Abstract
Despite the high impact of mental disorders in society, European mental health research is at a critical situation with a relatively low level of funding, and few advances been achieved during the last decade. The development of coordinated research policies and integrated research networks in mental health is lagging behind other disciplines in Europe, resulting in lower degree of cooperation and scientific impact.
To reduce more efficiently the burden of mental disorders in Europe, a concerted new research agenda is necessary. The ROAMER (Roadmap for Mental Health Research in Europe) project, funded under the European Commission's Seventh Framework Programme, aims to develop a comprehensive and integrated mental health research agenda within the perspective of the European Union (EU) Horizon 2020 programme, with a translational goal, covering basic, clinical and public health research.
ROAMER covers six major domains: infrastructures and capacity building, biomedicine, psychological research and treatments, social and economic issues, public health and well‐being. Within each of them, state‐of‐the‐art and strength, weakness and gap analyses were conducted before building consensus on future research priorities. The process is inclusive and participatory, incorporating a wide diversity of European expert researchers as well as the views of service users, carers, professionals and policy and funding institutions. Copyright © 2013 John Wiley & Sons, Ltd.
Keywords: Europe, health priorities, mental health research, mental disorders, well‐being research
Introduction
Europe has one of the highest levels of resourcing for mental health in the world, with an overall good, though regionally variable, supply of trained professionals, as well as coordinated policies and systems to support their interventions (WHO, 2005). Most importantly, policy‐makers in the European Union (EU) have acknowledged the tremendous size and burden caused by mental disorders and mental health problems in the EU and the need to respond in terms of improved policy, strategies and resources at the EU level. Starting with the 2005 European Commission (EC) Green Paper (EC, 2005), through to the 2008 European Pact on Mental Health and Well‐being (EC and WHO Europe, 2008), and culminating in the European Parliament Resolution of 19 February 2009 on Mental Health, the focus has been on a European strategy for mental health, while recognizing that much of the responsibility for implementation of actions rests with Member States. This envisions a coordinated and concerted response which needs to be proactive, evidence‐based, and directed to the design and implementation of comprehensive, integrated, effective and cost‐efficient mental health systems, together with the societal and policy changes needed to achieve the stated objectives. They should address mental health promotion, prevention and early targeted intervention, treatment and rehabilitation of mental disorders, care and recovery and social inclusion across the life span and for all societal groups.
Better understanding of the impact of mental disorders has acted as a catalyst for action. Mental disorders account for almost one third of the total disease burden for non‐communicable diseases, with depression alone being the largest component of Europe's total burden (WHO, 2010). Estimates of the cumulative lifetime risk for mental disorders suggest that up to the age 65, roughly 50% of the EU population will be affected by mental disorders at some point in their life (Wittchen et al., 2011). Enduring mental health problems are also associated with economic deprivation, poverty, stigma and social exclusion (MHE, 2007; Thornicroft et al., 2009; Brohan et al., 2011; Lasalvia et al., 2013), employment problems, including absenteeism, and loss of productivity (McDaid et al., 2008). Somatic co‐morbidity and mortality are also higher in individuals with mental disorders (Laursen et al., 2011; De Hert et al., 2011). Moreover, results from epidemiologic studies seem to indicate that the burden of mental disorders is increasing more than decreasing (Murray et al., 2012). The Global Burden of Disease Study 2010 estimated that the proportion of Disability Adjusted Life Years (DALY) caused by mental and behavioural disorders increased from 5.38% in 1990 to 7.44% in 2010, a figure similar to all neoplasms and higher than respiratory diseases, musculoskeletal disorders and diabetes (Murray et al., 2012).
Noteworthy, mental health is not merely the absence of mental disorders, but a resource of importance for the well‐being of individuals, families and societies (Wahlbeck, 2011a). Population mental health and well‐being have a significant impact on countries and their human, mental, social and economic capital. The mental health of Europeans is a crucial prerequisite for meeting the strategic employment, education and social inclusion targets of the EU.
Policies that aim to reduce the impact of mental disorders in Europe will not be optimally effective if we do not increase our knowledge of their determinants, on how to prevent them, and on how to improve the efficacy, effectiveness and cost effectiveness of interventions and their translation into clinical practice. Unfortunately, research resources for mental health in many European countries are relatively modest. For example, a study in Spain comparing the investment in research relative to DALY in the population, found that mean funding per DALY was €25.0 for all medical conditions, including mental disorders, which is much higher than the research funding devoted to specific mental disorders. For example, for depression the mean funding per DALY was €4.0, alcohol abuse €0.2, and bipolar disorder €2.9. Only schizophrenia (€35.8) exceeded the overall mean (Catalá López et al., 2009). In another study, Chevreul et al. (2012) compared public sector and not‐for‐profit sources of research funds for the prevention and treatment of mental health problems (excluding dementia) in France, the United Kingdom (UK) and the United States. Although the prevalence of mental health disorders is roughly the same in those three countries, accounting for 17% to 25% of the overall burden of disease, and with similar mental health expenditures per capita, the share of health budget and charitable research funding devoted to mental disorders ranged from 2% in France and 7% in the UK to 16% in the United States. Per capita funding also showed great variation ($1.1 in France, $3.5 in the UK and $17.2 in the United States in 2007).
Private funds allocated to the development of new treatments may also be decreasing in the area of psychiatry, since major pharmaceutical companies have withdrawn from key areas of neuroscience research. Deficiencies in the science that underpins drug discovery, the costs associated with those advances, and regulatory difficulties have also been reported as possible reasons for these decisions (Nutt and Goodwin, 2011).
Not only are research resources comparatively small at a national level, but there has been limited European coordination of approaches to mental disorder and mental health services research. The EU reports that research in brain disorders is less funded and more fragmented than in other areas when comparing research in the EU versus United States (COM, 2008). This has resulted in (i) a limited research on the promotion of well‐being, disorder prevention and early intervention; (ii) the absence of a clear route from basic discovery to potential preventive and therapeutic applications that remains today long and unpredictable until the point of a total lack of such a continuum; (iii) protracted and prohibitively expensive efforts before novel biological and psychosocial treatments and rehabilitation methods become available and are translated in order to significantly affect mental health burden on a population level; and (iv) the absence of population‐wide strategies using cost‐effective, and efficient promotion and preventive interventions across different developmental and life course stages and which promote social inclusion and reduction of stigma and discrimination.
In this context, the ROAMER (roadmap for mental health research in Europe) project, funded under the EC's Seventh Framework Programme (FP7), aims to develop a comprehensive and integrated mental health research roadmap, orientated to translational research, sensitive to potential shifts in future needs in light of demographic changes, aligned with the policies of the Horizon 2020 programme, and addressing a pragmatic and integrated approach to the development of a pan‐European strategy to matching mental health services to needs.
In this paper we outline the aims and methodological approach of ROAMER, putting this into the context of current research gaps in mental health and mental disorder research in the EU. We will illustrate this with examples drawn from biomedical, psychological, well‐being, social, economic and public health perspectives.
Methods
ROAMER aims at developing a roadmap on the promotion and integration of mental health research across European states. To ensure an effective and widely accepted roadmap, we want the process to be inclusive and participatory, incorporating a large diversity of research scientists from many disciplines and also incorporating the view of service users, carers, professionals, as well as policy and funding institutions. The project started in October 2011 and is taking place over three years.
Towards these goals ROAMER has established six domains: (i) infra‐structures and capacity building; (ii) biomedicine; (iii) psychological research and interventions; (iv) social and economic issues; (v) public health; (vi) well‐being; and a cross‐sectional task force on clinical research (Figure 1). Within each of the domains, work groups comprised of renowned scientists have been asked to participate. Participants were selected based on their expertise and, importantly, complementarity. These groups defined the scope of each domain and the main issues to be covered. They conducted an initial state‐of‐the‐art analysis of strength and weaknesses, enumerating core gaps in current knowledge, and delineated advances needed in research in their fields. This process was developed in three different phases centred around face‐to‐face meetings. Moreover, results were and will be presented to stakeholders (service users, carers, professionals, government and funding institutions, health service providers, and others) in specific consensus meetings (Figure 2). A much greater participation of scientists and stakeholders has been achieved and will be further promoted through mail and web‐based surveys. A survey among national stakeholders' associations about priorities for mental health research in Europe has been already conducted (Fiorillo et al., 2013). Documents are available on the ROAMER web page (http://www.roamer-mh.org). Consensus in each of the stages is being achieved using a modified Delphi method.
Figure 1.

Work plan strategy of the ROAMER project.
Figure 2.
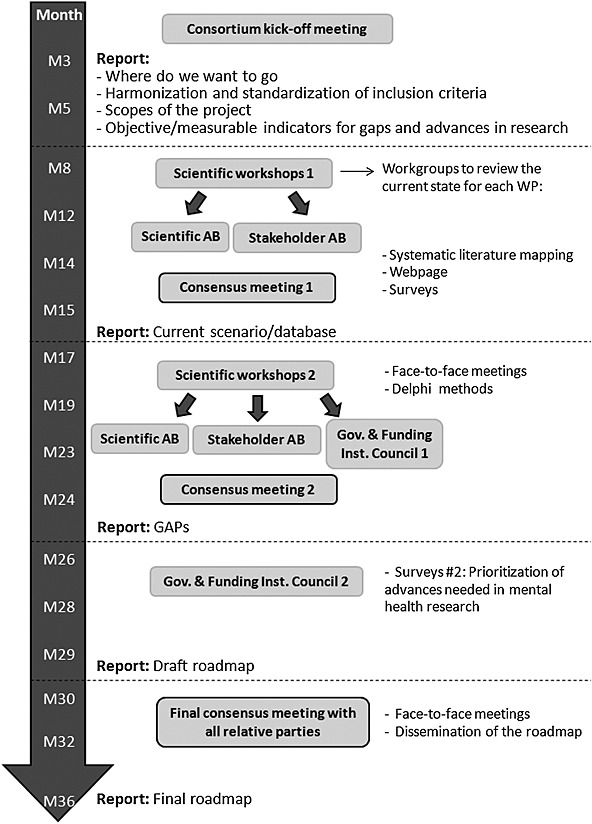
General outline of the project.
Discussion
Current gaps
Classification systems and biomedical research
Current diagnostic systems for mental disorders, such as the International Classification of Diseases, 10th revision (ICD‐10) and the Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV/DSM‐5), have facilitated great advances, both in clinical and public health terms. They have allowed the determination and comparison of the frequency and impact of mental disorders across countries, as well as the development of pharmacological and psychosocial treatments for specific conditions, and, importantly, facilitated the full consideration of mental disorders among somatic conditions. Moreover, they were also critical in the improvement of the detection of mental disorders by health care services and in advances in treatment adequacy. However, current classification systems have important limitations that may need to be solved to achieve significant further advances in understanding the aetiology and course of mental disorders, and the development of improved diagnostic tools and treatment strategies. To highlight such diagnostic classificatory problems one can cite three interrelated areas: comorbidity, biomarkers, genetic and optimized pharmacologic and psychological treatment research.
Comorbidity describes the well‐known phenomenon, that most people with one somatic or mental disorder are likely to also have other disorders, either concurrently or consecutively (Kessler et al., 2011). Comorbidity is associated with increased health service use, lower response to pharmacological and psychosocial interventions, and an overall worse prognosis (Buitelaar, 2012). The meaning and implications of comorbidity however remain unclear. Comorbidity can be explained based on a number of grounds. It could be simply an artefact of our current imperfect classification systems, it can mean that one disorder causes another disorder, or that one disorder is a risk factor for another or originate from disorders representing different stages or developments of an underlying condition or liability factor (Krueger and Markon, 2006). For example, prospective studies have located first onset of anxiety disorders typically in early childhood and adolescence (Beesdo et al., 2009), and found that a substantial proportion of individuals with early and primary anxiety disorders later on develop secondary affective, substance and also somatic disorders (Goodwin et al., 2002; Zimmermann et al., 2003; Sareen et al., 2005; Mathew et al., 2011). However, the research evidence for this finding and alternative models is limited and the knowledge about the meaning and implications in terms of diagnostic and treatment decisions, as well as the pathogenic mechanism behind such patterns remain unclear (Fava et al., 2014).
Further and similar research needs are evident with regard to the high rates of comorbidity between mental disorders and somatic disorders, such as depression and diabetes or cardiovascular disease (CVD). This pattern is associated with higher mortality (Fleischhacker et al., 2008), lower rates of access to mental health care, poorer response to treatment, and diagnostic difficulties such as the interpretation of symptoms such as fatigue, sleeping problems, loss of appetite, etc., that might be attributable to the somatic condition and/or the mental disorder (Van der Feltz‐Cornelis et al., 2010). Comorbidity is also associated with increased costs of care for managing somatic health problems and their complications (Molosankwe et al., 2012; Naylor et al., 2012). All these issues present further challenges to classification systems, but might also have significant implications for improved research into aetiological mechanisms (like shared or overlapping pathogenic mechanisms), the development of adequate treatment models, and, consequently, appropriate organization of health care services.
Imperfect diagnostic classificatory systems might also be co‐responsible for the recent failure to develop more potent and effective psychopharmacological treatments and powerful biomarkers. After the tremendous progress that has been made in pharmacotherapy of mental disorders in the 1980s and 1990s, there has recently been a marked decline in the development of new effective and well tolerated medications. Because many drug candidates fail to make the translational hurdle to clinical application, there have been claims that this might be due to imperfect diagnostic conventions. Similarly, a vast amount of resources has been devoted during the last decade to finding biomarkers that could serve diagnostic markers more reliably and validly than our current problematic behavioural or subjective psychopathological markers. Genetic research has identified hundreds of genetic variations and novel genes associated with major mental disorders, including schizophrenia (Craddock et al., 2009), depression (Shyn and Hamilton, 2010), autism (The Autism Genome Project Consortium, 2007) and addiction (Wong and Schumann, 2008). Moreover, several biochemical findings have been reported to be related to either the presence or severity of schizophrenia, depression and bipolar disorder. However, frequently these findings have not been replicated in similar studies (Kapur et al., 2012), and even when replicated they have been shown to be unspecific for a number of disorders. Similar problems are observed in studies on the familiar aggregation, when examining concordance in parent/offspring presence of mental disorders. These studies have focused on the concordance for specific mental disorders (Kendler et al., 1994; McGuffin et al., 1995; Hirshfeld‐Becker et al., 2012). However, we now know that some of these findings are unspecific and that parental mental disorders confer increased risk not only of concordant disorders but also for apparently unrelated mental disorders among offspring (Dean et al., 2010; McLaughlin et al., 2012).
The limitations of our current classification systems and the lack of success in detecting biomarkers have important implications for the delivery of the most appropriate care to people with mental disorders. Despite the advancements in some areas of medicine, personalized medicine (Langreth and Waldholz, 1999) is not progressing in psychiatry. “Stratified medicine”, the identification of biomarkers or cognitive tests that stratify a broad‐illness phenotype into a finite number of treatment‐relevant subgroups has been proposed as an alternative to personalized medicine in psychiatry. However, it is hard to envisage large‐scale application of these proposals until the earlier mentioned problems with classification systems are resolved (Kapur et al., 2012). For further discussions on biomedical issues relevant for mental health research, see Schumann et al. (2013).
Psychological research and treatments
Many of the problems listed earlier for biomedical research also apply to psychological interventions (see Wittchen et al., 2014). The effectiveness of various types of empirically supported psychological treatments and interventions such as cognitive behavioural therapy (CBT), interpersonal therapy (IPT), as well as Problem Solving Treatment (PST), Behavioural Analysis System of Psychotherapy (CBASP) and Mindfulness based cognitive therapy is well established in hundreds of randomized clinical trials and numerous reviews, particularly in areas like anxiety, depressive, somatoform, and eating disorders, where such methods are typically regarded as first‐line treatments (Arch and Craske, 2009; Jakobsen et al., 2011; Fjorback et al., 2011). Psychological therapies are also established as core elements in the treatment of substance use and most neurodevelopmental disorders and conditions [e.g. attention deficit hyperactivity disorder (ADHD); Rader et al., 2009]. For the group of classic psychodynamic and psychoanalytic methods similar strong evidence is generally lacking. Just recently, critical and empirically sound evaluation has been performed, providing evidence that these treatments are superior to non‐treatment conditions, but not exceeding the effect sizes and related methodological quality of studies on the effectiveness of CBT (Driessen et al., 2010; de Maat et al., 2009; Smit et al., 2012; Town et al., 2011; Leichsenring and Rabung, 2011; Gerber et al., 2011).
However, there is still a general lack of understanding why these treatments are effective, as well as more generally about the basic mechanisms of behaviour (in terms of initiation, maintenance and change). The critical trajectories and determinants from functional and adaptive‐normal to dysfunctional abnormal states and conditions, as well as the moderators and mediators of treatment‐related interventions remain under‐researched and unclear. Actually, although highly effective and despite some progress in clinical psychological research, little is known about the active ingredients and related mechanisms of action of evidence based psychotherapies. Further, we still do not know whether mechanisms governing these aspects of behaviour change are the same or different across groups of mental disorders, and whether individual genetic variation or different individual capacities (such as “self‐regulation”) could play a role.
Finally, there is a fundamental lack of knowledge on the state of research for psychological treatments and interventions in Europe in terms of personnel and financial research capacity, infrastructures, translation into clinical practice as well as dissemination and evaluation of outcomes on the individual and societal level. In fact, there is even a general lack of information about the degree to which psychological treatments are applied in EU countries, where and what kinds of research and service delivery programmes are in place, and how they are integrated into the wider network of mental health care infrastructure. As a result of this situation, Europe lacks even the most basic prerequisites for an evidence‐based clinical research policy for psychological treatments and interventions.
Social and economic impacts of well‐being and mental disorders
It is clear from our current understanding that the social and economic consequences of poor mental health across the life course can be profound. Many of these impacts fall outside health care systems. Participation rates in employment for people with mental health needs are much lower than for the general population, and much lower than for people with severe physical health problems (Levinson et al., 2010). Moreover, poor mental health in childhood can have consequences through the life‐course, with reduced rates of participation in higher education, lower rates of employment and lower levels of income for those who are employed, and increased risk of contact with criminal justice systems (Scott et al., 2001, Colman et al., 2009). In contrast, positive well‐being in childhood may have long‐term social and economic benefits in adulthood (Richards and Huppert, 2011).
While methods have been developed to help quantify the costs of poor mental health, many of the associated economic consequences of poor mental health remain unclear. For instance, remarkably little research has been undertaken in Europe to quantify the economic impacts of comorbid mental and somatic health problems, even though a number of studies looking at these issues in other parts of the world have been published (Molosankwe et al., 2012). Moreover, little is known about the economic benefits of better mental well‐being.
While some studies have looked at the economic benefits of actions to protect and promote mental health, particularly with regard to actions targeted at children and adolescents (Knapp et al., 2011; Mihalopoulos et al., 2011; McDaid and Park, 2011), major gaps remain in our knowledge. For instance, although the impact of work‐related stress and poor mental health on performance at work and rates of absenteeism have been described, studies looking at the effectiveness and economic benefits of actions both to prevent mental health problems in work and to help individuals return to work more quickly when they occur remain limited (McDaid and Park, 2011; Nieuwenhuijsen et al., 2008). In terms of treatment and support within the health care system, cost‐effectiveness studies have focused on pharmacotherapies with much less attention given to comparison with psychological and other interventions. New modes for interventions, such as the use of the Internet and home‐based interventions also merit much more careful economic analysis (Smit et al., 2011).
Another fundamental societal challenge related to mental illness is the social exclusion experienced by people with mental health problems. One key driver of social exclusion is public stigma (Evans‐Lacko et al., 2012), which is derived from (i) problems of knowledge (ignorance or misinformation); (ii) problems of attitudes (prejudice); and (iii) problems of behaviour (discrimination). Evidence in support of national anti‐stigma interventions is emerging in Europe (Smit et al., 2011); however, the impact and costs of social exclusion are under‐researched, as are the mechanisms for reducing stigma and misinformation, which is the primary cause of discrimination. Moreover, given the importance of employment as a key element in the recovery process for the majority of people with mental health problems, careful analyses not only of interventions to job activation and integration in work, but also of the role played by social welfare and legal systems in providing incentives and safeguards to encourage inclusion in work are also required. Too little is known about these mechanisms and any necessary viable solutions that are fair to all Europeans.
Public health and health services research
Public mental health aims at promoting health and preventing ill‐health at a population level through policies and large‐scale interventions. Public health clearly benefits from multinational research. Policies, health systems and population level mental health promotion and prevention interventions show great diversity across European countries with very little knowledge on how different structures and practices impact on the mental health of European citizens. Decisions are mostly based on political or social forces, and evidence is lacking to back many of them. Public mental health actions need to be better underpinned by valid research on the distribution of mental health and the magnitude of mental disorders in the population, as well as research on effective interventions to promote mental health, prevent mental health problems and improve mental health service provision. Therefore, there is a great need for a coordinated research action plan to gather the information required to establish an evidence base for national mental health policies and an EU mental health strategy, and to disseminate findings across the scientific community, to policy and funding institutions as well as to service users, carers, and professionals. This includes the comprehensive assessment of the quality of mental health care services, in general health care services such as primary and general hospital care as well as specialist mental health care, and identifying regional and cultural differences in Europe, based on valid and comparable mental health services data (Höschl, 2009; Wahlbeck, 2011b). Key topics in mental health services research relate to service delivery, the mental health workforce, novel health technologies, as well as the relationship between users and professional carers, and issues around governance and accountability. Development of evidence‐based initiatives to promote mental health and to prevent mental health problems is a key aim of public health research. On the policy level, research is needed to systematically evaluate population‐level natural experiments, such as shifts in mental health policies or in policies regarding determinants of mental health.
While translational research has been developed to some extent between basic science and clinical research, the link between basic and public health researchers is even weaker. Besides genetic epidemiology, there is still a long way to go to take advantage of the collaboration of basic, clinical and public health researchers. Long‐term international cohort studies are needed to establish the determinants of mental health and mental disorders. In this sense, the goal of the ROAMER project is to build bridges so that real translational research can be promoted. As an example, we may need to develop alternative databases to the current psychiatric diagnostic systems, which strongly encourage use of novel and alternative approaches to phenotypes of mental health.
Mental health services need to change their relationship with patients. Research to develop novel incentives for patient‐centred services and to define appropriate performance indicators is crucial to support the development of purchaser–provider models for mental health. The expert patient role, patient empowerment, as in shared decision‐making, and service evaluation needs to be better researched by mixed methods and service user‐led research approaches.
Opportunities created by better research use of routinely collected health care data and access to novel types of data from electronic patient records such as routine outcome monitoring and patient centred outcome research will be acknowledged in the roadmap, and the inclusion of service users in initiation, design, implementation and evaluation of mental health services research will be a core issue.
Well‐being
Well‐being is an emergent social and political priority in Europe. Well‐being reflects individuals' perception and evaluation of their own lives in terms of their affective states, psychological and social functioning (Keyes and Lopez, 2002). There are different components of well‐being. Experienced well‐being can be measured with instruments such as the Experience Sampling Method (Csikszentmihalyi and Larson, 1987) and the Day Reconstruction Method (Kahneman et al., 2004). Evaluative well‐being captures judgments of overall life satisfaction or fulfilment on distinct domains of personal functioning, such as autonomy, personal growth and achievement of life purposes. Current research across Europe into these two approaches offers different perspectives. Preliminary work suggests that different aspects of well‐being may have distinct physiological correlates. Measures of subjective well‐being also correlate highly with personality measures, such as neuroticism and extraversion, suggesting that well‐being may be a stable trait. However, longitudinal studies indicate only moderate stability of life satisfaction over time, suggesting that there are potentially modifiable environmental factors that may have an impact on subjective well‐being.
From a health perspective, the concept and measurement of well‐being goes beyond the mere presence or absence of illness or disability. Well‐being also incorporates the impact of positive health and functioning that has typically received little attention in health sciences. From both a policy and a health perspective, well‐being at any stage in life is an important outcome in and of itself. However, despite the fact that measures of well‐being could provide an important source of information for comparative effectiveness analyses of behavioural and biomedical interventions, they are currently not included in many intervention trials, probably also because of the many and sometimes diverging facets associated with the term and concept of well‐being.
Aspects of subjective well‐being have been associated with changes in life expectancy, as well as disease risk, mortality and disability. However the evidence definitively linking well‐being to specific health and economic outcomes at the population level is limited. In contrast to our knowledge about trends in, e.g. physical disability during old age, we know little about population and cohort trends in well‐being over time. At the individual level, there is a growing body of evidence for a distinct role of positive affect and life evaluations in predicting important health outcomes. Several lines of research suggest that positive psychological states, including both experienced positive emotions and evaluative components of well‐being, may play important roles in motivating behaviour change, in buffering against suffering associated with illness and its symptoms and in speeding recovery or preventing disease, whereas negative states may have the opposite effects. However, much of this work has been informed by global assessments of positive or negative affect averaged over time, apart from measures of time use or context.
Research infrastructure, training and funding
Besides the themes addressed earlier, three transversal elements are necessary to promote and advance mental health research in Europe: research infrastructures, training and funding.
When compared to other fields of health research, it is acknowledged that there is a lack of research units and transversal infrastructures (shared databases, cohorts, technical platforms, etc.) that can be either specific to mental health or generic but useable for mental health research (Thornicroft et al., 2002; Ayuso‐Mateos et al., 2011). Furthermore, existing entities and infrastructures suffer from a lack of visibility so that many researchers are not aware of their presence. Therefore, research activity in mental health could be greatly enhanced by better knowledge, both on the existence of and access to transversal infrastructures, as well as more awareness of related research units that could constellate to form research networks. This raises the question of the need for a body in charge of steering such communication and coordinating activities and, furthermore, performing knowledge brokering and thus bridging the current gap between research and decision‐making.
In terms of research training, there is a lack of dedicated programmes across Europe. This reflects insufficient investment in this area. A large share of existing programmes are offered in the UK which is, besides financial and social reasons, one of the factors in part explaining the “brain drain”, i.e. the migration of researchers from “Eastern” to “Western” Europe.
Finally sustainable and sufficient funding of mental health research is important, although as noted earlier, this is by far not the only factor required for progress. Most importantly, funders need to realize that there is a relative under‐funding of mental health research in many countries relative to the potentially avoidable health and economic burden of mental disorders (Chevreul et al., 2012), while resources allocated to this area have been previously estimated to yield a high return on investment (Health Economics Research Group et al., 2008).
Conclusions
In Europe, research in mental health and mental disorders is currently at a critical stage. Significant advances in knowledge have not been achieved during the last decade. For example, few new treatments have appeared and the search for biological markers has provided inconsistent results despite substantial efforts. Insufficient and uncoordinated communication between disciplines often results in a fragmented approach to mental health research, with a risk of dilution of its components in broader disciplines such as psychology, neuroscience, genetics, and public health. As a result, the development of coordinated research policies and integrated research networks in mental health is lagging behind other disciplines, resulting in a lower degree of cooperation between and within disciplines, and in a lower impact of its scientific output. Given the impact of mental disorders in society, the relatively low level of funding in research and the lack of a consistent European policy, a roadmap for mental health research is absolutely necessary. Against a background of limited resources for research, one key issue will be how to prioritize areas of research. Should this be done on the basis of burden of disease, on whether there are areas of “low hanging fruit” which might deliver early gains, on the priorities of sufferers and carers, or other criteria? Most likely, priorities will be based on a combination of factors. It is important to acknowledge too that Europe has special strengths which can play to in research: case registers and socialized healthcare systems enable epidemiological, genetic, economic and outcomes research; global telecommunication industries and a web‐literate population will support research into new models of remote and e‐health care; and a history of patient and carer involvement which encourages participatory research.
Declaration of interest statement
Dr Haro has been a consultant or made educational presentations for Eli Lilly & Company and Lundbeck, and has served on advisory boards for Eli Lilly & Company, Lundbeck, AstraZeneca and Hoffman‐LaRoche, Inc. Professor Meyer‐Lindenberg has been a consultant to or has received honoraria or grants from Abbott GmbH & Co. KG, Alexza Pharmaceuticals Inc., Astra Zeneca, Astra Zeneca GmbH, BASF SE, Bristol‐Myers Squibb GmbH & Co.KGaA, Defined Health, Desitin Arzneimittel GmbH, Elsevier, F. Hoffmann‐La Roche Ltd, Gerson Lehrmann Group (GLG), Groupo Ferrer Int., H. Lundbeck A/S, Janssen‐Cilag GmbH, Lilly Deutschland GmbH, Outcome Europe Sárl, Outcome Sciences Inc., Pfizer Pharma GmbH, Pricespective, Roche Pharma GmbH, Servier Deutschland GmbH. Professor van der Feltz‐Cornelis has received unrestricted grants for investigator initiated research and unrestricted grants for lectures from Eli Lilly. Professor van Os has received unrestricted investigator‐led research grants or recompense for presenting his research from Eli Lilly, Bristol‐Myers Squibb, Lundbeck, Organon, Janssen‐Cilag, GlaxoSmithKline, AstraZeneca, Pfizer and Servier, companies that have an interest in the treatment of psychosis. Dr Arango has been a consultant to or has received honoraria or grants from Abbot, AMGEN, AstraZeneca, Bristol‐Myers Squibb, Caja Navarra, CIBERSAM, Fundación Alicia Koplowitz, Instituto de Salud Carlos III, Janssen Cilag, Lundbeck, Merck, Ministerio de Ciencia e Innovación, Ministerio de Sanidad, Ministerio de Economía y Competitividad, Mutua Madrileña, Otsuka, Pfizer, Roche, Servier, Shire, Takeda and Schering Plough. Dr Evans‐Lacko has received consulting fees from Lundbeck. The other authors have not declared any conflicts of interest.
Acknowledgements
The ROAMER project has received funding from the European Union Seventh Framework Programme (FP7/2007‐2013) under grant agreement no. 282586, and from the National R&D Internationalization Programme of the Spanish Ministry of Science and Technology under reference ACI‐PRO‐2011‐1080.
References
- Arch J.J., Craske M.G. (2009) First‐line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatric Clinics of North America, 32(3), 525–547. DOI: 10.1016/j.psc.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Ayuso‐Mateos J.L., Wykes T., Arango C. (2011) The Madrid Declaration: why we need a coordinated Europe‐wide effort in mental health research. British Journal of Psychiatry, 198(4), 253–255. DOI: 10.1192/bjp.bp.110.082511 [DOI] [PubMed] [Google Scholar]
- Beesdo K., Knappe S., Pine D.S. (2009) Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM‐V. Psychiatric Clinics of North America, 32(3), 483–524, DOI: 10.1016/j.psc.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brohan E., Gauci D., Sartorius N., Thornicroft G., GAMIAN‐Europe Study Group (2011) Self‐stigma, empowerment and perceived discrimination among people with bipolar disorder or depression in 13 European countries: the GAMIAN–Europe study. Journal of Affective Disorders, 129(1–3), 56–63, DOI: 10.1016/j.jad.2010.09.001 [DOI] [PubMed] [Google Scholar]
- Buitelaar J.K. (2012) Understanding comorbidity: from epidemiological designs and model‐fitting approaches to systems biology as a new tool. European Child & Adolescent Psychiatry, 21(1), 1–3, DOI: 10.1007/s00787-011-0236-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalá López F., Alvarez Martín E., Gènova Maleras R., Morant Ginestar C. (2009) Relación en España entre la investigación sanitaria financiada por el sistema nacional de salud y la carga de enfermedad en la comunidad. Revista Española de Salud Pública, 83(1), 137–151. [DOI] [PubMed] [Google Scholar]
- Chevreul K., McDaid D., Farmer C.M., Prigent A., Park A.L., Leboyer M., Kupfer D.J., Durand‐Zaleski I. (2012) Public and non‐profit funding for research on mental disorders in the United Kingdom, France, and the United States of America. Journal of Clinical Psychiatry, 73(7), e906–e912, DOI: 10.4088/JCP.11r07418 [DOI] [PubMed] [Google Scholar]
- Colman I., Murray J., Abbott R.A., Maughan B., Kuh D., Croudace T.J., Jones P.B. (2009) Outcomes of conduct problems in adolescence: 40 year follow‐up of national cohort. British Medical Journal, 338, a2981, DOI: 10.1136/bmj.a2981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- COM (2008) 468 final. Towards Joint Programming in Research: Working together to tackle common challenges more effectively, Box 1, p. 5. http://ec.europa.eu/research/press/2008/pdf/com_2008_468_en.pdf [accessed 15 January 2013].
- Craddock N., O'Donovan M.C., Owen M.J. (2009) Psychosis genetics: modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophrenia Bulletin, 35(3), 482–490, DOI: 10.1093/schbul/sbp020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csikszentmihalyi M., Larson R. (1987) Validity and reliability of the experience‐sampling method. Journal of Nervous and Mental Disease, 175(9), 526–536. [DOI] [PubMed] [Google Scholar]
- DE Hert M., Correll C.U., Bobes J., Cetkovich‐Bakmas M., Cohen D., Asai I., Detraux J., Gautam S., Möller H.J., Ndetei D.M., Newcomer J.W., Uwakwe R., Leucht S. (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry, 10(1), 52–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Maat S., de Jonghe F., Schoevers R., Dekker J. (2009) The effectiveness of long‐term psychoanalytic therapy: a systematic review of empirical studies. Harvard Review of Psychiatry, 17(1), 1–23, DOI: 10.1080/10673220902742476 [DOI] [PubMed] [Google Scholar]
- Dean K., Stevens H., Mortensen P.B., Murray R.M., Walsh E., Pedersen C.B. (2010) Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Archives of General Psychiatry, 67(8), 822–829, DOI: 10.1001/archgenpsychiatry.2010.86 [DOI] [PubMed] [Google Scholar]
- Driessen E., Cuijpers P., de Maat S.C., Abbass A.A., de Jonghe F., Dekker J.J. (2010) The efficacy of short‐term psychodynamic psychotherapy for depression: a meta‐analysis. Clinical Psychology Review, 30(1), 25–36, DOI: 10.1016/j.cpr.2009.08.010 [DOI] [PubMed] [Google Scholar]
- European Commission (EC) (2005) Green Paper – Improving the mental health of the population. Towards a strategy on mental health for the European Union. http://europa.eu/legislation_summaries/public_health/health_determinants_lifestyle/c11570c_en.htm [accessed 21 January 2012].
- European Commission (EC) and World Health Organization (WHO) Europe (2008) EU high‐level conference. Brussels, 12–13 June 2008. European Pact for Mental Health and Well‐being http://ec.europa.eu/health/mental_health/docs/mhpact_en.pdf [accessed 15 January 2013].
- Evans‐Lacko S., Brohan E., Mojtabai R., Thornicroft G. (2012) Association between public views of mental illness and self‐stigma among individuals with mental illness in 14 European countries. Psychological Medicine, 42(8), 1741–1752, DOI: 10.1017/S0033291711002558 [DOI] [PubMed] [Google Scholar]
- Fava G.A., Tossani E., Bech P., Berrocal C., Chouinard G., Csillag C., Wittchen H.‐U., Rief W. (2014) Emerging clinical trends and perspectives on comorbid patterns of mental disorders in research. International Journal of Methods in Psychiatric Research, 23(Suppl. 1), 92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Luciano M., Del Vecchio V., Sampogna G., Obradors‐Tarragó C., Maj M., on behalf of the ROAMER Consortium . (2013) Priorities for mental health research in Europe: a survey among national stakeholders' associations within the ROAMER project. World Psychiatry, 12(2), 165–70, DOI: 10.1002/wps.20052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjorback L.O., Arendt M., Ornbøl E., Fink P., Walach H. (2011) Mindfulness‐based stress reduction and mindfulness‐based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica, 124(2), 102–119, DOI: 10.1111/j.1600-0447.2011.01704.x [DOI] [PubMed] [Google Scholar]
- Fleischhacker W.W., Cetkovich‐Bakmas M., De Hert M., Hennekens C.H., Lambert M., Leucht S., Maj M., McIntyre R.S., Naber D., Newcomer J.W., Olfson M., Osby U., Sartorius N., Lieberman J.A. (2008) Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. Journal of Clinical Psychiatry, 69(4), 514–519. [DOI] [PubMed] [Google Scholar]
- Gerber A.J., Kocsis J.H., Milrod B.L., Roose S.P., Barber J.P., Thase M.E., Perkins P., Leon A.C. (2011) A quality‐based review of randomized controlled trials of psychodynamic psychotherapy. American Journal of Psychiatry, 168(1), 19–28, DOI: 10.1176/appi.ajp.2010.08060843 [DOI] [PubMed] [Google Scholar]
- Goodwin R.D., Stayner D.A., Chinman M.J., Wu P., Tebes J.K., Davidson L. (2002) The relationship between anxiety and substance use disorders among individuals with severe affective disorders. Comprehensive Psychiatry, 43(4), 245–252. [DOI] [PubMed] [Google Scholar]
- Health Economics Research Group , Office of Health Economics , RAND Europe . (2008) Medical Research: What's it Worth? Estimating the Economic Benefits from Medical Research in the UK, London, UK Evaluation Forum. [Google Scholar]
- Hirshfeld‐Becker D.R., Micco J.A., Henin A., Petty C., Faraone S.V., Mazursky H., Bruett L., Rosenbaum J.F., Biederman J. (2012) Psychopathology in adolescent offspring of parents with panic disorder, major depression, or both: a 10‐year follow‐up. American Journal of Psychiatry, 169(11), 1175–1184. [DOI] [PubMed] [Google Scholar]
- Höschl C. (2009) European psychiatry: needs, challenges and structures. European Archives of Psychiatry and Clinical Neurosciences, 259(Suppl 2), S119–S122, DOI: 10.1007/s00406-009-0050-0 [DOI] [PubMed] [Google Scholar]
- Jakobsen J.C., Hansen J.L., Storebø O.J., Simonsen E., Gluud C. (2011) The effects of cognitive therapy versus ‘no intervention’ for major depressive disorder. PLoS One, 6(12), e28299, DOI: 10.1371/journal.pone.0028299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D., Krueger A.B., Schkade D.A., Schwarz N., Stone A.A. (2004) A survey method for characterizing daily life experience: the day reconstruction method. Science, 306(5702), 1776–1780. [DOI] [PubMed] [Google Scholar]
- Kapur S., Phillips A.G., Insel T.R. (2012) Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Molecular Psychiatry, 17(12), 1174–1179, DOI: 10.1038/mp.2012.105 [DOI] [PubMed] [Google Scholar]
- Kendler K.S., Gruenberg A.M., Kinney D.K. (1994) Independent diagnoses of adoptees and relatives as defined by DSM‐III in the provincial and national samples of the Danish Adoption Study of Schizophrenia. Archives of General Psychiatry, 51(6), 456–468. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Petukhova M., Zaslavsky A.M. (2011) The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Current Opinions in Psychiatry, 24(4), 307–12, DOI: 10.1097/YCO.0b013e3283477b22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes C.L.M., Lopez S.J. (2002) Towards a science of mental health: positive directions in diagnosis and interventions In Snyder C.R., Lopez S.J. (eds) Handbook of Positive Psychology, pp. 45–59, New York, Oxford University Press. [Google Scholar]
- Knapp M., McDaid D., Parsonage M. (eds). (2011) Mental Health Promotion and Mental Illness Prevention: The Economic Case, London, Department of Health. [Google Scholar]
- Krueger R.F., Markon K.E. (2006) Reinterpreting comorbidity: a model‐based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langreth R., Waldholz M. (1999) New era of personalized medicine: targeting drugs for each unique genetic profile. The Oncologist, 4(5), 426–427. [PubMed] [Google Scholar]
- Lasalvia A., Zoppei S., Van Bortel T., Bonetto C., Cristofalo D., Wahlbeck K., Bacle S.V., Van Audenhove C., van Weeghel J., Reneses B., Germanavicius A., Economou M., Lanfredi M., Ando S., Sartorius N., Lopez‐Ibor J.J., Thornicroft G., ASPEN/INDIGO Study Group (2013) Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross‐sectional survey. Lancet, 381(9860), 55–62, DOI: 10.1016/S0140-6736(12)61379-8 [DOI] [PubMed] [Google Scholar]
- Laursen T.M., Munk‐Olsen T., Gasse C. (2011) Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One, 6(9), e24597, DOI: 10.1371/journal.pone.0024597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichsenring F., Rabung S. (2011) Long‐term psychodynamic psychotherapy in complex mental disorders: update of a meta‐analysis. British Journal of Psychiatry, 199(1), 15–22, DOI: 10.1192/bjp.bp.110.082776 [DOI] [PubMed] [Google Scholar]
- Levinson D., Lakoma M.D., Petukhova M., Schoenbaum M., Zaslavsky A.M., Angermeyer M., Borges G., Bruffaerts R., de Girolamo G., de Graaf R., Gureje O., Haro J.M., Hu C., Karam A.N., Kawakami N., Lee S., Lepine J.P., Browne M.O., Okoliyski M., Posada‐Villa J., Sagar R., Viana M.C., Williams D.R., Kessler R.C. (2010) Associations of serious mental illness with earnings: results from the WHO World Mental Health surveys. British Journal of Psychiatry, 197(2), 114–121, DOI: 10.1192/bjp.bp.109.073635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew A.R., Pettit J.W., Lewinsohn P.M., Seeley J.R., Roberts R.E. (2011) Co‐morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychological Medicine, 41(10), 2023–2034, DOI: 10.1017/S0033291711000407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaid D., Knapp M., Medeiros H., and the MHEEN Group (2008) Employment and Mental Health: Assessing the Economic Impact and the Case for Intervention, London, London School of Economics and Political Science. [Google Scholar]
- McDaid D., Park A.L. (2011) Investing in mental health and well‐being: findings from the DataPrev project. Health Promotion International, 26(Suppl. 1), i108–i139, DOI: 10.1093/heapro/dar059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuffin P., Owen M.J., Farmer A.E. (1995) Genetic basis of schizophrenia. Lancet, 346(8976), 678–682. [DOI] [PubMed] [Google Scholar]
- McLaughlin K.A., Gadermann A.M., Hwang I., Sampson N.A., Al‐Hamzawi A., Andrade L.H., Angermeyer M.C., Benjet C., Bromet E.J., Bruffaerts R., Caldas‐de‐Almeida J.M., de Girolamo G., de Graaf R., Florescu S., Gureje O., Haro J.M., Hinkov H.R., Horiguchi I., Hu C., Karam A.N., Kovess‐Masfety V., Lee S., Murphy S.D., Nizamie S.H., Posada‐Villa J., Williams D.R., Kessler R.C. (2012) Parent psychopathology and offspring mental disorders: results from the WHO World Mental Health Surveys. British Journal of Psychiatry, 200(4), 290–299, DOI: 10.1192/bjp.bp.111.101253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental Health Europe (MHE) (2007) MHE Position on the EC/BEPA consultation paper on Europe's Social Reality. An Analysis from the Mental Health Perspective Based on Consultation with Mental Health Organisations in Europe http://www.mhe-sme.org/assets/files/publications/MHE-response-to-europe's-social-reality-stocktaking-exerci.pdf [accessed 15 January 2013].
- Mihalopoulos C., Vos T., Pirkis J., Smit F., Carter R. (2011) Do indicated preventive interventions for depression represent good value for money? Australia and New Zealand Journal of Psychiatry, 45(1), 36–44, DOI: 10.3109/00048674.2010.501024 [DOI] [PubMed] [Google Scholar]
- Molosankwe I., Patel A., José Gagliardino J., Knapp M., McDaid D. (2012) Economic aspects of the association between diabetes and depression: a systematic review. Journal of Affective Disorders, 142(S), s42–s55, DOI: 10.1016/S0165-0327(12)70008-3 [DOI] [PubMed] [Google Scholar]
- Murray C.J., Vos T., Lozano R., Naghavi M., Flaxman A.D., Michaud C., Ezzati M., Shibuya K., Salomon J.A., Abdalla S., Aboyans V., Abraham J., Ackerman I., Aggarwal R., Ahn S.Y., Ali M.K., Alvarado M., Anderson H.R., Anderson L.M., Andrews K.G., Atkinson C., Baddour L.M., Bahalim A.N., Barker‐Collo S., Barrero L.H., Bartels D.H., Basáñez M.G., Baxter A., Bell M.L., Benjamin E.J., Bennett D., Bernabé E., Bhalla K., Bhandari B., Bikbov B., Bin Abdulhak A., Birbeck G., Black J.A., Blencowe H., Blore J.D., Blyth F., Bolliger I., Bonaventure A., Boufous S., Bourne R., Boussinesq M., Braithwaite T., Brayne C., Bridgett L., Brooker S., Brooks P., Brugha T.S., Bryan‐Hancock C., Bucello C., Buchbinder R., Buckle G., Budke C.M., Burch M., Burney P., Burstein R., Calabria B., Campbell B., Canter C.E., Carabin H., Carapetis J., Carmona L., Cella C., Charlson F., Chen H., Cheng A.T., Chou D., Chugh S.S., Coffeng L.E., Colan S.D., Colquhoun S., Colson K.E., Condon J., Connor M.D., Cooper L.T., Corriere M., Cortinovis M., de Vaccaro K.C., Couser W., Cowie B.C., Criqui M.H., Cross M., Dabhadkar K.C., Dahiya M., Dahodwala N., Damsere‐Derry J., Danaei G., Davis A., De Leo D., Degenhardt L., Dellavalle R., Delossantos A., Denenberg J., Derrett S., Des Jarlais D.C., Dharmaratne S.D., Dherani M., Diaz‐Torne C., Dolk H., Dorsey E.R., Driscoll T., Duber H., Ebel B., Edmond K., Elbaz A., Ali S.E., Erskine H., Erwin P.J., Espindola P., Ewoigbokhan S.E., Farzadfar F., Feigin V., Felson D.T., Ferrari A., Ferri C.P., Fèvre E.M., Finucane M.M., Flaxman S., Flood L., Foreman K., Forouzanfar M.H., Fowkes F.G., Fransen M., Freeman M.K., Gabbe B.J., Gabriel S.E., Gakidou E., Ganatra H.A., Garcia B., Gaspari F., Gillum R.F., Gmel G., Gonzalez‐Medina D., Gosselin R., Grainger R., Grant B., Groeger J., Guillemin F., Gunnell D., Gupta R., Haagsma J., Hagan H., Halasa Y.A., Hall W., Haring D., Haro J.M., Harrison J.E., Havmoeller R., Hay R.J., Higashi H., Hill C., Hoen B., Hoffman H., Hotez P.J., Hoy D., Huang J.J., Ibeanusi S.E., Jacobsen K.H., James S.L., Jarvis D., Jasrasaria R., Jayaraman S., Johns N., Jonas J.B., Karthikeyan G., Kassebaum N., Kawakami N., Keren A., Khoo J.P., King C.H., Knowlton L.M., Kobusingye O., Koranteng A., Krishnamurthi R., Laden F., Lalloo R., Laslett L.L., Lathlean T., Leasher J.L., Lee Y.Y., Leigh J., Levinson D., Lim S.S., Limb E., Lin J.K., Lipnick M., Lipshultz S.E., Liu W., Loane M., Ohno S.L., Lyons R., Mabweijano J., MacIntyre M.F., Malekzadeh R., Mallinger L., Manivannan S., Marcenes W., March L., Margolis D.J., Marks G.B., Marks R., Matsumori A., Matzopoulos R., Mayosi B.M., McAnulty J.H., McDermott M.M., McGill N., McGrath J., Medina‐Mora M.E., Meltzer M., Mensah G.A., Merriman T.R., Meyer A.C., Miglioli V., Miller M., Miller T.R., Mitchell P.B., Mock C., Mocumbi A.O., Moffitt T.E., Mokdad A.A., Monasta L., Montico M., Moradi‐Lakeh M., Moran A., Morawska L., Mori R., Murdoch M.E., Mwaniki M.K., Naidoo K., Nair M.N., Naldi L., Narayan K.M., Nelson P.K., Nelson R.G., Nevitt M.C., Newton C.R., Nolte S., Norman P., Norman R., O'Donnell M., O'Hanlon S., Olives C., Omer S.B., Ortblad K., Osborne R., Ozgediz D., Page A., Pahari B., Pandian J.D., Rivero A.P., Patten S.B., Pearce N., Padilla R.P., Perez‐Ruiz F., Perico N., Pesudovs K., Phillips D., Phillips M.R., Pierce K., Pion S., Polanczyk G.V., Polinder S., Pope C.A. 3rd, Popova S., Porrini E., Pourmalek F., Prince M., Pullan R.L., Ramaiah K.D., Ranganathan D., Razavi H., Regan M., Rehm J.T., Rein D.B., Remuzzi G., Richardson K., Rivara F.P., Roberts T., Robinson C., De Leòn F.R., Ronfani L., Room R., Rosenfeld L.C., Rushton L., Sacco R.L., Saha S., Sampson U., Sanchez‐Riera L., Sanman E., Schwebel D.C., Scott J.G., Segui‐Gomez M., Shahraz S., Shepard D.S., Shin H., Shivakoti R., Singh D., Singh G.M., Singh J.A., Singleton J., Sleet D.A., Sliwa K., Smith E., Smith J.L., Stapelberg N.J., Steer A., Steiner T., Stolk W.A., Stovner L.J., Sudfeld C., Syed S., Tamburlini G., Tavakkoli M., Taylor H.R., Taylor J.A., Taylor W.J., Thomas B., Thomson W.M., Thurston G.D., Tleyjeh I.M., Tonelli M., Towbin J.A., Truelsen T., Tsilimbaris M.K., Ubeda C., Undurraga E.A., van der Werf M.J., van Os J., Vavilala M.S., Venketasubramanian N., Wang M., Wang W., Watt K., Weatherall D.J., Weinstock M.A., Weintraub R., Weisskopf M.G., Weissman M.M., White R.A., Whiteford H., Wiebe N., Wiersma S.T., Wilkinson J.D., Williams H.C., Williams S.R., Witt E., Wolfe F., Woolf A.D., Wulf S., Yeh P.H., Zaidi A.K., Zheng Z.J., Zonies D., Lopez A.D., AlMazroa M.A., Memish Z.A. (2012) Disability‐adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380(9859), 2197–2223. [DOI] [PubMed] [Google Scholar]
- Naylor C., Parsonage M., McDaid D., Knapp M., Fossey M., Galea A. (2012) Long‐term Conditions and Mental Health: The Cost of Co‐morbidities, London, The King's Fund. [Google Scholar]
- Nieuwenhuijsen K., Bültmann U., Neumeyer‐Gromen A., Verhoeven A.C., Verbeek J.H., van der Feltz‐Cornelis C.M. (2008) Interventions to improve occupational health in depressed people. Cochrane Database of Systematic Reviews, (2), CD006237, DOI: 10.1002/14651858.CD006237.pub2 [DOI] [PubMed] [Google Scholar]
- Nutt D., Goodwin G. (2011) ECNP Summit on the future of CNS drug research in Europe 2011: report prepared for ECNP by David Nutt and Guy Goodwin. European Neuropsychopharmacology, 21(7), 495–499, DOI: 10.1016/j.euroneuro.2011.05.004 [DOI] [PubMed] [Google Scholar]
- Rader R., McCauley L., Callen E.C. (2009) Current strategies in the diagnosis and treatment of childhood attention‐deficit/hyperactivity disorder. American Family Physician, 79(8), 657–665. [PubMed] [Google Scholar]
- Richards M., Huppert F.A. (2011) Do positive children become positive adults? Evidence from a longitudinal birth cohort study. The Journal of Positive Psychology, 6(1), 75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J., Cox B.J., Clara I., Asmundson G.J. (2005) The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depression and Anxiety, 21(4), 193–202. [DOI] [PubMed] [Google Scholar]
- Schumann G., Binder E.B., Holte A., de Kloet E.R., Oedegaard K.J., Robbins T.W., Walker‐Tilley T.R., Brown V.J., Buitelaar J., Ciccocioppo R., Cools R., Escera C., Fleischhacker W., Flor H., Frith C.D., Heinz A., Johnsen E., Kirschbaum C., Klingberg T., Lesch K.P., Lewis S., Maier W., Mann K., Martinot J.L., Meyer‐Lindenberg A., Müller C.P., Müller W.E., Nutt D.J., Persico A., Perugi G., Pessiglione M., Preuss U.W., Roiser J., Rossini P.M., Rybakowski J.K., Sandi C., Stephan K.E., Undurraga J., Vieta E., van der Wee N., Wykes T., Haro J.M., Wittchen H.U. (2013) Stratified medicine for mental disorders. European Neuropsychopharmacology. DOI: 10.1016/j.euroneuro.2013.09.010 [DOI] [PubMed] [Google Scholar]
- Scott S., Knapp M., Henderson J., Maughan B. (2001) Financial cost of social exclusion: follow up study of antisocial children into adulthood. British Medical Journal, 323(7306), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shyn S.I., Hamilton S.P. (2010) The genetics of major depression: moving beyond the monoamine hypothesis. Psychiatric Clinics of North America, 33(1), 125–140, DOI: 10.1016/j.psc.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit F., Lokkerbol J., Riper H., Majo M.C., Boon B., Blankers M. (2011) Modeling the cost‐effectiveness of health care systems for alcohol use disorders: how implementation of eHealth interventions improves cost‐effectiveness. Journal of Medical Internet Research, 13(3), e56, DOI: 10.2196/jmir.1694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit Y., Huibers M.J., Ioannidis J.P., van Dyck R., van Tilburg W., Arntz A. (2012) The effectiveness of long‐term psychoanalytic psychotherapy – a meta‐analysis of randomized controlled trials. Clinical Psychology Review, 32(2), 81–92, DOI: 10.1016/j.cpr.2011.11.003 [DOI] [PubMed] [Google Scholar]
- The Autism Genome Project Consortium (2007) Mapping autism risk loci using genetic linkage and chromosomal rearrangements. Nature Genetics, 39(10), 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G., Bindman J., Goldberg D., Gournay K., Huxley P. (2002) Creating the infrastructure for mental health research. Psychiatric Bulletin, 26, 403–406, DOI: 10.1192/pb.26.11.403 [DOI] [Google Scholar]
- Thornicroft G., Brohan E., Rose D., Sartorius N., Leese M., INDIGO Study Group . (2009) Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross‐sectional survey. Lancet, 373(9661), 408–415, DOI: 10.1016/S0140-6736(08)61817-6 [DOI] [PubMed] [Google Scholar]
- Town J.M., Abbass A., Hardy G. (2011) Short‐term psychodynamic psychotherapy for personality disorders: a critical review of randomized controlled trials. Journal of Personality Disorders, 25(6), 723–740, DOI: 10.1521/pedi.2011.25.6.723 [DOI] [PubMed] [Google Scholar]
- Van der Feltz‐Cornelis C.M., Ten Have M., Penninx B.W., Beekman A.T., Smit J.H., De Graaf R. (2010) Presence of comorbid somatic disorders among patients referred to mental health care in the Netherlands. Psychiatric Services, 61(11), 1119–1125, DOI: 10.1176/appi.ps.61.11.1119 [DOI] [PubMed] [Google Scholar]
- Wahlbeck K. (2011a) European mental health policy should target everybody. European Journal of Public Health, 21(5), 551–553, DOI: 10.1093/eurpub/ckr122 [DOI] [PubMed] [Google Scholar]
- Wahlbeck K. (2011b) European comparisons between mental health services. Epidemiology and Psychiatric Sciences, 20(1), 15–18. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Jacobi F., Rehm J., Gustavsson A., Svensson M., Jönsson B., Olesen J., Allgulander C., Alonso J., Faravelli C., Fratiglioni L., Jennum P., Lieb R., Maercker A., van Os J., Preisig M., Salvador‐Carulla L., Simon R., Steinhausen H.C. (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21, 655–679, DOI: 10.1016/j.euroneuro.2011.07.018 [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Knappe S., Andersson G., Araya R., Banos Rivera R.M., Barkham M., Bech P., Beckers T., Berger T., Berking M., Berrocal C., Botella C., Carlbring P., Chouinard G., Colom F., Csillag C., Cujipers P., David D., Emmelkamp P.M.G., Essau C.A., Fava G.A., Goschke T., Hermans D., Hofmann S.G., Lutz W., Muris P., Ollendick T.H., Raes F., Rief W., Riper H., Tossani E., van der Oord S., Vervliet B., Haro J.M., Schumann G. (2014) The psychological perspective on mental health and mental disorder research: introduction to the ROAMER work package 5 consensus document. International Journal of Methods in Psychiatric Research, 23(Suppl. 1), 15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C.C., Schumann G. (2008) Genetics of addictions: strategies for addressing heterogeneity and polygenicity of substance use disorders. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 363(1507), 3213–3222, DOI: 10.1098/rstb.2008.0104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2005) Mental Health Atlas, Geneva, WHO. [Google Scholar]
- World Health Organization (WHO) . (2010) Global Status Report on Non‐communicable Diseases, Geneva, WHO. [Google Scholar]
- Zimmermann P., Wittchen H.U., Höfler M., Pfister H., Kessler R.C., Lieb R. (2003) Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4‐year community study of adolescents and young adults. Psychological Medicine, 33(7), 1211–1222. [DOI] [PubMed] [Google Scholar]


