Abstract
[Purpose] This study aimed to measure the thickness of the muscles located on the ventral side of the hip joint and to identify the muscles involved in exercise against the load that results in femoral head translation in the ventral direction, which can be used as an index of exercise performance for the prevention and improvement of hip joint disease caused by femoral head translation. [Participants and Methods] The participants were 10 healthy young males. During the measurement task, we asked them to hold a 10 kgf load in the ventral direction to the femoral head in the supine position. We measured the thickness of the gluteus minimus, gluteus medius, tensor fascia latae, and iliopsoas both at rest and during exercise using ultrasonography. [Results] We compared muscle thicknesses at rest and during exercise and found that only the gluteus minimus had significantly lower values during exercise. We also compared the rate of change in muscle thickness and found that the gluteus minimus exhibited significantly higher values than those of the gluteus medius and tensor fasciae latae. [Conclusion] Our study indicates that the gluteus minimus is more involved than the gluteus medius, tensor fasciae latae, and iliopsoas in the exercise for the ventral displacement of the femoral head.
Keywords: Hip joint, Stabilization exercise, Ultrasonography
INTRODUCTION
The hip joint is structurally more stable than the scapulohumeral joint that is the same ball and socket joint. It has the femoral head that fits in the acetabulum, and it is strongly reinforced by the tissue around the joint1). The stability of the hip joint depends on many ligaments including iliofemoral ligament, pubofemoral ligament, ischiofemoral ligament, ligamentum teres, zona orbicularis, and deep arcuate ligament, all of which work closely to reinforce the joint capsule2). In addition to stabilizing those ligaments, the acetabular labrum plays a role to stabilize the hip joint because it increases the depth of the acetabulum and helps hip joint maintain a partial vacuum in it3). Although the hip joint is structurally stable, it has movements that are accessory physiologically. This has been confirmed by cadaveric study and ultrasonography4, 5). It is reported that the range of accessory movements of the hip joint vary with individual greatly. Studies on healthy adults report that accessory movements of the hip joint are about 2 mm long on average5). The femoral head glides to the dorsal direction during hip flexion and moves in the ventral direction during extension as a movement that is accessory physiologically6). The treatment to improve the decreased accessory movements for wider range of motion is known as joint mobilization5). In recent years, however, microinstability means not head position abnormalities hardly noticeable like femoral head position abnormality but the state in which accessory movement occurs excessively7). It is caused by the failure of passive stabilization mechanisms, such as bone structure, cartilage, capsule, ligament system, tendon, and acetabular labrum2, 3). A failure of the passive stabilization mechanism increases femoral head translation8,9,10), leading to a degenerative disease of the hip joint3). In particular, Sharman et al. designated excessive movements of the femoral head in the ventral direction as “femoral anterior glide syndrome” and reported that they are likely to occur not only in trauma but also in the movement where strong hip extension is performed repetitively6). Panjabi et al.11) recommends compensating the stability with the help of muscles to treat a failure of the passive stabilization mechanism. Based on the study on factors that activate the stabilization mechanism, Lewis et al.12, 13) reported that a decrease in the activity of iliopsoas muscle (IL) causes an increase in the deflection in the direction of venter during the flexion of hip joint. The IL has the function to stabilize the hip joint like rotator cuff muscles at the shoulder. It presumably not only contributes to the stabilization of the hip joint by muscle contraction but also helps the musculotendinous unit function as the anterior wall of the hip joint for the stabilization of the hip joint12). In addition, the anterior part of gluteus minimus (AGMI) and gluteus medius (AGME) supposedly controls femoral head translation3, 14,15,16). The muscle on the ventral side of the hip joint, such as IL, AGMI, and AGME, supposedly pulls the femoral head ventrally if only the muscle arrangement is taken into consideration. If, however, the stabilization mechanism mentioned above besides the muscle arrangement is taken into consideration, the function of muscle on the ventral side of the hip joint is unknown in the movement against the load that moves the femoral head in the ventral direction.
This study aimed to measure the thickness of the muscle located on the ventral side of the hip joint and to identify the muscles involved in exercise against the load that results in femoral head translation in the ventral direction, which can be used as an index of exercise performance for the prevention and improvement of hip joint disease caused by femoral head translation.
PARTICIPANTS AND METHODS
This study was participated by 10 healthy young males without complaints of pain that affects daily life, and subjects of the study were their dominant legs that they use to kick a ball. Mean (± standard deviation) age, height, and weight were 25.2 ± 4.5 years, 172.7 ± 4.9 cm, and 69.6 ± 6.35 kg, respectively. None of the participants had a history of orthopedic problems with legs or vertebrae. The protocol of this study was approved by the Ethics Committee of Saiseikai Kanazawa Hospital (Approval Number: Application No. 23 for 2018). Before the study, we explained objective and content of the study to the participants and told them that we will not use the data we obtain from this study for any other purpose than this study and that we will handle them strictly in confidence to prevent the leakage of personal information. We obtained written informed consent from all the participants before the study.
The measurement position was a supine position in the neutral position of the hip joint. The measurement task was the exercise to hold the femoral head in the ventral direction against the load (stabilization exercise). We fixed the pelvis and the distal part of the femur of the measurement limb with a belt to prevent joint movement of the hip joint from occurring during measurement. We created the ventral load on the femoral head by inserting a deflated ball on the dorsal side of the femoral head (distal to the ischial tuberosity) and loaded it by inflating the ball using an air pump (Fig. 1).
Fig. 1.
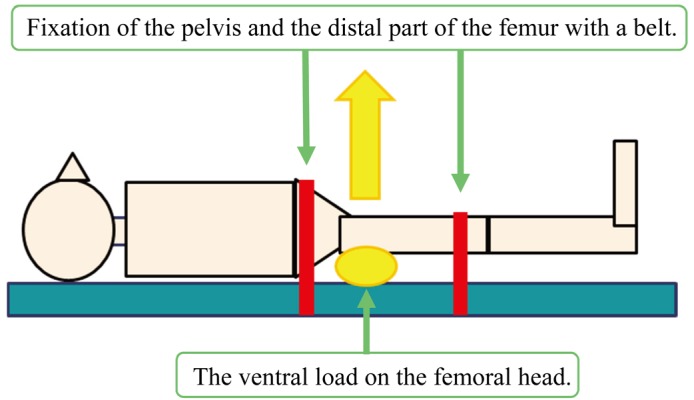
The measurement position.
We adjusted the load to make it 10 kgf using a hand-held dynamometer (Morby, Sakai Medical Co., Ltd., Tokyo, Japan) beforehand. We instructed the participants to hold the load up to the degree that they can hold any more and asked them not to use more strength than necessary. We measured muscle thickness using a linear probe (10 MHz) in B mode of an ultrasonography (LOGIQ e, GE Healthcare Japan, Tokyo, Japan), and the IL, AGME, AGMI, and imaged tensor fasciae latae (TFL) at rest and during stabilization exercise. We measured each trial twice. The measurement points of the AGME, AGMI, and TFL were at the distal 1/3 part of the line connecting the spina iliaca anterior superior, and the greater trochanter. Using Image J that is an image analysis program, we measured the thickness of each muscle on the basis of the fascia boundary with the help of the ultrasound image. We calculated average values of the two measurements and used them as muscle thickness values.
We used SPSS Ver. 24 (IBM SPSS Statistics, Japan IBM, Tokyo, Japan) for statistical analysis. After confirming whether the data have a normal distribution using the Shapiro-Wilk test, we compared muscle thicknesses at rest and those during stabilization exercise using paired t-test. To compare change rates of thickness (at rest/stabilizing exercise) of each muscle, we used one-way analysis of variance and Bonferroni multiple comparison to compare change rates of muscle thickness (at rest/stabilization exercise) of each muscle and considered values of p<0.05 as significant.
RESULTS
Table 1 shows the thickness at rest and during the stabilization exercise of each muscle, and Table 2 shows change rates of muscle thickness. All values are expressed as mean ± SD (standard deviation). We compared muscle thicknesses at rest and those during stabilization exercise and found that only AGMI was significantly lower during stabilization exercise than at rest and that none of other muscles was significantly different (Table 1). As for change rate of thickness of each muscle, we found that AGMI was significantly higher than AGME and TFL (Table 2).
Table 1. The thickness at rest and during the stabilization exercise of each muscle.
| Rest (cm) | Stabilization exercise (cm) | 95% confidence interval | ||
|---|---|---|---|---|
| The anterior part of gluteus minimus | 1.84 ± 0.35 | 1.66 ± 0.42* | 0.19 | 0.33 |
| The anterior part of gluteus medius | 1.23 ± 0.51 | 1.32 ± 0.48 | −0.27 | 0.10 |
| Tensor fascia latae | 1.38 ± 0.29 | 1.26 ± 0.33 | −0.23 | 0.04 |
| Iliopsoas | 2.87 ± 0.53 | 2.86 ± 0.55 | −0.03 | 0.04 |
*Significant difference compared to rest (p<0.05).
Table 2. Change rates of muscle thickness at rest/stabilization exercise (%).
| The anterior part of gluteus minimus | 113 |
| The anterior part of gluteus medius | 95* |
| Tensor fascia latae | 95* |
| Iliopsoas | 100 |
*Significant difference compared to gluteus minimus (p<0.05).
DISCUSSION
In this study, we wished to measure the thickness of muscle on the ventral side of the hip joint and clarify what muscles are involved in the exercise using the load that displaces the femoral head in the ventral direction. According to the results of this study, we found that the muscle thickness of AGMI was lower during stabilization exercise than at rest. Pappas et al.17) reported that changes in muscle morphology during muscle contraction are different at longitudinal muscle sites of the same muscle. Furthermore, Kinugasa et al.18) reported that because the muscle volume is constant, the muscle cross-sectional area decreases when the muscle stretches in the longitudinal direction. When muscle contraction occurs, the muscle cross-sectional area increases due to muscle shortening in some sites and decreases due to stretching along the muscle long axis in some sites. Therefore, it is presumed that muscle thickness decreases instead of increasing at the time of muscle contraction depending on the measurement site even in measurement performed by ultrasound imaging. The degree of change in muscle thickness cannot be an indicator to show the degree of muscle activity not only because of the effect on muscle thickness of the above measurement point but also because of several factors including extensibility and contraction pattern of muscle and fascia19). However, there is a possibility that change in muscle thickness activated the AGMI, though the degree of muscle activity is unknown. Simply put, muscle thickness should increase because the distance between the origin and insertion decreases when the femoral head is displaced in the ventral direction by load. However, because muscle thickness decreased, we presume that muscle contraction stretched the distal part of the AGMI that is the measurement point and decreased the muscle thickness. The rate of change of muscle thickness of the AGMI is bigger than that of the AGME or that of TFL. This indicates that the AGMI is more involved in the control of the ventral translation of the femoral head than other muscles. The AGMI has been shown to be attached to the hip joint capsule and contribute to the stabilization of the hip joint by pulling the hip joint capsule3, 15, 20). In particular, the AGMI is supposed to be involved in controlling the position of the femoral head in the acetabulum, because it becomes more active at the time of hip joint extension and late in the standing phase despite the absence of the moment arm in the hip joint extension direction3). In this study, we also considered that the AGMI resists ventral translation of the femoral head by pulling the hip joint capsule. The AGME also reduces the anterior displacement of the femoral head and stabilizes the hip joint14). However, the AGME is located closer to the surface than the AGMI. In addition, it is considered more suitable than the AGMI to stabilize the pelvis and adjust the femoral head under load3), though AGME is said to make anterior displacement smaller and stabilize the hip joint14). Therefore, there is a possibility that a large amount of muscle activity was not observed in the stabilization exercise in this study. Some problems with motor control besides the failure of the passive element cause ventral translation of the femoral head6). Results of this study suggest that persons with an excess of the femoral head’s ventral translation should practice exercise control using the AGMI activity. However, taking the position of the muscles into consideration, we can say that the hip dorsal muscle is involved in the control of the ventral translation and that not only the muscles located on the ventral side but also those located on the dorsal side are important. In particular, it is reported that the deep external rotators contribute to the stabilization of the femoral head in the acetabulum more than its movements as the external rotation muscle21,22,23) and that there is a large involvement in the stability of the hip joint because dislocation increases after surgical removal of deep external rotators24). It is reported that we can increase the ventral translation of the femoral head by lowering the muscle activity of the gluteus maximus at the time of hip extension12, 13). Based on these findings, we can say that we should take the AGMI into consideration for the muscles located on the ventral side. However, it is important to practice comprehensive training that takes muscles located at the dorsal of the hip joint into consideration for the muscle located on the ventral side. As the limitation of this study, we have to point out that slight movement of the hip joint in the extension direction occurred, though the fixation of the pelvis and femur was performed to the maximum. As a result, the muscles on the ventral side of the hip joint possibly can not only control the accessory movement but also antagonize the hip joint extension movement as the hip joint flexor. Therefore, it is necessary to analyze the actual hip joint movement including bone movement. At the same time, the AGMI may have been squeezed by the superficial muscle, resulting in a decrease in muscle thickness. Therefore, our future study aims to focus on the amount of muscle activity that can be evaluated directly, as mentioned above. In addition, it is difficult to know if the probe is in vertical contact with the muscle, which is another limitation of this study. In this study, measurements were taken in the supine position to ensure easy application of the load from the dorsal side to the hip joint and to eliminate the influence of posture control. However, since femoral head translation causes problems in daily life while standing or walking, it is necessary to investigate the control of ventral translation of the femoral head while standing or walking.
In conclusion, we can say that exercise against the load in the ventral direction of the femoral head resulted in a greater change in muscle thickness of the AGMI as compared with changes in the IL, AGME, and TFL. Therefore, it will be necessary to develop an exercise that places an emphasis also on the AGMI alike because AGMI is supposed to contribute to stabilizing the hip join in the ventral direction of the femoral head.
Conflict of interest
No potential conflicts of interest are disclosed.
Funding
This work was supported by JSPS KAKENHI Grant Number JP19K24181.
REFERENCES
- 1.Lewis CL, Laudicina NM, Khuu A, et al. : The human pelvis: variation in structure and function during gait. Anat Rec (Hoboken), 2017, 300: 633–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brockmeier SF. (ed): MRI-arthroscopy correlations. New York: Springer Science+Business Media, 2015, pp 411–424. [Google Scholar]
- 3.Retchford TH, Crossley KM, Grimaldi A, et al. : Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact, 2013, 13: 1–12. [PubMed] [Google Scholar]
- 4.Harding L, Barbe M, Shepard K, et al. : Posterior-anterior glide of the femoral head in the acetabulum: a cadaver study. J Orthop Sports Phys Ther, 2003, 33: 118–125. [DOI] [PubMed] [Google Scholar]
- 5.Loubert PV, Zipple JT, Klobucher MJ, et al. : In vivo ultrasound measurement of posterior femoral glide during hip joint mobilization in healthy college students. J Orthop Sports Phys Ther, 2013, 43: 534–541. [DOI] [PubMed] [Google Scholar]
- 6.Grant C, Pajaczkowski J: Conservative management of femoral anterior glide syndrome: a case series. J Can Chiropr Assoc, 2018, 62: 182–192. [PMC free article] [PubMed] [Google Scholar]
- 7.Dangin A, Tardy N, Wettstein M, et al. : Microinstability of the hip: a review. Orthop Traumatol Surg Res, 2016, 102: S301–S309. [DOI] [PubMed] [Google Scholar]
- 8.Smith MV, Panchal HB, Ruberte Thiele RA, et al. : Effect of acetabular labrum tears on hip stability and labral strain in a joint compression model. Am J Sports Med, 2011, 39: 103S–110S. [DOI] [PubMed] [Google Scholar]
- 9.Myers CA, Register BC, Lertwanich P, et al. : Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med, 2011, 39: 85S–91S. [DOI] [PubMed] [Google Scholar]
- 10.Bakshi NK, Bayer JL, Bigelow EM, et al. : The effect of capsulectomy on hip joint biomechanics. Orthop J Sports Med, 2017, 5: 2325967117733433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panjabi M, Abumi K, Duranceau J, et al. : Spinal stability and intersegmental muscle forces. A biomechanical model. Spine, 1989, 14: 194–200. [DOI] [PubMed] [Google Scholar]
- 12.Lewis CL, Sahrmann SA, Moran DW: Anterior hip joint force increases with hip extension, decreased gluteal force, or decreased iliopsoas force. J Biomech, 2007, 40: 3725–3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis CL, Sahrmann SA, Moran DW: Effect of position and alteration in synergist muscle force contribution on hip forces when performing hip strengthening exercises. Clin Biomech (Bristol, Avon), 2009, 24: 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Semciw AI, Pizzari T, Green RA: Intramuscular EMG placement for two segments of gluteus minimus and three segments of gluteus medius with unique orientation and function. J Sci Med Sport, 2011, 14: 92–93. [Google Scholar]
- 15.Walters J, Solomons M, Davies J: Gluteus minimus: observations on its insertion. J Anat, 2001, 198: 239–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gottschalk F, Kourosh S, Leveau B: The functional anatomy of tensor fasciae latae and gluteus medius and minimus. J Anat, 1989, 166: 179–189. [PMC free article] [PubMed] [Google Scholar]
- 17.Pappas GP, Asakawa DS, Delp SL, et al. : Nonuniform shortening in the biceps brachii during elbow flexion. J Appl Physiol 1985, 2002, 92: 2381–2389. [DOI] [PubMed] [Google Scholar]
- 18.Kinugasa R, Hodgson JA, Edgerton VR, et al. : Asymmetric deformation of contracting human gastrocnemius muscle. J Appl Physiol 1985, 2012, 112: 463–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whittaker JL, Stokes M: Ultrasound imaging and muscle function. J Orthop Sports Phys Ther, 2011, 41: 572–580. [DOI] [PubMed] [Google Scholar]
- 20.Beck M, Sledge JB, Gautier E, et al. : The anatomy and function of the gluteus minimus muscle. J Bone Joint Surg Br, 2000, 82: 358–363. [DOI] [PubMed] [Google Scholar]
- 21.Torry MR, Schenker ML, Martin HD, et al. : Neuromuscular hip biomechanics and pathology in the athlete. Clin Sports Med, 2006, 25: 179–197, vii. [DOI] [PubMed] [Google Scholar]
- 22.Neumann DA: Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther, 2010, 40: 82–94. [DOI] [PubMed] [Google Scholar]
- 23.Ward SR, Winters TM, Blemker SS: The architectural design of the gluteal muscle group: implications for movement and rehabilitation. J Orthop Sports Phys Ther, 2010, 40: 95–102. [DOI] [PubMed] [Google Scholar]
- 24.Khan RJ, Yao F, Li M, et al. : Capsular-enhanced repair of the short external rotators after total hip arthroplasty. J Arthroplasty, 2007, 22: 840–843. [DOI] [PubMed] [Google Scholar]


