Abstract
Anxiety disorder is a common psychiatric problem during late‐life, and frequently co‐occurs with depression. High comorbidity between anxiety and depression may partly be explained by the definition of the disorders and the assessment of both disorders with one instrument at the same time. The current study investigates the relation of current and past depression with anxiety disorders in the Rotterdam Study, a large population‐based cohort study of older adults in the Netherlands (n study population = 5565). DSM‐IV anxiety disorder was ascertained with the Munich version of the Composite International Diagnostic Interview. DSM‐IV depression was diagnosed with the Schedules for Clinical Assessment of Neuropsychiatry (SCAN) on a different day. Past depression was assessed from general practitioners' records, self‐report, and a prior SCAN interview. Of the 457 persons with an anxiety disorder, 11.6% had a comorbid major depression, and another 6.3% had other depressive syndromes. However, 49.3% of persons with an anxiety disorder experienced or had in the past experienced a depressive episode. Our study suggests that comorbid depression in older adults with anxiety disorders may be less prevalent than previously suggested. However, the relation of current anxiety disorders with past depression is substantial. Copyright © 2011 John Wiley & Sons, Ltd.
Keywords: anxiety disorder, depressive disorder, comorbidity, older adults, common method variance
Introduction
Anxiety disorder is a common psychiatric problem in late life, affecting 3 to 15% of older adults (Bryant et al., 2008). It is associated with considerable distress, impairment in quality of life, disability, and increased mortality and frequently co‐occurs with depression (van Hout et al., 2004; Beekman et al., 1998; Ayers et al., 2007; Seeman et al., 1995; de Beurs et al., 1999). Persons with both anxiety and depression experience more disability and distress than persons with a singular disorder (Cairney et al., 2008).
Comorbidity of depression with anxiety was recently reported to be as high in older adults as in younger persons (King‐Kallimanis et al., 2009). However, the reported frequency of comorbid anxiety and depression in persons aged over 55 varies. In the French ESPRIT study, only 12% of persons with an anxiety disorder also reported major depression (Ritchie et al., 2004). In a large Canadian study 23% of older adults with an anxiety disorder had a comorbid major depression (Cairney et al., 2008). However, generalized anxiety disorder (GAD), a common anxiety disorder in older adults (Bryant et al., 2008), was not assessed. Beekman et al. (2000), who included GAD in their study, found a comorbidity of 26% between anxiety and major depression. Kvaal et al. (2008) reported an even higher comorbidity; 65% of older adults with anxiety disorders had a depressive disorder, an additional 25% of persons with anxiety disorder had a subthreshold depressive syndrome. However, in this study the Geriatric Mental State‐Automated Geriatric Examination for Computer Assisted Taxonomy (GMS‐AGECAT), and not the Diagnostic and Statistical manual of Mental Disorders (DSM) was used to define depression and anxiety. In a retrospective study on the overlap between lifetime diagnoses of anxiety and depression, seven of the 19 persons (37%) with a lifetime diagnosis of anxiety disorder also had a lifetime diagnosis of major depression or dysthymia (Heun et al., 2000). Another eight persons had a subthreshold depressive disorder (42%). Despite the great variability, all studies conclude that there is substantial comorbidity between anxiety and depression in the older adult population.
Inconsistencies in the extent of comorbidity may partly be determined by methodological differences between studies. Commonly used instruments to diagnose anxiety and depression, such as the Composite International Diagnostic Interview (CIDI), the Mini‐International Neuropsychiatric Interview (MINI), GMS‐AGECAT or Diagnostic Interview Schedule (DIS), assess anxiety in parallel to depression. Similar wording of the interview items is used to ascertain the shared symptoms of anxiety and depression. When asked about both disorders during one interview session, respondents may be tempted to give consistent answers (McGuire, 1966). Consequently, comorbidity may be diagnosed more frequently if one assessment tool is used to diagnose anxiety and depression during one session, than if assessed by different instruments or in separate sessions. This “common method variance” could inflate the observed comorbidity between anxiety and depression (for a review see Podsakoff et al., 2003).
In the present study, we examined the comorbidity between anxiety and depression in a large population‐based cohort of older adults. We addressed the limitations of prior research by measuring current anxiety disorders and depression with different instruments on different days within a short time period to avoid common method variance. In addition, we used previously collected information on prior episodes of depression to estimate the comorbidity of current anxiety with current and past depression. This information was obtained by a clinical interview, self‐report and continuous monitoring of general practitioners' records. We hypothesized that, on the one hand, comorbidity between anxiety and depression would be relatively low compared to previous studies if not assessed with the same instrument. On the other hand, we expected the overlap between current anxiety and depression to increase substantially, when past depressions were accounted for.
Method
Study population
This study was embedded in the Rotterdam Study; a prospective population‐based cohort study of older adults to assess risk factors for chronic diseases (Hofman et al., 2007; Hofman et al., 2009). In 1990, all inhabitants of a district in Rotterdam aged 55 years and over were invited to participate, of which 7983 persons participated in the first round (baseline). This population was extended in 1999, with an additional cohort of 3011 persons aged 55 years and over. Every four years participants undergo an extensive home interview and physical examination at a research centre. The Medical Ethics Committee of the Erasmus Medical Centre approved the Rotterdam Study.
In the last examination round (2002–2005) anxiety disorders and depression were assessed. Of the 7609 eligible persons, 6007 participated in this round (Figure 1). We excluded 434 persons without valid anxiety or depression assessment and eight persons with bipolar disorder. The excluded persons (n = 442) were significantly older (mean age 75.5 versus 72.6) and more often female (68.8% versus 58.1%) than the included persons (n = 5565). For a selected sample of 3374 persons, data were available not only on current anxiety and depression, but also on past depression. The persons without data on past depression were more often male and younger (45.1% males versus 39.9% males, mean age of 68.5 years versus 75.2 years).
Figure 1.
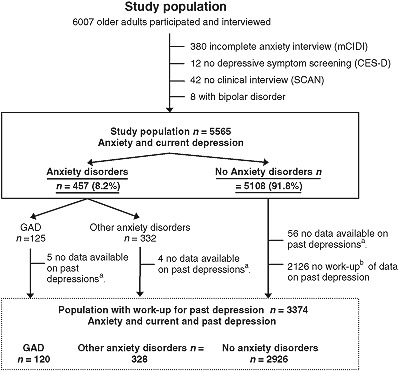
aPast depression as assessed by continuous monitoring of general practitioner (GP) records. bWork‐up of GP records for the complete cohort was not feasible and unnecessary and was therefore performed for part of the total study population. This selected sample was used only for calculation of current anxiety comorbidity with current and past depression combined. All other calculations were based on the total, unselected, study population (n = 5565). M‐CIDI, Munich Composite International Diagnostic Interview; CES‐D, Centre for Epidemiological Studies Depression Scale; SCAN, Schedules for Clinical Assessment of Neuropsychiatry; GAD, Generalized Anxiety Disorder.
Measures
Anxiety disorders
Anxiety disorders were diagnosed as part of the home interview. Trained lay interviewers conducted a slightly adapted version of the Munich version of the Composite International Diagnostic Interview (M‐CIDI) to assess the following anxiety disorders with a computerized diagnostic algorithm according to DSM‐IV criteria: GAD, panic disorder with or without history of agoraphobia, agoraphobia, social phobia and specific phobia. Obsessive compulsive disorder and post‐traumatic stress disorder were not assessed. The M‐CIDI was specifically designed to obtain DSM‐IV diagnoses of mental disorders and test–retest reliability for anxiety disorders is good (Kappa for any anxiety disorder: 0.81, Wittchen et al., 1998). Whereas the CIDI was not specifically designed for diagnosis in older adults, it is one of the most widely used instruments to diagnose anxiety disorders in older adults. In addition, the M‐CIDI has an important adjustment to simplify questions. Visual response cards were used for the most complicated questions. The assessments of anxiety disorders were implemented to measure point prevalence. For GAD, problems to recall symptoms ending up to 12 months ago were expected. Therefore, we assessed one‐month prevalence of GAD according to DSM‐IV criteria. GAD is a chronic disease with low recovery rates. Average duration of more than 10 years has been reported for GAD in older adults (Lenze et al., 2005). One‐month prevalence will presumably approximate one‐year prevalence (Weisberg, 2009; Lenze et al., 2005). For agoraphobia, social phobia, specific phobia and panic disorder “current” symptoms, such as avoidance of plane flights, were established more easily if ascertained over a longer period (the last year). Again, these disorders are generally chronic (Schuurmans et al., 2005) and our one‐year prevalence estimates are most likely good proxies of point prevalence.
Current depression
Assessment of depression has been described previously (Luijendijk et al., 2008). In short, during the home interview, participants were screened for symptoms of depression with the Center for Epidemiological Studies Depression (CES‐D) scale (Radloff, 1977). Screen‐positive persons (CES‐D‐score ≥ 16) were invited for a semi‐structured clinical interview with the Schedules for Clinical Assessment of Neuropsychiatry (SCAN, Wing et al., 1990). This interview was conducted by a trained clinician at the participant's home one week to two months (median time interval: two weeks) after the screening procedure and the anxiety interview. We were able to use the SCAN in this population‐based setting, because depression can be screened for with high sensitivity (Beekman et al., 1997). With a computerized DSM‐IV based diagnostic algorithm, major depression, minor depression and dysthymia during the past month were diagnosed. Although psychometric properties of the SCAN in older adults are unknown, it has been used repeatedly to diagnose depression in older adults in the Dutch population (Van den Berg et al., 2000). The depression section of the CIDI was not applied to this population.
Past depression
In the years between baseline and the anxiety assessment, information on past depressions was ascertained prospectively in three ways. First, during the examination of 1997 to 2001 all participants were screened for depression by CES‐D scale and screen‐positive persons were assessed with the SCAN interview as described earlier. Second, physicians conducted repeated interviews to assess self‐reported depression between subsequent assessment rounds (1997–2001 and 2002–2005). Third, general practitioner (GP)‐records and specialist letters were monitored actively for the occurrence of episodes of depressive syndromes during a mean period of nine years prior to anxiety assessment. Monitoring of GP‐records for the original cohort was almost complete. In the extended cohort, only depressive episodes of persons with an anxiety disorder were monitored. Monitoring is a time‐consuming procedure as it requires screening and coding of (mostly non‐digital) GP‐records. Monitoring of persons without anxiety disorders in the extended cohort was considered unnecessary as the number of controls exceeded the number of cases by 5:1. Retrospective information on life‐time episodes was collected at baseline.
Depression comprised major depression, minor depression and dysthymia diagnosed with SCAN, self‐reported depression if a health professional was consulted, and depression recorded by a GP or physician.
Assessment of other variables
Age, sex and marital status were recorded. Living status was coded as living alone compared to living with one or more people. Education was grouped into low level (primary education), intermediate (secondary education, vocational education) and high level education (higher education). Disability, or Activities of Daily Living, was assessed with the Stanford Health Assessment Questionnaire (Fries et al., 1982). This measures disability in eight fields (e.g. hygiene, eating, walking) with responses ranging from zero corresponding to “perform without difficulty” to three corresponding to “unable to do independently”. The mean score of all fields constitutes the Disability Index and the standard cut‐off of 0.5 indicated no disability versus mild to severe disability. We assessed functioning in basic daily activities with an adaptation of the Instrumental Activities of Daily Living (Lawton and Brody, 1969). Six areas were assessed (e.g. maintaining finances, meal preparation) with responses ranging from zero corresponding to “perform without difficulty” to three corresponding to “unable to do independently”. The mean score of the six items was calculated and a cut‐off of 0.5 (upper quartile) was selected to distinguish between no instrumental disability versus mild to severe instrumental disability. Cognitive capacity was assessed with the Mini Mental State Examination (MMSE), which assesses six broad areas of daily cognitive functions (Folstein et al., 1975). A cut‐off of 26 indicated adequate cognitive capacity versus impaired cognitive capacity. Participants were continuously monitored for occurrence of coronary heart disease as was previously described (Mattace‐Raso et al., 2006). Diagnoses were assigned according to the International Classification of Diseases, 10th Revision (ICD‐10). Coronary heart disease was defined as myocardial infarction (ICD‐10 I21), a percutaneous transluminal coronary angioplasty, a coronary artery bypass graft and other forms of acute (I24) or chronic ischemic heart disease (I25). Diabetes Mellitus cases were defined as having a fasting plasma glucose level of at least 7.0 mmol per litre, a non‐fasting plasma glucose level of at least 11.1 mmol per litre, or the use of oral antidiabetes medication, use of insulin or treatment by diet and registered by the GP as having diabetes (American Diabetes Association, 1997).
Statistical analysis
Percentages and means were computed to describe the baseline characteristics of the study population. We performed chi‐square tests and t‐tests to compare these characteristics between persons with and without anxiety disorder.
The prevalence of anxiety disorders was calculated from the percentage of anxiety disorders in the total study population (n = 5565, Figure 1). We also studied the comorbidity of current anxiety with current (major) depression in this total study population. Only the comorbidity between current anxiety and current and past depression was estimated using the selected sample of 3374 persons (Figure 1). To assess comorbidity we compared the depression rate of anxiety and non‐anxiety cases.
Comorbidity estimates are presented for all assessed subtypes of anxiety disorders separately. However, adjusted odds ratios were only calculated for GAD and agoraphobia separately. Specific phobia, social phobia and panic disorder were combined because numbers were too small to calculate stable estimates. In addition, we present analyses stratified by age.
Primarily, the one‐month prevalence of depression was used in the analyses. However, we reran analyses including depressions observed in one and two years before anxiety assessment to facilitate comparison with studies that provide a one‐year prevalence of depression. However, these results should be interpreted carefully as for GAD only a one‐month prevalence was assessed.
Adjusted odds ratios were computed to compare occurrence of depression in persons with and without anxiety disorder. We adjusted odds ratios for age and gender. Odds ratios were further adjusted for the following socio‐demographic variables: living status (living alone, yes or no), education and cognitive status (impaired cognitive status, yes or no, Vink et al., 2008). These variables have been associated to anxiety and depression and could potentially affect the comorbidity estimates. Because the age and gender adjusted analyses yielded similar results as the fully adjusted analyses we only present the fully adjusted results. All covariates had less than 2% missing values; therefore complete case analyses were performed. Statistical analyses were performed in SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
The point prevalence of anxiety disorders in this older adult population was 8.2% (n = 457). The most prevalent anxiety disorders were agoraphobia (4.0%, n = 221) and GAD (2.2%, n = 125). Sixteen per cent of the agoraphobia cases (n = 35), almost 25% of the GAD cases (n = 31) and more than 20% of the persons with other anxiety disorders (n = 37) had another comorbid anxiety disorder.
The one‐month prevalence of depression was 4.1%; about half fulfilled the DSM‐IV criteria for major depression. Characteristics of the study population are summarized in Table 1. Persons with a comorbid depression were more often living alone, and experienced more disability than persons with only an anxiety disorder. In addition, comorbid cases were more often diagnosed with coronary heart disease than non‐comorbid cases.
Table 1.
Characteristics of study population (n = 5565)a
| No anxiety disorder | Anxiety disorder | ||||
|---|---|---|---|---|---|
| n = 5108 | Agoraphobia,b n = 221 | GAD,b n = 125 | Other anxiety disorder,b, c n = 166 | All anxiety disorders, n = 457 | |
| Female (%) | 56.3 | 79.6*** | 77.8*** | 75.3*** | 78.0*** |
| Mean age (SD) | 72.6 (7.8) | 73.0 (7.4) | 72.0 (7.9) | 70.8 (7.1)** | 72.0 (7.4) |
| Age range (minimum age – maximum age) | 58.0‐100.1 | 59.5‐90.0 | 59.5‐91.9 | 59.4‐92.4 | 59.4‐92.4 |
| Living alone (%) | 33.9 | 36.2 | 37.6 | 40.4 | 37.0 |
| Educationd | |||||
| Low level (%) | 25.3 | 38.9*** | 32.8 | 33.9* | 35.5** |
| Intermediate level (%) | 61.3 | 54.6 | 59.5 | 53.3 | 55.6 |
| High level (%) | 13.4 | 6.5 | 7.8 | 12.7 | 8.9 |
| Marital Statusd | |||||
| Married (%) | 64.2 | 61.5 | 61.6 | 57.8* | 61.3 |
| Single (%) | 5.1 | 3.6 | 4.0 | 12.7 | 3.9 |
| Widowed (%) | 24.0 | 26.2 | 26.4 | 24.7 | 25.4 |
| Divorced (%) | 6.7 | 8.6 | 8.0 | 4.8 | 9.4 |
| Disability | |||||
| Functional: mild to severe (%) | 40.2 | 62.4*** | 62.3*** | 61.8*** | 61.5*** |
| Instrumental: mild to severe (%) | 24.6 | 27.4 | 34.4* | 30.9 | 29.1* |
| Physical health | |||||
| Coronary heart disease (%) | 6.2 | 4.5 | 5.6 | 6.0 | 5.0 |
| Diabetes Mellitus (%) | 17.1 | 14.5 | 13.7 | 17.5 | 14.7 |
| MMSE | |||||
| Impaired cognitive capacity (%) | 13.5 | 15.2 | 25.0** | 18.7 | 18.4** |
The population described in this table comprises the total study population.
Agoraphobia, generalized anxiety disorder (GAD) and other anxiety disorders represent non‐exclusive categories.
Other anxiety disorders comprise social phobia, specific phobia and panic disorder.
Overall test of significance was performed.
Note: Anxiety disorder groups were compared to the group without anxiety disorders with t‐tests and chi‐square tests. MMSE, Mini Mental State Examination.
*p < 0.05; **p < 0.01; ***p < 0.001.
Table 2 shows the comorbidity of current anxiety with current depression. Of the persons with a current anxiety disorder, 17.9% had a comorbid depression. In contrast, 2.8% of the persons without anxiety disorder had a current depression (adjusted odds ratio for depression in persons with anxiety: 7.0, 95% confidence interval (CI) 5.2–9.5). Next, we stratified the group of anxiety disorders into the following anxiety subtypes: GAD, agoraphobia, social phobia, specific phobia and panic disorder. Persons with GAD most often had a comorbid depression (40.8%), followed by persons with social phobia (25.8%). Persons with specific phobia least often had a comorbid depression (9.5%). Comorbidity estimates are also presented per age group in Table 2. The oldest age group included more anxiety cases with comorbid depression than the youngest age group [chi‐square test (χ 2) = 5.5, df = 1, p = 0.019].
Table 2.
Current anxiety disorders and depression comorbiditya
| No current depression n (%) | Current depressionb n (%) | |
|---|---|---|
| No anxiety disorder (n = 5108) | 4966 (97.2) | 142 (2.8) |
| All anxiety disorders (n = 457) | 375 (82.1) | 82 (17.9)*** |
| GAD (n = 125)c | 74 (59.2) | 51 (40.8)*** |
| Agoraphobia (n = 221)c | 194 (87.8) | 27 (12.2)*** |
| Other anxiety disorders (n = 166)c, d | 141 (84.9) | 25 (15.1)*** |
| Social phobia (n = 62)c | 46 (74.2) | 16 (25.8)*** |
| Specific phobia (n = 84)c | 76 (90.5) | 8 (9.5)** |
| Panic disorder (n = 30)c | 27 (90.0) | 3 (10.0) |
| Stratified by age | ||
| Age 58–70, n = 2343 | ||
| No anxiety disorder (n = 2144) | 2102 (98.0) | 42 (2.0) |
| All anxiety disorders (n = 199) | 170 (85.4) | 29 (14.6)*** |
| GAD (n = 56)c. | 35 (62.5) | 21 (37.5)*** |
| Agoraphobia (n = 84)c. | 77 (91.7) | 7 (8.3)** |
| Other anxiety disorders (n = 82)c., d. | 70 (85.4) | 12 (14.6)*** |
| Age 70–80, n = 2165 | ||
| No anxiety disorder (n = 1986) | 1931 (97.2) | 55 (2.8) |
| All anxiety disorders (n = 179) | 147 (82.1) | 32 (17.9)*** |
| GAD (n = 43)c | 27 (62.8) | 16 (37.2)*** |
| Agoraphobia (n = 95)c. | 84 (88.4) | 11 (11.6)*** |
| Other anxiety disorders (n = 62)c.,d. | 51 (82.3) | 11 (17.7)*** |
| Age 80–100, n = 1057 e | ||
| No anxiety disorder (n = 978) | 933 (95.4) | 45 (4.6) |
| All anxiety disorders (n = 79) | 58 (73.4) | 21 (26.6)*** |
| GAD (n = 26)c. | 12 (46.2) | 14 (53.8)*** |
| Agoraphobia (n = 42)c. | 33 (78.6) | 9 (21.4)*** |
| Other anxiety disorders (n = 22)c, d | 20 (90.9) | 2 (9.1) |
These numbers were based on the total study population (n = 5565).
Current depression as assessed with the Schedules for Clinical Assessment of Neuropsychiatry (SCAN) interview.
Generalized Anxiety Disorder (GAD), agoraphobia and other anxiety disorders represent non‐exclusive categories.
Other anxiety disorders comprised social phobia, specific phobia and panic disorder.
The age 80–100 group comprised significantly more comorbid depression cases than the youngest age group (p = 0.019 as tested with a chi‐square test).
Note: Anxiety categories were compared to the category without anxiety disorders with chi‐square tests or Fisher exact tests.
*p < 0.05; **p < 0.01; ***p < 0.001.
Comorbidity of anxiety and depression increased to 20.8% if we included all depressions established in the year before anxiety assessment. Including all depressions detected in the two years before anxiety assessment further increased this estimate of comorbidity to 22.1%.
For comparison with other studies, we also estimated comorbidity for major depression defined by DSM‐IV criteria. Of the persons with anxiety disorder 11.6% had a comorbid major depression, but only 1.3% of persons without anxiety had a major depression (adjusted odds ratio 8.9, 95% CI 6.0–13.1). Persons with GAD most often had a comorbid major depression (27.2%), followed by persons with social phobia (17.7%).
Table 3 shows the relation of current anxiety disorders and depression including past episodes of depression. Of the persons with an anxiety disorder 49.3% had a past depression, compared to 25.2% of persons without anxiety disorder (adjusted odds ratio 2.5, 95% CI 2.0‐3.1, Table 4). Persons with GAD and social phobia most often had a current or past depression (68.3% and 66.7% respectively).
Table 3.
Comorbidity between current anxiety and all depressions during follow‐upa
| No depression n (%) | Current or past depression n (%)b | ||
|---|---|---|---|
| No anxiety disorder (n = 5108) | 2190 (74.8) | 736 (25.2) | |
| All anxiety disorders (n = 448) | 227 (50.7) | 221 (49.3)*** | |
| GAD (n =120)c | 38 (31.7) | 82 (68.3)*** | |
| Agoraphobia (n = 218)c | 122 (56.0) | 96 (44.0)*** | |
| Other anxiety disorders (n = 164)c, d | 83 (50.6) | 81 (49.4)*** | |
| Social phobia (n = 60)c | 20 (33.3) | 40 (66.7)*** | |
| Specific phobia (n = 84)c | 49 (58.3) | 35 (41.7)*** | |
| Panic disorder (n = 30)c | 15 (50.0) | 15 (50.0)*** | |
| Stratified by age | |||
| Age 59–70, n = 815 | |||
| No anxiety disorder (n = 620) | 457 (73.7) | 163 (26.3) | |
| All anxiety disorders (n = 195) | 106 (54.4) | 89 (45.6)*** | |
| GAD (n = 54)c | 24 (44.4) | 30 (55.6)*** | |
| Agoraphobia (n = 83)c | 51 (61.4) | 32 (38.6)* | |
| Other anxiety disorders (n = 81)c, d | 40 (49.4) | 41 (50.6)*** | |
| Age 70–80, n = 1740 | |||
| No anxiety disorder (n = 1563) | 1157 (74.0) | 406 (26.0) | |
| All anxiety disorders (n = 177) | 85 (48.0) | 92 (52.0)*** | |
| GAD (n = 42)c. | 6 (14.3) | 36 (85.7)*** | |
| Agoraphobia (n = 94)c. | 50 (53.2) | 44 (46.8)*** | |
| Other anxiety disorders (n = 61)c, d | 31 (50.8) | 30 (49.2)*** | |
| Age 80–98, n = 819 | |||
| No anxiety disorder (n = 743) | 576 (77.5) | 167 (22.5) | |
| All anxiety disorders (n = 76) | 36 (47.4) | 40 (52.6)*** | |
| GAD (n = 24)c | 8 (33.3) | 16 (66.7)*** | |
| Agoraphobia (n = 41)c | 21 (51.2) | 20 (48.8)*** | |
| Other anxiety disorders (n = 22)c, d | 12 (54.2) | 10 (45.5)* | |
These numbers were based on the selective sample of n = 3374.
Current depression as assessed with the Schedules for Clinical Assessment of Neuropsychiatry (SCAN) interview and past depression as assessed by a clinical interview (SCAN), self‐report and continuous general practitioner (GP) record monitoring.
Generalized anxiety disorder (GAD), agoraphobia and other anxiety disorders represent non‐exclusive categories.
Other anxiety disorders comprised social phobia, specific phobia and panic disorder.
Note: Anxiety categories were compared to the category without anxiety disorders with chi‐square tests.
*p < 0.05; **p < 0.01; ***p < 0.001.
Table 4.
Association of anxiety with current and past depressiona
| Current depressionb | Current or past depressionc | |||
|---|---|---|---|---|
| n | OR (95% CI) | n | OR (95% CI) | |
| No anxiety | 5015 | Ref | 2890 | Ref |
| All anxiety | 448 | 7.0 (5.2–9.5) | 439 | 2.5 (2.0–3.1) |
| GAD | 121 | 22.1 (14.6–33.5) | 116 | 5.5 (3.7–8.3) |
| Agoraphobia | 216 | 4.4 (2.8–6.8) | 213 | 2.0 (1.5–2.8) |
| Other anxiety disordersd | 165 | 5.7 (3.6–9.2) | 163 | 2.3 (1.7–3.2) |
Complete case logistic regressions were performed. Analyses were adjusted for age, gender, education, living alone, and cognitive status.
Analyses were performed on the total study population of n = 5565.
Analyses were performed on the selected sample of n = 3374.
The category “Other anxiety disorders” comprised social phobia, specific phobia and panic disorder. Separate ORs were not calculated because of low numbers.
Note: OR, odds ratio; CI, confidence interval; GAD, generalized anxiety disorder.
Discussion
In this population‐based study of older adults, 18% of persons with a current anxiety disorder had a comorbid depression. Another one‐third had experienced depression in the past. Only about half of the persons with an anxiety disorder had never experienced depression.
Some studies observed similar comorbidity estimates, but many reported higher rates of comorbidity (Kvaal et al., 2008; Cairney et al., 2008; Beekman et al., 2000). This is despite the fact that previous studies generally applied a more stringent categorization of depression. In the current study, we estimated comorbidity of anxiety disorders with depressive syndromes (major depression, dysthymia and minor depression), whereas most previous research focussed on comorbid major depression only. Comorbidity of major depression with anxiety disorder in the current study was only 11.6%, which is lower than observed in other studies.
Several explanations for this discrepancy are conceivable. First, some studies in older adults did not apply DSM‐criteria to diagnose depressive disorders, but used GMS‐AGECAT, a case definition specifically designed for older adults. GMS‐AGECAT has been shown to identify more depressive cases than instruments applying DSM‐IV criteria (Newman et al., 1998). Indeed, the prevalence of depression in the study of Kvaal et al. (2008, 9.7%) who applied the GMS‐AGECAT system was much higher than the depressive syndrome prevalence in our study (4.1%). At the same time, the anxiety prevalence was much lower than in our study (3.1% versus 8.2%). Low anxiety prevalence in combination with high depression prevalence may account for the high observed comorbidity of 65% anxiety with depressive syndromes found in the study of Kvaal et al. (2008). Similarly, in the AMSTEL study, Schoevers et al. (2003) also applied the GMS‐AGECAT system and observed a depression prevalence of 12.9%. Not surprisingly, they found that as much as 60% of GAD cases had a comorbid depression. Most likely, the high comorbidity in these studies can be partly attributed to the diagnostic system used.
Second, differences in comorbidity estimates between studies may be explained by variation in the time frame of ascertainment. Most studies reported a one‐year prevalence of anxiety and depression (Cairney et al., 2008; King‐Kallimanis et al., 2009), and in some studies point prevalence was measured (Ritchie et al., 2004; Kvaal et al., 2008). An example of the latter is the ESPRIT study, Ritchie et al. (2004) reported a one‐month prevalence of anxiety and a 15‐day prevalence of depression. This may explain the low comorbidity between anxiety and depression observed in this cohort (12%). In the current study, to best assess point prevalence, we primarily reported the one‐year prevalence for anxiety disorders and the one‐month prevalence for depression and for GAD. Although these disorders are generally chronic (Beekman et al., 2002; Schuurmans et al., 2005), this may have contributed to the relatively low comorbidity estimate we observed. Comorbidity increased only slightly if we accounted for depressions detected in the one or two years before anxiety assessment. To estimate one‐year prevalence of depression we used multiple additional sources other than the SCAN interview. Also, for some extreme cases, depression assessment was two months after anxiety assessment. However, median time between depression and anxiety assessment was two weeks. Furthermore, both anxiety and depression in older persons are, as mentioned earlier, relatively chronic disorders. We therefore expect this time lag to hardly affect our comorbidity estimates.
Third, the studies described previously were, like the current study, population‐based studies of older adults. However, sample size varied. The study by Heun et al. (2000) for example, was a particularly small study, in which only 19 cases with anxiety disorder were identified. The study by Kvaal et al. (2008) included less than 100 persons with anxiety disorder. The estimates of comorbidity from these studies may not be very precise. A small sample size may further increase the between‐study‐variability in observed comorbidity. Cairney et al. (2008), Schoevers et al. (2003) and the current study report more precise estimates based on large studies with many cases of anxiety disorder.
Fourth, unlike the commonly used World Health Organization (WHO)‐CIDI, a structured interview performed by lay interviewers (Brugha et al., 2001), we used the semi‐structured SCAN interview conducted by clinicians to diagnose depression. Scoring of the SCAN interview does not rely on the participant's answers only, but also on the clinician's judgement. Structured lay interviews like the CIDI generally identify more cases than clinical interviews like the SCAN (Brugha et al., 2001; Haro et al., 2006). This most likely reduced comorbidity of depression with anxiety in our study if compared to studies using the CIDI. In addition, the SCAN and the CIDI were designed for use in adults, not specifically for older adults. This might limit reliability and validity of the diagnosis in this older age group. However, both the CIDI and the SCAN have been used previously to diagnose anxiety and depression in older adults (Cairney et al., 2008; Van den Berg et al., 2000).
Finally, most studies used the same instrument to diagnose anxiety and depression. If disorders are assessed with one measurement instrument and during one session, comorbidity may be diagnosed more frequently than if assessed by different instruments or in different situations. This “common method variance” can artificially increase the observed comorbidity between anxiety and depression (Podsakoff et al., 2003). To control the effect of common method variance, we diagnosed anxiety with the CIDI and depression with the SCAN and we conducted the interviews on different days. Merely using two different instruments on the same day, or the same instrument on different days to diagnose anxiety and depression might not be sufficient to abolish one of the causes of common method variance; the consistency effect (Podsakoff et al., 2003). The ESPRIT study (Ritchie et al., 2004) used the same instrument to assess both anxiety and depression, but in addition, a team of psychiatrists and psychologists also considered medical history, medication use and neurological assessment. This design also reduced common method variance. Notably, the ESPRIT study and the present study reported a relatively low comorbidity between anxiety and depression compared to studies using the same instrument to diagnose anxiety and depression.
To assess anxiety and depression with the same and with different instruments during one assessment round would have enabled us to estimate the extent of this common method variance. In the current study we did not assess anxiety with SCAN or depression with CIDI. Our primary aim was to estimate the comorbidity without inflation by this potential problem to give an indication of its possible extent.
An additional observation in the current study was the relatively high prevalence of low MMSE levels in participants with GAD. This may reflect an underlying etiological process. Cognitive impairment can increase the likelihood that stressful circumstances or events result in continued worries or anxiousness. Response bias due to cognitive impairment cannot be ruled out either (Knauper and Wittchen, 1994).
In the present study we examined prior depressions in persons with current anxiety disorders. Unlike most other studies assessing depression over longer periods of time, we did not depend on retrospective depression self‐report only. Prior episodes of depression were detected by continuous monitoring of GP‐records over a mean period of nine years, a previous interview round and previous depression self‐report. Combining multiple sources of retrospective and prospective ascertainment of past depression may reduce ascertainment bias often seen in other studies (Moffitt et al., 2009).
Continuous monitoring was, however, performed for most but not for the entire cohort. The original cohort was continuously monitored, whereas in the additional cohort persons without anxiety were not monitored. This selective sampling had some consequences for analyses on past depression. To overcome potential bias, we adjusted analyses for age and gender. In addition, we presented analyses stratified by age. These stratified analyses suggest that selection on age does not have a large effect on our results.
Half of all persons with an anxiety disorder had never experienced any depressive syndromes. Hence, in a substantial number of cases, pure anxiety disorders occurred. We observed few persons with pure GAD. In other studies GAD was also found to be highly comorbid with depression, whereas for example specific phobia and agoraphobia are known to be less comorbid with depression (King‐Kallimanis et al., 2009; Cairney et al., 2008).
Although comorbidity between current anxiety and depression was lower than observed in other studies of older adults, half of all persons with an anxiety disorder had had depression in their history. This suggests a common vulnerability for the two disorders. Kendler et al. (2003) demonstrated in a twin study that this vulnerability may comprise common genetic factors for anxiety and depression. A shared vulnerability might not necessarily lead to high comorbidity at one moment, but rather to an increased risk of any of the two disorders during life as observed in the current study. Environmental risk factors in susceptible persons may then determine which disorder will occur at a specific point in time (Kendler et al., 2003).
An alternative explanation for the high comorbidity between the two disorders is that anxiety disorders increase the risk for developing depression. Anxiety disorders other than GAD are generally thought to have an onset early in life during childhood and adolescence, whereas the onset of depression is mostly during adulthood (Merikangas et al., 1996; Regier et al., 1998). Indeed, several longitudinal studies reported that anxiety precedes depression (Wittchen et al., 2000; Bittner et al., 2004). However, the reverse was also observed (Merikangas et al., 2003; Pine et al., 1998). Whether anxiety and depression arise from the same diathesis or are risk factors for each other might differ per subtype of anxiety disorder.
In conclusion, our study implies that current comorbid depression in older adults with anxiety disorders may often be overestimated and less common than previously suggested. However, if past depression is taken into account, most persons with anxiety will have experienced depression.
Declaration of interest statement
The authors have no competing interests.
Acknowledgements
The Rotterdam Study is funded by the Erasmus Medical Centre and Erasmus University, Rotterdam; Netherlands Organization for the Health Research and Development (ZonMw); the Research Institute for Diseases in the Elderly (RIDE and RIDE2); the Ministry of Education, Culture and Science; the Ministry for Health, Welfare and Sports; the European Commission (DG XII); the Municipality of Rotterdam; and the Netherlands Genomics Initiative/Netherlands Organisation for Scientific Research project number 050‐060‐810. H. Tiemeier was supported by the VIDI grant of ZonMw (2009–017.106.370). R.S. Newson was supported by a post‐doctoral grant on healthy ageing from Unilever Corporate Research, UK. The funders had no role in the study design, data collection or data analysis.
We thank all persons involved in data collection of the Rotterdam Study and all participants for their valuable contributions to this study.
References
- American Diabetes Association (1997) Clinical practice recommendations 1997. Diabetes Care, 20(Suppl. 1), S1–70. [PubMed] [Google Scholar]
- Ayers C.R., Sorrell J.T., Thorp S.R., Wetherell J. L. (2007) Evidence‐based psychological treatments for late‐life anxiety. Psychological Aging, 22(1), 8–17. [DOI] [PubMed] [Google Scholar]
- Beekman A.T., Bremmer M.A., Deeg D.J., van Balkom A.J., Smit J.H., de Beurs E., van Dyck R., van Tilburg W. (1998) Anxiety disorders in later life: A report from the Longitudinal Aging Study Amsterdam. International Journal of Geriatric Psychiatry, 13(10), 717–726. [DOI] [PubMed] [Google Scholar]
- Beekman A.T., de Beurs E., van Balkom A.J., Deeg D.J., van Dyck R., van Tilburg W. (2000) Anxiety and depression in later life: Co‐occurrence and communality of risk factors. The American Journal of Psychiatry, 157(1), 89–95. [DOI] [PubMed] [Google Scholar]
- Beekman A.T., Deeg D.J., Van Limbeek J., Braam A.W., De Vries M.Z., Van Tilburg W. (1997) Criterion validity of the Center for Epidemiologic Studies Depression scale (CES‐D): Results from a community‐based sample of older subjects in the Netherlands. Psychological Medicine, 27(1), 231–235. [DOI] [PubMed] [Google Scholar]
- Beekman A.T., Geerlings S.W., Deeg D.J., Smit J.H., Schoevers R.S., de Beurs E., Braam A.W., Penninx B.W., van Tilburg W. (2002) The natural history of late‐life depression: A 6‐year prospective study in the community. Archives of General Psychiatry, 59(7), 605–611. [DOI] [PubMed] [Google Scholar]
- Bittner A., Goodwin R.D., Wittchen H.U., Beesdo K., Hofler M., Lieb R. (2004) What characteristics of primary anxiety disorders predict subsequent major depressive disorder? The Journal of Clinical Psychiatry, 65(5), 618–626, quiz 730. [DOI] [PubMed] [Google Scholar]
- Brugha T.S., Jenkins R., Taub N., Meltzer H., Bebbington P.E. (2001) A general population comparison of the Composite International Diagnostic Interview (CIDI) and the Schedules for Clinical Assessment in Neuropsychiatry (SCAN). Psychological Medicine, 31(6), 1001–1013. [DOI] [PubMed] [Google Scholar]
- Bryant C., Jackson H., Ames D. (2008) The prevalence of anxiety in older adults: Methodological issues and a review of the literature. Journal of Affective Disorders, 109(3), 233–250. [DOI] [PubMed] [Google Scholar]
- Cairney J., Corna L.M., Veldhuizen S., Herrmann N., Streiner D.L. (2008) Comorbid depression and anxiety in later life: Patterns of association, subjective well‐being, and impairment. The American Journal of Geriatric Psychiatry, 16(3), 201–208. [DOI] [PubMed] [Google Scholar]
- de Beurs E., Beekman A.T., van Balkom A.J., Deeg D.J., van Dyck R., van Tilburg W. (1999) Consequences of anxiety in older persons: Its effect on disability, well‐being and use of health services. Psychological Medicine, 29(3), 583–593. [DOI] [PubMed] [Google Scholar]
- Folstein M.F., Folstein S.E., McHugh P.R. (1975) “Mini‐mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. [DOI] [PubMed] [Google Scholar]
- Fries J.F., Spitz P.W., Young D.Y. (1982) The dimensions of health outcomes: The health assessment questionnaire, disability and pain scales. Journal of Rheumatology, 9(5), 789–793. [PubMed] [Google Scholar]
- Haro J.M., Arbabzadeh‐Bouchez S., Brugha T.S., de Girolamo G., Guyer M.E., Jin R., Lepine J.P., Mazzi F., Reneses B., Vilagut G., Sampson N.A., Kessler R.C. (2006) Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. International Journal of Methods in Psychiatric Research, 15(4), 167–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heun R., Papassotiropoulos A., Ptok U. (2000) Subthreshold depressive and anxiety disorders in the elderly. European Psychiatry, 15(3), 173–182. [DOI] [PubMed] [Google Scholar]
- Hofman A., Breteler M.M., van Duijn C.M., Janssen H.L., Krestin G.P., Kuipers E.J., Stricker B.H., Tiemeier H., Uitterlinden A.G., Vingerling J.R., Witteman J.C. (2009) The Rotterdam Study: 2010 objectives and design update. European Journal of Epidemiology, 24(9), 553–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofman A., Breteler M.M., van Duijn C.M., Krestin G.P., Pols H.A., Stricker B.H., Tiemeier H., Uitterlinden A.G., Vingerling J.R., Witteman J.C. (2007) The Rotterdam Study: objectives and design update. European Journal of Epidemiology, 22(11), 819–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Prescott C.A., Myers J., Neale M.C. (2003) The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry, 60(9), 929–937. [DOI] [PubMed] [Google Scholar]
- King‐Kallimanis B., Gum A.M., Kohn R. (2009) Comorbidity of depressive and anxiety disorders for older Americans in the national comorbidity survey‐replication. The American Journal of Geriatric Psychiatry, 17(9), 782–792. [DOI] [PubMed] [Google Scholar]
- Knauper B., Wittchen H.U. (1994) Diagnosing major depression in the elderly: Evidence for response bias in standardized diagnostic interviews? Journal of Psychiatric Research, 28(2), 147–164. [DOI] [PubMed] [Google Scholar]
- Kvaal K., McDougall F.A., Brayne C., Matthews F.E., Dewey M.E., Mrc C. (2008) Co‐occurrence of anxiety and depressive disorders in a community sample of older people: results from the MRC CFAS (Medical Research Council Cognitive Function and Ageing Study). International Journal of Geriatric Psychiatry, 23(3), 229–237. [DOI] [PubMed] [Google Scholar]
- Lawton M.P., Brody E.M. (1969) Assessment of older people: Self‐maintaining and instrumental activities of daily living. Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Lenze E.J., Mulsant B.H., Mohlman J., Shear M.K., Dew M.A., Schulz R., Miller M.D., Tracey B., Reynolds C.F. 3rd (2005) Generalized anxiety disorder in late life: Lifetime course and comorbidity with major depressive disorder. The American Journal of Geriatric Psychiatry, 13(1), 77–80. [DOI] [PubMed] [Google Scholar]
- Luijendijk H.J., van den Berg J.F., Dekker M.J., van Tuijl H.R., Otte W., Smit F., Hofman A., Stricker B.H., Tiemeier H. (2008) Incidence and recurrence of late‐life depression. Archives of General Psychiatry, 65(12), 1394–1401. [DOI] [PubMed] [Google Scholar]
- Mattace‐Raso F.U., van der Cammen T.J., Hofman A., van Popele N.M., Bos M.L., Schalekamp M.A., Asmar R., Reneman R.S., Hoeks A.P., Breteler M.M., Witteman J.C. (2006) Arterial stiffness and risk of coronary heart disease and stroke: The Rotterdam Study. Circulation, 113(5), 657–663. [DOI] [PubMed] [Google Scholar]
- McGuire W.J. (1966) Attitudes and opinions. Annual Review of Psychology, 17, 475–514. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., Angst J., Eaton W., Canino G., Rubio‐Stipec M., Wacker H., Wittchen H. U., Andrade L., Essau C., Whitaker A., Kraemer H., Robins L.N., Kupfer D.J. (1996) Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: Results of an international task force. The British Journal of Psychiatry. Supplement, (30), 58–67. [PubMed] [Google Scholar]
- Merikangas K.R., Zhang H., Avenevoli S., Acharyya S., Neuenschwander M., Angst J. (2003) Longitudinal trajectories of depression and anxiety in a prospective community study: The Zurich Cohort Study. Archives of General Psychiatry, 60(10), 993–1000. [DOI] [PubMed] [Google Scholar]
- Moffitt T.E., Caspi A., Taylor A., Kokaua J., Milne B.J., Polanczyk G., Poulton R. (2009) How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40(6), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman S.C., Sheldon C.T., Bland R.C. (1998) Prevalence of depression in an elderly community sample: A comparison of GMS‐AGECAT and DSM‐IV diagnostic criteria. Psychological Medicine, 28(6), 1339–1345. [DOI] [PubMed] [Google Scholar]
- Pine D.S., Cohen P., Gurley D., Brook J., Ma Y. (1998) The risk for early‐adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry, 55(1), 56–64. [DOI] [PubMed] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Lee J.Y., Podsakoff N.P. (2003) Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903. [DOI] [PubMed] [Google Scholar]
- Radloff L. (1977) The CES‐D Scale: A Self‐report Depression Scale for Research in the General Population. Applied Pyschological Measurement, 1(3), 385–401. [Google Scholar]
- Regier D.A., Rae D.S., Narrow W.E., Kaelber C.T., Schatzberg A.F. (1998) Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. The British Journal of Psychiatry. Supplement, (34), 24–28. [PubMed] [Google Scholar]
- Ritchie K., Artero S., Beluche I., Ancelin M.L., Mann A., Dupuy A.M., Malafosse A., Boulenger J.P. (2004) Prevalence of DSM‐IV psychiatric disorder in the French elderly population. The British Journal of Psychiatry, 184, 147–152. [DOI] [PubMed] [Google Scholar]
- Schoevers R.A., Beekman A.T., Deeg D.J., Jonker C., van Tilburg W. (2003) Comorbidity and risk‐patterns of depression, generalised anxiety disorder and mixed anxiety‐depression in later life: Results from the AMSTEL study. International Journal of Geriatric Psychiatry, 18(11), 994–1001. [DOI] [PubMed] [Google Scholar]
- Schuurmans J., Comijs H.C., Beekman A.T., de Beurs E., Deeg D.J., Emmelkamp P.M., van Dyck R. (2005) The outcome of anxiety disorders in older people at 6‐year follow‐up: Results from the Longitudinal Aging Study Amsterdam. Acta Psychiatrica Scandinavica, 111(6), 420–428. [DOI] [PubMed] [Google Scholar]
- Seeman T.E., Berkman L.F., Charpentier P.A., Blazer D.G., Albert M.S., Tinetti M.E. (1995) Behavioral and psychosocial predictors of physical performance: MacArthur studies of successful aging. Journal of Gerontology Series A: Biological Sciences & Medical Science, 50(4), M177–183. [DOI] [PubMed] [Google Scholar]
- Van den Berg M.D., Oldehinkel A.J., Brilman E.I., Bouhuys A.L., Ormel J. (2000) Correlates of symptomatic, minor and major depression in the elderly. Journal of Affective Disorders, 60(2), 87–95. [DOI] [PubMed] [Google Scholar]
- Van Hout H.P., Beekman A.T., de Beurs E., Comijs H., van Marwijk H., de Haan M., van Tilburg W., Deeg D.J. (2004) Anxiety and the risk of death in older men and women. The British Journal of Psychiatry, 185, 399–404. [DOI] [PubMed] [Google Scholar]
- Vink D., Aartsen M.J., Schoevers R.A. (2008) Risk factors for anxiety and depression in the elderly: A review. Journal of Affective Disorders, 106(1–2), 29–44. [DOI] [PubMed] [Google Scholar]
- Weisberg R.B. (2009) Overview of generalized anxiety disorder: Epidemiology, presentation, and course. The Journal of Clinical Psychiatry, 70 Suppl. 2, 4–9. [PubMed] [Google Scholar]
- Wing J.K., Babor T., Brugha T., Burke J., Cooper J.E., Giel R., Jablenski A., Regier D., Sartorius N. (1990) SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Archives of General Psychiatry, 47(6), 589–593. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Kessler R.C., Pfister H., Lieb M. (2000) Why do people with anxiety disorders become depressed? A prospective‐longitudinal community study. Acta Psychiatrica Scandinavica, Supplement, (406), 14–23. [PubMed] [Google Scholar]
- Wittchen H.U., Lachner G., Wunderlich U., Pfister H. (1998) Test–retest reliability of the computerized DSM‐IV version of the Munich‐Composite International Diagnostic Interview (M‐CIDI). Social Psychiatry and Psychiatric Epidemiology, 33(11), 568–578. [DOI] [PubMed] [Google Scholar]


