Abstract
Background:
Enhanced recovery (ER) protocols are increasingly being utilized in surgical practice. Outside of colorectal surgery, however, their feasibility, safety, and efficacy in major oncologic surgery have not been proven. This study compared patient outcomes before and after multispecialty implementation of ER protocols at a large comprehensive cancer center.
Methods:
Surgical cases performed from 2011–2016 and captured by an institutional NSQIP database were reviewed. Following exclusion of outpatient and emergent surgeries, 2747 cases were included in the analyses. Cases were stratified by presence or absence of ER compliance, defined by preoperative patient education and electronic medical record order set-driven opioid-sparing analgesia, goal-directed fluid therapy, and early postoperative diet advancement and ambulation.
Results:
Approximately half of patients were treated on ER protocols (46%) and the remaining on traditional postoperative (TP) protocols (54%). Treatment on an ER protocol was associated with decreased overall complication rates (20% vs. 33%, p <0.0001), severe complication rates (7.4% vs. 10%, p=0.010), and median hospital length of stay (4 vs. 5 days, p <0.0001). There was no change in readmission rates (ER vs. TP, 8.6% vs. 9.0%, p=0.701). Sub-analyses of high magnitude cases and specialty-specific outcomes consistently demonstrated improved outcomes with ER protocol adherence, including decreased opioid use.
Conclusions:
This assessment of a large-scale ER implementation in multispecialty major oncologic surgery indicates its feasibility, safety, and efficacy. Future efforts should be directed toward defining the long-term oncologic benefits of these protocols.
INTRODUCTION
For several decades fast-track and enhanced recovery (ER) surgical protocols have been described, mainly by European centers.[1] More recently, the concept of ER has been integrated into surgical practice in North America, resulting in a paradigm shift in perioperative care. ER is a multimodality approach to patient care that is implemented by a multidisciplinary team. The driving principle behind these evidence-based care pathways is that by reducing stress associated with surgery, patients are able to recover more rapidly and completely, thereby minimizing complications and delays in further treatment.[1, 2] As ER has been incorporated into more surgical specialties, data are rapidly accumulating that demonstrate the benefits of ER protocols on patient outcomes. These benefits include reduced postoperative complications and inpatient length of stay (LOS).[3–8] As personalized care and precision medicine have become increasingly importantly concepts, studies examining more patient-centric, long-term outcomes reflecting functional recovery are also being reported.[9–11]
Despite this revolution in perioperative care, much of the ER literature focuses on the impact of ER on patients undergoing non-oncologic procedures.[6, 8, 12] When oncologic patients are described, they often have early-stage disease amenable to less invasive surgical intervention.[13, 14] As colorectal surgeons were amongst the earliest to incorporate ER into their practice, the largest amount of oncologic data on ER exists in this patient cohort. However, the majority of oncologic specialties are underrepresented in the ER literature.[15–18] In order to address this knowledge gap, we assessed the impact of ER implementation on patient outcomes across multiple oncologic surgical specialties at a large comprehensive cancer center.
METHODS
Defining ‘Enhanced Recovery’ protocols
ER protocol implementation began in 2012 with a phased roll-out performed across disease sites and surgical specialties over a three-year period. Surgical specialties included in the analyses were Colorectal, Gynecology, Hepatobiliary, Thoracic, and Urology. Each service area program was formed around a multidisciplinary team that included surgery, anesthesia, nursing, pharmacy, nutrition, rehabilitation services, and informatics support. Provider education regarding the core components of ER was supplemented by presentations at regularly scheduled CME meetings, surgical service orientations, and other didactics. For the purpose of this study, ER protocol compliance was defined as patient care that included preoperative patient education on ER and use of both pre- and postoperative ordersets in the institutional electronic medical record that incorporated the four pillars of ER: multimodal opioid-sparing analgesia, goal-directed fluid therapy, early feeding, and early ambulation [1, 2, 19].
Patient education was carried out by providers and nursing staff at preoperative clinic visits. Patients received education on both the indicated operation and on ER principles and goals, with the objectives of reducing anxiety by transparently sharing plans of care and setting patient expectations regarding their perioperative experiences.[2, 19] For opioid-sparing multimodal analgesia, although each service had latitude to select the exact components, all used some combination of regional anesthetic options (e.g., epidural and transverse abdominus plane [TAP] blocks) with acetaminophen, non-steroidal anti-inflammatories, and non-narcotic neuromodulators. Goal-directed fluid therapy, performed both intraoperatively and postoperatively, involved titrating the amount of fluid being administered based on hemodynamic indices, low maintenance fluid rates, early discontinuance with per oral intake, and data-driven bolus strategies.[19, 20] Early feeding was built into ordersets, begun in most cases on post-operative day 0, and programmatically advanced to regular diet. Early ambulation was likewise hard-wired into ordersets and initiated in most cases on the day of surgery.[21–28]
National Surgical Quality Improvement Program (NSQIP) analysis
This study was approved by the University of Texas MD Anderson Cancer Center IRB and performed in compliance with the NSQIP data use agreement. For the entire duration of the study the center participated in the Essentials data collection model, capturing approximately 14% of the surgical volume across all specialties. Patient data were obtained from the institutional American College of Surgeons (ACS)-NSQIP database from January 2011 to December 2016 for the following surgical specialties: Colorectal, Gynecology, Hepatobiliary, Thoracic, and Urology. Both open and minimally-invasive surgical cases were included in the analyses, but all outpatient and emergent cases were excluded. For patients undergoing surgeries involving more than one surgical team, the operation was classified by the primary team’s specialty. The date of ER protocol initiation was determined for each specialty, and the cases from each specialty were subsequently divided into two cohorts: those treated on ER versus TP protocols.
Variable collection was performed by Surgical Clinical Reviewers trained in the analysis of medical records and audited by the ACS. Demographic and clinical information, operative details, and 30-day outcomes were included in the analyses. Age, American Society of Anesthesiologists (ASA) classification, preoperative functional status (defined as independent if assistance from another person for any activities of daily living was not required versus dependent if some or total assistance was required), and preoperative comorbidities were compared between patients treated on ER and TP protocols.[29] Wound class, operative time, and hospital length of stay (LOS) were assessed. Postoperative complications, as defined by the NSQIP Participant Use Data File, were compared between ER and TP cohorts and included wound infection, pneumonia, pulmonary embolism, urinary tract infection, renal failure, myocardial infarction, cardiac arrest, stroke, sepsis, and unplanned return to the operating room. A severe complication was defined per prior publications as having one or more of the following: organ space infection, wound dehiscence, pneumonia, unplanned intubation, acute renal failure, myocardial infarction, sepsis, septic shock, or unplanned return to the operating room.[10] 30-day readmission and mortality rates were also compared. Mortalities that occurred during a continuous postoperative admission lasting longer than 30 days were also included. Before implementation, throughout the study period, and after implementation, NSQIP patient outcomes reports were shared with each team and associated frontline providers. Likewise, individual teams internally reported their general and specialty-specific outcomes from existing department-level databases.
Analysis of high magnitude surgeries
A sub-analysis was performed to assess the effects of implementation of ER protocols on patients undergoing high-magnitude surgery. Case magnitude was determined by primary CPT RVU, and cases with RVU >30 were considered high magnitude. All variables included in the complete ER versus TP cohort analyses were also assessed in this sub-analysis.
Statistics
Statistical analyses were performed using JMP Pro software program (Version 12, SAS institute Inc., Cary, NC). Univariate analyses were performed using chi-square or Fisher’s exact test for categorical variables and the Mann-Whitney U test for continuous variables. Continuous variables are reported as median values and interquartile ranges. A two-tailed univariate p <0.05 was considered significant.
RESULTS
Study population demographics and clinical profile
A total of 2747 patients entered into the institutional NSQIP database between January 2011 and December 2016 were included in the analyses (Supplementary Figure 1). Median age at the time of surgery was 60 years (interquartile range [IQR] 51 to 68 years), 1548 (56%) were female, and the mean ASA score was 3. Fourteen percent of cases were performed laparoscopically, and the remainder were performed via an open surgical approach. Preoperative comorbidities are detailed in Table 1. 360 patients (13%) had diabetes, 1208 (43%) medication-controlled hypertension, and 82 (3%) required chronic steroids. 365 patients (13%) were documented smokers within the 12 months prior to surgery, although the overall rates of COPD and dyspnea were low. With regard to their oncologic diagnoses, 1335 (48%) received preoperative chemotherapy within 30 days of surgery and 495 (18%) received preoperative radiation within 90 days of surgery. At the time of surgery, 746 (27%) of patients had disseminated cancer and 72 (3%) reported loss of >10 percent of their body weight during the 6 months prior to surgery.
Table 1:
Clinical Characteristics, based on Recovery Protocol
| Factor | Total | Traditional | Enhanced Recovery |
p value |
|---|---|---|---|---|
| No. of patients | 2747 | 1495 (54) | 1252 (46) | |
| Surgical Subspecialty | ||||
| Colorectal | 663 (24) | 273 (18) | 390 (31) | |
| Gynecology | 634 (23) | 401 (27) | 233 (19) | |
| Hepatobiliary | 291 (11) | 230 (15) | 61 (5) | |
| Thoracic/Vascular | 856 (31) | 360 (26) | 466 (37) | |
| Urology | 303 (11) | 201 (13) | 102 (8) | |
| Preoperative | ||||
| Age, years, median (IQR) | 60 (51–68) | 60 (50–69) | 60 (51–68) | 0.742 |
| Gender, female | 1548 (56) | 856 (57) | 692 (55) | 0.296 |
| ASA score | ||||
| 1/2 | 347 (13) | 199 (13) | 148 (12) | -- |
| 3/4 | 2375 (87) | 1287 (87) | 1088 (88) | 0.270 |
| Diabetes | 360 (13) | 182 (12) | 178 (14) | 0.114 |
| Current smoker | 365 (13) | 215 (14) | 150 (12) | 0.065 |
| Dyspnea | 190 (7) | 98 (7) | 92 (7) | 0.415 |
| COPD | 128 (5) | 72 (5) | 56 (4) | 0.671 |
| HTN requiring medication | 1208 (43) | 686 (46) | 522 (42) | 0.027 |
| Disseminated cancer | 746 (27) | 443 (30) | 303 (24) | 0.001 |
| Steroid use | 82 (3) | 48 (3) | 34 (3) | 0.448 |
| >10% weight loss | 72 (3) | 46 (3) | 26 (2) | 0.102 |
| Bleeding disorder | 97 (4) | 61 (4) | 36 (3) | 0.088 |
| Preoperative radiation | 495 (18) | 240 (16) | 255 (20) | 0.004 |
| Preoperative chemotherapy | 1335 (48) | 693 (47) | 642 (51) | 0.014 |
| Perioperative | ||||
| MIS procedure | 394 (14) | 174 (12) | 220 (18) | <0.0001 |
| Wound classification | ||||
| Clean | 84 (3) | 50 (3) | 34 (3) | -- |
| Clean/contaminated | 2543 (93) | 1379 (92) | 1164 (93) | -- |
| Contaminated | 74 (3) | 38 (3) | 36 (3) | -- |
| Dirty/infected | 46 (2) | 28 (2) | 18 (1) | 0.862 |
| Operative time, minutes, median (IQR) | 218 (141–316) | 234 (152–335) | 198 (126–294) | <0.0001 |
IQR: interquartile range; ASA: American Society of Anesthesiologists; COPD: Chronic Obstructive Pulmonary Disease; HTN: hypertension; MIS: minimally invasive surgery
A total of 1252 (46%) of patients were treated on ER protocols. Compared to patients treated on TP protocols, patients on ER protocols had similar median age (60 vs. 60 years, p = 0.742) and rates of ASA ≥3 classification (88% vs. 87%, p = 0.270). Although patients treated on ER protocols had slightly lower rates of medication-controlled hypertension (42% vs. 46%, p = 0.027) and disseminated cancer (24% vs. 30%, p = 0.001), they were more likely to have undergone preoperative treatment with chemotherapy (51% vs. 47%, p = 0.014) and radiation (20% vs. 16%, p = 0.004).
Outcomes of patients treated on ER versus TP protocols
Compared to TP protocols, treatment on ER protocols was associated with decreased perioperative complications (Table 2). Specifically, patients on ER protocols were less likely to have complications (20% vs. 33%, p <0.0001) including severe complications (7% vs. 10%, p = 0.010). The median hospital LOS was lower for patients on ER protocols (4 vs. 5 days, p <0.0001). Despite the shorter LOS, unplanned 30-day readmission rates did not increase in the ER cohort (107 vs. 134 patients, 8.6% vs. 9.0%, p = 0.701). Lastly, while the 30-day mortality rates were low for both cohorts, a trend towards reduced mortality was observed amongst patients treated on ER protocols (0.2% vs. 0.6%, p = 0.256).
Table 2:
Postoperative Complications, based on Recovery Protocol
| Factor | Total n=2747 |
Traditional n=1495 (54) |
Enhanced Recovery n=1252 (46) |
p value |
|---|---|---|---|---|
| Superficial incisional SSI | 95 (3) | 64 (4) | 31 (3) | 0.010 |
| Deep incisional SSI | 15 (1) | 13 (1) | 2 (0.16) | 0.016 |
| Organ space infection | 88 (3) | 51 (3) | 37 (3) | 0.499 |
| Wound disruption/dehiscence | 35 (1) | 26 (2) | 9 (1) | 0.018 |
| Pneumonia | 80 (3) | 52 (3) | 28 (2) | 0.054 |
| Urinary tract infection | 81 (3) | 63 (4) | 18 (1) | <0.0001 |
| Transfusion ≤72 hrs of OR | 512 (19) | 344 (23) | 168 (13) | <0.0001 |
| Unplanned return to OR | 75 (3) | 46 (3) | 29 (2) | 0.241 |
| Any complication | 747 (27) | 493 (33) | 254 (20) | <0.0001 |
| Any severe complicationa | 244 (9) | 152 (10) | 92 (7) | 0.010 |
| LOS, days, median (IQR) | 4 (3–7) | 5 (3–7) | 4 (2–5) | <0.0001 |
| Mortality ≤30 days | 21 (1) | 12 (1) | 9 (1) | 0.802 |
| Readmission ≤30 days | 241 (9) | 134 (9) | 107 (9) | 0.701 |
SSI: surgical site infection; OR: operating room; IQR: interquartile range; LOS: length of stay
Severe complications include: organ space infection, wound disruption/dehiscence, pneumonia, unplanned intubation, acute renal failure, myocardial infarction, sepsis, septic shock, unplanned return to OR
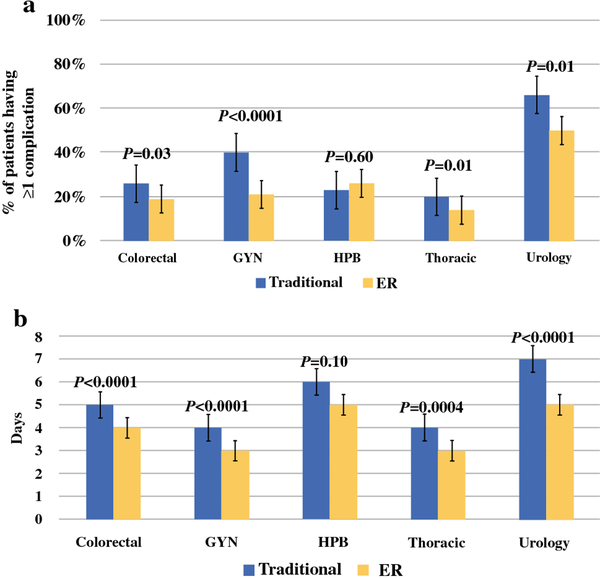
Individual specialty outcomes of patients treated on ER versus TP protocols
The previously described analyses were also performed on an individual basis for each of the surgical specialties included in the NSQIP database. These analyses demonstrated that many of the beneficial effects of ER protocol adoption observed for all cases were also seen within each specialty. Although the exact factors that significantly improved with ER protocol implementation differed for each specialty, these protocols uniformly resulted in decreased rates of complications (Figure 1a), including severe complications. This included decreased rates of surgical site infections following ER protocol implementation for all specialties except thoracic surgery, for which no change in the already low rates of SSIs was observed (1.0% vs. 2.8%, p = 0.085). Patients across all specialties treated on ER protocols also had shorter median hospital LOS (Figure 1b). Lastly, evaluation by the individual specialties of their patients’ average postoperative opioid use, measured as morphine-equivalent daily doses, demonstrated a 42 to 85 percent decrease in opioid use after ER protocol implementation.[30] Although no data regarding patient-reported pain scores is collected within the NSQIP database, results of previously published studies utilizing ER protocols suggest that the lower observed opioid use was associated with stable to improved patient reported pain scores.[31–33]
Figure 1.
Specialty-specific outcomes based on recovery protocol. Comparison of (a) complication rates and (b) median hospital length of stay between patients managed on Traditional vs. Enhanced Recovery Protocols.
Assessment of high magnitude case outcomes
To further assess the effects of ER protocol implementation on patient outcomes, and to better control for case complexity, a sub-analysis was performed on those patients undergoing high-magnitude surgeries (primary CPT RVU >30). 1022 cases (37%) satisfied this definition. High-magnitude cases by surgical subspecialty are shown in Supplementary Figure 2. Within this cohort of patients, 371 (36%) were treated on ER protocols. Compared to patients on TP protocols, ER protocol patients were less likely to have disseminated cancer at the time of surgery (19% vs. 36%, p <0.0001), but were more likely to have undergone radiation (27% vs. 19%, p = 0.001). Median procedure duration was similar between the ER and TP cohorts (327 vs. 326 minutes, p = 0.466). (Table 3).
Table 3:
Clinical Characteristics for High-Magnitude Casesb, based on Recovery Protocol
| Factor | Total | Traditional | Enhanced Recovery |
p value |
|---|---|---|---|---|
| No. of patients | 1022 | 651 (64) | 371 (36) | |
| Surgical Subspecialty | ||||
| Colorectal | 262 (26) | 111 (17) | 151 (41) | |
| Gynecology | 128 (13) | 82 (13) | 46 (12) | |
| Hepatobiliary | 291 (28) | 230 (35) | 61 (16) | |
| Thoracic/Vascular | 49 (5) | 32 (5) | 17 (5) | |
| Urology | 292 (29) | 196 (30) | 96 (26) | |
| Preoperative | ||||
| Age, years, median (IQR) | 60 (50–69) | 60 (50–60) | 60 (50–68) | 0.879 |
| Gender, female | 462 (45) | 287 (44) | 175 (47) | 0.341 |
| ASA score | ||||
| 1/2 | 126 (12) | 80 (12) | 46 (13) | -- |
| 3/4 | 889 (88) | 569 (88) | 320 (87) | 0.911 |
| Diabetes | 136 (13) | 82 (13) | 54 (15) | 0.375 |
| Current smoker | 129 (13) | 92 (14) | 37 (10) | 0.054 |
| Dyspnea | 54 (5) | 36 (6) | 18 (5) | 0.641 |
| COPD | 39 (4) | 26 (4) | 13 (4) | 0.694 |
| HTN requiring medication | 448 (44) | 289 (44) | 159 (43) | 0.634 |
| Disseminated cancer | 302 (30) | 232 (36) | 70 (19) | <0.0001 |
| Steroid use | 28 (3) | 21 (3) | 7 (2) | 0.207 |
| >10% weight loss | 22 (2) | 17 (3) | 5 (1) | 0.262 |
| Bleeding disorder | 40 (4) | 27 (4) | 13 (4) | 0.610 |
| Preoperative radiation | 225 (22) | 123 (19) | 102 (27) | 0.001 |
| Preoperative chemotherapy | 616 (60) | 395 (61) | 221 (60) | 0.730 |
| Perioperative | ||||
| Wound classification | ||||
| Clean | 18 (2) | 18 (3) | 0 (0) | -- |
| Clean/contaminated | 952 (93) | 600 (92) | 352 (95) | -- |
| Contaminated | 33 (3) | 19 (3) | 14 (4) | -- |
| Dirty/infected | 19 (2) | 14 (2) | 5 (1) | 0.002 |
| Operative time, min, median (IQR) | 327 (255–419) | 326 (251–422) | 327 (266–409) | 0.466 |
IQR: interquartile range; ASA: American Society of Anesthesiologists; COPD: Chronic Obstructive Pulmonary Disease; HTN: hypertension
Defined as RVU > 30
Compared to patients undergoing surgeries of any magnitude, patients undergoing high-magnitude operations had increased rates of perioperative complications (41% of cases with RVU >30 vs. 27% of all cases, p <0.0001), longer median LOS (6 vs. 4 days, p <0.0001), and higher readmission rates (13% vs. 8.8%, p = 0.0003). Despite this confirmation of increased case complexity, a beneficial effect of ER protocols was still observed, and many of the key findings from the analysis of the entire study population also held true for patients who underwent high-magnitude surgery. Specifically, patients undergoing more complex cancer surgery and on ER protocols were less likely than traditionally-treated patients to have any complication (35% vs. 44%, p = 0.002). The median LOS for the ER protocol-treated cohort was also shorter (5 vs. 6 days, p <0.0001), while no corresponding increase in 30-day readmissions was observed (14% vs. 12%, p = 0.348). No significant differences in the rates of severe complications or 30-day mortality were found in this sub-analysis; however, both were trending in a confirmatory direction in the ER cohort. (Table 4).
Table 4:
Clinical Characteristics for High-Magnitude Casesb, based on Recovery Protocol
| Factor | Total n=1022 |
Traditional n=651 (64) |
Enhanced Recovery n=371 (36) |
p value |
|---|---|---|---|---|
| Superficial incisional SSI | 51 (5) | 36 (6) | 15 (4) | 0.294 |
| Deep incisional SSI | 10 (1) | 8 (1) | 2 (0.54) | 0.281 |
| Organ space infection | 61 (6) | 38 (6) | 23 (6) | 0.814 |
| Wound disruption/dehiscence | 24 (2) | 16 (2) | 8 (2) | 0.760 |
| Pneumonia | 29 (3) | 19 (3) | 10 (3) | 0.836 |
| Mechanical ventilation >48 hrs | 8 (1) | 6 (1) | 2 (1) | 0.718 |
| Urinary tract infection | 48 (5) | 35 (5) | 13 (4) | 0.174 |
| Transfusion ≤72 hrs of OR | 305 (30) | 214 (33) | 91 (25) | 0.005 |
| Sepsis | 24 (2) | 17 (3) | 7 (2) | 0.462 |
| Unplanned return to OR | 45 (4) | 31 (5) | 24 (5) | 0.459 |
| Any complication | 416 (41) | 288 (44) | 128 (35) | 0.002 |
| Any severe complicationa | 136 (13) | 90 (14) | 46 (12) | 0.519 |
| LOS, days, median (IQR) | 6 (4–8) | 6 (5–8) | 5 (3–7) | <0.0001 |
| Mortality ≤30 days | 3 (0.29) | 3 (0.46) | 0 (0) | 0.558 |
| Readmission ≤30 days | 130 (13) | 78 (12) | 52 (14) | 0.348 |
SSI: surgical site infection; OR: operating room; IQR: interquartile range; LOS: length of stay
Defined as RVU >30
Severe complications include: organ space infection, wound disruption/dehiscence, pneumonia, unplanned intubation, acute renal failure, myocardial infarction, sepsis, septic shock, unplanned return to OR
DISCUSSION
This study found that the adoption of enhanced recovery protocols for the perioperative care of oncologic patients resulted in improved patient outcomes, including decreased rates of complications, reduced hospital LOS without a concomitant increase in readmission rates, and lower opioid utilization. These findings of ER protocol implementation at a large comprehensive cancer center mirror those reported in the ER literature for other surgical specialties.[3–8] To our knowledge this is the largest study to date looking at multi-specialty ER implementation within the setting of oncologic surgery, and so provides substantial evidence that ER protocols can be successfully utilized in the treatment of this complex patient population.
Unlike other reported ER studies, this analysis looked at ER implementation across multiple surgical specialties. Overall the findings for each specialty were similar to those for the entire cohort with regard to patient outcome improvement. Even if a significant improvement in an individual outcome was not seen, a trend in the improved direction was observed. An exception to this was the outcomes observed for the HPB group, which demonstrated equivalent patient outcomes following adoption of ER protocols. These findings were likely the result of smaller included case volume and later provider adoption of ER protocols. It should be noted that this group has previously published on their larger experience with implementation of ER protocols in liver surgery and demonstrated that these protocols resulted in improved patient outcomes.[10, 31, 34]
Perhaps more important than the effects seen following ER implementation for all cases were those seen amongst patients undergoing high-magnitude surgery. While it is challenging to amalgamate outcomes across multiple specialties, focusing on high-magnitude cases enabled analysis of a cohort of patients undergoing operations of more uniform complexity. This is reflected by the equivalent median procedure durations for patients undergoing high-magnitude surgery and treated on ER versus TP protocols (327 vs. 326 minutes, p = 0.466). That patients in the high magnitude cohort on ER protocols were also found to have improved outcomes, including decreased complications and reduced LOS, suggests the results of the analysis for all cases were not driven by a single specialty performing a large number of lower-complexity cases.
As all surgical programs engage in continuous quality improvement at some level, one critique of this study is that it is possible that other simultaneous initiatives contributed to the observed improved patient outcomes. For example, the hepatobiliary and colorectal groups developed a quality improvement program around urinary tract infections that preceded ER implementation, and the gynecology group designed a peri-operative bundle to reduce their rates of surgical site infections in parallel with their implementation. However, there were no ongoing system-wide improvements that could explain the consistency or magnitude of our cross-specialty findings, including the dramatic decrease in opioid utilization shared by all groups.
A second critique of the methodology may be the definition of ER protocol compliance. As previously discussed, the four pillars of ER protocols have been well described, and each pillar includes more than one patient intervention. Although specific interventions were not proscribed at an institutional level, each team designed ordersets and pathways that facilitated high compliance rates with multiple accepted individual elements. Several studies have shown that ER protocol compliance of ≥70 percent results in a demonstrable effect on patient outcomes.[1, 35, 36] Regarding the adherence to guidelines in this study, preoperative education, preoperative carbohydrate loading (where indicated), and preoperative multimodal non-narcotic oral analgesia were uniform. To facilitate consistent implementation and trainee education, electronically implemented ordersets (including the postoperative protocols and the analgesia plans) were utilized in over 90 percent of ER pathway patients across all disciplines. Each of these ordersets was designed to include >70 percent of recommended postoperative elements. Case audits demonstrated 60 to 100 percent compliance for each core component of the ER protocols (i.e., preoperative patient education and the four pillars of ER clinical care).
Lastly, the retrospective nature of this study makes it possible that other unmeasured confounding factors impacted our results. Although it is possible that confounding factors may have resulted in overestimation of the observed benefits of ER protocols, several elements of this study counter the potential for selection bias and support the conclusion that improvements in outcomes were attributable to ER protocol implementation. These include the NSQIP methodology, random case sampling, consistency of implementation within and across specialties, correlation with high-magnitude cases and large patient numbers.
CONCLUSION
This analysis of a multi-specialty enhanced recovery implementation at a large comprehensive cancer center demonstrates that not only is ER protocol implementation feasible for oncologic patients, but it is safe and effective in improving postoperative outcomes. This study provides evidence in support of ER utilization for a population of patients previously underrepresented in the ER literature. Considering the number of major oncologic operations performed annually across the world, wide scale adoption of ER protocols is likely to improve the outcomes of many patients. As postoperative complications and delayed postoperative recovery is known to prevent return to adjuvant treatment for oncologic patients, future work should focus on defining the potential long-term oncologic benefits of ER protocols.[9, 16, 37–39]
Supplementary Material
Case breakdown by specialty for all patients captured in the institutional NSQIP database from January 2011 – December 2016. Numbers above columns represent total number of cases performed by individual specialty. Percentages represent individual specialty’s contribution to traditional and ER cohorts.
Case breakdown by specialty for patients undergoing high magnitude surgeries captured in the institutional NSQIP database from January 2011 – December 2016. Numbers above columns represent total number of cases performed by individual specialty. Percentages represent individual specialty’s contribution to traditional and ER cohorts.
SYNOPSIS.
The benefit of enhanced recovery (ER) protocols is largely unproven for oncologic surgery. Using data from a large comprehensive cancer center NSQIP database, assessment of patient outcomes was performed before and after multispecialty ER implementation.
ACKNOWEDGEMENTS
The authors would like to recognize the contributions of Dr. Jay Shah, who was the original surgical lead for the Urology ER program and has since moved to another institution. In addition, we wish to thank our institution Surgical Clinical Reviewers, Annie Philip and Melony Levy, for their diligence and contributions to this study and to our broader patient quality improvement efforts.
Drs. Rebecca Marcus and Heather Lillemoe are supported by National Institutes of Health grant T32CA009599 and the MD Anderson Cancer Center support grant P30CA016672.
Footnotes
None of the authors have any conflicts of interest associated with this study.
ACS NSQIP Disclaimer: American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
The study was presented on March 22, 2018 as an oral abstract at Society of Surgical Oncology Annual Meeting, Chicago, IL.
REFERENCES
- 1.Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg 2017; 152: 292–298. [DOI] [PubMed] [Google Scholar]
- 2.Manso M, Schmelz J, Aloia T. ERAS-Anticipated outcomes and realistic goals. J Surg Oncol 2017; 116: 570–577. [DOI] [PubMed] [Google Scholar]
- 3.Connor S, Cross A, Sakowska M et al. Effects of introducing an enhanced recovery after surgery programme for patients undergoing open hepatic resection. HPB (Oxford) 2013; 15: 294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coolsen MM, van Dam RM, van der Wilt AA et al. Systematic review and meta-analysis of enhanced recovery after pancreatic surgery with particular emphasis on pancreaticoduodenectomies. World J Surg 2013; 37: 1909–1918. [DOI] [PubMed] [Google Scholar]
- 5.Hughes MJ, McNally S, Wigmore SJ. Enhanced recovery following liver surgery: a systematic review and meta-analysis. HPB (Oxford) 2014; 16: 699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau CS, Chamberlain RS. Enhanced Recovery After Surgery Programs Improve Patient Outcomes and Recovery: A Meta-analysis. World J Surg 2017; 41: 899–913. [DOI] [PubMed] [Google Scholar]
- 7.Song W, Wang K, Zhang RJ et al. The enhanced recovery after surgery (ERAS) program in liver surgery: a meta-analysis of randomized controlled trials. Springerplus 2016; 5: 207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Visioni A, Shah R, Gabriel E et al. Enhanced Recovery After Surgery for Noncolorectal Surgery?: A Systematic Review and Meta-analysis of Major Abdominal Surgery. Ann Surg 2018; 267: 57–65. [DOI] [PubMed] [Google Scholar]
- 9.Aloia TA, Zimmitti G, Conrad C et al. Return to intended oncologic treatment (RIOT): a novel metric for evaluating the quality of oncosurgical therapy for malignancy. J Surg Oncol 2014; 110: 107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Day RW, Cleeland CS, Wang XS et al. Patient-Reported Outcomes Accurately Measure the Value of an Enhanced Recovery Program in Liver Surgery. J Am Coll Surg 2015; 221: 1023–1030 e1021–1022. [DOI] [PubMed] [Google Scholar]
- 11.Neville A, Lee L, Antonescu I et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg 2014; 101: 159–170. [DOI] [PubMed] [Google Scholar]
- 12.Takamoto T, Hashimoto T, Inoue K et al. Applicability of enhanced recovery program for advanced liver surgery. World J Surg 2014; 38: 2676–2682. [DOI] [PubMed] [Google Scholar]
- 13.Alcantara-Moral M, Serra-Aracil X, Gil-Egea MJ et al. Observational cross-sectional study of compliance with the fast track protocol in elective surgery for colon cancer in Spain. Int J Colorectal Dis 2014; 29: 477–483. [DOI] [PubMed] [Google Scholar]
- 14.Schultz NA, Larsen PN, Klarskov B et al. Evaluation of a fast-track programme for patients undergoing liver resection. Br J Surg 2013; 100: 138–143. [DOI] [PubMed] [Google Scholar]
- 15.Bagnall NM, Malietzis G, Kennedy RH et al. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis 2014; 16: 947–956. [DOI] [PubMed] [Google Scholar]
- 16.Gustafsson UO, Oppelstrup H, Thorell A et al. Adherence to the ERAS protocol is Associated with 5-Year Survival After Colorectal Cancer Surgery: A Retrospective Cohort Study. World J Surg 2016; 40: 1741–1747. [DOI] [PubMed] [Google Scholar]
- 17.Li P, Fang F, Cai JX et al. Fast-track rehabilitation vs conventional care in laparoscopic colorectal resection for colorectal malignancy: a meta-analysis. World J Gastroenterol 2013; 19: 9119–9126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Vugt JL, Reisinger KW, Derikx JP et al. Improving the outcomes in oncological colorectal surgery. World J Gastroenterol 2014; 20: 12445–12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim BJ, Aloia TA. What Is “Enhanced Recovery,” and How Can I Do It? J Gastrointest Surg 2018; 22: 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel SH, Kim BJ, Tzeng CD et al. Reduction of Cardiopulmonary/Renal Complications with Serum BNP-Guided Volume Status Management in Posthepatectomy Patients. J Gastrointest Surg 2018; 22: 467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gustafsson UO, Scott MJ, Schwenk W et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012; 31: 783–800. [DOI] [PubMed] [Google Scholar]
- 22.Lassen K, Coolsen MM, Slim K et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012; 31: 817–830. [DOI] [PubMed] [Google Scholar]
- 23.Melloul E, Hubner M, Scott M et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 2016; 40: 2425–2440. [DOI] [PubMed] [Google Scholar]
- 24.Mortensen K, Nilsson M, Slim K et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Br J Surg 2014; 101: 1209–1229. [DOI] [PubMed] [Google Scholar]
- 25.Nelson G, Altman AD, Nick A et al. Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations--Part II. Gynecol Oncol 2016; 140: 323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nelson G, Altman AD, Nick A et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations--Part I. Gynecol Oncol 2016; 140: 313–322. [DOI] [PubMed] [Google Scholar]
- 27.Nygren J, Thacker J, Carli F et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012; 31: 801–816. [DOI] [PubMed] [Google Scholar]
- 28.Thorell A, MacCormick AD, Awad S et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 2016; 40: 2065–2083. [DOI] [PubMed] [Google Scholar]
- 29.Scarborough JE, Bennett KM, Englum BR et al. The impact of functional dependency on outcomes after complex general and vascular surgery. Ann Surg 2015; 261: 432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lasala JD, Heir JS, Mena GE et al. Implementation of an Enhanced Surgical Recovery Programme (ESRP) gynaecologic oncology: How much did intra-operative opioid administration decrease in first year post implementation? Clin Nutr ESPEN 2016; 12: e42–e43. [Google Scholar]
- 31.Aloia TA, Kim BJ, Segraves-Chun YS et al. A Randomized Controlled Trial of Postoperative Thoracic Epidural Analgesia Versus Intravenous Patient-controlled Analgesia After Major Hepatopancreatobiliary Surgery. Ann Surg 2017; 266: 545–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meyer LA, Lasala J, Iniesta MD et al. Effect of an Enhanced Recovery After Surgery Program on Opioid Use and Patient-Reported Outcomes. Obstet Gynecol 2018; 132: 281–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Haren RM, Mehran RJ, Mena GE et al. Enhanced Recovery Decreases Pulmonary and Cardiac Complications After Thoracotomy for Lung Cancer. Ann Thorac Surg 2018; 106: 272–279. [DOI] [PubMed] [Google Scholar]
- 34.Zimmitti G, Soliz J, Aloia TA et al. Positive Impact of Epidural Analgesia on Oncologic Outcomes in Patients Undergoing Resection of Colorectal Liver Metastases. Ann Surg Oncol 2016; 23: 1003–1011. [DOI] [PubMed] [Google Scholar]
- 35.Gotlib Conn L, McKenzie M, Pearsall EA, McLeod RS. Successful implementation of an enhanced recovery after surgery programme for elective colorectal surgery: a process evaluation of champions’ experiences. Implement Sci 2015; 10: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedziwiatr M, Kisialeuski M, Wierdak M et al. Early implementation of Enhanced Recovery After Surgery (ERAS(R)) protocol - Compliance improves outcomes: A prospective cohort study. Int J Surg 2015; 21: 75–81. [DOI] [PubMed] [Google Scholar]
- 37.Kim BJ, Caudle AS, Gottumukkala V, Aloia TA. The Impact of Postoperative Complications on a Timely Return to Intended Oncologic Therapy (RIOT): the Role of Enhanced Recovery in the Cancer Journey. Int Anesthesiol Clin 2016; 54: e33–46. [DOI] [PubMed] [Google Scholar]
- 38.Merkow RP, Bentrem DJ, Mulcahy MF et al. Effect of postoperative complications on adjuvant chemotherapy use for stage III colon cancer. Ann Surg 2013; 258: 847–853. [DOI] [PubMed] [Google Scholar]
- 39.Merkow RP, Bilimoria KY, Tomlinson JS et al. Postoperative complications reduce adjuvant chemotherapy use in resectable pancreatic cancer. Ann Surg 2014; 260: 372–377. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case breakdown by specialty for all patients captured in the institutional NSQIP database from January 2011 – December 2016. Numbers above columns represent total number of cases performed by individual specialty. Percentages represent individual specialty’s contribution to traditional and ER cohorts.
Case breakdown by specialty for patients undergoing high magnitude surgeries captured in the institutional NSQIP database from January 2011 – December 2016. Numbers above columns represent total number of cases performed by individual specialty. Percentages represent individual specialty’s contribution to traditional and ER cohorts.