Abstract
Background
Tuberculosis affected 2.7 million people in India in 2017. The Revised National TB Control Programme has achieved milestones in coverage, however quality of TB care remains highly variable and often poor, with significant gaps in provider knowledge, practices, and patients consistently lost to follow-up. These quality gaps are largely informed by studies on provider practices or objective chart abstractions and case data. Per the knowledge of the author, no review has been conducted on first-hand patient perspectives on the quality of TB care they receive. This mixed-methods literature review aims to synthesize evidence on user-experience and patient satisfaction with TB care in India and inform areas for service quality improvement.
Methods
Five medical databases, including PubMed, EMBASE, Global Health (Ovid), Web of Science, and CINAHL were searched for empirical studies on patient perspectives on TB health services published between January 1st, 2000 to December 31st, 2017. Studies in English with adult patients with any form of TB in the public or private health system were included. Studies prior to entering the health system, on distance to health facilities and cost were excluded. Seven Indian journals were hand searched and a grey literature search was conducted in GoogleScholar. Studies were assessed for methodological quality and thematic analysis was conducted by categorizing data using NVivo 12.
Results
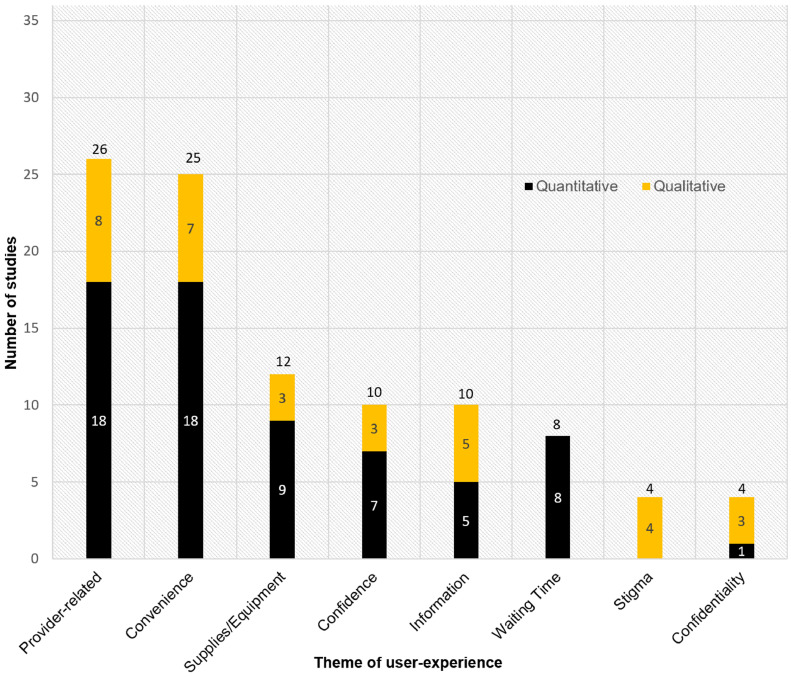
A total of 498 studies were screened, of which 23 met the inclusion criteria. 16 supplementary studies were identified from Indian journals and grey literature. Of the 39 total studies included most were quantitative (29; 74%), based in South India (17; 44%) and focused on drug-sensitive TB patients (19; 49%) within the public health system (25; 64%). Data collection methods were highly heterogenous which limited synthesis and comparisons across population demographics, health sectors, or regions. Overall quantitative patient satisfaction measured in seven studies was high. Two major themes identified were provider-related factors (n = 26 studies) and convenience (n = 25), and six minor themes were supplies and equipment availability (n = 12), confidence (n = 10), information and communication (n = 10), waiting time (n = 8), stigma (n = 4), and confidentiality (n = 4). Each reported positive and negative user-experiences. Most significantly, DOTS did not fit the daily needs and obligations of many patients, particularly due to conflicts with employment and frequency of visits; while positive provider support, information, and flexibility helped patients adhere to treatment.
Conclusion
Although quantitative patient satisfaction was found to be high, data were not collected using robust, validated tools. Qualitative and quantitative user-experiences in each theme were variable, making them both barriers and facilitators of good quality TB care. Poor user-experiences were often responsible for patients interrupting treatment or dropping out of TB care. Patient-centeredness, or user-friendliness of TB care can be improved by introducing individualized or flexible DOTS that is responsive to user circumstances and needs. User-experience data should be systematically collected using a standardized, national tool for identification of specific bottlenecks and successes in quality of TB care from the patients’ perspective.
Keywords: Tuberculosis, India, Quality of care, Patient satisfaction, User experience, Patient perspective
1. Introduction
India accounts for the highest burden of tuberculosis (TB) in the world, with 26% of all TB cases [1]. In 2017, there were an estimated 2.7 million new cases of TB and 420,000 related deaths. The Government of India has committed to the elimination of TB through rapid declines in disease burden, mortality, and morbidity by 2025 [2]. To achieve this, the Revised National TB Control Programme (RNTCP) has reached country-wide coverage of the TB programme and the Directly Observed Therapy, Short course (DOTS) strategy, providing free medications and diagnostic services at public health facilities. This strategy has treated more than 10 million people between its full launch in 1997 and 2017 [2]. While there has been significant progress in coverage and scale up of basic TB services, gaps in the quality of care still remain.
Quality of TB care has frequently been found to be substandard and highly variable across India's public and private health systems [3], [4], [5], [6]. Patients consult up to three providers and face delays of up to two months prior to receiving a proper diagnosis [7]. Simulated, standardized patient studies have shown that only 21% of private practitioners managed cases of TB correctly (when benchmarked loosely against the Standards of TB Care India) [8]. This has huge implications, as over 70% of general patients first seek care in the private sector [9] and 46% of all TB patients are managed there [10]. Within the public sector, a cascade of care analysis estimated that nearly one-fifth of prevalent TB patients (520,000 annually) interface with public TB services yet are either not successfully diagnosed or are lost to follow-up (LTFU) before starting treatment [11]. As such, whether it be the public sector [3,12] or private [6,[13], [14], [15], [16], [17], TB patients must navigate between and within health systems that possess several gaps in quality. Exploration of the user's experiences may be a key step to finding out why TB care may be “missing millions” that go undiagnosed, untreated, or unreported, despite patients engaging with the health system [12,18]. A previous systematic review of 47 studies on quality of TB care in India included studies that primarily evaluated chart abstractions and quantitative provider knowledge, attitudes, and practices [4]. No review has been conducted on the service user, i.e. the patient's perspective of the quality of TB care they receive.
Quality of care is fundamental to ensuring a patient's right to health and achieving optimal health outcomes, i.e. cure for TB patients [19]. According to the Lancet Global Health Commission on High-Quality Health Systems, health systems are underpinned by four values: for people, equitable, resilient, and efficient [19]. Due to the unique perspective of patients as first-hand service users, patient- or user-experience informs each value as a key component of the processes of care. Patient satisfaction is another measure that can be valuable for health service improvement when assessed using specific, well-designed, psychometrically-tested tools [20], [21], [22]. Hence, patient satisfaction (i.e. whether a patient's expectations of care are met [23]) and user-experience (i.e. what events and experiences occured within the health system) are some of the most important indicators of quality of care [20,[24], [25], [26], [27], [28]. Non-health industries recognize that positive customer satisfaction and reviews lead to economic benefits like company growth, recommendations, and customer loyalty [29]. Likewise, higher patient satisfaction and positive user-experiences have been positively associated with greater utilization of services, patient retention, adherence to treatment regimens, confidence in health systems, better quality of life, and improvements in objective health outcomes such as mortality and medical errors [30], [31], [32], [33], [34], [35].
Patient-centered care is where patients’ needs, preferences, and empowerment are central to healthcare delivery [36,37]; user-experience is considered especially important when determining the patient-centeredness of care delivery and identifying areas for improvement [23]. Patients’ evaluation of care has been applied for strategic decision-making, informing effective organization of care, and transforming provider practices and health systems, particularly in high-income settings using established tools such as the Consumer Assessment of Healthcare Providers and Systems (CAHPS) suite of surveys [38], [39], [40]. Patients are shifting from being passive receivers of care to active collaborative partners in health service delivery [24,27,30,[41], [42], [43], [44], [45]. Hence, as India's National Strategic Plan (2017 – 2025) prioritizes the provision of patient-centered care, this mixed-methods literature review seeks to provide a comprehensive overview of available evidence on the user-experiences and patient satisfaction with quality of care, amongst adult TB patients in India. The objective is to describe TB patient experiences (user-experience) within the Indian healthcare system. Results from this review may help identify gaps along the patient cascade of care from the patient's perspective, and areas for service quality improvement for the provision of patient-centered, high-quality TB care.
2. Methods
2.1. Search strategy and screening
A systematic search for studies from January 1st 2000 to December 31st 2017 was performed in 5 databases, including PubMed, EMBASE, Global Health (Ovid), Web of Science, and CINAHL. The search terms and search strategy were approved by a medical librarian and composed of variations of the following key terms: 1) tuberculosis, 2) patient satisfaction or experience or perspective, and 3) health care service delivery. This search was conducted for a larger systematic review of patient perspectives across all low- and middle-income countries [46]. For this focused review, studies specific to India were identified by searching “India” within the retrieved references in EndNote X7. Titles and abstracts were screened by two independent reviewers using the predetermined inclusion criteria below. Disagreements were resolved through discussion. Full-text articles were retrieved via EndNote or contacting authors, and screened by one reviewer. A brief grey literature search in Google Scholar was also conducted. In addition, to increase the yield of relevant articles, an electronic search of seven Indian journals related to TB and public or community health were hand searched for studies from January 1st 2000 to October 1st 2018 (see supplementary materials for the search strategy and journal list).
2.2. Inclusion and exclusion criteria
Studies were included if they were in English language and located in any region of India. The population was adult patients (older than 15 years of age) with presumptive TB or diagnosed with any form of TB (including comorbidities such as HIV-TB). There was no restriction on study design, the service being evaluated (e.g. screening, diagnosis, treatment, case management, counselling, other), or type of health system (public, private). The public sector was defined as any service provided by the government and/or under the RNTCP. The private sector was defined as any service outside of government-provided services including by private providers (PPs), non-profit organizations and informal providers (e.g. faith healers, pharmacy staff). PPs include practitioners of various systems of medicine, including modern allopathic medicine and Indian traditional medicine (i.e. ayurveda, yoga, unani, sidda, homeopathy (AYUSH)), and encompass facilities that range from small clinics to hundred-bed hospitals. Studies were excluded if they did not describe standard care (e.g. interventions, prison health systems), were not from the patient's perspective (e.g. family or provider perspective), and if they focused on patient experience outside of the quality of health system for TB (e.g. stigma in the community, knowledge of TB, HIV care). Data on the financial burden of TB care and distance to health facilities were excluded having been previously well-documented across several reviews [47], [48], [49], [50].
2.3. Data extraction and quality assessment
The following data was extracted from each study; study details (i.e. authors, publication year, setting, population, etc.), data collection methodology, and any relevant findings (see supplementary materials for data extraction form). The data were recorded and tracked using Microsoft Excel. Included studies were assessed for quality to describe the range of their methodological quality. Quantitative studies were assessed using the Critical Appraisal tool for Cross-Sectional Studies (AXIS) tool [51]. Qualitative studies were assessed using the CASP Qualitative Checklist [52]. For mixed-methods studies, the quantitative and qualitative components were assessed separately using their respective tools.
2.4. Data analysis
Thematic analysis was conducted for both quantitative and qualitative studies [53]. The results sections of each study were read line-by-line and relevant findings were categorized into themes and sub-themes, using NVivo 12 Pro software (QSR International Pvt. LTD, Melbourne, Australia). For qualitative studies, both author summaries of findings and patient quotes were coded. For quantitative studies, the variable labels from surveys were extracted as ‘themes’ in the same way conceptual themes are extracted from qualitative reports [54]. Guided by principles of segregated mixed-method synthesis by Sandelowski et al., themes were developed separately for quantitative and qualitative studies, then combined and presented complementarily [55]. Themes were developed in an inductive manner, with no predefined framework to guide the analysis. When synthesizing data, overlapping themes from the quantitative and qualitative analyses were combined and refined. Themes that did not overlap were maintained as their own conceptual themes. All evidence informing a theme were tabulated, including qualitative quotes and quantitative descriptive statistics. Studies that reported overall patient satisfaction percentages were tabulated separately. Major themes (greater than 50% of included studies containing the theme) and minor themes (less than 50%) were identified post hoc.
3. Results
3.1. Composition of included studies
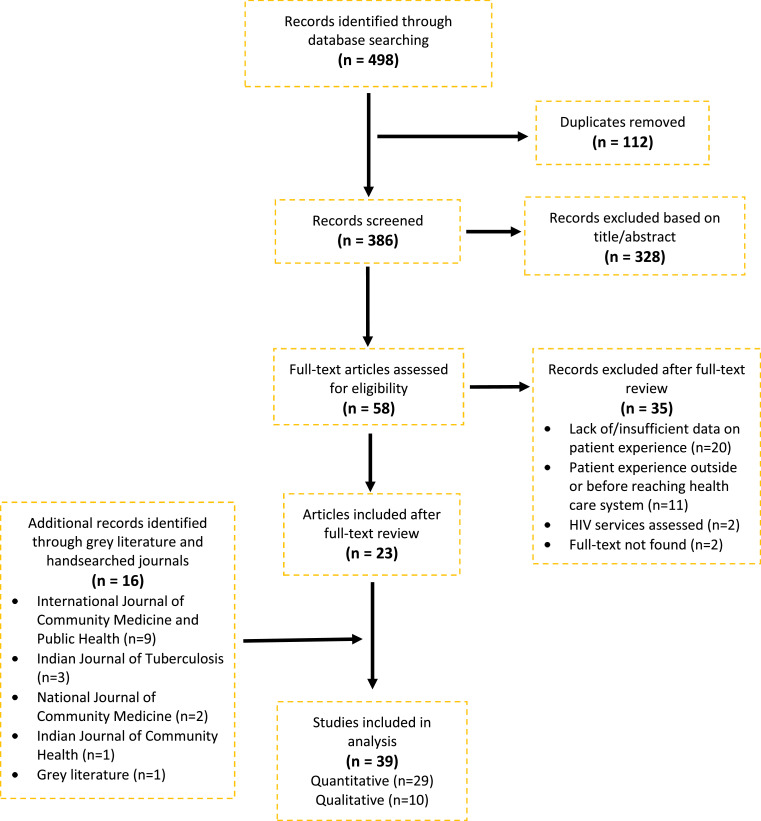
The search yielded 498 titles and abstracts for screening, of which 112 were duplicates and 23 met the inclusion criteria. Additionally, 16 studies were found from hand-searching journals and grey literature (Fig. 1). Of all 39 studies reviewed, 29 (74%) were quantitative and 10 (26%) were qualitative. Quantitative studies mainly used a questionnaire with a semi-structured or structured interview to collect data (27/29; 93%) and qualitative studies used in-depth interviews (7/10; 70%) and focus group discussions (3/10; 30%). As shown in Table 1, 25 studies (64%) assessed perceptions of services offered by the public health system/RNTCP, 1 (3%) assessed services in the private sector, and 13 (33%) assessed experiences in both. Seventeen studies (44%) were located in South India, 10 (26%) in North, 6 (15%) in West, 3 (8%) in Central and 1 (3%) in East. Two other studies (5%) were located in multiple regions of India. Most studies (19; 49%) evaluated perspectives of patients with drug-sensitive TB (DS-TB) (including pulmonary and extrapulmonary TB), 4 (10%) assessed presumptive TB patients, and 12 (31%) did not specify. Four (10%) studies assessed perspectives of MDR-TB or MDR-TB/HIV co-infected patients, all of which were qualitative.
Fig. 1.
PRISMA flow diagram for review on TB patient experience in India [56].
Table 1.
Characteristics of included studies (n = 39).
| Study | City, State or UT (Region) | Study design | Study setting | Type(s) of health service evaluated | Sample size | Study population |
|---|---|---|---|---|---|---|
| QUANTITATIVE (n = =29) | ||||||
| 1. Charles et al., 2010 | Chennai & Madurai, Tamil Nadu (South) | Cross-sectional | Community | Public, Private | 640 | Chest symptomatics |
| 2. Dandona et al., 2004 | Andhra Pradesh & Tamil Nadu (South), Maharashtra (West), Rajasthan (North) | NR | Government facilities | Public | 314 | PTB, EPTB patients |
| 3. Dhingra et al., 2004 | Delhi (North) | NR | New Delhi TB Centre | Public | 36 | PTB patients with pleural effusion |
| 4. Divija et al., 2015 | Tamil Nadu (South) | Cross-sectional | DOTS or DMC centres in 4 medical colleges | Public | 20 | NSP TB patients |
| 5. Goel et al., 2011 | Karnataka (South) | Cross-sectional | DOTS centres | Public | 98 | NSP TB patients receiving DOTS |
| 6. Grover et al., 2003 | Punjab (North) | Cross-sectional | Community | Public, Private | 192 | Chronic chest symptomatics |
| 7. Gupta et al., 2010 | Delhi (North) | Retrospective cohort | Tertiary-level TB institute | Public, Private | 366 | PTB, EPTB patients |
| 8. Gupta, 2015 | Uttar Pradesh (North) | Cross-sectional | DOTS centres | Public | 400 | Patients attending DOTS |
| 9. Haque et al., 2014 | Uttar Pradesh (North) | Longitudinal | DMCs | Public | 117 | Patients registered for DOTS |
| 10. Jaggarajama et al., 2009a | Chennai, Tamil Nadu (South) | Cross-sectional | Government facilities | Private | 104 | Patients who shifted from private to public health facility |
| 11. Jebamalar et al., 2018 | Chennai, Tamil Nadu (South) | Cross-sectional | Government facilities | Public, Private | 197 | Newly diagnosed PTB patients registered for intensive phase of Category 1 ATT) |
| 12. Mallick et al., 2017 | West Bengal (East) | Unmatched case control | Community (registered under RNTCP) | Public | 202 | NSP TB patients registered for DOTS [99 cases (treatment non-completion) + 103 controls (completion)] |
| 13. Mehra et al., 2013 | Uttarakhand (North) | Prospective descriptive | Referral hospital | Public | 98 | SP PTB patients that defaulted after referal to district TB centre for DOTS |
| 14. Mistry et al., 2016 | Maharashtra (West) | Retrospective survey | Slums | Public, Private | 76 | PTB patients who had completed treatment including TB-diabetes (n = 6) and TB-HIV (n = 4) |
| 15. Patel et al., 2013 | Ahmedabad, Gujarat (West) | Cross-sectional | DOTS centre | Public | 160 | PTB patients with treatment delay |
| 16. Paul et al., 2012 | West Bengal (East) and Andhra Pradesh (South) | Retrospective cohort | Government facilities | Public | 150 | PTB patients with treatment delay |
| 17. Pranavi et al., 2017 | Puducherry (South) | Cross-sectional | DMC | Public | 200 | Presumptive TB patients referred to DMC |
| 18. Rai et al., 2015 | Madhya Pradesh (Central) | Observational | DMC cum DOTS centres | Public | 67 | Non-adhering PTB, EPTB patients |
| 19. Rai et al., 2017 | Madhya Pradesh (Central) | Cross-sectional | DMC cum DOTS Centres | Public | 337 | Patients registered for DOTS |
| 20. Rashmi & Vijaykumar, 2010 | Karnataka (South) | Cross-sectional | Government PHC | Public | 30 | TB patients attending PHC |
| 21. Sawase et al., 2016 | Maharashtra (West) | Cross-sectional | DOTS centre in Malvani slum | Public | 65 | Smear positive, smear negative, & EPTB patients taking DOTS |
| 22. Selvam et al., 2007 | Tamil Nadu (South) | Cross-sectional | Government facilities | Public | 601 | NSP PTB patients, diagnosed and treated at government facilities |
| 23. Srinath 2018 | Karnataka (South) | Cross-sectional | TB Unit | Public | 160 | PTB patients that visit TB unit |
| 24. Srivastav and Mahajan, 2014 | Uttar Pradesh (North) | Cross-sectional | DMCs | Public | 220 | Diagnosed TB cases enrolled in DOTS |
| 25. Srivastava et al., 2017 | Uttar Pradesh (North) | Observational | DMCs | Public | 300 | PTB, EPTB patients registered at DMC |
| 26. Sudha et al., 2003 | Tamil Nadu (South) | Cross-sectional | Community | Public, Private | 98 | Chest symptomatics |
| 27. Sukumaran et al., 2002 | Kerala (South) | Longitudinal | District TB centres | Public | 100 | PTB patients registered for DOTS |
| 28. Tiwari & Wavare, 2015 | Madhya Pradesh (Central) | Cross-sectional | DOTS centre | Public | 150 | PTB, EPTB patients referred to DOTS centres |
| 29. Yamini et al., 2017 | Andhra Pradesh (South) | Cross-sectional | Tertiary care hospital | Public, Private | 100 | SPTB patients in hospital TB ward |
| QUALITATIVE (n = =10) | ||||||
| 30. Benbaba et al., 2015 b,c | Mumbai, Maharashtra (West) | NR | MSF Clinic | Public, Private | 12 | DR-TB patients |
| 31. Furin et al., 2014b | Mumbai, Maharashtra (West) | NR | MSF Clinic | Public, Private | 12 | HIV-MDR-TB coinfected patients |
| 32. Isaakidis et al., 2013b | Mumbai, Maharashtra (West) | NR | MSF Clinic | Public, Private | 12 | HIV-MDR-TB coinfected patients |
| 33. Jaiswal et al., 2003 | Delhi (North) | NR | Chest clinics and DOTS centres | Public | 40 | PTB, EPTB patients who stoped treatment |
| 34. Rakesh et al., 2016 | Kerala (South) | NR | Community | Public | 29 | TB patients that just completed treatment (or in last month) |
| 35. Singh et al., 2002 | Delhi (North) | NR | Chest clinics | Public | 59 | Patients who refused |
| or were denied DOTS | ||||||
| 36. Tripathi et al., 2015c | Uttar Pradesh (North) | Grounded theory | DR-TB Centres | Public | 12 | MDR-TB patients |
| 37. Yellapa et al., 2017 | Karnataka (South) | NR | Community | Public, Private | 4 | TB (n = 3) & TB-diabetes (n = 1) patients |
| 38. Yellappa et al., 2016d | Karnataka (South) | NR | Government facilities | Public, Private | 33 | PTB, EPTB patients |
| 39. Yellappa et al., 2017d | Karnataka (South) | NR | Government facilities | Public, Private | 33 | PTB, EPTB patients |
ATT = Anti-tubercular treatment, RNTCP = Revised National TB Control Program; DMC = Designated Microscopy Centre; DOTS = Directly Observed Therapy, Short course; PHC = Primary Health Centre; MSF = Médecines Sans Frontières; SP = smear-positive; NSP = new smear-positive; PTB = pulmonary TB; EPTB = extrapulmonary TB; MDR-TB = multi-drug resistant TB; WHO = World Health Organization. a = the study reported data from 1997 (pre-RNTCP) and 2005 (post-RNTCP) separately, only 2005 data were included in this review. b = data from these three studies originate from the same larger pool of data. c = these studies are mixed-method, however only their qualitative component was relevant and assessed for this review. d = data from these two studies originate from the same larger pool of data.
3.2. Quality assessment
The quality assessment found that 8 of 29 quantitative studies (28%) did not use a questionnaire that was pilot tested, 18 (62%) used a pretested questionnaire but did not describe the methodology of testing, and only 3 (10%) utilized and fully described pre-tested tools. None used previously published, validated and reliable tools. Information on non-responders was only included in 4 (14%) studies, which raises concerns over non-response bias. Five studies (17%) did not include information on ethics reviews or patient consent. Several studies did not adequately describe the methods (16; 55%), results (9; 31%), and discussions (18; 62%), with insufficient information to allow replication or lack of consideration of limitations. Qualitative studies fulfilled most criteria, however, none of the studies considered the relationship between the researcher and participants. Results of the full quality criteria and assessment can be viewed in the supplementary materials.
3.3. Themes of user-experience
Thirty-six (92%) studies in the review informed on themes of user-experience (the other three reported solely on overall patient satisfaction). Provider-related factors and convenience were major themes with more than 50% of studies including information on them, and supplies and equipment availability, confidence, information and communication, waiting time, stigma (enabled by the health system), and confidentiality were minor themes. Fig. 2 illustrates the number of studies that contained each theme. Major findings from each theme are summarized in Table 2. Evidence for each theme, including specific quantitative data and qualitative findings from each primary study are tabulated and available in the supplementary materials.
Fig. 2.
User-experience themes identified for TB quality of care in India.
Table 2.
Main findings on user-experience themes for quality of TB care.
| Theme | Key findings |
|---|---|
|
Provider-related factors (n = 26) Availability (n = 8) Technical capacity (n = 14) Respect (n = 16) |
|
|
Convenience (n = 25) Ease of use (n = 24) Continuity of care (n = 6) |
|
| Supplies and Equipment Availability (n = 12) |
|
| Confidence (n = 10) |
|
| Information and Communication (n = 10) |
|
| Waiting time (n = 8) |
|
| Stigma enabled by health system (n = 4) |
|
| Confidentiality (n = 4) |
|
RNTCP = Revised National TB Control Program; DMC = Designated Microscopy Centre; DOTS = Directly Observed Therapy, Short course; MDR-TB = Multi-Drug Resistant TB; MP = Madhya Pradesh; UP = Uttar Pradesh.
When the influence of factors including type of TB, geographic region, or type of health system were explored, no discernible patterns were observed. Most studies did not consistently define, report, or differentiate between variables; for example, although some studies did include EPTB, TB-Diabetes, and TB-HIV patients, their experiences were not disaggregated. This was consistent with studies evaluating both public and private sector care. Thus, it was determined appropriate to synthesize findings across all studies. Any differences with regards to these factors that may have emerged are noted in the below text.
3.3.1. Provider-related factors (26/36 studies; 72%)
Poor experiences with providers’ availability, technical capacity, or attitude often influenced patients to switch providers or not adhere to treatment [62,63,[72], [73], [74], [75], [76].
Availability: The consistent, reliable availability of health workers affected the user-experience of patients in 8 studies [58,59,68,72,73,[77], [78], [79]. In 2 quantitative studies in Uttar Pradesh (UP), a majority of patients agreed that a DOTS provider was regularly available [58,59]. In other regions, the irregular availability or absense of DOTS providers led to significantly more patients stopping treatment [COR: 11.9, 95% CI: 4.8, 29.8] [73], to patients facing barriers completing diagnosis or treatment [68,72], feeling dissatisfied [58,77], and missing injections and pills for DOTS [79].
Technical capacity: In 14 studies, the competence, efficiency and technical ability of health workers to provide TB services, including diagnosis, treatment, and counselling also impacted user-experiences [59,[61], [62], [63],66,71,74,75,[79], [80], [81], [82], [83], [84]. Several patients, predominantly in Mumbai and Karnataka, reported experiencing health system delays and frustration due long, redundant pathways to diagnosis [75,82], the doctor advising inappropriate, unneccesary diagnostic tests [75,80,81], suggesting and treating for incorrect diagnoses [74,75,81], and lengthy symptomatic treatments prior to a diagnosis [75,81]. Once diagnosed, patients also experienced provider-related barriers to initiating treatment [66]. In 3 studies in Delhi, several patients were refused enrollment in treatment as they were deemed unsuitable for the commitment required for DOTS [62,63,83]. For MDR-TB/HIV patients in Mumbai, DOTS providers did not supervise the drug intake, leaving patients to self-administer while sitting at the clinic [79]. Patients in Delhi and Karnataka expected health workers to provide psychological and medical support when facing side-effects but were disappointed to not receive appropriate counselling [62,84].
“If a patient gets vomiting sensation after taking tablets, TB centre staff should take care of the patient. But these people just ask the patient to go away and vomit.” [65 year old male TB patient, Karnataka] [84].
Alternatively, quantitative studies in rural Karnataka and UP report patients satisfied with professional competence, skill and efficiency to treat [71] and appreciation of personal attention for side effects through DOTS [59], respectively.
Respect: The behaviour and attitude of health workers were cited in 16 studies by patients as having impacted their user-experience [57], [58], [59], [60], [61], [62],68,73,75,[77], [78], [79],[83], [84], [85], [86]. In 5 studies that specifically quantified patient perceptions of providers’ behaviour or attitude, a majority of patients reported being satisfied or viewed it favourably [57], [58], [59], [60], [61]; 4 of these studies were conducted amongst patients attending DOTS in UP, while 1 study was in Madhya Pradesh (MP). Positive experiences are supported by qualitative evidence from Karnataka, Delhi and Mumbai where patients narrated instances where providers went out of their way to support patients psychologically [85], financially [62], or by adapting to patients’ unique needs and preferences for DOTS [79,84,85]. Patients greatly appreciated this flexibility and trust, particularly from PP's [84] and in rural regions [85] in South India, including DOTS providers coming early in the morning [84,85] or allowing patients to take their medicines at home where they are more comfortable when experiencing immediate side-effects [79].
On the other hand, rude behaviour of staff was blamed by some patients in various regions for dissatisfaction with care [58,77], dropping out of care [73], and as a barrier to completing treatment [68,78]. Patient narratives from qualitative studies in Delhi and Karnataka highlighted unhelpful staff attitude and disrespectful behaviour towards patients, in particular for not sympathizing with side-effects [62,75,84]. This disrespect caused patients to switch providers or refuse further DOT treatment.
3.3.2. Convenience (25/36 studies; 69%)
Ease of use: Twenty-four studies from across regions included patients impacted by the ease of use of TB care delivery, including the frequency of visits and schedules of DOTS centres [57], [58], [59], [60], [61], [62], [63], [64], [65],68,70,73,74,[76], [77], [78], [79],[83], [84], [85], [86], [87], [88], [89]. Out of these, 22 studies included patients finding the timing and schedule of care delivery inconvenient and difficult to use. Patients consistently found the frequency of DOTS visits to be a challenge and barrier during treatment [57,[60], [61], [62],64,68,70,76,84,85]. The unsuitable timings of clinics conflicted with work and daily activities, which were reported in 15 studies as reasons for DOTS non-compliance or interruption [63,65,73,74,79,83], delays during treatment and diagnosis [64,77,86,87], and as a general problem or dissatisfaction in availing treatment [57,58,60,78,88].
“…If he [another TB patient] does not go for his treatment, he will die and if he does not go for work, his children will die” [65 year old male TB patient, Karnataka][84].
Qualitative data reveal that patients had to make adjustments to their daily routines, and in some cases endure pain and breathlessness to reach the facility every alternate day [62,84,85]. Contrastingly, 2 studies in rural settings in UP and MP, reported a majority of patients finding timings of DOTS centres convenient or not affecting work [59,61]. Few studies included certain vulnerable populations that expressed facing further inconveniences and difficulties undertaking treatment; these included poor individuals, sole wage earners, and daily wage labourers [84,85], as well as persons with physical disabilities [88], respiratory co-morbidities [62], mental health issues [74], and the weak and ill [64,65] who found it arduous and unfeasible to physically attend and commit to DOTS regularly. Outside of DOTS, the frequency of visits to various labs and facilities during diagnosis was also a cause for negative user-experience [89].
Continuity of care: Ensuring continuity of care in circumstances requiring travel and attending social or emergency events was a concern for patients in 6 studies in various regions [62], [63], [64], [65],74,85]. Patients reported DOTS non-adherence due to having to leave town [63,65,74], attend family functions such as weddings [64,74,85], and emergencies such as an illness or death in the family [62,74]. Continuity was particularly a concern for patients with roots in rural villages who would need to travel back home, and those whose work requires migration for business or a new placement [62]. Two studies in Delhi reported that a notable number of patients had returned to their home village and halted treatment due to a lack of programme mechanisms facilitating re-entry into care [62,63].
3.3.3. Supplies and equipment availability (12/36 studies; 33%)
Twelve studies informed on the impact of supplies and equipment on patient perspectives [57,[62], [63], [64], [65], [66],68,70,71,78,84,88]. Having sufficient material resources at a health centre, such as a reliable supply of affordable medicines [57,62,84] and drinking water at the DOTS centre [88] facilitated a positive user-experience. Negative user-experiences were caused by inadequate supply or shortage of drugs [63,68,78], inadequate seating provision or drinking water at DOTS centre [65], and lack of diagnostic equipments [70,71]. In 1 study in rural West Bengal, a large number of patients reported a lack of diagnostic testing at the original clinic and subsequent need for referral to a Designated Microscopy Center (DMC) [66].
3.3.4. Confidence (10/36 studies; 28%)
In 10 studies from various regions, confidence emerged as a part of user-experiences [62,63,65,[67], [68], [69],73,82,86,89]. Patients reported a lack of faith, trust, or belief in the efficacy of their treatment [63,65,67,82], and in the RNTCP or a government doctor [62,68,73]. Lack of confidence in the treatment was cited in 5 studies by patients as a reason for treatment interruption [62,63] and non-completion [65,67,73]. Alternatively, some patients in South India expressed faith in their chosen provider (public or private) [69,89], and the trusted reputation of the DMC [86].
3.3.5. Information and communication (10/36 studies; 28%)
Out of 10 studies, 7 studies from South India and 3 from North reported some patients feeling frustrated or lost due to being provided inadequate information [58,62,65,[70], [71], [72],75,78,85,89]. This included information on the disease and prevention, the tests and explanation of test results, treatment regimens, side-effects and complications. In some cases, lack of awareness of a monitoring schedule led to MDR-TB patients missing follow-up examinations [70] and migrants not being aware of a transfer facility [74]. On the other hand, health education and communication from health workers helped several patients stay informed and be equipped to manage their side-effects and alcoholism [58,71,78,85].
3.3.6. Waiting time (8/36 studies; 22%)
Eight quantitative studies informed on waiting time [58,60,61,68,71,78,88,90]. A large proportion of patients in 2 studies were satisfied with the waiting time at DOTS centres in MP and Karnataka [61,71]. In Mumbai and UP, the waiting time to receive DOTS medicines for a majority of patients was less than 10 min in 2 studies, but longer than 20 min for some [60,88]. A small number of patients perceived waiting time as a barrier during treatment [78,90], diagnosis [68], and for having a satisfactory experience with care [58].
3.3.7. Stigma enabled by health system (4/36 studies; 11%)
Qualitative studies showed how aspects of TB care can promote stigma according to some patients [62,85,89,91]. For HIV/MDR-TB co-infected patients in Mumbai, taking medicines and experiencing side-effects in front of others during DOTS was embarrassing and demeaning and reinforced the stigma of having both TB and HIV [91]. Similarly in Karnataka, patients felt stigmatized during diagnosis when having to cough violently to produce a sputum sample in front of others [89]. In Delhi, being labelled and perceived as a “defaulter” prevented several patients from being able to re-join treatment or be treated with respect from health staff [62].
3.3.8. Confidentiality (4/36 studies; 11%)
Confidentiality emerged as a concern for patients in 4 studies based in South India [84,85,89,92]. Patients were found to prefer taking DOTS from a distant place [84,85] or visiting a private provider or a non-community DOTS provider [84,85,92], even if its inconvenient, in order to protect their confidentiality and avoid social stigma. Coughing to produce a sputum sample for diagnosis also required privacy, and patients were willing to go home or switch providers to achieve this [89].
“I was offered treatment from a DOT provider nearby, but I denied due to confidentiality issues.’’ [24 year old female with lymph TB, Kerala] [85].
3.4. Patient satisfaction
Seven out of 39 included studies (18%) directly measured patient satisfaction with various aspects of TB care in India, including services provided at a DOTS centre or DMC, RNTCP treatment, DOTS medicines, and treatment with current provider (including private) (Table 3) [57,58,60,61,[93], [94], [95]. No meta-analysis was conducted due to the high level of variability in aspects of care assessed and sampling methodologies. The proportion of patients reporting as satisfied or fully satisfied ranged between 68% and 97% amongst all studies. Out of the 7 studies, 5 (71%) were in North India and 6 (86%) evaluated satisfaction within public sector care. In other studies, general dissatisfaction with services was reported by patients a reason for discontinuing care with a provider [77,90], initial provider-preference [69,92], treatment interruption [67,73], and delay in diagnosis [86,87].
Table 3.
Patient satisfaction reported for TB care in India (n = 7).
| STUDY, YEAR State (Region), Health Sector Evaluated |
SAMPLE SIZE | SATISFACTION REPORTED | SATISFACTION WITH |
|---|---|---|---|
|
Dhingra et al., 2004 Delhi (North), Public |
36 |
97% satisfied 2.8% unsatisfied |
DOTS medicines |
|
Gupta, 2015 Uttar Pradesh (North), Public |
400 |
67.8% highly satisfied 16.7% just satisfied 15.5% not satisfied |
RNTCP treatment |
|
Grover et al., 2003 Chandigarh (North), Public/Private |
192 | 70% satisfied | Treatment with current provider |
|
Rai et al., 2017 Madhya Pradesh (Central), Public |
337 |
71.5% fully satisfied 28.5% somewhat satisfied |
Services provided at DMC cum DOTS centres |
|
Srivastav and Mahajan, 2014 Uttar Pradesh (North), Public |
220 |
78.6% fully satisfied 8.2% somewhat satisfied 13.2% unsatisfied |
Services provided at DOT centers |
|
Srivastava et al., 2017 Uttar Pradesh (North), Public |
300 |
87% satisfied 13% not satisfied |
Services of the DMC |
|
Sukumaran et al., 2002 Kerala (South), Public |
100 |
91% satisfied 6% unhappy 3% stopped treatment after 2nd month |
DOTS |
4. Discussion
This review of 39 studies provided a comprehensive overview of available data on user-experience with quality of TB care in India. Overall, user-experience was highly impacted by two major themes: providers and convenience, as well as six minor themes of confidence, supplies and equipment, information, waiting time, stigma, and confidentiality. Negative and positive experiences were reported for each theme, suggesting that they act as both barriers and facilitators, and as important determinants of good quality care from the patients’ perspective. The themes were also observed to interact and overlap in some instances; providers often enabled convenience, determined information received, and inspired confidence in care; while convenience (particularly the structure of DOTS) impacted confidentiality and stigma, choice of providers, and was enabled by available supplies and short waiting times.
Seven studies that directly quantified patient satisfaction reported a majority of patients being satisfied with various aspects of care. High overall satisfaction with TB care has been found in several other low- and middle-income countries (LMICs), including Brazil, Ethiopia, Nigeria, and South Africa, although they often mask substantive shortcomings in specific aspects of care such as staff availability [31,[96], [97], [98]. Similarly, in this review, major deficiencies that often influenced patients to give up treatment or switch providers, were 1) dissatisfaction with the inconvenient timings and frequency of visits for DOTS which conflicted with work, travel, emergencies and other life priorities; and 2) providers being unavailable, disrespectful, or unable to diagnose, treat or counsel patients appropriately.
One explanation for the discrepancy between high patient satisfaction and varying or negative user-experiences is the limitations in the measure of patient satisfaction. Satisfaction is only an indication of acceptable or expected care, as opposed to superior service [99,100]. Hence, patient satisfaction is based on subjective expectations of care, which in turn can be influenced by an individual's personal characteristics and sociodemographic variables such as present health status, education, or age [101], [102], [103], [104]. Vulnerable populations can be most unwilling to express criticism as they fear losing health services as a consequence [105]. In several studies in this review, patients’ main reasons for reporting high satisfaction were early improvement from symptoms and free medicines available [57,60,95]. Hence, it is possible that present health status (early symptomatic relief) and socio-economic status of TB patients, that are largely low-income [106], [107], [108], may have influenced their expectations.
In addition, the questionnaires used in the quantitative studies to evaluate both patient satisfaction and user-experiences were not previously published, validated or reliable, which is important when collecting accurate data on patient views for improvements in quality of care [109]. Further, most studies were in a limited number of Southern and Northern States, largely within the public sector amongst pulmonary, drug-sensitive TB patients, and did not stratify experiences of people in poverty or with disabilities and comorbidities. This demonstrated the dearth of patient perspective studies in several high-burden regions of the country, on patients with DR-TB and comorbidities, within the private sector, and amongst vulnerable populations.
Regardless, available user-experiences data can provide insight into gaps in quality of care and why patients may be leaving public TB services. Barriers and facilitators related to the major themes, provider and convenience, have been reported by patients in many other LMICs, including the aforementioned countries, as well as Burkina Faso, Iran, Pakistan, and Senegal [96,[110], [111], [112], [113], [114], [115], [116], [117], [118]. Stigma from healthworkers [119], information and communication [96,111], waiting time [96,97,115], confidence [116,120] and confidentiality [96,110] were also factors in some studies, including in Nepal and Vietnam. The common themes demonstrate that these aspects of quality of TB care may be important for users globally in a variety of contexts. This review also re-iterated findings in these studies and previous literature reviews on patients’ appreciation of an individualized and flexible DOTS approach to enhance convenience and patient-centered care [121], [122], [123], [124], [125]. Additional themes in these studies that did not play a major role in this review included patient involvement or autonomy in decision-making [110], general conditions of facilities (i.e. cleanliness) and amenities (such as toilets) [96,97,112,115], co-ordination or organization of care [96,111], as well as additional support services such as nutrition and food supplements [111,112]. This could be because the studies in this review did not evaluate these aspects in their questionnaires and interviews, however these are important to explore in the Indian context for future research.
Several patients in this review were found to switch between public and private health sectors due to poor user-experiences, often including limited provider support and mistrust of the public health system. When undertaking treatment with PPs, some patients perceived greater protection of confidentiality and allowance of flexibility in DOTS, and hence more user-friendly or patient-centered care. Studies from TB providers’ perspective support this finding as they express patients prefer them due to a lack of confidence in the often overburdened public sector, where patients feel alienated and ignored due to less time with the doctor [126,127]. PPs describe how their TB patients prefer private facilities because of convenience and personalized care that is able to meet individual needs, as opposed to the rigid control activities of the district TB programme. It has been noted that the rigid enforcement of DOTS may be threatening optimal adherence and patient dignity, particularly for vulnerable groups [128], [129], [130].
The perceived enhanced convenience, confidentiality and confidence in the private sector may explain why some patients prefer to receive care with PPs, despite the provision of free medicines and diagnostics by the government. However, public practitioners have been found to be more technically competent compared to PPs, with regards to detecting and treating TB appropriately [126,131,132]. This is an important consideration as user-experiences were largely impacted by the kind of provider patients choose, have access to, or the DOTS provider they are assigned, consistent with systematic reviews and studies showing patient-practitioner relationship being the most important health service factor impacting satisfaction [104,133].
In addition to the provider, patient- and context-related factors also play a role in determining user-experiences and explaining the variability in this review. This includes socio-economic status or the caste system which is highly relevant in the Indian context. Lower social caste has been significantly associated with longer waiting times (p < 0.0001) in private facilities [134]. Studies on TB providers’ perspectives in India suggest that they may treat patients differently, providing poor and less educated patients with less information and agency as they question their ability to understand medical information and perceive them as irrational when prioritizing life concerns over adherence [126,127,135]. Varying gender roles may have also influenced experiences. Both women and men may find the structure of DOTS inconvenient, as generally female TB patients struggle with managing daily child-care and household responsibilities [136,137], and male TB patients are concerned with retaining employment, being typically the primary earners [138,139]. Studies in South India and Maharashtra have also found that women face greater social consequences of having TB, such as marriageability, divorce, familial rejection and harassment [136], [137], [138], [139], [140], [141]; this may make confidentiality and stigma a greater concern amongst women. Further, predominantly more male TB patients are impacted by addiction to substances (primarily alcohol and tobacco) [64,65,93,141,142] which suggests additional counselling needs from providers.
Differences in experiences may also be due to varying urban and rural contexts. Rural facilities may not always be equipped with full diagnostic services, making availability of supplies and equipment a greater concern [143,144]. In addition, patients from rural regions living and working in urban regions also have unique needs as indicated in this review, particularly for maintaining continuity of DOTS when temporarily migrating for work or family emergencies. This aligns with the finding that rural-to-urban migration may increase the risk of loss-to-follow-up amongst TB patients [143,145]. Further, important commitments such as weddings, festivals, and functions have been previously associated with TB treatment non-completion in several regions of India [146]. The cultural significance of such events may be unique to the Indian context and explored further with regards to maintaining continuity of TB care.
5. Limitations
This study has certain limitations. Firstly, the data analysed in the review were often part of studies wherein the primary goal was to assess diagnostic delays, care-seeking pathways, provider-preference, or patient adherence to treatment, not to directly assess patient satisfaction or experiences. This may have also skewed answers and results to be more negative as the sample in several studies consisted of patients who stopped or delayed care or were dissatisfied with services. Secondly, only one reviewer conducted the full-text screening, data extraction and analysis, therefore there is a possibility of bias in the study selection and results presented. Thirdly, the search strategy did not contain keywords related to India (such as RNTCP or names of States) and only searched seven journals, which may have resulted in missing some studies. Finally, included studies did not report disaggregated data and were heterogenous in data collection, thus data synthesis was limited and no concrete conclusions could be made on specific factors affecting user-experience and patient satisfaction.
6. Recommendations for TB programme and future research
For greatest impact within the TB programme, two broad, interconnected areas in line with the major user-experience themes are recognized as areas for quality improvement: the interpersonal aspect of care and the patient-centeredness of care. For improving interpersonal care, providers should be adequately trained in TB care, particularly with an emphasis on the practices of counselling, information-giving, and empathy, including ways to support and understand patients’ side-effects and external circumstances. To improve the patient-centeredness of care, DOTS should be negotiated in partnership with the user according to their unique needs and circumstances. Flexibility in DOTS has become increasingly accepted and may make for more efficient TB control in resource-limited settings, as it focuses on the most at-risk populations that require adherence monitoring [147,148]. This can involve the co-design of an individualized schedule, location, and provider with patients that ensures adherence while being logistically feasible and emotionally desirable to patients. The schedule should also be dynamically adaptable to maintain continuity of care during life events and migration. The scale-up and institutionalization of effective digital innovations, such as 99DOTS and videoDOTS, may also promote the user-friendliness of DOTS [123,149,150].
To design these service quality improvements, it is recommended that the programme use principles of human-centered design, including end-user engagement in every stage of decision-making and strategizing. User consultations and joint working groups with patients, providers, and programme staff could enable the co-design of services that ensures patient satisfaction, user empowerment, and improved TB programme performance, as well as introduce equity and human-centeredness in a traditionally top-down approach [41,151]. In addition, it is recommended that the TB programme develop or adapt a tool to assess patient perspectives nationally and collect user-experience data systematically as part of routine monitoring and evaluation activities. A validated, standardized tool that includes qualitative narratives and disaggregates demographic data will allow for user-experience to be measured across states, sectors, populations, and types of TB for robust comparative assessments and identification of targeted populations, regions, and interventions for service quality improvement [152]. In so doing, the programme will not only be able to pinpoint bottlenecks for effective decision-making and resource-allocation, but also highlight areas where service delivery is achieving high user-satisfaction and successful outcomes, to emulate. Harnessing user-experience data in this way to inform service quality improvements is likely to improve patient retention, usability, confidence and value of public sector TB care.
7. Conclusion
This review identified several important themes of user-experience with TB quality of care in India, particularly provider-related factors of availability, respect and technical capacity, as well as convenience, namely the schedule and frequency of DOTS that can conflict with patients’ daily lives. While several aspects of care were viewed favourably by patients, poor user-experiences were often responsible for patients stopping treatment and dropping-out of the public health system. Patient-centeredness, or the user-friendliness of TB care can be improved by introducing individualized and flexible DOTS, and ensuring trained, compassionate providers. Due to heterogeneity amongst studies, there is a need for standardized data collection using validated tools to allow for stronger conclusions and assessments of experiences across populations and contexts, and to collect missing data on vulnerable people, patients with DR-TB and comorbidities, and the private sector. To close gaps in the cascade of care and reach the ‘missing’ millions, it will be important to address these quality of care dimensions that are important to patients and to co-design a more user-centric system with them.
Decleration of Competing Interest
The Author declares that there is no conflict of interest.
Acknowledgments
Acknowledgements
The author is grateful to Danielle Cazabon and Tripti Pande (McGill International TB Centre) for their invaluable and substantive guidance through every step of this study, including developing the protocol, screening studies, and reviewing multiple drafts. Prof. Madhukar Pai (McGill University, McGill International TB Centre) is also thanked for his gracious support in initiating and encouraging this research. The author also thanks Genevieve Gore (McGill University) for her contributions to formulating the search strategy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jctube.2019.100127.
Appendix. Supplementary materials
References
- 1.World Health Organization. Global tuberculosis report 2018 [Internet]. 2018[cited 2018 Oct 26]. Available from:https://www.who.int/tb/publications/global_report/en/.
- 2.Central TB Division. National strategic plan 2017 - 2025. 2017.
- 3.Pai M., Sharma S.K. Are we providing quality care to our patients with tuberculosis? Indian J Med Res. 2007;125(4):491–497. [PubMed] [Google Scholar]
- 4.Satyanarayana S, Subbaraman R, Shete P, Gore G, Das J, Cattamanchi A. Quality of tuberculosis care in India: a systematic review. Int J Tuberc Lung Dis. 2015;19(7):751–763. doi: 10.5588/ijtld.15.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis. 2014;18(3):255–266. doi: 10.5588/ijtld.13.0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwan A, Daniels B, Saria V, Satyanarayana S, Subbaraman R, McDowell A. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med. 2018;15(9) doi: 10.1371/journal.pmed.1002653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis. 2014;18(3):255–266. doi: 10.5588/ijtld.13.0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das J., Kwan A., Daniels B., Satyanarayana S., Subbaraman R., Bergkvist S. Use of standardised patients to assess quality of tuberculosis care: a pilot, cross-sectional study. Lancet Infect Dis. 2015;15(11):1305–1313. doi: 10.1016/S1473-3099(15)00077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health & Family Welfare. National health policy 2017 [Internet]. 2017[cited 2018 Jul 13]. Available from:http://164.100.158.44/showfile.php?lid=4276.
- 10.Satyanarayana S, Nair SA, Chadha SS, Shivashankar R, Sharma G, Yadav S. From where are tuberculosis patients accessing treatment in India? Results from a cross-sectional community based survey of 30 districts. PLoS One [Internet] 2011;6(9) doi: 10.1371/journal.pone.0024160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166304/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Subbaraman R, Nathavitharana RR, Satyanarayana S, Pai M, Thomas BE, Chadha VK. The tuberculosis cascade of care in India’s public sector: a systematic review and meta-analysis. PLoS Med. 2016;13(10) doi: 10.1371/journal.pmed.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subbaraman R, Nathavitharana RR, Satyanarayana S, Pai M, Thomas BE, Chadha VK. The tuberculosis cascade of care in India’s public sector: a systematic review and meta-analysis. PLoS Med. 25 Oct 2016;13(10) doi: 10.1371/journal.pmed.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Datta K, Bhatnagar T, Murhekar M. Private practitioners’ knowledge, attitude and practices about tuberculosis, Hooghly district, India. Indian J Tuberc. Oct 2010;57(4):199–206. [PubMed] [Google Scholar]
- 14.Bharaswadkar S, Kanchar A, Thakur N, Shah S, Patnaik B, Click ES. Tuberculosis management practices of private practitioners in Pune municipal corporation, India. PLoS ONE. 2014;9(6):e97993. doi: 10.1371/journal.pone.0097993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uplekar MW, Shepard DS. Treatment of tuberculosis by private general practitioners in India. Tubercle. Dec 1991;72(4):284–290. doi: 10.1016/0041-3879(91)90055-w. [DOI] [PubMed] [Google Scholar]
- 16.Das J., Kwan A., Daniels B., Satyanarayana S., Subbaraman R., Bergkvist S. Use of standardised patients to assess quality of tuberculosis care: a pilot, cross-sectional study. Lancet Infect Dis. Nov 2015;15(11):1305–1313. doi: 10.1016/S1473-3099(15)00077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Udwadia Z.F., Pinto L.M., Uplekar M.W. Tuberculosis management by private practitioners in Mumbai, India: has anything changed in two decades? PLoS One [Internet] 9 Aug 2010;5(8) doi: 10.1371/journal.pone.0012023. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2918510/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Padayatchi N, Daftary A, Naidu N, Naidoo K, Pai M. Tuberculosis: treatment failure, or failure to treat? Lessons from India and South Africa. BMJ Global Health. 1 Jan 2019;4(1) doi: 10.1136/bmjgh-2018-001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kruk M.E., Gage A.D., Arsenault C., Jordan K., Leslie H.H., Roder-DeWan S. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. Nov 2018;6(11):e1196–e1252. doi: 10.1016/S2214-109X(18)30386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fitzpatrick R. Surveys of patients satisfaction: i–Important general considerations. BMJ. 13 Apr 1991;302(6781):887–889. doi: 10.1136/bmj.302.6781.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manary M.P., Boulding W., Staelin R. Glickman S.W.The patient experience and health outcomes. N Engl J Med. 2013;368:201–203. doi: 10.1056/NEJMp1211775. [DOI] [PubMed] [Google Scholar]
- 22.Al-Abri R., Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. Jan 2014;29(1):3–7. doi: 10.5001/omj.2014.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agency for Healthcare Research and Quality. What is patient experience? [Internet]. 2016[cited 2018 Jul 24]. Available from: /cahps/about-cahps/patient-experience/index.html.
- 24.Al-Abri R., Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. Jan 2014;29(1):3–7. doi: 10.5001/omj.2014.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151–155. doi: 10.4103/0974-2077.74491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta K.S., Rokade V. Importance of quality in health care sector: a review. J Health Manage [Internet] 6 Mar 2016 Available from: http://journals.sagepub.com/doi/pdf/10.1177/0972063415625527. [Google Scholar]
- 27.Vuori H. Patient satisfaction—does it matter? Int J Qual Health Care. 1 Sep 1991;3(3):183–189. doi: 10.1093/intqhc/3.3.183. [DOI] [PubMed] [Google Scholar]
- 28.Kruk M.E., Gage A.D., Arsenault C., Jordan K., Leslie H.H., Roder-DeWan S. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. Nov 2018;6(11):e1196–e1252. doi: 10.1016/S2214-109X(18)30386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shirley ED, Sanders JO. Patient satisfaction: implications and predictors of success. J Bone Joint Surg-Am Vol. May 2013;95(10) doi: 10.2106/JBJS.L.01048. e69-1–4. [DOI] [PubMed] [Google Scholar]
- 30.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 1 Jan 2013;3(1) doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nezenega ZS, Gacho YH, Tafere TE. Patient satisfaction on tuberculosis treatment service and adherence to treatment in public health facilities of Sidama zone, South Ethiopia. BMC Health Serv Res. 22 Mar 2013;13:110. doi: 10.1186/1472-6963-13-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dang BN, Westbrook RA, Black WC, Rodriguez-Barradas MC, Giordano TP. Examining the link between patient satisfaction and adherence to HIV care: a structural equation model. PLoS ONE. 2013;8(1):e54729. doi: 10.1371/journal.pone.0054729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dubina M.I., O'Neill J.L., Feldman S.R. Effect of patient satisfaction on outcomes of care. Expert Rev Pharmacoecon Outcomes Res. Oct 2009;9(5):393–395. doi: 10.1586/erp.09.45. [DOI] [PubMed] [Google Scholar]
- 34.Mehta S. Service quality as predicator of patient satisfaction: a study of the health care sector. J Health Manag. 1 Jun 2011;13(2):211–229. [Google Scholar]
- 35.Larson E, Leslie HH, Kruk ME. The determinants and outcomes of good provider communication: a cross-sectional study in seven African countries. BMJ Open. 2017;7(6) doi: 10.1136/bmjopen-2016-014888. 02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.What is patient-centered care? [Internet] NEJM Catalyst. 2017 https://catalyst.nejm.org/what-is-patient-centered-care/ [cited 2018 Nov 1]. Available from: [Google Scholar]
- 37.Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 3 Dec 2008;20(12):600–607. doi: 10.1111/j.1745-7599.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- 38.Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & commentary. Measuring patient experience as a strategy for improving primary care. Health Aff (Millwood) May 2010;29(5):921–925. doi: 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
- 39.Sower V., Duffy J., Kilbourne W., Kohers G., Jones P. The dimensions of service quality for hospitals: development and use of the KQCAH scale. Health Care Manage Rev. 2001;26(2):47–59. doi: 10.1097/00004010-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Bacon CT, Mark B. Organizational effects on patient satisfaction in hospital medical-surgical units. JONA J Nurs Admin. May 2009;39(5):220–227. doi: 10.1097/NNA.0b013e3181a23d3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bate P, Robert G. Methods and practices of experience-based design. Radcliffe Publishing; 2007. Bringing user experience to healthcare improvement: the concepts. 221. [Google Scholar]
- 42.Bjertnaes O.A., Sjetne I.S., Iversen H.H. Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Qual Saf. 1 Jan 2012;21(1):39–46. doi: 10.1136/bmjqs-2011-000137. [DOI] [PubMed] [Google Scholar]
- 43.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 1 Feb 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 44.Pomey M-P, Ghadiri DP, Karazivan P, Fernandez N, Clavel N. Patients as partners: a qualitative study of patients’ engagement in their health care. PLoS One [Internet] 9 Apr 2015;10(4) doi: 10.1371/journal.pone.0122499. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391791/ [cited 2018 Oct 27]Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vogus TJ, McClelland LE. When the customer is the patient: lessons from healthcare research on patient satisfaction and service quality ratings. Hum Resour Manage Rev. 1 Mar 2016;26(1):37–49. [Google Scholar]
- 46.Cazabon D, Pande T, Sen P, Daftary A, Arsenault C, Bhatnagar H, et al. Patient experience in tuberculosis care services in low-and-middle income countries: a systematic review of quantitative studies. Unpublished manuscript *Both first authors contributed equally to this work.
- 47.Barter DM, Agboola SO, Murray MB, Bärnighausen T. Tuberculosis and poverty: the contribution of patient costs in sub-Saharan Africa – a systematic review. BMC Public Health. 14 Nov 2012;12(1):980. doi: 10.1186/1471-2458-12-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tanimura T, Jaramillo E, Weil D, Raviglione M, Lönnroth K. Financial burden for tuberculosis patients in low- and middle-income countries: a systematic review. Eur Respir J. 1 Jan 2014 doi: 10.1183/09031936.00193413. erj01934-2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cai J, Wang X, Ma A, Wang Q, Han X, Li Y. Factors associated with patient and provider delays for tuberculosis diagnosis and treatment in Asia: a systematic review and meta-analysis. PLoS ONE. 25 Mar 2015;10(3) doi: 10.1371/journal.pone.0120088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 14 Jan 2008;8(1):15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 1 Dec 2016;6(12) doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Critical Appraisal Skills Programme. CASP qualitative checklist [Internet]. 2018[cited 2018 Oct 1]. Available from:https://casp-uk.net/casp-tools-checklists/.
- 53.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 10 Jul 2008;8(1):45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Popay J., (Jennie), Roberts H.M., (Helen), Sowden A., (Amanda), Petticrew M., (Mark), Arai L., (Lisa), Rodgers M., (Mark) Institute for Health Research; Jan 2006. Guidance on the conduct of narrative synthesis in sytematic reviews [Internet]https://tees.openrepository.com/tees/handle/10149/133990 [cited 2018 Jul 24]. Available from: [Google Scholar]
- 55.Sandelowski M., Voils C.I., Barroso J. Defining and designing mixed research synthesis studies. Res Sch. 2006;13(1):29. [PMC free article] [PubMed] [Google Scholar]
- 56.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. PLoS Med. 21 Jul 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Srivastava K, Gupta A, Saxena R, Sharma RP, Midha T. Patient’s satisfaction regarding directly observed treatment short course under RNTCP in a district of North India. Int J Commun Med Public Health. 2017;4(5):1536–1541. [Google Scholar]
- 58.Gupta S. Evaluation of patient satisfaction level undergoing DOTS therapy in Meerut District of Uttar Pradesh. J Adv Med Dent Sci Res. 2015;3(2):34–37. [Google Scholar]
- 59.Haque M, Dhirendra K, Shaili V. A study on socio-demographic profile and feasibility of DOTS provider registered under RNTCP in Varanasi district Uttar Pradesh. Indian J Community Health. 2014;26(1):107–110. [Google Scholar]
- 60.Srivastav S, Mahajan H. Satisfaction levels among patients availing DOTS services in Bundelkhand Region (UP), India: evidence from patient exit-interviews. Ann Tropic Med Public Health. 2014;7(2):116–119. [Google Scholar]
- 61.Rai N, Singh S, Kushwah S, Dubey D. A cross sectional study on evaluation of satisfaction level of TB patients enrolled for directly observed treatment, short course chemotherapy in a district of Central India. Int J Commun Med Public Health. 2017 [Google Scholar]
- 62.Jaiswal A, Singh V, Ogden J, Porter J, Sharma P, Sarin R. Adherence to tuberculosis treatment: lessons from the urban setting of Delhi, India. Tropic Med Int Health. 2003;8(7):625–633. doi: 10.1046/j.1365-3156.2003.01061.x. [DOI] [PubMed] [Google Scholar]
- 63.Gupta S, Gupta S, Behera D. Reasons for interruption of anti-tubercular treatment as reported by patients with tuberculosis admitted in a tertiary care institute. Indian J Tuberc. 2010;58(1):11–17. [PubMed] [Google Scholar]
- 64.Patel PG, Bala DV, Vagela SD. Correlates of delayed initiation of treatment after confirmed diagnosis under RNTCP: a cross sectional study in Ahmedabad Municipal Corporation, India. NatlJ Commun Med. 2013;4(4):550–554. [Google Scholar]
- 65.Srinath MP. Reasons for default and death among tuberculosis cases treated under revised national tuberculosis control program in selected tuberculosis units of Bangalore urban district of Karnataka state. Int J Commun Med Public Health. 23 Jul 2018;5(8):3270–3275. [Google Scholar]
- 66.Paul D., Busireddy A., Nagaraja S.B., Satyanarayana S., Dewan P.K., Nair S.A. Factors associated with delays in treatment initiation after tuberculosis diagnosis in two districts of India. Plos One [Internet] Jul 2012;7(7) doi: 10.1371/journal.pone.0039040. http://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0039040&type=printable Available from:://WOS:000306354700006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mehra D, Kaushik RM, Kaushik R, Rawat J, Kakkar R. Initial default among sputum-positive pulmonary TB patients at a referral hospital in Uttarakhand, India. Trans R Soc Trop Med Hyg. Sep 2013;107(9):558–565. doi: 10.1093/trstmh/trt065. [DOI] [PubMed] [Google Scholar]
- 68.Dandona R, Dandona L, Mishra A, Dhingra S, Venkatagopalakrishna K, Chauhan LS. Utilization of and barriers to public sector tuberculosis services in India. Natl Med J India. Nov 2004;17(6):292–299. [PubMed] [Google Scholar]
- 69.Selvam J, Wares F, Perumal M, Gopi P, Sudha G, Chandrasekaran V. Health-seeking behaviour of new smear-positive TB patients under a DOTS programme in Tamil Nadu, India, 2003. Int J Tuberculosis Lung Disease. 2007;11(2):161–167. [PubMed] [Google Scholar]
- 70.Tripathi U, Nagaraja S, Tripathy J, Sahu S, Parmar M, Rade K. Follow-up examinations: are multidrug-resistant tuberculosis patients in Uttar Pradesh, India, on track? Public Health Action. 2015;5(1):59–64. doi: 10.5588/pha.14.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rashmi VB. Client satisfaction in rural India for primary health care - a tool for quality assessment. Al Ameen J Med Sci. 2010;3(2):109–114. [Google Scholar]
- 72.Divija P, Purty A, Stalin P, Zile S, Govindarajan S, Velavan A. Initial default among tuberculosis patients diagnosed in selected medical colleges of Puducherry: issues and possible interventions. Int J Med Sci Public Health. 2015;4(7):957–960. [Google Scholar]
- 73.Mallick A, Haldar S, Sarkar S, Kundu S, Sinha S, Sadhukhan SK. Unmatched case control study on risk factors of defaulter among newly diagnosed TB patients on DOTS registered under RNTCP in Hooghly district, West Bengal, India. Int J Commun Med Public Health. 2017;4(10):3678. [Google Scholar]
- 74.Tiwari S., Wavare R.R. Reasons for non-compliance and profile of tuberculosis patients in urban area of Indore. Natl J Commun Med. 2015;6(1):55–59. [Google Scholar]
- 75.Yellappa V., Lefevre P., Battaglioli T., Devadasan N., Van der Stuyft P. Patients pathways to tuberculosis diagnosis and treatment in a fragmented health system: a qualitative study from a south Indian district. BMC Public Health [Internet] Aug 2017;17(635) doi: 10.1186/s12889-017-4627-7. https://bmcpublichealth.biomedcentral.com/track/pdf/10.1186/s12889-017-4627-7 Available from: //WOS:000406977500001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rai N, Kushwah SS, Singh SP, Dubey D. An assessment of treatment compliance among patients on DOTS under revised national tuberculosis control programme in district Rewa, Madhya Pradesh, India. Int J Commun Med Public Health. 2015:373–379. [Google Scholar]
- 77.Charles N., Thomas B., Watson B., Raja Sakthivel M., Chandrasekeran V., Wares F. Care seeking behavior of chest symptomatics: a community based study done in South India after the implementation of the RNTCP. PloS one [Internet] 20 Sep 2010;5(9) doi: 10.1371/journal.pone.0012379. http://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0012379&type=printable Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yamini K, Rao BT, Valleswary K. Socio demographic determinants of health care seeking behaviour among tuberculosis patients admitted in the isolation ward of tertiary care hospital: a health belief model. Int J Commun Med Public Health. 2017;4(12):4668–4675. [Google Scholar]
- 79.Benbaba S, Isaakidis P, Das M, Jadhav S, Reid T, Furin J. Direct observation (DO) for drug-resistant tuberculosis: do we really DO? PLoS ONE. 2015;10(12) doi: 10.1371/journal.pone.0144936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Goel K., Kondagunta N., Soans S.J., Bairy A.R., Goel P. Reasons for patient delays & health system delays for tuberculosis in South India. Indian J Commun Health. 2011;23(2):87–89. [Google Scholar]
- 81.Mistry N, Rangan S, Dholakia Y, Lobo E, Shah S, Patil A. Durations and delays in care seeking, diagnosis and treatment initiation in uncomplicated pulmonary tuberculosis patients in Mumbai, India. PLoS ONE. 2016;11(3) doi: 10.1371/journal.pone.0152287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Furin J, Isaakidis P, Reid A, Kielmann K. “I’m fed up”: experiences of prior anti-tuberculosis treatment in patients with drug-resistant tuberculosis and HIV. Int J Tubercul Lung Dis. 2014;18(12):1479–1484. doi: 10.5588/ijtld.14.0277. [DOI] [PubMed] [Google Scholar]
- 83.Singh V, Jaiswal A, Porter J, Ogden J, Sarin R, Sharma P. TB control, poverty, and vulnerability in Delhi, India. Tropic Med Int Health. 2002;7(8):693–700. doi: 10.1046/j.1365-3156.2002.00909.x. [DOI] [PubMed] [Google Scholar]
- 84.Yellappa V, Lefevre P, Battaglioli T, Narayanan D, van der Stuyft P. Coping with tuberculosis and directly observed treatment: a qualitative study among patients from South India. BMC Health Serv Res [Internet] 2016;16(283) doi: 10.1186/s12913-016-1545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rakesh P, Shibu B, Krishnaveni V, Vishnu N, Swapna P, Thomas S. Patients’ perception towards directly observed treatment - a qualitative study from Kollam district, Kerala, southern India. Indian J Tubercul. 2016;64(2):93–98. doi: 10.1016/j.ijtb.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 86.Pranavi S, Murugan V, Kalaiselvan G. Health seeking behavior and reasons for “patient‐related” diagnostic delay among pulmonary tuberculosis suspects attending designated microscopy centre of medical college in rural Puducherry. Int J Commun Med Public Health. 2017;4(4):1314–1318. [Google Scholar]
- 87.Jebamalar J, Senthilkumar P, Ramola M. Health seeking behaviour in pulmonary tuberculosis: a cross sectional study. Int J Commun Med Public Health. 2018;5(4):1346. [Google Scholar]
- 88.Sawase GB, Acharya S, Shinde RR. A cross-sectional study to assess the perceptions and experiences of tuberculosis patients about directly observed treatment in an urban slum, in Mumbai, Maharashtra, India. Int J Commun Med Public Health. 22 Dec 2016;3(12):3515–3519. [Google Scholar]
- 89.Yellapa V, Devadasan N, Krumeich A, Pant Pai N, Vadnais C, Pai M. How patients navigate the diagnostic ecosystem in a fragmented health system: a qualitative study from India. Glob Health Action. 2017;10(1) doi: 10.1080/16549716.2017.1350452. N.PAG-N.PAG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sudha G, Nirupa C, Rajasakthivel M, Sivasusbramanian S, Sundaram V, Bhatt S. Factors influencing the care-seeking behaviour of chest symptomatics: a community-based study involving rural and urban population in Tamil Nadu, South India. Tropic Med Int Health TM & IH. Apr 2003;8(4):336–341. doi: 10.1046/j.1365-3156.2003.01010.x. [DOI] [PubMed] [Google Scholar]
- 91.Isaakidis P, Rangan S, Pradhan A, Ladomirska J, Reid T, Kielmann K. “I cry every day”: experiences of patients co-infected with HIV and multidrug-resistant tuberculosis. Tropic Med Int Health. 2013;18(9):1128–1133. doi: 10.1111/tmi.12146. [DOI] [PubMed] [Google Scholar]
- 92.Jaggarajamma K, Balambal R, Muniyandi M, Vasantha M, Beena T, Nirupa C. Perceptions of tuberculosis patients about private providers before and after implementation of revised National Tuberculosis Control Programme. Indian J Tubercul. 2009;56(4):185–190. [PubMed] [Google Scholar]
- 93.Dhingra V, Rajpal S, Aggarwal N, Aggarwal JK. Treatment of tuberculosis pleural effusion patients and their satisfaction with DOTS – 1½ year follow up. Indian J Tubercul. 2004;51(t):209–212. [Google Scholar]
- 94.Grover A, Kumar R, Jindal S. Treatment seeking behaviour of chest symptomatics. Ind J Tubercul. 2003;50:87–94. [Google Scholar]
- 95.Sukumaran P, Venugopal KP, Majooran RS. A social study of compliance with DOTS. Ind J Tubercul. 2002;49:205–208. [Google Scholar]
- 96.Portela MC, Lima SML, Brito C, Ferreira VMB, Escosteguy CC, de Vasconcellos MTL. Tuberculosis control program and patient satisfaction, Rio de Janeiro, Brazil. Revista de Saúde Pública. Jun 2014;48(3):497–507. doi: 10.1590/S0034-8910.2014048004793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bao V.N., LaMontagne S., Nhung N.V., Nga L.T.Barriers to access and use of public TB diagnostic services in Vietnam [Internet]. Vietnam: USAID; [cited 2018 Oct 23]. Available from:https://path.org/resources/barriers-to-access-and-use-of-public-tb-diagnostic-services-in-vietnam/.
- 98.Chimbindi N, Bärnighausen T, Newell M-L. Patient satisfaction with HIV and TB treatment in a public programme in rural Kwazulu-Natal: evidence from patient-exit interviews. BMC Health Serv Res. 23 Jan 2014;14:32. doi: 10.1186/1472-6963-14-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sofaer S, Firminger K. Patient perceptions of the quality of health services. Annu Rev Public Health. 2005;26(1):513–559. doi: 10.1146/annurev.publhealth.25.050503.153958. [DOI] [PubMed] [Google Scholar]
- 100.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1 Dec 1997;45(12):1829–1843. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 101.Bjertnaes O.A., Sjetne I.S., Iversen H.H. Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Qual Saf. 1 Jan 2012;21(1):39–46. doi: 10.1136/bmjqs-2011-000137. [DOI] [PubMed] [Google Scholar]
- 102.Sofaer S, Firminger K. Patient perceptions of the quality of health services. Annu Rev Public Health. 2005;26(1):513–559. doi: 10.1146/annurev.publhealth.25.050503.153958. [DOI] [PubMed] [Google Scholar]
- 103.Farley H, Enguidanos ER, Coletti CM, Honigman L, Mazzeo A, Pinson TB. Patient satisfaction surveys and quality of care: an information paper. Ann Emerg Med. 1 Oct 2014;64(4):351–357. doi: 10.1016/j.annemergmed.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 104.Crow R, Gage H, Hampson S, Hart J. The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature. Clinic Govern Bradford. 2003;8(4):352. doi: 10.3310/hta6320. [DOI] [PubMed] [Google Scholar]
- 105.Zaslavsky A.M., Hochheimer J.N., Schneider E.C., Cleary P.D., Seidman J.J., McGlynn E.A. Impact of sociodemographic case mix on the HEDIS measures of health plan quality. Med Care. Oct 2000;38(10):981–992. doi: 10.1097/00005650-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 106.Muniyandi M., Ramachandran R., Balasubramanian R., Narayanan P.R. Socio-economic dimensions of tuberculosis control: review of studies over two decades from Tuberculosis Research Center. J Commun Dis. Mar 2006;38(3):204–215. [PubMed] [Google Scholar]
- 107.Muniyandi M., Ramachandran R. Socioeconomic inequalities of tuberculosis in India. Expert Opin Pharmacother. Jul 2008;9(10):1623–1628. doi: 10.1517/14656566.9.10.1623. [DOI] [PubMed] [Google Scholar]
- 108.Oxlade O, Murray M. Tuberculosis and poverty: why are the poor at greater risk in India? PLoS ONE. 19 Nov 2012;7(11):e47533. doi: 10.1371/journal.pone.0047533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wensing M., Elwyn G. Research on patients’ views in the evaluation and improvement of quality of care. Qual Saf Health Care. Jun 2002;11(2):153–157. doi: 10.1136/qhc.11.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Behzadifar M., Mirzaei M., Behzadifar M., Keshavarzi A., Behzadifar M., Saran M. Patients’ experience of tuberculosis treatment using directly observed treatment, short-course (DOTS): a qualitative study. Iran Red Crescent Med J [Internet] 25 Apr 2015;17(4) doi: 10.5812/ircmj.17(4)2015.20277. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4443395/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Serapelwane MG, Davhana–Maselesele M, Masilo GM. Experiences of patients having tuberculosis (TB) regarding the use of directly observed treatment short-course (DOTS) in the North West Province, South Africa. Curationis. 27 Sep 2016;39(1):9. doi: 10.4102/curationis.v39i1.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Getahun B, Nkosi ZZ. Satisfaction of patients with directly observed treatment strategy in Addis Ababa, Ethiopia: a mixed-methods study. PLoS ONE. 9 Feb 2017;12(2) doi: 10.1371/journal.pone.0171209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Khan M.A., Walley J.D., Witter S.N., Shah S.K., Javeed S. Tuberculosis patient adherence to direct observation: results of a social study in Pakistan. Health Policy Plan. Nov 2005;20(6):354–365. doi: 10.1093/heapol/czi047. [DOI] [PubMed] [Google Scholar]
- 114.Sanou A., Dembele M., Theobald S., Macq J. Access and adhering to tuberculosis treatment: barriers faced by patients and communities in Burkina Faso. Int J Tuberc Lung Dis. Dec 2004;8(12):1479–1483. [PubMed] [Google Scholar]
- 115.Onyeonoro U.U., Chukwu J.N., Nwafor C.C., Meka A.O., Omotowo B.I., Madichie N.O. Evaluation of patient satisfaction with tuberculosis services in Southern Nigeria. Health Serv Insights. 13 Oct 2015;8:25–33. doi: 10.4137/HSI.S27177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gerrish K, Naisby A, Ismail M. Experiences of the diagnosis and management of tuberculosis: a focused ethnography of Somali patients and healthcare professionals in the UK. J Adv Nurs. Oct 2013;69(10):2285–2294. doi: 10.1111/jan.12112. [DOI] [PubMed] [Google Scholar]
- 117.Rundi C. Understanding tuberculosis: perspectives and experiences of the people of Sabah, East Malaysia. J Health Popul Nutr. Apr 2010;28(2):114–123. doi: 10.3329/jhpn.v28i2.4880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hane F, Thiam S, Fall AS, Vidal L, Diop AH, Ndir M. Identifying barriers to effective tuberculosis control in Senegal: an anthropological approach. Int J Tuberc Lung Dis. May 2007;11(5):539–543. [PubMed] [Google Scholar]
- 119.Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. 16 Aug 2007;7:211. doi: 10.1186/1471-2458-7-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dodor EA. The feelings and experiences of patients with tuberculosis in the Sekondi-Takoradi metropolitan district: implications for TB control efforts. Ghana Med J. Dec 2012;46(4):211–218. [PMC free article] [PubMed] [Google Scholar]
- 121.Lienhardt C, Ogden JA. Tuberculosis control in resource-poor countries: have we reached the limits of the universal paradigm? Tropic Med Int Health. 1 Jul 2004;9(7):833–841. doi: 10.1111/j.1365-3156.2004.01273.x. [DOI] [PubMed] [Google Scholar]
- 122.Macq J.C.M., Theobald S., Dick J., Dembele M. An exploration of the concept of directly observed treatment (DOT) for tuberculosis patients: from a uniform to a customised approach. Int J Tuberc Lung Dis. Feb 2003;7(2):103–109. [PubMed] [Google Scholar]
- 123.van de Berg S., Jansen-Aaldring N., de Vries G., van den Hof S. Patient support for tuberculosis patients in low-incidence countries: a systematic review. PLoS One [Internet] 10 Oct 2018;13(10) doi: 10.1371/journal.pone.0205433. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179254/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kibret KT, Moges Y, Memiah P, Biadgilign S. Treatment outcomes for multidrug-resistant tuberculosis under DOTS-Plus: a systematic review and meta-analysis of published studies. Infect Dis Poverty. 17 Jan 2017;6(1):7. doi: 10.1186/s40249-016-0214-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 24 Jul 2007;4(7):e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Fochsen G, Deshpande K, Thorson A. Power imbalance and consumerism in the doctor-patient relationship: health care providers’ experiences of patient encounters in a rural district in India. Qual Health Res. 1 Nov 2006;16(9):1236–1251. doi: 10.1177/1049732306293776. [DOI] [PubMed] [Google Scholar]
- 127.Ergler CR, Sakdapolrak P, Bohle H-G, Kearns RA. Entitlements to health care: why is there a preference for private facilities among poorer residents of Chennai, India? Soc Sci Med. 1 Feb 2011;72(3):327–337. doi: 10.1016/j.socscimed.2010.09.042. [DOI] [PubMed] [Google Scholar]
- 128.Verma G., Upshur R.E., Rea E., Benatar S.R. Critical reflections on evidence, ethics and effectiveness in the management of tuberculosis: public health and global perspectives. BMC Med Ethics. 12 Mar 2004;5:2. doi: 10.1186/1472-6939-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Selgelid M.J., Reichman L.B. Ethical issues in tuberculosis diagnosis and treatment. Int J Tuberc Lung Dis. Jun 2011;15(Suppl 2):9–13. doi: 10.5588/ijtld.10.0434. [DOI] [PubMed] [Google Scholar]
- 130.Sagbakken M., Frich J.C., Bjune G.A., Porter J.D. Ethical aspects of directly observed treatment for tuberculosis: a cross-cultural comparison. BMC Med Ethics. 2 Jul 2013;14:25. doi: 10.1186/1472-6939-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Satyanarayana S., Subbaraman R., Shete P., Gore G., Das J., Cattamanchi A. Quality of tuberculosis care in India: a systematic review. Int J Tuberc Lung Dis. Jul 2015;19(7):751–763. doi: 10.5588/ijtld.15.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vandan N, Ali M, Prasad R, Kuroiwa C. Assessment of doctors’ knowledge regarding tuberculosis management in Lucknow, India: a public-private sector comparison. Public Health. Jul 2009;123(7):484–489. doi: 10.1016/j.puhe.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 133.Rao K.D., Peters D.H., Bandeen-Roche K. Towards patient-centered health services in India—a scale to measure patient perceptions of quality. Int J Qual Health Care. 1 Dec 2006;18(6):414–421. doi: 10.1093/intqhc/mzl049. [DOI] [PubMed] [Google Scholar]
- 134.Shaikh M, Miraldo M, Renner A-T. Waiting time at health facilities and social class: evidence from the Indian caste system. PLoS ONE. 15 Oct 2018;13(10) doi: 10.1371/journal.pone.0205641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Willems S., De Maesschalck S., Deveugele M., Derese A., De Maeseneer J. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. Feb 2005;56(2):139–146. doi: 10.1016/j.pec.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 136.Rajeswari R, Balasubramanian R, Muniyandi M, Geetharamani S, Thresa X, Venkatesan P. Socio-economic impact of tuberculosis on patients and family in India. Int J Tuberc Lung Dis. Oct 1999;3(10):869–877. [PubMed] [Google Scholar]
- 137.Nair DM, George A, Chacko KT. Tuberculosis in Bombay: new insights from poor urban patients. Health Policy Plan. Mar 1997;12(1):77–85. doi: 10.1093/heapol/12.1.77. [DOI] [PubMed] [Google Scholar]
- 138.Somma D., Thomas B.E., Karim F., Kemp J., Arias N., Auer C. Gender and socio-cultural determinants of TB-related stigma in Bangladesh, India, Malawi and Colombia. Int J Tuberc Lung Dis. Jul 2008;12(7):856–866. [PubMed] [Google Scholar]
- 139.Atre SR, Kudale AM, Morankar SN, Rangan SG, Weiss MG. Cultural concepts of tuberculosis and gender among the general population without tuberculosis in rural Maharashtra, India. Tropic Med Int Health. 1 Nov 2004;9(11):1228–1238. doi: 10.1111/j.1365-3156.2004.01321.x. [DOI] [PubMed] [Google Scholar]
- 140.Hatherall B, Newell JN, Emmel N, Baral SC, Khan MA. “Who will marry a diseased girl?” marriage, gender, and tuberculosis stigma in Asia. Qual Health Res. 30 Nov 2018 doi: 10.1177/1049732318812427. 1049732318812427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Balasubramanian R., Garg R., Santha T., Gopi P.G., Subramani R., Chandrasekaran V., et al. Gender disparities in tuberculosis: report from a rural DOTS programme in south India [Internet]. 2004. Available from: https://www.ingentaconnect.com/content/iuatld/ijtld/2004/00000008/00000003/art00009%3bjsessionid=fcattcpj0nmns.x-ic-live-01#. [PubMed]
- 142.Bhattacharya T, Ray S, Biswas P, Das DK. Barriers to treatment adherence of tuberculosis patients: a qualitative study in West Bengal, India. Int J Med Sci Public Health. 2018;7(5):396–402. [Google Scholar]
- 143.Tripathy JP, Srinath S, Naidoo P, Ananthakrishnan R, Bhaskar R. Is physical access an impediment to tuberculosis diagnosis and treatment? A study from a rural district in North India. Public Health Action. 21 Sep 2013;3(3):235–239. doi: 10.5588/pha.13.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Subbaraman R, Thomas BE, Sellappan S, Suresh C, Jayabal L, Lincy S. Tuberculosis patients in an Indian mega-city: where do they live and where are they diagnosed? PLoS ONE. 2017;12(8) doi: 10.1371/journal.pone.0183240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mandal A, Basu M, Das PP, Mukherjee S, Das S, Roy N. Magnitude and reasons of initial default among new sputum positive cases of pulmonary tuberculosis under RNTCP in a district of West Bengal, India [Internet]. 2015. Available from:.
- 146.Vijay S., Kumar P., Chauhan L.S., Vollepore B.H., Kizhakkethil U.P., Rao S.G. Risk factors associated with default among new smear positive TB patients treated under DOTS in India. PLoS One [Internet] 2010;5(4) doi: 10.1371/journal.pone.0010043. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2850369/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lienhardt C, Ogden JA. Tuberculosis control in resource-poor countries: have we reached the limits of the universal paradigm? Tropic Med Int Health. 1 Jul 2004;9(7):833–841. doi: 10.1111/j.1365-3156.2004.01273.x. [DOI] [PubMed] [Google Scholar]
- 148.Macq J.C.M., Theobald S., Dick J., Dembele M. An exploration of the concept of directly observed treatment (DOT) for tuberculosis patients: from a uniform to a customised approach. Int J Tuberc Lung Dis. Feb 2003;7(2):103–109. [PubMed] [Google Scholar]
- 149.Subbaraman R., de Mondesert L., Musiimenta A., Pai M., Mayer K.H., Thomas B.E. Digital adherence technologies for the management of tuberculosis therapy: mapping the landscape and research priorities. BMJ Glob Health [Internet] 11 Oct 2018;3(5) doi: 10.1136/bmjgh-2018-001018. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6195152/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Alipanah N, Jarlsberg L, Miller C, Linh NN, Falzon D, Jaramillo E. Adherence interventions and outcomes of tuberculosis treatment: a systematic review and meta-analysis of trials and observational studies. PLoS Med. 2018;15(7) doi: 10.1371/journal.pmed.1002595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Macq J, Torfoss T, Getahun H. Patient empowerment in tuberculosis control: reflecting on past documented experiences. Tropic Med Int Health. 25 Jun 2007;12(7):873–885. doi: 10.1111/j.1365-3156.2007.01858.x. [DOI] [PubMed] [Google Scholar]
- 152.Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & commentary. Measuring patient experience as a strategy for improving primary care. Health Aff (Millwood) May 2010;29(5):921–925. doi: 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.