1. Introduction
Good oral health and control of oral disease protects a woman's health & quality of life before and during pregnancy and has the potential to reduce the transmission of pathogenic bacteria from mothers to their children. Prenatal and oral health providers are limited in providing oral health care during pregnancy by their lack of understanding about its impact and safety.
In the normal progression of pregnancy there is increase of oestrogen by 10 fold and progesterone by 30 fold.1 Neglected oral hygiene with fluctuation of hormones in pregnancy tends to increase the incidence of oral diseases like gingivitis.2 High levels of circulating progesterone leads to pregnancy gingivitis. This is characterized by redness, edema& higher tendency towards bleeding. Many researchers also suggest association of periodontitis & adverse pregnancy outcomes like low birth weight and premature birth.3 So, oral health now being considered to be important part of routine antenatal examination in some developed countries & now it is becoming important part of examination in developing countries.
Oral changes seen in different trimesters of pregnancy includes various symptoms like gingivitis, gingival hyperplasia, pyogenic granuloma with salivary changes. There is an increase levels of circulating oestrogen causing gingivitis & gingival hyperplasia in pregnant females.4 As pregnancy is not the primary cause for periodontal disease, but this increase the existing condition prevailing in the individual5, 6, 7, 8 Recent upsurge in interest in periodontal diseases in pregnancy is attributed to their association with adverse pregnancy outcome.6, 7, 8 There is also a positive association between periodontal disease & risk of preeclampsia.9,10 Even there are studies which are suggesting that when periodontitis is being treated it prevents preterm birth & low birth weight.11
It also a common saying that mother “loses a tooth for every baby” but there is no medical literature supporting this statement. The possibility can be than pregnancy gingivitis may irritate the gum and can cause routine dental care uncomfortable which may lead to tooth decay & final tooth loss.12
Recent studies have shown a positive correlation between periodontal diseases and low birth weight but definite explanation has not yet found13
As we know “mouth is the mirror of body” so awareness of oral health is must for an individual. The presence of different physiological states such as puberty, pregnancy, and menopause should be given added consideration, because these conditions are known to modify the overall health status in women. The importance of oral health in pregnant women is of paramount significance, since it not only has a direct effect on pregnant females but also on the future of the child.
2. Materials and methods
2.1. Ethical clearance and informed consent
This study was conducted after obtaining ethical clearance from Ethical Committee and Institutional Review Board of college. Informed written consent was obtained from all participants in this study.
2.2. Sample selection
The study population comprised of 600 randomly selected pregnant females between 20 and 36 years of age visiting All India Institute of Medical Sciences, Rishikesh between Oct 2018 and March 2019.
The inclusion criteria for study were females with at least 20 teeth present in the mouth. Pregnant females were categorized on the basis of stage of pregnancy as first(200), second(200) and third (200)trimesters.
2.3. Questionnaire
A self-administered questionnaire from a reference article was considered. All relevant information regarding demographic details relating socioeconomic status (age, education, income and address), obstetric record (duration of pregnancy, any previous issues/miscarriages), awareness of oral hygiene(visit to dentist, importance of cleaning teeth, its effect on developing fetus), oral hygiene aids used (finger, stick, tooth brush, tooth paste, tooth powder, and tongue cleaner), frequency of tooth brushing (once, twice daily), tobacco use, awareness of cancer due to tobacco use, details of oral problems(if presents), and any other medical condition were recorded.14
2.4. Clinical assessment
Clinical examination of the oral cavity was done by experienced dentists for oral hygiene status, any ulcer or other finding. The periodontal status assessment was performed with the WHO recommended. Periodontal index (PI) and Gingival score (GI) and OHIP using standard criteria for its assessment. The score of GI, PI and OHIP was recorded for the study.
3. Observation & results
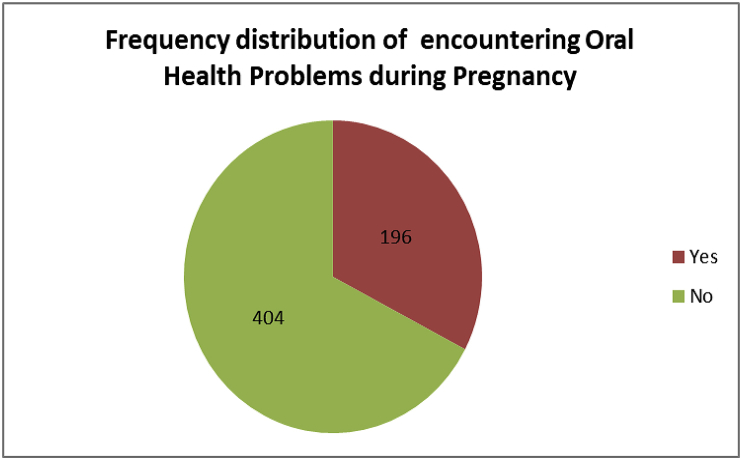
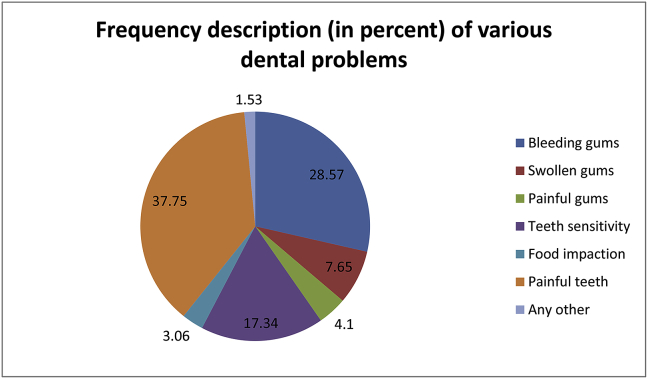
Out of 600, 196 (33%) pregnant females had some dental problem during pregnancy (Graph 1). Among them, painful teeth (37%) was the most common chief complaint followed by bleeding gums (28%), teeth sensitivity(17%) and which was followed by swollen gums(8%). (Graph 2).
Graph 1.
Frequency distribution of encountering Oral Health Problems during Pregnancy.
Graph 2.
Frequency description(in percent) of various dental problems.
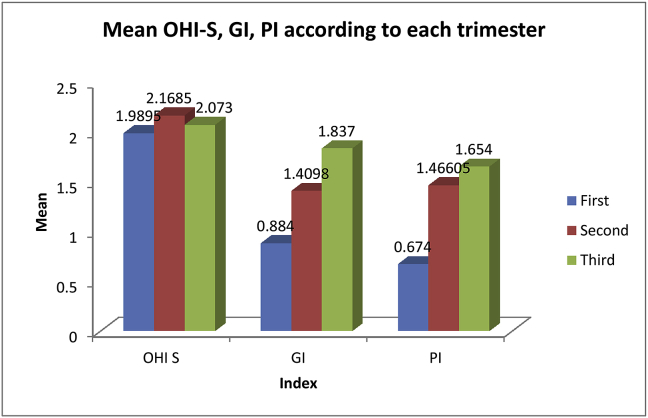
OHI score in pregnant females in Ist Trimester is 1.99, in IInd 2.17 and in IIIrd 2.07. this difference was statistically highly significant(P < 0.01). Interestingly, the trimester wise comparison showed a time-dependent increase in OHI score with duration of pregnancy. GI score in pregnant females in Ist trimester is 0.88, in IInd 1.41 and in IIIrd Trimester 1.84. this difference was statistically highly significant(P < 0.01). PI score in pregnant females in Ist Trimester is 0.67, in IInd 1.47 and 1.67 in IIrd Trimester (Graph 3).
Graph 3.
Mean OHI-S, GI, Pl according to each trimester.
Considering hygiene habits,98.5% in Ist Trimester, 94.5% in IInd Trimester and 97.5% in IIIrd Trimester were aware that cleaning is essential for teeth. Still only 69% the total subjects used to brush once daily which in turn affected the PI, GI and OHI score. Nearly 19% reported frequent mouth rinsing.
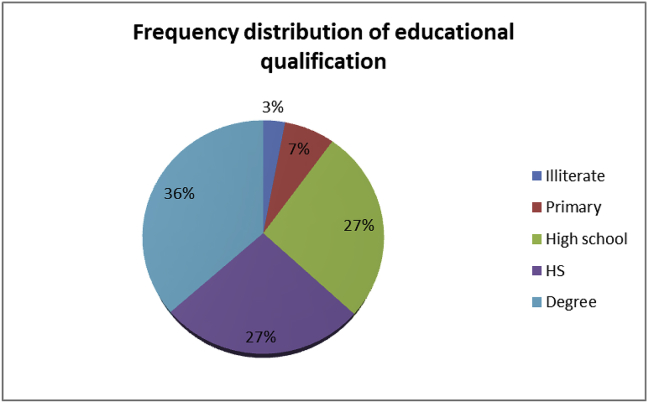
Out of 600 pregnant females 219 were graduates (36%) and (3%) were illiterate. (Table 1 & Graph 4).
Table 1.
Distribution of educational level among the patients in various trimesters.
| Educational level | First trimester |
Second trimester |
Third trimester |
|||
|---|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | Frequency | Percent | |
| Illiterate | 3 | 1.5 | 6 | 3.0 | 9 | 4.5 |
| Primary | 12 | 6.0 | 23 | 11.5 | 7 | 3.5 |
| High school | 48 | 24.0 | 62 | 31.0 | 51 | 25.5 |
| HS | 62 | 31.0 | 47 | 23.5 | 51 | 25.5 |
| Degree | 75 | 37.5 | 62 | 31.0 | 82 | 41.0 |
| Total | 200 | 100.0 | 200 | 100.0 | 200 | 100.0 |
Graph 4.
Frequency distribution of educational qualification.
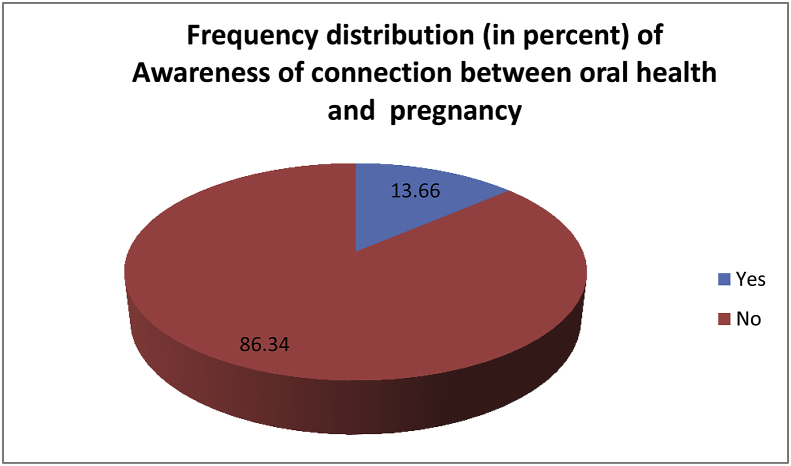
86% of the total female were not aware about the connection of the oral health during pregnancy. Table 2 & Graph 5) Nearly 14% (85/600) of pregnant females accepted that their poor tooth condition affects eating habit which in turn can negatively affect the child.
Table 2.
Frequency distribution (in percent) of Awareness of connection between oral health and pregnancy.
| Trimester | Yes |
No |
||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| First | 27 | 13.5 | 173 | 86.5 |
| Second | 34 | 17.0 | 166 | 83.0 |
| Third | 21 | 10.5 | 179 | 89.5 |
Graph 5.
Frequency distribution (in precent) of Awareness of Connection between oral health and pregnancy.
27% of pregnant females never visited to dentist, whereas 33% attended dental clinic whenever a problem occurred. 8% the pregnant female had visited the dentist for regular check-up. General health of the females stated that most females were anaemic.
4. Discussion
In this survey, 27% of pregnant females accepted that they never attended the dentist while more than half of this percentage reported some present dental problems. None of the pregnant females sought routine dental checkup during pregnancy. This number is much more greater than the previous studies in the USA, Australia and England. This raises serious concerns about dental awareness and care of pregnant females during 9-month of the period in developing countries like India. Most problems related to oral health can be simply prevented by regular dental checkups especially during pregnancy.
Our findings suggest a high prevalence of periodontal diseases among pregnant females. This condition usually starts appearing in the first trimester of pregnancy reported to be resulting from increased levels of progesterone and estrogen and causing an exaggerated gingival inflammatory reaction leading to severe periodontal diseases. The gingiva usually becomes erythematous, edematous and bleeds easily even on simple trauma.15 In the present study, the most common complaint of pregnant females was bleeding gums. In agreement with previous data in literature16, 17, 18 this study showed an increase in GI, PI and OHI score reflecting worsening of periodontal status as the pregnancy progresses. Interestingly, the trimester wise comparison showed a time-dependent increase in GI and PI score with duration of pregnancy.
Some studies have shown an association between periodontal disease and adverse pregnancy outcomes such as preterm labour and low birth weight,19 whereas other studies have shown no relation among the same.20 even as the research continues to conclude some cause-and –effect relation between oral health and pregnancy outcomes; it is prudent to keep the pregnant females free from any periodontal disease.
The study suggests a high literacy level still got low awareness regarding the effect of oral disease in growing baby.
Nearly 98.5%of total pregnant females agreed that cleaning of teeth is essential as results of earlier surveys in only 69% used to brush once a daily. This showed the poor attitude towards maintaining dental hygiene. Lack of awareness about the relation between oral hygiene and pregnancy was revealed by the fact that only 14% of the females were aware of the fact that it can adversely affect their baby.
5. Conclusion
Under the limitation of the present study, which was mainly relying on self-reported data which can be subjected to biases inherent to this method, it can be concluded that even educated females were unaware of the effects of oral diseases on unborn child. For the same purpose, there is need of interaction between dental practitioners and gynaecologists/other antenatal care providers to include routine dental checkup as a mandatory element during antenatal visits of pregnant females.
Financial support and sponsorship
Nil.
Declaration of competing interest
There are no conflicts of interest.
References
- 1.Dellinger Tracy M., Livingston H. Mark. Pregnancy: physiological changes and considerations for dental patients. Dent Clin N Am. 2006;50:677–697. doi: 10.1016/j.cden.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Soory M. Hormonal factors in periodontal disease. Dent Update. 2000;27:380–383. doi: 10.12968/denu.2000.27.8.380. [DOI] [PubMed] [Google Scholar]
- 3.Silk H., Douglass A.B., Douglass J.M., Silk L. Oral health during pregnancy. Am Fam Physician. 2008;77:1139–1144. [PubMed] [Google Scholar]
- 4.Yuan K., Wing L.Y., Lin M.T. Pathogenic roles of angiogenic factors in pyogenic granulomas in pregnancy are modulated by female sex hormones. J Periodontol. 2002;73:701–708. doi: 10.1902/jop.2002.73.7.701. [DOI] [PubMed] [Google Scholar]
- 5.Flynn T.R., Susaria S.M. Oral and maxillofacial surgery for the pregnant patient. Oral Maxillofac Surg Clin N Am. 2007;19:207–221. doi: 10.1016/j.coms.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Dasanayake A. Poor periodontal health of the pregnant woman as a risk factor for low birth weight. Ann Periodontol. 1998;3:206–212. doi: 10.1902/annals.1998.3.1.206. [DOI] [PubMed] [Google Scholar]
- 7.Lopez N.J., Smith P.C., Gutierrez J. Higher risk of preterm birth and low birth weight in women with periodontal disease. J Dent Res. 2002;81(1):58–63. doi: 10.1177/002203450208100113. [DOI] [PubMed] [Google Scholar]
- 8.Offenbacher S., Lieff S., Boggers K.A., Murtha A.P., Madianos P.N., Champagne C.M. Maternal periodontitis and prematurity. Part 1: obstetric outcomes of prematurity and growth restriction. Ann Periodontol. 2001;6(1):164–174. doi: 10.1902/annals.2001.6.1.164. [DOI] [PubMed] [Google Scholar]
- 9.Herrera J.A. Periodontal disease severity is related to high levels of C-reactive protein in pre-eclampsia. J Hypert. 2007;25:1459–1464. doi: 10.1097/HJH.0b013e3281139ea9. [DOI] [PubMed] [Google Scholar]
- 10.Barak S. Evidence of periopathogenic microorganisms in placentas of women with preeclampsia. J Periodontol. 2007;78:670–676. doi: 10.1902/jop.2007.060362. [DOI] [PubMed] [Google Scholar]
- 11.Jeffcoat M.K., Hauth J.C., Geurs N.C. Periodontal disease and preterm birth: results of a pilot intervention study. J Periodontol. 2003;74(8):1214–1218. doi: 10.1902/jop.2003.74.8.1214. [DOI] [PubMed] [Google Scholar]
- 12.Muherjee P.M., Almas K. Orthodontic considerations for gingival health during health pregnancy: a review. Int J Dent Hyg. 2010;8:3–9. doi: 10.1111/j.1601-5037.2009.00383.x. [DOI] [PubMed] [Google Scholar]
- 13.Sacco G., Carmagnola D., Abati S., Luglio P.F. Periodontal disease and preterm birth relationship. Minerva Stomatol. 2008;57:233–246. 246-50. [PubMed] [Google Scholar]
- 14.Saxena Payal, Gupta Saurabh Kumar, Yadav Sumitra. Oral health of pregnant females in central India: knowledge, awareness, and present status. J Educ Health Promot. 2017;6:102–109. doi: 10.4103/jehp.jehp_146_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vogt M., Sallum A.W., Cecatti J.G., Morais S.S. Factors associated with the prevalence of periodontal disease in low-risk pregnant women. Reprod Health. 2012;9:3. doi: 10.1186/1742-4755-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giglio J.A., Lanni S.M., Laskin D.M., Giglio N.W. Oral health care for the pregnant patient. J Can Dent Assoc. 2009;75:43–48. [PubMed] [Google Scholar]
- 17.Carrillo-de-Alboronz A., Figuero E., Herrera D., Bascones-Martinez A. Gingival changes during pregnancy. II. Influence of hormonal variations on the subgingival biofilm. J Clin Periodontol. 2010;37:230–240. doi: 10.1111/j.1600-051X.2009.01514.x. [DOI] [PubMed] [Google Scholar]
- 18.Tilakaratne A., Soory M., Ranasinghe A.W. Periodontal disease status during pregnancy and 3 months post-partum, in a rural population of Sr-Lankan wome. J Clin Periodontol. 2000;27:787–792. doi: 10.1034/j.1600-051x.2000.027010787.x. [DOI] [PubMed] [Google Scholar]
- 19.Xiong X., Buekens P., Fraser W.D., Beck J., Offenbacher S. Periodontal disease and adverse pregnancy outcomes. A Syst Rev Bjog. 2006;113:135–143. doi: 10.1111/j.1471-0528.2005.00827.x. [DOI] [PubMed] [Google Scholar]
- 20.Michalowicz B.S., Hodges J.S., DiAngelis A.J. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355:1885–1894. doi: 10.1056/NEJMoa062249. [DOI] [PubMed] [Google Scholar]