Abstract
Background:
Acromioclavicular (AC) joint separation is a common injury. The anatomic coracoclavicular ligament reconstruction (ACCR) technique is a viable treatment option, designed to restore the native joint anatomy.
Purpose:
To evaluate the clinical and radiographic outcomes of patients undergoing ACCR for the treatment of type III and V AC joint injuries with a minimum 2-year follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective chart review was performed on prospectively collected data. Patients who underwent ACCR for type III or V AC joint injuries between January 2003 and December 2015 were analyzed. Clinical outcome measures included the American Shoulder and Elbow Surgeons (ASES) score, Rowe score, Simple Shoulder Test (SST), and Constant-Murley (CM) score. To determine the clinical relevance of the ASES score, the minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptomatic state (PASS) were used. The pre- and postoperative coracoclavicular distance (CCD) and side-to-side difference in the CCD were measured for radiographic analysis.
Results:
A total of 43 patients (22 acute, 21 chronic) were included in the study. The mean patient age was 43.4 ± 11.4 years, with a mean follow-up of 3.4 years (range, 2.0-7.5 years). With regard to the ASES score, 92% of patients achieved the MCID, 81% achieved the SCB, and 49% reached or exceeded the PASS. There was no significant difference when stratifying by type (III vs V) or chronicity (acute vs chronic) of injury (both P > .05). The Rowe score improved from 66.6 ± 15.9 preoperatively to 88.6 ± 12.3 postoperatively, the CM score from 61.6 ± 18.8 to 87.4 ± 15.1, and the SST score from 6.2 ± 3.6 to 9.4 ± 3.7 (all P < .001). The postoperative side-to-side difference in the CCD was 3.1 ± 2.7 mm, with type III injuries (2.4 ± 1.9 mm) showing significantly lower measurements compared with type V (4.2 ± 3.4 mm) (P = .02). No significant trend was found between joint reduction and the improvement in clinical outcomes (P > .05).
Conclusion:
Patients undergoing ACCR for acute and chronic type III and V AC joint injuries maintained significant improvement in clinical and radiographic outcomes at a minimum 2-year follow-up. Additionally, 81% of patients reached the SCB after surgical reconstruction.
Keywords: anatomic coracoclavicular ligament reconstruction, ACCR, AC joint, acromioclavicular joint injury, shoulder surgery, clinical outcomes
Acromioclavicular (AC) joint injuries account for the vast majority of shoulder injuries, especially in athletes who engage in contact sports.3,5,13,22,28,29 Although the incidence of high-grade AC joint injuries requiring surgery is low, indications for the nonsurgical versus surgical treatment of type III and V injuries produce controversy.3,13,22,26 This disagreement has encouraged the development of multiple surgical techniques being proposed in the literature and may reflect a general dissatisfaction with treatment options and outcomes.3,5,6,13,26
Mazzocca et al23 described an anatomic coracoclavicular ligament reconstruction (ACCR) technique, utilizing a semitendinosus allograft to replicate the coracoclavicular ligament in its anatomic location. Biomechanically, along with other anatomic reconstruction techniques, this has been shown to be more effective in restoring native AC joint properties when compared with coracoacromial ligament transfer.8,15,20,24 More importantly, using these anatomic techniques may lead to more favorable clinical and radiographic outcomes.15,17,24,31,38 This technique has shown high subjective satisfaction rates among patients with a significant reduction in pain levels and improvement in shoulder function in the short term.6 These findings are consistent with other studies reporting on the short-term to midterm clinical and radiographic outcomes of ACCR using free tendon grafts.17,25,29,31,32,38 However, these studies were limited to a small patient population and short duration of follow-up.
Although this preliminary work is promising, longer term clinical and radiographic outcomes of patients undergoing ACCR have not yet been investigated. In addition, correlation between the maintenance of reduction and clinical outcomes is still poorly understood. The purpose of this study was to evaluate the clinical and radiographic outcomes of patients undergoing ACCR for the treatment of acute and chronic type III or V AC joint injuries with a minimum of 2-year follow-up. We hypothesized that patients undergoing ACCR would have significant clinical improvement with maintenance of radiographic reduction at final follow-up.
Methods
Patient Selection
A retrospective chart review was performed on patient data collected prospectively from an institutional shoulder registry. All patients were recruited from a single shoulder fellowship–trained surgeon’s practice (A.D.M.) between January 2003 and December 2015. Institutional review board approval was obtained before the initiation of the study. Patients eligible for study inclusion were those aged ≥18 years with an acute (defined as <6 months of nonoperative treatment) or chronic type III or V AC joint injury (defined by the Rockwood classification3) who underwent an ACCR procedure using a tendon allograft. All patients underwent a minimum of 1 month of nonoperative management, which included physical therapy. Those who were treated acutely included patients who failed to improve after a trial of nonoperative management or requested fixation based on a complete discussion of the risks and benefits of delayed treatment. A time of 6 months was chosen as chronic due to the 1-month nonoperative management period, which all patients received as the standard of care. Although there is some debate in the literature regarding the exact definition of chronicity in AC joint injuries,12 the trial of nonoperative management makes defining acute as 3 weeks unrealistic in this population. Exclusion criteria included patients with revision surgery; type I, II, IV, and VI injuries; and vulnerable populations (eg, prisoners, pregnant women, hospital employees).
Surgical Technique
Each patient underwent ACCR using a tendon allograft with interference screw fixation in the clavicle as previously described.6,23 With the patient in the beach-chair position, an incision was made starting at the posterior edge of the clavicle 3.5 cm medial to the AC joint and extending inferiorly toward the coracoid process. Dissection was performed to the deltotrapezial fascia with electrocautery. The fascia was elevated off the clavicle by creating full-thickness flaps. All soft tissues preventing proper joint reduction were resected, and a trial reduction was performed.6,23 Effort was made not to excise or damage the distal clavicle.
Once the clavicle was visualized, 2 bone tunnels were drilled into the clavicle according to the anatomic locations of the coracoclavicular ligaments. First, a 5-mm posteromedial tunnel was made, positioned 4.5 cm medial to the AC joint according to the anatomic insertion of the conoid ligament. Subsequently, a second anterolateral 5-mm tunnel was made, positioned 20 to 25 mm lateral to the center of the conoid tunnel, mimicking the trapezoid ligament. A minimum distance of 20 to 25 mm was maintained between tunnels, and the trapezoid tunnel was distanced at least 15 mm medially from the end of the clavicle to minimize susceptibility to clavicle fractures.6,23
Grafts were prepared from either semitendinosus or peroneus longus tendons. Under direct visualization, the graft was passed beneath the coracoid process from medial to lateral using a curved suture-passing device. Subsequently, the 2 limbs of the graft were crossed before being shuttled through the bone tunnels on the inferior aspect of the clavicle. Using the Hewson suture passer, the graft was first shuttled through the posteromedial tunnel. To remove any remaining slack, the graft was cyclically loaded by pulling it up on both ends. The lateral limb (trapezoid) graft was made 2 cm longer than the medial limb to re-create the AC joint capsule ligament.6,23 High-strength nonabsorbable suture was used to take the excess lateral limb and suture it to the posterior tissue on the acromial side, using a horizontal mattress technique.23 Any excess graft of the lateral limb was sutured to the trapezial fascia to re-create the posterior AC ligament.23
After visual and radiographic confirmation of AC joint reduction, graft limbs were secured sequentially (medial limb, then lateral limb) with interference screws while maintaining accurate reduction. Fixation was performed using interference screws (5.5 × 8–mm PEEK screw; Arthrex) placed along the anterior aspect of each tunnel, while tension on the graft limb was applied. Finally, graft limbs were secured onto the superior aspect of the clavicle, and the longer limb was used to reinforce the superior and posterior parts of the repaired AC capsule. Closure of the deltotrapezial fascia was performed with interrupted nonabsorbable sutures, with a running subcuticular closure performed on the epidermal layer.6,23
Postoperative Rehabilitation
Postoperative rehabilitation consisted of wearing a shoulder unloader brace (Lerman Shoulder Orthosis; DonJoy) for 6 weeks. This allowed for unloading of the shoulder to not apply stress to the AC joint reconstruction site. After 2 months postoperatively, patients were allowed to initiate upright range of motion exercises. If the patient was pain-free, strengthening exercises were implemented after 12 weeks, focusing on scapular stabilizers to decrease AC joint loads. Weight training was incorporated within 3 to 5 months, and contact athletic activity began as early as 6 months after surgery.6
Clinical Analysis
The primary outcome measure was the American Shoulder and Elbow Surgeons (ASES) score. Secondary clinical outcome measures included the Rowe score, the Simple Shoulder Test (SST), and the Constant-Murley (CM) score.7,21,30 These scores were collected preoperatively and at a minimum of 2 years postoperatively. The Single Assessment Numeric Evaluation (SANE) score was obtained at only the final postoperative visit.37 Previous studies have confirmed these scores in terms of reliability, validity, and responsiveness.2,14,33,37 To determine the clinical relevance of the ASES score, the minimal clinically important difference (MCID), the substantial clinical benefit (SCB), and the patient acceptable symptomatic state (PASS) were used.16 The MCID and SCB are used to quantify the clinical significance of a change in scores on an outcome measure.16 The PASS is used as a threshold score associated with patient satisfaction.16 While these metrics have not been examined in patients with AC joint injuries, they have been developed in shoulder arthroplasty36 and rotator cuff tear9 populations. Because current metrics are not available for patients with AC joint injuries, we utilized minimum changes from rotator cuff tears.9 These included an 11-point change for the MCID, a 17.5-point change for the SCB, and a final ASES score of 86.7 for the PASS.
Radiographic Analysis
For radiographic analysis of vertical displacement, the pre- and postoperative coracoclavicular distances (CCD; in mm) were measured on unweighted anterior-posterior bilateral Zanca view radiography as the distance between the tip of the coracoid and the inferior cortex of the clavicle.6,39,41 The side-to-side difference (in mm) in the CCD was obtained in relation to the noninjured contralateral side.
Statistical Analysis
Descriptive statistics including the mean and standard deviation for continuous variables, and the frequency and proportion for categorical variables were calculated to characterize the study groups. The change in the pre- to postoperative ASES score was used to determine which patients crossed the MCID and SCB thresholds. The final postoperative ASES score was used to determine whether patients met criteria for the PASS. Patients were then grouped according to injury severity (type III vs V) and chronicity (acute vs chronic). Differences in the proportion of patients meeting the MCID, SCB, and PASS thresholds between these groups were analyzed with the chi-square test or Fisher exact test when expected cell values were less than 5. Given the lack of adequate values for similar metrics, the mean values of the remaining outcome scores were compared. Differences in the magnitude of improvement (absolute difference between preoperatively and postoperatively) and final postoperative clinical scores and CCD were examined with an independent t test. Pearson correlation coefficients were generated to examine the relationship between postoperative clinical scores and the CCD. Results of inferential analysis are presented as 95% CIs.
Given that this was a retrospective analysis, the availability of data determined the sample size. A power analysis was performed to determine the capability of the sample size to detect a clinically meaningful difference for all patients from preoperative to postoperative MCID, SCB, and PASS thresholds for the ASES score. A sample size of 29 patients would provide 80% power to detect a 25% difference in the proportions of patients who achieved the MCID, SCB, or PASS at an alpha level of 0.05. The ASES score was the only outcome measure used for these metrics, as the Rowe score and SST have not been established for these parameters in this cohort. In addition, preoperative SANE scores were not collected in this study, so change could not be compared. The ASES score was also felt to be a better metric to use compared with the CM score, as it requires only patient subjective scoring. All analyses were performed with Stata statistical software (StataCorp).
Results
Participants
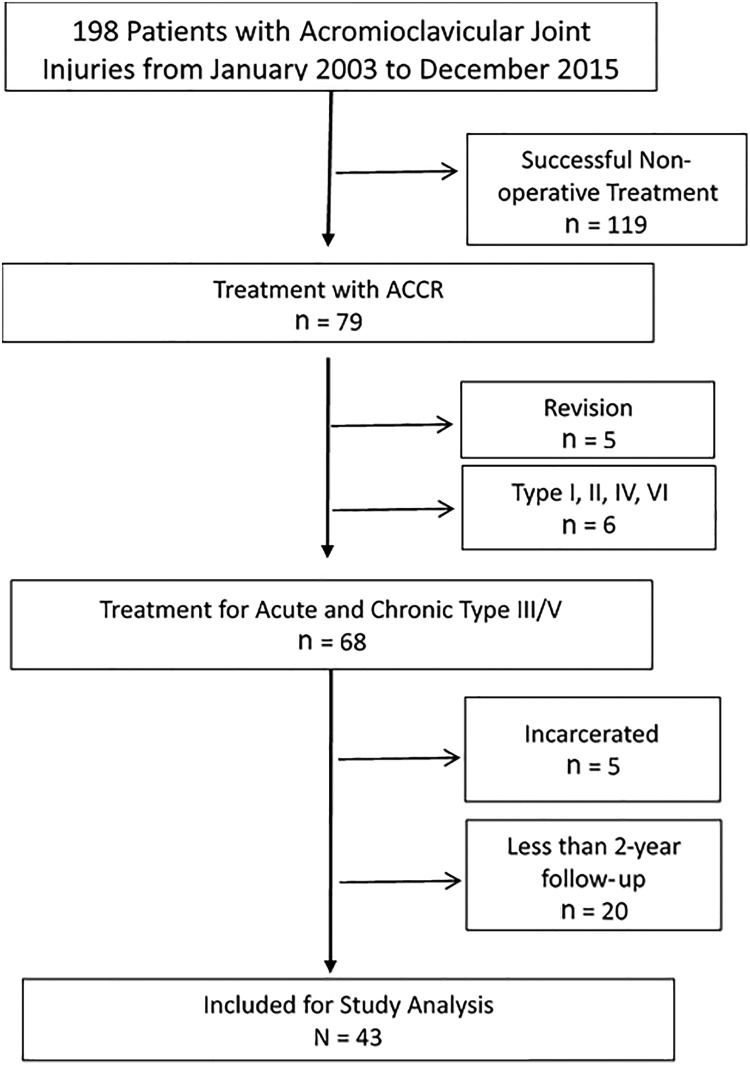
In a single surgeon’s (A.D.M.) practice, 79 patients underwent ACCR using a tendon allograft between January 2003 and December 2015. Of these patients, 43 patients (22 acute, 21 chronic) were eligible for inclusion in the study (Figure 1). The mean age of patients was 43.4 ± 11.4 years, with a mean follow-up of 3.4 years (range, 2.0-7.5 years). The median time from injury to surgery for chronic injuries was 15 months (interquartile range [IQR], 7-48 months). The median time from injury to surgery for acute injuries was 3 months (IQR, 2-5 months). The majority of patients were male (76.7%). Patient demographics are demonstrated in Table 1.
Figure 1.
Flow diagram demonstrating patients included for study analysis.
TABLE 1.
Patient Demographics (N = 43)a
| Sex | |
| Male | 33 (76.7) |
| Female | 10 (23.3) |
| Age, mean ± SD, y | 43.4 ± 11.4 |
| Follow-up, mean ± SD, y | 3.4 ± 1.2 |
| Dominant arm involved | 25 (58.1) |
| Injury pattern | |
| Acute | 22 (51.2) |
| Chronic | 21 (48.8) |
| Type III | 20 (46.5) |
| Type V | 23 (53.5) |
aData are shown as n (%) unless otherwise indicated.
Clinical Outcomes
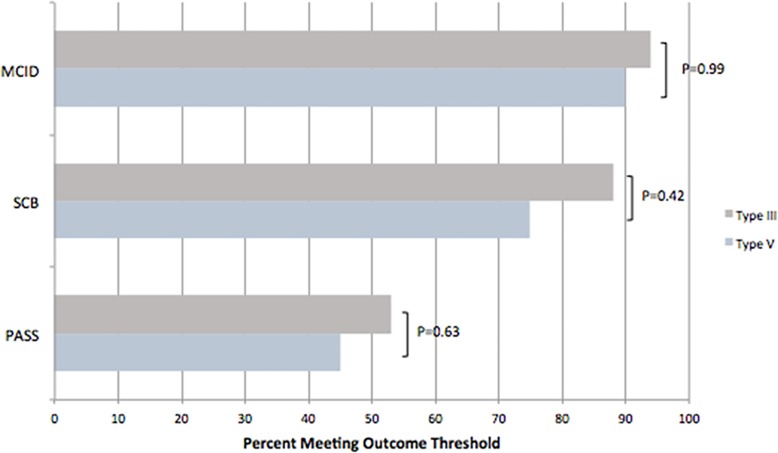
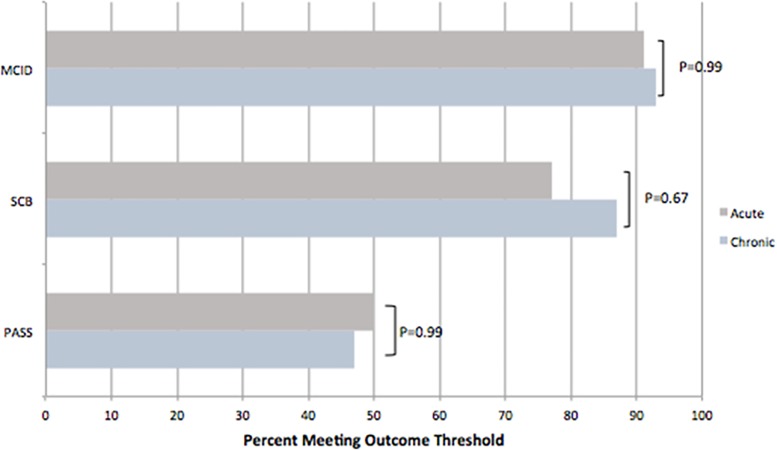
For all patients, 92% achieved the MCID, 81% met the SCB, and 49% reached or exceeded the PASS for the ASES score. When stratifying by type of injury (type III vs V), there was no statistically significant difference in the percentage of patients meeting the MCID (94% vs 90%, respectively [95% CI, –13% to 21%]), SCB (88% vs 75%, respectively [95% CI, –11% to 38%]), or PASS (53% vs 45%, respectively [95% CI, –24% to 40%]) (Figure 2). Similarly, when comparing the chronicity of injury (as defined by the parameters of the current study), there was no significant difference found in the percentage of patients meeting the MCID (91% vs 93%, respectively [95% CI, –20% to 15%]), SCB (77% vs 87%, respectively [95% CI, –34% to 15%]), or PASS (50% vs 47%, respectively [95% CI, –29% to 36%]) (Figure 3). The ASES score increased from 52.1 ± 19.9 (95% CI, 45.2-59.1) preoperatively to 82.0 ± 21.8 (95% CI, 74.4-89.6) postoperatively (P < .001).
Figure 2.
Percentage of patients with type III and V injuries who met the minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptomatic state (PASS) for the American Shoulder and Elbow Surgeons (ASES) score.
Figure 3.
Percentage of patients with acute and chronic injuries who met the minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptomatic state (PASS) for the American Shoulder and Elbow Surgeons (ASES) score.
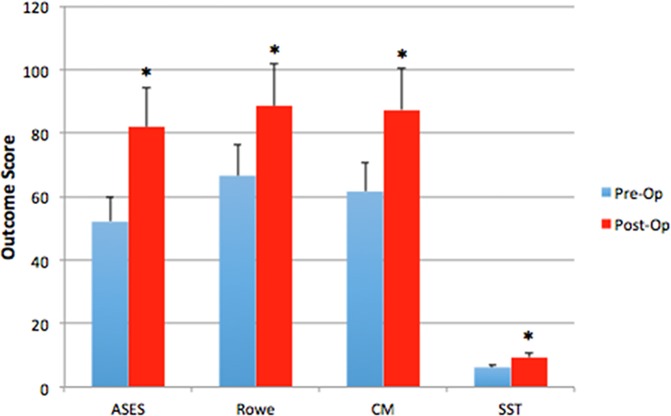
Additionally, there was a significant improvement in all secondary outcome measures from preoperatively to postoperatively. The Rowe score improved from 66.6 ± 15.9 (95% CI, 60.6-72.7) preoperatively to 88.6 ± 12.3 (95% CI, 83.9-93.2) postoperatively, the CM score from 61.6 ± 18.8 (95% CI, 54.1-69.0) preoperatively to 87.4 ± 15.1 (95% CI, 81.5-93.4) postoperatively, and the SST from 6.2 ± 3.6 (95% CI, 4.9-7.4) preoperatively to 9.4 ± 3.7 (95% CI, 8.1-10.7) postoperatively at final follow-up (all P < .001) (Figure 4). The postoperative SANE score for all patients was 85.7 ± 17.6 (95% CI, 79.6-91.9). At final follow-up, there were no significant trends in Rowe, CM, SST, and SANE scores between acute and chronic injuries (Table 2) or when comparing type III and V injuries (Table 3).
Figure 4.
Preoperative and postoperative clinical outcomes at final follow-up for all patients undergoing anatomic coracoclavicular ligament reconstruction. *Significant improvement (P < .001) when compared with preoperatively. ASES, American Shoulder and Elbow Surgeons; CM, Constant-Murley; SST, Simple Shoulder Test.
TABLE 2.
Postoperative and Change in Clinical Outcomes of Acute Versus Chronic Acromioclavicular Joint Injuriesa
| Postoperative | P Value | Change From Pre- to Postoperative | P Value | |
|---|---|---|---|---|
| Rowe | .32 | .99 | ||
| Acute | 90.9 ± 11.6 (85.0-96.9) | 21.9 ± 11.6 (16.0-27.9) | ||
| Chronic | 86.6 ± 12.6 (79.3-93.9) | 21.9 ± 14.5 (12.7-31.1) | ||
| CM | .49 | .38 | ||
| Acute | 90.4 ± 11.2 (84.5-96.4) | 28.7 ± 13.4 (21.6-35.8) | ||
| Chronic | 86.6 ± 18.1 (75.7-97.5) | 23.0 ± 19.3 (9.2-36.8) | ||
| SST | .27 | .76 | ||
| Acute | 10.3 ± 3.0 (8.7-11.9) | 3.6 ± 4.1 (1.4-5.8) | ||
| Chronic | 8.9 ± 4.0 (6.9-11.0) | 3.2 ± 3.3 (1.5-4.9) |
aData are shown as mean ± SD (95% CI). CM, Constant-Murley; SST, Simple Shoulder Test.
Table 3.
Postoperative and Change in Clinical Outcomes of Type III Versus Type V Acromioclavicular Joint Injuriesa
| Postoperative | P Value | Change From Pre- to Postoperative | P Value | |
|---|---|---|---|---|
| Rowe | .40 | .23 | ||
| Type III | 90.2 ± 11.5 (83.8-96.6) | 25.1 ± 12.6 (17.5-32.7) | ||
| Type V | 86.4 ± 13.7 (79.4-93.4) | 19.4 ± 12.5 (12.7-26.0) | ||
| CM | .31 | .91 | ||
| Type III | 90.8 ± 8.2 (86.4-95.1) | 25.6 ± 13.9 (17.5-33.6) | ||
| Type V | 85.3 ± 19.5 (74.1-96.5) | 26.2 ± 18.2 (15.2-37.2) | ||
| SST | .62 | .89 | ||
| Type III | 9.7 ± 3.9 (7.7-11.7) | 3.3 ± 4.1 (1.2-5.4) | ||
| Type V | 9.1 ± 3.6 (7.2-10.9) | 3.1 ± 3.7 (1.2-5.0) |
aData are shown as mean ± SD (95% CI). CM, Constant-Murley; SST, Simple Shoulder Test.
Radiographic Outcomes
When looking at the ipsilateral shoulder, the preoperative CCD (19.9 ± 6.4 mm [95% CI, 18.2-21.5]) was significantly higher (P < .001) than the CCD at final follow-up (9.7 ± 4.0 mm [95% CI, 8.6-10.7]). There was no significant difference in the pre- to postoperative difference in the CCD between acute (10.9 ± 6.9 mm [95% CI, 8.3-13.5]) and chronic (8.6 ± 6.9 mm [95% CI, 5.9-11.4]) injuries (P = .23). As expected, when comparing type III (7.9 ± 5.7 mm [95% CI, 5.7-10.2]) and type V (12.0 ± 8.0 mm [95% CI, 9.1-14.9]) injuries, type V injuries showed a significantly higher pre- to postoperative difference in the CCD (P = .03).
When comparing the ipsilateral (injured) to the contralateral shoulder, the postoperative side-to-side difference in the CCD was 3.1 ± 2.7 mm (95% CI, 2.4-3.8) for all patients. There was no statistically significant difference in the postoperative side-to-side difference in the CCD when comparing acute (2.9 ± 2.3 mm [95% CI, 2.7-3.1]) and chronic (3.3 ± 3.1 mm [95% CI, 2.1-4.4]) injuries (P = .67). However, type III injuries (2.4 ± 1.9 mm [95% CI, 1.7-3.0]) had a statistically significantly smaller postoperative side-to-side difference in the CCD when compared with type V injuries (4.2 ± 3.4 mm [95% CI, 2.7-5.6]) (P = .02).
We could not identify a significant trend between the postoperative side-to-side difference in the CCD and the improvement of pre- to postoperative values for the ASES, Rowe, SST, and CM scores (P > .05).
Complications
A total of 11 patients (25.6%) were found to have either clinical or radiographic complications after surgery. Heterotopic ossification at or around the AC joint was the most common complication (n = 3; 7.0%); however, only 1 patient required debridement and distal clavicle excision for pain. Also, 2 of these patients had type V injuries, and all were chronic (>6 months from initial injury). Moreover, 2 other patients (4.7%) had deep infections requiring incision and drainage within the first postoperative month, while 1 patient had a superficial infection that resolved with antibiotics only. The 2 patients with infections requiring debridement had undergone previous shoulder surgery for either rotator cuff repair or debridement, one of which was an acute type III injury. The other infection requiring debridement was a chronic type V injury. AC joint osteoarthritis was observed in 3 patients, with only 1 requiring distal clavicle excision because of pain. All 3 had chronic injuries, with 2 of them being type III. An additional 2 patients had radiographic failure (recurrence of dislocation) within the first 8 weeks of surgery; however, both reported significant clinical improvement without requiring revision surgery. Both had type V injuries that were chronic. Overall, the complication rate was 26%; however, the reoperation rate was only 9%, with no patient requiring revision reconstruction.
Discussion
The most important finding of this study was that patients undergoing ACCR for acute and chronic type III and V AC joint injuries maintained significant improvement in clinical and radiographic outcomes at a minimum 2-year follow-up. Additionally, this study found that 81% of patients reached the SCB threshold for the ASES score while only 49% of patients met the PASS criteria. Within the limitations of our study design, we did not observe a statistically significant relationship between the postoperative side-to-side difference in the CCD and the degree of improvement in clinical outcome scores. These findings are consistent with other studies reporting on clinical and radiographic outcomes after ACCR using free tendon grafts.§
A previously published case series of 16 patients who underwent the ACCR technique showed similar improvement in shoulder function and radiographic findings after a mean follow-up of 21 months (range, 6-68 months).6 Compared with our longer term results, these results highlight the ability of this technique to maintain reduction and shoulder function for patients with type III and V injuries.6 Using a similar reconstruction technique, Millett et al25 showed excellent clinical outcome scores and the maintenance of AC joint reduction with a mean side-to-side difference in the CCD of 2.3 mm in 24 patients who underwent treatment for type III and V injuries. Similar results were achieved by Parnes et al,29 who reported on 12 patients treated with an arthroscopic ACCR technique using double-bundle coracoid cerclage for type V injuries. Although our findings mirror other studies on clinical and radiographic outcomes after ACCR, prior studies were limited to a smaller patient population and shorter duration of follow-up.‖ In addition, this is the first study that we are aware of that demonstrates the percentage of patients who reached the SCB and PASS for AC joint reconstruction. Nearly half of patients achieved the designated PASS threshold, which was similarly found for rotator cuff surgery.9
A biomechanical explanation for these favorable clinical and radiographic outcomes may be the ability of this technique to restore native AC joint properties more effectively when compared with coracoacromial ligament transfer techniques.8,15,20,24 This biomechanical advantage has been supported by clinical studies comparing ACCR using free tendon grafts with a modified Weaver-Dunn procedure.17,31 A prospective study by Tauber et al31 demonstrated significantly superior functional and radiographic outcomes in patients who underwent ACCR using a semitendinosus graft at a mean follow-up of 3 years. These findings were confirmed by Hegazy et al17 in a similar fashion.
As radiographic loss of reduction remains a major challenge in the treatment of high-grade AC joint injuries, surgical techniques addressing both the AC capsule and coracoclavicular ligament have garnered attention in the current literature, aiming to restore their synergistic effect and to create a repair site with maximum stability.4,10,11,18,27 Thus, the ACCR technique reported on in this study utilized the longer limb of the free tendon allograft to reinforce the superior and posterior parts of the repaired AC capsule.6 Ensuring the integrity of the AC capsule by additional augmentation leads to improved translational and rotational stability, as demonstrated in several biomechanical investigations.11,27
However, the correlation between the maintenance of reduction and clinical outcomes is still poorly understood. Loss of reduction in patients treated with coracoacromial ligament transfer techniques has been reported to occur in up to 24% of cases, being associated with inferior functional outcomes.34,35 Even with additional augmentation, transfer of the coracoacromial ligament does not predictably maintain reduction of the reconstructed AC joint.19 As the ACCR technique has been biomechanically proven to better restore native joint properties,8,15,20,24 loss of reduction may be less likely to occur. Our study demonstrated that there was no correlation between functional outcomes and the maintenance of reduction, inferred from the postoperative side-to-side difference in the CCD. However, studies with larger patient populations, longer duration of follow-up, and more complete imaging (axillary and weighted views) are needed to determine to what extent loss of reduction may impair functional outcomes.
This study also found a complication rate of 26% at 2-year follow-up. This is similar to the findings of Millett et al,25 who found a complication rate of 25.8%. However, unlike their study, clavicle fracture and graft failure were not the most common modes of revision in the current cohort. Our study found that heterotopic ossification and osteoarthritis of the AC joint were the most common complications after surgery, with all occurring in patients whose surgery was greater than 6 months from injury. This supports that fixation occurring before 6 months may play a role in delaying degeneration of the AC joint.
There are several limitations to this study. Although outcomes were collected prospectively, data were reviewed retrospectively, which could create selection bias. Moreover, a considerable number of patients either did not have 2-year follow-up or could not be reached, potentially leading to transfer bias. In addition, patients did not have standard weightbearing or axillary views of the shoulder at follow-up. This may have resulted in missed horizontal or dynamic instability, which has more recently been identified as a potential cause for persistent pain and revision. It also limits the current study’s findings that maintained reduction did not correlate with clinical outcomes. Another limitation was that the MCID, SCB, and PASS thresholds that were used may not be appropriate for patients with AC joint injuries.9 As these metrics are derived from a rotator cuff tear population, it may not reflect those of patients with AC joint injuries.9 This was felt to be the closest population available for utilization; however, further studies are required to identify the threshold for the current patient cohort.25 Another limitation was the definition of acute and chronic injuries. Studies have varied in defining acute and chronic injures, with the lack of a true definition in the literature.12,25 This is likely because of the variation in nonoperative management. Given that all patients in this population underwent a minimum of 1 month nonoperative management, 6 months was chosen to separate acute and chronic groups. While this may not reflect more common definitions in the literature, our findings of greater complications at 6 months may give insight into the risks of delayed treatment. This study also did not include a control group (eg, nonoperative treatment) to compare the increased benefit of ACCR. Although all patients underwent a trial of nonoperative treatment, further studies are needed to truly identify whether greater improvement is seen with operative management. This is especially true for type III injuries, which can often be treated nonoperatively.3 Last, the patient population in the current study was older than the younger athletic population in whom these injuries have been described,3,13 making the results possibly less generalizable.
Conclusion
Patients undergoing ACCR using free tendon allografts for acute and chronic type III and V AC joint injuries maintained significant improvement in clinical and radiographic outcomes at a minimum 2-year follow-up. Additionally, 81% of patients reached the SCB after surgical reconstruction. Future studies comparing nonoperative treatment, as well as including weighted and axillary views, may give better insight into the added benefit of the ACCR technique.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.A.A. has received educational support from Arthrex and DonJoy; has received consulting fees from Biorez, Biomet, and DePuy; and has stock/stock options in Biorez. A.D.M. has received consulting fees from Arthrex and Astellas Pharma, research support from Arthrex, and honoraria from Arthrosurface. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the UConn Health Institutional Review Board (No. 17-066-3.2).
References
- 1. Baran S, Belisle JG, Granger EK, Tashjian RZ. Functional and radiographic outcomes after allograft anatomic coracoclavicular ligament reconstruction. J Orthop Trauma. 2018;32(4):204–210. [DOI] [PubMed] [Google Scholar]
- 2. Beaton D, Richards R. Assessing the reliability and responsiveness of 5 shoulder questionnaires. J Shoulder Elbow Surg. 1998;7:565–572. [DOI] [PubMed] [Google Scholar]
- 3. Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29(2):387–397. [DOI] [PubMed] [Google Scholar]
- 4. Beitzel K, Obopilwe E, Apostolakos J, et al. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med. 2014;42(9):2141–2148. [DOI] [PubMed] [Google Scholar]
- 5. Boffano M, Mortera S, Wafa H, Piana R. The surgical treatment of acromioclavicular joint injuries. EFORT Open Rev. 2017;2(10):432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2 suppl):37–46. [DOI] [PubMed] [Google Scholar]
- 7. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 8. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32(8):1929–1936. [DOI] [PubMed] [Google Scholar]
- 9. Cvetanovich GL, Gowd AK, Liu JN, et al. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(5):939–948. [DOI] [PubMed] [Google Scholar]
- 10. Debski RE, Parsons IM, Woo SL, Fu F. Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am. 2001;83(9):1344–1351. [DOI] [PubMed] [Google Scholar]
- 11. Dyrna F, Imhoff FB, Haller B, et al. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med. 2018;46(14):3471–3479. [DOI] [PubMed] [Google Scholar]
- 12. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2013;42(1):235–241. [DOI] [PubMed] [Google Scholar]
- 13. Frank RM, Cotter EJ, Leroux TS, Romeo AA. Acromioclavicular joint injuries: evidence-based treatment. J Am Acad Orthop Surg. 2019;27(17):e775–e788. [DOI] [PubMed] [Google Scholar]
- 14. Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the Simple Shoulder Test: psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–267. [DOI] [PubMed] [Google Scholar]
- 15. Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33(11):1723–1728. [DOI] [PubMed] [Google Scholar]
- 16. Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A. Research pearls: the significance of statistics and perils of pooling. Part 1: clinical versus statistical significance. Arthroscopy. 2017;33(6):1102–1112. [DOI] [PubMed] [Google Scholar]
- 17. Hegazy G, Safwat H, Seddik M, Al-Shal EA, Al-Sebai I, Negm M. Modified Weaver-Dunn procedure versus the use of semitendinosus autogenous tendon graft for acromioclavicular joint reconstruction. Open Orthop J. 2016;10:166–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Klimciewicz JJ, Williams GR, Sher JS, Karduna A, Des Jardins J, Iannotti JP. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg. 1999;8(2):119–124. [DOI] [PubMed] [Google Scholar]
- 19. LaPrade RF, Hilger B. Coracoclavicular ligament reconstruction using a semitendinosus graft for failed acromioclavicular separation surgery. Arthroscopy. 2005;21(10):1277. [DOI] [PubMed] [Google Scholar]
- 20. Lee SJ, Nicholas SJ, Akizuki KH, McHugh MP, Kremenic IJ, Ben-Avi S. Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med. 2003;31(5):648–655. [DOI] [PubMed] [Google Scholar]
- 21. Lippitt SB, Harryman DT, Matsen FA. A practical tool for evaluating function: the Simple Shoulder Test In: Matsen FA, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, Illinois: American Academy of Orthopaedic Surgeons; 1993:501–518. [Google Scholar]
- 22. Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35(2):316–329. [DOI] [PubMed] [Google Scholar]
- 23. Mazzocca AD, Conway JE, Johnson S, et al. The anatomic coracoclavicular ligament reconstruction. Oper Tech Sports Med. 2004;12(1):56–61. [Google Scholar]
- 24. Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2):236–246. [DOI] [PubMed] [Google Scholar]
- 25. Millett PJ, Horan MP, Warth RJ. Two-year outcomes after primary anatomic coracoclavicular ligament reconstruction. Arthroscopy. 2015;31(10):1962–1973. [DOI] [PubMed] [Google Scholar]
- 26. Moatshe G, Kruckeberg BM, Chahla J, et al. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthroscopy. 2018;34(6):1979–1995. [DOI] [PubMed] [Google Scholar]
- 27. Morikawa D, Dyrna F, Cote MP, et al. Repair of the entire superior acromioclavicular ligament complex best restores posterior translation and rotational stability [published online October 10, 2018]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-018-5205-y [DOI] [PubMed] [Google Scholar]
- 28. Pallis M, Cameron KL, Svoboda SJ, Owens BD. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med. 2012;40(9):2072–2077. [DOI] [PubMed] [Google Scholar]
- 29. Parnes N, Friedman D, Phillips C, Carey P. Outcome after arthroscopic reconstruction of the coracoclavicular ligaments using a double-bundle coracoid cerclage technique. Arthroscopy. 2015;31(10):1933–1940. [DOI] [PubMed] [Google Scholar]
- 30. Richards R, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. [DOI] [PubMed] [Google Scholar]
- 31. Tauber M, Gordon K, Koller H, Fox M, Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37(1):181–190. [DOI] [PubMed] [Google Scholar]
- 32. Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44(2):482–489. [DOI] [PubMed] [Google Scholar]
- 33. Thigpen CA, Shanley E, Momaya AM, et al. Validity and responsiveness of the Single Alpha-Numeric Evaluation for shoulder patients. Am J Sports Med. 2018;46(14):3480–3485. [DOI] [PubMed] [Google Scholar]
- 34. Tienen TG, Oyen JF, Eggen PJ. A modified technique of reconstruction for complete acromioclavicular dislocation: a prospective study. Am J Sports Med. 2003;31(5):655–659. [DOI] [PubMed] [Google Scholar]
- 35. Weinstein DM, McCann PD, McIlveen SJ, Flatow EL, Bigliani LU. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23(3):324–331. [DOI] [PubMed] [Google Scholar]
- 36. Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What change in American Shoulder and Elbow Surgeons score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016;474(12):2672–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Am J Sports Med. 1999;27(2):214–221. [DOI] [PubMed] [Google Scholar]
- 38. Yoo JC, Ahn JH, Yoon JR, Yang JH. Clinical results of single-tunnel coracoclavicular ligament reconstruction using autogenous semitendinosus tendon. Am J Sports Med. 2010;38(5):950–957. [DOI] [PubMed] [Google Scholar]
- 39. Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med. 1971;112(3):493–506. [DOI] [PubMed] [Google Scholar]
- 40. Zhu Y, Hsueh P, Zeng B, et al. A prospective study of coracoclavicular ligament reconstruction with autogenous peroneus longus tendon for acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2018;27(6):e178–e188. [DOI] [PubMed] [Google Scholar]
- 41. Zumstein MA, Schiessl P, Ambuehl B, et al. New quantitative radiographic parameters for vertical and horizontal instability in acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):125–135. [DOI] [PMC free article] [PubMed] [Google Scholar]