Abstract
Background and Purpose
Hamstring injuries (HSI) occur more commonly in baseball than are often appreciated and can impact the potential career of a player. Little is known about the historical incidence of these injuries in summer league players preparing for their upcoming collegiate season or being drafted by major league team(s). Summer league baseball players have a high historical incidence of HSI which are often unknown at the start of their summer league play. The purpose of this study was to administer a validated questionnaire to assess various factors regarding the prevalence of prior hamstring injuries, current symptoms of posterior thigh pain or hamstring injuries in amateur summer league baseball players, and to provide details on the injury history, time lost from injury, injury reocurrence, position, individual player physical characteristics and physical activities that might be associated with those injuries.
Study Design
Cross-sectional Observational Study
Method
A self-reported, validated questionnaire regarding the history, prevalence, reoccurrence and functional impact of HSI and posterior thigh pain was administered to and completed by 201 out of 251 summer league baseball players associated with the Cape Cod League and the Northwoods League at the start of the 2013-2015 seasons. The questionnaire was administered by certified athletic trainers associated with each team. Participation was voluntary and informed consent was obtained from all players.
Results
Forty seven out of 201 players surveyed reported a HSI history. Sixty-six percent of these players (N = 31) reported unilateral injuries and 34% (N = 16) reported bilateral injuries. Reoccurrence rate was 27.7% across all players. Approximately 1/3rd of all position players (catchers 33.3%, infielders 32.6% and outfielders 31.6%) reported a HSI history compared to 12.9% of all pitchers. Significant differences (p<.05) existed between the HSI and Non-HSI groups for self-reported symptoms, soreness, and pain, as well as function and quality of life. Within the HSI history group, players who batted left and threw right reported the most injuries.
Conclusion
A large number of position players and pitchers who report for summer league baseball have a history of posterior thigh pain and HSI. Those with prior injuries have a high reoccurrence rate. Position players have a higher incidence of injury than do pitchers.
Level of Evidence
3
Keywords: Baseball, hamstring injuries, Hamstring Outcome Score, incidence, movement system, posterior thigh pain
Introduction
Various epidemiologic studies have described the incidence, frequency, characteristics and types of injuries that commonly occur in interscholastic,1,2 intercollegiate,3,4 and professional baseball.5 As expected, injuries that involve the upper extremity, specifically the shoulder, elbow, hand and wrist, are the most common in this upper extremity dominant sport. However, other types of injuries can occur and can have an adverse impact on the players’ ability to train and participate in games. The impact of these non-throwing, non-upper extremity injuries are often underestimated and unappreciated, until significant time is lost on the playing field. Injuries to the hamstring complex are one such injury.
The literature discussing the incidence of hamstring injury for other sports is much more robust overall than the existing literature for baseball. Authors who have studied other sports report up to 29% of all injuries involve the hamstring complex6-16 which may be serious enough that prolonged time is lost from practice or play,8,17-22 and may be recurrent.17,21,23-26 However, only a few studies on hamstring injuries in baseball are available in the literature.1,3,5,25,27,28 These studies have mostly centered around high school and NCAA athletes, not those participating in summer league baseball. During the summer, leagues such as the Cape Cod League and the Northwoods League, operate in order to allow players to try to improve their skills and showcase their abilities in preparation for returning to college baseball or preparing for possible draft to the minor leagues.
Studies of athletes of other sports have detailed injury history, personal demographic and physical characteristics of the athlete and sport specific characteristics (position, type of activity, personal characteristics such as height, weight, side dominance) that may contribute to the knowledge of what type of player is more likely to incur a hamstring injury, and the sport specific factors that might contribute to or cause a hamstring injury in that particular sport.14,29,30 Information such as this is critical for the development of targeted conditioning and injury prevention programs, especially in developing players in order to try to prevent the occurrence and/or minimize the reoccurrence of hamstring injuries. These sport specific factor studies have stimulated the development of Hamstring Injury Prevention programs (HIP) which have been shown to be effective in decreasing the rate of acute and chronic hamstring injury in athletes in several sports.7,30-36 Recently, a study utilizing eccentric hamstring training in Major and Minor League baseball demonstrated a significant decrease in acute hamstring strains in addition to a decrease in time loss due to injury.27 However, adherence and compliance to such prevention programs has been inconsistent, therefore diminishing the ability to effectively decrease the hamstring injury rate.37
The purpose of this study was to administer a validated questionnaire to assess various factors regarding the prevalence of prior hamstring injuries, current symptoms of posterior thigh pain or hamstring injuries in amateur summer league baseball players, and to provide details on the injury history, time lost from injury, injury reocurrence, position, individual player physical characteristics and physical activities that might be associated with those injuries.
Methods
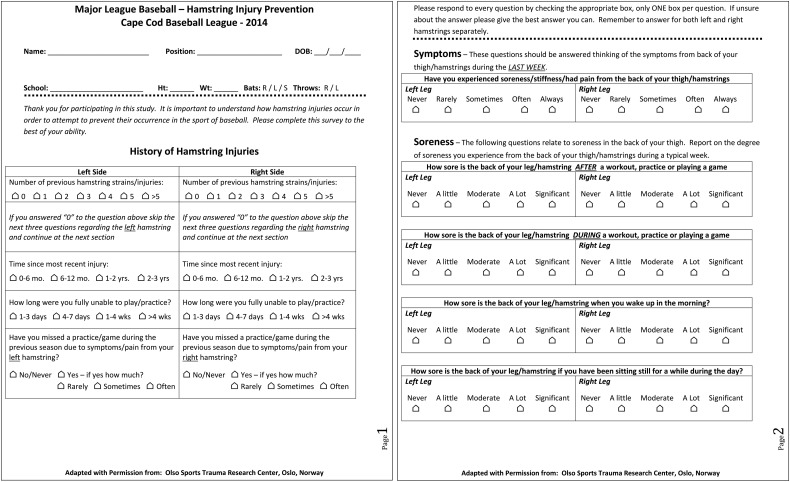
Summer league athletes completed a previously validated Hamstring Outcome Score (HaOS – Appendix 1) questionnaire created by the Oslo Sports Trauma Research Center (OSTRC).38 This self-reported questionnaire provides information regarding time lost from injury, frequency of injury and reoccurrence, and symptoms associated with these injuries for general physical activities associated with athletics (running, jogging, accelerating, walking up two steps at a time, etc). This questionnaire was specifically modified for baseball related activities to improve the contextuality for the sport of baseball with written permission from OSTRC. To maintain validity of the questionnaire, only slight adaptations were made to the questionnaire that increased its’ relevance to the sport of baseball (including characteristics regarding position, batting, throwing and activities associated within baseball such as “running to first base,” stopping after and sprinting to first base in the wording of the questions).
All questions were associated with general physical/athletic activities and the adapted vernacular was used to make sure the player understood the question, and to clarify how the question(s) related to the sport of baseball. This questionnaire consists of five subscales whose scores are reported as percentages, with 100% indicating no hamstring complaints or symptoms; each item/question within the subscale is scored on a scale of zero to four when analyzed by the researcher. Players were unaware of the value assigned to each response. Lower scores/totals are expected for players with a history of HSI or current problems, indicating more disability related to HSI. The HaOS total score is the mean value of the five subscales.
Part A: Previous Injury - Inquires about the number of previous injuries, time since their most recent injury, how long they were fully unable to practice/play for, whether or not they missed practice/play as a result of the injury and whether or not they had symptoms over the prior week.
Part B: Soreness - Acquires information regarding discomfort or soreness in the area of the “back of your thigh” during or after practice or play, symptom variation during the day and symptoms with sitting. The question seeks information on discomfort or soreness compared to pain associated with specifically described physical activites related to daily living or sport specific activities (as worded in Part C)
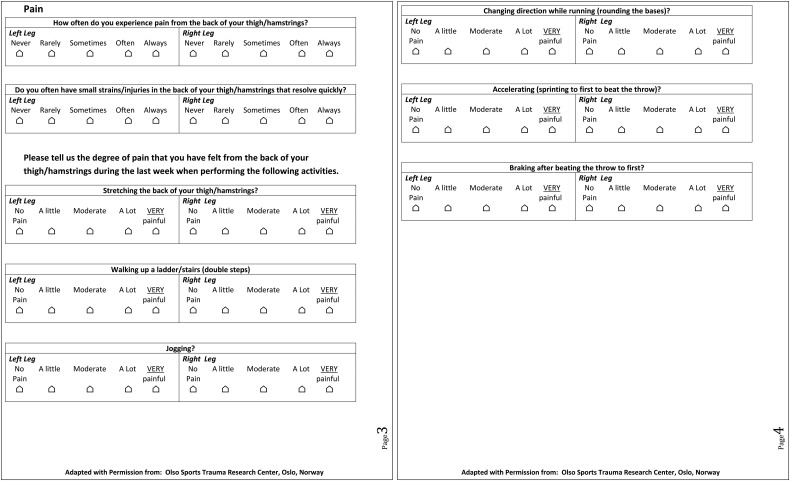
Part C: Pain - Provides information regarding the frequency of pain in the “back of the thigh/hamstrings” and how quickly symptoms may have resolved and whether or not they are symptomatic with general athletic activities such as stretching, walking up steps, jogging and baseball specific activities such as base running.
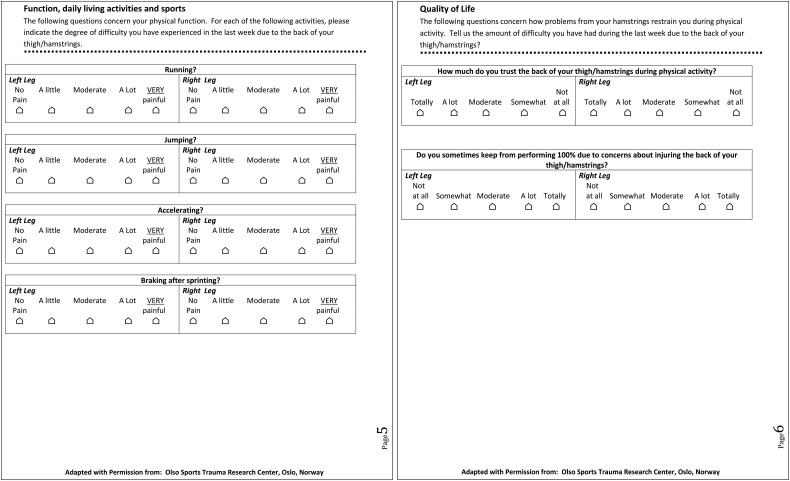
Part D: Function -Asks general questions regarding difficulty or posterior thigh pain in the prior week with general running, jumping, accelerating or decelerating after sprinting.
Part E: Quality of Life - Asks how much the athlete trusts their hamstring(s) during physical activity and whether they are able to perform at 100% due to any concerns about injuring/re-injuring their hamstring(s).
The questionnaire was administered to eight different summer league teams in the Cape Cod and Northwood's Leagues over a three-year period between 2013 and 2015. The questionnaire was confidentially administered to the athlete by a certified athletic trainer (ATC) associated with each team. A total 251 players on the teams’ rosters at the start of their summer league season were asked to complete the questionnaire. Completion of the questionnaire was voluntary on the part of each player, and no player completed the questionnaire more than once during the course of the study. Informed consent was obtained by all players who completed the questionnaire. The study was reviewed and granted approval by the Johns Hopkins Medicine Institutional Review Board.
Statistics
Results from the questionnaire were analyzed to assess the differences between players who reported a history of HSI and posterior thigh pain associated with physical activites to those players without a history of HSI and posterior thigh pain. Chi-square tests and t-tests were used to analyze player physical characteristics (age, height, weight, position, and batting and throwing handedness) and to make comparisons by position. HaOS outcome score comparisons were made using a Mixed Model, nesting players within teams. All assumptions for all models were assessed. Statistially significant differences were assessed using the alpha level set at p < 0.05.
Results
Out of the 251 players who were asked to complete the questionnaire, a total of 201 questionnaires were completed and analyzed, for a response rate of 80.1%. There was no significant difference in player age (p = 0.82) or weight (p = 0.097), but injured athletes were on average one inch shorter compared to their uninjured counterparts (p = 0.010). (Table 1). Over the course of the three-season study period, 47 (23.8%) of the 201 athletes who completed the survey reported having a HSI history. A total of 81 different hamstring injuries were reported by the 47 players. Forty-three injuries involved the left leg (53.1%) and 38 injuries involved the right leg (43.9%); there was no significant side difference (p = 0.490). However, there was a significant relationship between injuries and primary position played. Pitchers (12.2%) were significantly less likely (p = .015) to have had an HSI injury compared to position players: Catchers (33.3%), Infielders (32.6%), and Outfielders (31.6%). (Table 2)
Table 1.
Physical Characteristics Injured vs. Uninjured Players.
| Uninjured Players | Injured Players | ||||
|---|---|---|---|---|---|
| Number (%) | SD | Number (%) | SD | p-value | |
| Total Athletes N = 201 | 154 (76.6) | 47 (23.4) | |||
| Age (Years) | 20.29 | 1.03 | 20.33 | 0.97 | .821 |
| Height (Inches) | 73.17 | 2.14 | 72.18 | 2.53 | .010* |
| Weight (Pounds) | 197.53 | 19.94 | 192.02 | 19.49 | .097 |
= p<.05
Table 2.
Injury History by Position.
| Player Position | Total # Players | No Injury History | Injury History | % with Injury Hx |
|---|---|---|---|---|
| Catcher | 24 | 16 | 8 | 33.3% |
| Infield | 46 | 31 | 15 | 32.6% |
| Outfield | 38 | 26 | 12 | 31.6% |
| Pitcher | 93 | 81 | 12 | 12.9%* |
| Total | 201 | 154 | 47 | 23.8% |
P = .015
Table 3 details HSI history by position including prevalence, type (unilateral vs bilateral), and history of reoccurrence. Thirteen players (27.7%) reported a reoccurrence in the same leg. Thirty-one players (66%) reported unilateral injuries while 16 (34%) reported a HSI history in both hamstrings. Of the athletes who reported having bilateral injuries, five reported two occurrences in one leg, two reported two different occurrences in both legs and one reported three different injuries in each leg. There was no significant relationship between having bilateral or unilateral injuries and position (p = .692), or reoccurrence (p = .970).
Table 3.
Injury History: Reoccurrence, Unilateral and Bilateral Injuries.
| Player Position | Injury History | Recurrent Injuries | % Recurrent Injuries | Unilateral Injuries | % Unilateral Injuries | Bilateral Injuries | % Bilateral Injuries |
|---|---|---|---|---|---|---|---|
| Catcher | 8 | 2 | 25.0% | 5 | 62.5% | 3 | 37.5% |
| Infield | 15 | 5 | 33.3% | 9 | 60.0% | 6 | 40.0% |
| Outfield | 12 | 3 | 25.0% | 8 | 66.7% | 4 | 33.3% |
| Pitcher | 12 | 3 | 25.0% | 9 | 75.0% | 3 | 25.0% |
| Total | 47 | 13 | 27.7% | 31 | 66.0% | 16 | 34.0% |
Self reported data was also collected from the players regarding time lost from practice or play due to previous injury. The time lost to injury (an injury which prevented an athlete from participating in a subsequent training session or game) and severity (number of days away from practice or play) were defined using the definitions developed in the Union of European Football Associations (UEFA) Consensus Statement.39 Specific ranges and percentages of time lost are detailed in Table 4. Overall, 44% of injuries resulted in greater than one-week loss from baseball, while 56% lost less than one week. Ten out of 16 players (62.5%) with bilateral injuries lost more than one week from play while fifteen of the 31 (48.4%) players who had unilateral injury lost more than one week from play. Seven of thirteen players with recurrent injuries (53.8%) lost more than one week from play, and six of these seven players also had bilateral injuries.
Table 4.
.Self Reported Time Lost from Injury.
| Time Lost from Injury | N | Percent of HSI Players Time Lost | Summary Percentage |
|---|---|---|---|
| 1-3 Days | 25 | 39.68% | 55.56% |
| 4-7 Days | 10 | 15.87% | |
| 1-4 Weeks | 22 | 34.92% | 44.44% |
| 4 + Weeks | 6 | 9.52% |
HSI = Hamstring injury
Data stratified by handedness for batting and throwing is presented in Table 5. Athletes with HSI history more often batted right handed (n = 25) versus left handed (n = 19). Of the six players who identified as switch hitters, only one had an HSI history, and he threw right handed. A total of 37 different players with HSI history threw right handed and eight threw left handed. There was no significant relationship between history of injury with handedness as examined by batting (p = .410) or throwing (p = .607) in this group of 201 players.
Table 5.
Frequencies and Percent of Hamstring Injuries by Batting and Throwing Handedness Combinations.
| Total N (% within combination) | BAT LEFT THROW RIGHT | BAT LEFT THROW LEFT | BAT RIGHT THROW RIGHT | BAT RIGHT THROW LEFT | SWITCH HITTERS | TOTAL |
|---|---|---|---|---|---|---|
| No Injury History | 25 (68%) | 24 (77%) | 96 (80%) | 6 (86%) | 5 (83%) | 156 |
| Injury History | 12 (32%) | 7 (22%) | 24 (20%) | 1 (14%) | 1 (17%) | 45 |
| Total | 37 (100%) | 31 (100%) | 120 (100%) | 7 (100%) | 4 (100%) | 201 (100%) |
Interestingly, when examining HSI with batting preference and throwing dominance simultaneously, a difference is noted between players with and without a HSI history. While not statisticially significant, 32% percent (12/37) of all players who batted left handed and threw right handed had an HSI history, while the percent of players with other combinations for batting and throwing who also had a HSI history ranged from 14-22% (χ2 = 3.05; p = .550).
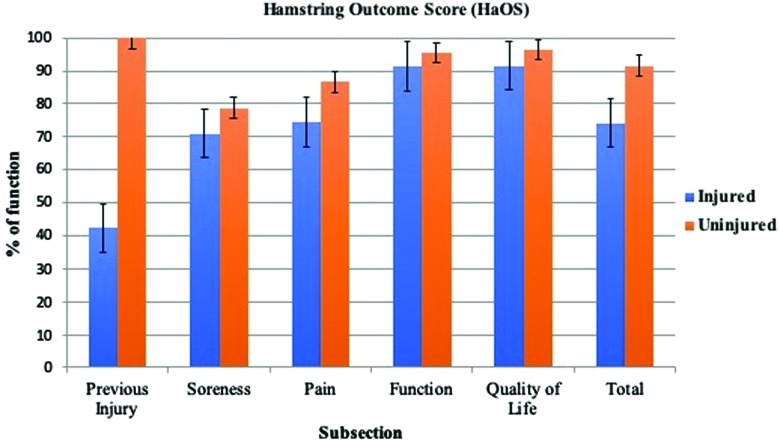
The Hamstring Outcome Score (HaOS) was used to provide detail and information on the number of previous hamstring injuries suffered by the players, including side of injury and the impact of posterior thigh pain and hamstring injury on the player's physical function. A Mixed Model was used to analyze HaOS total and subscale scores, nesting athletes within teams. This analytic method helps to account for any correlation that might be seen because athletes who played for the same teams may be more likely to have similar scores than two players from different teams since these “teammates” are subjected to similar training methodologies, acute and chronic loading and conditioning programs. In addition, this accomodates for the variation in number of responses per team, ranging from 8 to 31. There were significant differences found between players with and without HSI history for total HaOS score, with uninjured players scoring significantly higher on all the subscales (p < .05) (Table 6, Figure 1).
Table 6.
Means and Standard Errors from Mixed Model comparison of HaOS for HSI and non-HSI athletes.
| HaOS Section and Total Scores. Mixed Model Results | |||||
|---|---|---|---|---|---|
| No Injury History | History of Injury | ||||
| Mean | SE | Mean | SE | p-value | |
| Previous Injury and Symptoms | 82.67 | 1.57 | 72.41 | 2.87 | .002* |
| Soreness | 86.97 | 1.07 | 81.78 | 1.95 | .021* |
| Pain | 94.76 | 0.62 | 90.24 | 1.16 | .001* |
| Function | 96.63 | 0.64 | 93.78 | 1.21 | .039* |
| Quality of Life | 94.32 | 1.12 | 89.58 | 2.02 | .042* |
| Total Score | 90.94 | 0.79 | 84.79 | 1.43 | <.001* |
HaOS – Hamstring Outcome Score
HSI – Hamstring Injury
= p<0.05
Figure 1.
Hamstring Outcome Score (HaOS). Graph depicting HaOS Outcome Scores for the five subsections and total score for injured and uninjured players. A score of 100% reflects full function and no impairment.
Table 7 presents the results of the percentage of players who stated that they had symptoms of posterior thigh pain or soreness the week prior to the administration of the questionnaire. Differences are demonstrated between the groups regarding their responses to specific questions about symptoms and soreness relative to work outs. The higher value responses for athletes with a HSI history would be expected. As would be expected, the HSI group also responded that they had more soreness with the variety of activities asked about on the survey.
Table 7.
Self Reported Symptoms and Soreness Responses Reported as % of Athletes who responded.
| Symptoms Prior Week | Sore After Workout | Sore During Workout | Sore Waking in AM | Sore Sitting Still | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Uninjured Athletes | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | |
| Value | |||||||||||
| Never | 0 | 51.3% | 49.4% | 36.4% | 37.0% | 72.7% | 71.4% | 61.0% | 60.4% | 68.8% | 68.8% |
| Rarely/A Little | 1 | 32.5% | 32.5% | 48.1% | 48.7% | 25.3% | 25.3% | 30.5% | 29.9% | 23.4% | 22.7% |
| Sometimes/Moderate | 2 | 15.6% | 17.5% | 14.9% | 14.3% | 1.9% | 3.2% | 7.8% | 9.1% | 6.5% | 7.1% |
| Often/A lot | 3 | 0.6% | 0.6% | 0.0% | 0.0% | 0.0% | 0.0% | 0.6% | 0.6% | 1.3% | 1.3% |
| Always/Significant | 4 | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Hamstring Injury Athletes | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | |||||||||||
| Never | 0 | 34.0% | 29.8% | 38.3% | 38.3% | 55.3% | 59.6% | 48.9% | 53.2% | 72.3% | 74.5% |
| Rarely/A Little | 1 | 25.5% | 34.0% | 34.0% | 38.3% | 27.7% | 27.7% | 31.9% | 27.7% | 17.0% | 17.0% |
| Sometimes/Moderate | 2 | 34.0% | 29.8% | 23.4% | 19.1% | 17.0% | 12.8% | 12.8% | 12.8% | 6.4% | 4.3% |
| Often/A lot | 3 | 4.3% | 4.3% | 4.3% | 4.3% | 0.0% | 0.0% | 4.3% | 4.3% | 2.1% | 2.1% |
| Always/Significant | 4 | 2.1% | 2.1% | 0.0% | 0.0% | 0.0% | 0.0% | 2.1% | 2.1% | 2.1% | 2.1% |
Table 8 provides details on the frequency of posterior thigh pain and whether or not pain was present with baseball related activities such as stretching, base running, sprinting to first base, decelerating after reaching first base or rounding the bases. Again, as would be expected, players without HSI never or rarely had symptoms with these activities. Players with HSI had more frequent pain, more pain with stretching and symptoms took longer to resolve. However, their results regarding pain with running activities were very similar to those players without HSI.
Table 8.
Self Reported Pain with Baseball Related Activities (reported as % of athletes who responded).
| Pain Frequency | Frequency of “Small Injuries” | Pain with Stretch | Pain with Double Steps | Pain with Jogging | Pain with Rounding Base | Pain with Sprinting to 1st | Pain with Braking After 1st | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uninjured Athletes | Left | Right | Left | Right | Uninjured Athletes | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | |
| Value | ||||||||||||||||||
| Never | 0 | 69.5% | 66.9% | 72.7% | 72.7% | Never | 68.8% | 67.5% | 90.3% | 90.3% | 89.0% | 87.7% | 92.2% | 92.2% | 86.4% | 85.7% | 93.5% | 91.6% |
| Rarely | 1 | 26.0% | 27.3% | 22.7% | 22.1% | A Little | 23.4% | 23.4% | 9.1% | 9.1% | 10.4% | 11.7% | 6.5% | 6.5% | 11.0% | 11.0% | 5.8% | 7.8% |
| Sometimes | 2 | 3.9% | 5.2% | 2.6% | 3.9% | Moderate | 6.5% | 7.8% | 0.6% | 0.6% | 0.6% | 0.6% | 1.3% | 1.3% | 2.6% | 3.2% | 0.6% | 0.6% |
| Often | 3 | 0.6% | 0.6% | 1.9% | 1.3% | A Lot | 1.3% | 1.3% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Always | 4 | 0.0% | 0.0% | 0.0% | 0.0% | Significant | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Hamstring Injury Athletes | Left | Right | Left | Right | Hamstring Injury Athletes | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | Left | Right | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | ||||||||||||||||||
| Never | 0 | 51.1% | 57.4% | 48.9% | 53.2% | Never | 57.4% | 57.4% | 89.4% | 91.5% | 80.9% | 83.0% | 78.7% | 76.6% | 74.5% | 74.5% | 72.3% | 78.7% |
| Rarely | 1 | 34.0% | 27.7% | 34.0% | 31.9% | A Little | 27.7% | 23.4% | 8.5% | 6.4% | 14.9% | 10.6% | 21.3% | 19.1% | 23.4% | 19.1% | 19.1% | 14.9% |
| Sometimes | 2 | 12.8% | 10.6% | 17.0% | 14.9% | Moderate | 12.8% | 17.0% | 2.1% | 2.1% | 4.3% | 6.4% | 0.0% | 4.3% | 2.1% | 2.1% | 6.4% | 2.1% |
| Often | 3 | 2.1% | 4.3% | 0.0% | 0.0% | A Lot | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 4.3% | 2.1% | 4.3% |
| Always | 4 | 0.0% | 0.0% | 0.0% | 0.0% | Significant | 2.1% | 2.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
Discussion
This study has attempted to identify some specific characteristics regarding hamstring injuries that are incurred among summer league baseball players, identify athletes who have a history of HSI or reoccurrence, and factors that are associated with these injuries.
While a statistically significant one-inch difference in height was demonstrated for playes in this study with a history of HSI (Table 1) it should not be considered clinically significant as, based on the age range of these players, many may have been actively growing and changing.
Baseball studies in the current literature tend to discuss and focus on the incidence of injury per athletic exposure (AE), the overall injury rate (IR) during practice and games, and the number or percent each type of injury accounts for, with some discussion of recurrence.1,2,3,4,40 Injuries to the area described as “upper leg/thigh” account for between 8.2% to 14.5% of these high school baseball injuries and are most commonly labeled as “muscle strains”. 1,2 Dalton et al. reported the epidemiology of hamstring strains for 25 different NCAA sports using data gathered between 2009-2014. Overall, baseball accounted for 4.8% of all hamstring strain injuries reported during this period.40 Further stratification by body part revealed that “upper leg muscle tendon strains” accounted for 8.3% of practice injuries and 11% of all game related injuries.3 NCAA data has demonstrated that lower extremity injury accounted for over 50% of all injuries in NCAA athletes,4 and that for baseball, the lower extremity is the second most common area injured during practice or games, accounting for 35% of all collegiate baseball injuries. None of these studies however provide insight into HSI history by position.
This study provides detail regarding baseball related HSI by player position (Table 2). Twenty four percent of players who completed the questionnaire reported a history of HSI. While the percentage of position players who report a history of HSI is similar (31.6 to 33.3%) pitchers reports significantly fewer injuries (12.9%, p = .015). This difference may be due to the activity profiles of these different positions (i.e. the amount of running, base running, changes in direction and start and stop activities associated with the specific positions). Compared to position players, pitchers may not be as involved in the type of activities that may cause HSI (base running type activities).3
This study also provides insight into whether these injuries tend to be unilateral or bilateral, and the rate of recurrence (Table 3), although no statistically significant differences were seen between players of varied positions. Recurrence was not uncommon in this population of players with a history of HSI. The recurrence rate in this group of elite players (27.7%) was higher than that reported by Dalton et al (16%) across all NCAA baseball teams.40 The difference in the rate of recurrence in this study may be related to the quality of the players associated in these elite summer leagues compared to non-elite level players who may make up the majority of collegiate teams. The higher recurrence rate could be related to the amount of practice or game play time by these elite summer league players during their collegiate seasons, although this was not monitored during this study. The athlete exposure rate (AE) and injury rate (IR) may have been higher in this group as one would expect elite players to see more practice and game play time than none elite, general collegiate population players. 1,2,3,40 Summer leagues, such as the Cape Cod League and Northwoods League are showcase leagues whose teams accept only the best college baseball players in the country, who may eventually be drafted by major league baseball teams. Many more players, while talented enough for collegiate ball, may not see the same practice and play time as elite players. The higher incidence of recurrence reported in this study might also be due to stopping play and “resting” at the end of the players’ college seasons and then quickly starting up again at the start of summer league. The adherence of these athletes to conditioning programs for strength, endurance and flexibility may decrease during this “rest” period between seasons, although this was not monitored in the current study. These elite players may then quickly start their season or activity without consideration regarding conditioning. This suggestion should be considered by the sports medicine and conditioning staffs in order to prospectively target groups who have a prior history of HSI to incorporate the appropriate injury prevention activities into the start of the summer league season.
The amount of time lost from practice or competitive play can be significant and may have negative ramifications for both the individual's and the team's overall performance.41-44 Lower extremity injury for the purpose of this manuscript was defined to specifically encompass injury to the hamstring or the posterior thigh. The total number of days missed due to injury was quantified and each athlete's injuries were categorized by severity defined by the UEFA Consensus Statement.39
Historically, Powel et al report that 31% of injured high school baseball players missed more than seven days,2 while 25% of NCAA injuries were considered severe and players missed >10 days.3 The amount of time missed due to injury that was reported by the athletes who completed this survey (Table 4) is similar to other reports.1-3,5,27,45 Data from those publications are based on injury data bases and documentation from athletic trainers, physicians or other members of the sports medicine team. Given that data from the current study was based on retrospective recall of the HSI by the athlete, the ultimate accuracy of the data (under or over estimation of time missed) could be subject to question and recall accuracy or bias. However, the amount of time missed is still significant from a season participation perspective, and is aligned with other published reports.1-4 In this study 35% of all players who reported HSI reported that they lost between one and four weeks of play due to injury, and approximately 10% stated they lost more than four weeks. Efforts to prevent or reduce primary injury, or certainly the recurrence of injury would appear to be worth strong consideration.
Fifty six percent of players lost less than seven days of practice or play in this study with 40% reporting only one to three days lost from HSI. While this brief time loss (one to three days) might be attributable simply to “muscle soreness” from an alteration or change in their conditioning program once reporting to a summer league team, the report from any player of any time lost from practice or play must be carefully considered given the history of recurrence of HSI in an athletic population population.14 This study could not relate the type or amount of time lost due to injury to be typically associated with delayed onset muscle soreness (DOMS) that might be associated with the onset, change or increase of training load associated with being part of an elite summer league team as mentioned above. For this reason, the study attempted to have the players promptly fill out the questionnaire upon reporting to the team and prior to the commencement of summer league training if possible to minimize the impact of a change in their program.
All players (pitchers and position players) reported arm dominance for both batting and throwing (Table 5). While not statistically significantly different from other groups, players with HSI who batted Left and threw Right accounted for the largest percentage of HSI history (32%) within this group, followed by those who batted Left and threw Left (22%). A larger sample size may be necessary to achieve sufficient power to determine if any relationships exist between batting and throwing side and HSI. Exploring the relationship of batting and throwing preference and its’ association with HSI history in the NCAA or Major and Minor League Baseball injury surveillance system may be warranted. Players with HSI and who bat left-handed, may need to be considered for a rehabilitation or conditioning program to specifically address their risk. Further study of how left-handed hitters finish their swing, leave the batters’ box and sprint to first base may need to be considered for future research.
A statistically significant difference between all subscale scores and the total score of the HaOS was demonstrated between the two groups (Table 6). This type of finding is in agreement with investigations of athletes from other sports, such as elite level soccer, that used the HaOS.38 The HaOS is a good tool that may be used to identify players with prior HISI and potential risk for recurrent injury. This survey could help teams identify those players who need specific rehabilitation, training and conditioning programs to mitigate chance of injury recurrence or further injury.
As expected, there was a higher percentage of players with no history of HSI reporting symptoms “never or rarely” compared to players with a history of HSI (Table 7 and Table 8). Players with HSI reported “sometimes having symptoms or moderate symptoms” on a more frequent basis than non HSI players. The higher percentage of injured HSI players reporting “sometimes or having moderate” symptoms with baseball related running activity is in agreement with the findings of other studies that demonstrated that up to 76% of HSI occur with base running.3
As demonstrated by other reports, base running is considered to be a primary mechanism of HSI in baseball players.3,5,28 While the current study did not assess the mechanism of injury or when the injury occurred, athletes with HSI responded that they had more pain during baseball related activities such as rounding the bases, sprinting to first base or braking after first compared to those who did not have a history of HSI (Table 8). These baseball running activities are similar of those reported in other sports (sprinting, stopping/starting, change of direction) that are related to HSI. It should be noted that of the athletes who reported no HSI, 14% reported that they had also had pain sprinting to first base, and one third of this group responded that they had pain with stretching. Responses such as these may need to be considered in the design, incorporation and compliance with general stretching and conditioning programs, not only for baseball athletes with HSI, but also for those baseball players with no history of HSI, especially if the goal of these programs is injury prevention.
Each player was allowed to determine what “sore” meant or what “small injuries” meant when they filled out the HaOS questionnaire. “Soreness” and “small Injuries” may be interpreted differently by individuals. Given that this was a self-reported questionnaire the authors felt that it was best to let each athlete determine what this meant for themselves, rather forcing an operational definition that may not make sense to them.
While one might expect those players with HSI to report symptoms, a large percentage of athletes without a history of HSI also reported hamstring soreness in the week prior to the survey, were sore after their workout or had discomfort/pain with stretching (Table 7). However, they did not report time lost from practice or play. This report of soreness may have been associated with DOMS from transitioning between seasons or diversification of training programs associated with their summer league teams. The percentage of athletes answering “never or rarely/a little” was similar between the groups regarding soreness after a workout. However, the HSI group reported soreness “sometimes/moderate” more frequently than the non-HSI group. Soreness during a workout or that lingers may be something for sports medicine personnel to consider in helping to identify athletes at risk. Similar response percentages were demonstrated when athletes with and without a history of HSI answered a question on their perception of the “frequency of small injuries” they experience in their posterior thigh/hamstring area (Table 8). This should also be considered when attempting to identify the baseball player at risk.
The limitations of this study include that this survey is based on a retrospective self-report of injury rather than on objective data collected during the season by members of the sports medicine staff, hence being subject to inherent recall bias. However, the data is consistent with the current HSI rates reported in the baseball literature. In addition, the posterior thigh and hamstring injuries that were reported were not verified by any type of imaging study nor by a physician. However, these athletes are were NCAA athletes (largely Division I) and had access to physicians and certified Athletic Trainers (ATC) which may have been instrumental in diagnosis and treatment of previous injuries. In addition, both the Cape Cod League and the Northwoods League each have at least one ATC on staff. Since the summer league is a continuation of a competitive spring season, the notion of overload (training, innings played, etc.) and fatigue from continued play is a consideration. The athletes in this study were coming out of highly competitive programs, so ostensibly, their NCAA seasons could extend into late May and early June (including conference tournaments and potentially the College World Series).
Clinical Relevance and Conclusions
Understanding the prevalence of posterior thigh pain and HSI history in summer league baseball players will assist sports medicine staff in designing and implementing effective injury reduction and rehabilitation programs. The results of this study demonstrate that approximately one third of all position players and almost 13% of pitchers who report to summer league baseball, in hope of and preparation for being drafted by Major League Baseball, report a history of hamstring injury. Approximately one third of these injuries are bilateral. The reported reoccurrence rate of injury is greater than 25%. Reviewing the HSI history of summer league players would be useful at the start of the season. Consideration should then be given to developing appropriate injury reduction and optimal conditioning programs.
Appendix 1
References
- 1.Collins CL Comstock RD. Epidemiological features of high school baseball injuries in the United States, 2005-2007. Pediatrics. 2008;121(6):1181-1187. [DOI] [PubMed] [Google Scholar]
- 2.Powell JW Barber-Foss KD. Injury patterns in selected high school sports: a review of the 1995-1997 seasons. J Athl Train. 1999;34(3):277-284. [PMC free article] [PubMed] [Google Scholar]
- 3.Dick R Sauers EL Agel J, et al. Descriptive epidemiology of collegiate men's baseball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):183-193. [PMC free article] [PubMed] [Google Scholar]
- 4.Hootman JM Dick R Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319. [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad CS Dick RW Snell E, et al. Major and minor league baseball hamstring injuries: epidemiologic findings from the major league baseball injury surveillance system. Am J Sports Med.. 2014;42(6):1464-1470. [DOI] [PubMed] [Google Scholar]
- 6.Askling C Karlsson J Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13(4):244-250. [DOI] [PubMed] [Google Scholar]
- 7.Brooks JH Fuller CW Kemp SP Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297-1306. [DOI] [PubMed] [Google Scholar]
- 8.Croisier JL Forthomme B Namurois MH Vanderthommen M Crielaard JM. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30(2):199-203. [DOI] [PubMed] [Google Scholar]
- 9.Ekstrand J Healy JC Walden M Lee JC English B Hagglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112-117. [DOI] [PubMed] [Google Scholar]
- 10.Hagglund M Walden M Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767-772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Opar DA Williams MD Timmins RG Hickey J Duhig SJ Shield AJ. The effect of previous hamstring strain injuries on the change in eccentric hamstring strength during preseason training in elite Australian footballers. Am J Sports Med. 2015;43(2):377-384. [DOI] [PubMed] [Google Scholar]
- 12.Orchard J MJ Lord S Garlick D. . Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1999;25(1):81-85. [DOI] [PubMed] [Google Scholar]
- 13.Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6 Suppl):S2-8. [PubMed] [Google Scholar]
- 14.Thorborg K. What are the most important risk factors for hamstring muscle injury? Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2014;24(2):160-161. [DOI] [PubMed] [Google Scholar]
- 15.Kujala UM Orava S Jarvinen M. Hamstring injuries. Current trends in treatment and prevention. Sports Med (Auckland, NZ). 1997;23(6):397-404. [DOI] [PubMed] [Google Scholar]
- 16.Orchard J Marsden J Lord S Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25(1):81-85. [DOI] [PubMed] [Google Scholar]
- 17.Askling CM Malliaropoulos N Karlsson J. High-speed running type or stretching-type of hamstring injuries makes a difference to treatment and prognosis. Br J Sports Med. 2012;46(2):86-87. [DOI] [PubMed] [Google Scholar]
- 18.Cross KM Gurka KK Saliba S Conaway M Hertel J. Comparison of hamstring strain injury rates between male and female intercollegiate soccer athletes. Am J Sports Med. 2013;41(4):742-748. [DOI] [PubMed] [Google Scholar]
- 19.Hickey JT Timmins RG Maniar N Williams MD Opar DA. Criteria for progressing rehabilitation and determining return-to-play clearance following hamstring strain injury: A systematic review. Sports Med. (Auckland, NZ). 2017;47(7):1375-1387. [DOI] [PubMed] [Google Scholar]
- 20.Petersen J Thorborg K Nielsen MB Holmich P. Acute hamstring injuries in Danish elite football: a 12-month prospective registration study among 374 players. Scand J Med Sci Sports. 2010;20(4):588-592. [DOI] [PubMed] [Google Scholar]
- 21.Sherry MA Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J of orthopaedic and sports physical therapy. 2004;34(3):116-125. [DOI] [PubMed] [Google Scholar]
- 22.De Vos RJ Reurink G Goudswaard GJ Moen MH Weir A Tol JL. Clinical findings just after return to play predict hamstring re-injury, but baseline MRI findings do not. Br J Sports Med. 2014;48(18):1377-1384. [DOI] [PubMed] [Google Scholar]
- 23.Croisier JL. Factors associated with recurrent hamstring injuries. Sports Med.. 2004;34(10):681-695. [DOI] [PubMed] [Google Scholar]
- 24.Cross KM Gurka KK Saliba S Conaway M Hertel J. Comparison of thigh muscle strain occurrence and injury patterns between male and female high school soccer-athletes. J Sport Rehabil. 2017:1-35. [DOI] [PubMed] [Google Scholar]
- 25.Malliaropoulos N Ghrairi M Zerguini Y Padhiar N. Soft tissue injuries are still a challenge in musculoskeletal sports and exercise medicine. Br J Sports Med. 2016;50(24):1487. [DOI] [PubMed] [Google Scholar]
- 26.Opar DA Williams MD Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med.(Auckland, NZ). 2012;42(3):209-226. [DOI] [PubMed] [Google Scholar]
- 27.Seagrave RA 3rd Perez L McQueeney S Toby EB Key V Nelson JD. Preventive effects of eccentric training on acute hamstring muscle injury in professional baseball. Orthop J Sports Med. 2014;2(6):2325967114535351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalton SL Kerr ZY Dompier TP. Epidemiology of Hamstring Strains in 25 NCAA Sports in the 2009-2010 to 2013-2014 Academic Years. Am J Sports Med. 2015. [DOI] [PubMed] [Google Scholar]
- 29.Hagglund M Walden M Ekstrand J. Risk factors for lower extremity muscle injury in professional soccer: the UEFA Injury Study. Am J Sports Med. 2013;41(2):327-335. [DOI] [PubMed] [Google Scholar]
- 30.Shield AJ Bourne MN. Hamstring injury prevention practices in elite sport: evidence for eccentric strength vs. lumbo-pelvic training. Sports Med.. 2018;48(3):513-524. [DOI] [PubMed] [Google Scholar]
- 31.Bourne MN Duhig SJ Timmins RG, et al. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: implications for injury prevention. Br J Sports Med. 2017;51(5):469-477. [DOI] [PubMed] [Google Scholar]
- 32.Al Attar WSA Soomro N Sinclair PJ Pappas E Sanders RH. Effect of Injury prevention programs that Include the nordic hamstring exercise on hamstring injury rates in soccer players: A systematic review and meta-analysis. Sports Med. 2017;47(5):907-916. [DOI] [PubMed] [Google Scholar]
- 33.Almeida MO Maher CG Saragiotto BT. Prevention programmes including Nordic exercises to prevent hamstring injuries in football players (PEDro synthesis). Br J Sports Med. 2018. [DOI] [PubMed] [Google Scholar]
- 34.Ribeiro-Alvares JB Marques VB Vaz MA Baroni BM. Four weeks of nordic hamstring exercise reduce muscle injury risk factors in young adults. J Strength Condit Research. 2018;32(5):1254-1262. [DOI] [PubMed] [Google Scholar]
- 35.Sugiura Y Sakuma K Sakuraba K Sato Y. Prevention of hamstring injuries in collegiate sprinters. Orthop J Sports Med. 2017;5(1):2325967116681524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van der Horst N. Preventing hamstring injuries in football through enhanced exercise and RTP strategies. Br J Sports Med. 2018;52(10):684-685. [DOI] [PubMed] [Google Scholar]
- 37.Bahr R Thorborg K Ekstrand J. Evidence-based hamstring injury prevention is not adopted by the majority of Champions League or Norwegian Premier League football teams: the Nordic Hamstring survey. Br J Sports Med. 2015;49(22):1466-1471. [DOI] [PubMed] [Google Scholar]
- 38.Engebretsen AH Myklebust G Holme I Engebretsen L Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38(6):1147-1153. [DOI] [PubMed] [Google Scholar]
- 39.Fuller CW Ekstrand J Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clinl J Sports Med. 2006;16(2):97-106. [DOI] [PubMed] [Google Scholar]
- 40.Dalton SL Kerr ZY Dompier TP. Epidemiology of hamstring strains in 25 ncaa sports in the 2009-2010 to 2013-2014 academic years. Am J Sports Med. 2015;43(11):2671-2679 [DOI] [PubMed] [Google Scholar]
- 41.Clarsen B Bahr R. Matching the choice of injury/illness definition to study setting, purpose and design: one size does not fit all! Br J Sports Med. 2014;48(7):510-512. [DOI] [PubMed] [Google Scholar]
- 42.Hodgson L Gissane C Gabbett TJ King DA. For debate: consensus injury definitions in team sports should focus on encompassing all injuries. Clin J Sports Med. 2007;17(3):188-191. [DOI] [PubMed] [Google Scholar]
- 43.Mueller-Wohlfahrt HW Haensel L Mithoefer K, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47(6):342-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rae K Orchard J. The Orchard sports injury classification system (osics) version 10. Clin J Sports Med. 2007;17(3):201-204. [DOI] [PubMed] [Google Scholar]
- 45.Camp CL Dines JS van der List JP, et al. Summative report on time out of play for major and minor league baseball: An analysis of 49,955 injuries from 2011 through 2016. Am J Sports Med. 2018;46(7):1727-1732. [DOI] [PubMed] [Google Scholar]