Abstract
The Singapore Mental Health Study (SMHS) is a population‐based, cross‐sectional, epidemiological study on the Singapore multi‐ethnic adult population. This article provides an overview of the research design and methods used which took into consideration the unique characteristics of the country and its multi‐ethnic population. A face‐to‐face household survey of Singapore residents aged 18 years and above was undertaken from 2009 to 2010. The nationally representative probability sample was derived using a disproportionate stratified sampling method. In order to increase precision for subgroup estimations the design was stratified with over‐sampling of Malays, Indians and those aged 65 years and above. Respondents were assessed using the English, Chinese (computerized) and Malay (paper and pencil based) version of the Composite International Diagnostic Interview (CIDI) 3.0 to establish lifetime and 12‐month prevalence of mental disorders, the current use of mental health services (both Western and traditional services), the treatment gaps and loss of role functioning. Copyright © 2012 John Wiley & Sons, Ltd.
Keywords: Singapore, epidemiology, mental disorder, Composite International Diagnostic Interview, research design
Introduction
Mental illness is not only a growing public health concern but also a major social and economic issue affecting individuals and families throughout the world. The World Health Organization (WHO) reported that approximately 450 million individuals worldwide suffer from some form of neuropsychiatric disorders in their lifetime; community‐based epidemiological studies have estimated rates of lifetime prevalence of mental disorders among adults ranging from 12.2% to 48.6% and in a one‐year period, there are 8.4% to 29.1% who suffer from at least one form of mental disorder (WHO, 2001).
Singapore is a multi‐ethnic country in southeast Asia, with a resident population of 3.6 million (Statistics Singapore, 2009) of which 75.6% are Chinese, 13.6% are Malays and 8.7% are Indians. The per capita gross national product (GNP) is among the highest in the region, and the standard of living is comparable to that of developed countries. Changes in disease patterns that are consistent with those in more advanced societies, i.e. from infectious diseases and nutritional deficiencies to chronic diseases have also been observed in Singapore over this time period. However, in Singapore, we have yet to make a comprehensive and detailed study of the prevalence rates of mental illnesses, severity of mental disorders and the needs and unmet needs of those with mental illnesses. The studies to date have established the prevalence of a rather limited range of mental illnesses mainly the mood and anxiety disorders. One of the earliest studies, carried out in 1978 (by the Ministry of Health), revealed a prevalence of 8.4% of the population as suffering from “neurosis”. The Singapore Mental Health Survey measured psychoemotional symptoms in 3020 subjects aged between 13–65 years and estimated the population minor psychiatric morbidity (MPM) prevalence rate to be 16.6% (Fones et al., 1998). The National Mental Health Survey conducted in 2003 on adults aged 20–59 years living in the community, reported lifetime prevalence of depression to be 5.6% and that of anxiety disorders to be 3.4% (Chua et al., 2004).
Singapore initiated its first ever National Mental Health Blueprint and Policy in the year 2007 (Chong, 2007). The Blueprint proposes a population‐based public health model, which focuses on the epidemiologic surveillance of the health of this population, on health promotion, and access to and evaluation of community‐based services. The extensive and in‐depth study described here will establish the baseline data that will enable the subsequent evaluation of the impact of this Blueprint. It will also identify illnesses with high disease burden, help‐seeking patterns, and the unmet needs of those with mental disorders. Such information is vital in the scaling up of a country's mental health services to enable the rational allocation of resources.
The Singapore Mental Health Study (SMHS) aims to (i) conduct a population‐based survey to establish the prevalence of mental disorders in the adult Singapore resident population including the elderly; (ii) assess the spectrum and distribution of different types of mental illnesses across gender, ethnicities and age; (iii) develop and validate a culturally valid instrument for assessing positive mental health and subsequently establish the level of positive mental health in the Singapore population; (iv) describe the current use of mental health services (both Western and traditional services) and the level of unmet need; (v) identify facilitators and barriers to mental health treatment; (vi) evaluate the financial, social and personal costs associated with mental illness.
This paper sets out to describe the methodology of the survey, i.e. the instruments selected, sampling strategy, training and the quality assurance measures that were put in place to ensure scientific rigor in conducting the survey.
Methodology
Main instrument
After considering various instruments for the study, we decided to implement a battery of instruments, including the Composite International Diagnostic Interview (CIDI), and instruments measuring gambling, nicotine addiction, and chronic conditions. We decided to use the CIDI for a number of reasons: (i) it has been widely used across many countries, and therefore it allows us to perform cross‐country comparison analysis; (ii) a Chinese version is available; (iii) it can be administered by lay interviewers; (iv) it captures vital information on service use, pharmacology and social relationships.
WHO CIDI
The WHO developed the CIDI (Wittchen, 1994; WHO, 1990) based on extensive cross‐national field trials, for use in cross‐national epidemiological surveys (Bijl et al., 1998; Kessler et al., 1994; Vega et al., 1998; Wittchen et al., 1998). The WHO World Mental Health (WMH) Survey Initiative was created in 1998 which further improved the CIDI by including dimensional information along with the categorical information that existed in previous CIDI versions and the number of disorders were also expanded (Kessler and Ustun, 2004).
The CIDI 3.0 is a fully structured diagnostic instrument, which assesses lifetime and recent prevalence of disorders using the definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM‐IV) and the International Classification of Disease, 10th Revision (ICD‐10) Classification of Mental and Behavioral Disorders. One can choose to use the PAPI (paper and pencil interview) form or its computerized form [more commonly referred to as computer assisted personal interviewing (CAPI)]. Although the CAPI and PAPI instruments cover essentially the same information, one of the major differences between the two versions is the ability of the CAPI technique to better handle more elaborate procedural processes like skip patterns, complex randomization routines, and question fills. However, these differences do not affect the comparability of the resulting data between the two modes of instrumentation. For the SMHS, we used the computerized version of the English and Chinese CIDI 3.0 and the PAPI version of the translated CIDI in Bahasa Melayu. For each disorder, a screening section was administered to all respondents. All participants answering positively to a specific screening question were then referred to the respective diagnostic section of the questionnaire. Given the limitations imposed by time and the administrative burden on the respondent, we decided to use only selected modules from the CIDI. The modules were identified based on inputs from a Stakeholder Board. This Board comprising representatives from various stakeholders (Ministry of Health, voluntary organizations working with mentally ill clients, clinicians, sociologists, and representatives from the major ethnic groups in Singapore) advised the SMHS team on the modules that were considered locally relevant. The disorders were selected based on the main consideration of what would be of relevance to the country and its policy‐makers and service providers especially in the wake of the first ever National Mental Health Blueprint and Policy which was implemented in 2007. The eventual group of disorders chosen was in turn guided by a review of studies in the extant published literature, commissioned reports and white papers. Through these processes, we identified major depressive disorder (MDD), generalized anxiety disorder (GAD), obsessive compulsive disorder (OCD), alcohol use disorders and pathological gambling to be of particular importance. There is presently a dearth of local data on these disorders and information of their prevalence rates, variation in disease distribution among the ethnic groups, the extent of unmet needs (including treatment gaps and time taken to access care), and the associated comorbidity were thought to be particularly important for the planning, development and evaluation of mental health services.
Since its independence in 1965, Singapore has attained steady economic growth and prosperity, the political situation has remained stable with no civil strife nor has it fought any wars or experienced any major disasters (either natural or man‐made) and the rate of violent crime and accidents has been relatively low; we therefore decided to exclude post‐traumatic stress disorder from the study. The stringent anti‐drug laws and its effective enforcement have resulted in low rates of substance abuse in Singapore. The legal requirement to report known cases of illict substance abuse to the law enforcement agencies would also make it difficult to obtain reliable data on substance abuse in a household survey. The following DSM‐IV mental disorders were finally included in the survey: psychotic disorders (screening without further differential diagnosis); mood disorders (unipolar and bipolar); anxiety disorders (GAD and OCD); and alcohol abuse disorders (abuse and dependence), nicotine dependence and gambling disorders (probable pathological gambling) (Table 1).
Table 1.
CIDI modules included in the Singapore Mental Health Survey
| Module | Brief description |
|---|---|
| Screening section | i. Some socio‐demographic data captured includes age, gender, marital status, weight, height, rating of own physical and mental health and comparing it with a year before. |
| ii. Screening section includes screening of panic, intermittent explosive disorder, depression, mania, anxiety and phobia (specific and social). | |
| Depression | Module organized into symptoms; severity (duration of symptoms and distress experienced); onset of illness, course (episodes, duration); lifetime and 12‐month prevalence; |
| Effect on functioning; help seeking; treatment gap; family history. | |
| Mania | Module organized in a manner similar to Depression module. |
| Anxiety disorders | Includes: panic attacks, specific phobias (animal, water, heights, etc.), social phobia, agoraphobia, GAD. |
| Services | Includes information on service utilization. |
| Details of health care provider consulted: who, when, satisfaction, quality of help received, first visit, last visit, etc. | |
| Pharmacoepidemiology | Includes information on medications taken for nerves and emotional problems in the past one‐year. |
| Alcohol use | Establishment of use and onset of use; |
| Abuse and dependence criteria; | |
| Onset, recency, course. | |
| OCD | Symptom check list for obsessive thoughts and compulsive behavior. |
| Psychosis screen | Symptom checklist for psychosis: |
| Exploration into whether these symptoms were associated with medical illness, substance abuse, etc. | |
| Social networks | Explores relationships with relatives, friends and partner. |
| Family burden | Burden of care: physically taking care, emotional support. |
| Effect of this problem: embarrassment, depression, anxiety, financial cost. | |
| 30‐Day functioning | Impact of health problem on every day activities; on social functioning; on physical functioning. |
| Feelings of embarrassment and discrimination because of health problems. |
A significant limitation is that schizophrenia and other non‐affective psychoses, although important mental disorders are not included in the core WMH assessment because previous validation studies showed they are overestimated in lay‐administered interviews like the CIDI (Kendler et al., 1996). For the purposes of SMHS we used the Psychosis screen used in CIDI 3.0 which gives us the prevalence of psychotic symptoms in the community.
The use of the CIDI requires successful completion of a training program offered by an official WHO CIDI Training and Research Center (CIDI‐TRC). Three members of the study team were trained at the University of Michigan's CIDI Training and Reference Center and three other members attended a three‐day training in Beijing conducted by the Institute of Mental Health Peking University and were certified in the use of the Chinese CIDI.
Language of administration
Singapore is a multiracial and multicultural city‐state. The literacy rate is over 95%, with English as the predominant official language and the main medium of instruction in the education system. Thus, English is widely used, especially among the younger generations. Chinese, Malay and Tamil are the three other official languages and are taught as second languages in the schools and are widely spoken among the older generation in the respective ethnic groups.
The Chinese language CIDI has been recently developed by the WMH‐CIDI group in China and this was adapted for use in our survey. Translation of all the modules used in SMHS was carried out into Bahasa Melayu (the official written language of the Malays). The Bahasa Melayu version of CIDI 3.0 was translated from the English version. The translation procedure was an adaptation of the guidelines outlined by the WHO. A composite translation was derived from two independent forward translations. An expert panel comprising the professional translators, content experts and a layperson was convened to identify and resolve any inadequate expressions in the translation and discrepancies between the translated and original version. Cognitive interviews and pre‐testing were conducted with individuals representing the target population to assess whether the translated version was understood in the manner intended and to identify items that were misinterpreted. Given the time constraints and lack of familiarity with Blaise software development (platform for computerized CIDI), we decided to use the PAPI version of the Malay CIDI.
The choice of the language depended on the respondent. In those cases where the interviewer did not speak the language preferred by the respondent, these cases were returned to the supervisor at the earliest with an indication of the preferred language. These cases were re‐allocated and the time taken to re‐allocate cases as well as time taken to re‐contact the respondent were closely monitored. According to census data (2000), the most frequently spoken languages at home among the Indian resident population in Singapore were Tamil (42.9%), English (35.6%) and Malay (11.6%); 9.9% of Indians reported the use of other languages (Statistics Singapore, 2000). The CIDI was not translated into Tamil for this study as we made the assumption that the majority of the Indian population would still be conversant in English; and that the need for a Tamil version would be re‐assessed in light of subsequent field data.
Supplementary instruments
Four other PAPI instruments were used in the survey. The socio‐demographic form collected information on age, gender, ethnicity, marital status (single, married, and previously married: separated/divorced/widowed), living situation, employment and personal finances. The South Oaks Gambling Screen (SOGS) is a brief 20‐item questionnaire used to screen for pathological or compulsive gambling. The SOGS is based on the DSM‐III criteria for pathological gambling. It may be either self‐administered or interviewer‐administered. For the purposes of our study it was self‐administered, however for respondents who were not literate the interviewer administered it. Internal consistency and test–retest reliability of this questionnaire has been established (Lesieur and Blume, 1987). SOGS has been widely used in epidemiological studies; it correlates with the DSM‐IV criteria items as well as psychosocial and gambling‐related problems (Tang et al., 2010). The modified Fagerstrom Test for Nicotine Dependence (FTND) is a short six‐item instrument for assessing the intensity of physical addiction to nicotine (Heatherton et al., 1991). The overall score on the FTND is significantly associated with the intention to quit smoking, the history of 24‐hour quit attempts in the last year, the cigarette type (regular or light) and the number of pack‐years (Haddock et al., 1999), suggesting that the instrument has adequate criterion‐related and predictive validity. Studies have also found FTND to be a valuable tool for studies of nicotine dependence in large epidemiological samples (Vink et al., 2005).
A modified version of the CIDI chronic medical conditions checklist was used to gather data on the prevalence of medical illnesses in the population. Data was collected on 15 conditions such as asthma, diabetes, hypertension, cancer, etc. The illnesses chosen were those that are prevalent in Singapore as per local data. All supplementary instruments were also translated into Chinese and Bahasa Melayu.
Adaptation of the CIDI and other instruments for the Singapore context
Even though the CIDI has been widely used in many countries, we adapted it to the Singapore context in a methodical and systematic fashion as shown in Figure 1.
Figure 1.
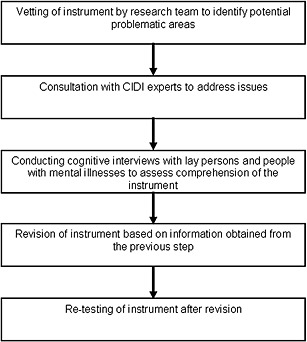
Adaptation of instrument for the Singapore population.
Cognitive interview process
A total of 40 cognitive interviews were conducted with a total of 36 participants, including 18 patients with mental illnesses who were recruited by purposive sampling through referrals from psychiatrists at the Institute of Mental Health, in order to assess respondents' understanding of items in the English CIDI instrument. The sample profile included equal numbers of men and women and Chinese, Malays and Indians. Each module was assessed on the basis of responses to at least three cognitive interviews. Questions from the CIDI 3.0 were read to the participants and the participants were instructed to think aloud as they answered each question. Ambiguous items and responses were further probed using standardized probes to the questionnaire. All the interviews were audiotaped, documented and evaluated. From the data collected, participants were able to comprehend and provide relevant answers to the CIDI 3.0 questionnaire. Although participants were aware that certain terms and expressions were not commonly used in Singapore context, they commented that these factors did not hinder their overall comprehension of the questions and decision‐making on the options. Similar cognitive interviews were also used to evaluate the Chinese and Malay version of the CIDI and no major issues were identified.
Sample
The SMHS was a population‐based, cross‐sectional epidemiological study of adult Singapore residents aged 18 years and above living in Singapore. The sampling frame was based on a national population registry from the Ministry of Home Affairs (MHA) Singapore, which is a database of all citizens, permanent residents and foreigners in Singapore, and is updated daily based on administrative data.
The residents who were younger than 18 years, without any address or with overseas addresses as of July 2009 and all foreigners were excluded from the frame. The researchers were provided an initial computer‐generated list of individuals together with gender, addresses and age of those who met the requirements. A probability sample was randomly selected using a disproportionate stratified sampling design with 16 strata defined according to ethnicity (Chinese, Malay, Indian, Others) and age groups (18–34, 35–49, 50–64, 65 and above). The residents aged 65 and above, Malays and Indians were over‐sampled to ensure that sufficient sample size would be achieved to improve the reliability of estimates for the subgroups analysis. We used criteria set by the Singapore census to define the different ethnicities in the current study (Singapore Census, 2001). It is compulsory for every Singapore citizen and permanent resident who is 15 years of age and older to have an identity document known as the National Registration Identity Card (NRIC). The front side of the card indicates the holder's name, race, date of birth, sex and country of birth. Information on this card was used for verifying the personal details of the respondent. The residents who were incapable of doing an interview due to severe physical or mental conditions or language barrier, those with incorrect address or those living outside the country; those residing in institutions, hospitals and prisons for the entire field period of the study were also excluded from the study.
This study involved a single‐stage design without geographic clustering. The sample size numbers were calculated by running statistical power calculations for single and two proportions to determine what sample sizes are necessary overall, as well as for subgroups (i.e. age and ethnicity), to produce a precise estimate with a margin of error equal to 0.05 for different disorders. We assumed the required statistical power to be 0.80, while the Type 1 error rate is controlled at α = 0.05, as is standard. Note that if Type 2 error = β, then power = 1 – β. We generated two types of power calculations for the estimated rates of depression (5.6%), anxiety disorder (3.4%), smoking (14%), nicotine dependence (9%) and probable pathological gambling (2.1%). The prevalence estimates were obtained from available local data. In the first approach, we assumed different margins of error and computed the necessary sample size for each set up. In the second approach, we assumed certain realistic sample sizes (e.g. n = 5000, 6500, 7000) and computed the margin of error for key quantities of interest. We found that the margin of error for the overall prevalence estimate was between 1.5% and 3.0%, while the margin of error for the strata defined by age and ethnic groups was 1.0% to 3.5% where those above 65 years of age and Malay and Indian ethnicity were oversampled. Our design effect after oversampling by age and ethnicity was in the range 1.1–2.17. Note that as the margin of error (or precision) of a binary proportion depends on the estimate, we also computed the relative standard error (RSE), which is acceptable if < 30% (Klein et al., 2002).
We found that the RSE was appropriate for more prevalent disorders but high and above 30% for disorders such as probable gambling. Using these two approaches, we determined that a target sample size of 6500 samples would provide sufficient precision to measure the prevalence of these conditions. Thus, assuming an eligibility rate of 65% and a response rate of 65%, a sample of approximately 15,000 persons was needed for this study.
In order to make inference of prevalence of mental disorders to the entire population of Singapore residents, the final datasets will be weighted to the population. The weighting of the data can be taken into account in data analyses using SAS software version 9.2.
The selection of the household member identified from the sampling frame was determined using a screening approach at the first contact made by the interviewer. This screening process involved a brief interview with standard procedures to identify the right member of the household. In this approach, the interviewer contacted any member of the household and identified the member(s) of the household who matched the age, ethnicity and gender criteria as provided by the record, the person identified thus was chosen for the interview. If there was more than one person who met the criteria then a respondent was selected using the last birthday approach. This approach ensures that the selection of the respondent remains random and there is no bias introduced by the interviewer at this point.
The conduct of the survey
The conduct of the fieldwork was awarded to a commercial survey firm after careful deliberation by the researchers involved in the study. The survey firm identified interviewers who were older than 21 years of age, experienced in door‐to‐door surveys and with appropriate computer skills for conducting the survey. Interviewers were trained by Institute of Mental Health staff in batches of 10 to 15 over a three‐week period. The interviewers were trained on the ethical aspects of the study including taking written informed consents, proper administration of the CIDI and supplementary questionnaires, proper conduct of the structured interviews as well as in the logistics of the fieldwork. Each interviewer was assessed by the Institute of Mental Health trainers on all aspects of the fieldwork before being allowed to proceed with the actual fieldwork. The survey firm also observed mock interviews conducted by the interviewers before allocating the cases to them. In all, 87 interviewers were trained (in six batches) over the course of the study. The pilot phase of the study was launched in early October 2009 after obtaining approvals from the relevant Institutional Review Boards. Each household was alerted through letters sent via regular mail about the survey a week before the expected first contact; and contact numbers that they could call to make an appointment. Field supervisors and Institute of Mental Health staff accompanied interviewers during the first week of their field interviews to identify and resolve problems on the ground. Vigorous attempts were made to establish a contact – each household was approached to a maximum of 10 times at different days and times to ensure a high probability of contact. The team also designed “While you were out” letters to respondents who were not in their homes, with instructions to contact the survey firm. A list of help lines of psychological units of various hospitals and counselling centres were provided to all respondents before the initiation of the interview. Respondents were paid an inconvenience fee of S$50 on completion of the interview. A press conference for the local major press, radio and televisions stations was held to create public awareness of the survey and its importance. At the point of completion of the field period the survey had recruited 6616 respondents with a response rate of 75.9%. Regular meetings were held with the interviewers and field executives and this continued through the entire survey to ensure early identification of any emergent problems in the field. Figure 2 shows the schematic flow of the field survey.
Figure 2.
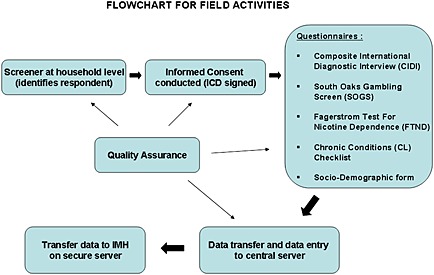
Flowchart for field activities.
Replicate release and response rate
The selected 15,000 individual were divided into 30 batches of 500 each and six batches constituted one replicate of 3000 cases. The distribution of age, gender and ethnicity in each replicate was designed to be similar to that of the original sample provided. The required sample size was achieved over a one‐year period with release of four replicates and one batch (total of 13,500 cases). Survey was continued until all the released cases were contacted. Of these, respondents at 9116 addresses (67.5%) were successfully identified while at 2256 (16.1%) addresses selected respondent could not be identified (non‐match), 1070 (7.9%) refused to be screened, 633 (4.7%) could not be contacted despite maximum contact attempts, 402 (3%) were incomplete addresses or demolished or vacant housing units and 23 (0.2%) were voided due to frame error.
Among the 9116 matched respondents, 6648 (72.9%) respondents were interviewed, 845 (9.4%) refused to participate in the study, 664 (7.3%) were either away for the entire duration of the survey (535), were not contactable within maximum contact attempts (84) or were deceased (45), 554 (6.1%) respondents had permanently moved to another location or country and 396 (4.3%) were ineligible due to language barrier or incapability to conduct the survey. Of the completed interviews, 32 were voided due to quality failure and were not included in the analysis. The overall response rate for the study after excluding the ineligible 396 cases was 75.9% (n = 6616).
No significant differences were found among responders and non‐responders with respect to age and gender. However, there were significantly more non‐responders belonging to Chinese and Other ethnic groups. Information on other auxiliary variables were not available for non‐responders and could not be used for assessing predictors of non‐response.
Quality assurance for the Singapore Mental Health Study
It is vital to maintain a high level of quality assurance throughout the study. In the following section we describe these measures in detail.
Quality assurance in the selection of the field staff
Interviewers were required to have a minimum of secondary level education, proficiency in at least one of the languages used for the survey, necessary computer skills and relevant experience. Selected interviewers underwent the three‐week training in various aspects of survey administration and record keeping. During the sessions and at the end of the training, interviewers were evaluated using one‐to‐one mock interviews conducted with the trainers and a lay respondent. Key evaluation criteria were, understanding of study objectives and intent of the questions, correct administration and data collection, language proficiency and ethical conduct. Internal quality control was ensured through regular training, retraining and mentoring of interviewers. Regular debrief meetings with the interviewers and field executives were held for problem identification and troubleshooting. A log of these decisions was maintained for future reference.
Quality assurance during the survey
Uniform information flow
Standard disposition codes were set for tracking the progress of field visits. These codes were captured in the record management systems and extracted to generate several productivity reports.
Quality assurance in survey administration
Regular field visits were conducted to accompany interviewers on the field. After obtaining the respondent's permission, a senior member of the team supervised the complete data collection process to observe the consent taking, interviewing, and probing and clarification process for each interviewer when they first started fieldwork. Additionally, the method of recording data was reviewed for frequent cancellations, overwriting and incorrect skips. To avoid errors in data collection due to interviewer fatigue, the number of cases released to interviewers was controlled. We also tracked the number of interviews completed in a day and for each week. Apart from field observation, 20% of cases completed by an interviewer were subjected to detailed verification. A validation script was designed to aid this process. Respondents were recontacted; 5% through face‐to‐face validation and 15% via telephone to evaluate the interview. Thirty‐two cases were rejected in all based on several criteria; some of the important reasons were error in identifying the correct respondent (68%), interviewing respondents who are unable to understand the language of the instrument resulting in translations done by interviewer and/or family member (16%), and missing consent forms (4%). A record of complaints and observations was maintained for each interviewer during the survey.
Quality assurance in productivity
Several productivity reports were designed to (1) track the case assignment and completion rate, (2) aid transparency in progress per replicate and interviewer, (3) identification of outliers and errors and (4) decision‐making and troubleshooting. Screening and interview summary reports provided information on successful identification of selected respondent and completion of interviews, respectively. Interviewer report was designed to obtain information on completion rate for each field interviewer. An aging report was generated to inspect whether the cases were worked at a steady rate. A validation report was generated to document the findings from field validation conducted by the independent validation team. Reports were routinely monitored to observe trends, outliers (such as sudden high rate of competes or refusals) and clarification (such as wrong coding, discrepancy from earlier reports, calculation errors, etc.).
Quality control in data processing
Pre‐coded data entry was conducted to record the information in the PAPI questionnaires. Data entry and abstraction software are programmed for ease of data entry and verification with the previous entry. A detailed data flow was created to document the transfer of information from the system to key personnel. Logic checks were tested at the time of data verification. Research data was compared with the field data to avoid discrepancies in the number of completed interviews.
Conclusions
The SMHS incorporates multi‐disciplinary approaches and high standards of epidemiological research that are essential for the comprehensive evaluation of mental health in Singapore. The study has some limitations. First, it was not possible to establish the prevalence of all mental disorders due to limitations of time, costs, and tolerability of respondents. In this study, we chose those disorders that are likely to have the greatest impact locally and this selection was made from a comprehensive review of the scientific literature, consultation with our Stakeholders Board, and based on expert consensus. Second, this was a household sample so it excluded those who were residents of nursing homes, hospitals and prisons for the entire field period of the survey. These groups could possibly have higher rates of mental disorders than the general population but they also comprise a very small proportion of the total Singapore population. Third, about 24% of the sample was not interviewed due to “non‐response” of the sample which could lead to underestimation of the true rates – for example, in the US National Comorbidity Survey (also on mental disorders), special efforts were made to estimate the rate of disorders among persons who initially refused to participate in the Survey through a briefer interview, and it showed that persons who initially declined to be interviewed had higher rates of mental disorders than those who did agree to participate (Kessler et al., 1994). Lastly we did not do a clinical validation of the diagnoses generated by CIDI.
Despite these limitations, the study will provide a wealth of hitherto unavailable information on the rates of mental illness, about the social and economic impact of such disorders in Singapore, and on the help‐seeking behaviors of those with mental illness. The findings will indicate the state of our mental health as a nation, how many of those who are ill are actually receiving treatment or had received help and what are the consequences of being mentally ill in Singapore. The findings will have wider ramifications on health policies and the way we treat those with mental illness. It will establish a focus and an infrastructure of such expertise for further research in this field and for other groups of disorders. Dissemination of findings will not only aid mental health awareness among the population but also create international reputation for Singapore in this field.
Declaration of interest statement
The authors have no competing interests.
Acknowledgements
This research was supported by funding from the Singapore Millennium Foundation and the Ministry of Health, Singapore.
References
- Bijl R.V., van Zessen G., Ravelli A., de Rijk C., Langendoen Y. (1998) The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Social Psychiatry and Psychiatric Epidemiology, 33, 581–586, DOI: 10.1007/s00127-002-0566-3 [DOI] [PubMed] [Google Scholar]
- Chong S.A. (2007) Mental health in Singapore: a quiet revolution? Annals, Academy of Medicine, Singapore, 36, 795–796. [PubMed] [Google Scholar]
- Chua H.C., Lim L., Ng T.P., Lee T., Mahendran R., Fones C., Kua E.H. (2004) The prevalence of psychiatric disorders in Singapore adults. Annals, Academy of Medicine, Singapore, 33, S102. [Google Scholar]
- Fones C.S.L., Kua E.H., Ng T.P., Ko S.M. (1998) Studying the mental health of a nation – a preliminary report of a population survey in Singapore. Singapore Medical Journal, 39, 251–255. [PubMed] [Google Scholar]
- Haddock C.K., Lando H., Klesges R.C., Talcott G.W., Renaud E.A. (1999) A study of the psychometric and predictive properties of the Fagerström Test for Nicotine Dependence in a population of young smokers. Nicotine & Tobacco Research, 1, 59–66, DOI: 10.1080/14622299050011161 [DOI] [PubMed] [Google Scholar]
- Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerstrom K.O. (1991) The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction, 86, 1119–1127, DOI: 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- Kendler K.S., Gallagher T.J., Abelson J.M., Kessler R.C. (1996) Lifetime prevalence, demographic risk factors and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Archives of General Psychiatry, 53, 1022–1031. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., McGonagle K.A., Zhao S., Nelson C.B., Hughes M., Eshleman S., Wittchen H.U., Kendler K.S. (1994) Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51, 8–19. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Ustun T.B. (2004) The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13, 93–121, DOI: 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein R.J., Proctor S.E., Boudreault M.A., Turczyn K.M. (2002) Healthy People 2010 Criteria for Data Suppression, Statistical Notes, no. 24, Hyattsville, MA, National Center for Health Statistics. [PubMed] [Google Scholar]
- Lesieur H.R., Blume S.B. (1987) The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. American Journal of Psychiatry, 144, 1184–1188. [DOI] [PubMed] [Google Scholar]
- Singapore Census . (2001) Singapore Census of Population 2000: Statistical Release 1 – Demographic Characteristics, Singapore, Department of Statistics. [Google Scholar]
- Statistics Singapore . (2000) http://www.singstat.gov.sg/pubn/papers/people/c2000adr-literacy.pdf [8 April 2010].
- Statistics Singapore . (2009) http://www.singstat.gov.sg/pubn/popn/population2009.pdf [25 January 2010].
- Tang C.S., Wu A.M., Tang J.Y., Yan E.C. (2010) Reliability, validity, and cut scores of the south oaks gambling screen (SOGS) for Chinese. Journal of Gambling Studies, 26, 145–158, DOI: 10.1007/s10899-009-9147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega W.A., Kolody B., Aguilar‐Gaxiola S., Alderete E., Latalano R., Caraveo‐Anduaga J. (1998) Lifetime prevalence of DSM‐III‐R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry, 55, 771–778. [DOI] [PubMed] [Google Scholar]
- Vink J.M., Willemsen G., Beem A.L., Boomsma D.I. (2005) The Fagerstrom Test for Nicotine Dependence in a Dutch sample of daily smokers and ex‐smokers. Addictive Behaviors, 30, 575–579, DOI: 10.1016/j.addbeh.2004.05.023 [DOI] [PubMed] [Google Scholar]
- Wittchen H.U. (1994) Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): a critical review. Journal of Psychiatric Research, 28, 57–84. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Perkonigg A., Lachner G., Nelson C.B. (1998) Early Developmental Stages of Psychopathology study (EDSP): objectives and design. European Addiction Research, 4, 18–27, DOI: 10.1159/000018921 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (1990) Composite International Diagnostic Interview (CIDI, Version 1.0), Geneva, WHO. [Google Scholar]
- World Health Organization (WHO) . (2001) Mental Health: New Understanding, New Hope. The World Health Report, Geneva, WHO. [Google Scholar]


