Abstract
Background
Tuberculosis is a common cause of mortality and morbidity among people living with HIV/AIDS. Despite the increased prognosis of tuberculosis among HIV infected patients, diagnosis of pulmonary tuberculosis (PTB) smear microscopy has a low sensitivity due to low bacterial load in a sputum specimen of HIV patients. Having alternative specimens for increasing detection of Mycobacterium tuberculosis (Mtb) is very important.
Objective
The aim of this study was to evaluate the efficacy of urine as clinical specimen for the diagnosis of pulmonary tuberculosis in people living with HIV.
Method
A total of 117 HIV-seropositive individuals from three public health facilities in Addis Ababa, Ethiopia were enrolled consecutively from December 2013 to July 2014. A total of 117 paired morning sputum and urine samples were simultaneously collected from anti-retroviral therapy (ART) naïve PTB suspected individuals living with HIV. Both sputum and urine samples were processed for culture using Lowenstein-Jensen medium, and the left was subjected to PCR using RD9 primers. Chi-square test and kappa value were used to compare different methods used.
Result
Out of 117 suspected PTB HIV-infected people, sputum culture alone detected more mycobacterial isolates 33 (28.2%) than the urine specimen alone 17 (14.5%). Of the 33 patients positive for sputum culture, 13 patients were observed as a urine culture positive. Of the 84 individuals negative for mycobacterial by sputum culture, four (4.8%) were urine culture positive and thus, the sensitivity, and the agreement between urine culture as compare to sputum culture were 39.4% and 0.49, respectively. On the other hand, the sensitivity of RD9-based PCR directly on urine was 72.7% by considering sputum culture as a reference standard. Moreover, RD9-based PCR directly on sputum detected 9 (7.7%) individuals who were sputum culture negative for M. Tuberculosis. The detection rate of M. tuberculosis from urine in patients those who couldn't produce sputum were 9(34.6%).
Conclusion
PCR and culture examination of urine samples also can improve the detection rate of M. tuberculosis in PTB suspected HIV positive individuals.
Keywords: Diagnosis, PCR, Pulmonary tuberculosis, TB-HIV infected, Tuberculosis
Abbreviation: AFB, Acid fast bacilli; CTAB, cetyltrimethylammonium bromide; DERC, Departmental Ethical Review and Research Committee; DMIP, Department of Medical Microbiology, Immunology and Parasitology; HIV, human immunodeficiency virus; L–J, Lowenstein–Jensen; Mtb, Mycobacterium tuberculosis; TB, tuberculosis; MTC, Mycobacterium tuberculosis complex; PCR, polymerase chain reaction; PTB, pulmonary tuberculosis
1. Background
In 2013, an estimated 1.1 million (13%) of the 9.0 million people who developed TB worldwide were HIV-positive. The African Region accounted for 78% of the estimated number of HIV-positive incident TB cases. In Ethiopia, the prevalence of HIV co-infection among TB patients revealed varying rates of HIV seropositivity in active TB patients ranging from 6.6% to 52.1% [1], [2], [3], [4], [5].
HIV/ AIDS fuels the TB epidemics in many ways, such as promoting progression to active tuberculosis by weakening of the immune system, increasing the risk of reactivation of latent TB infection, as well as increasing chance of TB infection once exposed to tubercle bacilli [6]. People co-infected with TB and HIV is 29 times more likely to develop active TB disease than people without HIV [7]. Also, in patients who are HIV-positive with depressed immunity (low CD4 count), the pattern of presentation is a deviation from the normal, both in clinical features and investigation findings [8]. Tuberculosis and HIV co-infections are associated with special diagnostic and therapeutic challenges and constitute an immense burden on healthcare systems of heavily infected countries like Ethiopia [9].
Unlike the straightforward diagnosis and typical presentation of pulmonary tuberculosis (PTB) in HIV seronegative individuals, the diagnosis of PTB in HIV/AIDS is more difficult [10]. This might be associated with inability or difficulty for patients to produce a sputum sample, a problem that is particularly common in young children and HIV-positive patients [11,12]. In these relatively immunodeficient patient groups, a diminished inflammatory response may inhibit sputum production. Induced sputum techniques [13], nasopharyngeal aspirates [14], fiber-optic bronchoscopy [15], or the string test [16] may all be used to retrieve pulmonary secretions from patients unable to provide a sputum sample but may cause logistical, cost, or biosafety challenges [17,18]. Excretion of tubercle bacilli through the kidneys and demonstrated in the urine of active TB patients was confirmed by studies carried out in HIV- positive cases and HIV– negative cases [19]. This study showed that urine could be used as an adjunct specimen due to the convenience and non-invasive nature of the collection.
Even though Ethiopia harbors the majority of TB in HIV cases, there are no documented data showing use of alternative specimen that could scale up detection of Mtb in PTB/HIV coinfected patients who couldn't produce sputum. Therefore, this study was aimed to evaluate the utility of urine as a clinical specimen for diagnosing PTB in people living with HIV, using culture, smear, and PCR methods.
2. Methods
2.1. Study degnin and population
A health institutional based cross-sectional study, between December 2013 and July 2014, was conducted on 143 TB/HIV coinfection who attended the three public health facilities (Teklehaymanot Health Center, Zewuditu Memorial Hospital and Police Referral Hospital) in Addis Ababa, Ethiopia. Study participants were enrolled. HIV seropositive ART naïve PTB suspected individuals were the target study groups. Patients taking anti-tuberculosis treatment, Isoniazid prevention therapy, suspected to have extra pulmonary TB and those who refused were excluded from the study. The study was approved by the Institutional Ethical Review Board and Research Committee of Microbiology, Immunology and Parasitology, Addis Ababa University. Records of patients were manipulated only by researchers. Each patient was taught to provide paired morning sputum and urine for smear microscopy, culture, and RD9-PCR. The Samples were kept at 4 °C and transported to the Aklilu Lemma Institute of Pathobiology (ALIPB) TB laboratory within 4 h of collected and processed for concentrated Ziehl—Nielsen, culture, and PCR. Positive results were conveyed to nurses and doctors for further management.
2.2. Bacteriological procedure
2.2.1. Culture
After an early morning urine sample (50 ml) was collected simultaneously from the patients and controls for three consecutive days, and all three samples were then pooled and processed on the third day. The pooled urine specimens from each patient were centrifuged at 3000 g for 20 min. The resulting pellet was decontaminated with an equal amount of 4% NaOH. After incubation for 15 min, the suspension was neutralized with phosphate-buffered saline (PBS; pH 6.8) and again centrifuged at 10,000 rpm for 20 min [21].
After complete liquefying and mixing, sputum specimens was digested and decontaminated by the N-acetyl-l-cysteine-NaOH method and centrifuged for 15 min at 3000 g [20]. The pellets of decontaminated sputum and urine specimens were resuspended in PBS; smears were made for Ziehl—Neelsen staining and 0.1 ml was inoculated on Lowenstein Jensen slants for culture isolation. The combined bacteriological methods (culture and smear microscopy) were considered as a reference standard. Isolates from the positive cultures were preserved with freezing media and at the same time heat killed in water bath at 80°C for 1 h The frozen and heat killed isolates were stored at −20 °C for further molecular identification as described below.
2.2.2. DNA isolation and PCR
Fifty milliliter of urine specimens was centrifuged at 3000 g for 20 min; the supernatant was removed, and the pellet was suspended in 2 ml of 4%NaOH. After incubation for 15 min, 40 ml of phosphate buffered saline (PBS) was added and again centrifuged at 3000 g for 20 min. The pellets were resuspended in 1 ml of PBS, and aliquots of 100 µl were stored at −80 °C for analysis [21]. Two hundred and fifty microliter urine or 250 μl sputum sample was separately mixed with 500 μl 1 × TE buffer (TrisEDTA) and centrifuge for 20 min at 1200 g. The pellets were re-suspended in TE buffer, and 50 μl of 10 mg/ml lysozyme was added, mixed well and incubated for 1 h at 37 °C. Seventy micro-liter sodium dedocylsulphate (Sigma, St. Louis, Mo.) with concentration of 2% and 6 μl of 10 mg/ml proteinase K (VWR international Ltd., poole, BH151TD, England) were then added, mixed, and incubated for 10 min at 65 °C. Afterwards, 100 μl of 5 M NaCl was added and vortexed and following the addition of 80 μl of pre-warmed cetyltrimethyl ammonium bromide (CTAB) /NaCl (Sigma, St. Louis, MO) in pure water, and the mixture was incubated at 65 °C for 10 min. Approximately equal volume 700–800 of readymade phenol: chloroform: isoamyl alcohol (VWR international Ltd., poole, BH151TD, England) in proportion of 25:24:1 was added, after vortexing for at least 10 s and centrifuging for 10 min at 12,000 rpm. The resultant upper phase was transferred to a clean tube with 0.6 vol. of isopropanol and mixed gently. The tubes were then moved slowly upside down to precipitate the nucleic acid and incubated at −20 °C overnight. Spun in a Microfuge for 15 min at 12,000 rpm, the precipitate was washed by 70% cold ethanol to remove CTAB/NaCl and the supernatant was removed. The pellet was permitted to air dry for 15 min and above. Finally, it was re-suspended in 1 × TE buffer (Sigma, St. Louis, MO) solution (from 20 μ to 50 μ) based on the size of the pellet for RD 9 PCR amplification. Positive and negative controls were run in the whole procedures. The genomes of the isolates were analyzed by PCR for the presence or the absence of regions of difference (RD 9) originally described as being deleted in the genomes of BCG isolates relative to the sequence of M. tuberculosis H37Rv [22]. A multi primer PCR assay with three primers was used to detect RD 9 [20]. The internal control known M. tuberculosis (MTB) was included in every PCR in order to check for the presence of PCR inhibitors while Qiagen water was used as negative control. The result was interpreted as M. tuberculosis (RD9 present) when a band of 396 bp was observed comparing to commercially available ladder, divided by 100 bp.
2.3. Statistical analysis
All data were entered into Epi Data version 3.1 and exported to SPSS software version 16.0 for analysis. Chi-square test (χ2) and kappa value were used for urine specimen versus sputum specimen, and for method evaluation respectively. The sensitivity, specificity, negative and positive predictive were determined for microscopic examination of urine and bacteriological culture of urine by considering sputum culture as a gold standard.
Overall workflow is indicated in Fig. 1
Fig. 1.
Overall workflow.
3. Results
3.1. Socio-demographic characteristic of the study participants
A total of 143 eligible study participants were included. However, only 117 participants gave both urine and sputum samples. Twenty-six of the study participants gave only a urine sample. The participants' age ranges from 19 to 61 years with a mean of 34.5 ± 8.89. The majority of the participants (60.1%) were married and 19.6% of them came from a rural area (Table 1).
Table 1.
Socio-demographic characteristic of the study participants in Addis Ababa, Ethiopia (N = 143).
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Age | 18–27 | 21 | 14.7% |
| 28–37 | 76 | 53.1% | |
| 38–47 | 28 | 19.6% | |
| 48–57 | 13 | 9.1% | |
| >57 | 5 | 3.5% | |
| Gender | Male | 55 | 38.5% |
| Female | 88 | 61.5% | |
| Residence | Urban | 115 | 80.4% |
| Rural | 28 | 19.6% | |
| Marital status | Single | 28 | 19.6% |
| Married | 86 | 60.1% | |
| Divorced | 12 | 8.4% | |
| Widow | 17 | 11.9% | |
| Occupation | Employed | 64 | 44.8% |
| Housewife | 30 | 21% | |
| Daily labored | 32 | 22.4% | |
| Merchant | 10 | 7% | |
| Farmer | 7 | 4.8% | |
| Educational status | Non educated | 18 | 12.6% |
| Elementary school(1–8) | 35 | 24.5% | |
| High school(9–12) | 78 | 54.5% | |
| Higher education (diploma/degree) | 12 | 8.4% |
3.2. Bacteriological finding in the sputum and urine sample
Sputum and urine samples from 117 HIV positive suspected PTB patients were subjected to smear, culture and PCR examinations. Out of 45 (31.5%) PTB cases detected, 30 (66.7%) were from urine specimens and 40 (88.9%) from sputum specimens. Of these, 17 (14.5%) were urine culture positive on L–J, 7 (6%) were urine smear-positive and 29 (24.8%) were urine RD9- based PCR positive, while of the sputum sample, 11 (9.4%) were positive by ZN staining, 33 (28.2%) were culture positive and the PCR gave 40 (34.2%) positive. As expected the detection rate of PCR was higher than the culture and smear which is statistically significant (χ2 = 61.7, p = 0.001) (Table 2).
Table 2.
Mycobacterium detection rates of various diagnostic methods applied to urinary and pulmonary specimens from pulmonary tuberculosis suspected HIV infected patients.
| Specimen type | sputum (n = 117) | Urine (n = 117) | Both sputum and urine |
|---|---|---|---|
| L–J culture | |||
| Percentage of culture-positive | 28.2% (33/117) | 14.5%(17/117) | 31.6%(37/117) |
| Smear Microscopy | |||
| Percentage of smear-positive | 9.4% (11/117) | 6% (7/117) | 13.7% (16/117) |
| PCR | |||
| Percentage of PCR positive | 34.2% (40/117) | 24.8% (24/117) | 37.6% (44/117) |
3.3. Bacteriological finding in the urine of sputum scarce patients
Out of 26 patients who failed to produce sputum sample, 9 (34.6%) were positive with urine samples. Of which 1 (3.8%) was smear positive; 3 (11.5%) were culture positive and 9 (34.6%) were PCR positive. All urine smear and culture positive samples were positive by RD9-based PCR
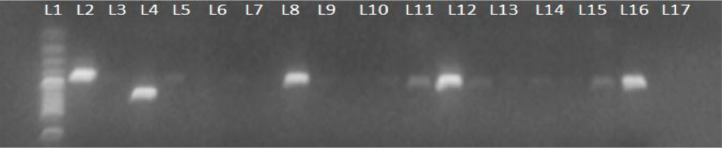
DNA extracted pellet from urine was amplified with RD9 primer and produced band at 396 compared with standard 100 bp ladder and known positive control (Fig. 2)
Fig. 2.
Detection of Mbt RD9 using primers for short and large amplicons.
3.4. Mycobacterium detection rate in urine specimens from pulmonary tuberculosis
From 117 urine sample, 17 (14.5%) were urine culture-positive. However, the culture isolation rate was significant (54.5%) (χ2 = 15.5, p < 0.001) when urine was collected from patients who were sputum smear and culture positive as compared to those patients whose sputum samples were smear negative, culture negative, PCR positive (75%). The detection rate of Mtb increased by 3.4% [from 28.2% to 31.6%] when urine culture conducted in parallel with sputum culture. Overall 30 of 45 (66.7%) sputum confirmed PTB patients were found RD9-based PCR positive. Urine RD9-based PCR positivity could reach as high as 100% in sputum smear-positive cases. The application of RD9-based PCR for urine samples had a highest diagnostic yield in sputum smear and/or culture confirmed patients as compared with smear and /or culture unconfirmed patients (χ2 = 37.6, p < 0.001) (Table 3).
Table 3.
Mycobacteria detection rate of various in vitro diagnostic methods applied to urine specimen from PTB patients.
| Detection rate of Mtb from suspected PTB cases (n = 117) (and result of sputum sample) | Detection rate of mycobacteria in urine | ||
|---|---|---|---|
| Microscopy | L–J culture | PCR | |
| Smear, culture and PCR positive (n = 11) | 5 (45.5%) | 6 (54.5%) | 11 (100%) |
| Smear negative, culture and PCR positive (n = 22) | 2 (7.7%) | 9 (34.5%) | 14 (53.8%) |
| Smear negative, culture negative and PCR positive (n= 7) | 0 | 4 (50%) | 6 (75%) |
L–J, Lewiston Jensen media; PCR, polymerase chain reaction.
3.5. Comparison of urine and sputum in diagnosis of PTB
The comparison of both urine and sputum cultures showed that the sputum culture detected more mycobacterial isolates [33 (28.2%)] than urine culture [17 (14.5%)]. Of the 84 sputum culture-negative cases, four (4.8%) where urine culture-positive. Thirteen of 33 (39.4%) sputum culture positive samples were positive by urine culture, and 4 of the remaining 84 (4.8%) sample has concordant result between urine culture as compare with sputum culture with 39.4% sensitivity and 89.3% specificity. Twenty four of 33 (72.7%) sputum cultures positive samples were positive by urine RD9-based PCR and 9 of 84 (10.7%) patients were positive by urine RD9-based PCR with sensitivity (72.7%) and specificity (89.3%). The measures of agreement between urine smear, culture and RD9-based PCR as compare to sputum culture were 0.28, 0.46, and 0.59 (kappa), respectively. The agreement is considered to be fair, moderate and good respectively (Table 4).
Table 4.
Comparison of urine and sputum specimen for the diagnosis of active PTB in people living with HIV by using sputum culture as old standard, in Addis Ababa, Ethiopia.
| Urine sample | Sputum culture positive | Sensitivity | Specificity | PPV | NPV | Kappa value | |||
|---|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Total | |||||||
| Smear | Positive | 7 | 0 | 7 | 21.2% | 100% | 100% | 76.4% | 0.279 |
| Negative | 26 | 84 | 110 | ||||||
| Total | 33 | 84 | 117 | ||||||
| Culture | Positive | 13 | 4 | 17 | 39.4% | 95.2% | 76.5% | 80% | 0.406 |
| Negative | 20 | 80 | 100 | ||||||
| Total | 33 | 84 | 117 | ||||||
| PCR | Positive | 24 | 9 | 33 | 72.7% | 89.3% | 72.7% | 89.3% | 0.620 |
| Negative | 9 | 75 | 84 | ||||||
| Total | 33 | 84 | 117 | ||||||
PPV, positive predicted value; NPV, negative predicted value.
4. Discussion
In the 21st century, utilization of urine as a clinical specimen for the diagnosis of many diseases gets attention, especially with the emergence of HIV and future hope for those who cannot produce sputum or smear negatives. The bacteriologically confirmed pulmonary TB among HIV-infected patients from sputum was 33 (28.2%), of which 24 (72.7%) were urine PCR positive. It showed lower sensitivity and specificity (72.7% and 95.3%, respectively) as compared with sputum cultures. The obtained results were lower than other studies [21,[23], [24], [25]]. Of 33 PTB patients identified, 13 (39.4%) were also urine culture positive. Although urine culture for PTB detection was not good enough like sputum culture sputum, the urine culture positivity of four participants (4.8%) who were sputum culture negative highlighted that, if urine culture is carried out in parallel with sputum culture it increase the number of positive TB cases of people living with HIV. Our finding was slightly lower than a study by Gopinath [21], in which MTC successfully grew in 9.7% of urine sample from 81 patients suspected to be suffering PTB using the conventional solid culturing methods but similar to the finding of Challu et al. in Bangalore [26]. Urine culture has increased the detection of Mtb by 3.4% [from 28.2% to 31.6%] that is consistent with the research conducted in India and elsewhere [21,[26], [27], [28]] where the detection rate was increased by 4.9% [from 56.8% to 61.7%]. Besides increasing the chance of Mtb detection, urine specimen minimizes the use of more invasive techniques for collecting samples, such as BAL and gastric lavage and reduces the aerosol [21,29]. The higher detection observed by this group (compared with our results) may be as a result of a larger volume of urine and improved decontamination/ concentration techniques could improve the sensitivity of urine culture. However, in this study, we used chlorhexidine method as previous study [21,23,25,28,29]. The sensitivity of 45.5% is too low to suggest that urine specimen should replace sputum specimens for TB diagnosis, and is higher than the sensitivity reported in other studies [22,30].
The data presented in our study could strengthen previous reports indicating urine as an alternative specimen for diagnosis of pulmonary tuberculosis in people living with HIV. WHO put strategies to reduce TB disease by recommending modern molecular techniques, but in areas with high HIV prevalence getting specimen for the diagnosis of PTB in coinfected individuals is the other challenge in TB diagnosis [31]. An alternative to sputum specimens are BAL and gastric lavage fluids [21,32], but collection of these specimens is often hurting and tongue-tied which makes these specimens put in insignificant advantage [32]. Thus when the easily available urine specimen subjected to culture and PCR, the detection rate of Mtb in patients those who couldn't produce sputum (cough without expectoration) was 34.6%. This is promising result for HIV/TB co-infected persons although a study done in India reported no urine sample from a sputum-scarce patient was smear- or L–J culture-positive [21].
Excretion of M. tuberculosis through urine was confirmed by several recent studies using modern diagnostic tools [23,25,27,29]. In the present study, detection of Mtb from urine showed 35.1% of PTB cases excreted M. tuberculosis in their urine. This finding was slightly higher than the study conducted in India, where the excretion rate was (26.1%) [21,33]. This difference might be due to a difference in the study population. When the easily available urine specimen supported by PCR and culture, it can identify 91% of PTB cases [21,26,27]. This finding may lead us using urine as a diagnostic aid in immunosuppressed patients has a potential to improve the detection of Mtb.
5. Conclusion
The combination of urine and sputum had higher accuracy than either sample alone. Surprisingly, when we use urine as a clinical specimen for the diagnosis of PTB, we were able to detect an additional 10.7% of PTB cases whe PCR used as diagnotic test. These findings are highly significant and encouraging when urine culture also improve the mycobacteria detection rate. Sputum should remain the diagnostic specimen of choice for PTB; however, urine should not be neglected, particularly valuable in patients unable to produce sputum specimens as it could be used as an alternative specimen.
We recommend that when sputum specimens have failed to confirm the diagnosis, a urine sample could be used for culture, PCR tests and also for other simple tests that could be developed as point-of-care.
Declaration
Ethics statement
The study has been approved by the Departmental Ethical Review and Research Committee (DERC) of the department of Medical Microbiology, Immunology and Parasitology (DMIP) (Protocol No. 1/T/2013, On meeting No. 23rd) of Addis Ababa University. Written informed consent was obtained from all study participants before the interview and sample collection.
Consent for publication
Not applicable.
Availability of data and material
All important datasets that support the conclusions of this article are included within the article.
Funding
The work was a M.Sc. research of the first author and it was funded by the Medical Microbiology, Immunology and Parasilogy Department, College of Health Science of the Addis Ababa University.
CRediT authorship contribution statement
Alemu Chemeda: Data curation, Formal analysis, Writing - original draft. Tamrat Abebe: Writing - original draft. Gobena Ameni: Funding acquisition, Supervision, Project administration. Adane Worku: Investigation, Methodology. Adane Mihret: Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
We acknowledge the technical support provided by police referral Hospital, Zewuditu Memorial Hospital, and the Teklehaymanot Health Center. Our special thanks and appreciation also goes to all the study participants who voluntarily participate in this study. Lastly but not least, we also thank Aklilu Lemma Research Institution of Pathobiology for their consistent support with reagents and other materials during the project work.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jctube.2019.100125.
Contributor Information
Alemu Chemeda, Email: alemuchemedaifa@yahoo.com.
Tamrat Abebe, Email: tamrat.abebe@aau.edu.et.
Appendix. Supplementary materials
References
- 1.Ahmed Yassin M. HIV and tuberculosis coinfection in the southern region of Ethiopia: a prospective epidemiological study. Scand J Infect Dis. 2004;36(9):670–673. doi: 10.1080/00365540410020848. [DOI] [PubMed] [Google Scholar]
- 2.Demissie M., Lindtjørn B., Tegbaru B. Human immunodeficiency virus (HIV) infection in tuberculosis patients in Addis Ababa. Ethiopian J Health Dev. 2000;14(3) [Google Scholar]
- 3.Gellete A., Kebede D., Berhane Y. Tuberculosis and HIV infection in southern Ethiopia. Ethiopian J Health Dev (EJHD) 2017;11(1) [Google Scholar]
- 4.Kassu A. Coinfection and clinical manifestations of tuberculosis in human immunodeficiency virus-infected and-uninfected adults at a teaching hospital, northwest Ethiopia. J Microbiol Immunol Infect. 2007;40(2):116. [PubMed] [Google Scholar]
- 5.Mitike G., Kebede D., Yeneneh H. HIV infection and antituberculosis drug resistance among pulmonary tuberculosis patients in Harar Tuberculosis Centre, Ethiopia. East Afr Med J. 1997;74(3):154–157. [PubMed] [Google Scholar]
- 6.Harries A.D. Deaths from tuberculosis in sub-Saharan african countries with a high prevalence of HIV-1. Lancet. 2001;357:1519–1523. doi: 10.1016/S0140-6736(00)04639-0. [DOI] [PubMed] [Google Scholar]
- 7.WHO, Global Tuberculosis report . 2014. , in WHO Report. [Google Scholar]
- 8.Affusim C.C., Kesieme E., Abah V.O. The pattern of presentation and prevalence of tuberculosis in HIV-seropositive patients seen at Benin city, Nigeria. Int Sch Res Notices. 2012;2012:1–6. [Google Scholar]
- 9.Federal Ministry of Health (FMOH) 2007. HIV Prevention and Control Office: Single Point HIV Prevalence Estimate. . Addis Ababa, Ethiopia. [Google Scholar]
- 10.Batungwanayo J. Impact of human immunodeficiency virus infection on clinical and radiographic presentation of PTB in Kigali, Rwanda. Am Rev Respir Dis. 1992;146:53–56. doi: 10.1164/ajrccm/146.1.53. [DOI] [PubMed] [Google Scholar]
- 11.Hartung T.K. Suspected PTB in rural South Africa-sputum induction as a simple diagnostic tool? S Afr Med J. 2002;92:455–458. [PubMed] [Google Scholar]
- 12.Banada P.P. A novel sample processing method for rapid detection of tuberculosis in the stool of pediatric patients using the Xpert MTB/RIF Assay. PLoS ONE. 2016;11(3) doi: 10.1371/journal.pone.0151980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conde M.B. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am J Respir Crit Care Med. 2003;167:723–725. doi: 10.1164/rccm.2111019. [DOI] [PubMed] [Google Scholar]
- 14.Franchi L.M. Detection of Mycobacterium tuberculosis in nasopharyngeal aspirate samples in children. Lancet. 1998;352:1681–1682. doi: 10.1016/s0140-6736(05)61454-7. [DOI] [PubMed] [Google Scholar]
- 15.Maartens G. Advances in adult pulmonary tuberculosis. Curr Opin Pulm Med. 2002;8:173–177. doi: 10.1097/00063198-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Moore D. Appropriate technology in tuberculosis diagnostics. Lancet. 2005;365:1541–1542. doi: 10.1016/S0140-6736(05)66453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Getahun H. Development of a standardized screening rule for tuberculosis in people livign with HIV in resource-contrained settings: individual participant data meta-analysis of observational studies. PLoS Med. 2011;8:1371. doi: 10.1371/journal.pmed.1000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DiNardo A.R. Use of string test and stool specimens to diagnose pulmonary tuberculosis. Int J Infect Dis. 2015;41:50–52. doi: 10.1016/j.ijid.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aceti A. Identification of HIV patients with active pulmonary tuberculosis using urine based polymerase chain reaction assay. Thorax. 1999;54:145–146. doi: 10.1136/thx.54.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kubica G. Sputum digestion and decontamination with N-acetyl-l-cysteine—sodium hydroxide for culture of mycobacteria. Am Rev Respir Dis. 1963;87(5):775–779. doi: 10.1164/arrd.1963.87.5.775. [DOI] [PubMed] [Google Scholar]
- 21.Gopinath K., Singh S. Urine as an adjunct specimen for the diagnosis of active pulmonary tuberculosis. Int J Infect Dis. 2009;13(3):374–379. doi: 10.1016/j.ijid.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 22.Parsons L.M. Rapid and simple approach for identification of Mycobacterium tuberculosis complex isolates by PCR-based genomic deletion analysis. J Clin Microbiol. 2002;40(7):2339–2345. doi: 10.1128/JCM.40.7.2339-2345.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heydari A.A., Danesh M.R.M., Ghazvini K. Urine PCR evaluation to diagnose pulmonary tuberculosis. Jundishapur J Microbiol. 2014;7(3) doi: 10.5812/jjm.9311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kafwabulula M. Evaluation of PCR-based methods for the diagnosis of tuberculosis by identification of mycobacterial DNA in urine samples. Int J Tuber Lung Dis. 2002;6(8):732–737. [PubMed] [Google Scholar]
- 25.Torrea G. PCR-based detection of the Mycobacterium tuberculosis complex in urine of HIV-infected and uninfected pulmonary and extrapulmonary tuberculosis patients in Burkina Faso. J Med Microbiol. 2005;54(1):39–44. doi: 10.1099/jmm.0.45688-0. [DOI] [PubMed] [Google Scholar]
- 26.Challu V.K. Recovery of tubercle bacilli from urine of pulmonary tuberculosis patients and its comparison with the corresponding sputum isolates. Indian J TB. 1989;36:107–111. [Google Scholar]
- 27.Bentz R.R. The incidence of urine cultures positive for Mycobacterium tuberculosis in a general tuberculosis patient population 1, 2. Am Rev Respir Dis. 1975;(5):647–650. doi: 10.1164/arrd.1975.111.5.647. [DOI] [PubMed] [Google Scholar]
- 28.Sechi L.A. Detection of Mycobacterium tuberculosis by PCR analysis of urine and other clinical samples from AIDS and non-HIV-infected patients. Mol Cell Probes. 1997;11(4):281–285. doi: 10.1006/mcpr.1997.0119. [DOI] [PubMed] [Google Scholar]
- 29.Rebollo M.J. Blood and urine samples as useful sources for the direct detection of tuberculosis by polymerase chain reaction. Diagn Microbiol Infect Dis. 2006;56(2):141–146. doi: 10.1016/j.diagmicrobio.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 30.Noordhoek G.T. Sensitivity and specificity of PCR for detection of Mycobacterium tuberculosis: a blind comparison study among seven laboratories. J Clin Microbiol. 1994;32(2):277–284. doi: 10.1128/jcm.32.2.277-284.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koole O. Evaluation of the 2007 WHO guideline to improve the diagnosis of tuberculosis in ambulatory HIV-positive adults. PLoS ONE. 2011;6(4):e18502. doi: 10.1371/journal.pone.0018502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dickson S.J. Comparison of bronchoscopy and gastric washings in the investigation of smear-negative pulmonary tuberculosis. Clin Infect Dis. 2003;37(12):1649–1653. doi: 10.1086/379716. [DOI] [PubMed] [Google Scholar]
- 33.Cannas A. Mycobacterium tuberculosis DNA detection in soluble fraction of urine from pulmonary tuberculosis patients. Int J Tuber Lung Dis. 2008;12(2):146–151. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All important datasets that support the conclusions of this article are included within the article.