Azithromycin is a component of empirical treatment regimens for Neisseria gonorrhoeae infections, but antimicrobial susceptibility testing for this agent is technically challenging. We compared the intertest variability, MIC values, and CLSI/EUCAST categorization of clinical and reference isolates of N. gonorrhoeae treated with azithromycin by testing 107 clinical isolates and nine reference isolates by agar dilution and in duplicates using MIC test strips (Liofilchem, Italy) and Etests (bioMérieux, France).
KEYWORDS: agar dilution, azithromycin, Etest, gradient MIC, MIC test strip, Neisseria gonorrhoeae, variability, breakpoints
ABSTRACT
Azithromycin is a component of empirical treatment regimens for Neisseria gonorrhoeae infections, but antimicrobial susceptibility testing for this agent is technically challenging. We compared the intertest variability, MIC values, and CLSI/EUCAST categorization of clinical and reference isolates of N. gonorrhoeae treated with azithromycin by testing 107 clinical isolates and nine reference isolates by agar dilution and in duplicates using MIC test strips (Liofilchem, Italy) and Etests (bioMérieux, France). Replicate isolate agreement within 1 log2 between duplicate tests was 87% for MIC test strips and 100% for Etests (P < 0.001). Essential agreement with the agar dilution method was higher for Etests (91%) than for MIC test strips (44%, P < 0.001). The geometric mean MIC was highest for MIC test strips (0.8 mg/liter) and significantly higher than both Etest (0.47 mg/liter, P < 0.001) and agar dilution (0.26 mg/liter, P < 0.001) methods. Etest MICs were higher than those obtained with agar dilution (P < 0.001). Agar dilution, MIC test strip, and Etest methods categorized 96%, 85%, and 95% (P = 0.003) of clinical isolates, respectively, as susceptible/wild type according to CLSI/EUCAST criteria. Our results illustrate the difficulties underlying azithromycin susceptibility testing for N. gonorrhoeae and demonstrate that results can vary using different methods. This variability could influence antimicrobial resistance reporting between laboratories involved in N. gonorrhoeae surveillance programs.
INTRODUCTION
Antimicrobial resistance is an important factor undermining treatment of Neisseria gonorrhoeae infections worldwide (1). Current empirical treatment regimens usually include azithromycin in combination with other antibiotics. Robust surveillance for azithromycin susceptibility is warranted, as resistance is increasing worldwide (2), likely due to increased use of macrolides for other indications in the general population (3). However, antimicrobial susceptibility testing for azithromycin is technically challenging due to the need to use MIC techniques, issues with reproducibility of results, and limited clinical outcome data to define breakpoints. These challenges were compounded until recently by the lack of interpretative criteria (4). As a result, essential surveillance information for azithromycin is limited, particularly in low- and middle-income countries (1).
Non-wild-type azithromycin strains have acquired mutations that block the interaction of the drug with its binding site or promote efflux of the drug (e.g., mtrR promoter mutations). Mutations in 23S rRNA, e.g., C2611T and A0259G, particularly those that involve all four alleles, have been associated with treatment failures (4).
Agar dilution is the gold standard for determining the MIC of azithromycin against N. gonorrhoeae, but it is labor intensive, is time consuming, and does not present results in a clinically relevant time frame (5). There are now several azithromycin gradient MIC strips available, and the limited comparison studies available demonstrate promising equivalence of these methods (5–7).
Our laboratory tests N. gonorrhoeae isolates, predominantly derived from patients attending the Auckland Regional Sexual Health Service for antimicrobial susceptibility against several antibiotics (8), and annually submits gonococcal antimicrobial susceptibility data to the World Health Organization (WHO) Western Pacific Region gonococcal antimicrobial surveillance program (GASP). Testing of N. gonorrhoeae isolates for azithromycin using MIC test strips (Liofilchem, Italy) started in mid-2017. Rates of nonsusceptibility to azithromycin in the latter 6 months of 2017 were high, with 20% of isolates categorized as resistant according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria at that time (9). Consequently, we sought to compare the performance of different methods of azithromycin MIC determination for clinical isolates and reference strains of N. gonorrhoeae.
MATERIALS AND METHODS
One hundred sixteen N. gonorrhoeae isolates, comprising 107 clinical isolates, and nine reference strains were included in the study. The clinical isolates were obtained from consecutive nonduplicate samples submitted to the LabPLUS Microbiology Department from 30 June 2017 to 4 November 2017. Isolates were originally tested using gradient diffusion strips (MIC test strip; Liofilchem, Roseto degli Abruzzi, Italy) and stored at −80°C. The reference isolates tested were those provided by the GASP 2018 external quality assurance program, Western Pacific Region.
For the study, each clinical isolate and controls were thawed, subcultured twice, initially onto New York City agar (Fort Richard, Auckland, New Zealand) and then chocolate agar (Fort Richard, Auckland, New Zealand); each subculture was then incubated for 20 to 24 h at 36 ± 1°C in 5% CO2.
The azithromycin gradient diffusion method (range, 0.016 to 256 mg/liter) was performed using the commercially available assays from the two manufacturers: MIC test strip (Liofilchem, Roseto degli Abruzzi, Italy) and Etest (bioMérieux, Marcy-l’Etoile, France). The testing was carried out on GC agar base (Difco, BD, Sparks, MD) supplemented with 1% Remel GCHI Enrichment (Thermo Scientific, Waltham, MA), called GCS agar, prepared in-house according to the manufacturer’s instructions and stored in sealed plastic bags for 2 to 3 days at 4°C prior to use. A 0.5 McFarland suspension in 0.9% saline was prepared for each isolate, evenly spread using a cotton swab onto GCS agar, and allowed to dry for 10 min before the azithromycin strips were applied and immediately incubated at 36 ± 1°C in 5% CO2. Following 20 to 24 h of incubation, the MICs were determined by reading the lowest antibiotic concentration that inhibited growth, according to the manufacturers’ instructions. Testing was performed in duplicates on separate days for Etest, once for the MIC test strip (in order to obtain duplicate results), and all results were read by two operators. Where operators disagreed with the interpretation, arbitration was by repeat testing. N. gonorrhoeae ATCC 49226 and WHO P were used as quality control (QC) strains and were within the QC range for each run.
The azithromycin agar dilution (range, 0.03 to 256 mg/liter) was performed according to the Clinical and Laboratory Standards Institute (CLSI) agar dilution method (10). A stock solution of azithromycin powder (Sigma-Aldrich, St. Louis, MO) was prepared, and aliquots were stored at −80°C. On the day of preparation of each dilution series, the required volume of GCS agar was prepared, and the azithromycin working solution and double dilution concentrations from 0.03 to 256 mg/liter were prepared from the thawed stock solution. Each dilution was then added to the base medium, poured into labeled plates, allowed to set, and stored in sealed plastic bags at 4°C. Each azithromycin agar dilution series was used within a day of preparation.
For the agar dilution susceptibility procedure, a 0.5 McFarland suspension in 0.9% saline (108 CFU/ml) was prepared for each isolate and diluted 1:10 to give 107 CFU/ml and using a Steer’s replicator. A final inoculum of 104 CFU/ml was inoculated to the surface of each plate. The plates were then incubated for 20 to 24 h at 35 ± 1°C in 5% CO2, following which the MICs were determined by reading the lowest antibiotic concentration that inhibited growth.
Data analysis.
The MIC values were rounded up to the nearest doubling dilution (log2) with essential agreement defined as within one log2 dilution. For duplicates, the highest MIC was recorded. The percentage agreement was determined from gradient MIC values that were within one log2 dilution of the agar dilution MIC value. Chi-square or Fisher exact tests were used to compare groups. Wilcoxon signed-rank test and Student's t test was used to compare paired and unpaired MICs, respectively.
RESULTS
In total, 116 N. gonorrhoeae isolates were tested using agar dilution and in duplicated using MIC test strips and Etest gradient MICs. These comprised 107 consecutive nonduplicate clinical isolates and nine reference isolates. Replicate isolate agreement within one log2 between duplicate tests was lower for the MIC test strip (86%) than for the Etest (100%) (P < 0.001) (Table 1).
TABLE 1.
Test reproducibility: within method agreement for MIC test strip and Etest MIC values between two repeats for clinical and reference isolates
| Isolate type | No. of isolates tested in duplicates | Gradient MIC range (mg/liter) | No. (%) of isolates with MIC difference between replicates of: |
||
|---|---|---|---|---|---|
| ±1 Log2 dilution | ±2 Log2 dilution | ±>2 Log2 dilution | |||
| MIC test strip | |||||
| Clinical | 107 | 0.06 to 16.0 | 92 (86) | 14 | 1 |
| Reference | 9 | 0.5 to >256 | 9 (100) | 0 | 0 |
| Etest | |||||
| Clinical | 107 | 0.06 to 8 | 107 (100) | 0 | 0 |
| Reference | 9 | 0.5 to >256 | 9 (100) | 0 | 0 |
Compared with agar dilution, agreement, within one log2 dilution, was lower for the MIC test strip (52/116 [46%]) than for the Etest (106/116 [91%]) (P < 0.001) (Table 2). The MIC test strip agreement with Etest MICs was higher, with 95/107 (88%) clinical isolates testing within one log2 dilution of the other gradient strip method.
TABLE 2.
Summary of MIC determinations using MIC test strip and Etest azithromycin gradient MICs compared to agar dilution MIC valuesa
| Method | No. of isolates with MIC difference versus agar dilution of: |
Essential agreement (n [%]) | Categorical agreement (n [%]) | ||||
|---|---|---|---|---|---|---|---|
| ≥−2 Log2 dilution | −1 Log2 dilution | 0 | +1 Log2 dilution | ≥+2 Log2 dilution | |||
| QC strains (n = 9) | |||||||
| MIC test strip | 0 | 0 | 1 | 4 | 4 | 5 (56) | 8 (89) |
| Etest | 0 | 0 | 4 | 5 | 0 | 9 (100) | 9 (100) |
| Clinical isolates (n = 107) | |||||||
| MIC test strip | 0 | 0 | 4 | 43 | 60 | 47 (44) | 96 (90) |
| Etest | 0 | 2 | 26 | 69 | 10 | 97 (91) | 106 (99) |
The higher MIC of replicate gradient strips was used.
Using the current CLSI/EUCAST criteria, 96%, 85%, and 95% (P = 0.003) of clinical isolates were categorized as susceptible (11)/wild type (12) by agar dilution, MIC test strip, and Etest methods, respectively.
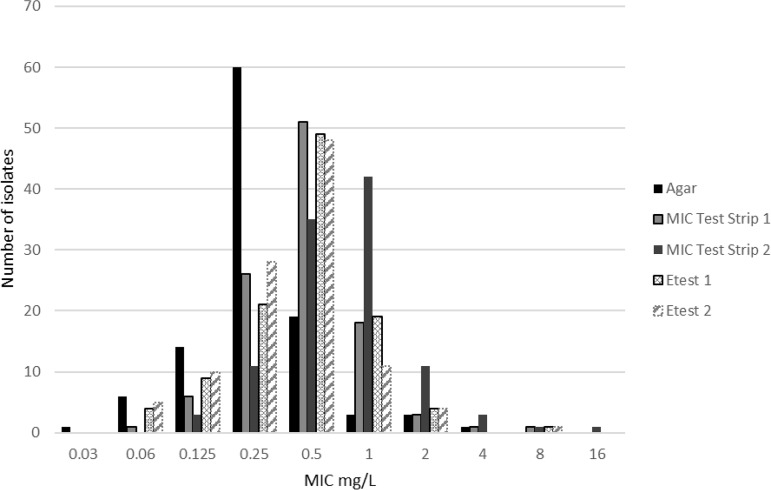
The geometric mean MIC was higher for isolates tested using the MIC test strip (0.80 mg/liter) than using the Etest (0.47 mg/liter) and agar dilution (0.26 mg/liter), and the MIC50 and MIC90 also varied between methods (Table 3). The distribution of MICs by method is shown in Fig. 1. The MICs for isolates tested by the MIC test strip and Etest were higher than those for the same isolates tested by agar dilution (P < 0.001) and higher for the MIC test strip than for the Etest (P < 0.001). These significant differences between MICs according to methods also held true if the lower MIC of the MIC test strip or Etest replicate was considered, with a higher geometric mean MIC for the MIC test strip (0.45 mg/liter) than for both the Etest (0.35 mg/liter P = 0.002) and agar dilution (0.26 mg/liter P < 0.001) method, and a higher geometric mean MIC with the Etest than with agar dilution (P < 0.001).
TABLE 3.
Comparison of MICs and CLSI categorical criteria for 107 clinical isolates by CLSI reference agar dilution, MIC test strip, and Etesta
| Method | No. (%) of susceptible isolates | P value | MIC (mg/liter) |
|||
|---|---|---|---|---|---|---|
| 50% | 90% | Mode | Geometric mean | |||
| Agar dilution | 103 (96) | 0.25 | 0.5 | 0.25 | 0.26 | |
| MIC test strip | 91 (85) | 0.01 | 1 | 2 | 1 | 0.79 |
| Etest | 102 (95) | 0.73 | 0.5 | 1 | 0.5 | 0.47 |
The higher MIC of replicate gradient strips is presented.
FIG 1.
Comparison of MIC values for clinical isolates by testing method: agar dilution, MIC test strip, and Etest. Replicate MIC values are provided for gradient strip methods.
For the WHO reference isolates, using the MIC test strip, 2/9 MICs were outside the given external quality assurance reference range, whereas all agar dilution and Etest values fell within the given ranges (Table 4).
TABLE 4.
Reference isolate MIC resultsa
| Reference strain | MIC (mg/liter) from: |
|||||
|---|---|---|---|---|---|---|
| Reference strain expected range | Agar dilution | MIC test strip 1 | MIC test strip 2 | Etest 1 | Etest 2 | |
| 18GQ01 | 2–8 | 4 | 16 | 32 | 4 | 2 |
| 18GQA02 | 0.5–2 | 0.5 | 1 | 1 | 1 | 0.5 |
| 18GQA03 | >256 | >256 | >256 | >256 | >256 | >256 |
| 18GQA04 | 0.125–0.5 | 0.25 | 0.5 | 0.5 | 0.5 | 0.5 |
| 18GQA05 | 0.125–0.5 | 0.25 | 0.5 | 1 | 0.5 | 0.5 |
| 18GQA06 | 0.5–2 | 1 | 2 | 2 | 1 | 1 |
| WHO L GQA18 | 0.25–1 | 0.25 | 1.0 | 0.5 | 0.5 | 0.25 |
| WHO P GQA18 | 2–8 | 2 | 8 | 8 | 4 | 4 |
| ATCC 49226 GQA18 | 0.25–1 | 0.5 | 0.5 | 1 | 0.5 | 0.5 |
Individual replicate MIC values are presented (WHO GASP quality assurance program, 2018). For data analysis, the higher of replicate MICs was used.
Multiple lots of gradient strips were tested sequentially during the study (MIC test strip lots: 72016024, 92016130, 12417092, and 41618028; Etest lots: 1006341260 and 1006730870). Mean MICs were higher for MIC test strip lot 41618028 than for other lots (0.790 mg/liter versus 0.456 mg/liter, respectively, P = 0.01), whereas they did not differ significantly for Etest lots (0.389 mg/liter versus 0.387 mg/liter, P = 0.32). No association was apparent for GC agar batches.
DISCUSSION
Azithromycin resistance is an emerging issue globally (2) and locally in New Zealand (13). Resistance is concerning, because the currently recommended empirical dual treatment regime relies on azithromycin to protect ceftriaxone activity (14), and high rates of resistance to this agent could hasten development of ceftriaxone resistance.
We compared the performance of two gradient MIC strips, the Etest and MIC test strip, for MIC determination of clinical and reference isolates of N. gonorrhoeae against the reference method of agar dilution, and we found that there were significant differences in the MICs depending on the gradient strip used. This variability was most striking for the MIC test strip, which demonstrated poor agreement (44%) for clinical isolates compared with agar dilution results, and provided out-of-range results for 2/9 WHO quality assurance reference strains.
In contrast, Etest MICs were more comparable to agar dilution results, demonstrating 91% essential agreement with the reference method. Similar findings have been reported for Etest and the agar dilution MIC method previously (6, 15) and support the use of the Etest for the determination of N. gonorrhoeae susceptibility to azithromycin for the use in surveillance programs.
However, the mean and modal MICs obtained by both gradient strip methods were higher than those determined by the agar dilution MIC method. In consequence, agreement between the two gradient strip methods was higher (88%) than that obtained for each method compared with the agar dilution MIC method, consistent with a previous study which found good agreement when comparing the Etest and the MIC test strip (7). This finding is notable as it suggests that future comparison studies of gradient MIC strips should continue to include the agar dilution MIC method as the reference method.
Recently, CLSI introduced a susceptible-only breakpoint for azithromycin (4), and in January 2019, EUCAST replaced their previous breakpoints with an epidemiological cutoff value (ECOFF); both institutes set their values at 1 mg/liter (12). These changes reflect uncertainties around microbiological and clinical failure rates for individuals harboring strains of N. gonorrhoeae with azithromycin MICs of >1 mg/liter, particularly when administered with another agent (4).We found that 4% of samples tested using the agar dilution MIC method, 5% using Etests, and 15% using MIC test strips did not fall within the CLSI susceptible breakpoint/tested above the EUCAST ECOFF. The proportion of samples above the susceptible breakpoint/ECOFF was significantly higher using the MIC test strip, in keeping with the higher MICs for isolates tested using this method.
We are not aware that these findings have been reported before, and they imply that differing methods could account, in part, for differences in azithromycin susceptibility rates between laboratories partaking in national or supranational surveillance activities. However, we recognize the need for further studies in order to confirm the validity and generalizability of our findings.
In particular, we recognize that agar dilution was performed once for isolates, and though, in our laboratory, we find this method reproducible for clinical and quality control strains, it is possible that the medium quality may have biased the results.
We also recognize that we present only phenotypic results for our clinical isolates and reference strains. Molecular sequence data were available for WHO reference strains L and P (16), and phenotypic susceptibility results were consistent with genotypic results for these strains, with azithromycin MICs above the CLSI breakpoint for WHO P conferred by an mtrR promoter sequence mutation promoting macrolide efflux.
Prior to January 2019, EUCAST published susceptible/intermediate/resistant (SIR) breakpoints for azithromycin (9). Interpretation of our isolate MICs using these breakpoints illustrates more significant differences between the methods used, with resistance rates of 57% for the MIC test strip and 23% for Etest compared with 7% for agar dilution, likely due to issues with reproducibility and clustering of isolates around these breakpoints (4). These findings support EUCAST’s decision to remove the SIR breakpoints.
In summary, we compared azithromycin susceptibility testing for Neisseria gonorrhoeae using two gradient strip methods. We found significant differences in intertest variability, MIC essential agreement, and EUCAST/CLSI categorization dependent on the method used. Our findings suggest that the methods used for azithromycin categorization should be considered when comparing the results from antimicrobial surveillance programs.
REFERENCES
- 1.World Health Organization. 2014. Antimicrobial resistance: global report on surveillance, 2014. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.George CRR, Enriquez RP, Gatus BJ, Whiley DM, Lo YR, Ishikawa N, Wi T, Lahra MM. 2019. Systematic review and survey of Neisseria gonorrhoeae ceftriaxone and azithromycin susceptibility data in the Asia Pacific, 2011 to 2016. PLoS One 14:e0213312. doi: 10.1371/journal.pone.0213312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olesen SW, Torrone EA, Papp JR, Kirkcaldy RD, Lipsitch M, Grad YH. 2019. Azithromycin susceptibility among Neisseria gonorrhoeae isolates and seasonal macrolide use. J Infect Dis 219:619–623. doi: 10.1093/infdis/jiy551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kersh EN, Allen V, Ransom E, Schmerer M, St Cyr S, Workowski K, Weinstock H, Patel J, Ferraro MJ. 9 April 2019. Rationale for a Neisseria gonorrhoeae susceptible only interpretive breakpoint for azithromycin. Clin Infect Dis doi: 10.1093/cid/ciz292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enriquez RP, Goire N, Kundu R, Gatus BJ, Lahra MM. 2016. A comparison of agar dilution with the calibrated dichotomous sensitivity (CDS) and Etest methods for determining the minimum inhibitory concentration of ceftriaxone against Neisseria gonorrhoeae. Diagn Microbiol Infect Dis 86:40–43. doi: 10.1016/j.diagmicrobio.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Papp JR, Rowlinson M-C, O'Connor NP, Wholehan J, Razeq JH, Glennen A, Ware D, Iwen PC, Lee LV, Hagan C. 2018. Accuracy and reproducibility of the Etest to detect drug-resistant Neisseria gonorrhoeae to contemporary treatment. J Med Microbiol 67:68–73. doi: 10.1099/jmm.0.000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jönsson A, Jacobsson S, Foerster S, Cole MJ, Unemo M. 2018. Performance characteristics of newer MIC gradient strip tests compared with the Etest for antimicrobial susceptibility testing of Neisseria gonorrhoeae. APMIS 126:822–827. doi: 10.1111/apm.12887. [DOI] [PubMed] [Google Scholar]
- 8.McAuliffe G, Smith M, Brokenshire M, Forster R, Reid M, Roberts S. 2018. Keeping track of antimicrobial resistance for Neisseria gonorrhoeae in Auckland, New Zealand: past, present and future considerations. N Z Med J 131:71–77. [PubMed] [Google Scholar]
- 9.European Committee on Antimicrobial Susceptibility Testing. 2015. Breakpoint tables for interpretation of MICs and zone diameters. Version 5.0, 2015. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_5.0_Breakpoint_Table_01.pdf.
- 10.Clinical and Laboratory Standards Institute. 2018. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, 11th ed Document M07-A10 Clinical Laboratory and Standards Institute, Wayne, PA. [Google Scholar]
- 11.Clinical Laboratory and Standards Institute. 2019. Performance standards for antimicrobial susceptibility testing, 29th ed Document M100-29 Clinical Laboratory and Standards Institute, Wayne, PA. [PubMed] [Google Scholar]
- 12.European Committee on Antimicrobial Susceptibility Testing. 2019. Breakpoint tables for interpretation of MICs and zone diameters, version 9.0, 2019. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_9.0_Breakpoint_Tables.pdf.
- 13.Lee RS, Seemann T, Heffernan H, Kwong JC, Gonçalves da Silva A, Carter GP, Woodhouse R, Dyet KH, Bulach DM, Stinear TP, Howden BP, Williamson DA. 2018. Genomic epidemiology and antimicrobial resistance of Neisseria gonorrhoeae in New Zealand. J Antimicrob Chemother 73:353–364. doi: 10.1093/jac/dkx405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. 2015. Sexually transmitted diseases treatment guidelines. Centers for Disease Control and Prevention, Atlanta, GA. [Google Scholar]
- 15.Gose S, Kong CJ, Lee Y, Samuel MC, Bauer HM, Dixon P, Soge OO, Lei J, Pandori M. 2013. Comparison of Neisseria gonorrhoeae MICs obtained by Etest and agar dilution for ceftriaxone, cefpodoxime, cefixime and azithromycin. J Microbiol Methods 95:379–380. doi: 10.1016/j.mimet.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Unemo M, Golparian D, Sánchez-Busó L, Grad Y, Jacobsson S, Ohnishi M, Lahra MM, Limnios A, Sikora AE, Wi T, Harris SR. 2016. The novel 2016 WHO Neisseria gonorrhoeae reference strains for global quality assurance of laboratory investigations: phenotypic, genetic and reference genome characterization. J Antimicrob Chemother 71:3096–3108. doi: 10.1093/jac/dkw288. [DOI] [PMC free article] [PubMed] [Google Scholar]