7 to 2.3. In the current study, saliva samples were collected before and 1, 10, and 20 minutes after the TSST. The TSST measures were assessed only once at baseline (before deployment) to predict stress‐related, adverse, mental health outcomes. Due to logistical restrictions in our study, the full TSST was conducted in only 296 out of 621 soldiers. We found no evidence of selection effects; assignment to the TSST was random, entirely due to logistics (availability of the assessment rooms), and not based on willingness to participate or any personal characteristic.
Figure 6.
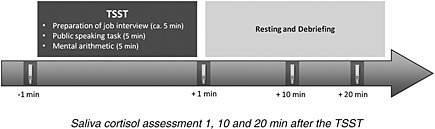
Procedure of the Trier Social Stress Test (TSST).
Hair cortisol
Hair cortisol analysis constitutes a novel method for the retrospective assessment of integrated cortisol secretion over extended periods of time (for a review, see Russell et al., 2012). Recently, hair cortisol has been validated as an index of long‐term cortisol secretion in a number of human and animal studies (e.g. Davenport et al., 2006; Kirschbaum et al., 2009; Stalder et al., 2010; Thomson et al., 2010). Additionally, evidence has shown that hair cortisol levels can serve as a biological marker of chronic stress (e.g. Dettenborn et al., 2010; Kalra et al., 2007; Van Uum et al., 2008). In the current study, hair strands were taken before and 12 months after deployment. Hair was cut as close to the scalp as possible from a posterior vertex position, and steroid concentrations were determined in the most proximal 2‐cm segment (Figure 7). Based on an average hair growth rate of 1 cm per month (Wennig, 2000), each segment was assumed to represent the cumulative two‐month steroid exposure prior to sampling. Based on hair lengths, we assumed that hair strand collection would be possible for approximately 40–50% of soldiers.
Figure 7.

A scalp‐near hair segment is used for the analysis of cumulative steroid levels.
Summary and conclusions
This paper presented an overview of the methods and procedures used in the PID‐PTSD+3 project, a long‐term comprehensive research programme for investigating deployment effects on mental health in the German military. This is the first study of its kind in the German military and among soldiers deployed in the ISAF mission. To our knowledge, it is the only study to determine the prevalence and incidence of PTSD and other mission‐related mental disorders, diagnosed according to the DSM‐IV‐TR, by personal clinical interviews in a representative sample of deployed soldiers compared to a matched control group of non‐deployed soldiers. The study strengths are (a) the reliance on representative samples of ISAF‐mission soldiers, (b) the comparison of pre‐ and post‐mission mental health, (c) coverage of a broader spectrum of mental disorders than covered in previous studies, (d) a prospective‐longitudinal study component of soldiers examined before and after deployment, (e) inclusion of a wide range of established and novel risk factors, (f) the incorporation of experimental and psychobiological stress measures to assess higher order cognitive factors, and (g) a high response rate of 85 to 93% in both the cross‐sectional and longitudinal components.
This study used representative samples, a complex design, and sophisticated measurements aimed to address issues left out of previous studies (Kessler et al., 2008). In particular, the PID‐PTSD+3 study did not rely solely on questionnaire measures, but administered state of the art diagnostic interviews to evaluate a broad spectrum of mental disorders, according to DSM‐IV‐TR criteria. Our design and modifications are specifically aimed to examine the proportion of increased PTSD prevalence that could be directly attributable to mission‐related events. This provided greater precision than previous studies for estimating the risk for incident deployment‐related and non‐deployment‐related disorders, the role of pre‐existing (pre‐mission) mental disorders that might have worsened due to mission‐related stress or events, and the role of comorbid conditions in the persistence and severity of PTSD. Thus, our findings are expected to provide considerable advances in our understanding of a wide spectrum of adverse mental health outcomes beyond PTSD, and the degree to which adverse mental outcomes and PTSD are attributable to deployment events and conditions. Our use of retrospective and prospective data will enable analysis of trajectories and determinants that predict relationships between deployment‐related stress and the occurrence of subclinical psychopathological conditions and subthreshold and threshold DSM‐IV mental disorders.
Because, to our knowledge, the PID‐PTSD+3 project is the first study to combine these sampling, design, and instrumental features, it will be difficult to make direct study comparisons and population generalizations. There is some evidence (Bohnert and Breslau, 2011; Smith et al., 2007a, 2007b, 2008) that the reliability is similar between self‐reported and “objective” medical data. However, we expect substantial differences between our findings and those of other studies based on screening methods, self‐report only measures, or telephone interviews, particularly with regard to the incidence risk and estimated rates of PTSD and other mental disorders. Furthermore, we expect our findings to differ from those found in UK and US samples, due to the considerably different mission characteristics, including the degree of combat exposure, deployment location and duration, pre‐mission selection routines, inclusion of reservists, different tasks undertaken, the proportion of combat units, pre‐deployment training at home, and veteran administration system compensation policies (Jones and Wessely, 2007). Data comparisons among different national studies should always consider socio‐cultural and mission differences that are most likely to affect mental health outcomes, the sample constitution, willingness to participate, and response behaviour.
Based on recent critical reviews in PTSD research (Richardson et al., 2010; Stein et al., 2009; Wittchen et al., 2009), we strongly believe that the core question of our project regarding the frequency of mission‐related mental health problems, is best addressed by using personal, face‐to‐face, standardized diagnostic instruments that allow derivation of DSM‐IV‐TR diagnoses. The cross‐sectional and lifetime assessments of DSM‐IV diagnoses based on the CIDI (Wittchen and Pfister, 1997) were reliable, finely‐graded psychopathological assessments with respect to temporal characteristics. In addition, this approach enabled direct comparisons with a wide range of available community data (e.g. Alonso et al., 2011; Breslau et al., 1999; Karam et al., 2010; Kessler, 2000; Kessler et al., 2008, 2011; Nock et al., 2010; Perkonigg et al., 2000; Wittchen et al., 2000). Furthermore, private, face‐to‐face interviews provided optimal confidentiality, shielded subjects from career consequences (negative or positive), and avoided reporting biases (Warner et al., 2011). The additional continuous measures, like established symptom severity scales, supplemented the diagnostic assessment, facilitated comparisons with screening studies, and provided a basis for future analyses aimed at modelling improved cutoff scores or identifying novel screening indices.
The prospective‐longitudinal study components will allow validation of the cross‐sectional findings with a stronger reliance on retrospective information. It will also promote the development of improved measures for predicting, in particular, severe mental health complications and PTSD. In this programme, we focused on a comprehensive examination of pre‐existing psychopathology and mental disorders that might represent reliable risk factors for developing severe mental disorders after deployment. However, we also explored novel markers of susceptibility by including experimental psychological constructs. These indirect measurements of disposition were expected to be less influenced and biased by subjectivity than verbal questionnaire responses. This approach explored whether stress‐regulation measures, cognitive processing assessments, and higher order cognitive factors could enhance the predictions of PTSD and related disorders.
The PID‐PTSD+3 had a number of limitations. First, due to specific deployment characteristics of the German Army in the ISAF mission (average four months deployment, emphasis on peace keeping rather than combat, etc.), the study findings cannot easily be generalized to other deployment missions. Second, sampling was conducted in 2009 (cross‐sectional) and 2011 (longitudinal study); thus, the outcomes were restricted to the mission‐related incidences and circumstances of those years. Third, the stratified random sampling procedures were not sufficiently powered to detect mission‐related incidence risks for all groups of deployed soldiers; in particular, although consistent with the true numbers deployed, the proportion of females was too small to allow detailed analyses. Fourth, although the eligibility criteria reflected random processes, and thus, were unlikely to have introduced bias, we could not entirely exclude the possibility of selective attrition. Fifth, the average time of outcome assessment was 12 months; thus, we cannot exclude the possibility that some soldiers may have experienced a delayed onset of combat‐related mental health problems after the 12‐month period. Finally, despite the availability of objective information about significant events that occurred during the mission, which may have been directly related to some soldiers, we relied on the accuracy of the recall and self‐reporting of the soldiers during the interview assessments.
Despite these potential limitations, we believe that this study programme represents a considerable methodological improvement over previous studies. This approach is expected to provide greater precision than previous studies for investigating central research questions concerning deployment‐related mental health outcomes.
Declaration of interest statement
The authors report no competing interests.
Acknowledgements
This study was funded by the German Defence Ministry and the Medical Office thereof (Bundesministerium der Verteidigung, represented by Sanitätsamt der Bundeswehr; Project Funding number M/SAB X/9A004).
The project was logistically supported by the staff of the “Center of Military Mental Health” (Zentrum für Psychiatrie und Psychotraumatologie am Bundeswehrkrankenhaus) in Berlin. Oberstarzt PD MD Peter Zimmermann was the Project officer. The project was also supported by an internal army Steering and Advisory Board of the Bundeswehr and a scientific advisory board (Professor Dr Ronald C. Kessler; Professor Matthew J. Friedman, MD, PhD; Professor Ariel Shalev; Professor Yosep Zohar).
The study was approved by the TUD Ethics Board (EK 72022010), after internal Bundeswehr approval, and was performed according to ICH‐GCP (Good Clinical Practice)‐Guidelines.
References
- Alonso J., Vilagut G., Chatterji S., Heeringa S., Schoenbaum M., Ustun T.B., Rojas‐Farreras S., Angermeyer M., Bromet E., Bruffaerts R., de Girolamo G., Gureje O., Haro J.M., Karam A.N., Kovess V., Levinson D., Liu Z., Medina‐Mora M.E., Ormel J., Posada‐Villa J., Uda H., Kessler R.C. (2011) Including information about co‐morbidity in estimates of disease burden: results from the World Health Organization World Mental Health Surveys. Psychological Medicine, 41(1), 873–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) . (2000) Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revised), Washington, DC, APA. [Google Scholar]
- Bar‐Haim Y., Lamy D., Pergamin L., Bakermans‐Kranenburg M.J., van IJzendoorn M.H. (2007) Threat‐related attentional bias in anxious and nonanxious individuals: a meta‐analytic study. Psychological Bulletin, 133(1), 1–24. [DOI] [PubMed] [Google Scholar]
- Becker S.O., Ichino A. (2002) Estimation of average treatment effects based on propensity scores. The Stata Journal, 2, 358–377. [Google Scholar]
- Breslau N., Chilcoat H.D., Kessler R.C. (1999) Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit area survey of trauma. The American Journal of Psychiatry, 156(6), 902.907. [DOI] [PubMed] [Google Scholar]
- Bohnert K.M., Breslau N. (2011) Assessing the performance of the short screening scale for post‐traumatic stress disorder in a large nationally‐representative survey. International Journal of Methods in Psychiatric Research, 20(1), E1–E5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Capaldi V.F., Guerrero M., Killgore W. (2011) Sleep disruptors among returning combat veterans from Iraq and Afghanistan. Military Medicine, 176(8), 879–888. [DOI] [PubMed] [Google Scholar]
- Choi W.J., McHugh R.B. (1989) A reduction factor in goodness‐of‐fit and independence tests for clustered and weighted observations. Biometrics, 45, 979–996. [PubMed] [Google Scholar]
- Clohessy S., Ehlers A. (1999) PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology, 38(Part 3), 251–265. [DOI] [PubMed] [Google Scholar]
- Davenport M.D., Tiefenbacher S., Lutz C.K., Novak M.A., Meyer J.S. (2006) Analysis of endogenous cortisol concentrations in the hair of rhesus macaques. General and Comparative Endocrinology, 147, 255–261. [DOI] [PubMed] [Google Scholar]
- Davis R.N., Nolen‐Hoeksema S. (2000) Cognitive inflexibility among ruminators and nonruminators. Cognitive Therapy and Research, 24, 699–711. [Google Scholar]
- Dettenborn L., Tietze A., Bruckner F., Kirschbaum C. (2010) Higher cortisol content in hair among long‐term unemployed individuals compared to controls. Psychoneuroendocrinology, 35, 1404–1409. [DOI] [PubMed] [Google Scholar]
- Dickerson S.S., Kemeny M.E. (2004) Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychological Bulletin, 130, 355–391. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Mayou R.A., Bryant B. (1998) Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology, 107(3), 508–519. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Steil R., Winter H., Foa E.B. (1996) Deutsche Übersetzung der Posttraumatic Stress Diagnostic Scale (PDS), Oxford, Department of Psychiatry, University Warneford Hospital. [Google Scholar]
- Fear N.T., Jones M. (2010) What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet, 375, 1783–1797. [DOI] [PubMed] [Google Scholar]
- Foa E.B. (1995) Posttraumatic Stress Diagnostic Scale. Minneapolis, MN, National Computer Systems. [Google Scholar]
- Foa E.B., Ehlers A., Clark D.M., Tolin D.F., Orsillo S.M. (1999) The Posttraumatic Cognitions Inventory (PTCI): development and validation. Psychological Assessment, 11(3), 303–314. [Google Scholar]
- Foley P., Kirschbaum C. (2010) Human hypothalamus‐pituitary‐adrenal axis responses to acute psychosocial stress in laboratory settings. Neuroscience and Biobehavioral Review, 35, 91–96. [DOI] [PubMed] [Google Scholar]
- Frueh B.C., Elhai J.D., Acierno R. (2010) The future of posttraumatic stress disorder in the DSM. Psychological Injury and Law, 3, 260–270. [Google Scholar]
- Hoefler M., Pfister H., Lieb R., Wittchen H.U. (2005) The use of weights to account for non‐response and drop‐out. Social Psychiatry and Psychiatric Epidemiology, 4, 291–299. [DOI] [PubMed] [Google Scholar]
- Hoge C.W., Auchterlonie J.L., Milliken C.S. (2006) Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association, 295(9), 1023. [DOI] [PubMed] [Google Scholar]
- Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. (2004) Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13. [DOI] [PubMed] [Google Scholar]
- Iversen A.C., Fear N.T., Ehlers A., Hacker Hughes J., Hull L., Earnshaw M., Greenberg N., Rona R., Wessely S., Hotopf M. (2008) Risk factors for post‐traumatic stress disorder among UK Armed Forces personnel. Psychological Medicine, 38, 511–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen A.C., van Staden L., Hacker Hughes J., Browne T., Hull L., Hall J., Greenberg N., Rona R, Hotopf M., Wessely S., Fear N.T. (2009) The prevalence of common mental disorders and PTSD in the UK military: using data from a clinical interview‐based study. BMC Psychiatry, 9, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson I.G., Ryan M.A.K., Hooper T.I., Smith T.C., Amoroso P.J., Boyko E.J., Gackstetter G.D., Wells T.S., Bell N.S. (2008) Alcohol use and alcohol‐related problems before and after military combat deployment. Journal of the American Medical Association, 300(6), 663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E., Wessely S. (2007) A paradigm shift in the conceptualization of psychological trauma in the 20th century. Journal of Anxiety Disorders, 21(2), 164–175. [DOI] [PubMed] [Google Scholar]
- Kalra S., Einarson A., Karaskov T., Van Uum S., Koren G. (2007) The relationship between stress and hair cortisol in healthy pregnant women. Clinical and Investigative Medicine, 30, E103–E107. [DOI] [PubMed] [Google Scholar]
- Karam E.G., Andrews G., Bromet E., Petukhova M., Ruscio A.M., Salamoun M., Sampson N., Stein D.J., Alonso J., Andrade L.H., Angermeyer M., Demyttenaere K., de Girolamo G., de Graaf R., Florescu S., Gureje O., Kaminer D., Kotov R., Lee S., Lepine J.P., Medina‐Mora M.E., Browne M.A.O., Posada‐Villa J., Sagar R., Shalev A.Y., Takeshima T., Tomov T., Kessler R.C. (2010) The role of criterion A2 in the DSM‐IV diagnosis of posttraumatic stress disorder. Biological Psychiatry, 68(5), 465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. (2000) Posttraumatic stress disorder: the burden to the individual and to society. The Journal of Clinical Psychiatry, 61, 4–14. [PubMed] [Google Scholar]
- Kessler R.C., Keane T.M., Ursano R.J., Mokdad A., Zaslavsky A.M. (2008) Sample and design considerations in post‐disaster mental health needs assessment tracking surveys. International Journal of Methods in Psychiatric Research, 17, 6–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Ormel J., Petukhova M., McLaughlin K.A., Green J.G., Russo L.J., Stein D J., Zaslavsky A.M., Aguilar‐Gaxiola S., Alonso J., Andrade L., Benjet C., de Girolamo G., de Graaf R., Demyttenaere K., Fayyad J., Haro J.M., Hu C.Y., Karam A., Lee S., Lepine J.P., Matchsinger H., Mihaescu‐Pintia C., Posada‐Villa J., Sagar R., Ustun T.B. (2011) Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Archives of General Psychiatry, 68(1), 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D.W., King L.A., Vogt D.S. (2003) Manual for the Deployment Risk and Resilience Inventory (DRRI): A Collection of Measures for Studying Deployment‐related Experiences of Military Veterans. Boston, MA, National Center for PTSD. [Google Scholar]
- Kirschbaum C., Pirke K.M., Hellhammer D.H. (1993) The “Trier Social Stress Test” – a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28, 76–81. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C., Tietze A., Skoluda N., Dettenborn L. (2009) Hair as a retrospective calendar of cortisol production – increased cortisol incorporation into hair in the third trimester of pregnancy. Psychoneuroendocrinology, 34, 32–37. [DOI] [PubMed] [Google Scholar]
- Kleim B., Ehlers A. (2008) Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal Of Consulting and Clinical Psychology, 76(2), 231–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulka R.A., Schlenger W.E., Fairbank J.A., Jordan B.K., Hough R.L., Marmar C.R., Weiss D.S. (1991) Assessment of posttraumatic stress disorder in the community: prospects and pitfalls from recent studies of Vietnam veterans. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 3(4), 547–560. [Google Scholar]
- Kurth T., Walker A.M., Glynn R.J., Chan K.A., Gaziano J.M., Berger K., Robins J.M. (2006) Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity‐based weighting under conditions of nonuniform effect. American Journal of Epidemiology, 163, 262–270. [DOI] [PubMed] [Google Scholar]
- Lachner G., Wittchen H.U., Perkonigg A., Holly A., Schuster P., Wunderlich U., Tuerk, D. , Garczynski E., Pfister H. (1998) Structure, content and reliability of the Munich Composite International Diagnostic Interview (M‐CIDI) substance use sections. European Addiction Research, 4, 28–41. [DOI] [PubMed] [Google Scholar]
- LeardMann C.A., Smith T.C., Smith B., Wells T.S., Ryan M.A.K. (2009) Baseline self reported functional health and vulnerability to post‐traumatic stress disorder after combat deployment: prospective US military cohort study. British Medical Journal, 338, b1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod C., Mathews A., Tata P. (1986) Attentional bias in emotional disorders. Journal of Abnormal Psychology, 95(1), 15–20. [DOI] [PubMed] [Google Scholar]
- Maercker A., Bromberger F. (2005) Checklisten und Fragebogen zur Erfassung traumatischer Ereignisse in deutscher Sprache. Trierer Psychologische Berichte, 32, Heft 2. [Google Scholar]
- Meewisse M.L., Olff M., Kleber R., Kitchiner N.J., Gersons B.P.R. (2011) The course of mental health disorders after a disaster: predictors and comorbidity. Journal of Traumatic Stress, 24(4), 405–413. [DOI] [PubMed] [Google Scholar]
- Mental Health Advisory Team (MHAT IV) . (2006) Operation Iraqi Freedom 05–07. Final Report, Chartered by the Office of the Surgeon Multinational Force‐Iraq and Office of the Surgeon General United States Army Medical Command, 17 November.
- Nock M.K., Hwang I., Sampson N.A., Kessler R.C. (2010) Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Molecular Psychiatry, 15(8), 868–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner I.K., Vogt A., Raselli C., Stoecklin M., Opwis K., Kappos L. (2005) The FSMC (Fatigue Scale for Motor and Cognitive Functions): a new patient‐reported outcome measure for cognitive and motor fatigue in multiple sclerosis. Multiple Sclerosis, 11, 66. [DOI] [PubMed] [Google Scholar]
- Pérez‐Edgar K., Bar‐Haim Y., McDermott J., Gorodetsky E., Hodgkinson C.A., Goldman D., Fox N.A. (2010) Variations in the serotonin‐transporter gene are associated with attention bias patterns to positive and negative emotion faces. Biological Psychology, 83(3), 269–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkonigg A., Kessler R., Storz S., Wittchen H. (2000) Traumatic events and post‐traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101(1), 46–59. [DOI] [PubMed] [Google Scholar]
- Perkonigg A., Pfister H., Stein M.B., Hofler M., et al (2005) Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. The American Journal of Psychiatry, 162(7), 1320–1327. [DOI] [PubMed] [Google Scholar]
- Richardson L.K., Frueh B.C., Acierno R. (2010) Prevalence estimates of combat‐related PTSD: a critical review. The Australian and New Zealand Journal of Psychiatry, 44(1), 4–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riemann D., Backhaus J. (1996) Behandlung von Schlafstörungen, Weinheim, Psychologie Verlags Union. [Google Scholar]
- Rogers R.D., Monsell S. (1995) Costs of a predictible switch between simple cognitive tasks. Journal of Experimental Psychology. General, 124(2), 207–231. [Google Scholar]
- Rosenbaum P.R., Rubin D.B. (1983) The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55. [Google Scholar]
- Royall R. (1986) Model robust inference using maximum likelihood estimators. International Statistical Review, 54, 221–226. [Google Scholar]
- Russell E., Koren G., Rieder M., Van Uum S. (2012) Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology, 37(5), 589–601. [DOI] [PubMed] [Google Scholar]
- Shear M.K., Bjelland I., Beesdo K., Gloster A.T., Wittchen H.U. (2007) Supplementary dimensional assessment in anxiety disorders. International Journal of Methods in Psychiatric Research, 16(1), 52–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B., Chu L.K., Smith T.C., Amoroso P.J., Boyko E.J., Hooper T.I., Gackstetter G.D., Ryan M.A.K., for the Millennium Cohort Study Team (2008) Challenges of self‐reported medical conditions and electronic medical records among members of a large military cohort. BMC Medical Research Methodology, 8, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B., Wingard D.L., Ryan M.A.K., Macera C.A., Patterson T.L., Slymen D.J., for the Millennium Cohort Study Team (2007a) US military deployment during 2001–2006: comparison of subjective and objective data sources in a large prospective health study. Annals of Epidemiology, 17(12), 976–982. [DOI] [PubMed] [Google Scholar]
- Smith T.C., Smith B., Jacobson I.G., Corbeil T.E., Ryan M.A.K., for the Millennium Cohort Study Team (2007b) Reliability of standard health assessment instruments in a large, population‐based cohort study. Annals of Epidemiology, 17(7), 525–532. [DOI] [PubMed] [Google Scholar]
- Stalder T., Kirschbaum C., Heinze K., Steudte S., Foley P., Tietze A., Dettenborn L. (2010) Use of hair cortisol analysis to detect hypercortisolism during active drinking phases in alcohol‐dependent individuals. Biological Psychology, 85, 357–360. [DOI] [PubMed] [Google Scholar]
- StataCorp . (2011) Stata Statistical Software: Release 12.0, College Station, TX, Stata Corporation. [Google Scholar]
- Steil R., Ehlers A. (2000) Dysfunctional meaning of posttraumatic intrusions in chronic PTSD. Behaviour Research and Therapy, 38(6), 537–558. [DOI] [PubMed] [Google Scholar]
- Sundin J., Fear N.T., Hull L., Jones N., Dandeker C., Hotopf M., Wessely S., Rona R.J. (2010) Rewarding and unrewarding aspects of deployment to Iraq and its association with psychological health in UK military personnel. International Archives of Occupational and Environmental Health, 83, 653–663. [DOI] [PubMed] [Google Scholar]
- Stein D.J., Cloitre M., Nemeroff C.B., Nutt D.J., Seedat S., Shalev A.Y., Wittchen H.U., Zohar J. (2009) Cape Town consensus on posttraumatic stress disorder. CNS Spectrums, 14(1), 52–58. [PubMed] [Google Scholar]
- Sutherland K., Bryant R.A. (2005) Self‐defining memories in post‐traumatic stress disorder. British Journal of Clinical Psychology, 44(4), 591–598. [DOI] [PubMed] [Google Scholar]
- Thomson S., Koren G., Fraser L.A., Rieder M., Friedman T.C., Van Uum S.H. (2010) Hair analysis provides a historical record of cortisol levels in Cushing's syndrome. Experimental and Clinical Endocrinology & Diabetes, 118, 133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Üstün T.B., Kostanjsek N., Chatterji S., Rehm J. (2010) Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0), Geneva, World Health Organization. [Google Scholar]
- Van Uum S.H., Sauve B., Fraser L.A., Morley‐Forster P., Paul T.L., Koren G. (2008) Elevated content of cortisol in hair of patients with severe chronic pain: a novel biomarker for stress. Stress, 11, 483–488. [DOI] [PubMed] [Google Scholar]
- Vasterling J.J., Proctor S.P., Friedman M.J., Hoge C.W., Heeren T., King L.A., King D.W. (2010) PTSD symptom increases in Iraq‐deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress, 23(1), 41–51. [DOI] [PubMed] [Google Scholar]
- Warner C.H., Appenzeller G.N., Grieger T., Belenkiy S., Breitbach J., Parker J., Warner C.M., Hoge C. (2011) Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Archives of General Psychiatry, 68(10), 1065–1071. [DOI] [PubMed] [Google Scholar]
- Wells T.S., LeardMann C.A., Fortuna S.O., Smith B., Smith T.C., Ryan M.A.K., Boyko E.J., Blazer D. (2010) A prospective study of depression following combat deployment in support of the wars in Iraq and Afghanistan. American Journal of Public Health, 100(1), 90–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennig R. (2000) Potential problems with the interpretation of hair analysis results. Forensic Science International, 107, 5–12. [DOI] [PubMed] [Google Scholar]
- WHOQOL Group . (1998) Devolopment of the World Health Organization WHOQOL‐BREF quality of life assessment. Psychological Medicine, 28, 551–558. [DOI] [PubMed] [Google Scholar]
- Williams J.M.G., Broadbent K. (1986) Autobiographical memory in suicide attempters. Journal of Abnormal Psychology 95, 144–149. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Gloster A., Beesdo K., Schoenfeld S., Perkonigg A. (2009) Posttraumatic stress disorder: diagnostic and epidemiological perspectives. CNS Spectrums, 14(1), 5–12. [PubMed] [Google Scholar]
- Wittchen H.U., Jacobi F. (2008) The DEGSCIDI (Deutscher Epidemiologischer Gesundheitssurvey), unpublished manuscript, Technische Universität Dresden, Dresden, 2009.
- Wittchen H., Kessler R., Pfister H., Lieb M. (2000) Why do people with anxiety disorders become depressed? A prospective‐longitudinal community study. Acta Psychiatrica Scandinavica, 102, 14–23, DOI: 10.1111/j.0065-1591.2000.acp29[dash]03.x [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Lachner G., Wunderlich U., Pfister H. (1998) Test–retest reliability of the computerized DSM‐IV version of the Munich‐Composite International Diagnostic Interview (M‐CIDI). Social Psychiatry and Psychiatric Epidemiology, 33(11), 568–578. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Pfister H. (eds). (1997) DIA‐X‐Interviews: Manual für Screening‐Verfahren und Interview; Interviewheft Längsschnittuntersuchung (DIA‐X‐Lifetime); Ergänzungsheft (DIA‐X‐Lifetime); Interviewheft Querschnittuntersuchung (DIA‐X‐Monate); Ergänzungsheft (DIA‐X‐Monate); PC‐Programm zur Durchführung des Interviews (Längs‐ und Querschnittuntersuchung); Auswertungsprogramm, Frankfurt, Swets and Zeitlinger. [Google Scholar]
- Wittchen H.‐U., Schönfeld S., Recknagel R., Siegert J. (2009) CIDI‐Military version (MI), unpublished manual and computer‐assisted personal interview, Technische Universität Dresden, Dresden, 2009.
- Zigmond A.S., Snaith R.P. (1983) The hospital anxiety and depression scale. Acta Psychiatrica Scandinavia, 67(6), 361–370. [DOI] [PubMed] [Google Scholar]


