Abstract
This article introduces the design, sampling, field procedures and instruments used in the ZInEP Epidemiology Survey. This survey is one of six ZInEP projects (Zürcher Impulsprogramm zur nachhaltigen Entwicklung der Psychiatrie, i.e. the “Zurich Program for Sustainable Development of Mental Health Services”). It parallels the longitudinal Zurich Study with a sample comparable in age and gender, and with similar methodology, including identical instruments. Thus, it is aimed at assessing the change of prevalence rates of common mental disorders and the use of professional help and psychiatric sevices. Moreover, the current survey widens the spectrum of topics by including sociopsychiatric questionnaires on stigma, stress related biological measures such as load and cortisol levels, electroencephalographic (EEG) and near‐infrared spectroscopy (NIRS) examinations with various paradigms, and sociophysiological tests. The structure of the ZInEP Epidemiology Survey entails four subprojects: a short telephone screening using the SCL‐27 (n of nearly 10,000), a comprehensive face‐to‐face interview based on the SPIKE (Structured Psychopathological Interview and Rating of the Social Consequences for Epidemiology: the main instrument of the Zurich Study) with a stratified sample (n = 1500), tests in the Center for Neurophysiology and Sociophysiology (n = 227), and a prospective study with up to three follow‐up interviews and further measures (n = 157). In sum, the four subprojects of the ZInEP Epidemiology Survey deliver a large interdisciplinary database. Copyright © 2014 John Wiley & Sons, Ltd.
Keywords: epidemiology, health services research, stress, stigma, event related potentials, NIRS, sociophysiology
Background
Introduction
Over recent decades, psychiatric epidemiology has brought the real world into psychiatry – and vice versa. Today, mental disorders are known to be much more frequent than many clinicians, politicians and the lay public had previously assumed. Moreover, subthreshold disorders have come into focus and have been recognized as a major source of burden. Another step further on, dimensional concepts are supplementing both the crude categorical concepts of mental disorders as well as their more sophisticated derivatives. Meanwhile, the use of health services has been shown to lie far below the actual need for professional help, due to lack of knowledge, inappropriate attitudes and other reasons.
A great deal of new information has come from large population studies: the Epidemiologic Catchment Area Survey (Regier and Kaelber, 1995), the National Comorbidity Survey (NCS) in the United States (Kessler et al., 1994), the British National Psychiatric Morbidity Survey (Jenkins et al., 1998), the German National Health Interview and Examination Survey – Mental Health Supplement (Jacobi et al., 2002), and the PsyCoLaus Study (Preisig et al., 2009). Finally, recent cross‐sectional studies have used very large samples, i.e. the World Mental Health Survey (Kessler et al., 2007).
Longitudinal surveys have revealed new perspectives on the complex interplay of risk factors, genetics, behavioral processes and brain systems involved in the etiopathogenesis of comorbid mental disorders, syndromes and symptoms, for example the Swedish Conscripts Study (Andreasson et al., 1987), the Northern Finland 1966 Birth Cohort (Rantakallio, 1988), the Zurich Study (Angst et al., 1984), the Munich Early Developmental Stages of Psychopathology Study (Wittchen et al., 1998), the Netherlands Mental Health Survey and Incidence Study (NEMESIS) (Bijl et al., 1998), the NCS‐R (Kessler et al., 2005) or the recently started NEMESIS II (de Graaf et al., 2010).
Further major advances in psychopathology will require a sufficient grasp of the complexity of the matter. Few disciplines and methodological approaches are able to meet this challenge, and one among them is epidemiology. This was the background for initiating the ZInEP Epidemiology Survey in Zurich, which is one of six ZInEP projects (Zürcher Impulsprogramm zur nachhaltigen Entwicklung der Psychiatrie, i.e. the “Zurich Program for Sustainable Development of Mental Health Services”).
The ZInEP Epidemiology Survey is basically geared to parallel the longitudinal Zurich Study in many instances (Angst et al., 1984; Angst et al., 2005). It seizes the opportunity to combine information from a new cross‐sectional survey with the information from an existing longitudinal survey. However, the current survey widens the spectrum of topics by including sociopsychiatric questionnaires on stigma, stress related biological measures such as allostatic load and cortisol levels, electroencephalographic (EEG) and near‐infrared spectroscopy (NIRS) examinations with various paradigms, and sociophysiological tests. It delivers a large interdisciplinary database which enables us to combine and exchange questions and answers from epidemiology and other disciplines. This paper introduces the aims and the design of the ZInEP Epidemiology Survey. Furthermore it describes the sampling, the field procedures and the instruments used in this survey.
Aims
The preliminary aims of the survey were in parallel to the surveys mentioned earlier: to generate further comprehensive information about mental health and mental disorders in the general population. This target also included subthreshold syndromes and symptoms, comorbidity patterns, risk factors and triggers, burdens and attributions. However, we were interested in outcomes such as the use of health services and all related factors: subjective motives and hurdles, i.e. stigmatization and self‐stigmatization, perceived availability of services and experiences the subjects had had with services in the past.
Moreover, by constructing parallels to the Zurich Study we aimed to obtain a direct basis for comparative analyses. In particular, we aimed to assess whether prevalence rates of common mental disorders (CMD) and use of health services have changed. If so, we wanted to disentangle whether this change had occurred in time or due to age effects or by cohort succession. Thus we adapted a specific sample design for this purpose (see later).
Four major and several minor aims extend the spectrum of the Zurich Study. The major extensions were the following:
a broader coverage of psychosis‐near symptoms and signs in order to display new perspectives on psychosis
addressing the role of stress in the interactions between depression and psychosis symptoms; this extension also included a series of biological parameters and was embedded in an add‐on study supported by the Swiss National Science Foundation (grant # 3247B0‐122071)
assessment of personality disorders
assessment of attitudes, stigmatization and related behavioral parameters.
The minor extensions included further (psycho)pathological topics (attention deficit hyperactivity disorder (ADHD), post‐traumatic stress disorder (PTSD), dyslexia and stuttering, mental pain), risk factors (obstetric complications, traumatic experiences in childhood), protective factors (resilience) and related variables such as coping abilities.
Design
General design
The general design of the ZInEP Epidemiology Survey comprised four consecutive subprojects (Figure 1; see also http://www.zinep.ch/epidemiologie/informationforresearchers for more detailed information about the sex‐age‐subsamples in each subproject):
A short telephone screening using the SCL‐27 (Hardt et al., 2004), a short form of the SCL‐90‐R (Derogatis, 1977), in order to construct a stratified sample for subproject 2 and preselect samples for subprojects 3 and 4 (see sampling details later).
A comprehensive interview, which included a semi‐structured diagnostic face‐to‐face interview using a short form of the Structured Psychopathological Interview and Rating of the Social Consequences for Epidemiology (SPIKE) used in the Zurich Study (Angst et al., 1984; Angst et al., 2005), as well as several additional self‐reporting tools, i.e. checklists filled in by the participants. Apart from a fixed set of questionnaires, further modules addressing psychosis and personality disorders were supplemented in a proportion of 55:45%. The modular design of the checklists was aimed at saving time and containing attrition of the participants.
Tests in the Center for Neurophysiology and Sociophysiology to assess several neurophysiological and biological markers related to psychosis proneness, stress vulnerability, and allostatic (cumulative stress) load (Table 1).
Up to three prospective bimonthly follow‐up interviews and saliva probes focusing on life events, stress perception, biological stress levels, major changes in symptom load, in particular regarding psychotic symptoms.
Figure 1.
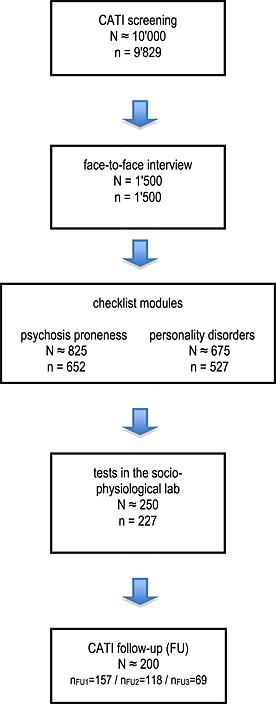
Study design of the ZInEP Epidemiology Survey: subprojects with preliminary sample projections (uppercase N) and definitive samples (lowercase n) (more detailed information is displayed at http://www.zinep.ch/epidemiologie/informationforresearchers/).
Table 1.
Measures of allostatic load
| Physical examination a | |
|---|---|
| Systolic and diastolic blood pressure | Indexes of cardiovascular activity/two measurements |
| Waist/hip ratio and body mass index | Indexes for more chronic levels of metabolism and adipose tissue deposition, thought to be influenced by increasing glucocorticoid activity |
| Blood measurements b | |
| Serum HDL, LDL and total cholesterol levels | Indexes of long‐term atherosclerotic risk |
| Fastening pro‐insulin and fastening glucose | Integrated measure of glucose metabolism during a period of several days |
| High sensitivity C‐reactive protein (CRP) | Inflammatory marker, risk factor for cardiovascular disease |
| D‐dimer, fibrinogen | Indexes or haemostatic functioning |
| DHEA‐S | Functional HPA axis antagonist |
| Norepinephrine, epinephrine | Indexes of sympathetic nervous system activity |
| Saliva c | |
| Cortisol excretion | Measure of HPA axis activity |
| Urinary excretion d | |
| Urinary albumin/creatinine | Albumin creatinine ratio as measure of subclinical nephropathy |
Blood pressure will be determined from three readings in the sitting position after a five‐minute rest period on the dominant arm.
Blood will be collected into appropriate tubes and be either immediately shipped to the laboratory for same day analysis or centrifuged and stored at −80 °C. High sensitivity C‐reactive protein and pro‐insulin will be determined using a commercially available high‐sensitivity assay.
Saliva: see earlier.
Spot urine.
Parallels and extensions of the study design with regard to the Zurich Study
Following basic methodological features were adopted from the Zurich Study. Firstly, the basic screening and stratification procedure was used in order to obtain a sample enriched by cases with a high symptom load for the main interview. Stratification procedures such as the present two‐stage procedure are a common strategy employed to save time and resources (Dunn et al., 1999). In the ZInEP Epidemiology Survey, participants scoring above the 75th percentile on the global severity index (GSI) of the SCL‐27 (high‐scorers) and participants scoring below this cutoff (low‐scorers) were sampled at a ratio of 60:40%.
The second basic parallel with the Zurich Study is related to the age structure of the sample. As mentioned earlier, the Zurich Study is a panel study based on two birth cohorts (1958 and 1959), which were interviewed seven times. Thus the age of these cohorts at each interview was defined by the year of interview. We adapted the related age years in selecting our samples (see Figure 2). The parallelized samples of the Zurich Study and the ZInEP Epidemiology Survey should help in interpreting any changes that might have occurred in time or due to age effects or by cohort succession.
Figure 2.
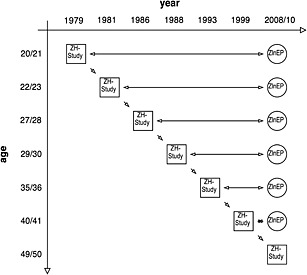
The Zurich Study panel and the age structure of the ZInEP Epidemiology Survey.
Last but not least, the parallels between the Zurich Study and the present survey relate to use of similar instruments. For the purposes of the ZInEP Epidemiology Survey we used the Mini‐SPIKE, a shortened form of the SPIKE (Structured Psychopathological Interview and Rating of the Social Consequences of Psychological Disturbances for Epidemiology – Version 10), which was developed in the Zurich Study.
Furthermore, the ZInEP Epidemiology Survey extends the spectrum of the Zurich Study (see also sections entitled “Aims”, and “Survey instruments and procedures”). On the design level this is in particular due to the subprojects 3 and 4. The tests in the Center for Neurophysiology and Sociophysiology (subproject 3) and the embedded prospective study (subproject 4) particularly add neurophysiological and biological markers to epidemiological information derived from the survey.
Projections on sample sizes
The expectations and estimates related to the sample sizes were based on the needs and parameters of the face‐to‐face interviews (subproject 2). A sample of 1500 subjects, stratified by sex, age and SCL‐27 status was assumed to require up to 10,000 screening interviews and a preliminary base of about 20,000 addresses. By offsetting the stratification, the sample would represent 3600 persons. The tests in the Center for Neurophysiology and Sociophysiology and the follow‐up interviews were planned with a subgroup of the face‐to‐face sample, i.e. 200–250 subjects, depending mainly on the ease of acquiring and reaching the subjects for the time‐consuming tests and interviews.
Methods
Place and time
The catchment area, the canton of Zurich, is a mixed urban–rural area with a population of 1.35 million, which comprises about one sixth of the total Swiss population. Zurich is the capital of the canton. With approximately 400,000 residents, it is the largest city and at the same time the economic center of Switzerland. About 20% of the residents are foreigners.
The ZInEP Epidemiology Survey, i.e. the screening and the face‐to‐face interviews, started in August 2010. The tests in the Center for Neurophysiology and Sociophysiology started in February 2011 and the follow‐up interviews two months later. The screening finished in May 2012 and all other subprojects in September 2012.
The interviews and tests were scheduled to follow at least two months after the preceding interview or test. Most of the examinations took place within 2–4 months since the last one. A participant who underwent all interviews including the testing in the Center for Neurophysiology and Sociophysiology and all follow‐up interviews was accompanied at least one year by the ZInEP team. If more than a half year had gone by between the screening and the tests in the Center for Neurophysiology and Sociophysiology, the SCL‐27 interview was repeated.
Sample design and steps in sample construction
The ZInEP Epidemiology Survey aimed to recruit a representative sample of 20 to 41 years old adults comparable in gender and age to the assessment periods of the Zurich Study. In analogy to the Zurich Study, the population was restricted to Swiss residents.
The steps in sample construction and deriving subsamples were the following (for more information see http://www.zinep.ch/epidemiologie/informationforresearchers):
Obtain addresses from the municipalities for each sample: The resident registration offices of all municipalities of the canton of Zurich were contacted and asked to send us the addresses of Swiss residents with the indicated years of birth. Since the focus was on specific years of birth (or age groups), this was the only efficient approach to reaching the target group. We provided general information about the study for the offices, the approval of the Ethics Committee, the sampling scheme, the screening questionnaire and, on request, further material such as the regulations of the data protection office of the canton of Zurich. We also offered any technical help on request.
Allocate phone numbers to a market and field research institute: The addresses were sent to the marketing and field research institute GfK (Growth for Knowledge) in Hergiswil, Switzerland, to identify the corresponding telephone numbers. This agency had also been selected to carry out the screening interviews. The proportion of residents with a published landline number decreased from 60% encountered in rural areas (i.e. at the beginning of the study) to 40% met in urban areas (i.e. at the end of the study). Additionally, we established mail contact in subgroups with low proportions in order to reach potential participants without landline numbers.
Draw random subsamples for the screening: The random selection of participants from the pool with known phone numbers was carried out by the research group. The quotes were adapted continuously depending on the response rates.
After the screening, stratify the subsamples into high‐ and low‐scorers according to the screening results, i.e. the GSI‐scores of the SCL‐27 and draw random subsamples for the face‐to‐face interviews: The stratified sample for the face‐to‐face interview was constructed as following. As mentioned earlier, participants scoring above the 75th percentile of the SCL‐27 general severity score (high‐scorers) and participants scoring below this cutoff (low‐scorers) in each of the 12 sex‐birth‐year subgroups (see also Figure 2) were sampled in a relation of 3:2. Thus, among the 1500 participants in the face‐to‐face interview, there were 900 high‐scorers and 600 low‐scorers. In each of the 12 sex‐birth‐year subgroups there were 75 high‐scorers and 50 low‐scorers. Almost all high‐scorers were included in the face‐to‐face interview. In this study, we received a re‐weighting factor of 4.5 for the low‐scorers in order to re‐establish the population proportions. This results in a virtual sample of 3600 persons after re‐weighting.
-
After the face‐to‐face interviews, build subsamples for tests in the Center for Neurophysiology and Sociophysiology and the follow‐up interviews: The subsamples for the tests in the Center for Neurophysiology and Sociophysiology and the follow‐up interviews were constructed according to the outcomes of two psychoticism scales (Rössler et al., 2007) – the schizophrenia nuclear symptoms scale (SNS) and the schizotypal signs scale (STS) – which were included in the screening interview. We introduced four subsamples according to the following criteria:
highest quintile on both scales
highest quintile on the SNS, any quintile on the STS
highest quintile on the STS, any quintile on the SNS
controls with low overall GSI‐scores, no use of professional help
This design equals a modified between‐group comparison. The controls were not asked to participate in the follow‐up interviews.
Fieldwork
At the beginning, i.e. before the screening interview, participants received an introductory letter with a brochure and general information about the study. Further material was made available on a website. In case of questions, the participants could contact the research team via a hotline or by email.
Before each face‐to‐face or follow‐up interview, participants were informed by another letter communicating that they had been selected for the next survey part and introducing the interview or the tests. The participants were asked to give their written informed consent for each survey part in which they participated.
The screening interviews (survey part one) were accomplished by the market and field research institute GfK using computer assisted telephone interviews (CATIs). In sum, 14 professional telephone interviewers were put on this interview, and seven of them covered 76% of all 9829 interviews. The interviewers were trained before the beginning of the study and twice during the study in accordance with the instructions from the research team. Supervision was provided by the GfK senior staff as well as by the research team who also had the opportunity to listen in on the interviews periodically. The research team intervened if analyses revealed that an interviewer induced any deviating response patterns.
The average duration of the screening interview was 14.0 (standard deviation [SD] 3.6, range 7.1–55.9) minutes. At the end of the screening interview the participants were asked whether they would agree to participate in the second part of the survey if their name were drawn by random selection. All participants who gave a positive answer or were undecided were included as available for the next survey part.
The face‐to‐face interviews (part two of the survey) and the following survey parts were organized by the research team and accomplished by 21 extensively trained clinical psychologists. Six of them accomplished 61% of all 1500 interviews. The research team provided continuous supervision of the interviewers based on various outcome parameters (interview duration, response patterns, return of checklists, positive answers regarding continuing participation, symptom load, and symptom patterns). The interviewer team met periodically for training, but also for the exchange of experiences in order to improve the instruments and interview procedures.
The participants could choose to be interviewed either at home (presupposing the absence of other persons in the room) or at the research offices of the Psychiatric University Hospital in Zurich. Overall, 67% of the participants chose the second alternative.
The interviews were designed as semi‐structured computer assisted personal interviews (CAPIs). The interview templates were developed with SPSS Data Entry Builder (version 4). The average duration of the face‐to‐face interviews was 144 minutes (SD 55, range 50–765).
An integral part of the interview were self‐reporting instruments (checklists) which could be filled in immediately after the face‐to‐face interview or later at home. To favor the former case, we paid interviewers a bonus for subjects who agreed. In the latter case, we asked participants to return the questionnaires within the following two weeks. In cases of noncompliance we firstly reminded them to return the checklists by letter and subsequently by telephone.
We expected most participants to complete the checklists within one to two hours. The voluminous set of checklists was a compromise between the aim of covering as many topics as possible, the length of the face‐to‐face interview, and a reasonable versus ambitious load of homework. As a further measure to enrich the information base we divided the first part of the checklists, i.e. a fourth of the set, into a psychoticism module and a personality disorder module (see also Figure 1).
All participants in part two of the survey were offered a shopping voucher of 20 Swiss francs as an incentive. At the end of the face‐to‐face interview they were asked whether they would agree to participate in parts three and four of the survey if random selection were to draw their ID number. Again, all participants who gave a positive answer or were undecided were included as available for the next survey part.
The tests in the Center for Neurophysiology and Sociophysiology (part three of the survey) took a whole day. They were carried out by a biologist and three assistants (psychology students) who underwent several training cycles. In addition, physicians from the Psychiatric University Hospital of Zurich were involved in the procedure of blood sampling.
The participants were asked to bring four saliva probes assembled the day before as well as three probes collected on the day of the examination and to come to the Center for Neurophysiology and Sociophysiology with an empty stomach and without having smoked beforehand. During the day at the Center for Neurophysiology and Sociophysiology the participants were interviewed, provided saliva, blood and urine probes, completed computer‐based tests, and underwent several tests involving EEG and NIRS measurements. All participants in part three (and four) of the survey received an incentive of 100 Swiss francs.
Up to three follow‐up interviews (part four of the survey) were carried out bimonthly after the day at the Center for Neurophysiology and Sociophysiology in CATI format. We selected an interviewer from part two for this task. The interviews focused on stress vulnerability, life events and change of symptom load. If a change since the previous interview occurred, the interview was supplemented by further questionnaires and the participant was again asked to provide saliva probes for measuring cortisol levels.
Feedback
At the end of the face‐to‐face interview and the day at the Center for Neurophysiology and Sociophysiology the participants were asked whether they would like to be informed of their personal results at the end of the study. For this purpose we created a webpage and selected several questionnaires and tests for display. For data security reasons, the logins were first sent to the participants and, second, the passwords were supplied by recorded delivery.
Ethical and data security issues
The ZInEP Epidemiology Survey was approved by the Ethics Committee of the canton of Zurich (KEK). The data assessment and storage procedures were evaluated by the data protection office of the canton of Zurich.
Survey instruments and procedures
The list of instruments is displayed in Table 2. The main instruments of the screening (SCL) and the face‐to‐face interview (SPIKE) were adopted from the Zurich Study in order to ascertain comparability of the results.
Table 2.
Topics, questionnaires, scales and tests in the ZInEP Epidemiology Survey
| Survey part | Topic | Issue/instrument/questions | source / comments |
|---|---|---|---|
| Screening | Demographics | Questions based on Swiss Household Panel | http://www.swisspanel.ch |
| interview | Mental health | SCL‐27 | (Hardt et al., 2004) |
| SCL‐90‐subscales SNS, STS, hostility | (Derogatis, 1977; Rössler et al., 2007) | ||
| Substance use (smoking, alcohol use) | Questions based on Swiss Health Survey 2007 | http://www.bfs.admin.ch | |
| Attitudes towards mental disorders and treatment | Questions based on survey from Swiss National | (Lauber et al., 2000) | |
| Research Foundation project no 32‐52571.97 | |||
| Face‐to‐face | Demographics | Mini‐SPIKE | (Angst and Dobler‐Mikola, 1985) |
| interview | Mental health: | Mini‐SPIKE | (Angst and Dobler‐Mikola, 1985) |
| sleep, neurasthenia, panic, generalized anxiety | |||
| disorder, specific phobia, social phobia, | |||
| agoraphobia, depression, suicidality, | |||
| hypomania, obsessive‐compulsive disorder, | |||
| psychosis symptoms, eating disorders | |||
| Substance use: | Mini‐SPIKE, self‐constructed life chart, CAGE | (Angst and Dobler‐Mikola, 1985; Ewing, 1984) | |
| smoking, alcohol use, illicit drug use | |||
| Use of professional and/or lay help | Adapted from SPIKE and modified | (Angst and Dobler‐Mikola, 1985) | |
| Mental disorders among relatives | self‐constructed questions | ||
| Treatment, help seeking | Self‐constructed questions | ||
| Social network, partnership | Adapted from SPIKE (modified version of the | (Weissman and Paykel, 1974) | |
| Social Adjustment Scale, Weissman/Paykel ) | |||
| Expressed emotions | Perceived Criticism Scale (modified) | (Hooley and Teasdale, 1989) | |
| Acute somatic diseases | self‐constructed questions | ||
| Chronic somatic diseases | Self‐constructed questions | ||
| Accidents | Self‐constructed questions | ||
| Attitudes towards mental disorders and treatment | Emotional Reactions to Mental Illness Scale (ERMIS) | (Angermeyer and Matschinger, 2003) | |
| Obstetric complications | questions based on the Obstetric Complications Scale | (Littman and Parmelee, 1978) | |
| Sexual hormones | Self‐constructed questions | Only women | |
| Stuttering, handedness, mother language | Stuttering questions adapted from Craig et al. | (Craig et al., 2002) | |
| handedness questions adapted from Vuoksimaa et al. | (Vuoksimaa et al., 2009) | ||
| Checklists | Personality | Big Five Inventory short form (BFI‐S) | (Schupp and Gerlitz, 2008) |
| Bem Sex Role Inventory (BSRI) | (Schneider‐Düker and Kohler, 1988) | ||
| The Brief Core Schema Scale (BCSS) | (Fowler et al., 2006) | ||
| Positive and Negative Affects Schedule (PANAS) | (Krohne et al., 1996; Watson et al., 1988) | ||
| Mental health/psychosis symptoms | SIAPA: Anomale Sinneswahrnehmungen | (Bunney et al., 1999) | |
| CEQ: Creative Experiences Questionnaire | (Merckelbach et al., 2001) | ||
| Paranoia Checklist | (Freeman et al., 2005; Lincoln et al., 2009) | ||
| Interpersonal Intolerance of Ambiguity Scale (SIA) | (Wolfradt and Rademacher, 1999) | ||
| Schizotypal Personality Questionnaire – Brief (SPQ‐B) | (Raine and Benishay, 1995) | ||
| Mental health/personality disorders | Sensation Seeking Scales, Form V (SSS‐V) SSS‐V | (Beauducel et al., 2003; Zuckerman, 1994) | |
| Assessment of DSM‐IV Personality Disorders (ADP‐IV) | (Doering et al., 2007; Schotte et al., 1998) | ||
| Mental health/ADHD | ADHD Self‐Rating Behaviour Questionnaire | (Rosler et al., 2004) | |
| Wender Utah Rating Scale Short Form (WURS‐K) | (Retz‐Junginger et al., 2003) | ||
| Mental health/PTSD | PTSD Screening‐Scale | (Breslau et al., 1999) | |
| Peritraumatic Dissociation Experiences Questionnaire | (Marmar et al., 1994) | ||
| Mental health/depression, suicidality | Mental Pain (surfeit of the pain subscale) | (Orbach et al., 2004) | |
| The Gotland Male Depression Scale | (Rutz, 1999; Rutz et al., 1995; Walinder and Rutz, 2001) | ||
| Mental health/stress | Trier Inventory for the Assessment of Chronic Stress (TICS) | (Schulz and Schlotz, 1999) | |
| (short form SSCS) | |||
| Perceived Stress Scale | (Cohen et al., 1983; Grassel et al., 2007) | ||
| Maslach Burnout Inventory – General Survey | (Maslach et al., 1996) | ||
| Mental health/risk factors | Adverse experiences in childhood – adapted from SPIKE | ||
| Childhood Trauma Questionnaire | (Bernstein et al., 1994) | ||
| Trauma History Questionnaire | (Green, 1996) | ||
| Life Events: modified version of the Life Events Inventory | (Tennant and Andrews, 1976) | ||
| developed by Tennant/Andrews | |||
| Mental health/protective factors | Brief COPE | (Carver, 1997) | |
| Connor Davidson Resilience Scale (CD‐RISC) | (Connor and Davidson, 2003) | ||
| Dyslexia | Dyslexia‐Checklist by Smythe and Everatt | (ADysTrain, 2009) | |
| Attitudes towards mental disorders and treatment | Attitudes Toward Seeking Professional Psychological | (Fischer and Farina, 1995) | |
| Help Scale‐Short Form (ATSPPH‐SF) | |||
| Perceived Devaluation‐Discrimination Questionnaire | (Link et al., 1989) | ||
| Stigma Stress Questionnaire | (Rüsch et al., 2009a; Rüsch et al., 2009c) | ||
| Stigma Coping Orientation Scales (SCOS) | (Link et al., 2002) | ||
| Depression Literacy Questionnaire | (Griffiths et al., 2004) | ||
| Self‐Stigma in Mental Illness Scale | (Corrigan et al., 2006) | ||
| Barriers to Care Evaluation Scale | (Clement et al., 2012) | ||
| Tests at the | Sexual hormones (estradiol, progesterone, testosterone) | Blood samples | |
| Center for | Stress parameters/allostatic load | Blood, saliva and urine samples | |
| Neurophysiology and | (height, weight, hip/waist ratio, serum HDL, LDL and total | (Seeman et al., 2001) | |
| Sociophysiology | body cholesterol levels; fastening pro‐insulin and fastening | ||
| glucose; high sensitivity C‐reactive Protein (CRP); D‐dimer, | |||
| fibrinogen; DHEA‐S; norepinephrine and epinephrine levels; | |||
| urinary albumin and creatinine) | |||
| Stress parameters/cortisol | Cortisol | Saliva samples from day before and same day | |
| Mental health/psychosis | PANSS | (Kay et al., 1987) | |
| Jumping to Conclusions | (Colbert and Peters, 2002; McKay et al., 2006) | ||
| Sociophysiology | Reading the Mind in the Eyes Test | (Baron‐Cohen et al., 2001) | |
| Digit‐Symbol Coding Test | (Wechsler, 1997) | ||
| Electroencephalography (EEG) | High‐frequency somatosensory evoked potentials (HF‐SEP) | (Kawohl et al., 2007; Norra et al., 2004) | |
| Loudness dependence of auditory evoked potentials | (Gudlowski et al., 2009; Juckel et al., 2003) | ||
| (LDAEP) | |||
| Mismatch negativity (MMN) | (Heekeren et al., 2008; Umbricht and Krljes, 2005) | ||
| NoGo‐anteriorization | (Fallgatter, 2001; Fallgatter and Strik, 1999) | ||
| Near‐infrared spectroscopy (NIRS) | Verbal Fluency test | (Ehlis et al., 2007; Herrmann et al., 2003) | |
| Emotional Stroop test | (Williams et al., 1996) | ||
| Handedness | Edinburgh Handedness Inventory | (Oldfield, 1971) | |
| Follow‐up | Mental health | Perceived events and distress (semi‐structured interview) | Self‐constructed questions |
| interviews | SCL‐27 | (Hardt et al., 2004) | |
| BCSS | (Fowler et al., 2006) | ||
| CD‐RISC2 (abbreviated Connor‐Davidson Resilience Scale) | (Vaishnavi et al., 2007) | ||
| Optional: SPQ‐B | (Raine and Benishay, 1995) | ||
| Stress parameters/cortisol | Optional: cortisol | Saliva samples | |
| Attitudes towards mental disorders and treatment | Client Sociodemographic and Service Receipt Inventory | (Roick et al., 2001) assessed after six months | |
| Mental health service use | Service Use Questionnaire | (Rüsch et al., 2009b) |
Screening instrument
The main instrument of the screening interview was the SCL‐27 (Hardt et al., 2004), i.e. an abbreviated version of the SCL‐90‐R (Derogatis, 1977). It consists of six instead of the original nine subscales covering symptoms of:
depression
dysthymia
vegetative symptoms
agoraphobia
social phobia
mistrust
Just as the SCL‐90‐R, the SCL‐27 also yields an overall score: the GSI. The Cronbach's α of the SCL‐27‐GSI as well as the correlation with the SCL‐90‐R‐GSI were shown to be over 0.9 (Hardt et al., 2004).
We supplemented the screening interview with questions from the original SCL hostility subscale, the SCL psychoticism subscale and the SCL paranoid ideation subscale. While the hostility questions were supposed to help us assign the most experienced interviewers to hostile interviewees, the latter questions were included because of the particular emphasis on subclinical psychosis symptoms in this survey.
Diagnostic instrument
The Mini‐SPIKE applied in the face‐to‐face interview is basically a short form of the SPIKE, the diagnostic instrument of the Zurich Study. It covers symptoms and further diagnostic parameters (length, recurrence, burden) of common mental disorders over the past 12 months.
The SPIKE was first developed in the 1970s (Binder et al., 1982). Initially, it was based on preliminary versions of the Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM‐III). Later, it adopted the DSM‐III‐R and DSM‐IV criteria as they were published. As an exception, the neurasthenia module is based on the International Classification of Diseases, 10th revision (ICD‐10) criteria. The SPIKE covers most common mental disorders. Each diagnostic module of the SPIKE is introduced by a screening question including examples, thus rendering the SPIKE a semi‐structured interview. Positive screening questions elicit detailed questions on symptoms, on subjective distress, on attribution of causes for the symptoms, and on seeking help. Each module is completed by anamnestic questions on symptoms experienced in the past and help seeking.
Validity and reliability testing with the SPIKE was carried out regarding depression and anxiety at the beginning of the Zurich Study when the subjects were in their twenties (Angst et al., 2005). The SPIKE rating of the diagnostic level of depression was found to have high sensitivity and modest specificity (0.95 and 0.59, respectively, for major depression; 0.83 and 0.63, respectively, for minor depression). Likewise, the SPIKE had good sensitivity for detecting subthreshold depression, anxiety and mania (i.e. respective kappas of 0.90, 0.83, 0.67). A limitation with respect of later interviews and also the ZInEP Epidemiology Survey is the narrow age range to which the psychometric assessment primarily applies.
While 17 modules of the Mini‐SPIKE correspond to the SPIKE, the Mini‐SPIKE differs in some instances from its predecessor:
somatoform complaints (except sleep), making up the initial somatic modules of the SPIKE, were excluded in order to enter in medias res and to downsize the face‐to‐face interview length
for the same reason, the questions on use of help were centralized into a separate module
topics such as PTSD or ADHD were not included in the face‐to‐face interview but were covered by checklists
subjective distress was displayed both on an analogue visual scale and on the Pictorial Representation of Illness and Self Measure (PRISM) (Buchi and Sensky, 1999)
the modules covering substance use were extended by life‐charts in order to improve the lifetime information on substance use
Additional questionnaires in the face‐to‐face interview and in the checklists
The face‐to‐face interview was rounded off by several further modules including both conventional SPIKE extensions (social network and support) and new instruments. The latter focused on prevalence of somatic diseases and accidents, on risk factors such as mental disorders among relatives and obstetric complications, and on further single issues which were considered to be preferably covered in the face‐to‐face framework (expressed emotions, social distance, stuttering). Like the Zurich Study, the ZInEP Epidemiology Survey also used a checklist section. In contrast to the Mini‐SPIKE the checklist section was clearly enlarged (see Table 2). More detailed information is displayed at http://www.zinep.ch/epidemiologie/informationforresearchers/.
Modules in the Center for Neurophysiology and Sociophysiology
The day at the Center for Neurophysiology and Sociophysiology combined five different kinds of examinations (see also Table 2 and the webpage mentioned earlier):
questionnaires, partly worked through in face‐to‐face interviews (e.g. the Positive and Negative Syndrome Scale [PANSS]) and partly filled in as checklists
tests, either computer assisted or in paper‐and‐pencil style
biological measurements including blood, saliva and urine probes
EEG measurements
NIRS measurements
Modules in the prospective follow‐up study
The bimonthly follow‐up interviews focused on the effects of the incidence of stressful life events or changing psychopathology scores on psychotic symptoms. The former were assessed by a semi‐structured interview entailing both questions on changes and life events during the past weeks as well as their subjective burden score on a 10‐point scale. Psychopathology scores were again assessed by the SCL‐27 (Hardt et al., 2004) supplemented by questions covering psychosis symptoms. Moreover, we also routinely applied the Brief Core Schema Scale (BCSS; Fowler et al., 2006) and a short form of the Connor‐Davidson resilience scale (CD‐RISC‐2) (Vaishnavi et al., 2007).
In the case of relevant stressors (defined by a cutoff of five points on a 10‐point subjective burden scale) or in the case of relevant change of the SCL‐27 GSI (defined by one standard deviation change with respect to the previous interview – only in follow‐up interviews 2 and 3) the interview was extended by the Schizotypal Personality Questionnaire – Brief (SPQ‐B; Raine and Benishay, 1995). In addition, the participants were asked again to provide a day set of four saliva probes following the same scheme as earlier.
At the third and last follow‐up we used a previously validated Service Use Questionnaire (Rüsch et al., 2009b) to assess mental health service use over the past six months.
Response
The baseline population comprised about 108,000 men and women. In the first step, foreign residents (25% in young adults and slightly over 40% in middle aged adults) were excluded from the baseline. Nearly 40% of the over 57,000 addresses we received from the municipalities were implemented in constructing the screening sample (see Table 3). In 20.2% of the implemented addresses no contact at all could be established, in 6.1% contact was not possible for technical reasons or unavailability, and in 16.0% a person other than the target person refused further contact. If the target person be reached, the response rate was 73.9% (males: 70.6%, females: 77.6%).
Table 3.
Inclusion and participation in the subprojects of the ZinEP Epidemiology Survey
| Information | Included | Not included/refused/drop‐out | Differentiation |
|---|---|---|---|
| Addresses: | |||
| received | 57,400 | ||
| implemented preliminarily | 24,623 | ||
| implemented by GfK in fieldwork | 23,041 | ||
| Preliminary contact established: | |||
| yes | 18386 | ||
| no (no response, telephone responder) | 4655 | ||
| Contact established to target person: | |||
| yes | 13,295 | ||
| no | 5091 | ||
| contact not appropriatea | 1409 | ||
| negative reply by third person | 3,682 | ||
| Screening CATI: | |||
| yes | 9829 | ||
| refused to participate | 3466 | ||
| Face‐to‐face interviews: | |||
| completed | 1500 | ||
| refused to participate | 810 | ||
| Checklists: | |||
| completed | 1179 | ||
| module psychosis | 652 | ||
| module personality disorders | 527 | ||
| not completed | 321 | ||
| complementary checklists completed in the Center for Neurophysiology and Sociophysiology | |||
| module psychosis | 90 | ||
| module personality disorders | 134 | ||
| Tests in the Center for Neurophysiology and Sociophysiology: | |||
| completed | 227 | ||
| controls | 37 | ||
| high SNS/STS scores | 68 | ||
| high SNS scores | 48 | ||
| high STS scores | 76 | ||
| completed, but excluded | 8 | ||
| excluded because of altered scores | 6 | ||
| aborted examination | 2 | ||
| refused to participate | 202 | ||
| contact not possible | 34 | ||
| primary drop‐out | 143 | ||
| secondary drop‐out (after initial ok) | 25 | ||
| Follow‐up CATI | |||
| follow‐up 1 completed | 154 | ||
| refused to participate at follow‐up 1 | 2 | ||
| follow‐up 2 completed | 118 | ||
| refused to participate at follow‐up 2 | 4 | ||
| follow‐up 3 completed | 67 | ||
| refused to participate at follow‐up 3 | 8 | ||
Incorrect phone number person (416); communication not possible (518); not available during study period (280); other reasons
In the next step, among the 9829 screened persons, 6515 (66.3%) initially agreed or were not definitively against carrying out a face‐to‐face interview (males: 70.6%, females: 77.6%). When actually asked for an appointment, 64.9% thereof (males: 69.4%, females: 60.0%) showed up.
The checklists after the face‐to‐face interview were not returned by 21.4% of study participants (n = 321) (males: 28.4% [n = 213], females: 14.4% [n = 108]) despite two personal reminders. This was double the magnitude of missing returns in the Zurich Study. In more detail, not only did females respond more readily than males, but also middle‐aged age groups more readily than younger ones and SCL‐27‐low‐scorers more readily than high‐scorers. The range of missing checklists varied between 44% in the groups of young male high‐scorers and 2% in middle‐aged female low‐scorers.
The participation rate in tests at the Center for Neurophysiology and Sociophysiology was 53.8%. After removal of incorrectly classified participants and aborted tests, 227 subjects remained in this subsample. Of these, 157 subjects engaged in the first follow‐up CATI. Their further participation was precluded by a limited time frame for the follow‐up interviews.
As expected, the response patterns were skewed by two main factors: urbanicity and education level. Regarding urbanicity, 38.7% of the population (restricted to the birth years used in this study) lived in one of the two major cities (Zurich, Winterthur), whereas the proportion of face‐to‐face interviewees from Zurich and Winterthur was 56.8%. The skewing factors regarding education level are displayed in Table 4. Persons with a low education status or administrative and technical professions had higher refusal rates in each survey part than persons with a university background and high educational level.
Table 4.
Education level of participants and drop‐outs of the screening and face‐to‐face interview samples
| Highest education level | Screening participants | Screening dropouts | Face‐to‐face participants | Face‐to‐face dropouts | Populationa |
|---|---|---|---|---|---|
| Primary level | 4.7 | 11.8 | 5.0 | 5.9 | 8.0 |
| Crafts/administrative/technical professions (basic level) | 38.9 | 51.5 | 34.3 | 47.4 | 41.6 |
| Secondary school level, college | 18.0 | 10.4 | 19.6 | 18.8 | 13.7 |
| High level professional formation, technical college, university | 38.4 | 26.3 | 41.1 | 27.8 | 36.7 |
| Total | 100 | 100 | 100 | 100 | 100 |
The population refers to Swiss residents with same birth years such as in the study sample.
Consequently, urbanicity and education level – together with the sample stratification scheme along SCL‐27 GSI scores – are key variables in determining weighting scores to represent the population of young and middle‐aged adults in analyses of the data. We adopted a three‐step weighting procedure following partly the procedure of the Swiss Household Panel (Voorpostel et al., 2010). In the first step, weights were introduced to adjust for the non‐response and under‐representation regarding to urbanicity and education level while rougly accounting for the sex‐birth year structure of the face‐to‐face sample. In the second step, calibration was applied to adjust the weights such that the totals of the stratification variable (high‐/low‐scorer status on SCL‐27) were re‐established in each sex‐birth year subgroup. In the third step, the weights were finally adjusted for the proportion of each sex‐birth year subgroup within the population of the 20–40 year old Swiss citizens in the canton of Zurich, again retaining the totals of the stratification variable. The mean of the step 1 weights was 1.01 (SD = 0.58, range 0.43–5.01), the mean of the adjusted step 2 weights was 1.00 (SD = 0.57, range 0.39–5.24) and similarly of step 3: 1.00 (SD = 0.59, range 0.36–5.99). The final weights resulted from combining the latter with the design weights according to the stratification of the sample (one for the high‐scorer status and 4.5 for the low‐scorer status on SCL‐27) and had a mean of 2.4 (SD = 2.35, range 0.41–21.94).
Discussion
This report introduces the Epidemiology Survey of ZInEP, a new study in psychiatric epidemiology carried out in Zurich, Switzerland. While the survey parallels the Zurich Study in many instances, it provides a new large database which will be relevant for mental health services research, stigma research and interdisciplinary research including neurobiology, sociophysiology and genetics. Among other things, the survey put particular emphasis on psychosis syndromes and their link to stress vulnerability. In this context, the survey pursued new approaches by integrating a subproject with tests in the Center for Neurophysiology and Sociophysiology and by embedding a prospective study assessing stressful events and their consequences for psychosis syndromes. The survey provides a model of how epidemiological and experimental research can be combined.
The survey was subject to several limitations. A major obstacle was the ongoing disappearance of landline telephone numbers, which are being replaced by mobile phones or kept private in order to avoid commercial calls. The survey took place in the midst of this process. The proportion of mobiles may be particularly high in the following four subgroups: (1) highly mobile subjects no longer living in their parents’ home but not having their own family either, (2) participants starting a new working career or having a job requiring high mobility, (3) subjects with low financial resources, and (4) subjects who are marginalized and/or have severe mental or substance abuse problems. This profile, in particular the subgroups two and four, may be quite similar to the profile of drop‐outs in population surveys, for example, also in the Zurich Study (Eich et al., 2003). However, surveys that rely on specific samples drawn from the population such as birth year groups, appear to be less and less feasible.
In sum, the four subprojects of the ZInEP Epidemiology Survey deliver a large database providing not only comprehensive information on issues in psychiatric epidemiology but also a great deal of material for interdisciplinary approaches with a spectrum ranging from health services to experimental pathological research.
Declaration of interest statement
The authors have no competing interests.
Acknowledgements
ZInEP was supported by a private donation. The donor had no further role in the experimental design, the collection, analysis, and interpretation of data, the writing of this report or the decision to submit this paper for publication. The ZInEP Epidemiology Survey, in particular research in the Center for Neurophysiology and Sociophysiology, was supported by the Swiss National Science Foundation (grant # 3247B0‐122071). The population and education data was provided by the Swiss Federal Statistical Office. Cristina Lubini‐Müller, senior interviewer in the ZInEP Epidemiology Survey and in the Zurich Study, was of great importance for us.
Ajdacic‐Gross V., Müller M., Rodgers S., Warnke I., Hengartner M. P., Landolt K., Hagenmuller F., Meier M., Tse L.‐T., Aleksandrowicz A., Passardi M., Knöpfli D., Schönfelder H., Eisele J., Rüsch N., Haker H., Kawohl W., Rössler W. (2014), The ZInEP Epidemiology Survey: background, design and methods, International Journal of Methods in Psychiatric Research, 23, pages 451–468, doi: 10.1002/mpr.1441
References
- ADysTrain . (2009) Legasthenie bei jungen Erwachsenen – 12 Handbücher, Graz: ADysTrain. [Google Scholar]
- Andreasson S., Allebeck P., Engstrom A., Rydberg U. (1987) Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet, 2(8574), 1483–1486. [DOI] [PubMed] [Google Scholar]
- Angermeyer M.C., Matschinger H. (2003) The stigma of mental illness: effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatrica Scandinavica, 108(4), 304–309. [DOI] [PubMed] [Google Scholar]
- Angst J., Dobler‐Mikola A. (1985) The Zurich Study – a prospective epidemiological study of depressive, neurotic and psychosomatic syndromes. IV. Recurrent and nonrecurrent brief depression. European Archives of Psychiatry and Neurological Sciences, 234(6), 408–416. [DOI] [PubMed] [Google Scholar]
- Angst J., Dobler‐Mikola A., Binder J. (1984) The Zurich study – a prospective epidemiological study of depressive, neurotic and psychosomatic syndromes. I. Problem, methodology. European Archives of Psychiatry and Neurological Sciences, 234(1), 13–20. [DOI] [PubMed] [Google Scholar]
- Angst J., Gamma A., Neuenschwander M., Ajdacic‐Gross V., Eich D., Rossler W., Merikangas K.R. (2005) Prevalence of mental disorders in the Zurich Cohort Study: a twenty year prospective study. Epidemiologia e Psichiatria Sociale, 14(2), 68–76. [DOI] [PubMed] [Google Scholar]
- Baron‐Cohen S., Wheelwright S., Hill J., Raste Y., Plumb I. (2001) The “Reading the Mind in the Eyes” test revised version: a study with normal adults, and adults with asperger syndrome or high‐functioning autism. Journal of Child Psychology and Psychiatry, 42(2), 241–251. [PubMed] [Google Scholar]
- Beauducel A., Strobel A., Brocke B. (2003) Psychometrische Eigenschaften und Normen einer deutschsprachigen Fassung der Sensation Seeking‐Skalen, Form V, Diagnostica, 49(2), 61–72. [Google Scholar]
- Bernstein D.P., Fink L., Handelsman L., Foote J., Lovejoy M., Wenzel K., Sapareto E., Ruggiero J. (1994) Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry, 151(8), 1132–1136. [DOI] [PubMed] [Google Scholar]
- Bijl R.V., van Zessen G., Ravelli A., de Rijk C., Langendoen Y. (1998) The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Social Psychiatry and Psychiatric Epidemiology, 33(12), 581–586. [DOI] [PubMed] [Google Scholar]
- Binder J., Dobler‐Mikola A., Angst J. (1982) A prospective epidemiological study of psychosomatic and psychiatric syndromes in young adults. Psychotherapy and Psychosomatics, 38(1), 128–140. [DOI] [PubMed] [Google Scholar]
- Breslau N., Peterson E.L., Kessler R.C., Schultz L.R. (1999) Short screening scale for DSM‐IV posttraumatic stress disorder. American Journal of Psychiatry, 156(6), 908–911. [DOI] [PubMed] [Google Scholar]
- Buchi S., Sensky T. (1999) PRISM: Pictorial Representation of Illness and Self Measure. A brief nonverbal measure of illness impact and therapeutic aid in psychosomatic medicine. Psychosomatics, 40(4), 314–320. [DOI] [PubMed] [Google Scholar]
- Bunney W.E., Jr , Hetrick W.P., Bunney B.G., Patterson J.V., Jin Y., Potkin S.G., Sandman C.A. (1999) Structured Interview for Assessing Perceptual Anomalies (SIAPA). Schizophrenia Bulletin, 25(3), 577–592. [DOI] [PubMed] [Google Scholar]
- Carver C.S. (1997) You want to measure coping but your protocol's too long: consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. [DOI] [PubMed] [Google Scholar]
- Clement S., Brohan E., Jeffery D., Henderson C., Hatch S.L., Thornicroft G. (2012) Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry, 12, 1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983) A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Colbert S.M., Peters E.R. (2002) Need for closure and jumping‐to‐conclusions in delusion‐prone individuals. Journal of Nervous and Mental Disease, 190(1), 27–31. [DOI] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R. (2003) Development of a new resilience scale: the Connor–Davidson Resilience Scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. [DOI] [PubMed] [Google Scholar]
- Corrigan P.W., Watson A.C., Barr L. (2006) The self‐stigma of mental illness: Implications for self‐esteem and self‐efficacy. Journal of Social and Clinical Psychology, 25(9), 875–884. [Google Scholar]
- Craig A., Hancock K., Tran Y., Craig M., Peters K. (2002) Epidemiology of stuttering in the community across the entire life span. Journal of Speech, Language, and Hearing Research, 45(6), 1097–1105. [DOI] [PubMed] [Google Scholar]
- de Graaf R., Ten Have M., van Dorsselaer S. (2010) The Netherlands Mental Health Survey and Incidence Study‐2 (NEMESIS‐2): design and methods. International Journal of Methods in Psychiatric Research, 19(3), 125–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L.R. (1977) SCL‐90. Administration, Scoring and Procedures Manual for the R (Revised) Version and Other Instruments of the Psychopathology Rating Scale Series, Chicago, IL, John Hopkins University School of Medicine. [Google Scholar]
- Doering S., Renn D., Hofer S., Rumpold G., Smrekar U., Janecke N., Schatz D.S., Schotte C., DeDoncker D., Schussler G. (2007) Validation of the “Assessment of DSM‐IV Personality Disorders (ADP‐IV)” Questionnaire. Zeitschrift für Psychosomatische Medizin und Psychotherapie, 53(2), 111–128. [DOI] [PubMed] [Google Scholar]
- Dunn G., Pickles A., Tansella M., Vazquez‐Barquero J.L. (1999) Two‐phase epidemiological surveys in psychiatric research. British Journal of Psychiatry, 174(2), 95–100. [DOI] [PubMed] [Google Scholar]
- Ehlis A.‐C., Herrmann M.J., Plichta M.M., Fallgatter A.J. (2007) Cortical activation during two verbal fluency tasks in schizophrenic patients and healthy controls as assessed by multi‐channel near‐infrared spectroscopy. Psychiatry Research: Neuroimaging, 156(1), 1–13. [DOI] [PubMed] [Google Scholar]
- Eich D., Ajdacic‐Gross V., Condrau M., Huber H., Gamma A., Angst J., Rossler W. (2003) The Zurich Study: participation patterns and Symptom Checklist 90‐R scores in six interviews, 1979–99. Acta Psychiatrica Scandinavica, Supplement (418), 11–14. [DOI] [PubMed]
- Ewing J.A. (1984) Detecting alcoholism. The CAGE questionnaire. JAMA, 252(14), 1905–1907. [DOI] [PubMed] [Google Scholar]
- Fallgatter A.J. (2001) Electrophysiology of the prefrontal cortex in healthy controls and schizophrenic patients: a review. Journal of Neural Transmission, 108(6), 679–694. [DOI] [PubMed] [Google Scholar]
- Fallgatter A.J., Strik W.K. (1999) The NoGo‐anteriorization as a neurophysiological standard‐index for cognitive response control. International Journal of Psychophysiology, 32(3), 233–238. [DOI] [PubMed] [Google Scholar]
- Fischer E.H., Farina A. (1995) Attitudes toward seeking professional psychological help: a shortened form and considerations for research. Journal of College Student Development, 36(4), 368–373. [Google Scholar]
- Fowler D., Freeman D., Smith B., Kuipers E., Bebbington P., Bashforth H., Coker S., Hodgekins J., Gracie A., Dunn G., Garety P. (2006) The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non‐clinical and psychosis samples. Psychological Medicine, 36(6), 749–759. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P.A., Bebbington P.E., Smith B., Rollinson R., Fowler D., Kuipers E., Ray K., Dunn G. (2005) Psychological investigation of the structure of paranoia in a non‐clinical population. British Journal of Psychiatry, 186(5), 427–435. [DOI] [PubMed] [Google Scholar]
- Grassel E., Bock V., Rosanowski F. (2007) Critical factors for subjective burden of mothers of children with developmental language disorders. HNO, 55(7), 575–582. [DOI] [PubMed] [Google Scholar]
- Green B. (1996) Trauma History Questionnaire In Stamm B.H. (ed.) Measurement of Stress, Trauma, and Adaptation, pp. 366–369, Lutherville, MD: Sidran Press. [Google Scholar]
- Griffiths K.M., Christensen H., Jorm A.F., Evans K., Groves C. (2004) Effect of web‐based depression literacy and cognitive‐behavioural therapy interventions on stigmatising attitudes to depression: randomised controlled trial. British Journal of Psychiatry, 185(4), 342–349. [DOI] [PubMed] [Google Scholar]
- Gudlowski Y., Özgürdal S., Witthaus H., Gallinat J., Hauser M., Winter C., Uhl I., Heinz A., Juckel G. (2009) Serotonergic dysfunction in the prodromal, first‐episode and chronic course of schizophrenia as assessed by the loudness dependence of auditory evoked activity. Schizophrenia Research, 109(13), 141–147. [DOI] [PubMed] [Google Scholar]
- Hardt J., Egle U.T., Kappis B., Hessel A., Brahler E. (2004) Symptom Checklist SCL‐27. Psychotherapie, Psychosomatik, Medizinische Psychologie, 54(5), 214–223. [DOI] [PubMed] [Google Scholar]
- Heekeren K., Daumann J., Neukirch A., Stock C., Kawohl W., Norra C., Waberski T.D., Gouzoulis‐Mayfrank E. (2008) Mismatch negativity generation in the human 5HT2A agonist and NMDA antagonist model of psychosis. Psychopharmacology, 199(1), 77–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann M.J., Ehlis A.C., Fallgatter A.J. (2003) Frontal activation during a verbal‐fluency task as measured by near‐infrared spectroscopy. Brain Research Bulletin, 61(1), 51–56. [DOI] [PubMed] [Google Scholar]
- Hooley J.M., Teasdale J.D. (1989) Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. Journal of Abnormal Psychology, 98(3), 229–235. [DOI] [PubMed] [Google Scholar]
- Jacobi F., Wittchen H.U., Holting C., Sommer S., Lieb R., Hofler M., Pfister H. (2002) Estimating the prevalence of mental and somatic disorders in the community: aims and methods of the German National Health Interview and Examination Survey. International Journal of Methods in Psychiatric Research, 11(1), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins R., Bebbington P., Brugha T.S., Farrell M., Lewis G., Meltzer H. (1998) British psychiatric morbidity survey. British Journal of Psychiatry, 173(1), 4–7. [DOI] [PubMed] [Google Scholar]
- Juckel G., Gallinat J., Riedel M., Sokullu S., Schulz C., Möller H.J., Müller N., Hegerl U. (2003) Serotonergic dysfunction in schizophrenia assessed by the loudness dependence measure of primary auditory cortex evoked activity. Schizophrenia Research, 64(2–3), 115–124. [DOI] [PubMed] [Google Scholar]
- Kawohl W., Waberski T.D., Darvas F., Norra C., Gobbelé R., Buchner H. (2007) Comparative source localization of electrically and pressure‐stimulated multichannel somatosensory evoked potentials. Journal of Clinical Neurophysiology, 24(3), 257–262. [DOI] [PubMed] [Google Scholar]
- Kay S.R., Flszbein A., Opfer L.A. (1987) The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261–276. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Angermeyer M., Anthony J.C., De Graaf R., Demyttenaere K., Gasquet I., De Girolamo G., Gluzman S., Gureje O., Haro J.M., Kawakami N., Karam A., Levinson D., Medina Mora M.E., Oakley Browne M.A., Posada‐Villa J., Stein D.J., Adley Tsang C.H., Aguilar‐Gaxiola S., Alonso J., Lee S., Heeringa S., Pennell B.E., Berglund P., Gruber M.J., Petukhova M., Chatterji S., Ustun T.B. (2007) Lifetime prevalence and age‐of‐onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry, 6(3), 168–176. [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. (2005) Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., McGonagle K.A., Zhao S., Nelson C.B., Hughes M., Eshleman S., Wittchen H.U., Kendler K.S. (1994) Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- Krohne H.W., Egloff B., Kohlmann C.‐W., Tausch A. (1996) Untersuchungen mit einer deutschen Version der " Positive and Negative Affect Schedule" (PANAS). Diagnostica, 42(2), 139–156. [Google Scholar]
- Lauber C., Nordt C., Sartorius N., Falcato L., Rossler W. (2000) Public acceptance of restrictions on mentally ill people. Acta Psychiatrica Scandinavica, Supplement(407), 26–32. [DOI] [PubMed]
- Lincoln T.M., Peter N., Schafer M., Moritz S. (2009) Impact of stress on paranoia: an experimental investigation of moderators and mediators. Psychological Medicine, 39(7), 1129–1139. [DOI] [PubMed] [Google Scholar]
- Link B., Cullen F.T., Struening E., Shrout P.E. (1989) A modified labelling theory approach to mental disorders: an empirical assessment. American Sociological Review, 54(3), 400–423. [Google Scholar]
- Link B.G., Struening E.L., Neese‐todd S., Asmussen S., Phelan J.C. (2002) On describing and seeking to change the experience of stigma. American Journal of Psychiatric Rehabilitation, 6(2), 201–231. [Google Scholar]
- Littman B., Parmelee A.H., Jr (1978) Medical correlates of infant development. Pediatrics, 61(3), 470–474. [DOI] [PubMed] [Google Scholar]
- Marmar C.R., Weiss D.S., Schlenger W.E., Fairbank J.A., Jordan B.K., Kulka R.A., Hough R.L. (1994) Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. American Journal of Psychiatry, 151(6), 902–907. [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S., Leiter M.P. (1996) MBI: Maslach Burnout Inventory Manual, Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- McKay R., Langdon R., Coltheart M. (2006) Need for closure, jumping to conclusions, and decisiveness in delusion‐prone individuals. Journal of Nervous and Mental Disease, 194(6), 422–426. [DOI] [PubMed] [Google Scholar]
- Merckelbach H., Horselenberg R., Muris P. (2001) The Creative Experiences Questionnaire (CEQ): a brief self‐report measure of fantasy proneness. Personality and Individual Differences, 31(6), 987–995. [Google Scholar]
- Norra C., Waberski T.D., Kawohl W., Kunert H.J., Hock D., Gobbelé R., Buchner H., Hoff P. (2004) High‐frequency somatosensory thalamocortical oscillations and psychopathology in schizophrenia. Neuropsychobiology, 49(2), 71–80. [DOI] [PubMed] [Google Scholar]
- Oldfield R.C. (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia, 9(1), 97–113. [DOI] [PubMed] [Google Scholar]
- Orbach I., Giboa‐Schechtman E., Johan M., Mikulincer M. (2004) Tolerance for Mental Pain Scale, Ramat‐Gan: Department of Psychology, Bar‐Ilan University. [Google Scholar]
- Preisig M., Waeber G., Vollenweider P., Bovet P., Rothen S., Vandeleur C., Guex P., Middleton L., Waterworth D., Mooser V., Tozzi F., Muglia P. (2009) The PsyCoLaus study: methodology and characteristics of the sample of a population‐based survey on psychiatric disorders and their association with genetic and cardiovascular risk factors. BMC Psychiatry, 9, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A., Benishay D. (1995) The SPQ‐B: A brief screening instrument for schizotypal personality disorder. Journal of Personality Disorders, 9(4), 346–355. [Google Scholar]
- Rantakallio P. (1988) The longitudinal study of the northern Finland birth cohort of 1966. Paediatric and Perinatal Epidemiology, 2(1), 59–88. [DOI] [PubMed] [Google Scholar]
- Regier D.A., Kaelber C.T. (1995) The Epidemiologic Catchment Area (ECA) program: studying the prevalence and incidence of psychopathology In Tsuang M.T., Tohen M., Zahner G.E.P. (eds) Textbook in Psychiatric Epidemiology, pp. 135–155, New York: John Wiley & Sons. [Google Scholar]
- Retz‐Junginger P., Retz W., Blocher D., Stieglitz R.D., Georg T., Supprian T., Wender P.H., Rosler M. (2003) [Reliability and validity of the Wender‐Utah‐Rating‐Scale short form. Retrospective assessment of symptoms for attention deficit/hyperactivity disorder]. Nervenarzt, 74(11), 987–993. [DOI] [PubMed] [Google Scholar]
- Roick C., Kilian R., Matschinger H., Bernert S., Mory C., Angermeyer M.C. (2001) [German adaptation of the client sociodemographic and service receipt inventory – an instrument for the cost of mental health care]. Psychiatrische Praxis, 28(Suppl. 2), S84–S90. [DOI] [PubMed] [Google Scholar]
- Rosler M., Retz W., Retz‐Junginger P., Thome J., Supprian T., Nissen T., Stieglitz R.D., Blocher D., Hengesch G., Trott G.E. (2004) Tools for the diagnosis of attention‐deficit/hyperactivity disorder in adults. Self‐rating behaviour questionnaire and diagnostic checklist. Nervenarzt, 75(9), 888–895. [DOI] [PubMed] [Google Scholar]
- Rössler W., Riecher‐Rössler A., Angst J., Murray R., Gamma A., Eich D., van Os J., Ajdacic Gross V. (2007) Psychotic experiences in the general population: a twenty‐year prospective community study. Schizophrenia Research, 92(1–3), 1–14. [DOI] [PubMed] [Google Scholar]
- Rüsch N., Corrigan P.W., Powell K., Rajah A., Olschewski M., Wilkniss S., Batia K. (2009a) A stress‐coping model of mental illness stigma: II. Emotional stress responses, coping behavior and outcome. Schizophrenia Research, 110(1–3), 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüsch N., Corrigan P.W., Wassel A., Michaels P., Larson J.E., Olschewski M., Wilkniss S., Batia K. (2009b) Self‐stigma, group identification, perceived legitimacy of discrimination and mental health service use. British Journal of Psychiatry, 195(6), 551–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüsch N., Corrigan P.W., Wassel A., Michaels P., Olschewski M., Wilkniss S., Batia K. (2009c) A stress‐coping model of mental illness stigma: I. Predictors of cognitive stress appraisal. Schizophrenia Research, 110(1–3), 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutz W. (1999) Improvement of care for people suffering from depression: the need for comprehensive education. International Clinical Psychopharmacology, 14(Suppl. 3), S27–S33. [DOI] [PubMed] [Google Scholar]
- Rutz W., von Knorring L., Pihlgren H., Rihmer Z., Walinder J. (1995) Prevention of male suicides: lessons from Gotland study. Lancet, 345(8948), 524. [DOI] [PubMed] [Google Scholar]
- Schneider‐Düker M., Kohler A. (1988) Die Erfassung von Geschlechterrollen – Ergebnisse zur deutschen Neukonstruktion des Bem‐Sex‐Role‐Inventory. Diagnostica, 34(4), 256–270. [Google Scholar]
- Schotte C.K., de Doncker D., Vankerckhoven C., Vertommen H., Cosyns P. (1998) Self‐report assessment of the DSM‐IV personality disorders. Measurement of trait and distress characteristics: the ADP‐IV. Psychological Medicine, 28(5), 1179–1188. [DOI] [PubMed] [Google Scholar]
- Schulz P., Schlotz W. (1999) Das Trierer Inventar zur Erfassung von chronischem Streß (TICS): Skalenkonstruktion, teststatistische Überprüfung und Validierung der Skala Arbeitsüberlastung. Diagnostica, 45(1), 8–19. [Google Scholar]
- Schupp J., Gerlitz J.‐Y. (2008) BFI‐S: Big Five Inventory‐SOEP In Glöckner‐Rist A. (ed.) Zusammenstellung sozialwissenschaftlicher Items und Skalen (ZIS Version 1200), Bonn: GESIS. [Google Scholar]
- Seeman T.E., McEwen B.S., Rowe J.W., Singer B.H. (2001) Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences USA, 98(8), 4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennant C., Andrews G. (1976) A scale to measure the stress of life events. Australian and New Zealand Journal of Psychiatry, 10(1), 27–32. [DOI] [PubMed] [Google Scholar]
- Umbricht D., Krljes S. (2005) Mismatch negativity in schizophrenia: a meta‐analysis. Schizophrenia Research, 76(1), 1–23. [DOI] [PubMed] [Google Scholar]
- Vaishnavi S., Connor K., Davidson J.R. (2007) An abbreviated version of the Connor–Davidson Resilience Scale (CD‐RISC), the CD‐RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Research, 152(2–3), 293–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voorpostel M., Tillmann R., Lebert F., Weaver B., Kuhn U., Lipps O., Ryser V.‐A., Schmid F., Wernli B. (2010) Swiss Household Panel Userguide (1999–2009), Wave 11, Lausanne: FORS. [Google Scholar]
- Vuoksimaa E., Koskenvuo M., Rose R.J., Kaprio J. (2009) Origins of handedness: a nationwide study of 30,161 adults. Neuropsychologia, 47(5), 1294–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walinder J., Rutz W. (2001) Male depression and suicide. International Clinical Psychopharmacology, 16(Suppl. 2), S21–S24. [DOI] [PubMed] [Google Scholar]
- Watson D., Clark L.A., Tellegen A. (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wechsler D. (1997) Wechsler Adult Intelligence Scale – Third Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Weissman M., Paykel E.S. (1974) The Depressed Woman: Study of Social Relationships, Chicago, IL: University of Chicago Press. [Google Scholar]
- Williams J.M.G., Mathews A., MacLeod C. (1996) The emotional Stroop task and psychopathology. Psychological Bulletin, 120(1), 3–24. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Perkonigg A., Lachner G., Nelson C.B. (1998) Early developmental stages of psychopathology study (EDSP): objectives and design. European Addiction Research, 4(1–2), 18–27. [DOI] [PubMed] [Google Scholar]
- Wolfradt U., Rademacher J. (1999) Interpersonale Ambiguitätsintoleranz als klinisches Differentialkriterium: Skalenentwicklung und Validierung. [Interpersonal intolerance of ambiguity as a clinical differential criterium: Scale development and validation]. Zeitschrift für Differentielle und Diagnostische Psychologie, 20(3), 72–79. [Google Scholar]
- Zuckerman M. (1994) Behavioral Expressions and Biosocial Bases of Sensation Seeking, Cambridge: Cambridge University Press. [Google Scholar]


